Recognition and management of maternal sepsis Sepsis Sepsis


















- Slides: 20

Recognition and management of maternal sepsis

Sepsis • Sepsis is now the leading cause of direct maternal deaths in the UK • Often more difficult to diagnose in pregnancy and postnatally with insidious onset followed by rapid deterioration

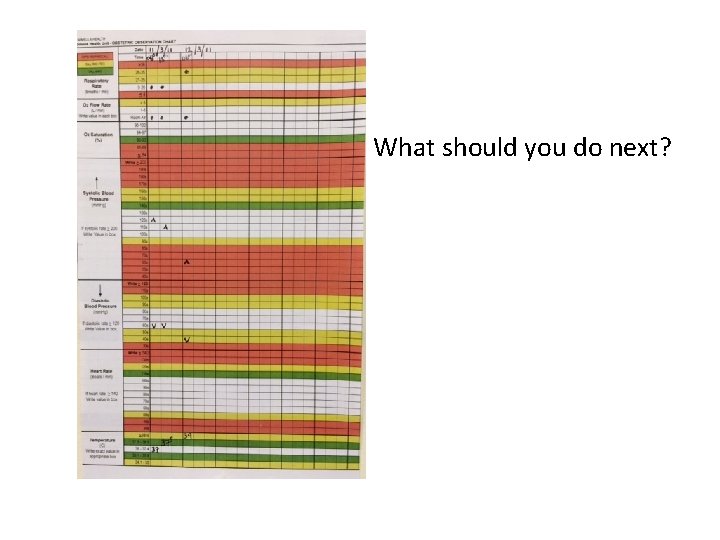
CMACE – recognition • Plotting Clinical observations (heart rate, blood pressure, respiratory rate and temperature) regularly in women with suspected sepsis may help in the recognition of sepsis

Signs of sepsis • Tachycardia (HR > 100 bpm) • Low oxygen saturations (less than 95% on air) • Raised respiratory rate (RR > 24) • Poor peripheral perfusion (cap refill > 2 seconds) • High or low temp (> 38 o. C or < 35 o. C) • Clamminess • Hypotension (systolic BP < 90 mm. Hg) • Rash or mottled skin • Confusion

Symptoms of sepsis • Diarrhoea • Vaginal discharge • Vomiting • Wound infection • Abdominal pain • Dysuria • Rash • Low urine output (less than 0. 5 ml/kg/hr) • Sore throat • Sputum

Group A streptococcus • The most common cause of maternal death from infection in the UK • Community-based infection – 5– 30% asymptomatic carriers on throat or skin – streptococcal sore throat: one of most common bacterial infections of childhood • All maternal deaths either had, or worked with, young children

Risk factors for group A streptococcal sepsis • Working with or having young children • Immediate postnatal period • Winter

Additional risk factors for sepsis • Retained products of conception • Manual removal • Following an invasive intrauterine procedure (e. g. amnio, CVS) • Prolonged ruptured membranes • Cervical suture • Impaired immunity • Caesarean section • Diabetes mellitus • Premature labour • Water birth • Obesity
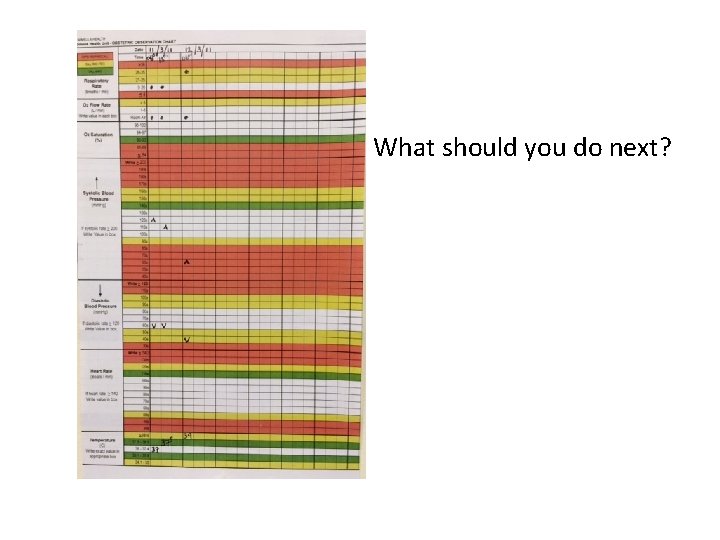
What should you do next?

