Redesign of VCH Allied Health Professional Leadership Staff



- Slides: 15

Redesign of VCH Allied Health Professional Leadership Staff Forums Aug 8 - 12, 2011 Susan Wannamaker Jo Clark Judith Bowen
Agenda • Role of Professional Practice Leadership • Driving Forces for Redesign • Why a Regional Structure for Allied Leadership – Vision • • Overview of Current State Characteristics of Redesign Project Leadership, Proposed Timelines Next Steps
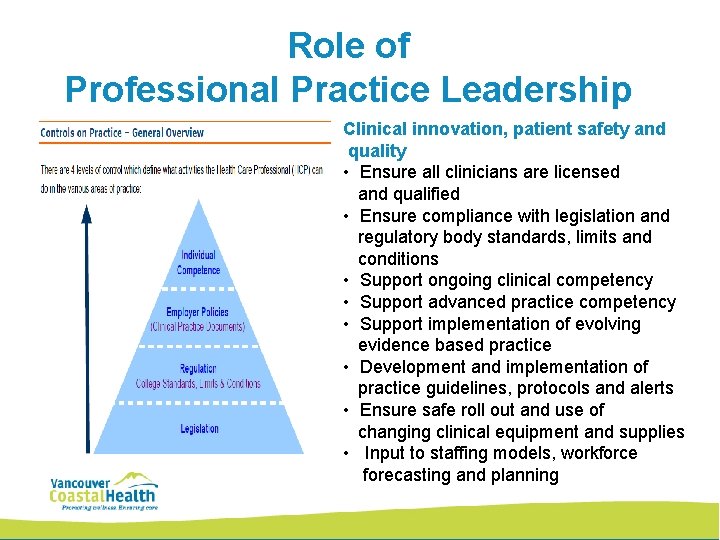
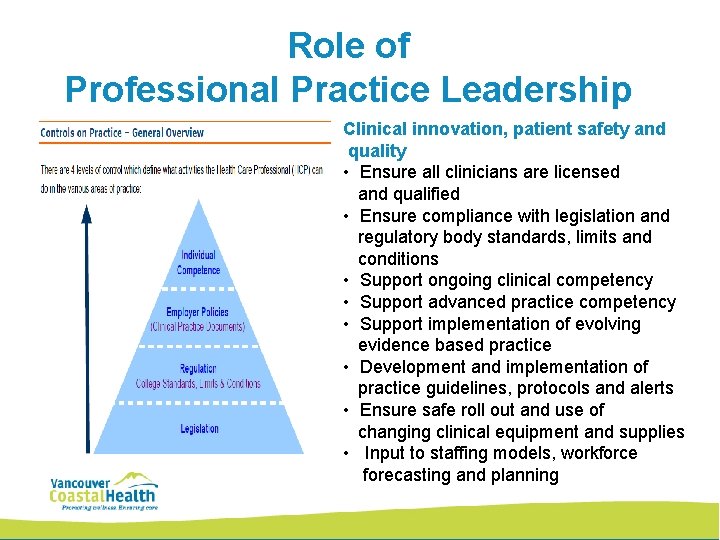
Role of Professional Practice Leadership Clinical innovation, patient safety and quality • Ensure all clinicians are licensed and qualified • Ensure compliance with legislation and regulatory body standards, limits and conditions • Support ongoing clinical competency • Support advanced practice competency • Support implementation of evolving evidence based practice • Development and implementation of practice guidelines, protocols and alerts • Ensure safe roll out and use of changing clinical equipment and supplies • Input to staffing models, workforce forecasting and planning
Driving Forces for Redesign • The current allied health practice leadership structure is patched together from resourced (acute care facilities) to unresourced areas (community and rural health) • No regional structure for allied health leadership • Allied health professional leadership structure has not been reviewed or restructured since the development of the health authority in 2002 • The historical leadership structure has been driven by dated language in the collective agreement • It functions on consultation and consensus, with ‘committees’ that do not have full jurisdiction for all practitioners across the health authority • Patients, clients and residents do not receive consistent and equitable services across the health authority
