Red Flags for Developmental Delays in Deafhoh Children

- Slides: 51
Red Flags for Developmental Delays in Deaf/hoh Children Susan Wiley, MD Cincinnati Children’s Hospital Medical Center Cincinnati, OH. Mary Pat Moeller, Ph. D Boys Town National Research Hospital Omaha, Nebraska
• In the past 12 months, we have not had a significant financial interest or other relationship with the manufacturer(s) of the product(s) or provider(s) of the service(s) that will be discussed in our presentation. • This presentation will not include discussion of pharmaceuticals or devices that have not been approved by the FDA or if you will be discussing unapproved or "off-label" uses of pharmaceuticals or devices.
Objectives • To gain knowledge of the risk factors for developmental delays in children who are deaf/hoh. • To be able to identify children with potential additional developmental disabilities. • To develop an intervention plan for confirming and treating an additional disability.
Developmental Screening A brief assessment designed to identify children who need more intensive diagnosis or evaluation in order to improve child health and well being.
Developmental Surveillance • Surveillance = periodic assessments over time • An on-going process (similar to growth curves). • Screening tools used to enhance the surveillance process. • Brief, objective, validated test with broad developmental focus. • Performed at set points in time. • Differentiate children with no concern from those needing additional investigation.
Why does it matter? • Identifying additional concerns early can allow for more effective intervention strategies. • Screening for developmental concerns allows for a pro-active approach to overall child development. • The age of identification of an additional disability tends to be delayed in children who are deaf/hoh.
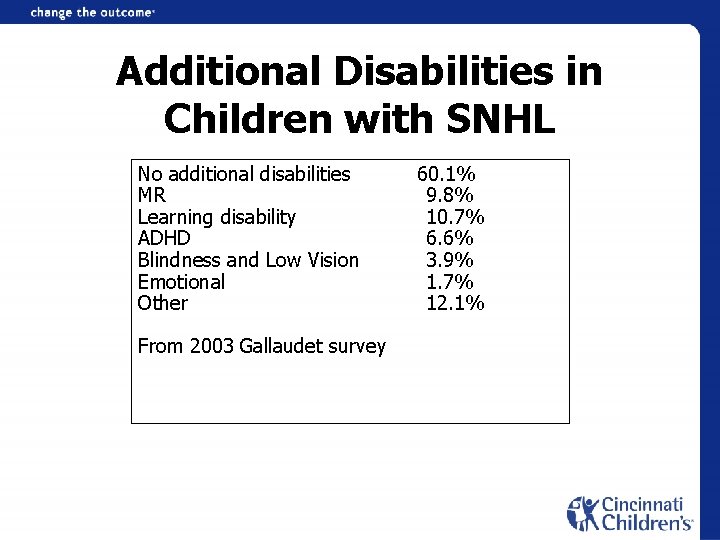
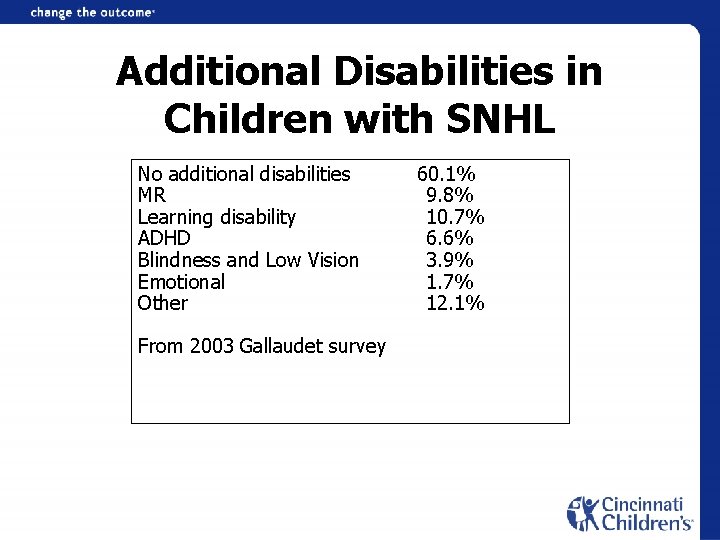
Additional Disabilities in Children with SNHL No additional disabilities 60. 1% MR 9. 8% Learning disability 10. 7% ADHD 6. 6% Blindness and Low Vision 3. 9% Emotional 1. 7% Other 12. 1% From 2003 Gallaudet survey
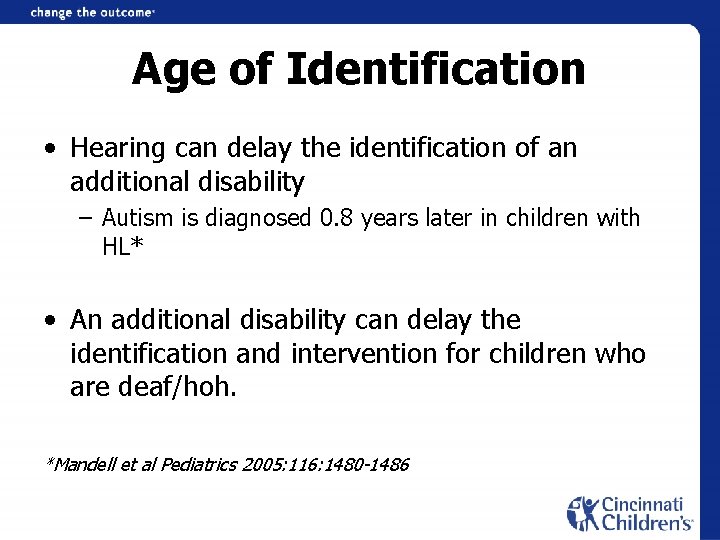
Age of Identification • Hearing can delay the identification of an additional disability – Autism is diagnosed 0. 8 years later in children with HL* • An additional disability can delay the identification and intervention for children who are deaf/hoh. *Mandell et al Pediatrics 2005: 116: 1480 -1486
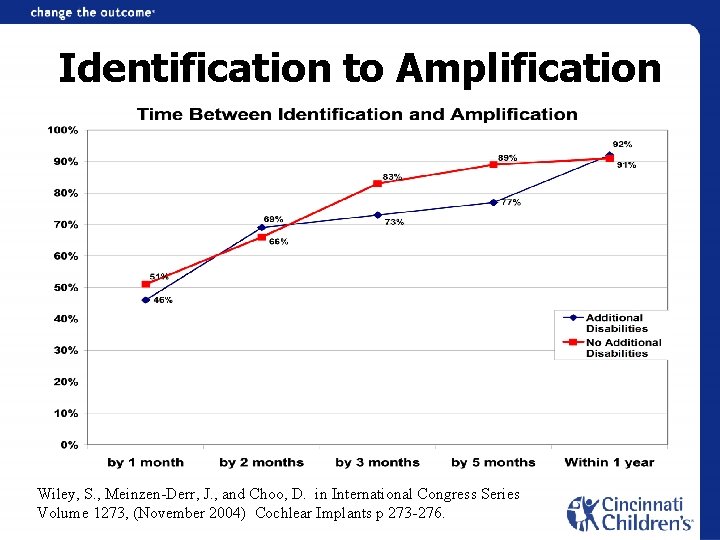
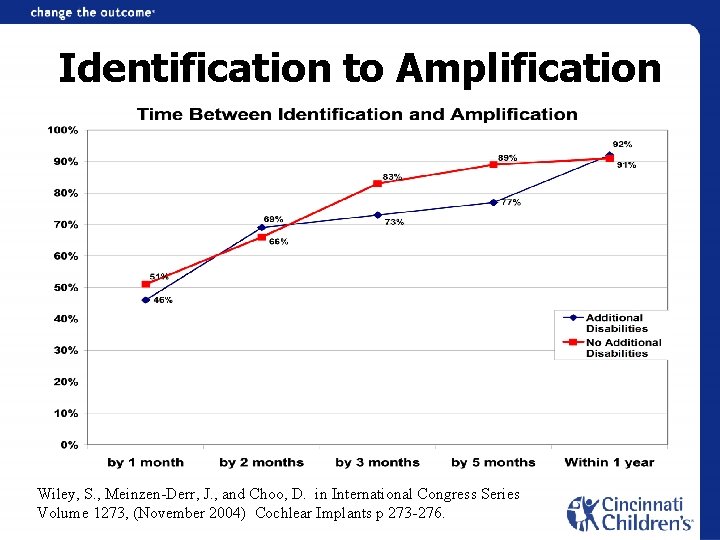
Identification to Amplification Wiley, S. , Meinzen-Derr, J. , and Choo, D. in International Congress Series Volume 1273, (November 2004) Cochlear Implants p 273 -276.
