Reducing Hospital Admissions Reflecting on your Practice Mary








- Slides: 55
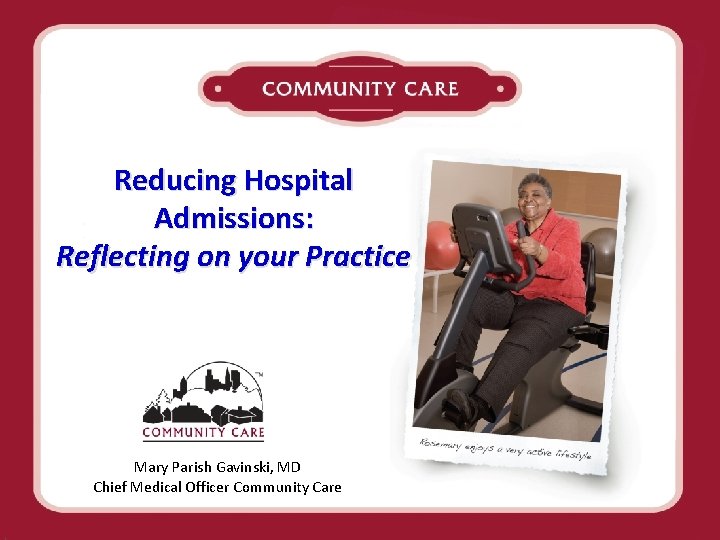
Reducing Hospital Admissions: Reflecting on your Practice Mary Parish Gavinski, MD Chief Medical Officer Community Care

Community Care, Inc Programs Current Census Integrated Dual Programs: 1342 members PACE: 665 members (in 2 counties) Partnership (SNP): 677 members (in 9 counties) Family Care (MLTC): 9, 381 members (in 11 Counties)
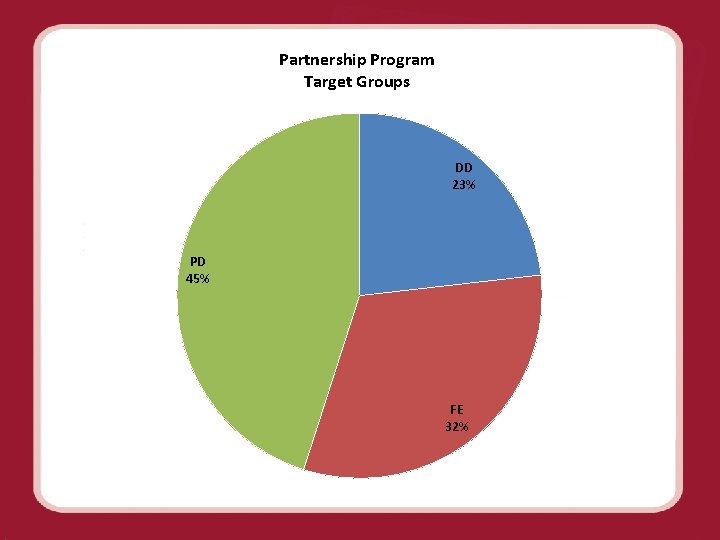
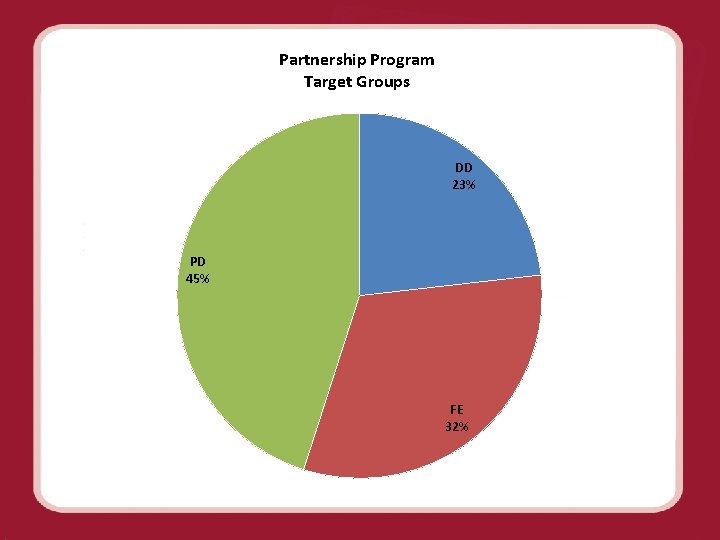
Partnership Program Target Groups DD 23% PD 45% FE 32%

CMS Partnership for Patients • Nearly one in five Medicare patients discharged from the hospital is readmitted within 30 days. • That’s approximately 2. 6 million seniors at a cost of over $26 billion every year.
CMS Partnership for Patients • Launched in April 2011 by CMS as a publicprivate partnership • Supports physicians, nurses and other clinicians working in and out of hospitals to make patient care safer and to support effective transitions of patients from hospitals to other settings. • The Community-based Care Transitions Program tests models for improving care transitions in order to reduce hospital readmissions.
CMS Partnership for Patients The two goals of the CMS partnership are to: ü Keep patients from getting injured or sicker. By the end of 2013, preventable hospital-acquired conditions would decrease by 40% compared to 2010. Achieving this goal would mean approximately 1. 8 million fewer injuries to patients with more than 60, 000 lives saved over three years. ü Help patients heal without complication. By the end of 2013, preventable complications during a transition from one care setting to another would be decreased so that all hospital readmissions would be reduced by 20% compared to 2010. Achieving this goal would mean more than 1. 6 million patients would recover from illness without suffering a preventable complication requiring re-hospitalization within 30 days of discharge.
The Project • CMS Requirements for Special Needs Plans (SNP) – Quality Improvement Project or QIP – Chronic Care Improvement Program Project or CCIP • WI DHS requirements for Managed Care Organizations (MCO) – Long Term Care Project or PIP – In addition, for those organizations with acute/primary care services, an Acute/Primary Care Project PIP- we used the QIP
Community Care’s Reflective Practice Hospital Analysis Quality Improvement Project (QIP) • Supports a national Health and Human Services initiative known as: – Partnership for Patients • Required focus for the QIP is – “Decreasing Hospital Readmissions” • A readmission is defined as a hospitalization within 30 days of discharge from a hospital • 3 year project for Partnership (we added PACE internally) • Project Goal: reduce readmissions by 3% • Intervention: – Team Reflective Practice Hospital Analysis
Background on QIP • Follow the QI cycle of Plan, Do, Study, Act • Aligned with national health initiatives • Consolidated several initiatives on reducing admissions/readmissions in the agency

Community Care QIP • Hospital readmission rate defined as hospitalization within 30 days of the index hospitalization discharge date. • CCI overall Partnership Program rate for Jan-June 2012 was 29. 2% • Initial rate for project target counties was 32% • Affects 211 members
Community Care QIP • Organizational goal is to reduce readmissions 3% • Initial intervention is for Interdisciplinary Team to use Reflective Practice and a Hospital Discharge Summary Form tool to analyze each admission or readmission • Borrowed a similar form used by another MCO reduced readmissions.

Community Care Reflective Practice Hospital Analysis*: A strategy to enhance critical thinking and problem Solving * Thanks to Cathy Rapp- CCI*
What is reflection “Active, persistent and careful consideration of belief, knowledge, or experience. ” “Thinking with a purpose. ” Dewey. “Thinking back on what we’ve done…to discover how our ‘knowing in action’ may have contributed to an unexpected outcome. ” Schoen. “A process of reviewing an experience of practice in order to describe, analyze, evaluate and so inform learning about practice. ” practice. Reid
What is reflective practice? Process that connects what we know, with what we experience, and what we learn from those experiences. Purposeful approach to thinking about our clinical practice. Goal is to move from “reflecting on action” (past tense), to “reflecting in action” (in the moment). Schoen
The processes of reflection Ø Awareness of an event, situation, experience that bears examination – causes discomfort Ø Critical analysis of the situation Ø Openness to new information and perspectives Ø Thoughtful examination of the experience Ø Development of a new perspective ü Changes in thoughts , feelings, actions
Reflective Practice Frameworks • Simply a guideline for approaching “how” we do reflection. • Provide a systematic approach to the process • Key components of any framework: – Description of what happened – Evaluation of that event – Actions that occur as a result of the reflection
Why Reflective Practice at CCI Deepen critical thinking and problem solving skills Enhance teamwork, professional relationships Improve our clinical practice Enhance member outcomes
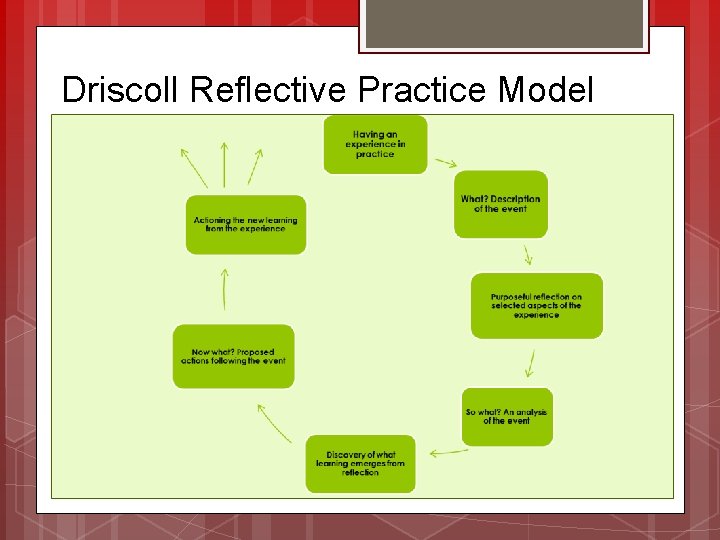
The CCI Reflective Practice Model Driscoll’s What A So model happened? clear description of the event what? What went well? What didn’t go well? What are the key learnings based on the analysis Now What? What will we do differently (or the same) based on the analysis? What actions do we need to take based on analysis?
