Refeeding Syndrome Objectives To discuss the pathophysiology of
Refeeding Syndrome
Objectives • To discuss the pathophysiology of refeeding syndrome • To diagnose refeeding syndrome • To discuss prevention and management of refeeding syndrome
Definition of refeeding syndrome • Electrolyte abnormality(ies) due to refeeding which result to the following complications: respiratory failure, cardiac arrhythmias, and encephalopathy which may lead to death when not immediately diagnosed and managed. • The main electrolyte abnormality is usually hypophosphatemia • This condition usually occurs in severely malnourished patients Stanga Z. Sobotka L. Refeeding syndrome. Basics in Clinical Nutrition 4 th ed 2011; Galen Publishing, Czech Republic: 427 -32.
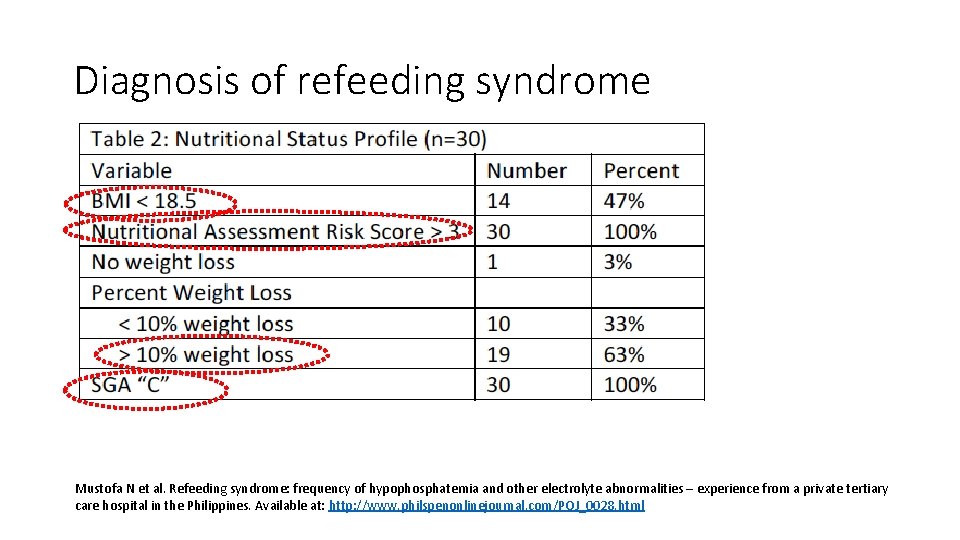
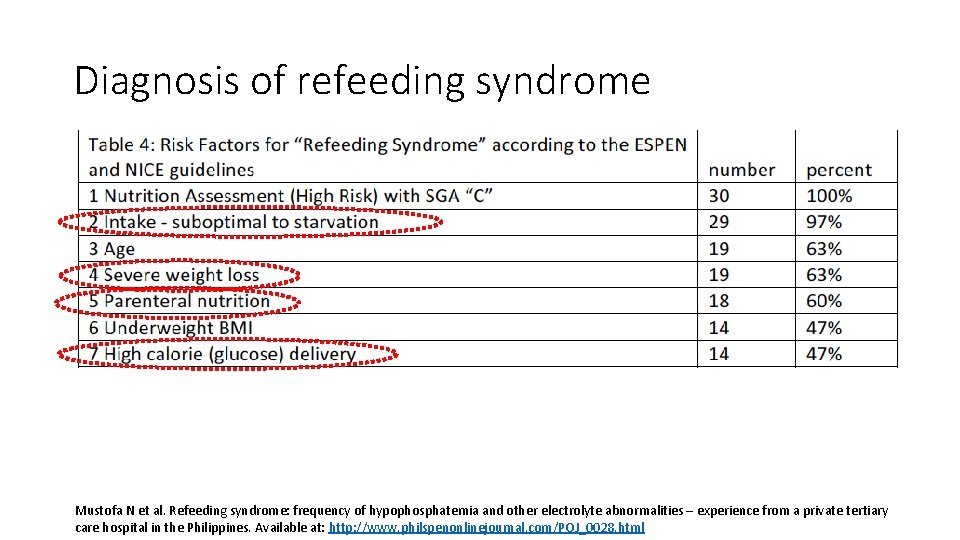