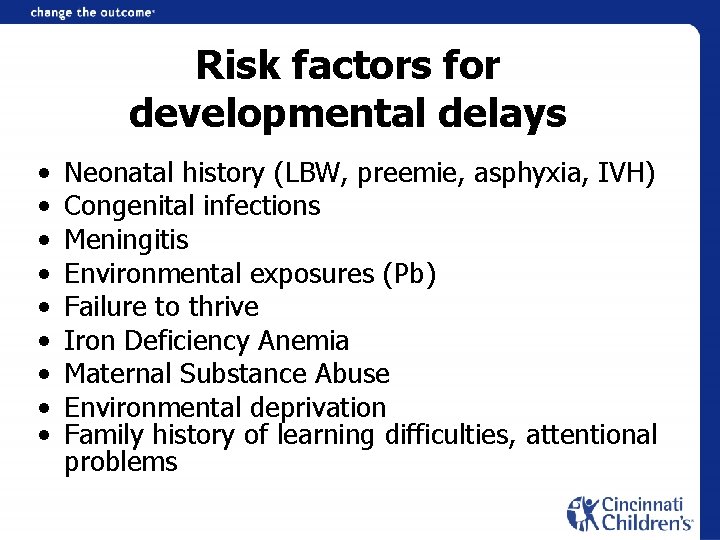
Risk factors for developmental delays • • • Neonatal history (LBW, preemie, asphyxia, IVH) Congenital infections Meningitis Environmental exposures (Pb) Failure to thrive Iron Deficiency Anemia Maternal Substance Abuse Environmental deprivation Family history of learning difficulties, attentional problems
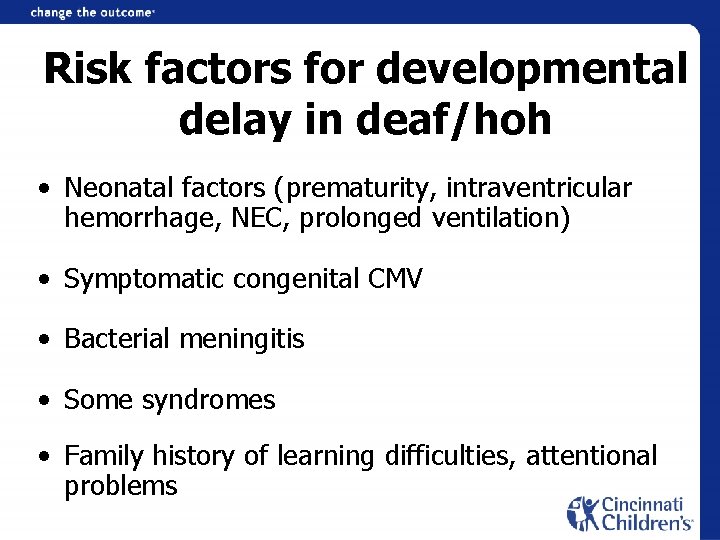
Risk factors for developmental delay in deaf/hoh • Neonatal factors (prematurity, intraventricular hemorrhage, NEC, prolonged ventilation) • Symptomatic congenital CMV • Bacterial meningitis • Some syndromes • Family history of learning difficulties, attentional problems
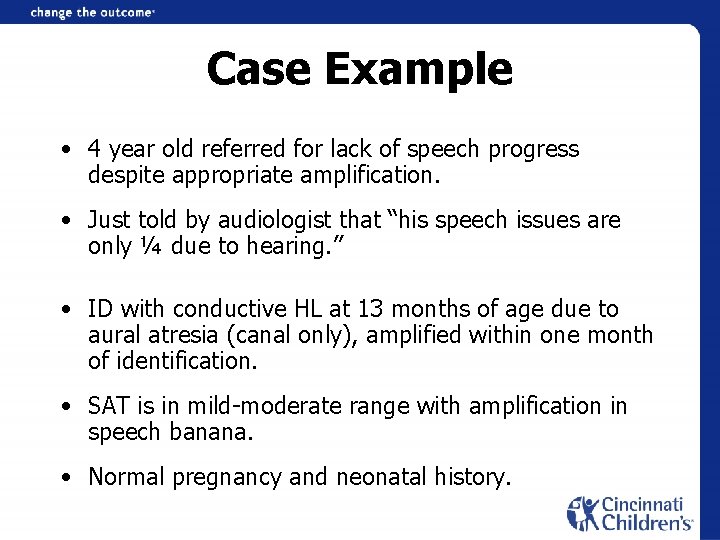
Case Example • 4 year old referred for lack of speech progress despite appropriate amplification. • Just told by audiologist that “his speech issues are only ¼ due to hearing. ” • ID with conductive HL at 13 months of age due to aural atresia (canal only), amplified within one month of identification. • SAT is in mild-moderate range with amplification in speech banana. • Normal pregnancy and neonatal history.
