REACTIVE ARTHRITIS Definition Reactive arthritis Re A refers










- Slides: 34
REACTIVE ARTHRITIS
Definition • Reactive arthritis (Re. A) refers to acute nonpurulent arthritis complicating an infection elsewhere in the body • In recent years, the term has been used primarily to refer to spondyloarthropathies following enteric or urogenital infections and occurring predominantly in individuals with the histocompatibility antigen HLAB 27
Reiter’s Syndrome • First reported in 1916 by Hans Reiter as a clinical triad of arthritis, nongonococcal urethritis, and conjunctivitis. • The definition of Reiter’s syndrome has been evolving. The term has been used interchangeably with “reactive arthritis, ” • In 1981 the American Rheumatism Association defined the syndrome by the following criteria: – A peripheral arthritis lasting longer than one month associated with urethritis or cervicitis or diarrhea.
ETIOLOGY AND PATHOGENESIS • The first bacterial infection noted to be causally related to Re. A was S. flexneri. An outbreak of shigellosis among Finnish troops in 1944 resulted in numerous cases of Re. A
REACTIVE ARTHRITIS • Postveneral: Chlamydia trachomatis • Postdysentric: Shigella, Salmonella, Yersinia, and Campylobacter, Clostridium difficile, Ureaplasma urealyticum
EPIDEMIOLOGY • Re. A occurs predominantly in individuals who have inherited the B 27 gene; in most series, 60 to 85% of patients are B 27 positive • In epidemics of arthritogenic bacterial infection, e. g. , S. flexneri, it has been estimated that Re. A develops in ~20% of exposed B 27 -positive individuals
EPIDEMIOLOGY • 18 to 40 years of age • sex ratio in Re. A following enteric infection is nearly 1: 1 • whereas venereally acquired Re. A is predominantly confined to men
