Rationale for Radiation Therapy for Nerve Denervation Ron
- Slides: 23
Rationale for Radiation Therapy for Nerve Denervation Ron Waksman, Issi Barbash Washington Hospital Center
Ron Waksman, MD §Consulting Fee §Abbott Laboratories §Biotronik, Inc. §Boston Scientific Corporation §Medtronic, Inc. §Merck and Company, Inc.
§ Honoraria § Abbott Laboratories § Boston Scientific Corporation § Medtronic, Inc. Consulting Fee § Merck and Company, Inc.
Background • Renal sympathetic efferent and afferent lie immediately adjacent to the wall of the renal arteries • Historical experience of radical surgical approaches for sympathetic denervation were successful in lowering BP with the cost of high rates of morbidity and mortality • Renal sympathetic denervation was achieved more recently with a percutaneous catheter based approach utilizing radio frequency ablation
Limitations of RF-ablation mediated-renal denervation • Potential damage to vascular endothelium with late vascular stenosis • Inconsistent Efficacy • Localized effect to the location of ablation and need for multiple ablations • Long procedure time • Pain during treatment
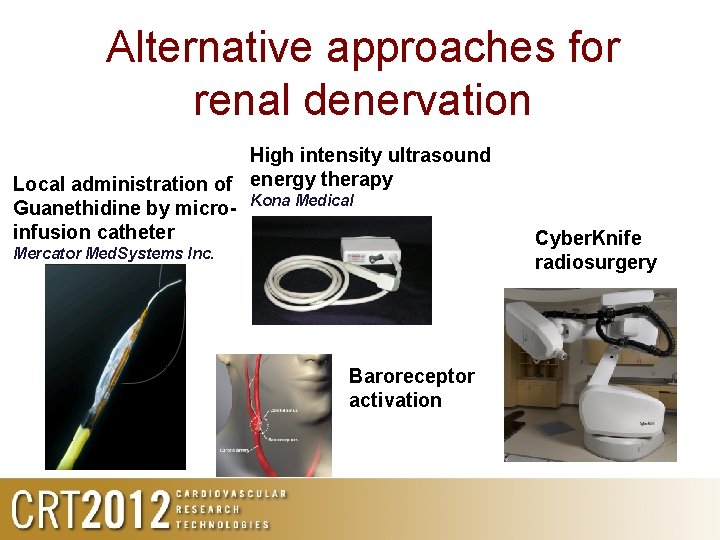
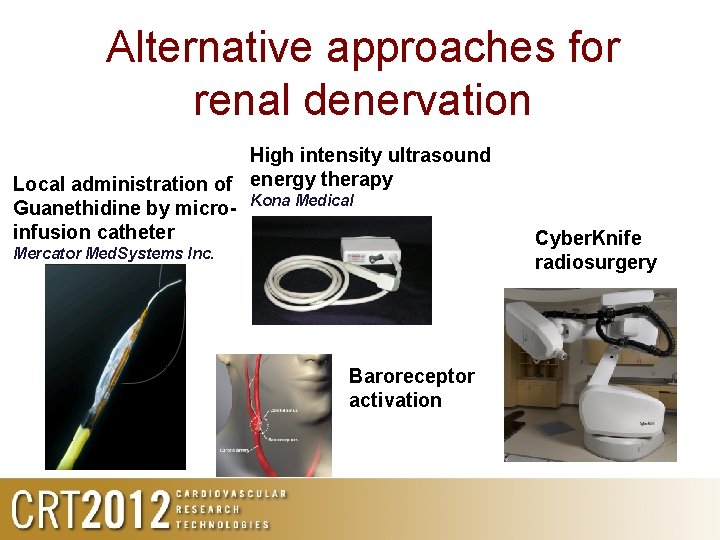
Alternative approaches for renal denervation High intensity ultrasound Local administration of energy therapy Guanethidine by micro- Kona Medical infusion catheter Mercator Med. Systems Inc. Baroreceptor activation Cyber. Knife radiosurgery
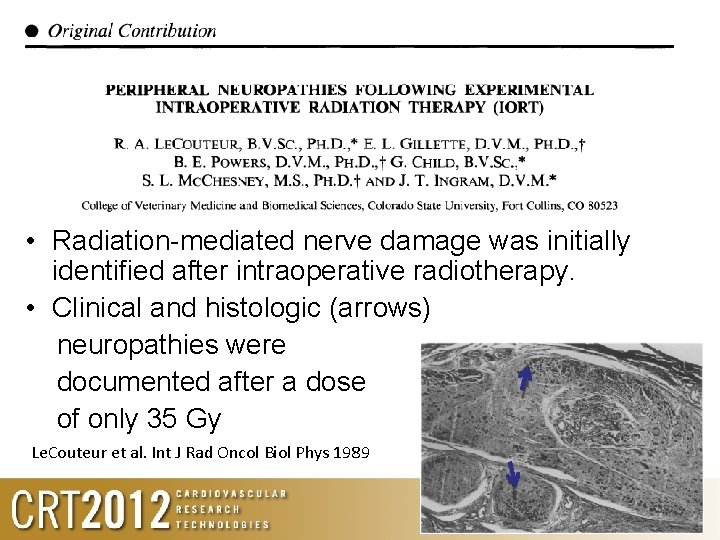
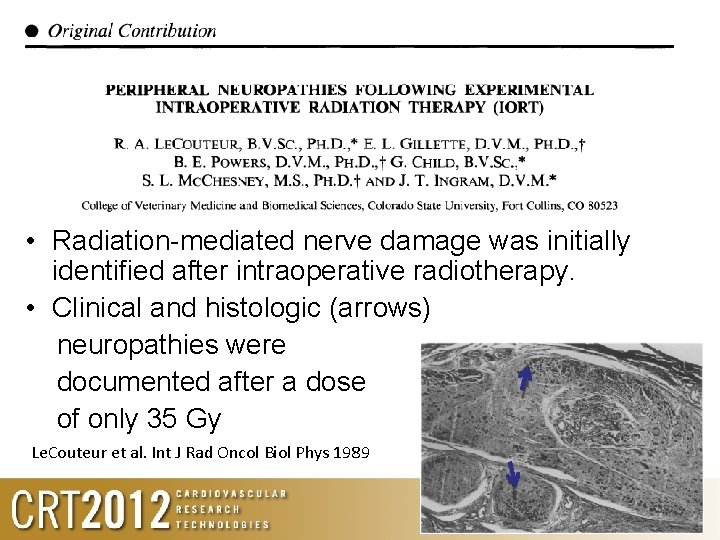
• Radiation-mediated nerve damage was initially identified after intraoperative radiotherapy. • Clinical and histologic (arrows) neuropathies were documented after a dose of only 35 Gy Le. Couteur et al. Int J Rad Oncol Biol Phys 1989