Why a Regional Structure for Allied Health Leadership A Regional Allied Health Structure will provide: • Equitable access to the highest level of quality and care across VCH • Accountability, consistent standards of care • Alignment of local, regional, provincial and academic strategies and plans and human resource planning • Education capacity as well as academic and leadership development • Innovation and people focus • Smoothing of practice resources across primary, home and community, acute, rehabilitation and residential care settings across urban to rural and remote • Cost efficiency
Vision for Allied Leadership • Regional allied health leadership framework will provide for access to equitable care, standardized, safe, evidence-based interventions, innovation and quality • Construction of an overall model of service that is based on a VCH- wide framework of leadership for all the allied health professions • Achieve HSPBA Association engagement

Allied Health Professions (Excluding Lab, Pharmacy and DI) • • • Occupational Therapy (284 Fte) Physiotherapy (249 Fte) Social Work (172 Fte) Respiratory Therapy (123 Fte) Dietetics (89 Fte) • Speech-Language Pathology (62 Fte) • Recreation Therapy (26 Fte) • Psychology (18 Fte) • Audiology (15 Fte) • Spiritual Care (6 Fte) • Music Therapy (5 Fte) All clinical and practice leadership positions are included in contract

CURRENT STATE - Allied Health Practice Support Variation Across the Health Authority
Characteristics of Redesign Process • Early union engagement • Transparent with frequent communication • Data and discussion inform decision-making • Includes standard ways of working together • Is an inclusive process that engages all levels of the organization and stakeholders Outcome • People focused: a) Patient – safety, quality and equity in consistent, standardized and evidence based allied health services; b) Staff – practice support, competency development and education • Redistribution of practice support positions to provide representation and clinical guidance across the continuum of care (home and community care, acute, rehabilitation, residential, rural) • Promotes active participation and contribution in design • Cost effective
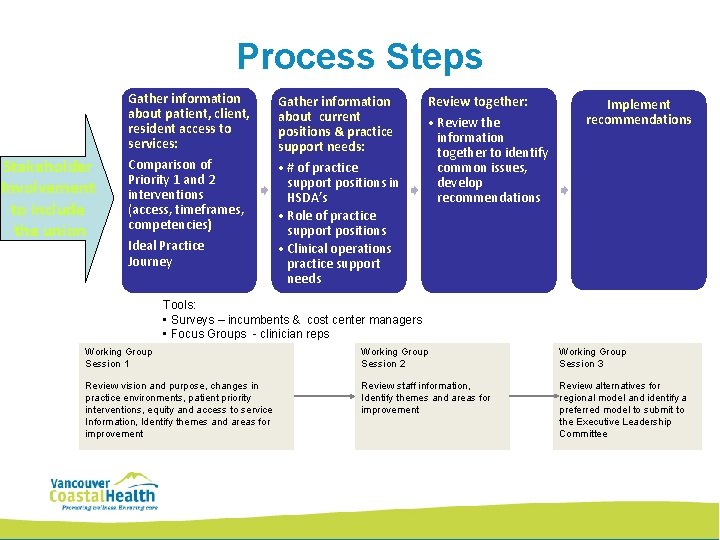
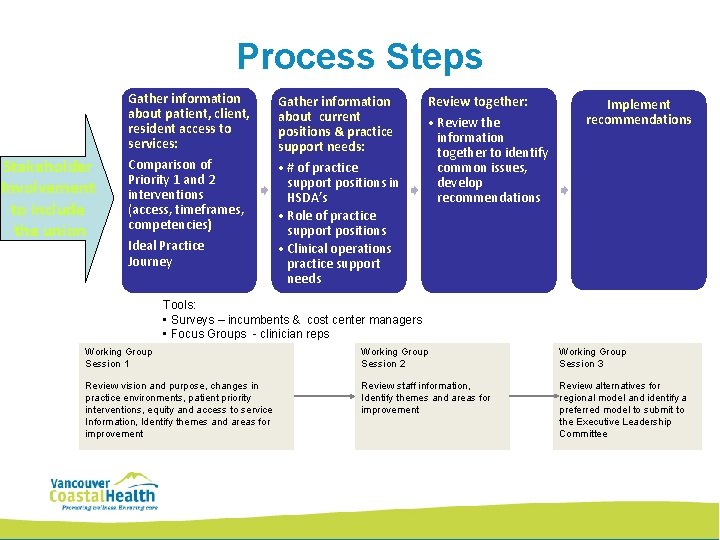