Diagnosis of refeeding syndrome Mustofa N et al. Refeeding syndrome: frequency of hypophosphatemia and other electrolyte abnormalities – experience from a private tertiary care hospital in the Philippines. Available at: http: //www. philspenonlinejournal. com/POJ_0028. html
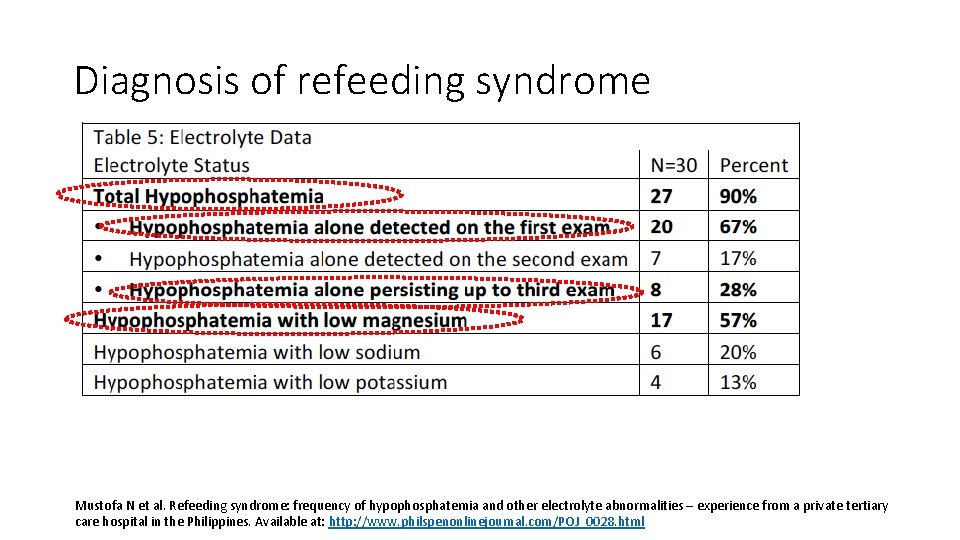
Diagnosis of refeeding syndrome Mustofa N et al. Refeeding syndrome: frequency of hypophosphatemia and other electrolyte abnormalities – experience from a private tertiary care hospital in the Philippines. Available at: http: //www. philspenonlinejournal. com/POJ_0028. html
Diagnosis of refeeding syndrome Mustofa N et al. Refeeding syndrome: frequency of hypophosphatemia and other electrolyte abnormalities – experience from a private tertiary care hospital in the Philippines. Available at: http: //www. philspenonlinejournal. com/POJ_0028. html
Diagnosis of refeeding syndrome • High index of suspicion: “This problem may not be only cardiac. . . ” • Severely malnourished • Elderly • On parenteral nutrition with/without high glucose load • When you have all of the above – request for phosphate and magnesium blood test