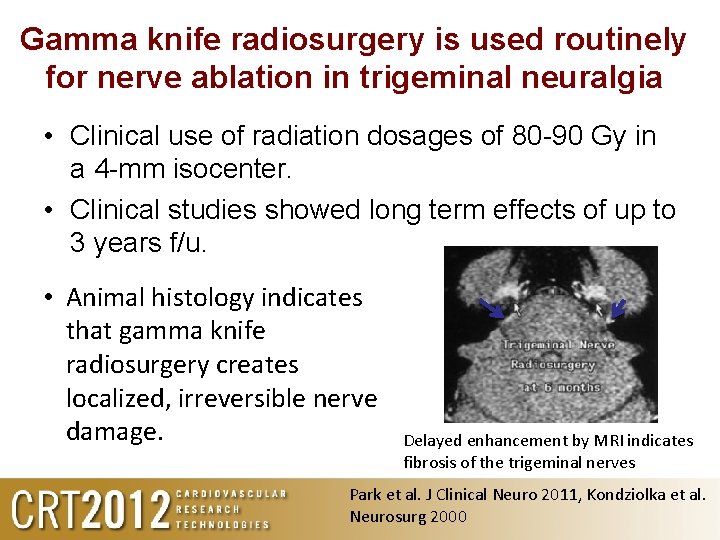
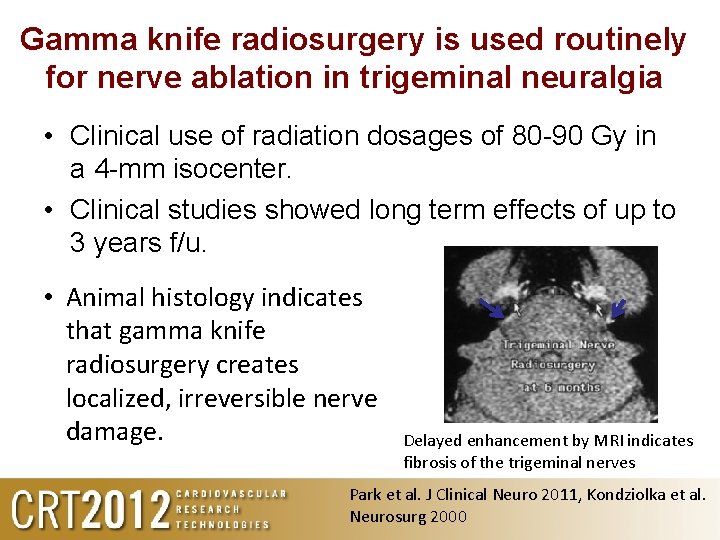
Gamma knife radiosurgery is used routinely for nerve ablation in trigeminal neuralgia • Clinical use of radiation dosages of 80 -90 Gy in a 4 -mm isocenter. • Clinical studies showed long term effects of up to 3 years f/u. • Animal histology indicates that gamma knife radiosurgery creates localized, irreversible nerve damage. Delayed enhancement by MRI indicates fibrosis of the trigeminal nerves Park et al. J Clinical Neuro 2011, Kondziolka et al. Neurosurg 2000
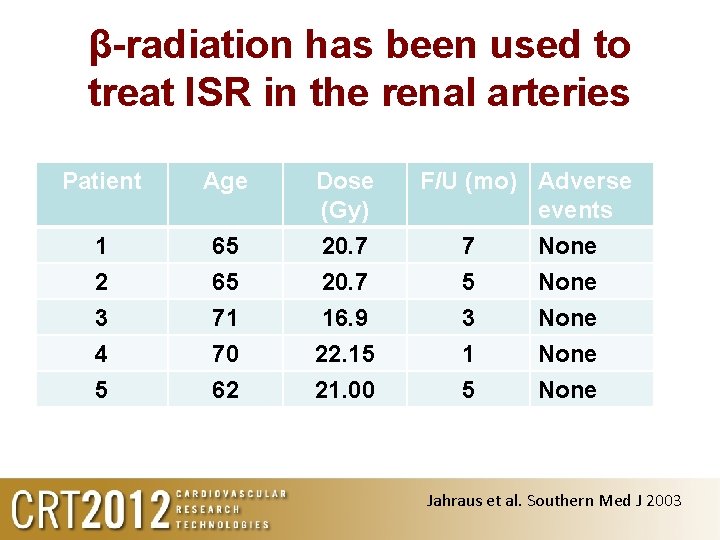
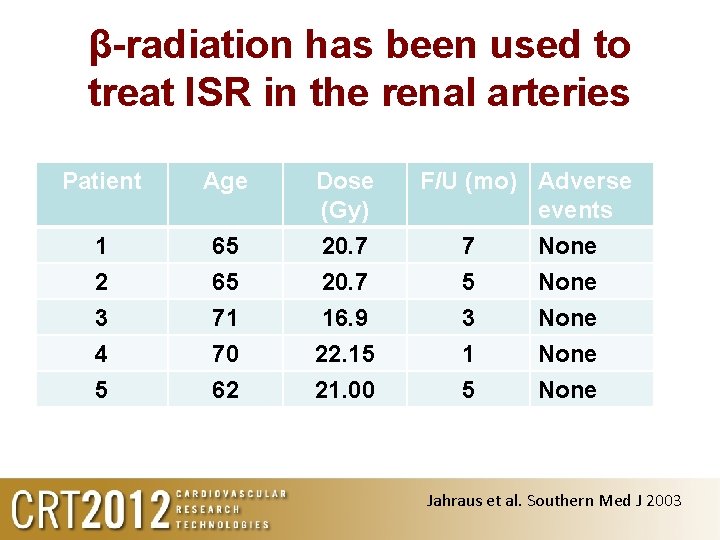
β-radiation has been used to treat ISR in the renal arteries Patient Age Dose (Gy) 1 2 3 4 5 65 65 71 70 62 20. 7 16. 9 22. 15 21. 00 F/U (mo) Adverse events 7 5 3 1 5 None None Jahraus et al. Southern Med J 2003
