Recurrent PID Subsequent STI and Reproductive Health Outcomes
Recurrent PID, Subsequent STI, and Reproductive Health Outcomes: Findings from the PID Evaluation and Clinical Health (PEACH) Study Maria Trent, MD, MPH Debra Bass, MS Roberta Ness, MD, MPH Catherine Haggerty, Ph. D, MPH Funding: Centers for Disease Control and Prevention: K 01 DP 001128 -02; Agency for Healthcare Research and Quality Development: HS 08358 -05
Disclosures • I have no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or providers (s) of commercial services discussed in this CME activity. • I do not intend to discuss off-label use of products in this presentation
Background • PID is a common reproductive health disorder • Associated with significant reproductive morbidity: – Tubal infertility – Ectopic pregnancy – Chronic pelvic pain (CPP) • Risk estimates of morbidity based on Scandinavian cohort of PID inpatients enrolled 1960 -1984 – Subsequent shifts in the biological organisms causing PID – Management shifted to outpatient setting • Re-analysis of the impact of recurrent PID and STIs warranted
Objective • To examine the risk of longitudinal adverse outcomes associated with recurrent STIs and PID among urban American women with mildmoderate PID • To determine the potential impact of adolescence on the observed longitudinal outcomes

Methods • Secondary data analysis • PID Evaluation and Clinical Health (PEACH)Study – Women 14 -38 years with mild-moderate PID – Urban Settings in United States – Randomized to inpatient/outpatient treatment – Baseline interview & gynecologic exam (endometrial biopsies, STI testing) – Visits at 5 and 30 days – Telephone interview quarterly x 84 months

Approach to Analysis PEACH 831 Women 14 -38 years Mild-Moderate PID Randomized to Inpatient/ Outpatient Arms Main PEACH Analysis No Difference in Outcomes by group Re-Analysis based on Recurrent PID/STI Adolescent Sub-Analysis (≤ 19 yrs) N=209