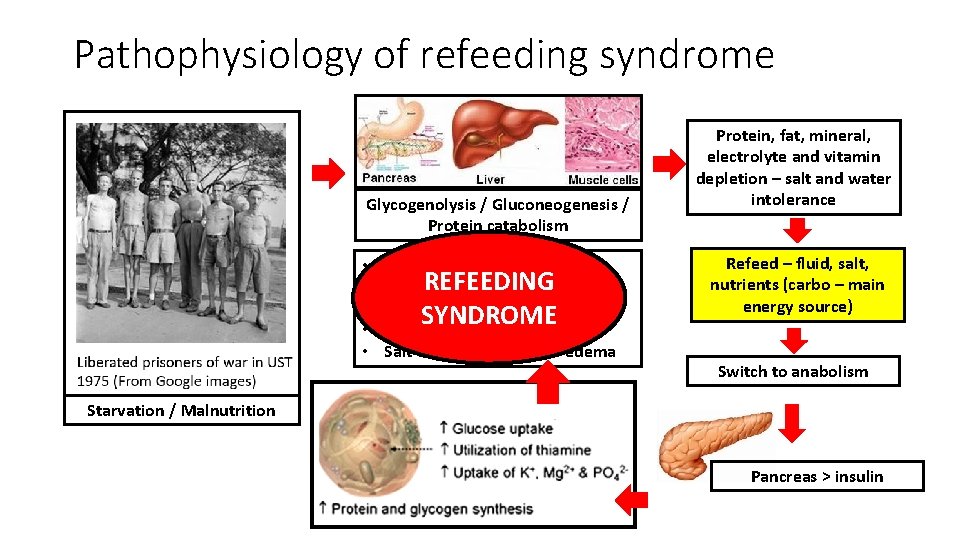
Pathophysiology of refeeding syndrome Glycogenolysis / Gluconeogenesis / Protein catabolism • • • Hypophosphatemia REFEEDING Hypomagnesemia SYNDROME Thiamine deficiency Salt & water retention - edema Protein, fat, mineral, electrolyte and vitamin depletion – salt and water intolerance Refeed – fluid, salt, nutrients (carbo – main energy source) Switch to anabolism Starvation / Malnutrition Pancreas > insulin
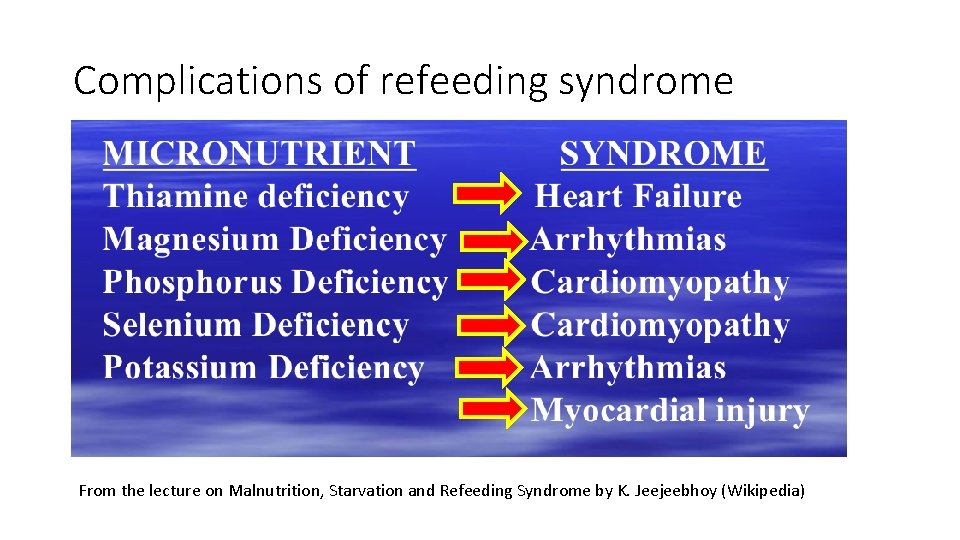
Complications of refeeding syndrome From the lecture on Malnutrition, Starvation and Refeeding Syndrome by K. Jeejeebhoy (Wikipedia)
Refeeding syndrome in the Philippines
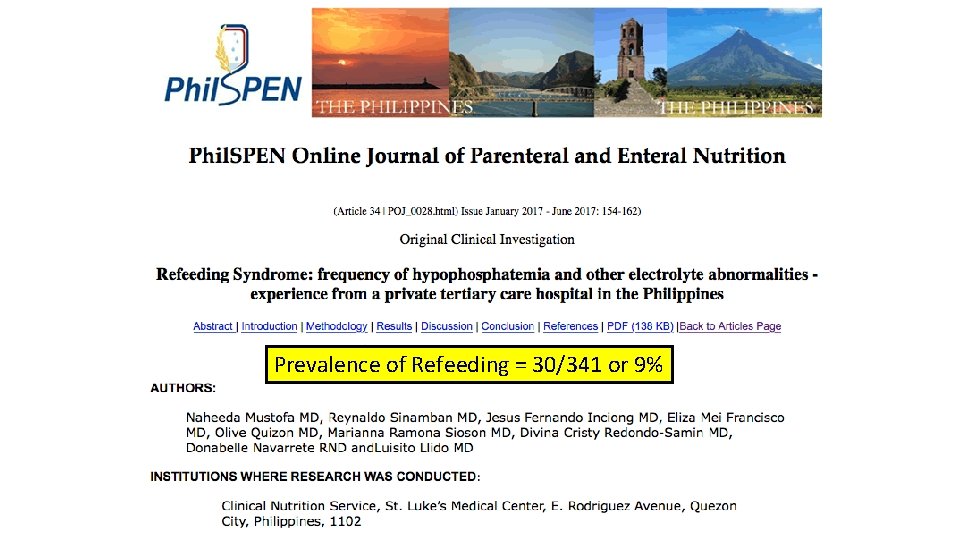
Prevalence of Refeeding = 30/341 or 9%
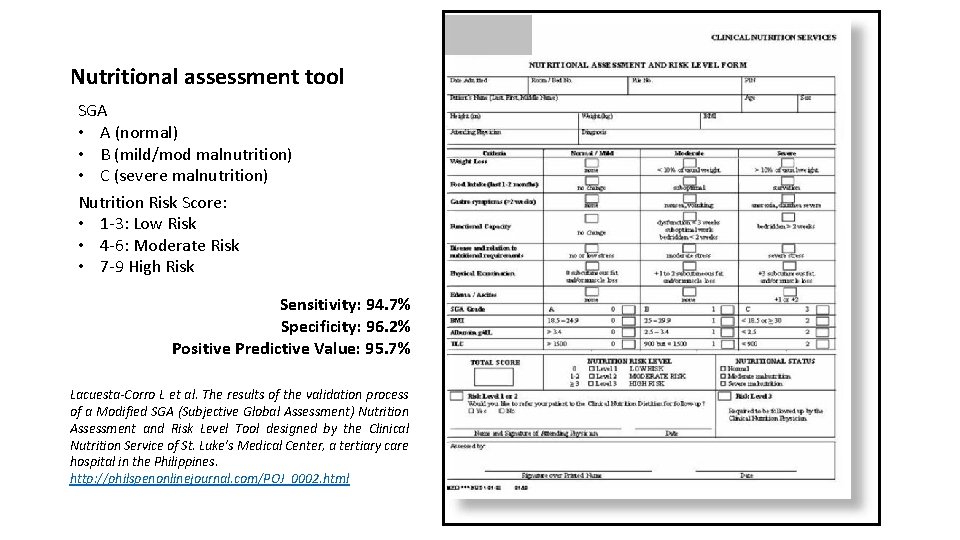
