Rational use of antibiotics in cholangitis Towards efficient
Rational use of antibiotics in cholangitis “Towards efficient and safe management” AZZA BARAKA PROFESSOR OF CLINICAL PHARMACOLOGY FACULTY OF MEDICINE-ALEXANDRIA UNIVERSITY
OBJECTIVES What is meant by rational use of antibiotics? Antibiotics belonging to the same class are not meant to be equal. How to be vigilant towards antibiotics ADRs?
Rationalize Antibiotic Use Choice • Duration Indication Timing • Decrease ADRs
Cholangitis Coretip The main importance of this condition is that it is a very treatable condition if treated appropriately, But the mortality can be high if there is delay in correct treatment
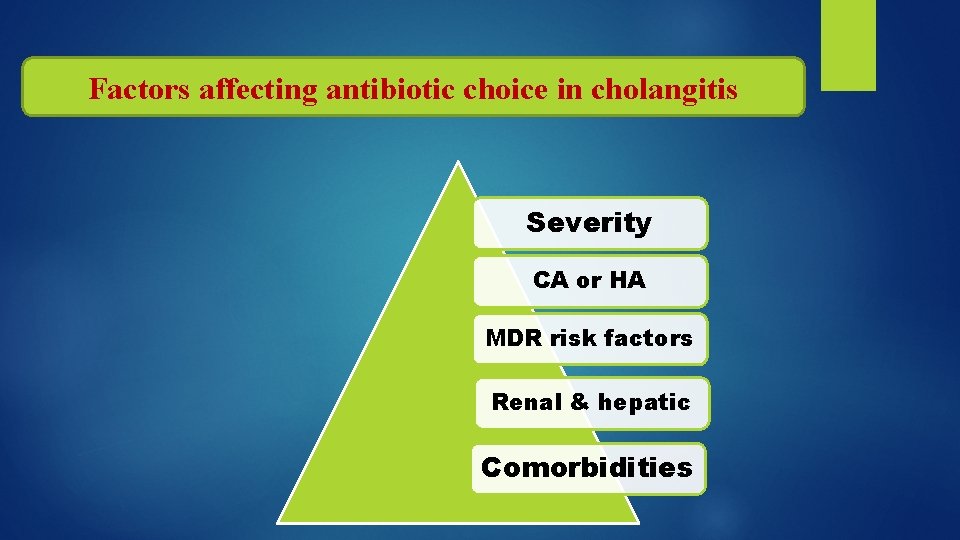
Factors affecting antibiotic choice in cholangitis Severity CA or HA MDR risk factors Renal & hepatic Comorbidities
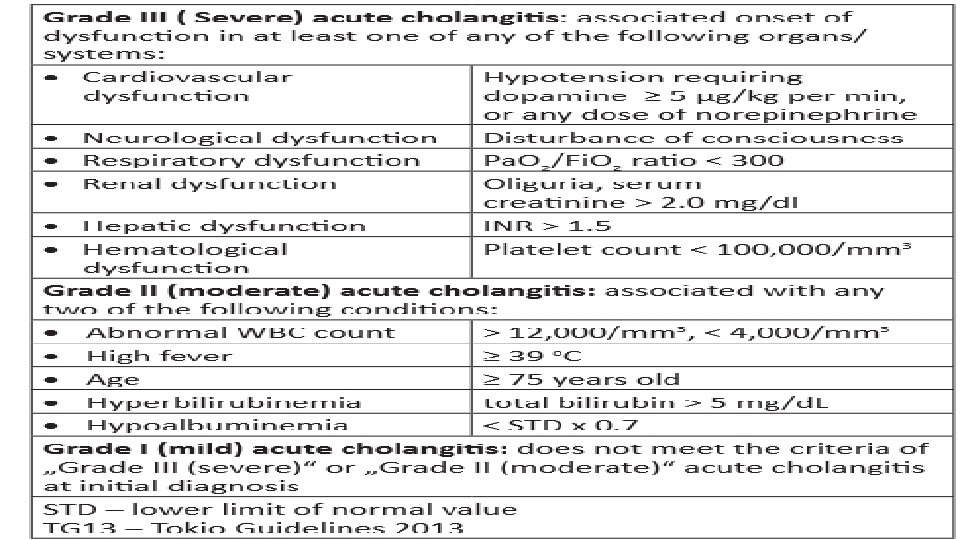
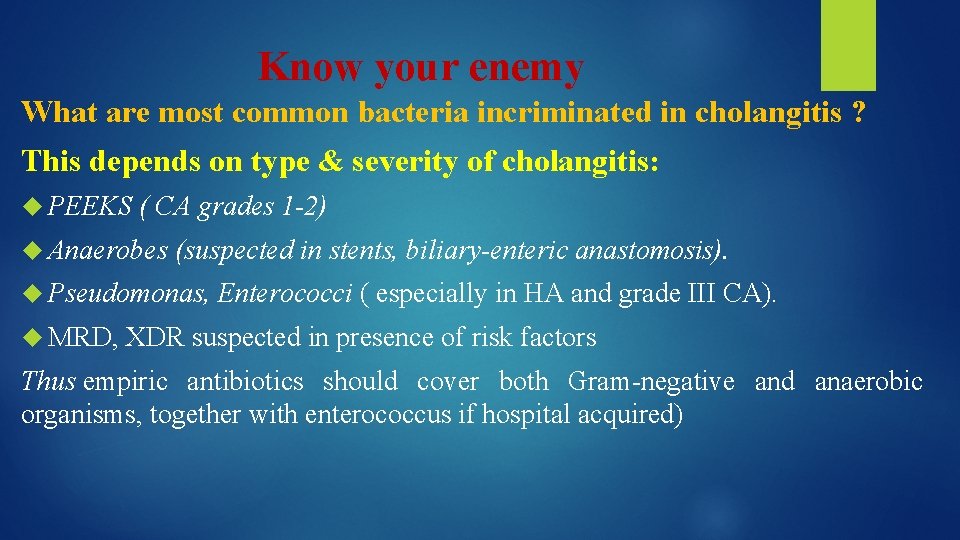