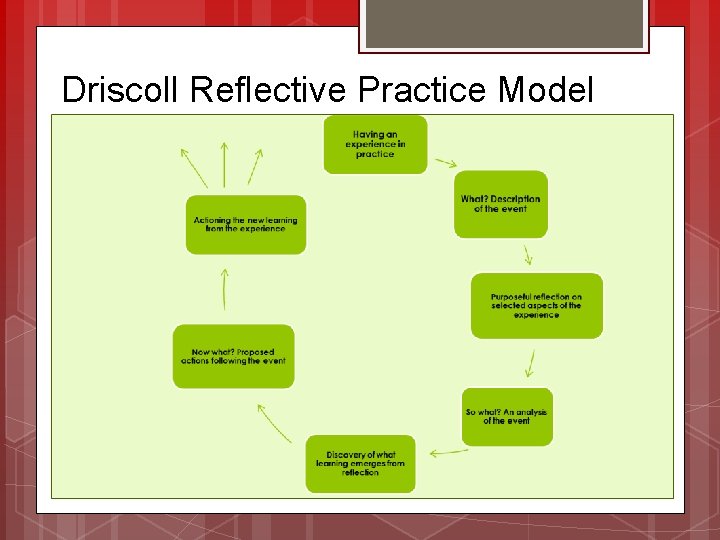
Driscoll Reflective Practice Model

Facilitating Reflective Practice Create a safe place to share thoughts and ideas during team meeting Core practices Stay neutral listen actively Ask questions Synthesize ideas Paraphrase
Core Practices (cont. ) Stay on track Test assumptions Collect and record all ideas Give and receive feedback (how is the session going? ) Provide summaries
Action plan Make the RPHA conversations a routine process at your site Ask questions to stimulate thought and conversation. Contribute. Summarize actions and next steps. Share key learnings as appropriate.
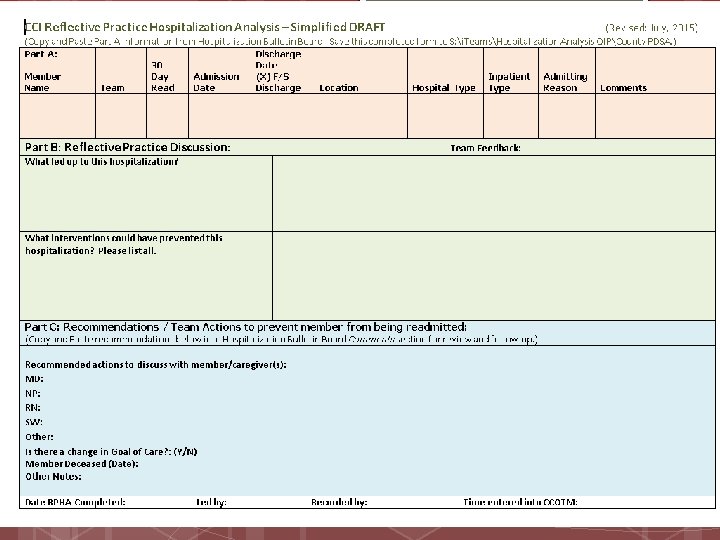
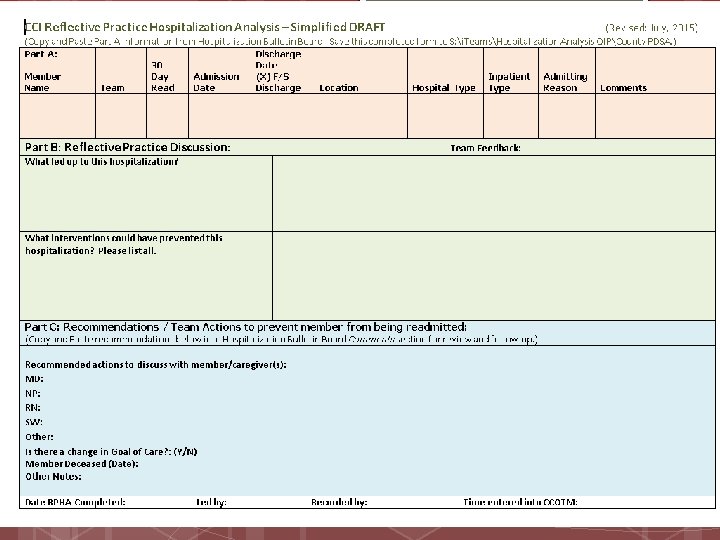
Community Care QIP • The form is a vehicle for facilitating a case analysis like a root cause analysis • Will foster understanding of what could have prevented the hospitalization • Will help to collect information on what trends we have with readmissions
PDSA 1 • One county was chosen as the pilot site for our first QIP PDSA • Staff were trained on Reflective Practice, the use of the tool and four hospital analysis processes were completed • Feedback included: difficulty pulling the team thru this new process; difficulties making the process a priority at every team meeting; and specific form changes and modifications • From a quality perspective, it was determined the process was still being refined and more research, support, and analysis was needed.



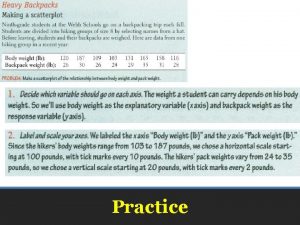
Community Care Reflective Practice Hospital Analysis*: Practice
Practice • Divide into groups of four or five • Take a “discipline card” that is not your discipline if possible. • Those of you with facilitator will lead the discussion using the questions in part C • The rest of you will follow the information inside your discipline or team card. • Before you begin, take a minute and read the case, your discipline card and try to reflect on a similar case you may have had. • Ad lib using the attributes of your card.
Scenario 1. What occurred leading up to hospitalization. 2. What went well with this member (related to the events pre-hospitalization) 3. What could have been done differently to prevent this hospitalization 4. Key learnings about this case 5. What is our action plan to prevent this member from being rehospitalized
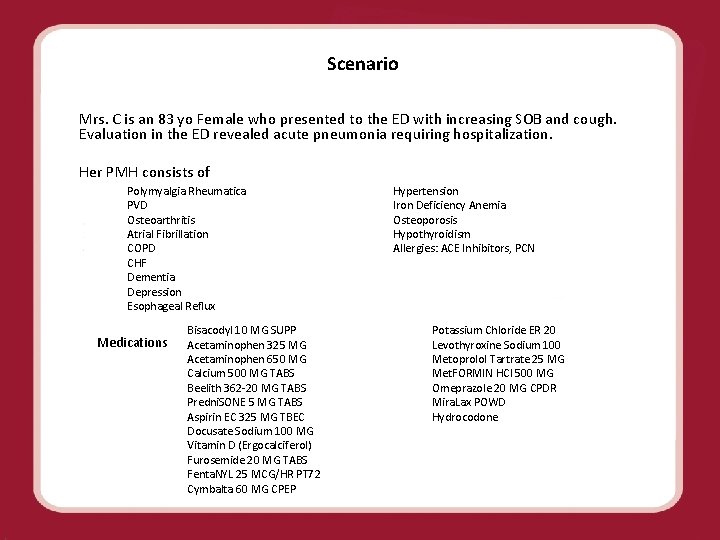
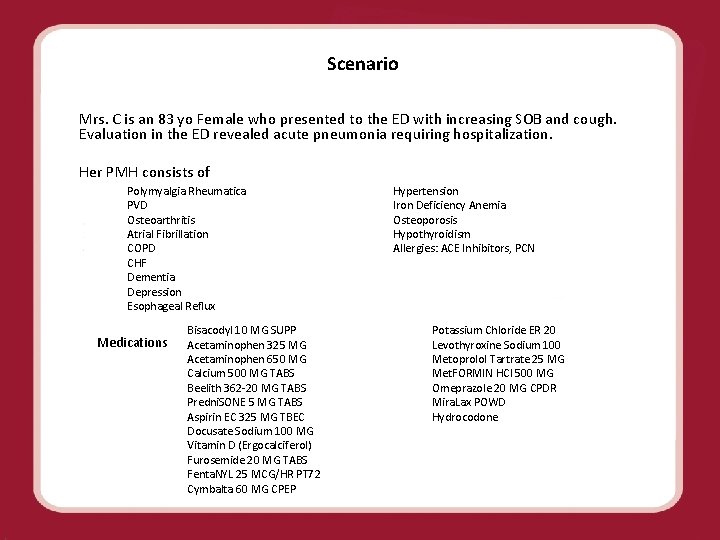