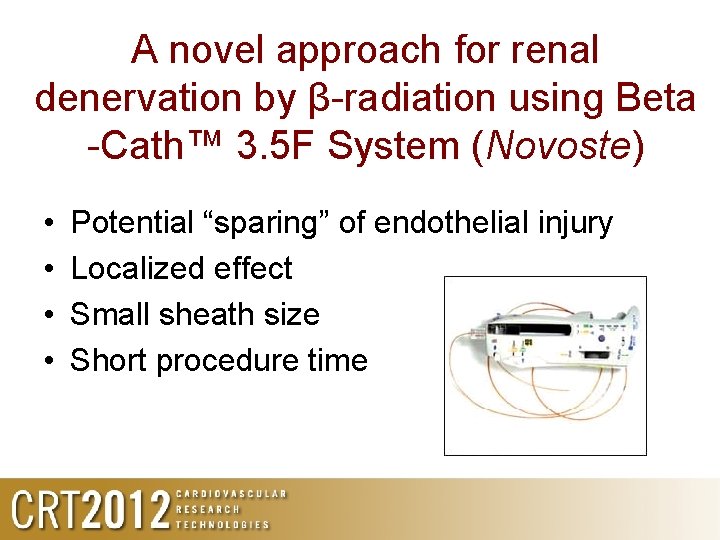
A novel approach for renal denervation by β-radiation using Beta -Cath™ 3. 5 F System (Novoste) • • Potential “sparing” of endothelial injury Localized effect Small sheath size Short procedure time
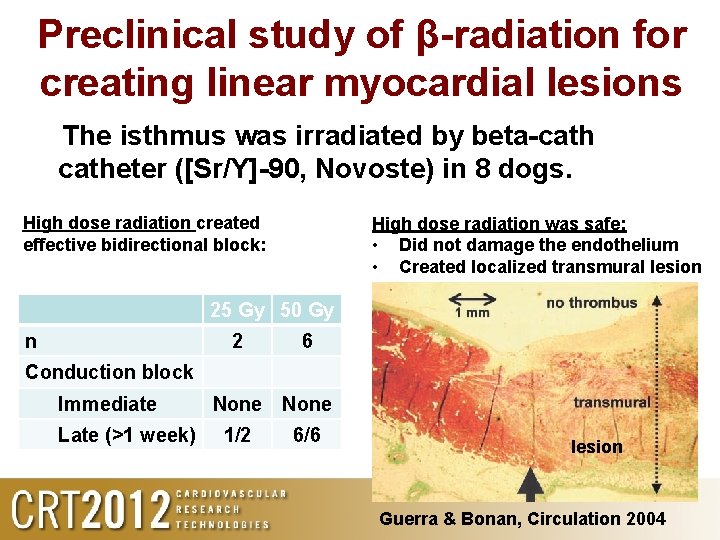
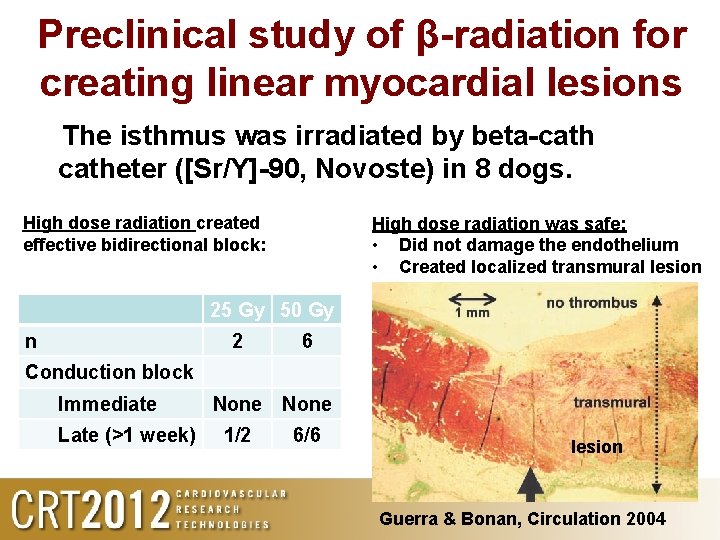
Preclinical study of β-radiation for creating linear myocardial lesions The isthmus was irradiated by beta-catheter ([Sr/Y]-90, Novoste) in 8 dogs. High dose radiation created effective bidirectional block: High dose radiation was safe: • Did not damage the endothelium • Created localized transmural lesion 25 Gy 50 Gy n 2 6 Conduction block Immediate Late (>1 week) None 1/2 6/6 lesion Guerra & Bonan, Circulation 2004
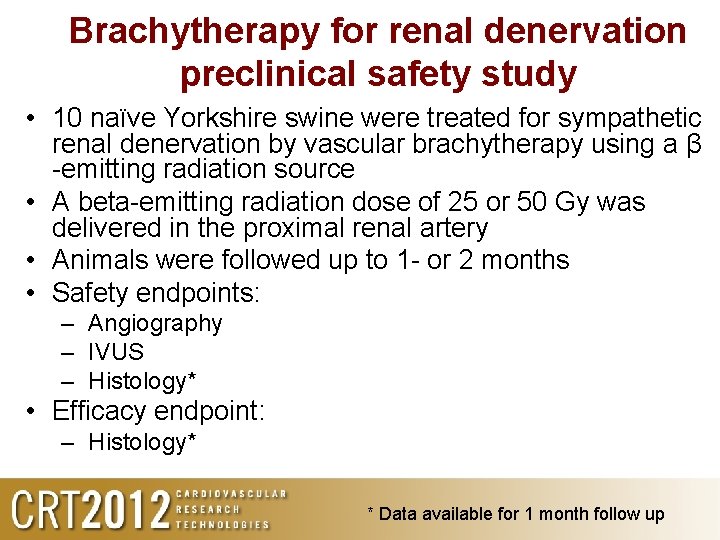