Know your enemy What are most common bacteria incriminated in cholangitis ? This depends on type & severity of cholangitis: PEEKS ( CA grades 1 -2) Anaerobes (suspected in stents, biliary-enteric anastomosis). Pseudomonas, Enterococci ( especially in HA and grade III CA). MRD, XDR suspected in presence of risk factors Thus empiric antibiotics should cover both Gram-negative and anaerobic organisms, together with enterococcus if hospital acquired)
Antibiotic factors SPECTRUM
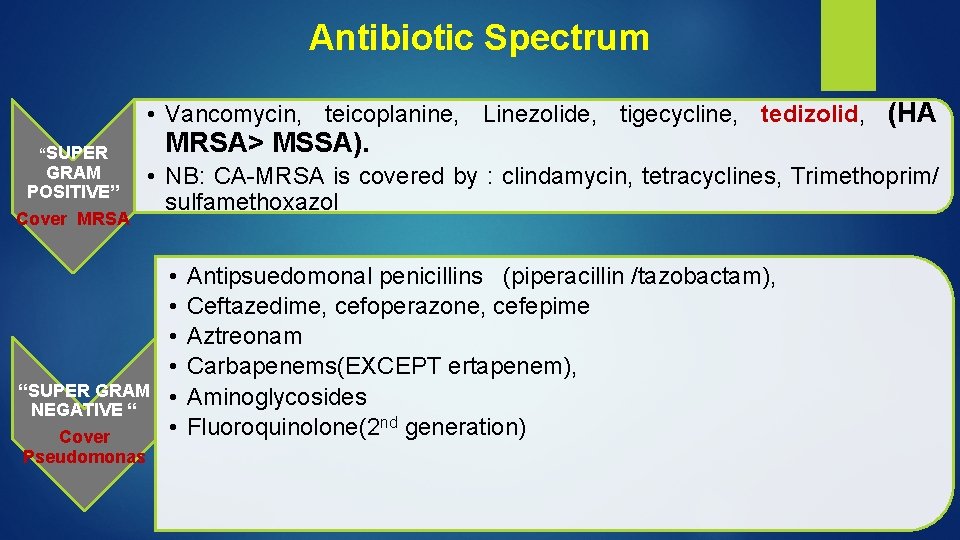
Antibiotic Spectrum • Vancomycin, teicoplanine, Linezolide, tigecycline, tedizolid, (HA “SUPER GRAM POSITIVE” Cover MRSA> MSSA). • NB: CA-MRSA is covered by : clindamycin, tetracyclines, Trimethoprim/ sulfamethoxazol “SUPER GRAM NEGATIVE “ Cover Pseudomonas • • • Antipsuedomonal penicillins (piperacillin /tazobactam), Ceftazedime, cefoperazone, cefepime Aztreonam Carbapenems(EXCEPT ertapenem), Aminoglycosides Fluoroquinolone(2 nd generation)