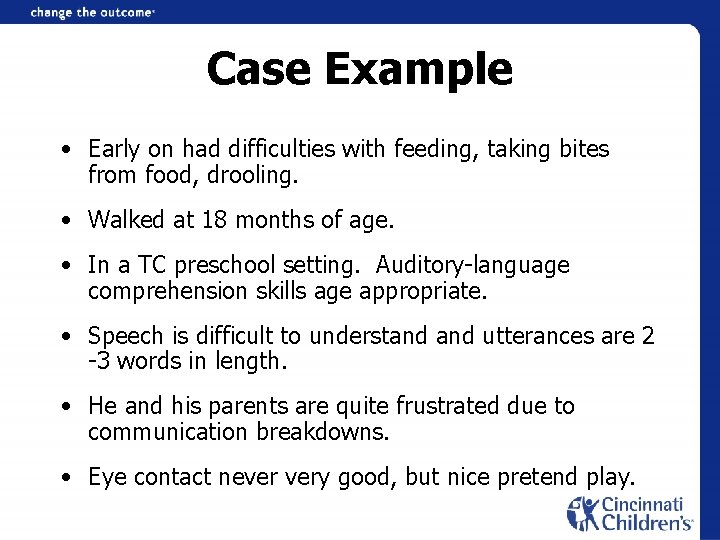
Case Example • Early on had difficulties with feeding, taking bites from food, drooling. • Walked at 18 months of age. • In a TC preschool setting. Auditory-language comprehension skills age appropriate. • Speech is difficult to understand utterances are 2 -3 words in length. • He and his parents are quite frustrated due to communication breakdowns. • Eye contact never very good, but nice pretend play.
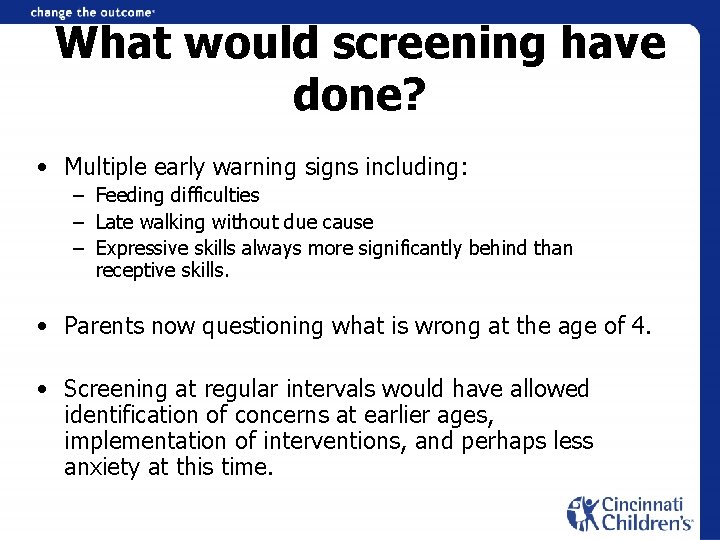
What would screening have done? • Multiple early warning signs including: – Feeding difficulties – Late walking without due cause – Expressive skills always more significantly behind than receptive skills. • Parents now questioning what is wrong at the age of 4. • Screening at regular intervals would have allowed identification of concerns at earlier ages, implementation of interventions, and perhaps less anxiety at this time.
What did he need? • Diagnosed with apraxia of speech and fine motor apraxia, monitoring eye contact following interventions • Interventions such as – – OT PT oral-motor stimulation effective expressive communication system at earlier ages • May have decreased current frustrations and parent’s surprise of the problem.
Gross Motor • Common misconception: – Children who are deaf walk later because they can’t hear. • Children generally walk between 9 -15 months of age. • Family patterns are common (all children walking at 14 -15 months of age).
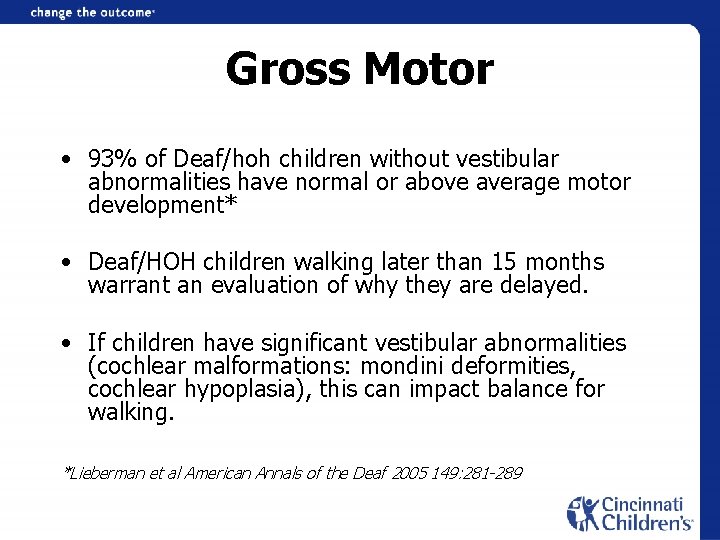
Gross Motor • 93% of Deaf/hoh children without vestibular abnormalities have normal or above average motor development* • Deaf/HOH children walking later than 15 months warrant an evaluation of why they are delayed. • If children have significant vestibular abnormalities (cochlear malformations: mondini deformities, cochlear hypoplasia), this can impact balance for walking. *Lieberman et al American Annals of the Deaf 2005 149: 281 -289
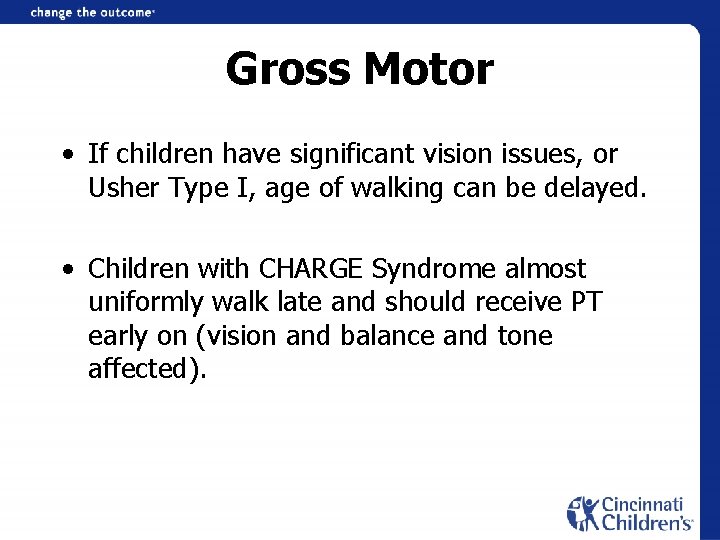
Gross Motor • If children have significant vision issues, or Usher Type I, age of walking can be delayed. • Children with CHARGE Syndrome almost uniformly walk late and should receive PT early on (vision and balance and tone affected).