PATHOLOGY • Synovial histology is similar to that of other inflammatory arthropathies • Enthesitis is a common clinical finding
ETIOLOGY AND PATHOGENESIS • Most, if not all, of the triggering organisms produce lipopolysaccharide (LPS) and share a capacity to attack mucosal surfaces, to invade host cells, and survive intracellularly
ETIOLOGY AND PATHOGENESIS • Antigens from Chlamydia, Yersinia, Salmonella, and Shigella have been shown to be present in the synovium and/or synovial fluid leukocytes of patients with Re. A for long periods following the acute attack
ETIOLOGY AND PATHOGENESIS • T cells that specifically respond to antigens of the inciting organism are typically found in inflamed synovium but not in peripheral blood of patients with Re. A • The role of HLA-B 27 in Re. A also remains to be determined
CLINICAL FEATURES • The clinical manifestations of Re. A constitute a spectrum that ranges from an isolated, transient monarthritis to severe multisystem disease • Antecedent infection 1 to 4 weeks before the onset of symptoms • Constitutional symptoms are common
CLINICAL FEATURES • The musculoskeletal symptoms are usually acute in onse • Arthritis is usually asymmetric and additive • The joints of the lower extremities, especially the knee, ankle, and foot joints are the most common sites of involvement, but the wrist and fingers can be involved as well
CLINICAL FEATURES • The arthritis is usually quite painful, and tense joint effusions are not uncommon, especially in the knee • Dactylitis, or "sausage digit” • Tendinitis and fasciitis are particularly characteristic lesion: Achilles insertion, the plantar fascia • Spinal and low-back pain are quite common