Scenario Mrs. C is an 83 yo Female who presented to the ED with increasing SOB and cough. Evaluation in the ED revealed acute pneumonia requiring hospitalization. Her PMH consists of Polymyalgia Rheumatica PVD Osteoarthritis Atrial Fibrillation COPD CHF Dementia Depression Esophageal Reflux Medications Bisacodyl 10 MG SUPP Acetaminophen 325 MG Acetaminophen 650 MG Calcium 500 MG TABS Beelith 362 -20 MG TABS Predni. SONE 5 MG TABS Aspirin EC 325 MG TBEC Docusate Sodium 100 MG Vitamin D (Ergocalciferol) Furosemide 20 MG TABS Fenta. NYL 25 MCG/HR PT 72 Cymbalta 60 MG CPEP Hypertension Iron Deficiency Anemia Osteoporosis Hypothyroidism Allergies: ACE Inhibitors, PCN Potassium Chloride ER 20 Levothyroxine Sodium 100 Metoprolol Tartrate 25 MG Met. FORMIN HCl 500 MG Omeprazole 20 MG CPDR Mira. Lax POWD Hydrocodone
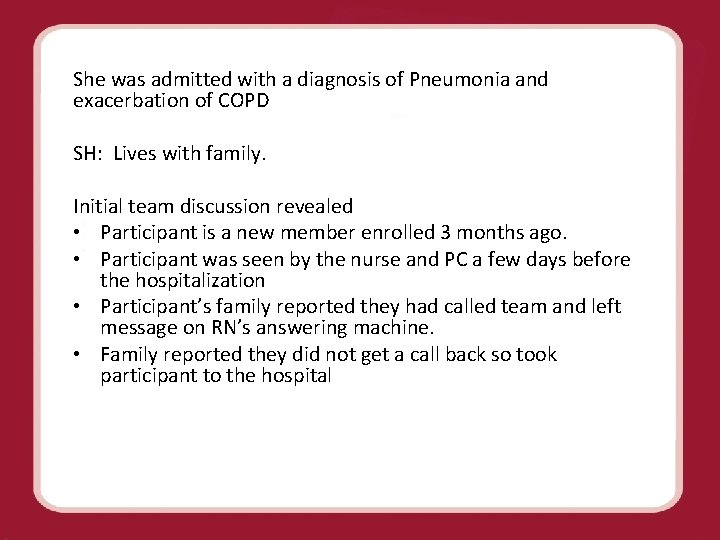
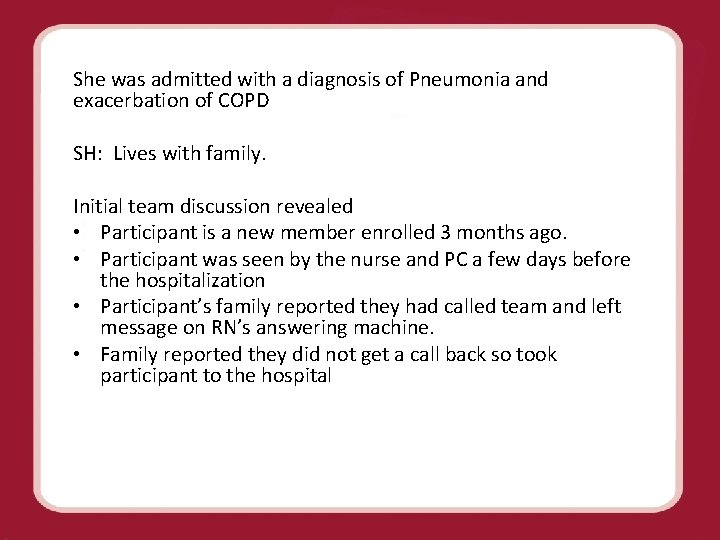
She was admitted with a diagnosis of Pneumonia and exacerbation of COPD SH: Lives with family. Initial team discussion revealed • Participant is a new member enrolled 3 months ago. • Participant was seen by the nurse and PC a few days before the hospitalization • Participant’s family reported they had called team and left message on RN’s answering machine. • Family reported they did not get a call back so took participant to the hospital
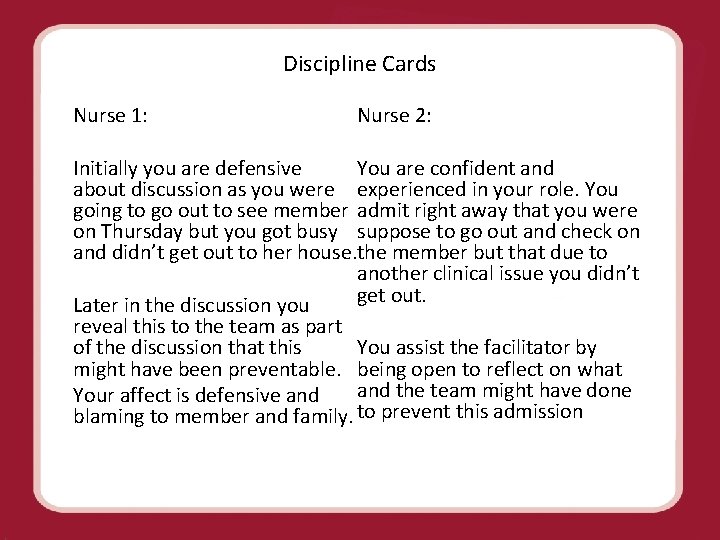
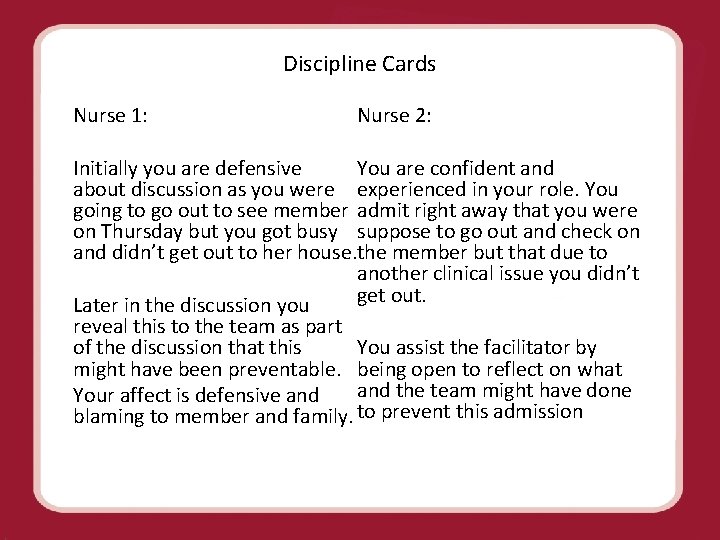
Discipline Cards Nurse 1: Nurse 2: You are confident and Initially you are defensive about discussion as you were experienced in your role. You going to go out to see member admit right away that you were on Thursday but you got busy suppose to go out and check on and didn’t get out to her house. the member but that due to another clinical issue you didn’t get out. Later in the discussion you reveal this to the team as part of the discussion that this You assist the facilitator by might have been preventable. being open to reflect on what Your affect is defensive and the team might have done blaming to member and family. to prevent this admission
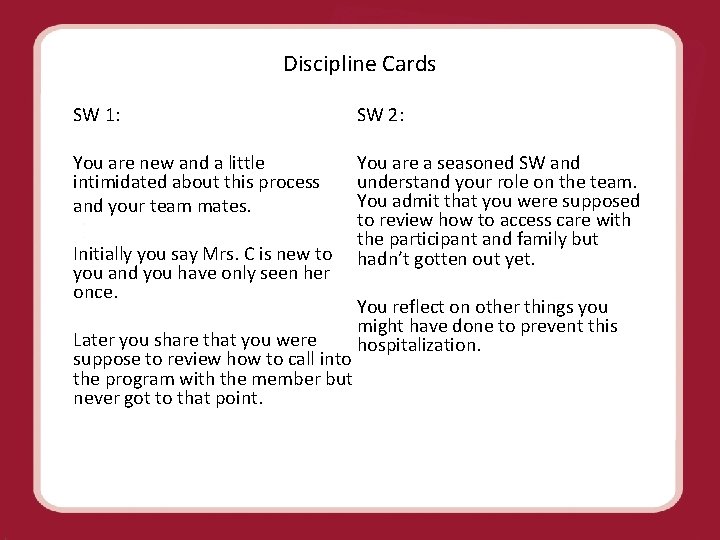
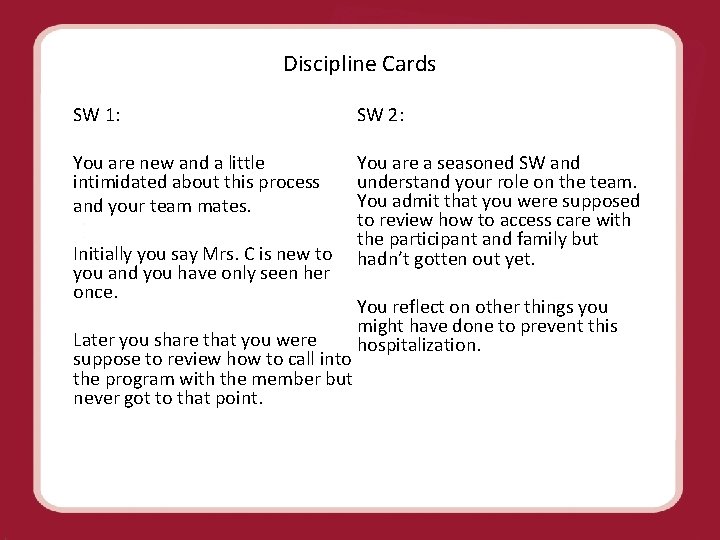
Discipline Cards SW 1: SW 2: You are new and a little You are a seasoned SW and intimidated about this process understand your role on the team. You admit that you were supposed and your team mates. to review how to access care with the participant and family but Initially you say Mrs. C is new to hadn’t gotten out yet. you and you have only seen her once. You reflect on other things you might have done to prevent this Later you share that you were hospitalization. suppose to review how to call into the program with the member but never got to that point.