Methods • Data evaluated using bivariate & multiple regression analyses • Analysis approved by Johns Hopkins IRB
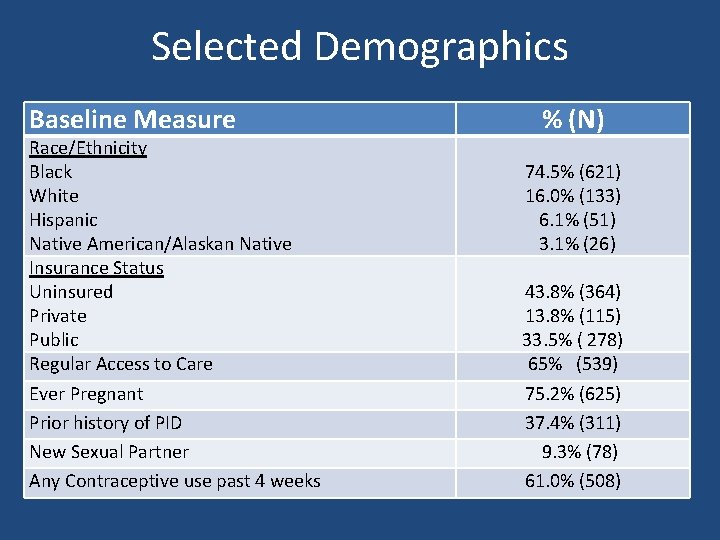
Selected Demographics Baseline Measure Race/Ethnicity Black White Hispanic Native American/Alaskan Native Insurance Status Uninsured Private Public Regular Access to Care Ever Pregnant Prior history of PID New Sexual Partner Any Contraceptive use past 4 weeks % (N) 74. 5% (621) 16. 0% (133) 6. 1% (51) 3. 1% (26) 43. 8% (364) 13. 8% (115) 33. 5% ( 278) 65% (539) 75. 2% (625) 37. 4% (311) 9. 3% (78) 61. 0% (508)
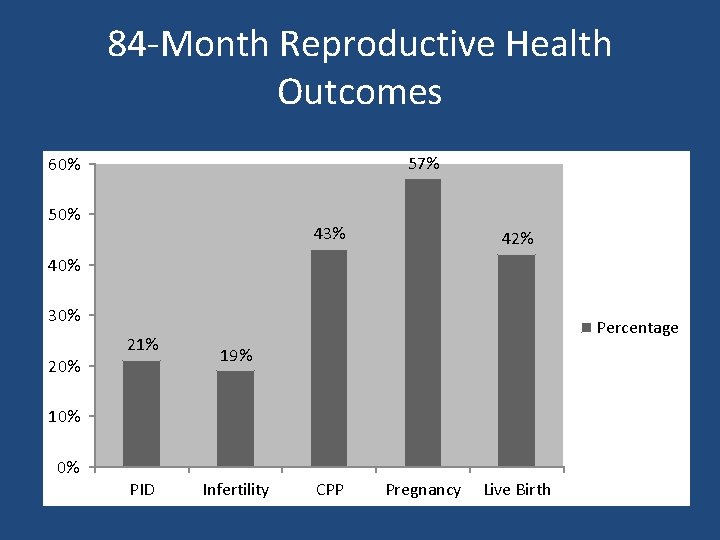
84 -Month Reproductive Health Outcomes 57% 60% 50% 43% 42% 40% 30% 21% Percentage 19% 10% 0% PID Infertility CPP Pregnancy Live Birth
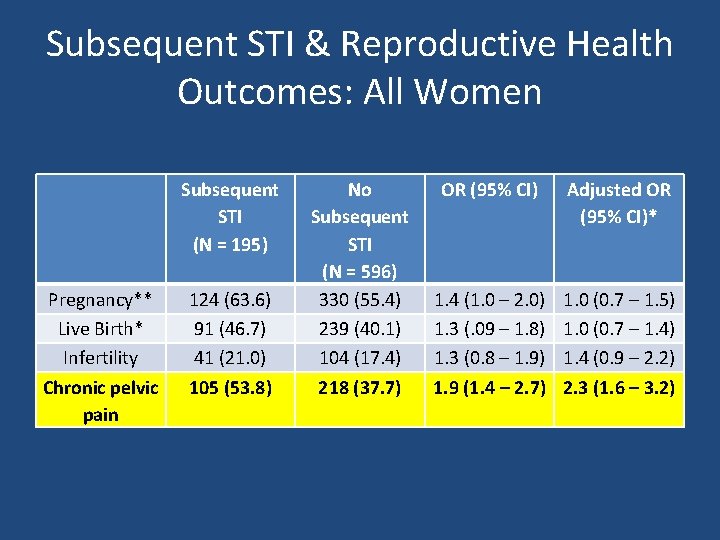
Subsequent STI & Reproductive Health Outcomes: All Women Subsequent STI (N = 195) Pregnancy** Live Birth* Infertility Chronic pelvic pain 124 (63. 6) 91 (46. 7) 41 (21. 0) 105 (53. 8) No Subsequent STI (N = 596) 330 (55. 4) 239 (40. 1) 104 (17. 4) 218 (37. 7) OR (95% CI) Adjusted OR (95% CI)* 1. 4 (1. 0 – 2. 0) 1. 3 (. 09 – 1. 8) 1. 3 (0. 8 – 1. 9) 1. 9 (1. 4 – 2. 7) 1. 0 (0. 7 – 1. 5) 1. 0 (0. 7 – 1. 4) 1. 4 (0. 9 – 2. 2) 2. 3 (1. 6 – 3. 2)
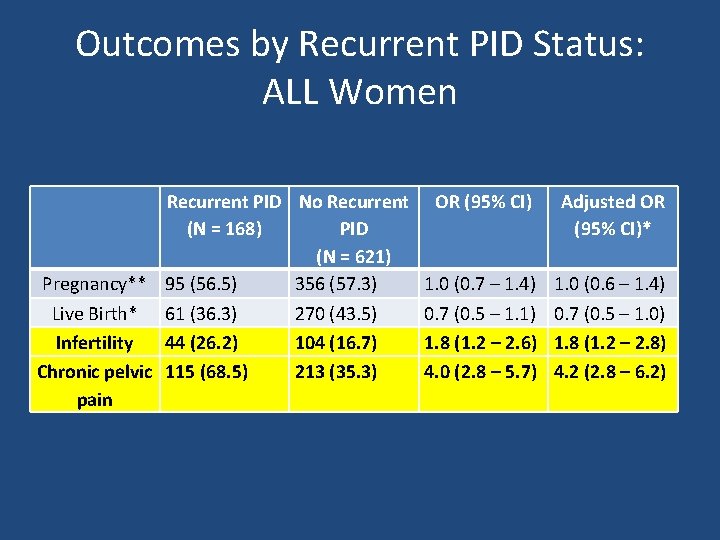
Outcomes by Recurrent PID Status: ALL Women Recurrent PID No Recurrent (N = 168) PID (N = 621) Pregnancy** 95 (56. 5) 356 (57. 3) Live Birth* 61 (36. 3) 270 (43. 5) Infertility 44 (26. 2) 104 (16. 7) Chronic pelvic 115 (68. 5) 213 (35. 3) pain OR (95% CI) Adjusted OR (95% CI)* 1. 0 (0. 7 – 1. 4) 0. 7 (0. 5 – 1. 1) 1. 8 (1. 2 – 2. 6) 4. 0 (2. 8 – 5. 7) 1. 0 (0. 6 – 1. 4) 0. 7 (0. 5 – 1. 0) 1. 8 (1. 2 – 2. 8) 4. 2 (2. 8 – 6. 2)
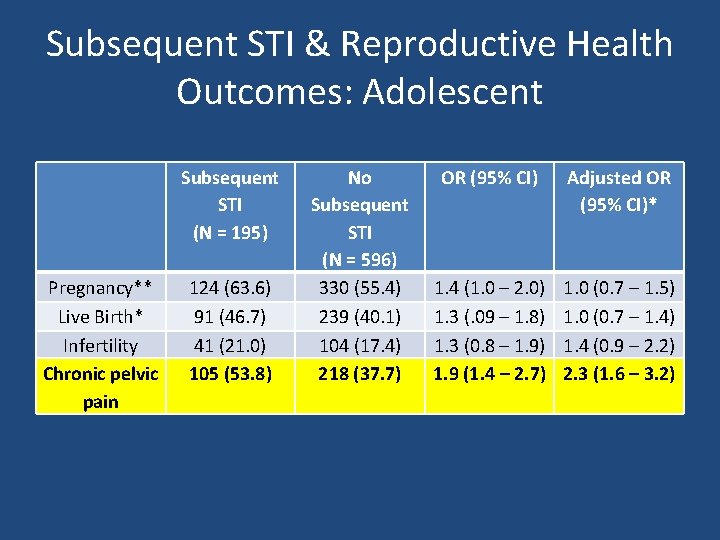