Process Steps Stakeholder Involvement to include the union Gather information about patient, client, resident access to services: Comparison of Priority 1 and 2 interventions (access, timeframes, competencies) Ideal Practice Journey Gather information about current positions & practice support needs: • # of practice support positions in HSDA’s • Role of practice support positions • Clinical operations practice support needs Review together: • Review the information together to identify common issues, develop recommendations Implement recommendations Tools: • Surveys – incumbents & cost center managers • Focus Groups - clinician reps Working Group Session 1 Working Group Session 2 Working Group Session 3 Review vision and purpose, changes in practice environments, patient priority interventions, equity and access to service Information, Identify themes and areas for improvement Review staff information, Identify themes and areas for improvement Review alternatives for regional model and identify a preferred model to submit to the Executive Leadership Committee
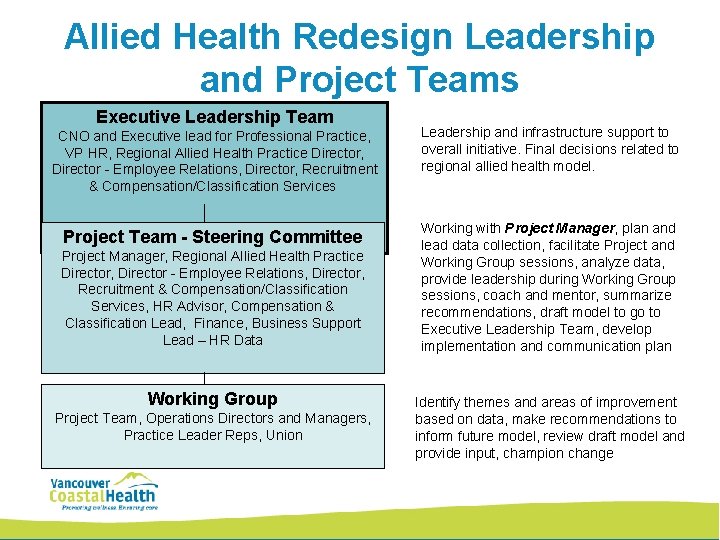
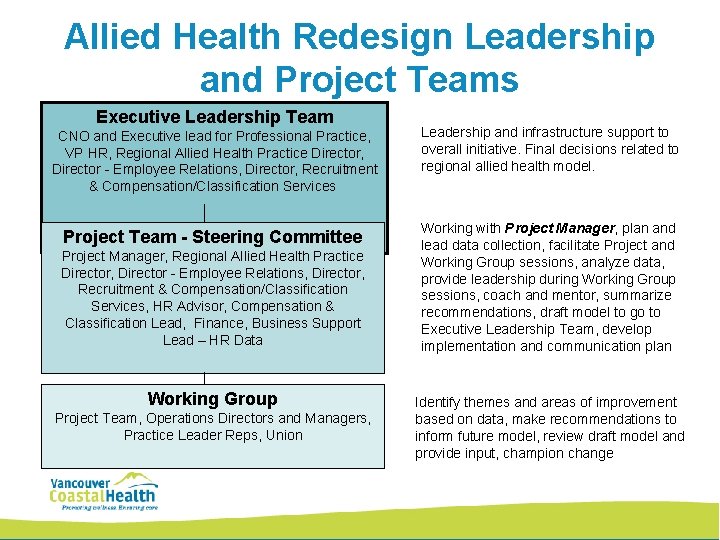
Allied Health Redesign Leadership and Project Teams Executive Leadership Team CNO and Executive lead for Professional Practice, VP HR, Regional Allied Health Practice Director, Director - Employee Relations, Director, Recruitment & Compensation/Classification Services Leadership and infrastructure support to overall initiative. Final decisions related to regional allied health model. Project Team - Steering Committee Working with Project Manager, plan and lead data collection, facilitate Project and Working Group sessions, analyze data, provide leadership during Working Group sessions, coach and mentor, summarize recommendations, draft model to go to Executive Leadership Team, develop implementation and communication plan Project Manager, Regional Allied Health Practice Director, Director - Employee Relations, Director, Recruitment & Compensation/Classification Services, HR Advisor, Compensation & Classification Lead, Finance, Business Support Lead – HR Data Working Group Project Team, Operations Directors and Managers, Practice Leader Reps, Union Identify themes and areas of improvement based on data, make recommendations to inform future model, review draft model and provide input, champion change