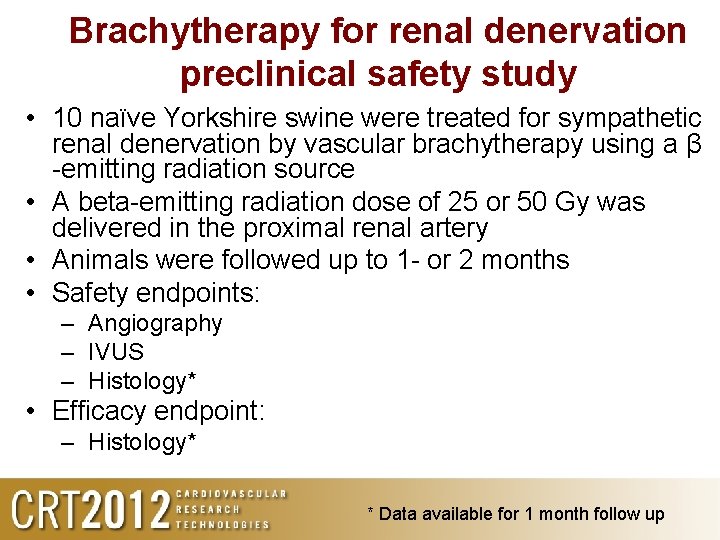
Brachytherapy for renal denervation preclinical safety study • 10 naïve Yorkshire swine were treated for sympathetic renal denervation by vascular brachytherapy using a β -emitting radiation source • A beta-emitting radiation dose of 25 or 50 Gy was delivered in the proximal renal artery • Animals were followed up to 1 - or 2 months • Safety endpoints: – Angiography – IVUS – Histology* • Efficacy endpoint: – Histology* * Data available for 1 month follow up
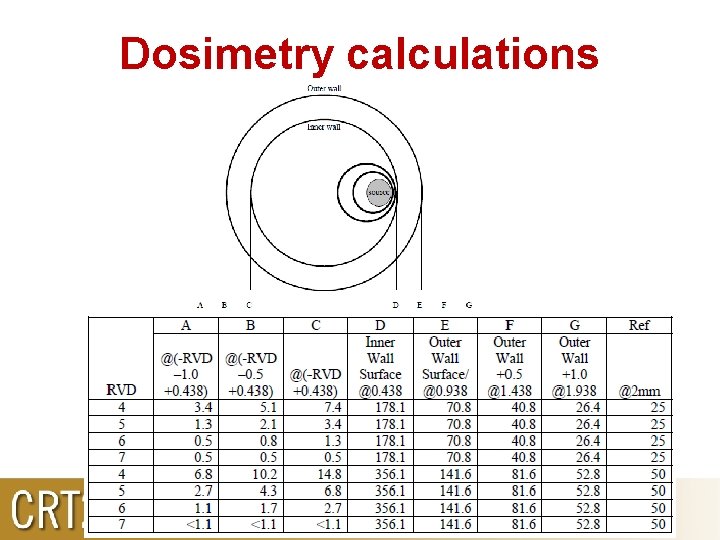
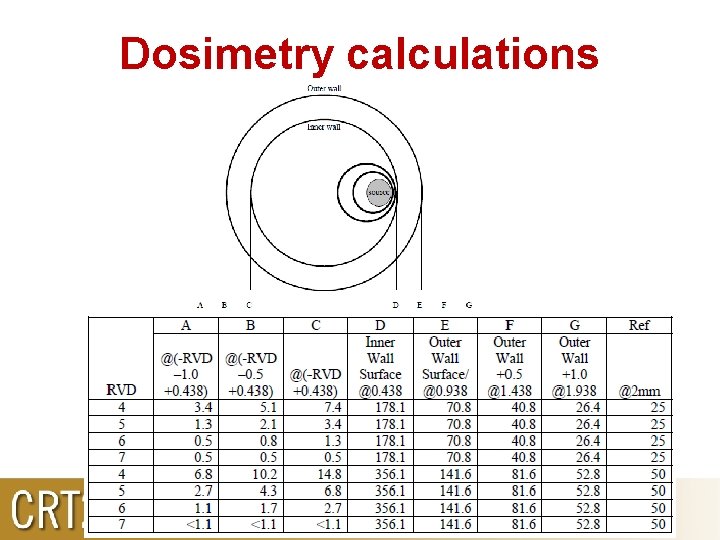
Dosimetry calculations
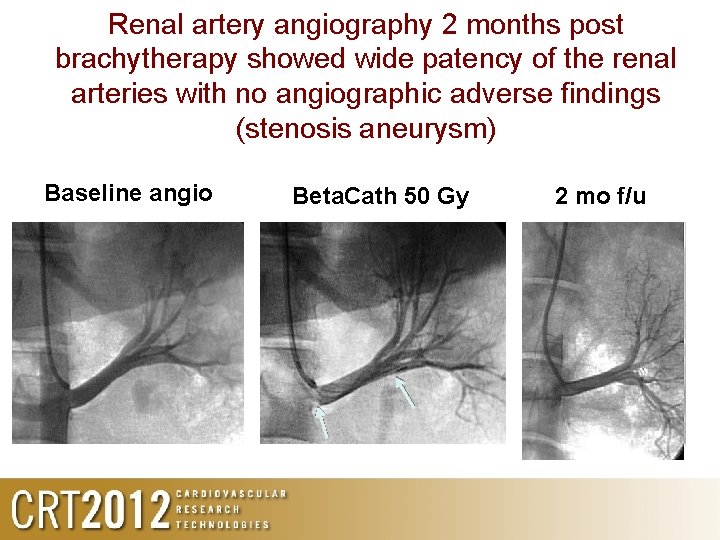
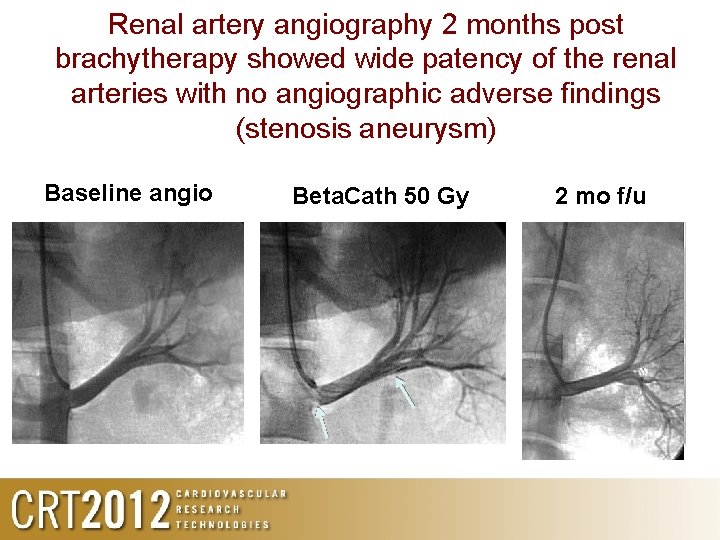
Renal artery angiography 2 months post brachytherapy showed wide patency of the renal arteries with no angiographic adverse findings (stenosis aneurysm) Baseline angio Beta. Cath 50 Gy 2 mo f/u