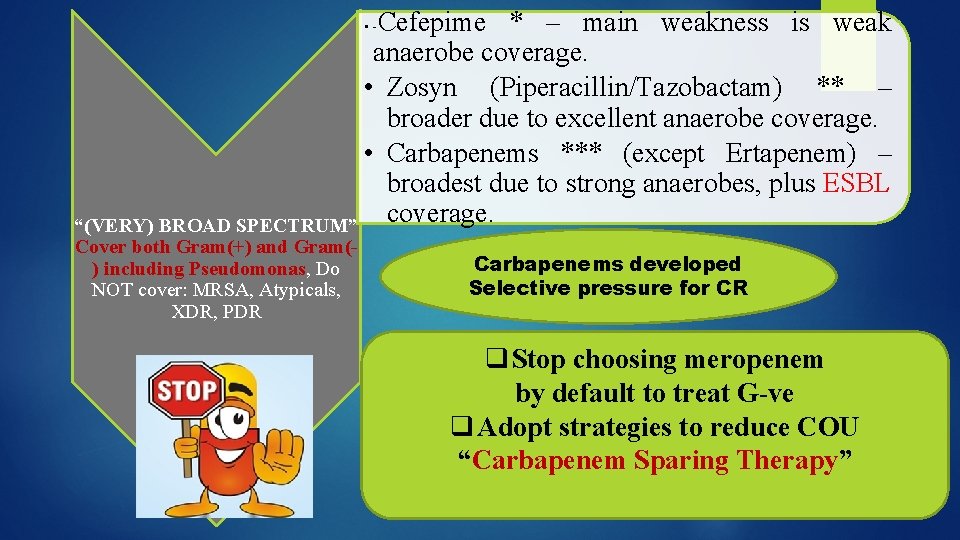
Cefepime * – main weakness is weak anaerobe coverage. • Zosyn (Piperacillin/Tazobactam) ** – broader due to excellent anaerobe coverage. • Carbapenems *** (except Ertapenem) – broadest due to strong anaerobes, plus ESBL “(VERY) BROAD SPECTRUM” coverage. • - Cover both Gram(+) and Gram() including Pseudomonas, Do NOT cover: MRSA, Atypicals, XDR, PDR Carbapenems developed Selective pressure for CR q Stop choosing meropenem by default to treat G-ve q Adopt strategies to reduce COU “Carbapenem Sparing Therapy”
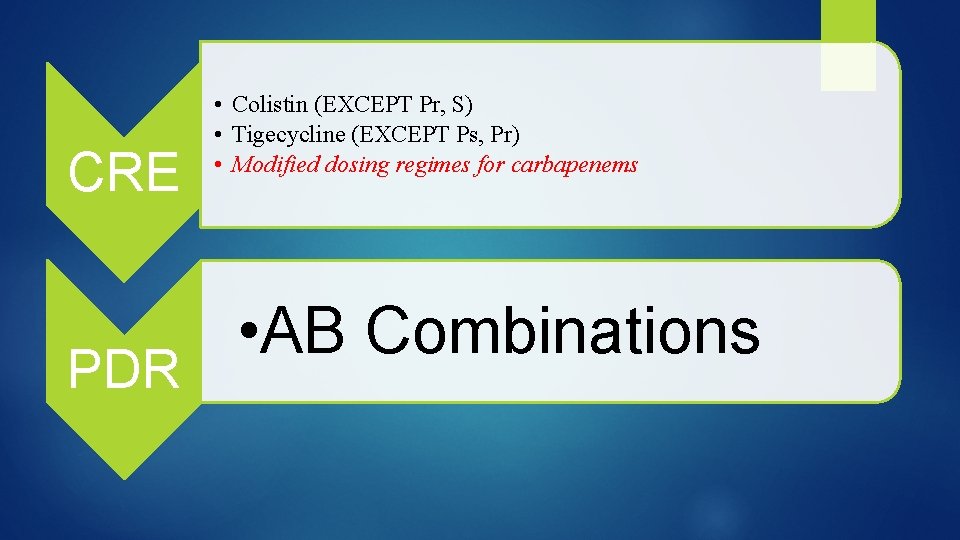
CRE PDR • Colistin (EXCEPT Pr, S) • Tigecycline (EXCEPT Ps, Pr) • Modified dosing regimes for carbapenems • AB Combinations
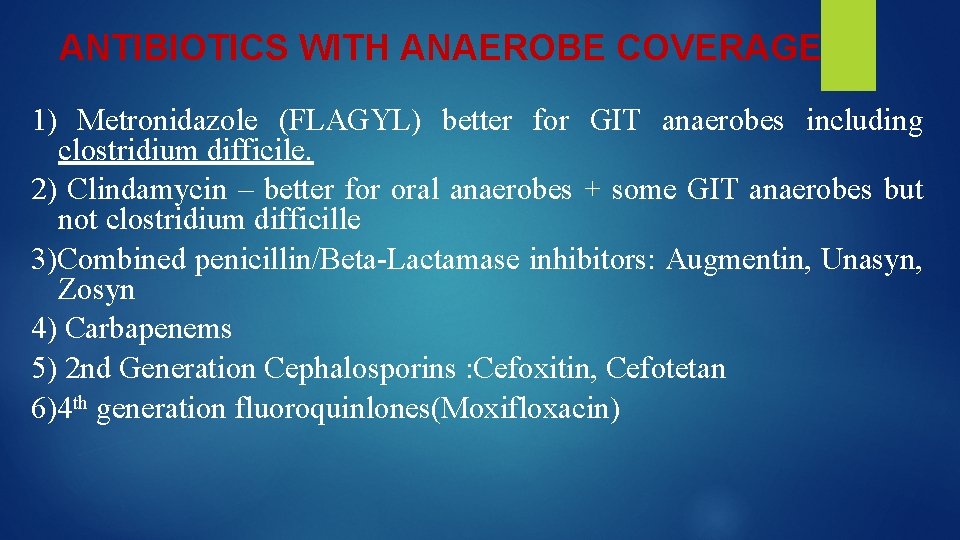