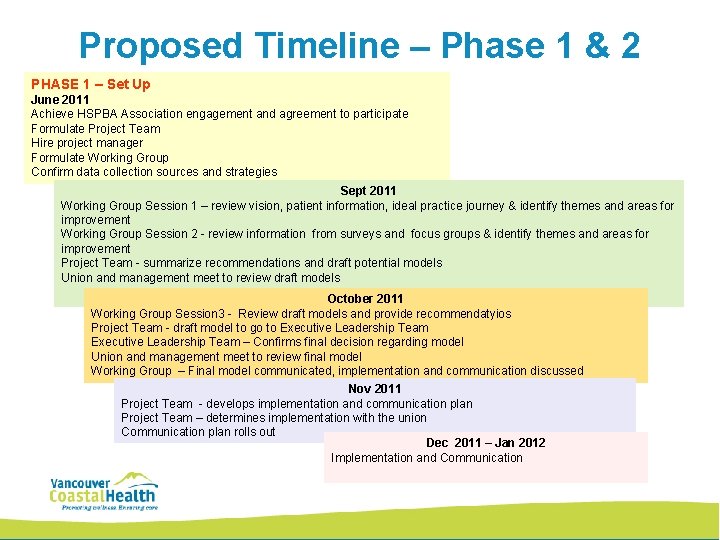
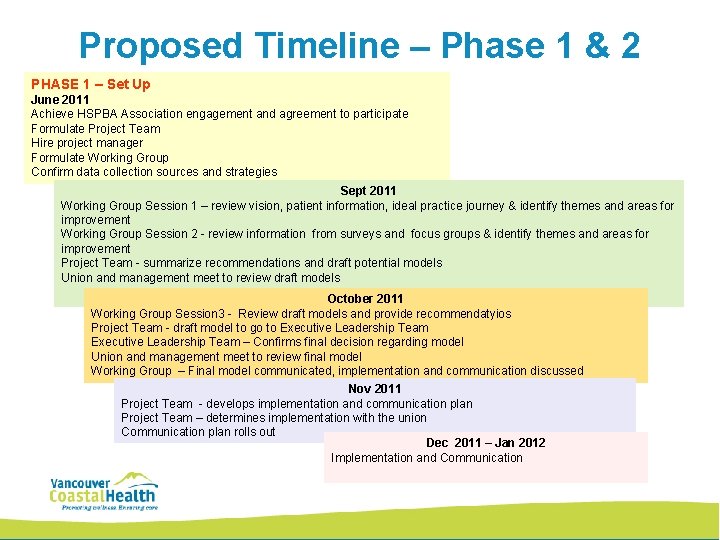
Proposed Timeline – Phase 1 & 2 PHASE 1 – Set Up June 2011 Achieve HSPBA Association engagement and agreement to participate Formulate Project Team Hire project manager Formulate Working Group Confirm data collection sources and strategies Sept 2011 PHASE 2 - Occupational Therapy and Physiotherapy Working Group Session 1 – review vision, patient information, ideal practice journey & identify themes and areas for July – Sept 2011 improvement Project Team - data collection Working Group Session 2 - review information from surveys and focus groups & identify themes and areas for improvement Project Team - summarize recommendations and draft potential models Union and management meet to review draft models October 2011 Working Group Session 3 - Review draft models and provide recommendatyios Project Team - draft model to go to Executive Leadership Team – Confirms final decision regarding model Union and management meet to review final model Working Group – Final model communicated, implementation and communication discussed Nov 2011 Project Team - develops implementation and communication plan Project Team – determines implementation with the union Communication plan rolls out Dec 2011 – Jan 2012 Implementation and Communication
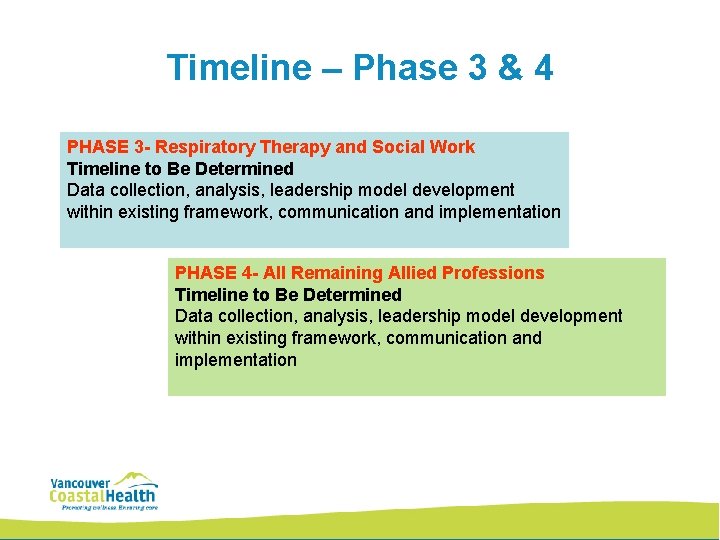
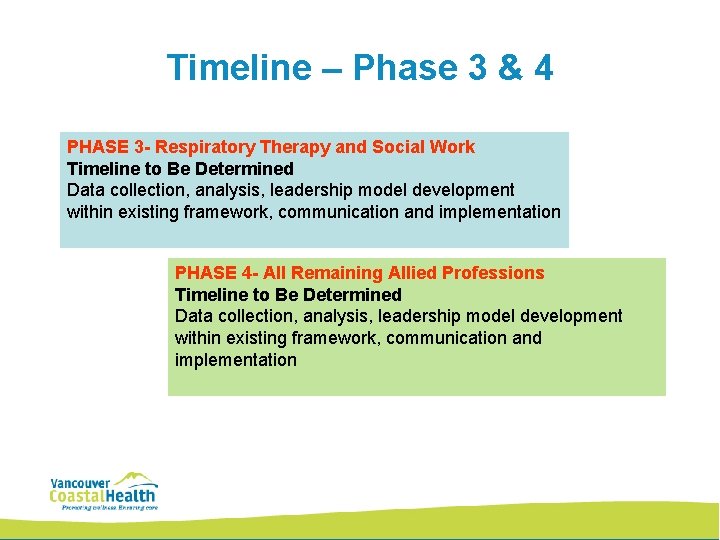
Timeline – Phase 3 & 4 PHASE 3 - Respiratory Therapy and Social Work Timeline to Be Determined Data collection, analysis, leadership model development within existing framework, communication and implementation PHASE 4 - All Remaining Allied Professions Timeline to Be Determined Data collection, analysis, leadership model development within existing framework, communication and implementation