Subsequent STI & Reproductive Health Outcomes: Adolescent Subsequent STI (N = 195) Pregnancy** Live Birth* Infertility Chronic pelvic pain 124 (63. 6) 91 (46. 7) 41 (21. 0) 105 (53. 8) No Subsequent STI (N = 596) 330 (55. 4) 239 (40. 1) 104 (17. 4) 218 (37. 7) OR (95% CI) Adjusted OR (95% CI)* 1. 4 (1. 0 – 2. 0) 1. 3 (. 09 – 1. 8) 1. 3 (0. 8 – 1. 9) 1. 9 (1. 4 – 2. 7) 1. 0 (0. 7 – 1. 5) 1. 0 (0. 7 – 1. 4) 1. 4 (0. 9 – 2. 2) 2. 3 (1. 6 – 3. 2)
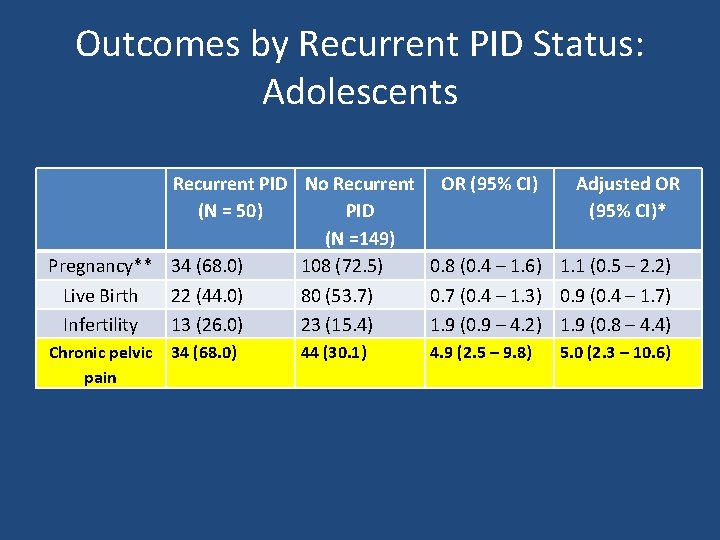
Outcomes by Recurrent PID Status: Adolescents Recurrent PID No Recurrent OR (95% CI) Adjusted OR (N = 50) PID (95% CI)* (N =149) Pregnancy** 34 (68. 0) 108 (72. 5) 0. 8 (0. 4 – 1. 6) 1. 1 (0. 5 – 2. 2) Live Birth 22 (44. 0) 80 (53. 7) 0. 7 (0. 4 – 1. 3) 0. 9 (0. 4 – 1. 7) Infertility 13 (26. 0) 23 (15. 4) 1. 9 (0. 9 – 4. 2) 1. 9 (0. 8 – 4. 4) Chronic pelvic pain 34 (68. 0) 44 (30. 1) 4. 9 (2. 5 – 9. 8) 5. 0 (2. 3 – 10. 6)
Conclusions • Women with recurrent PID are more likely to report infertility and CPP at 84 months • Substantiates the relationship between recurrent PID and adverse – Modern microbiology – Outpatient and inpatient care approaches • Highlights CPP as a major adverse outcome and recurrent lower genital tract infection (STI) as a key contributor • Supports to the concept of tertiary prevention – Upper genital tract disease = smaller, well defined public health – Adolescents are also an important sub-target
Limitations • Limited Generalizability – Demographics – Trial Participation • Contraception • Clinical Criteria for PID – Endometrial biopsies – Mimics clinical practice • Self-Reported Longitudinal Outcomes – Supported by medical record review
Implications • Young women with a history of PID are a clearly defined target group for public health intervention. • Acute PID should prompt linkage of affected patients to tailored STI risk-reduction services to prevent the adverse outcomes associated with PID
- Slides: 16