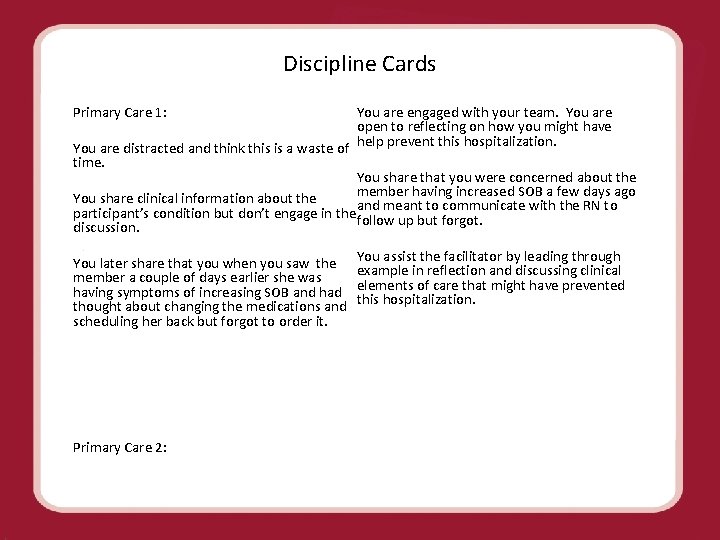
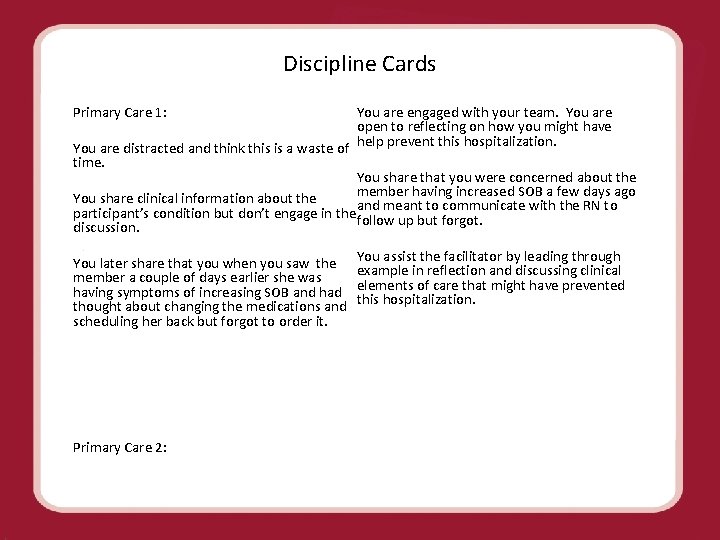
Discipline Cards You are engaged with your team. You are Primary Care 1: open to reflecting on how you might have You are distracted and think this is a waste of help prevent this hospitalization. time. You share that you were concerned about the member having increased SOB a few days ago You share clinical information about the participant’s condition but don’t engage in the and meant to communicate with the RN to follow up but forgot. discussion. You later share that you when you saw the You assist the facilitator by leading through example in reflection and discussing clinical member a couple of days earlier she was having symptoms of increasing SOB and had elements of care that might have prevented thought about changing the medications and this hospitalization. scheduling her back but forgot to order it. Primary Care 2:
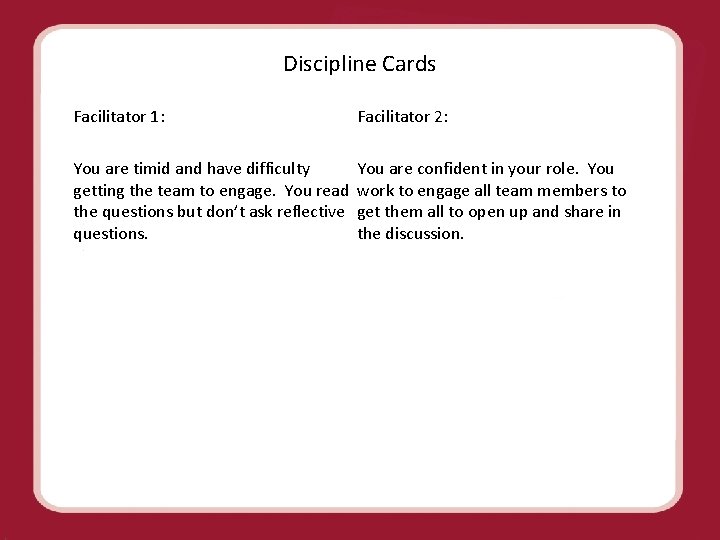
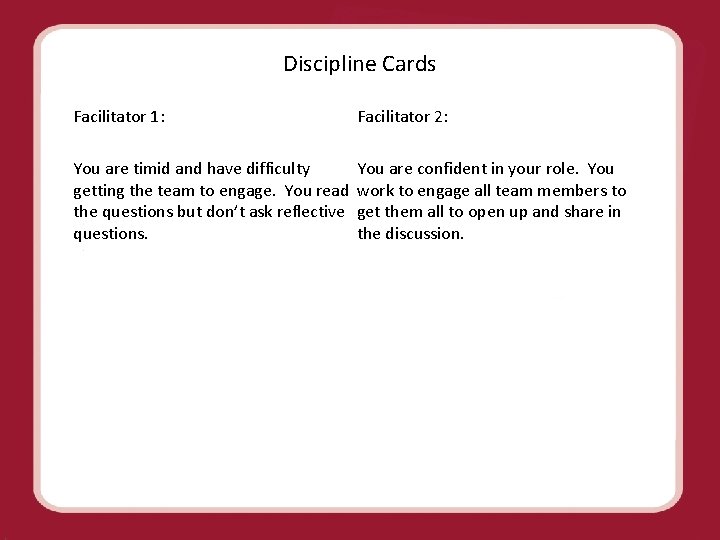
Discipline Cards Facilitator 2: Facilitator 1: You are timid and have difficulty You are confident in your role. You getting the team to engage. You read work to engage all team members to the questions but don’t ask reflective get them all to open up and share in questions. the discussion.
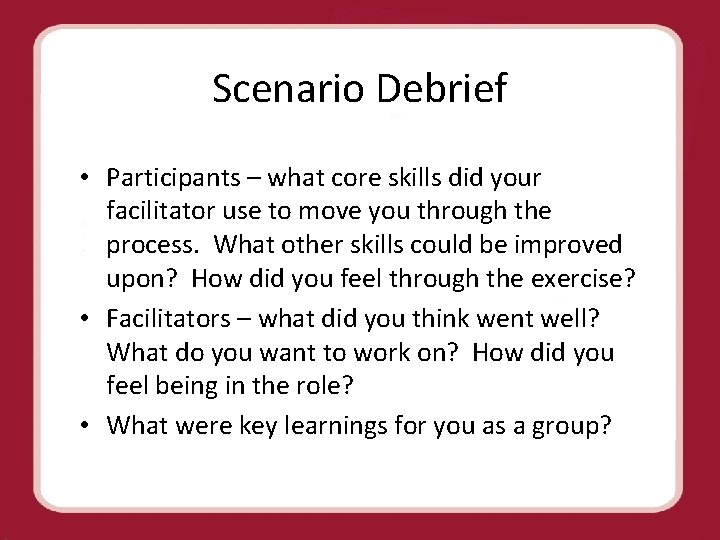
Scenario Debrief • Participants – what core skills did your facilitator use to move you through the process. What other skills could be improved upon? How did you feel through the exercise? • Facilitators – what did you think went well? What do you want to work on? How did you feel being in the role? • What were key learnings for you as a group?
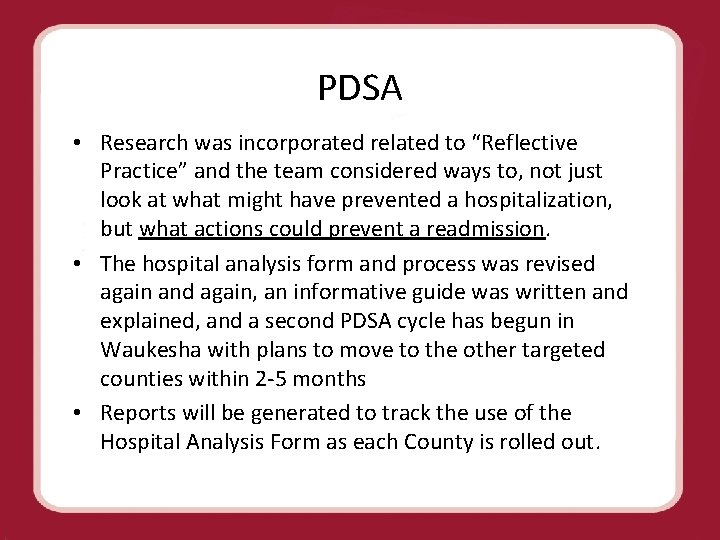
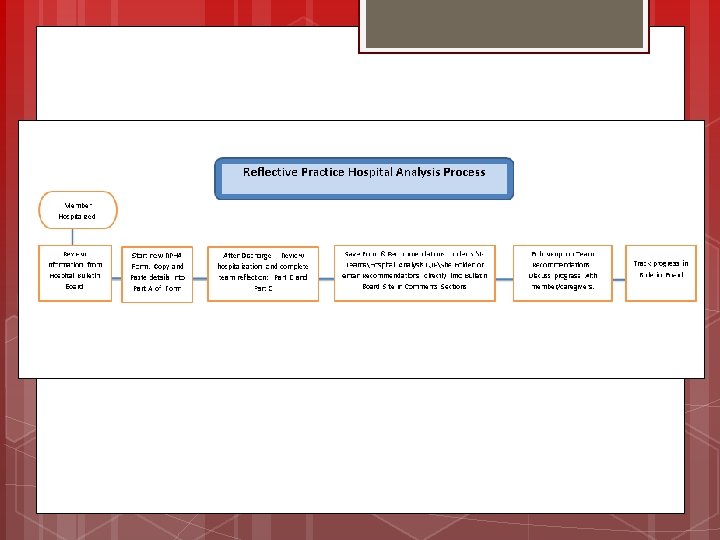
PDSA • Research was incorporated related to “Reflective Practice” and the team considered ways to, not just look at what might have prevented a hospitalization, but what actions could prevent a readmission. • The hospital analysis form and process was revised again and again, an informative guide was written and explained, and a second PDSA cycle has begun in Waukesha with plans to move to the other targeted counties within 2 -5 months • Reports will be generated to track the use of the Hospital Analysis Form as each County is rolled out.