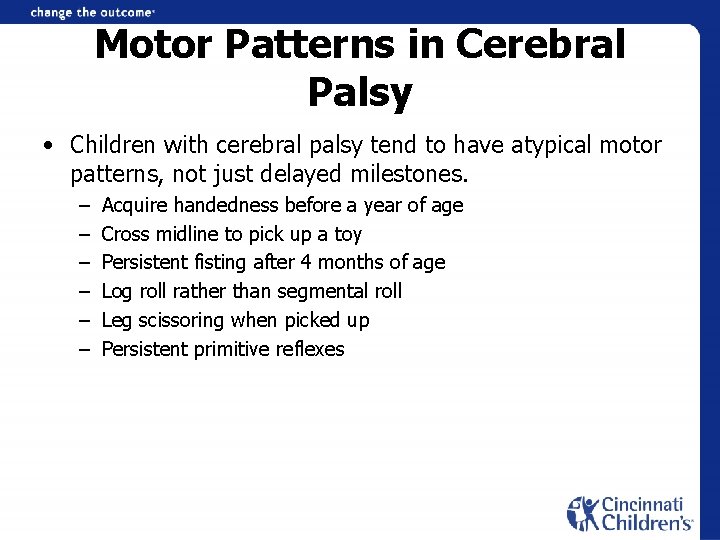
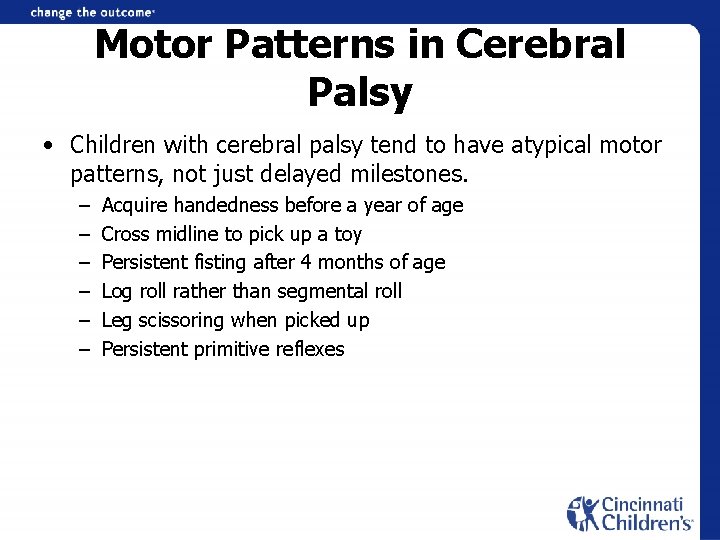
Motor Patterns in Cerebral Palsy • Children with cerebral palsy tend to have atypical motor patterns, not just delayed milestones. – – – Acquire handedness before a year of age Cross midline to pick up a toy Persistent fisting after 4 months of age Log roll rather than segmental roll Leg scissoring when picked up Persistent primitive reflexes
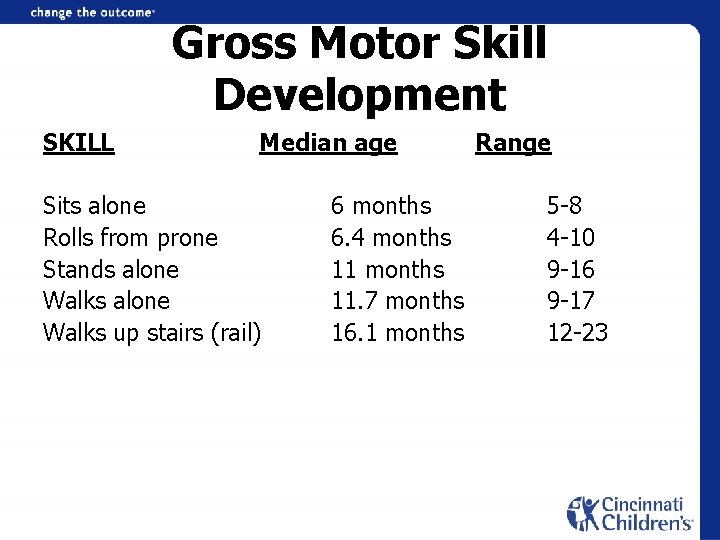
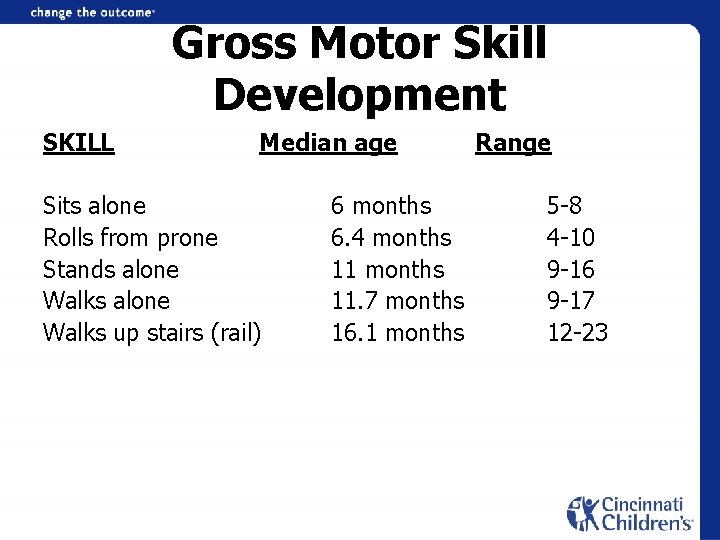
Gross Motor Skill Development SKILL Median age Sits alone Rolls from prone Stands alone Walks up stairs (rail) 6 months 6. 4 months 11. 7 months 16. 1 months Range 5 -8 4 -10 9 -16 9 -17 12 -23
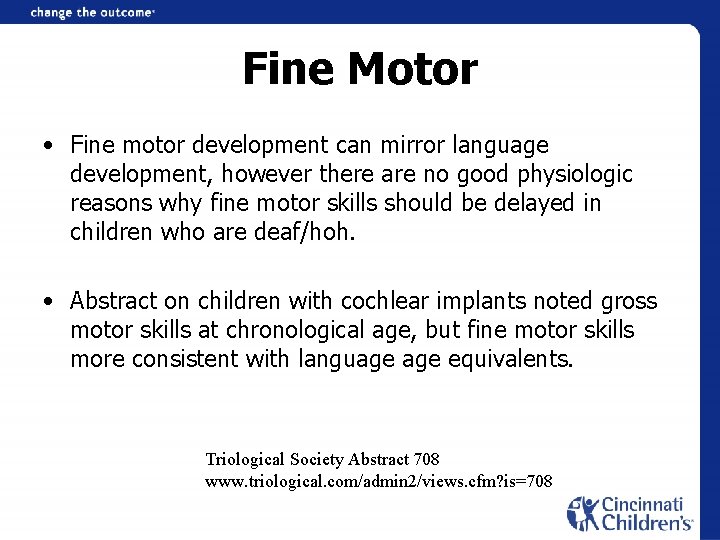
Fine Motor • Fine motor development can mirror language development, however there are no good physiologic reasons why fine motor skills should be delayed in children who are deaf/hoh. • Abstract on children with cochlear implants noted gross motor skills at chronological age, but fine motor skills more consistent with language equivalents. Triological Society Abstract 708 www. triological. com/admin 2/views. cfm? is=708