Benefit of Redesign • Patient, staff, practice and operations-centered approach to provide: – equity in nature/position and quality of allied health services across VCH – equity in access to practice support and education for allied health clinicians • Establishment of lean, consistent practice leadership structure through collaboration and engagement of HAS, BCGEU and CUPE with practice and clinical operations • Redistribution of practice support positions to support all sectors and jurisdictions (acute, community, residential, rural) • Reinvestment in front line clinical services addressing known gaps in access to care through redesign • Retainment of our staff as valued members of VCH team; FTEs will not be reduced; plan to: – reassign to regional responsibilities – maintain clinical positions intact with decrease to appropriate grade level
Next Steps • Allied Health Staff Forums (August) • Surveys - Grade 3 – 6 PT and OT and managers of those cost centers (Aug- Sept) • Focus Groups – Clinician Reps (Aug- Sept) • Working Group sessions – stakeholder input (Sept – Oct)
 Vch investment group ag
Vch investment group ag Vch employee engagement
Vch employee engagement Vch employee engagement
Vch employee engagement List of all allied health professions
List of all allied health professions Allied health recovery request
Allied health recovery request Cumulative index of nursing and allied health
Cumulative index of nursing and allied health The allied health profession service improvement project
The allied health profession service improvement project The allied health profession service improvement project
The allied health profession service improvement project Allied health postgrad
Allied health postgrad Allied health professionals
Allied health professionals What is allied health professionals
What is allied health professionals Ouhsc allied health
Ouhsc allied health Quarter redesign
Quarter redesign Getting organizational redesign right
Getting organizational redesign right Bh redesign
Bh redesign Job analysis process
Job analysis process