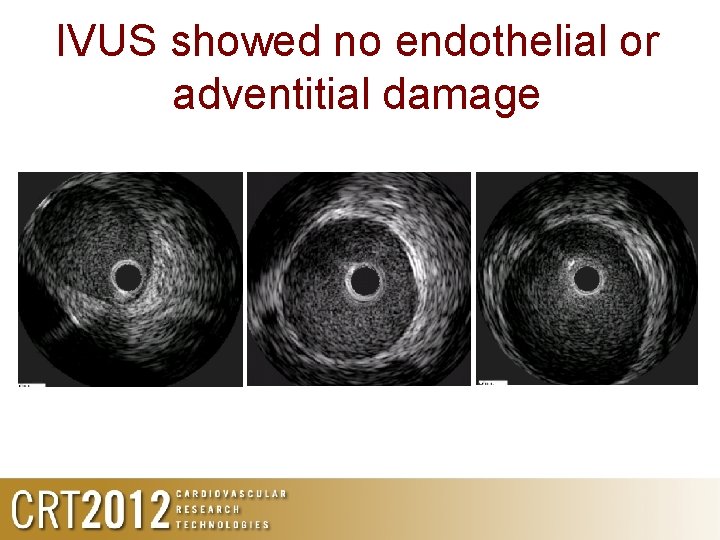
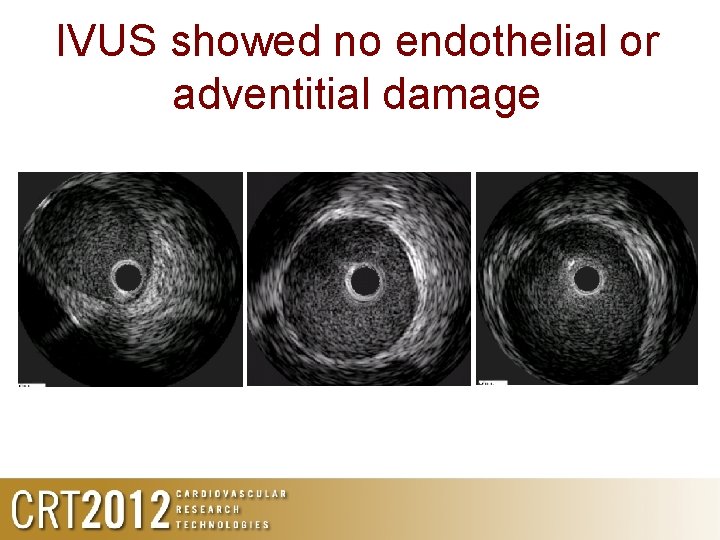
IVUS showed no endothelial or adventitial damage
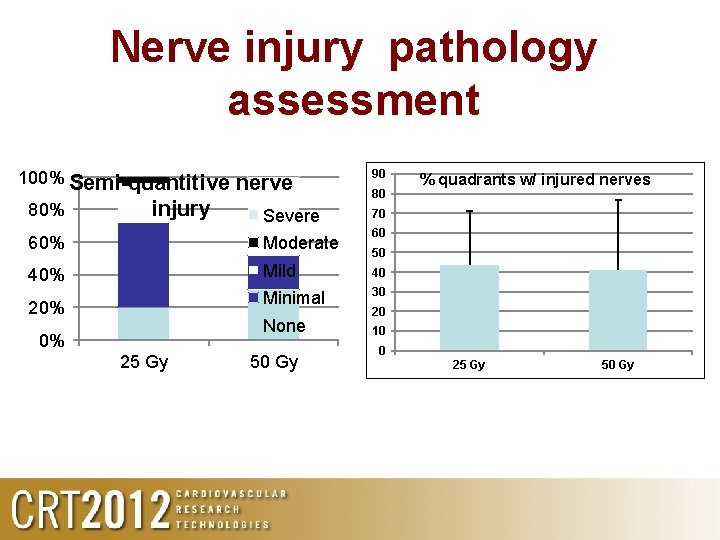
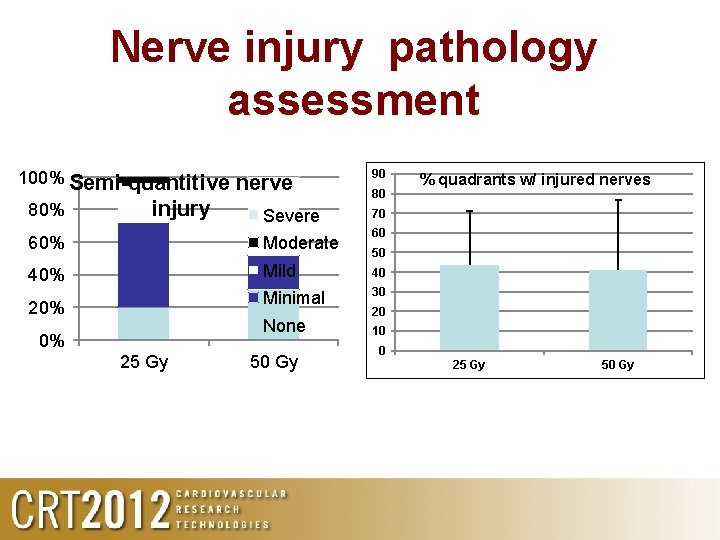
Nerve injury pathology assessment 100% Semi-quantitive 80% injury nerve Severe 90 80 70 60 60% Moderate 40% Mild 40 Minimal 30 20% None 0% 25 Gy 50 Gy % quadrants w/ injured nerves 50 20 10 0 25 Gy 50 Gy
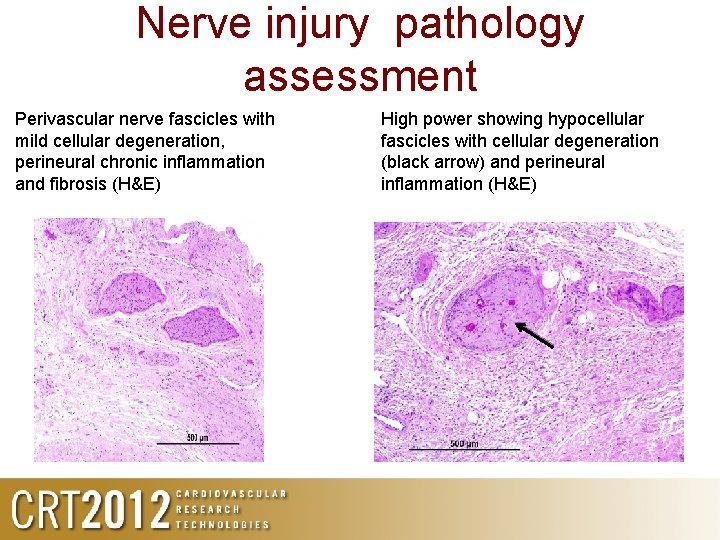
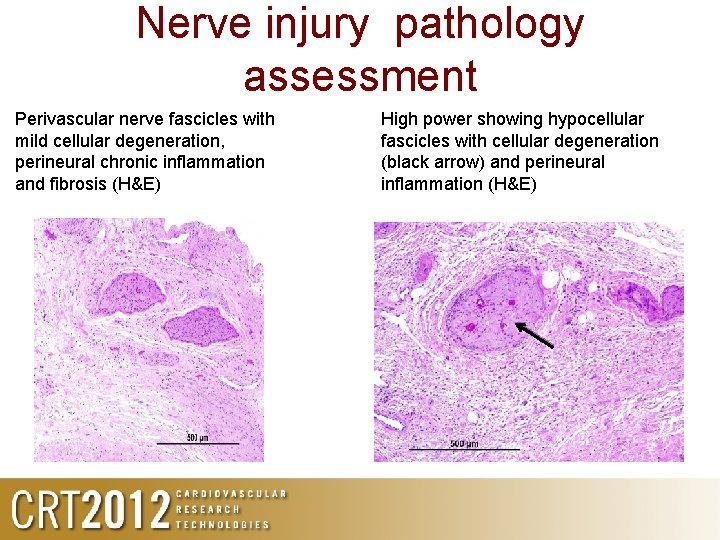
Nerve injury pathology assessment Perivascular nerve fascicles with mild cellular degeneration, perineural chronic inflammation and fibrosis (H&E) High power showing hypocellular fascicles with cellular degeneration (black arrow) and perineural inflammation (H&E)
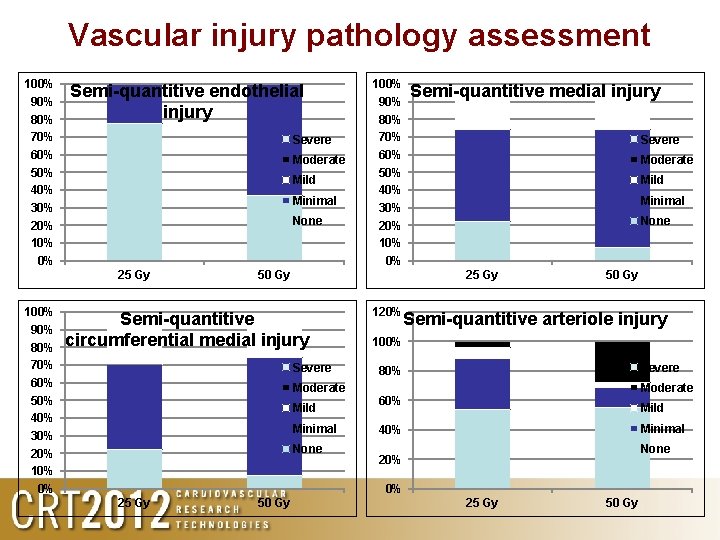
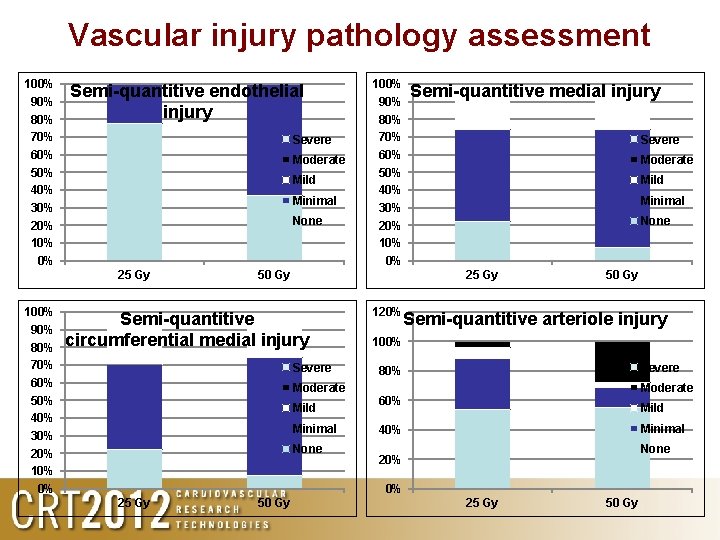