ANTIBIOTICS WITH ANAEROBE COVERAGE 1) Metronidazole (FLAGYL) better for GIT anaerobes including clostridium difficile. 2) Clindamycin – better for oral anaerobes + some GIT anaerobes but not clostridium difficille 3)Combined penicillin/Beta-Lactamase inhibitors: Augmentin, Unasyn, Zosyn 4) Carbapenems 5) 2 nd Generation Cephalosporins : Cefoxitin, Cefotetan 6)4 th generation fluoroquinlones(Moxifloxacin)
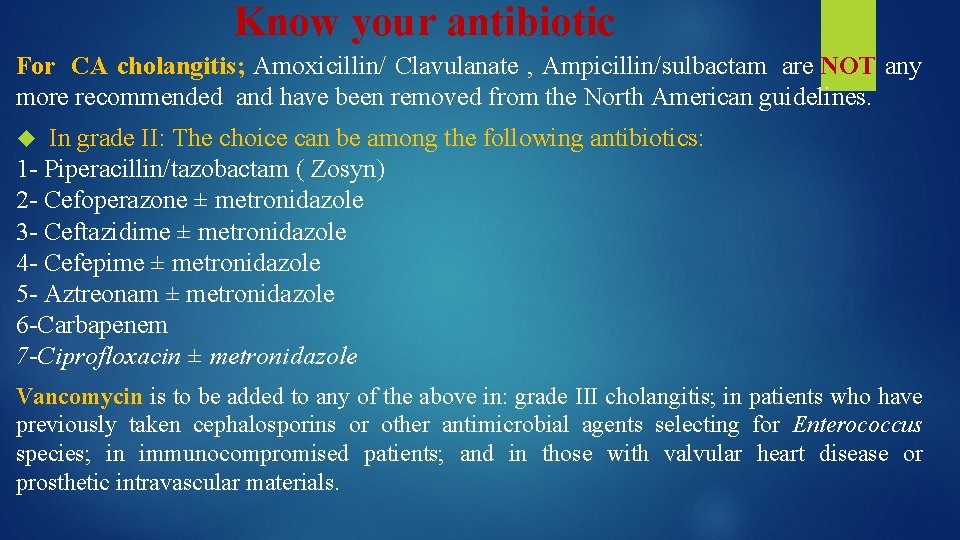
Know your antibiotic For CA cholangitis; Amoxicillin/ Clavulanate , Ampicillin/sulbactam are NOT any more recommended and have been removed from the North American guidelines. In grade II: The choice can be among the following antibiotics: 1 - Piperacillin/tazobactam ( Zosyn) 2 - Cefoperazone ± metronidazole 3 - Ceftazidime ± metronidazole 4 - Cefepime ± metronidazole 5 - Aztreonam ± metronidazole 6 -Carbapenem 7 -Ciprofloxacin ± metronidazole Vancomycin is to be added to any of the above in: grade III cholangitis; in patients who have previously taken cephalosporins or other antimicrobial agents selecting