Initial management • Call for help • Airway – high-flow O 2 • Breathing • Circulation – IV access – IV fluids – Blood tests

Monitoring
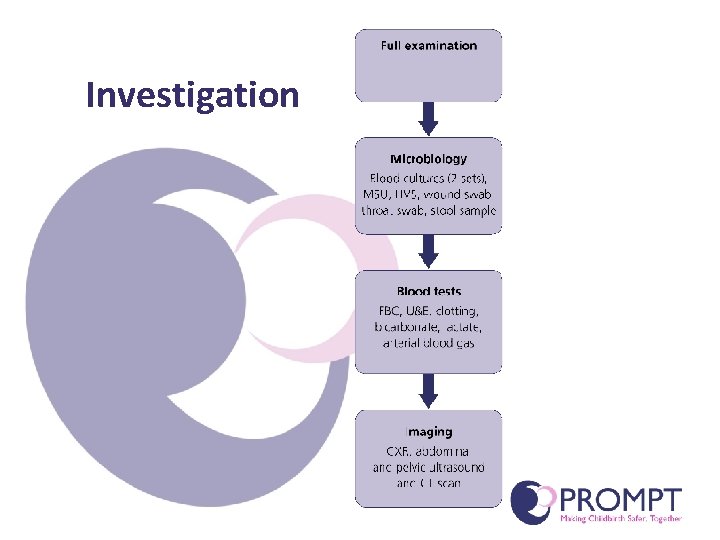
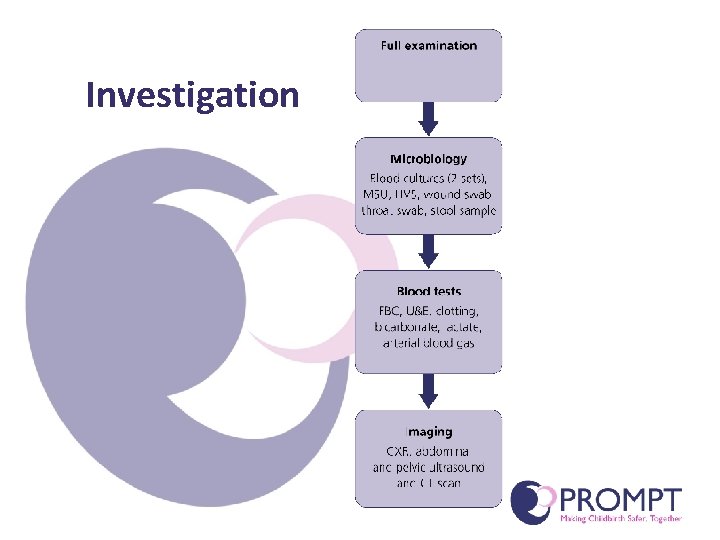
Investigation

Treatment

Prompt IV antibiotic treatment • High-dose broad-spectrum IV antibiotic therapy (e. g. 1. 5 g cefuroxime and 500 mg metronidazole), in accordance with known patient allergies, should be given ASAP • Administration should not be delayed for the results of microbiological testing • If possible, take blood cultures prior to antibiotics, but the commencement of antibiotic treatment should not be delayed. • A microbiologist should be contacted early for advice • If already extremely ill, deteriorates or does not improve within 24 hours of treatment, then additional or alternative IV antibiotics such as gentamicin and clindamycin or tazocin should be used

Fluid resuscitation • Hypotension and/or an elevated serum lactate level (> 4 mmol/l) should be treated with IV fluid bolus • Give an initial minimum fluid challenge of 20 ml/kg IV crystalloid – A 75 kg septic patient should be given at least 1500 ml of intravenous crystalloid stat • If there is no improvement in the hypotension and/or the serum lactate level following the fluid bolus, the patient should be transferred to intensive care

Surviving Sepsis Campaign (SSC) • Implementation of the ‘resuscitation bundle’ within the first 6 hours associated with reductions in mortality from sepsis

Surviving Sepsis Campaign: ‘the resuscitation bundle’ Daniels R, Nutbeam T, Mc. Namara G, Galvin C. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emergency Medicine Journal. 2011 May 19; 28(6): 507– 12.

Sepsis Six • Developed in the UK in an attempt to simplify the Surviving Sepsis Campaign guidance and improve uptake • Implementation of the Sepsis Six has been associated with reduced mortality and an increase in the implementation of the full SSC ‘resuscitation bundle’

Sepsis Six • • • Give 100% O 2 Take blood cultures Give IV broad-spectrum antibiotics Give IV fluid therapy Measure lactate and haemoglobin Measure hourly urine output (catheter) All within the FIRST HOUR Daniels R, Nutbeam T, Mc. Namara G, Galvin C. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emergency Medicine Journal. 2011 May 19; 28(6): 507– 12.

Summary • Be aware of sepsis and beware sepsis • If sepsis is suspected in the community, urgent referral is indicated • The onset of life-threatening sepsis can be insidious, with extremely rapid clinical deterioration • High-dose IV antibiotics ASAP • Fluid resuscitation • Measure lactate • Early liaison with microbiology and intensive care