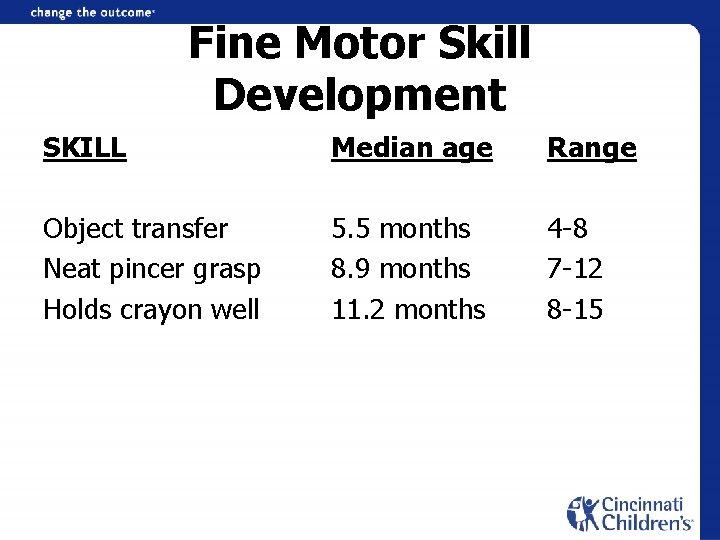
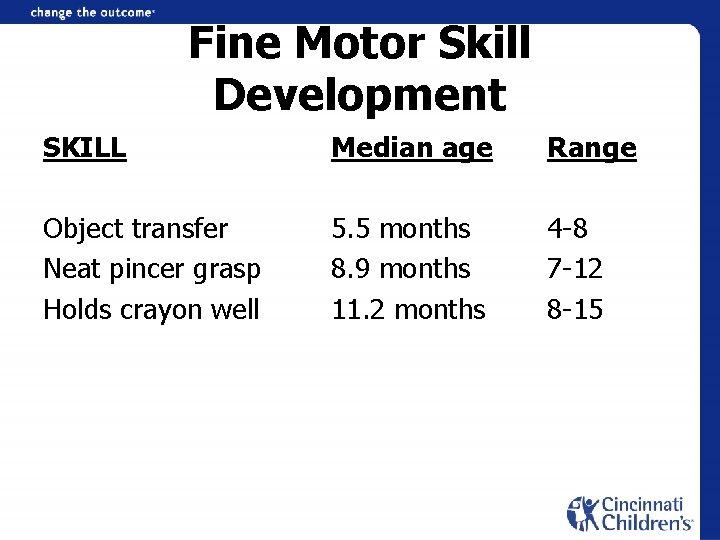
Fine Motor Skill Development SKILL Median age Range Object transfer Neat pincer grasp Holds crayon well 5. 5 months 8. 9 months 11. 2 months 4 -8 7 -12 8 -15
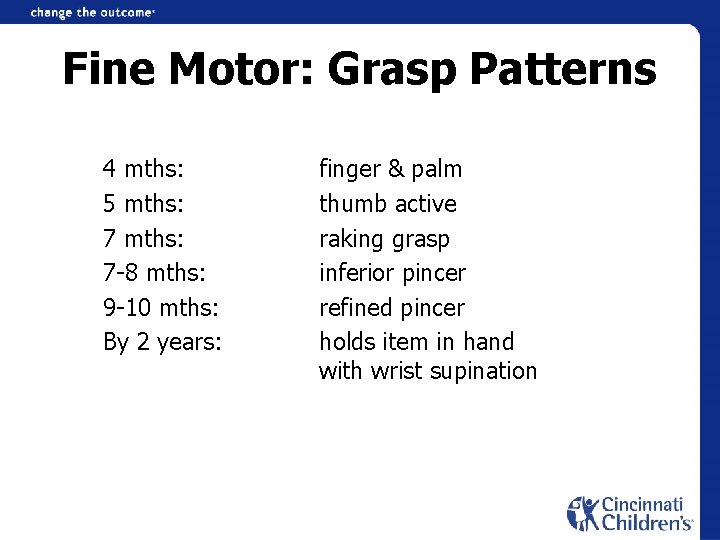
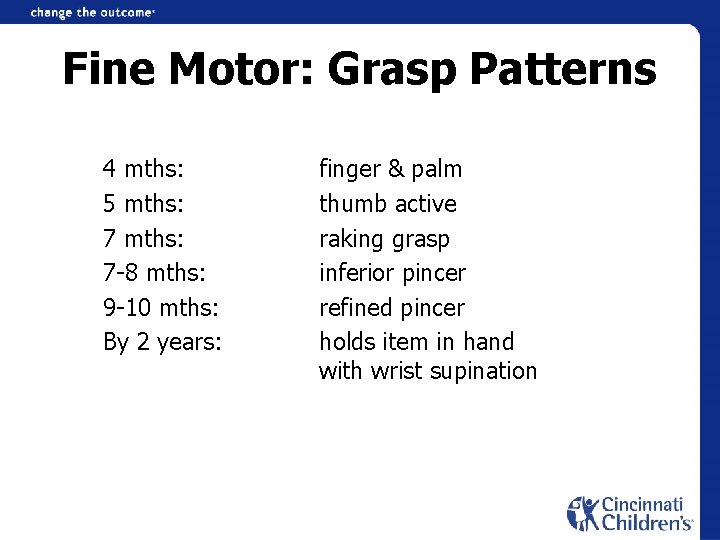
Fine Motor: Grasp Patterns 4 mths: 5 mths: 7 -8 mths: 9 -10 mths: By 2 years: finger & palm thumb active raking grasp inferior pincer refined pincer holds item in hand with wrist supination
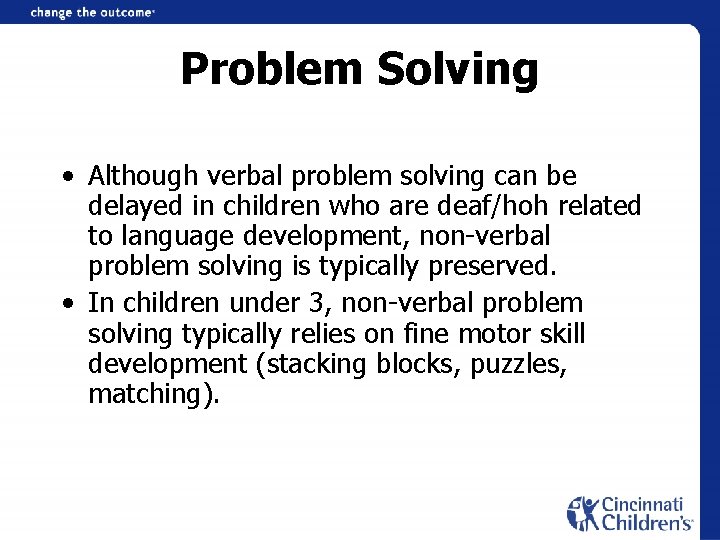
Problem Solving • Although verbal problem solving can be delayed in children who are deaf/hoh related to language development, non-verbal problem solving is typically preserved. • In children under 3, non-verbal problem solving typically relies on fine motor skill development (stacking blocks, puzzles, matching).