Nutritional assessment tool SGA • A (normal) • B (mild/mod malnutrition) • C (severe malnutrition) Nutrition Risk Score: • 1 -3: Low Risk • 4 -6: Moderate Risk • 7 -9 High Risk Sensitivity: 94. 7% Specificity: 96. 2% Positive Predictive Value: 95. 7% Lacuesta-Corro L et al. The results of the validation process of a Modified SGA (Subjective Global Assessment) Nutrition Assessment and Risk Level Tool designed by the Clinical Nutrition Service of St. Luke’s Medical Center, a tertiary care hospital in the Philippines. http: //philspenonlinejournal. com/POJ_0002. html
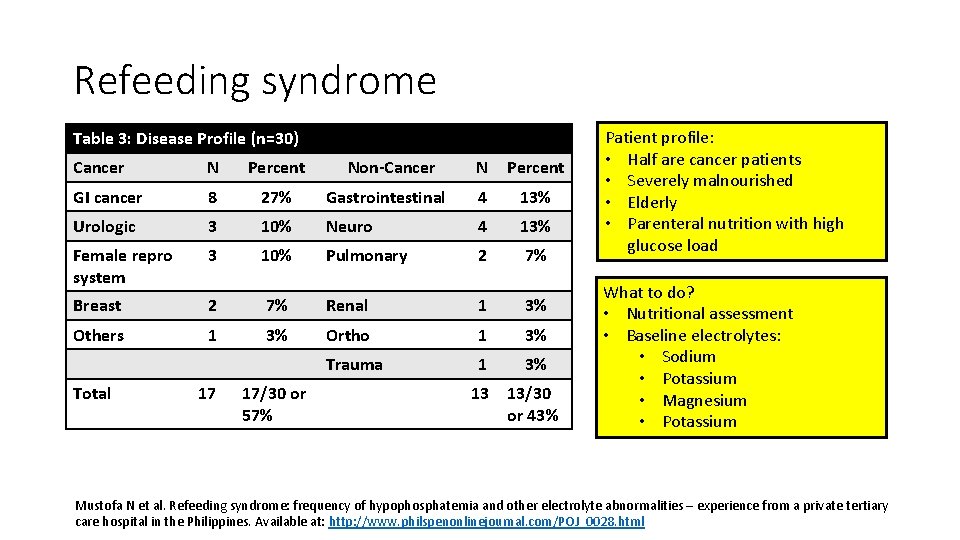
Refeeding syndrome Table 3: Disease Profile (n=30) Cancer N Percent GI cancer 8 27% Urologic 3 Female repro system N Percent Gastrointestinal 4 13% 10% Neuro 4 13% 3 10% Pulmonary 2 7% Breast 2 7% Renal 1 3% Others 1 3% Ortho 1 3% Trauma 1 3% Total 17 17/30 or 57% Non-Cancer 13 13/30 or 43% Patient profile: • Half are