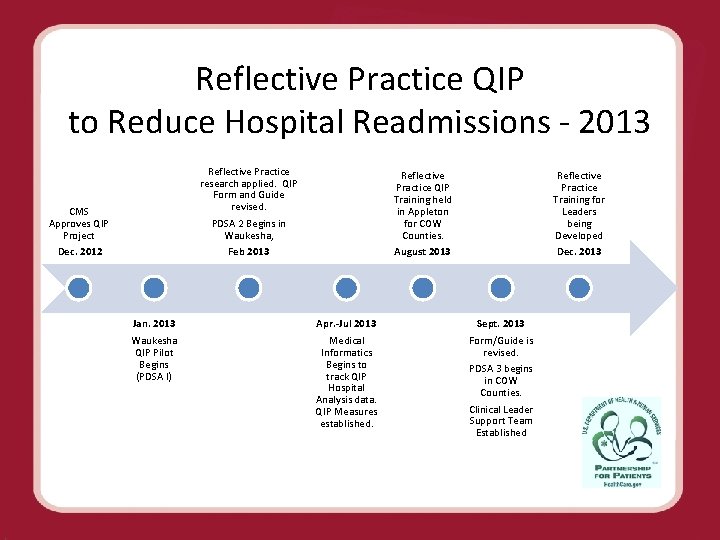
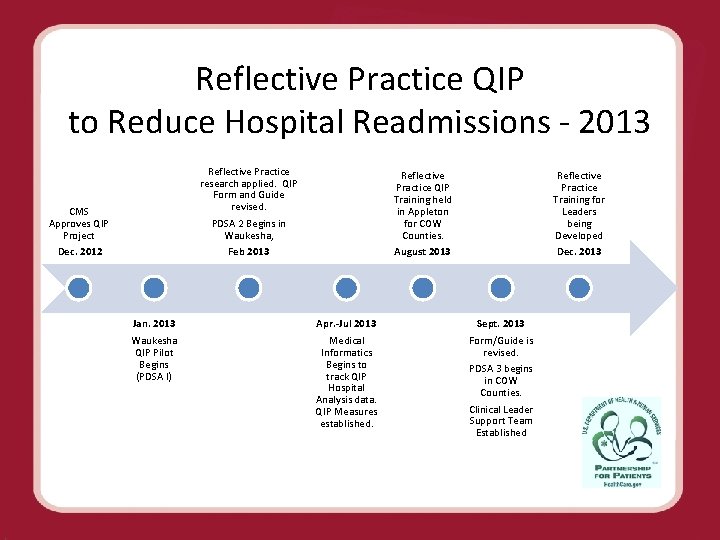
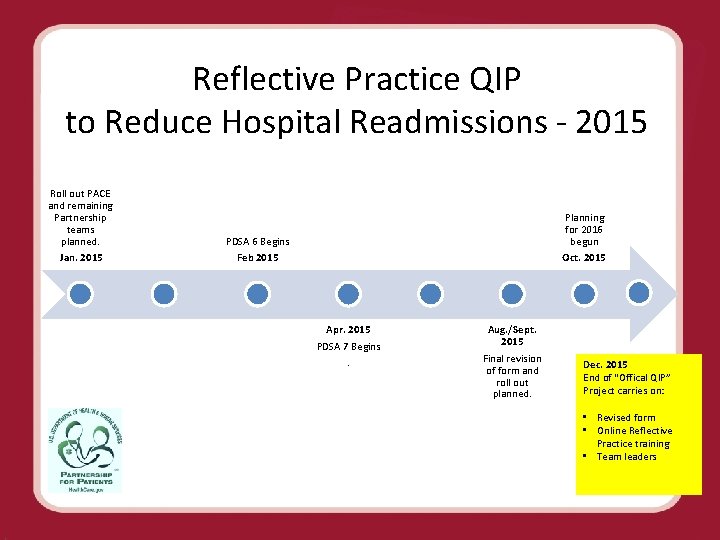
Reflective Practice QIP to Reduce Hospital Readmissions - 2013 CMS Approves QIP Project Dec. 2012 Jan. 2013 Waukesha QIP Pilot Begins (PDSA I) Reflective Practice research applied. QIP Form and Guide revised. PDSA 2 Begins in Waukesha, Reflective Practice QIP Training held in Appleton for COW Counties. Reflective Practice Training for Leaders being Developed Feb 2013 August 2013 Dec. 2013 Apr. -Jul 2013 Medical Informatics Begins to track QIP Hospital Analysis data. QIP Measures established. Sept. 2013 Form/Guide is revised. PDSA 3 begins in COW Counties. Clinical Leader Support Team Established
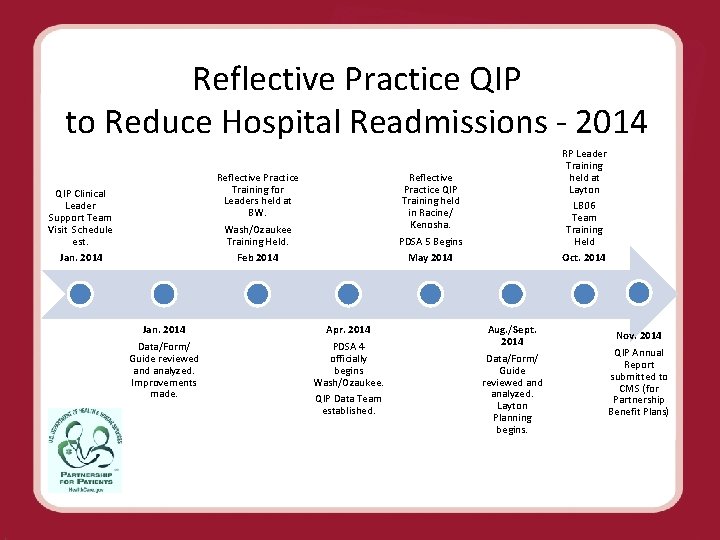
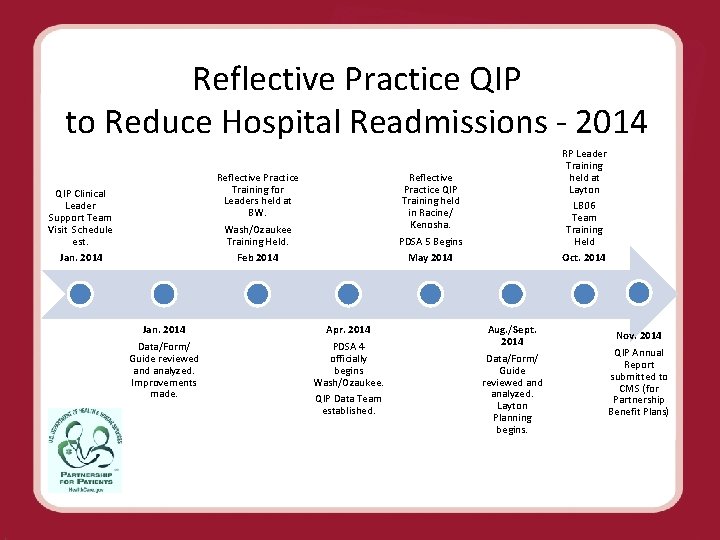
Reflective Practice QIP to Reduce Hospital Readmissions - 2014 QIP Clinical Leader Support Team Visit Schedule est. Reflective Practice Training for Leaders held at BW. Wash/Ozaukee Training Held. Jan. 2014 Feb 2014 Jan. 2014 Data/Form/ Guide reviewed analyzed. Improvements made. RP Leader Training held at Layton LB 06 Team Training Held Reflective Practice QIP Training held in Racine/ Kenosha. PDSA 5 Begins May 2014 Apr. 2014 PDSA 4 officially begins Wash/Ozaukee. QIP Data Team established. Oct. 2014 Aug. /Sept. 2014 Data/Form/ Guide reviewed analyzed. Layton Planning begins. Nov. 2014 QIP Annual Report submitted to CMS (for Partnership Benefit Plans)
Initial year Summary • The Reflective Practice Hospital Analysis Form is a vehicle for facilitating a team reflective case analysis, similar to a root cause analysis • Goal is to foster understanding of what could have prevented the hospitalization as well as what actions could prevent a future hospitalization • The QIP will also help us collect information on hospitalizations and readmission trends • This project is one of several CCI projects focused on reducing hospitalizations and readmissions.