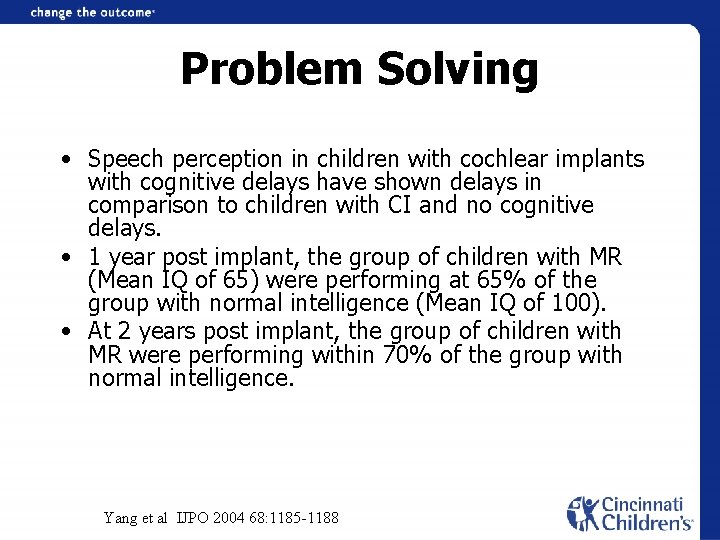
Problem Solving • Speech perception in children with cochlear implants with cognitive delays have shown delays in comparison to children with CI and no cognitive delays. • 1 year post implant, the group of children with MR (Mean IQ of 65) were performing at 65% of the group with normal intelligence (Mean IQ of 100). • At 2 years post implant, the group of children with MR were performing within 70% of the group with normal intelligence. Yang et al IJPO 2004 68: 1185 -1188
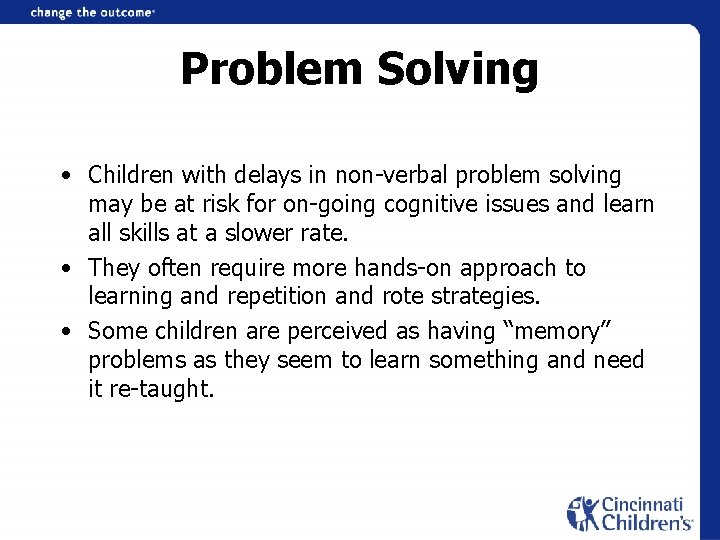
Problem Solving • Children with delays in non-verbal problem solving may be at risk for on-going cognitive issues and learn all skills at a slower rate. • They often require more hands-on approach to learning and repetition and rote strategies. • Some children are perceived as having “memory” problems as they seem to learn something and need it re-taught.

Communication/Language • Possible Red Flags (matter of degree) • Slow learning rate in spite of strong intervention; gap CA/LA widens • Can be hard to differentiate from “limited opportunity” (device use, parent involvement, personal resources, second language use, quality of program, program access, response to Rx) • Learning rate does not match “expectations” (i. e. , in relation to residual hearing or communication access) • Lack of synchrony of auditory, speech, language development
Communication/Language • Possible Red Flags: Young Child – Need for extended processing time – Qualitative differences in comprehension • Over-reliance on comprehension strategies – Extensive gaps between receptive & expressive language (in either direction) – May acquire basic vocabulary, but especially slow in acquiring: • • Relational concepts (perceptual vs. conceptual) Diverse semantic classes Question understanding Basic grammatical relations
Communication/Language • Possible Red Flags: Young Child – Limited gesture development; motor imitation difficulties – Difficulty combining modalities (receptive and/or expressive)…need for chaining • May have shifting modality preferences – Problems with retention and generalization of learned information – Word learning differences (cannot assume same associations, classification skills) – Auditory learners may focus on “gestalt” (giant words) – Perseveration; Persistent echolalia in speech and/or sign; slow changes from imitation to spontaneous productions – Atypical play development – Restricted range of pragmatic functions
Communication/Language • Possible Red Flags: Preschool • “Expectation” of non-understanding; weak meta-cognitive skills • Difficulty attending to and integrating multiple pieces of information • Atypical semantic errors (Daddy is holeing the ground with that big fork!) • Difficulties processing sequentially & planning common routines • Formulation challenges in expressive language (word storage and retrieval difficulties; sequential planning) • Social difficulties • In responding to cognitive-linguistic demands of classroom • Child temperament: mismatch?