cancer patients • Severely malnourished • Elderly • Parenteral nutrition with high glucose load What to do? • Nutritional assessment • Baseline electrolytes: • Sodium • Potassium • Magnesium • Potassium Mustofa N et al. Refeeding syndrome: frequency of hypophosphatemia and other electrolyte abnormalities – experience from a private tertiary care hospital in the Philippines. Available at: http: //www. philspenonlinejournal. com/POJ_0028. html
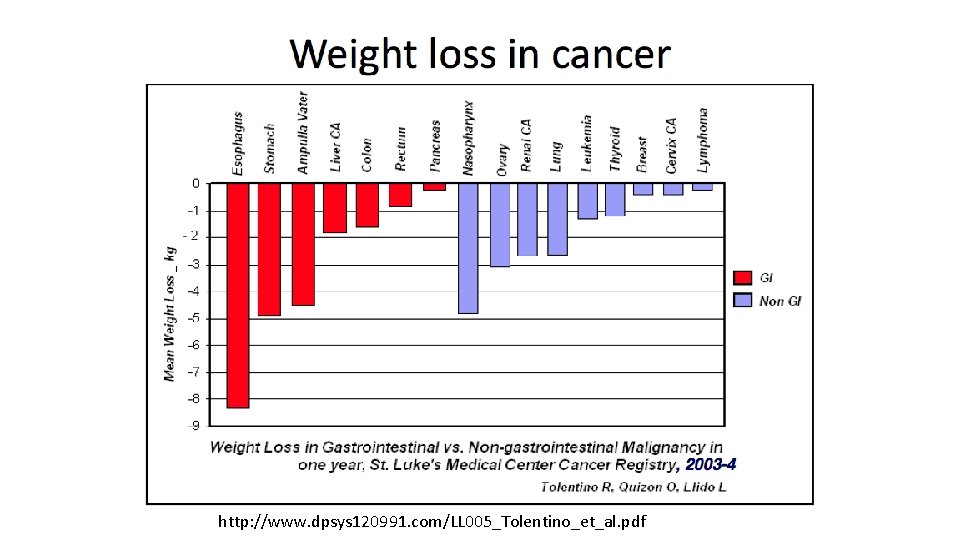
http: //www. dpsys 120991. com/LL 005_Tolentino_et_al. pdf

Outcomes of refeeding syndrome Outcome Number (%) Length of Stay • 1 -7 days 11 (37%) • 8 -15 days 12 (40%) • 16 -25 days 5 (17%) • 26 -35 days 4 (13%) ICU admission 6 (29%) Ventilator support 10 (33%) Arrhythmias 7 (23%) Mortality 5 (17%) Discharged improved 23 (83%) Discharged unimproved 2 (7%) Mustofa N et al. Refeeding syndrome: frequency of hypophosphatemia and other