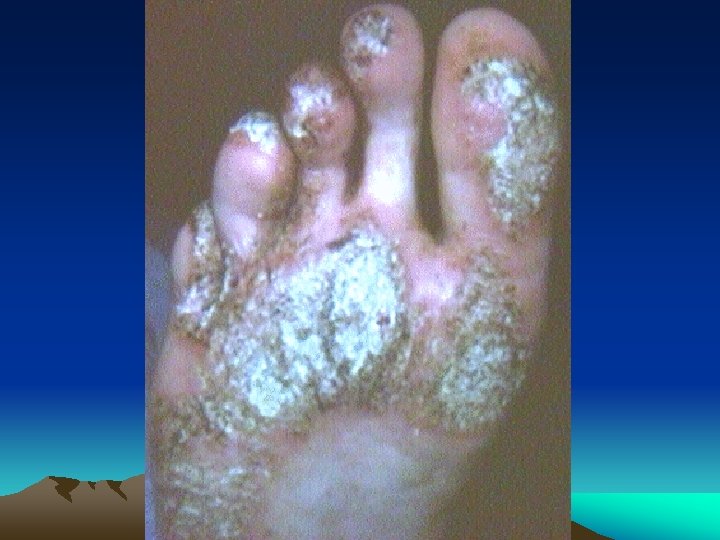
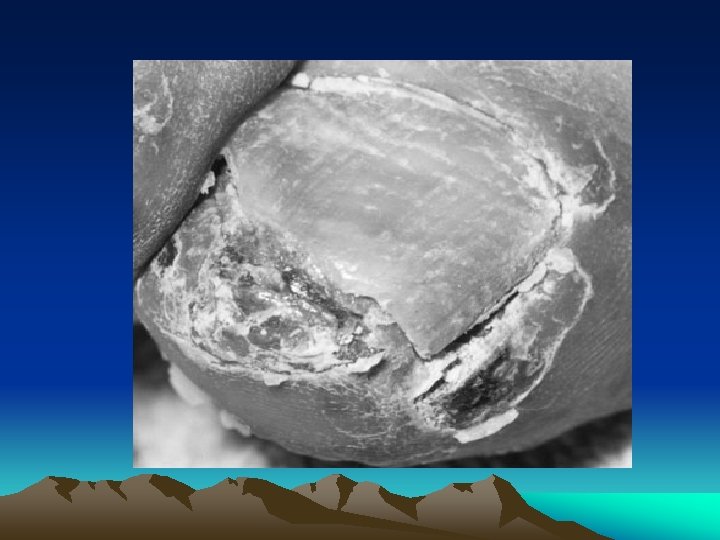
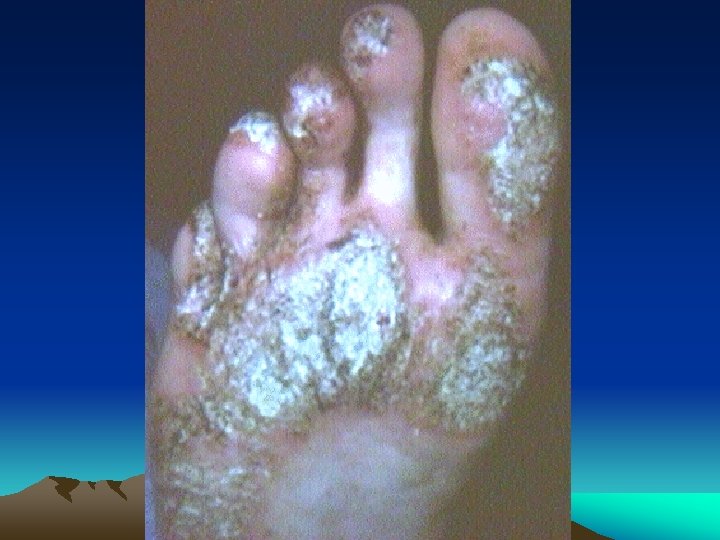
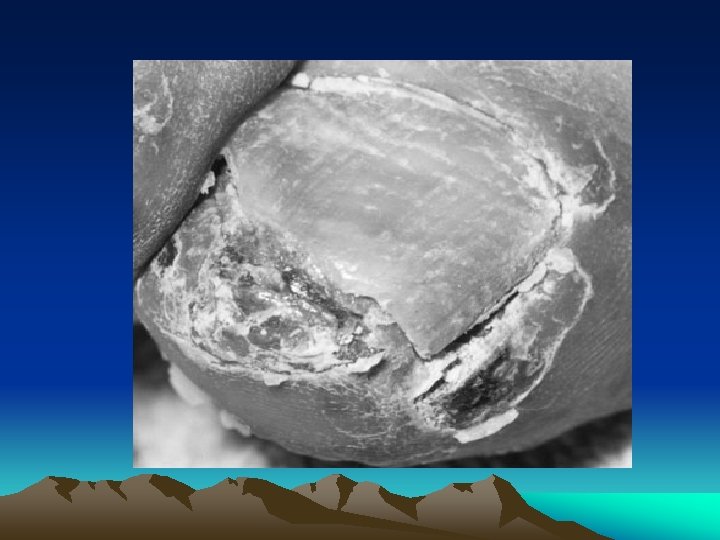
CLINICAL FEATURES • Urogenital lesions: urethritis, Prostatitis cervicitis or salpingitis • Eye: conjunctivitis, anterior uveitis • Mucocutaneous lesions: Oral ulcers keratoderma blenorrhagica, circinate balanitis, Nail changes • Heart: cardiac conduction defects, aortic insufficiency


LABORATORY FINDINGS • ESR • CRP • HLA-B 27
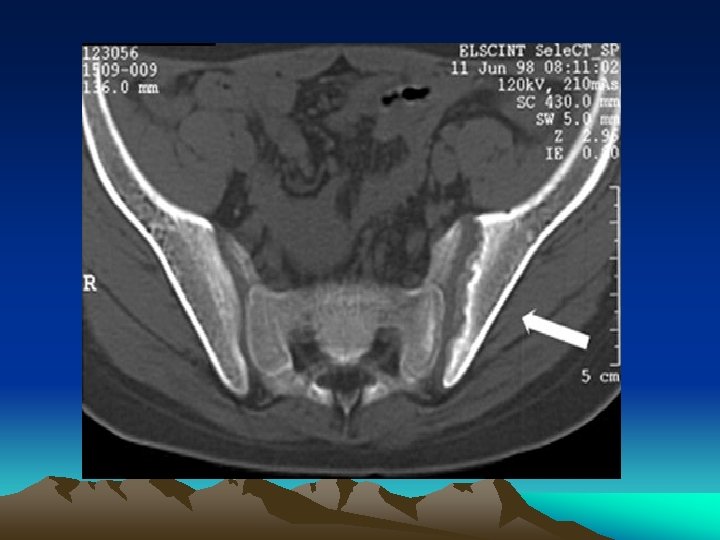
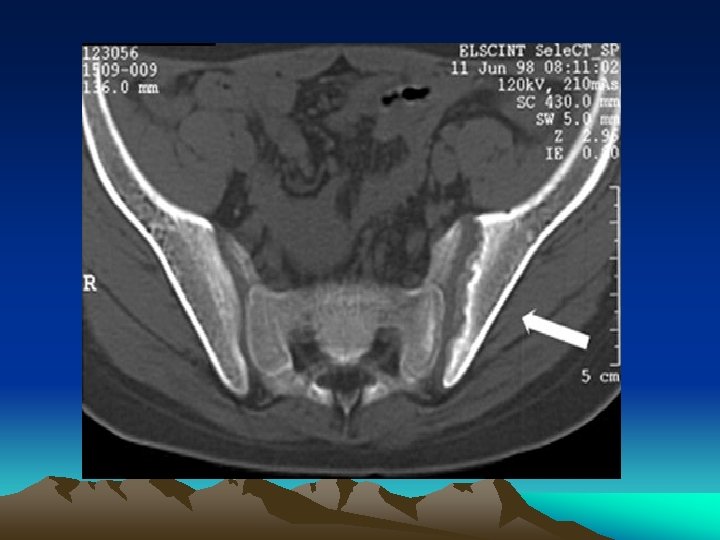
Imaging • Early disease: – Soft tissue swelling. – Reactive new bone formation, not joint erosion. – Linear periostitis and periosteal spurs
Imaging • Spinal changes: – Asymmetric paravertebral ossification of lower thoracic and upper lumbar vertebrae. – Sacroiliitis is the single most important hallmark of Reiter’s and other spondyloarthropathies. Up to 70 % of chronic Reiter’s patients will show sacroiliac changes on lumbar spine examination




DIAGNOSIS • Re. A is a clinical diagnosis • No definitively diagnostic laboratory test or radiographic finding • The diagnosis should be entertained in any patient with an acute inflammatory, asymmetric, additive arthritis or tendinitis • Synovial fluid aspiration and analysis may be helpful in excluding septic or crystalinduced arthritis.
TREATMENT • • • NSAIDs(Indomethacin 150 mg) Doxycycline Minocycline Corticosteroids Sulfasalazine MTX
Course • Long-term follow-up studies suggest that some joint symptoms persist in 30 to 60% of patients with Re. A • Recurrences of the acute syndrome are common(25%) • Secondary AS