for Enterococcus species; in immunocompromised patients; and in those with valvular heart disease or prosthetic intravascular materials.
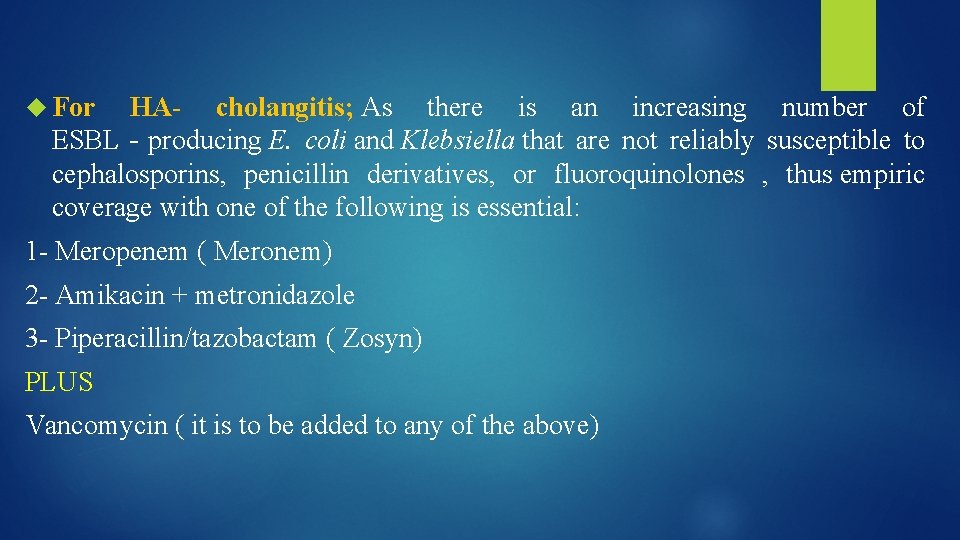
For HA- cholangitis; As there is an increasing number of ESBL‐producing E. coli and Klebsiella that are not reliably susceptible to cephalosporins, penicillin derivatives, or fluoroquinolones , thus empiric coverage with one of the following is essential: 1 - Meropenem ( Meronem) 2 - Amikacin + metronidazole 3 - Piperacillin/tazobactam ( Zosyn) PLUS Vancomycin ( it is to be added to any of the above)
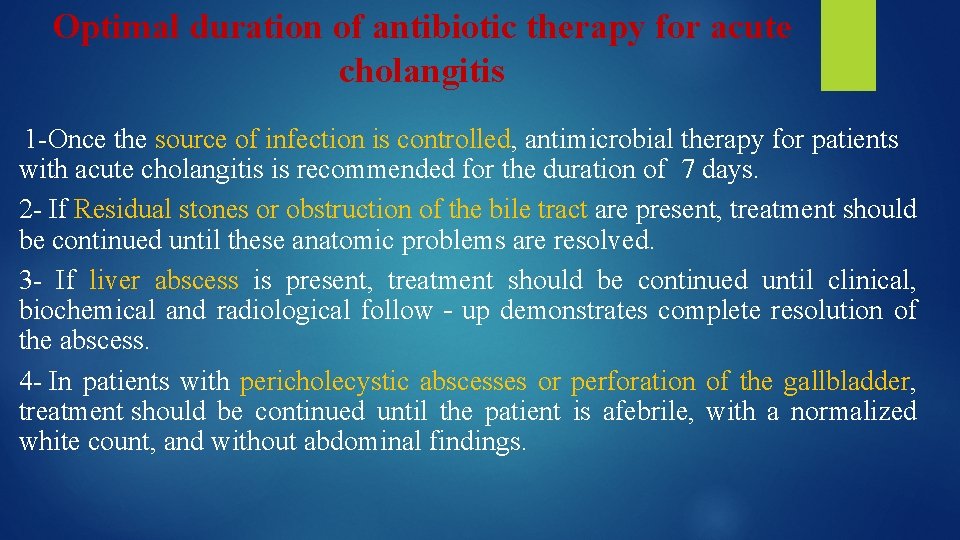
Optimal duration of antibiotic therapy for acute cholangitis 1 -Once the source of infection is controlled, antimicrobial therapy for patients with acute cholangitis is recommended for the duration of 7 days. 2 - If Residual stones or obstruction of the bile tract are present, treatment should be continued until these anatomic problems are resolved. 