Vascular injury pathology assessment 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Semi-quantitive endothelial injury Severe Moderate Mild Minimal None 25 Gy 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 50 Gy Semi-quantitive medial injury Severe Moderate Mild Minimal None 25 Gy Semi-quantitive circumferential medial injury Severe Moderate Mild Minimal None 120% 50 Gy Semi-quantitive arteriole injury 100% Severe 80% Moderate 60% Mild Minimal 40% None 20% 0% 25 Gy 50 Gy
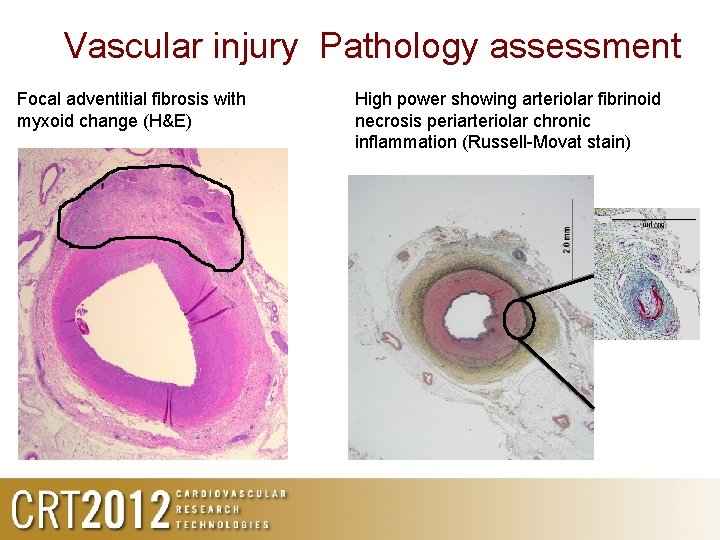
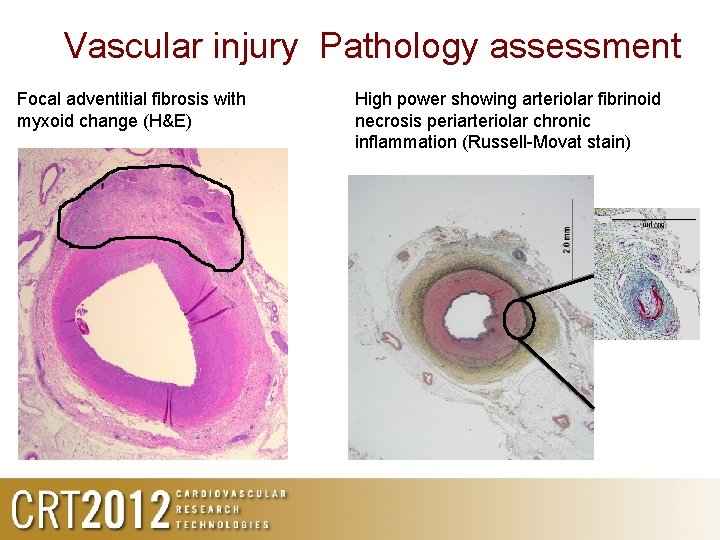
Vascular injury Pathology assessment Focal adventitial fibrosis with myxoid change (H&E) High power showing arteriolar fibrinoid necrosis periarteriolar chronic inflammation (Russell-Movat stain)
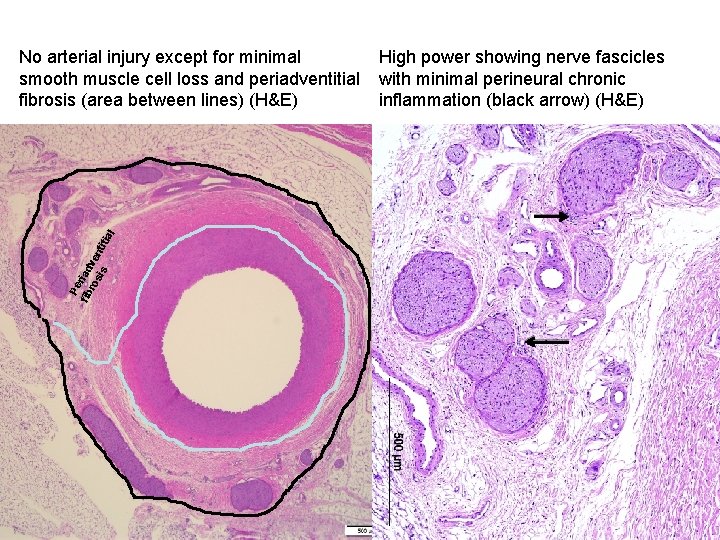
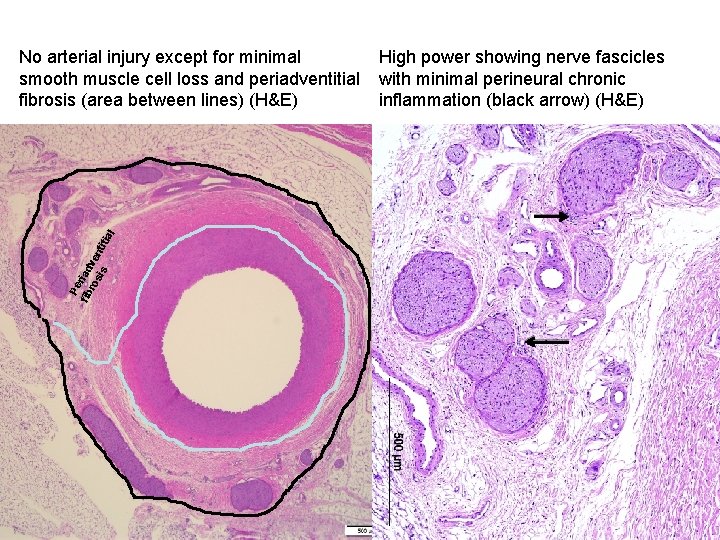