Communication/Language • Possible Red Flags: Preschool • Processing based on contextual, extra-linguistic or non-linguistic cues for understanding (key words; predictions; global response strategy) • Unusual focus of attention • Behavioral responses increase when language is challenging • Difficulty responding to questions at varied levels of abstraction &/or supports; tracking topics in discourse
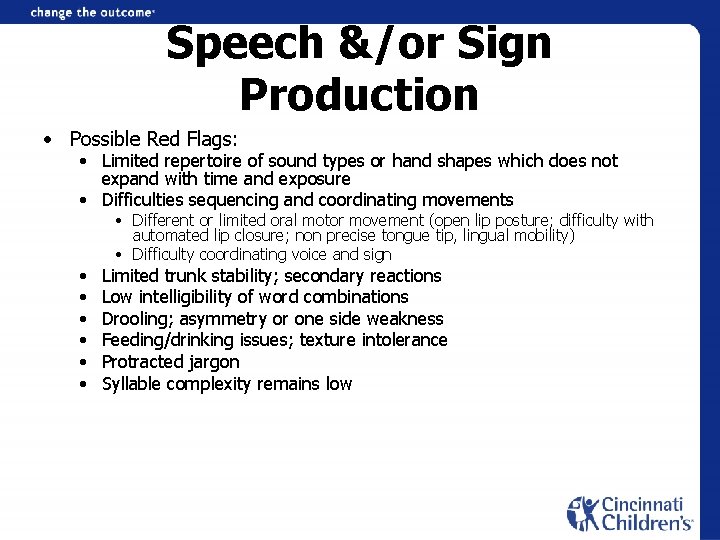
Speech &/or Sign Production • Possible Red Flags: • Limited repertoire of sound types or hand shapes which does not expand with time and exposure • Difficulties sequencing and coordinating movements • • Different or limited oral motor movement (open lip posture; difficulty with automated lip closure; non precise tongue tip, lingual mobility) • Difficulty coordinating voice and sign Limited trunk stability; secondary reactions Low intelligibility of word combinations Drooling; asymmetry or one side weakness Feeding/drinking issues; texture intolerance Protracted jargon Syllable complexity remains low
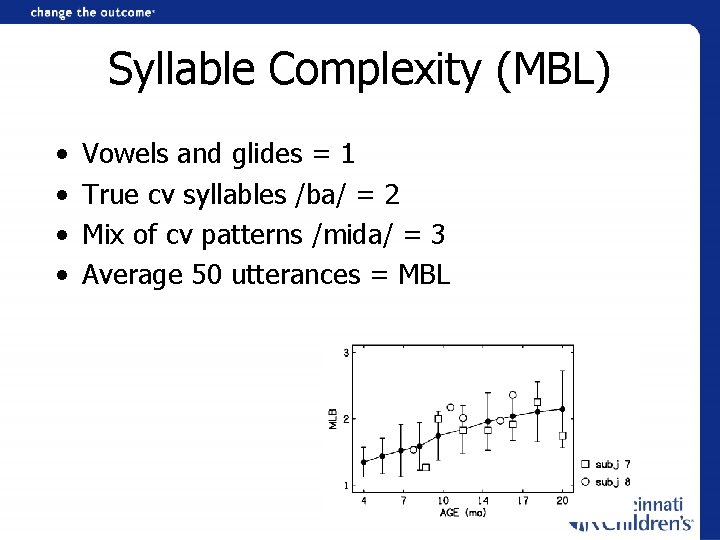
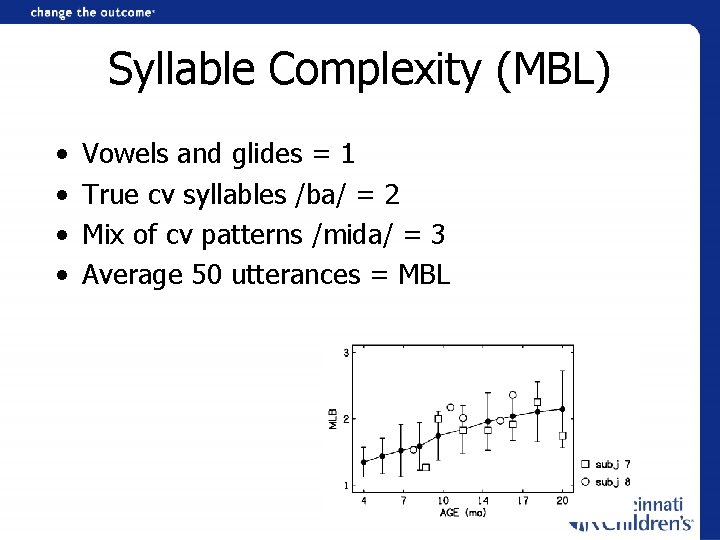
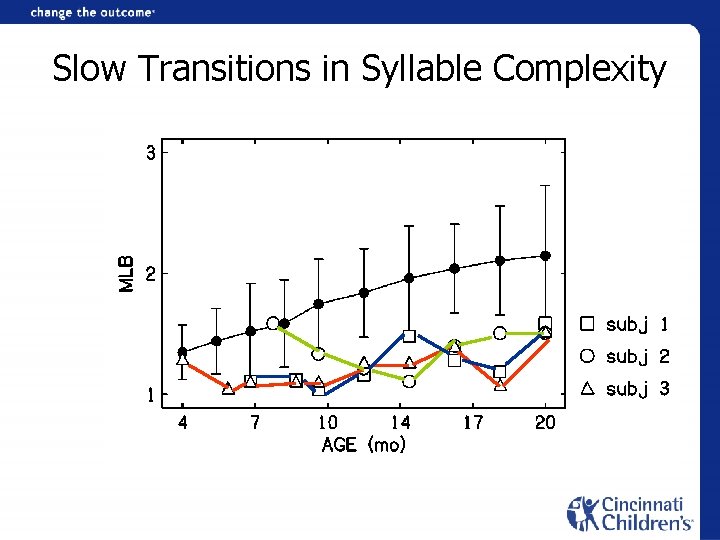
Syllable Complexity (MBL) • • Vowels and glides = 1 True cv syllables /ba/ = 2 Mix of cv patterns /mida/ = 3 Average 50 utterances = MBL
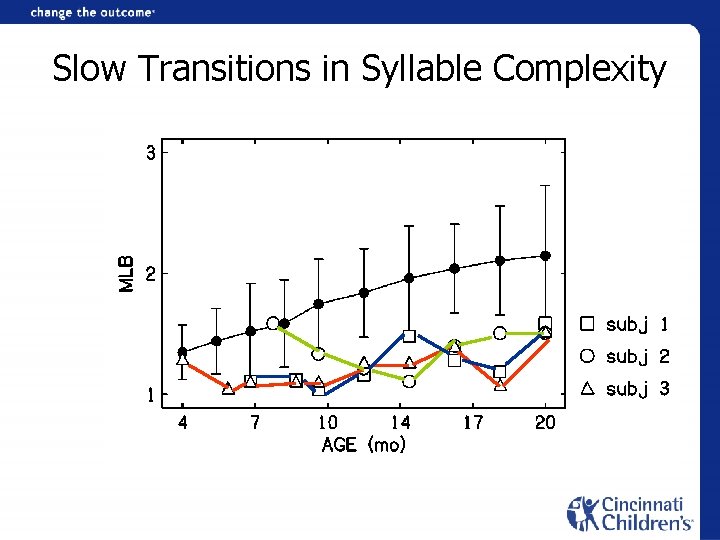
Slow Transitions in Syllable Complexity
Sensory Integration Dysfunction Definition • Sensory Integration is the organization of sensation from the body and the environment for use.