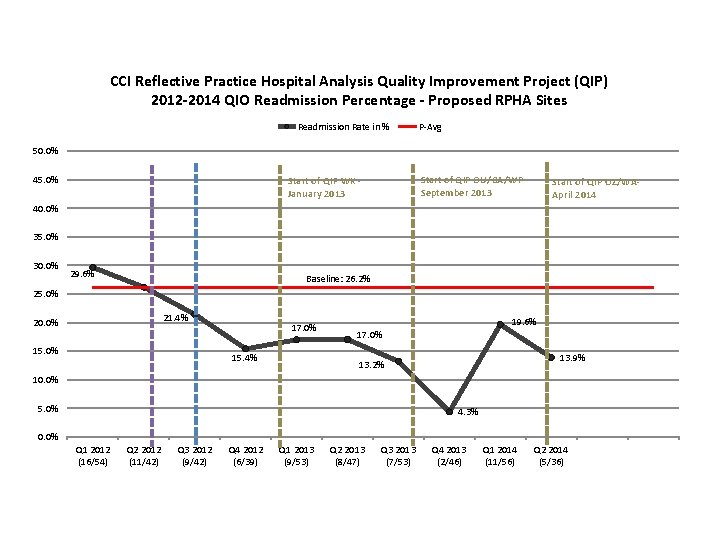
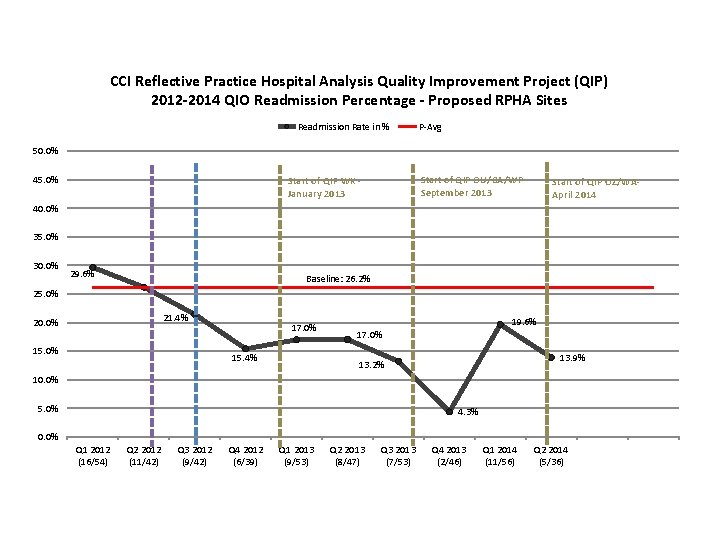
CCI Reflective Practice Hospital Analysis Quality Improvement Project (QIP) 2012 -2014 QIO Readmission Percentage - Proposed RPHA Sites Readmission Rate in % P-Avg 50. 0% 45. 0% Start of QIP OU/CA/WP- September 2013 Start of QIP WK - January 2013 Start of QIP OZ/WA- April 2014 40. 0% 35. 0% 30. 0% 29. 6% Baseline: 26. 2% 25. 0% 21. 4% 20. 0% 15. 0% 17. 0% 15. 4% 19. 6% 17. 0% 13. 9% 13. 2% 10. 0% 5. 0% 4. 3% 0. 0% Q 1 2012 (16/54) Q 2 2012 (11/42) Q 3 2012 (9/42) Q 4 2012 (6/39) Q 1 2013 (9/53) Q 2 2013 (8/47) Q 3 2013 (7/53) Q 4 2013 (2/46) Q 1 2014 (11/56) Q 2 2014 (5/36)
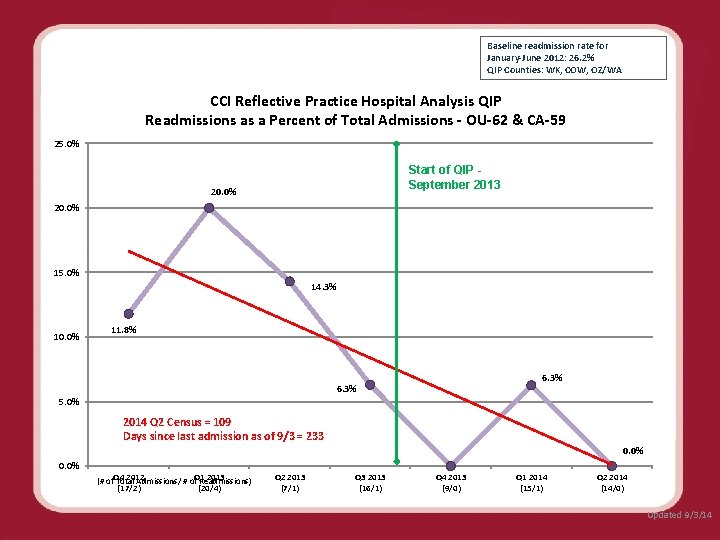
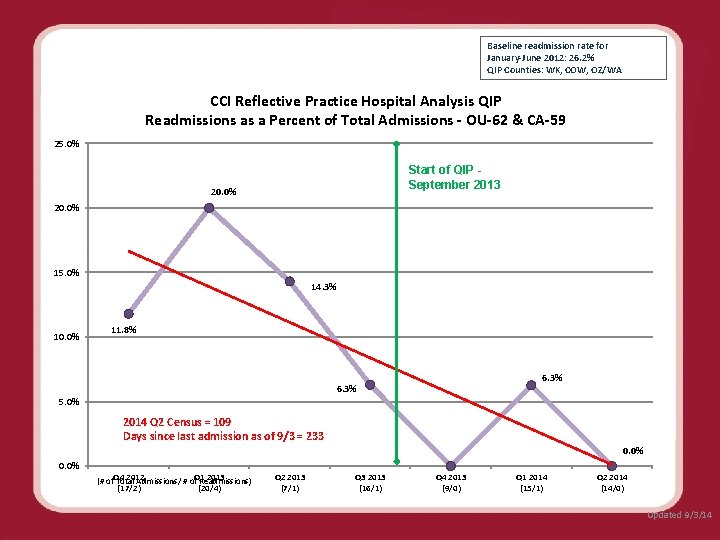
Baseline readmission rate for January-June 2012: 26. 2% QIP Counties: WK, COW, OZ/WA CCI Reflective Practice Hospital Analysis QIP Readmissions as a Percent of Total Admissions - OU-62 & CA-59 25. 0% Start of QIP September 2013 20. 0% 15. 0% 14. 3% 10. 0% 11. 8% 6. 3% 5. 0% 2014 Q 2 Census = 109 Days since last admission as of 9/3 = 233 0. 0% Q 4 2012 Q 1 2013 Q 2 2013 Q 3 2013 Q 4 2013 Q 1 2014 Q 2 2014 (# of Total Admissions/ # of Readmissions) (17/2) (20/4) (7/1) (16/1) (9/0) (15/1) (14/0) Updated 9/3/14
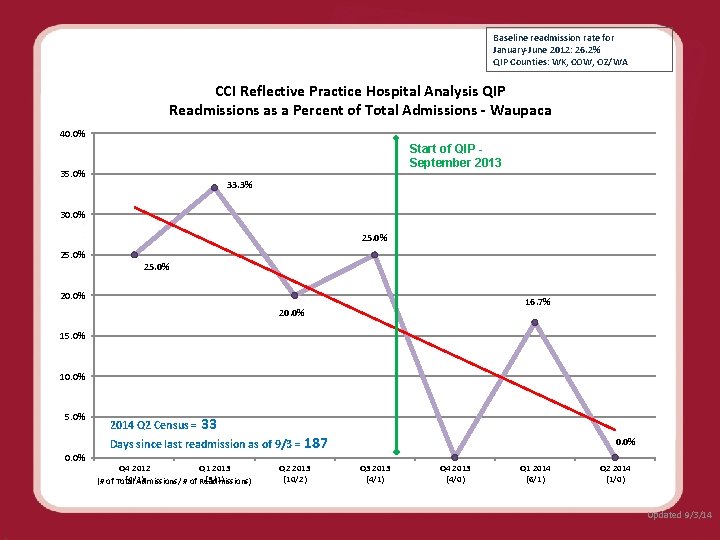
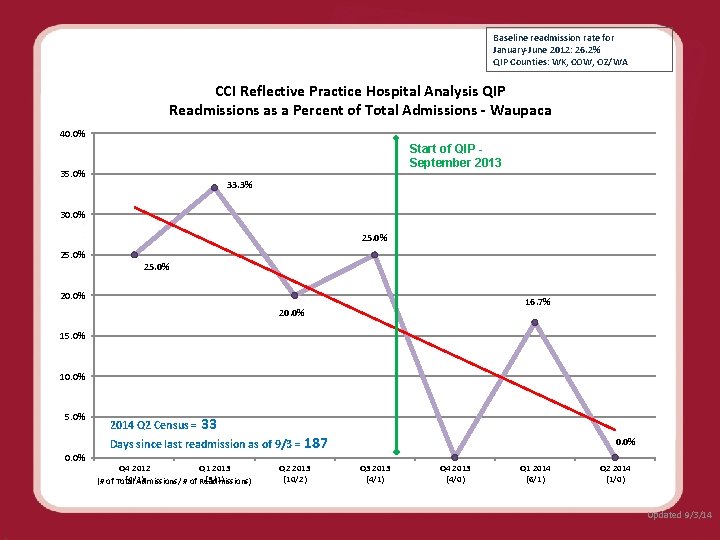
Baseline readmission rate for January-June 2012: 26. 2% QIP Counties: WK, COW, OZ/WA CCI Reflective Practice Hospital Analysis QIP Readmissions as a Percent of Total Admissions - Waupaca 40. 0% Start of QIP September 2013 35. 0% 33. 3% 30. 0% 25. 0% 20. 0% 16. 7% 15. 0% 10. 0% 5. 0% 0. 0% 2014 Q 2 Census = 33 Days since last readmission as of 9/3 = 187 0. 0% Q 4 2012 Q 1 2013 Q 2 2013 Q 3 2013 Q 4 2013 Q 1 2014 Q 2 2014 (4/1) (3/1) (10/2) (4/1) (4/0) (6/1) (1/0) (# of Total Admissions/ # of Readmissions) Updated 9/3/14
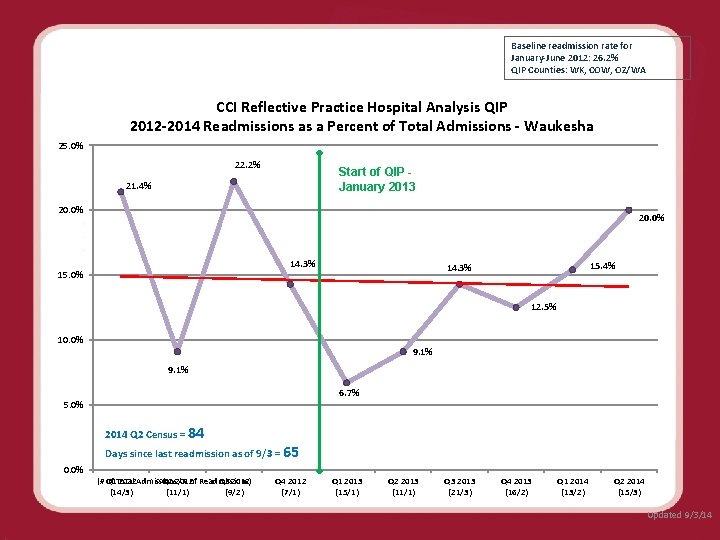
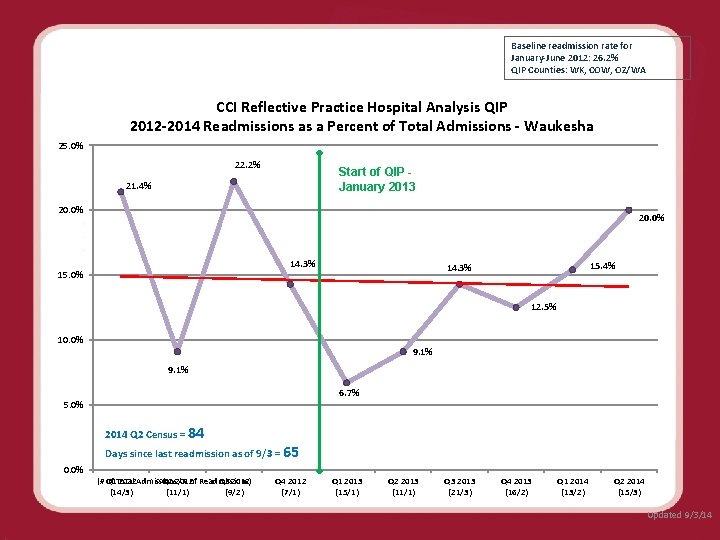
Baseline readmission rate for January-June 2012: 26. 2% QIP Counties: WK, COW, OZ/WA CCI Reflective Practice Hospital Analysis QIP 2012 -2014 Readmissions as a Percent of Total Admissions - Waukesha 25. 0% 22. 2% Start of QIP January 2013 21. 4% 20. 0% 14. 3% 15. 0% 15. 4% 14. 3% 12. 5% 10. 0% 9. 1% 6. 7% 5. 0% 2014 Q 2 Census = 84 Days since last readmission as of 9/3 = 65 0. 0% (# of Total Admissions/ # of Readmissions) Q 1 2012 Q 2 2012 Q 3 2012 (14/3) (11/1) (9/2) Q 4 2012 (7/1) Q 1 2013 (15/1) Q 2 2013 (11/1) Q 3 2013 (21/3) Q 4 2013 (16/2) Q 1 2014 (13/2) Q 2 2014 (15/3) Updated 9/3/14
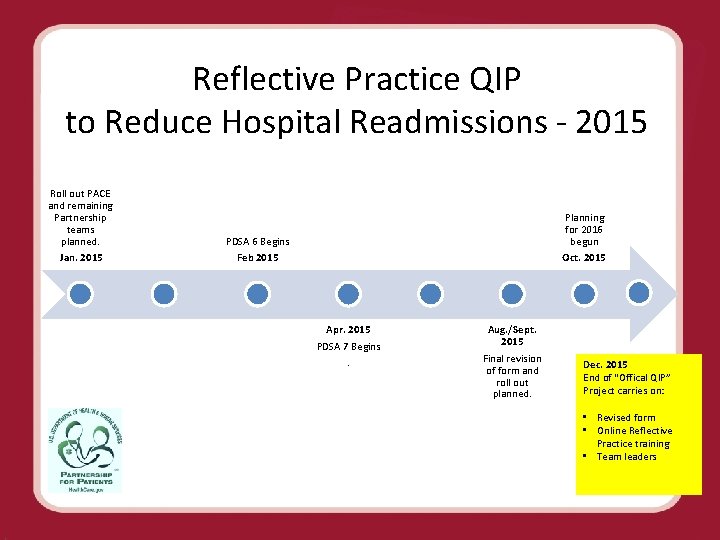
Reflective Practice QIP to Reduce Hospital Readmissions - 2015 Roll out PACE and remaining Partnership teams planned. Jan. 2015 Planning for 2016 begun Oct. 2015 PDSA 6 Begins Feb 2015 Apr. 2015 PDSA 7 Begins. Aug. /Sept. 2015 Final revision of form and roll out planned. Dec. 2015 End of “Offical QIP” Project carries on: • Revised form • Online Reflective Practice training • Team leaders
B. Wagner, 2013, QIP
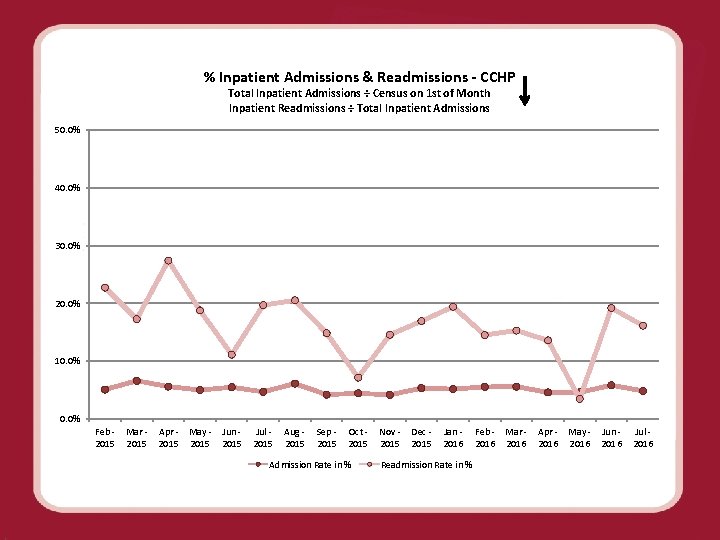
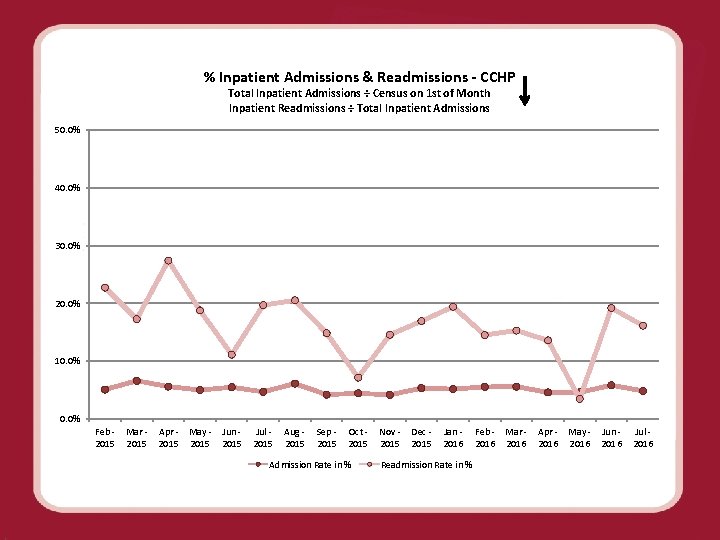