electrolyte abnormalities – experience from a private tertiary care hospital in the Philippines. Available at: http: //www. philspenonlinejournal. com/POJ_0028. html
Management of Refeeding
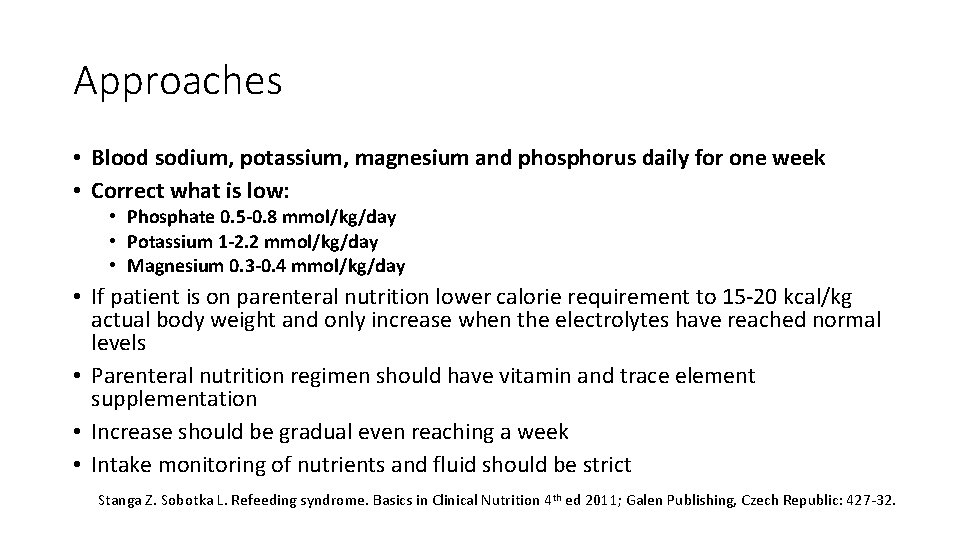
Approaches • Blood sodium, potassium, magnesium and phosphorus daily for one week • Correct what is low: • Phosphate 0. 5 -0. 8 mmol/kg/day • Potassium 1 -2. 2 mmol/kg/day • Magnesium 0. 3 -0. 4 mmol/kg/day • If patient is on parenteral nutrition lower calorie requirement to 15 -20 kcal/kg actual body weight and only increase when the electrolytes have reached normal levels • Parenteral nutrition regimen should have vitamin and trace element supplementation • Increase should be gradual even reaching a week • Intake monitoring of nutrients and fluid should be strict Stanga Z. Sobotka L. Refeeding syndrome. Basics in Clinical Nutrition 4 th ed 2011; Galen Publishing, Czech Republic: 427 -32.