Types of Sensory Issues • Sensory Overload (hyper-reactive) – high arousal, inability to focus attention, negative affect, impulsive or defensive action • Hyporeaction – manage input by withdrawing, easily over-looked • Sensory Defensiveness – hyper-vigilant to avoid sensory overload
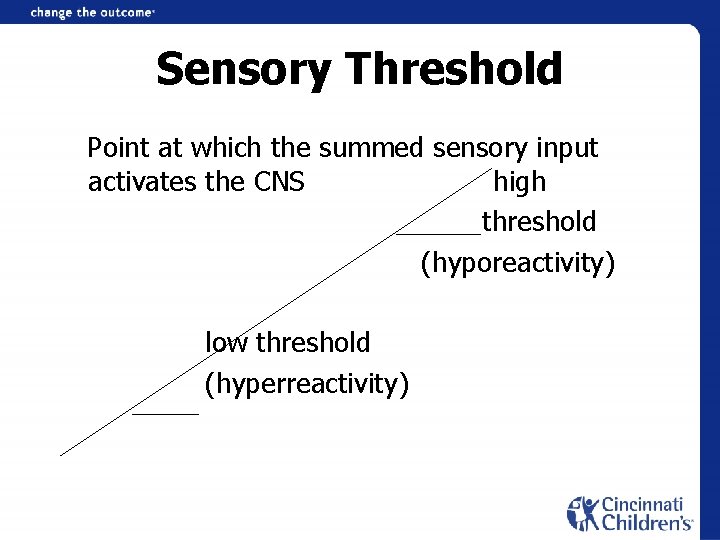
Sensory Threshold Point at which the summed sensory input activates the CNS high threshold (hyporeactivity) low threshold (hyperreactivity)
Diagnosis • Sensory profile questionnaire • Look at patterns of sensory issues (movement, vestibular, touch, auditory stimuli, visual stimuli, taste/texture) • Important to focus treatment on the pattern of issues (one treatment protocol will not help every child, must individualize programming)
Treatment • Helping parents/professionals understand the child’s responses • Modify the environment for better “fit” • Sensory diet • Child-directed • Make activities purposeful
Case Example 2 • Profoundly deaf, identified at 11 months • Developmental history of hypotonia, tactile defensiveness, motor overflow, poor eye contact, slow learning rate, limited social interaction with peers • Strong family support; optimal stimulation through sign language • Referred by preschool teacher due to concerns for low intelligibility of sign productions
Case Example 2 • Diagnostic teaching with language specialist and occupational therapist • Analysis revealed rule based sign errors (praxisrelated) – – 4 rules explained all errors Reversal of sign path Unable to cross midline Non dominant hand inaccurate
Case Example 2 • Occupational therapist observed: – – – Reduced proprioceptive perception Weak bilateral coordination and motor planning Reduced proximal trunk stability ATNR present Motor overflow and associated reactions Avoidance of crossing midline
Case Example 2 • Successive approximation based on motor complexity (break down-build up) • Increase visual and perceptual salience • Model matching side by side • Target contrastive patterns • Massed motor practice in functional contexts • Presentation to facilitate midline crossing • Guidance and support of motor plan
Case Example 2 • Motor based sign errors resolved in response to sensory integration approach • Persistent difficulties in socialization, attention and compulsive behaviors • Learned language in practiced contexts; did not generalize to social use • Strength in episodic memory used to promote social interaction, symbolic play • Team approach needed throughout school years
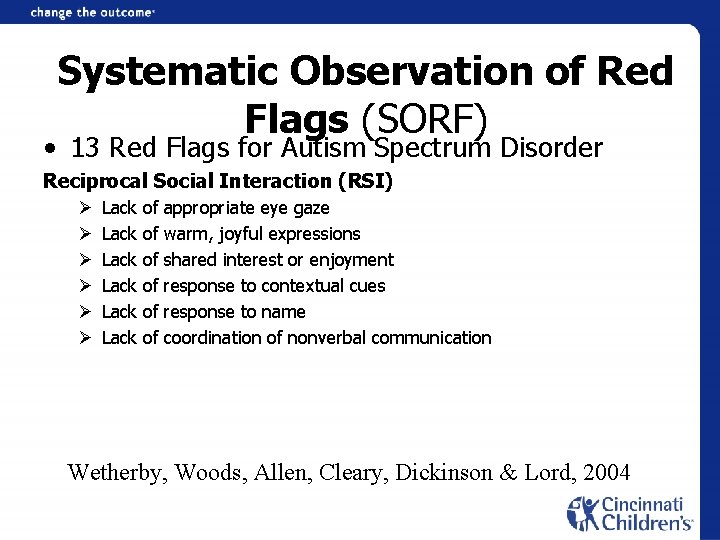
Systematic Observation of Red Flags (SORF) • 13 Red Flags for Autism Spectrum Disorder Reciprocal Social Interaction (RSI) Ø Ø Ø Lack of appropriate eye gaze Lack of warm, joyful expressions Lack of shared interest or enjoyment Lack of response to contextual cues Lack of response to name Lack of coordination of nonverbal communication Wetherby, Woods, Allen, Cleary, Dickinson & Lord, 2004
Systematic Observation of Red Flags (SORF) Communication (COM) Ø Unusual prosody Ø Lack of showing Ø Lack of pointing Ø Lack of communicative vocalizations with consonants Wetherby, Woods, Allen, Cleary, Dickinson & Lord, 2004
Systematic Observation of Red Flags (SORF) Repetitive Behaviors & Restricted Interests (RBRI) Ø Repetitive movements with objects Ø Repetitive movements or posturing of body Ø Lack of playing with a variety of toys Wetherby, Woods, Allen, Cleary, Dickinson & Lord, 2004
Visual Impairments • Deaf children are 2 -3 times more likely to develop vision problems than hearing peers (Guy et al, 2003) – 15. 3% incidence of refractive errors hearing children – 39. 1% in group of deaf children • Usher Syndrome (3 types) • Should have a full ophthalmologic evaluation • Need regular vision evaluations
Characteristics of Students with Multiple Disabilities • • Heterogeneity History of struggles Behavioral challenges High need for adult attention High need for task variation Difficulty with generalization Language and communication differences Synergistic effects of combined challenges
Rules to Guide Instruction: • Need for differentiated instruction and expectations (will not learn the same material in same time with same methods) • Focus on the donut, not the hole • Build communication one link at a time (task analysis); Carefully address comprehension • Celebrate successes great and small Dr. T. Jones, Gallaudet University
Rules to Guide Instruction: • If a dead man can do it, it is not an appropriate objective • May benefit from “break down-build up” in language learning • On-line analysis and revision is critical (Cycles of hypothesize – observe – modify – observe – hypothesize…) • Help the child/family organize for learning • Use meaningful contexts to make concepts explicit Dr. T. Jones, Gallaudet University