% Inpatient Admissions & Readmissions - CCHP Total Inpatient Admissions ÷ Census on 1 st of Month Inpatient Readmissions ÷ Total Inpatient Admissions 50. 0% 40. 0% 30. 0% 20. 0% 10. 0% Feb - Mar - Apr - May - Jun - Jul - 2015 2015 Aug - Sep - Oct - Nov - Dec - Jan - Feb - Mar - Apr - May - Jun - Jul - 2015 2015 2016 2016 Admission Rate in % Readmission Rate in %
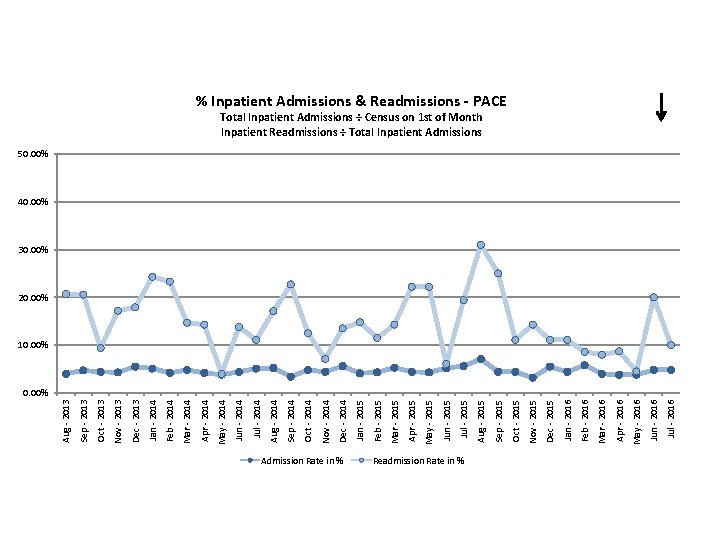
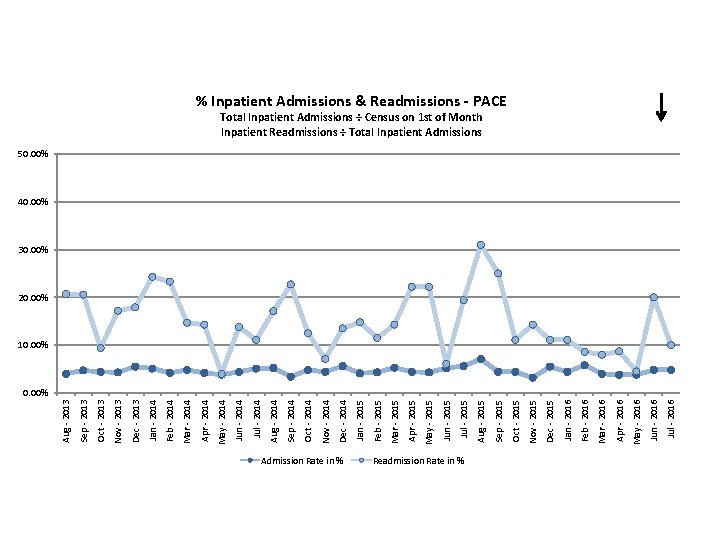
Admission Rate in % Readmission Rate in % Jul - 2016 Jun - 2016 May - 2016 Apr - 2016 Mar - 2016 Feb - 2016 Jan - 2016 Dec - 2015 Nov - 2015 Oct - 2015 Sep - 2015 Aug - 2015 Jul - 2015 Jun - 2015 May - 2015 Apr - 2015 Mar - 2015 Feb - 2015 Jan - 2015 Dec - 2014 Nov - 2014 Oct - 2014 Sep - 2014 Aug - 2014 Jul - 2014 Jun - 2014 May - 2014 Apr - 2014 Mar - 2014 Feb - 2014 Jan - 2014 Dec - 2013 Nov - 2013 Oct - 2013 Sep - 2013 Aug - 2013 % Inpatient Admissions & Readmissions - PACE Total Inpatient Admissions ÷ Census on 1 st of Month Inpatient Readmissions ÷ Total Inpatient Admissions 50. 00% 40. 00% 30. 00% 20. 00% 10. 00%
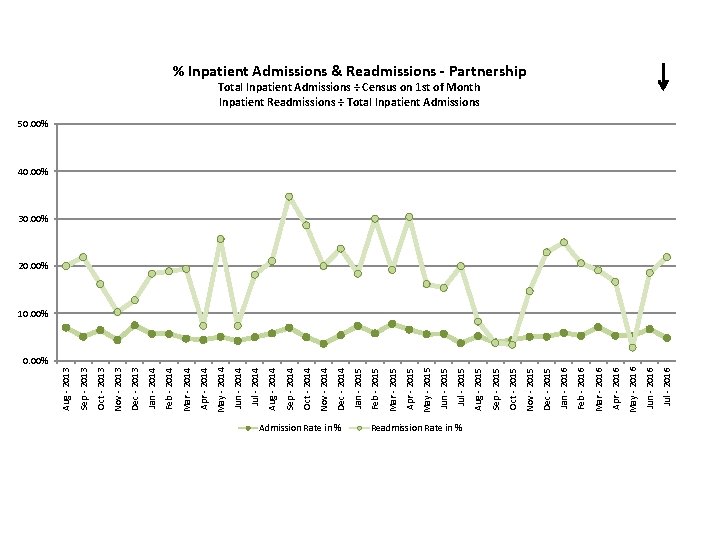
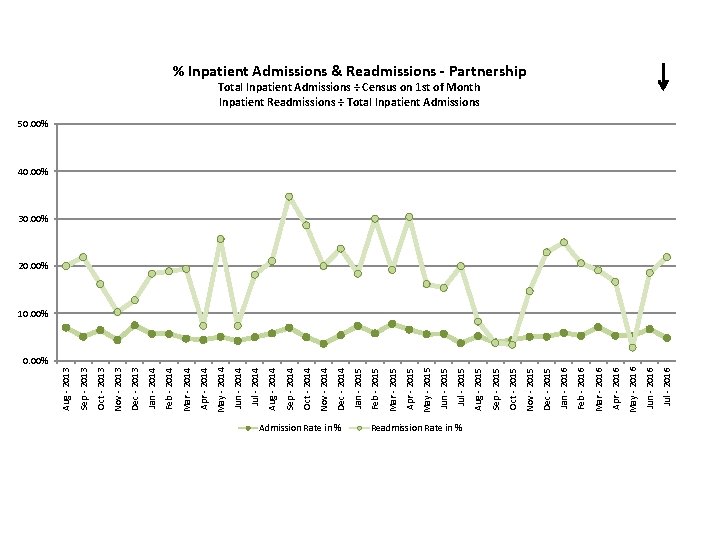
Admission Rate in % Readmission Rate in % Jul - 2016 Jun - 2016 May - 2016 Apr - 2016 Mar - 2016 Feb - 2016 Jan - 2016 Dec - 2015 Nov - 2015 Oct - 2015 Sep - 2015 Aug - 2015 Jul - 2015 Jun - 2015 May - 2015 Apr - 2015 Mar - 2015 Feb - 2015 Jan - 2015 Dec - 2014 Nov - 2014 Oct - 2014 Sep - 2014 Aug - 2014 Jul - 2014 Jun - 2014 May - 2014 Apr - 2014 Mar - 2014 Feb - 2014 Jan - 2014 Dec - 2013 Nov - 2013 Oct - 2013 Sep - 2013 Aug - 2013 % Inpatient Admissions & Readmissions - Partnership Total Inpatient Admissions ÷ Census on 1 st of Month Inpatient Readmissions ÷ Total Inpatient Admissions 50. 00% 40. 00% 30. 00% 20. 00% 10. 00%
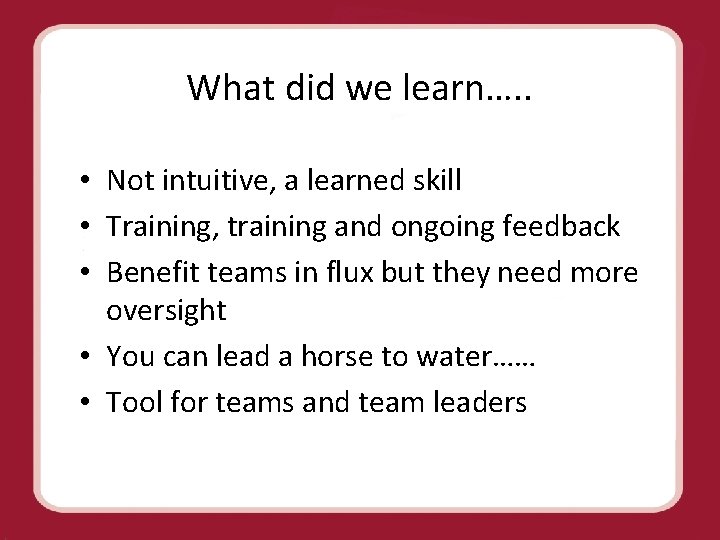
What did we learn…. . • Not intuitive, a learned skill • Training, training and ongoing feedback • Benefit teams in flux but they need more oversight • You can lead a horse to water…… • Tool for teams and team leaders
CCI Readmissions QIP TEAM: Dr. Mary Gavinski, Executive Sponsor Bonni Wagner Nancy Leipzig Tiffany Anderson Kather Bob Alm Ann Seffernick Cindy Cowie and Team QIP Quality Coordinator Regional Director Nurse Practitioner Site Manager Medical Informatics Senior Clinical Leader Support Team: Dr. Gavinski Chris Brand Cathy Rapp Dr. Almas 53 Kelly Carter
Questions? ? ?
References Bens, Ingrid (2005). Facilitating with Ease! San Francisco: Jossey-Bass. Publishing. Bulman and Schutz (2008). Reflective Practice in Nursing, 4 th edition. United Kingdom: Blackwell Publishing. Freshwater, D et al (2008). International Textbook of Reflective Practice in Nursing. United Kingdom: Blackwell Publishing. Manthey, M (2001). Reflective practice. Creative Nursing, 2, p. 3 -5. O’Connor, Mary (2013). Reflection as a self-care strategy. Voice of Nursing Leadership, July, p. 8 -10. Regmi and Naidoo (2013). Understanding the processes of writing papers reflectively. Nurse Researcher, 20: 6, p. 33 -39.
 Cappagh admissions
Cappagh admissions Types of hospital admissions
Types of hospital admissions What is reducing sugar
What is reducing sugar Fates of glucose
Fates of glucose Fehling's test
Fehling's test Reducing vs. non-reducing sugars
Reducing vs. non-reducing sugars Mary wollstonecraft mary a fiction
Mary wollstonecraft mary a fiction Identifying oxidizing and reducing agents