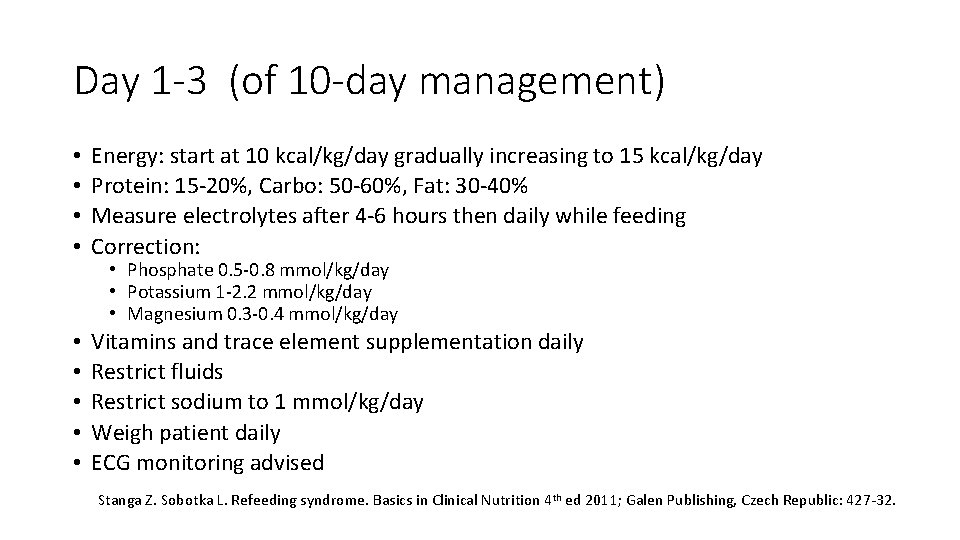
Day 1 -3 (of 10 -day management) • • Energy: start at 10 kcal/kg/day gradually increasing to 15 kcal/kg/day Protein: 15 -20%, Carbo: 50 -60%, Fat: 30 -40% Measure electrolytes after 4 -6 hours then daily while feeding Correction: • • • Vitamins and trace element supplementation daily Restrict fluids Restrict sodium to 1 mmol/kg/day Weigh patient daily ECG monitoring advised • Phosphate 0. 5 -0. 8 mmol/kg/day • Potassium 1 -2. 2 mmol/kg/day • Magnesium 0. 3 -0. 4 mmol/kg/day Stanga Z. Sobotka L. Refeeding syndrome. Basics in Clinical Nutrition 4 th ed 2011; Galen Publishing, Czech Republic: 427 -32.
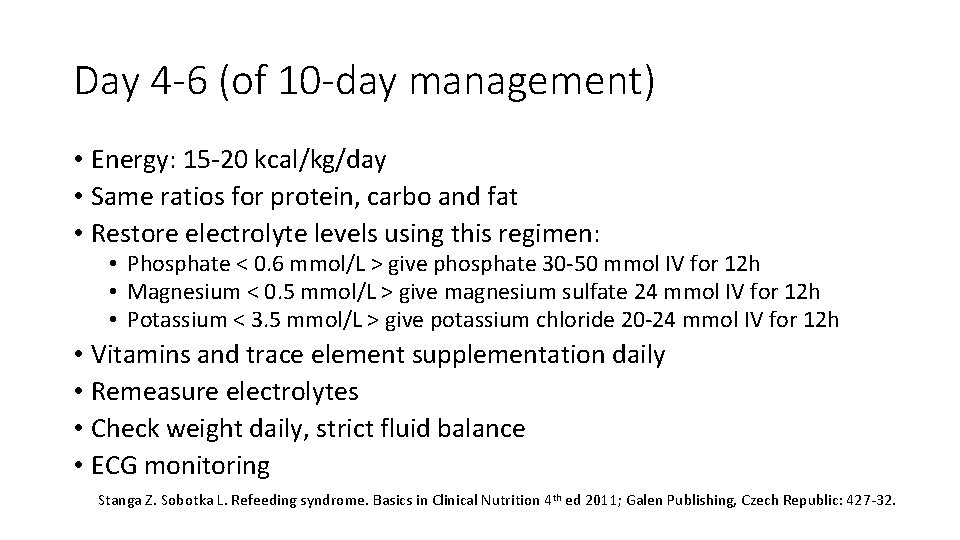
Day 4 -6 (of 10 -day management) • Energy: 15 -20 kcal/kg/day • Same ratios for protein, carbo and fat • Restore electrolyte levels using this regimen: • Phosphate < 0. 6 mmol/L > give phosphate 30 -50 mmol IV for 12 h • Magnesium < 0. 5 mmol/L > give magnesium sulfate 24 mmol IV for 12 h • Potassium < 3. 