Pe fib riad ro ve sis nt itia l No arterial injury except for minimal smooth muscle cell loss and periadventitial fibrosis (area between lines) (H&E) High power showing nerve fascicles with minimal perineural chronic inflammation (black arrow) (H&E)
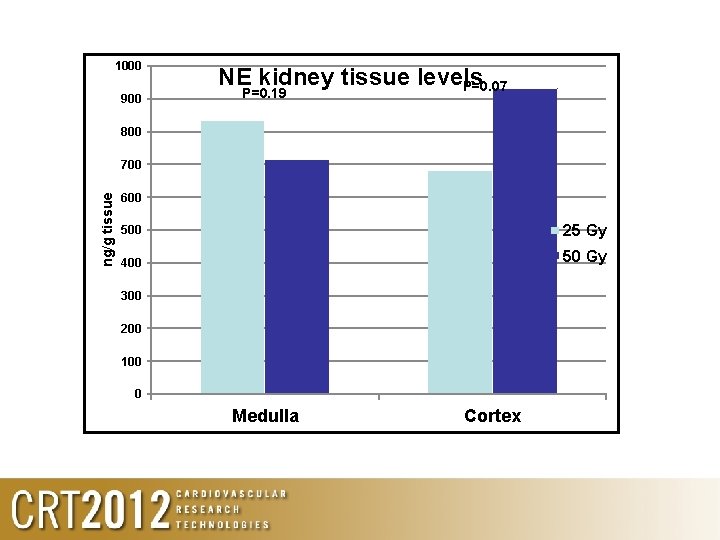
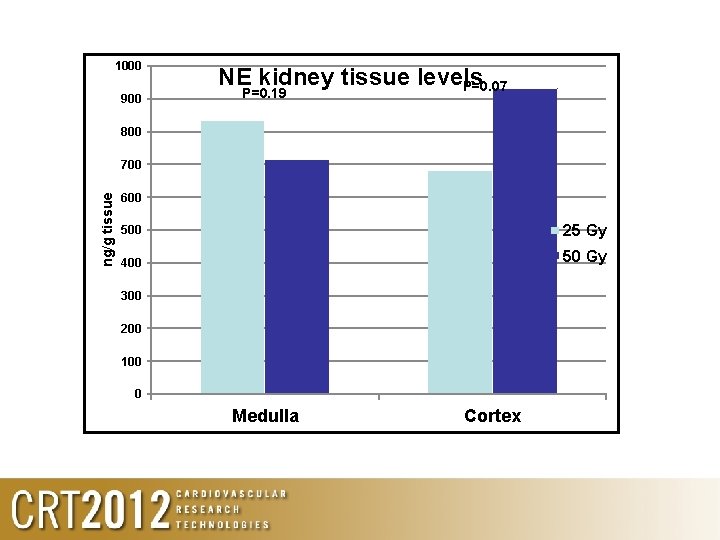
1000 900 NE kidney tissue levels P=0. 07 P=0. 19 800 ng/g tissue 700 600 500 25 Gy 400 50 Gy 300 200 100 0 Medulla Cortex
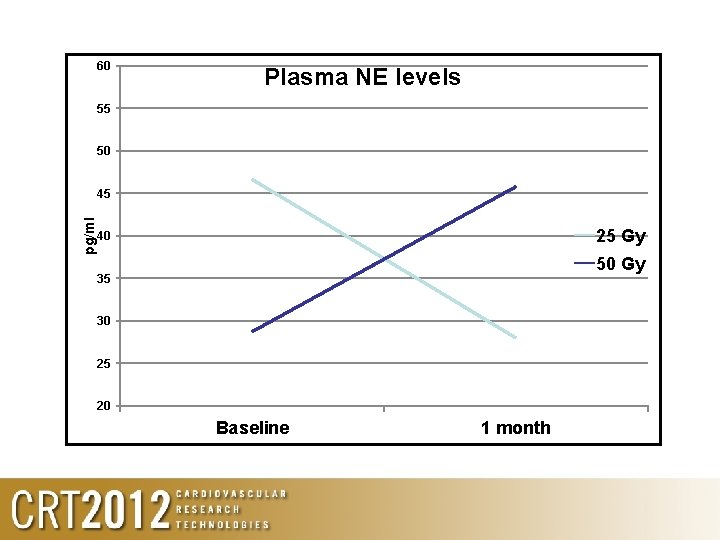
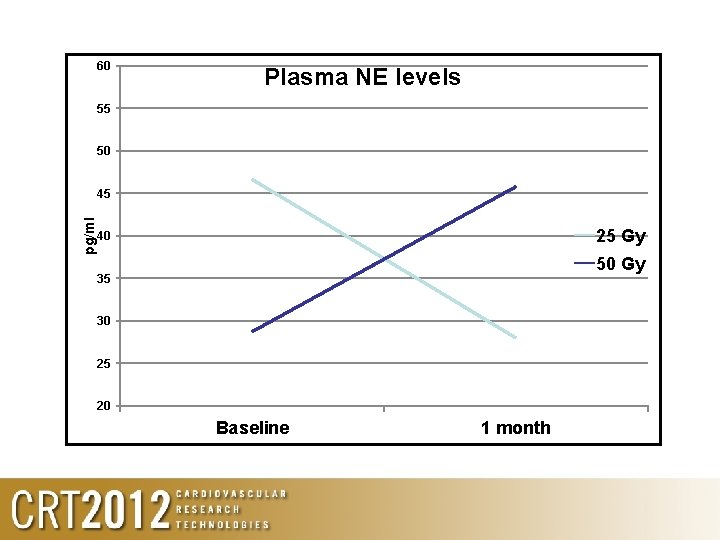
60 Plasma NE levels 55 50 pg/ml 45 25 Gy 40 50 Gy 35 30 25 20 Baseline 1 month
Conclusions • Renal denervation using β-emitting radiation is feasible • β-emitting radiation cause renal nerve damage • In the tested dosages (25 -50 Gy) there is minimal vascular damage • Further clinical studies are required to assess efficacy