Identifying oxidizing and reducing agents Victoria and albert ward st mary's hospital
Victoria and albert ward st mary's hospital Hand reflecting sphere
Hand reflecting sphere Emtma e103
Emtma e103 Which is the best surface for reflecting heat radiation
Which is the best surface for reflecting heat radiation Heat energy transfer
Heat energy transfer Which is the best surface for reflecting heat radiation
Which is the best surface for reflecting heat radiation Which is the best surface for reflecting heat radiation
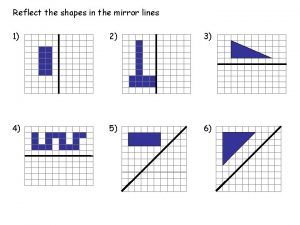
Which is the best surface for reflecting heat radiation Reflecting points on a coordinate plane worksheet
Reflecting points on a coordinate plane worksheet Emit and reflect
Emit and reflect Which is the best surface for reflecting heat radiation
Which is the best surface for reflecting heat radiation Partializing social work
Partializing social work Reflecting god's character verse
Reflecting god's character verse Reflecting shapes
Reflecting shapes Because of convection, the warmest air in a room _____.
Because of convection, the warmest air in a room _____. A refracting telescope produces an image using a(n) ____.
A refracting telescope produces an image using a(n) ____. Reflections on trusting trust ken thompson
Reflections on trusting trust ken thompson Shifting reflecting and stretching graphs
Shifting reflecting and stretching graphs Number of pharmacist required for 250 bed hospital
Number of pharmacist required for 250 bed hospital Give us your hungry your tired your poor
Give us your hungry your tired your poor Uc davis admissions portal
Uc davis admissions portal Slu admissions counselors
Slu admissions counselors Admissions funnel
Admissions funnel Coast guard academy admissions
Coast guard academy admissions Pine view school admissions
Pine view school admissions Mira costa admissions
Mira costa admissions Interrogatories sample
Interrogatories sample Hamline graduate programs
Hamline graduate programs Usf applicant portal
Usf applicant portal Uci admission counselor
Uci admission counselor University of florida rolling admissions
University of florida rolling admissions University central florida international student insurance
University central florida international student insurance Chapter 32 admissions transfers and discharges
Chapter 32 admissions transfers and discharges Requirements for west point
Requirements for west point Admissions uaf
Admissions uaf Nau graduate college
Nau graduate college Dual enrollment osu
Dual enrollment osu Brag packet cca
Brag packet cca Canyon crest academy admissions
Canyon crest academy admissions Cal state dominguez hills admissions
Cal state dominguez hills admissions Admissions to schools act 2018
Admissions to schools act 2018 Victorian tertiary admissions centre founded
Victorian tertiary admissions centre founded Chattahoochee tech gpa requirements
Chattahoochee tech gpa requirements Moraine valley nursing program reviews
Moraine valley nursing program reviews Bexley selection test 2019
Bexley selection test 2019 Uams sap
Uams sap The door david hammons
The door david hammons U of d mercy school of dentistry
U of d mercy school of dentistry Belmont hill admissions
Belmont hill admissions