5 mmol/L > give potassium chloride 20 -24 mmol IV for 12 h • Vitamins and trace element supplementation daily • Remeasure electrolytes • Check weight daily, strict fluid balance • ECG monitoring Stanga Z. Sobotka L. Refeeding syndrome. Basics in Clinical Nutrition 4 th ed 2011; Galen Publishing, Czech Republic: 427 -32.
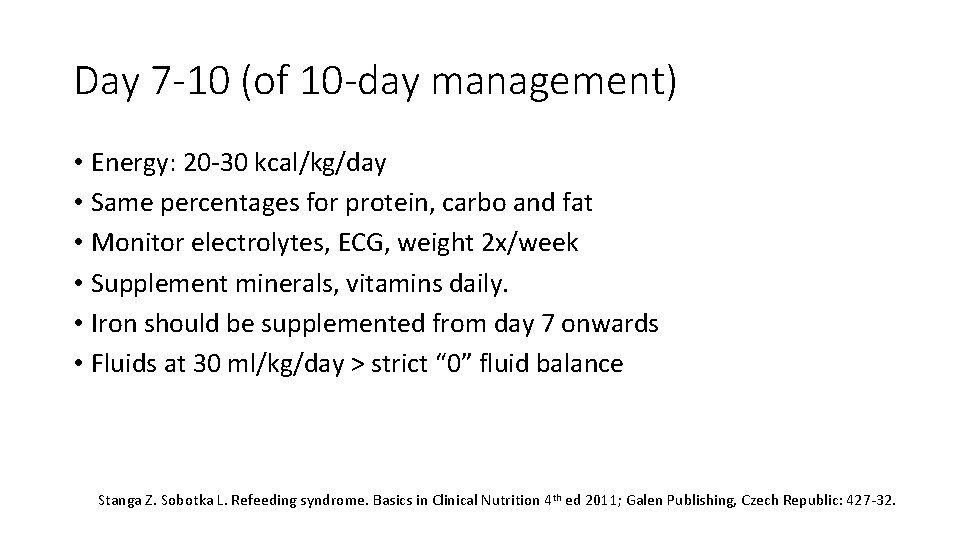
Day 7 -10 (of 10 -day management) • Energy: 20 -30 kcal/kg/day • Same percentages for protein, carbo and fat • Monitor electrolytes, ECG, weight 2 x/week • Supplement minerals, vitamins daily. • Iron should be supplemented from day 7 onwards • Fluids at 30 ml/kg/day > strict “ 0” fluid balance Stanga Z. Sobotka L. Refeeding syndrome. Basics in Clinical Nutrition 4 th ed 2011; Galen Publishing, Czech Republic: 427 -32.
Recap • Severely malnourished patient • Check the following blood values: • Na, K, Cl, P, Mag (= Check all four!) • When phosphate and/or magnesium is low, • Diagnosis = Refeeding • Start the 10 -day management for refeeding – “Start very small and very slow” > very gradual increase until goals are reached on day 10”
Thank You
- Slides: 22