3 - If liver abscess is present, treatment should be continued until clinical, biochemical and radiological follow‐up demonstrates complete resolution of the abscess. 4 - In patients with pericholecystic abscesses or perforation of the gallbladder, treatment should be continued until the patient is afebrile, with a normalized white count, and without abdominal findings.
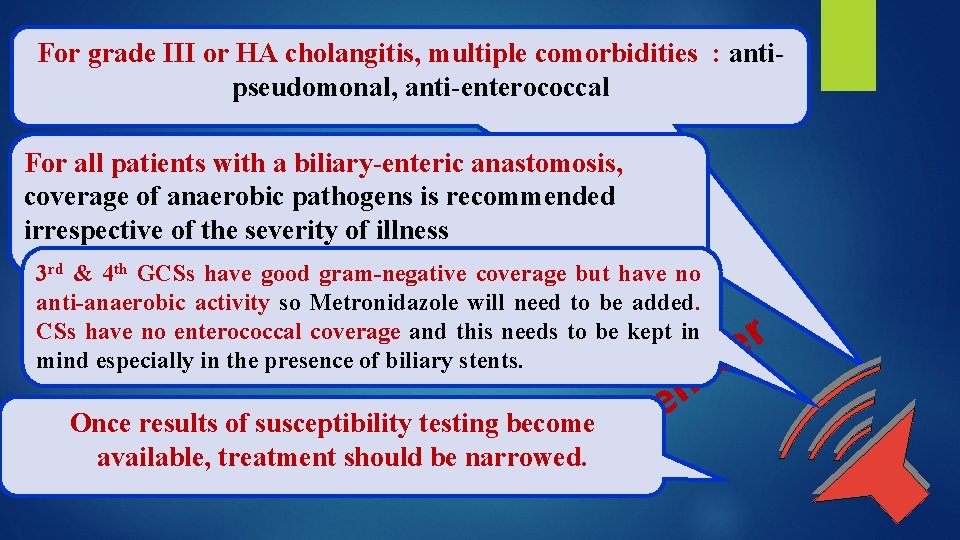
For grade III or HA cholangitis, multiple comorbidities : antipseudomonal, anti-enterococcal For all patients with a biliary-enteric anastomosis, coverage of anaerobic pathogens is recommended irrespective of the severity of illness 3 rd & 4 th GCSs have good gram-negative coverage but have no anti-anaerobic activity so Metronidazole will need to be added. CSs have no enterococcal coverage and this needs to be kept in mind especially in the presence of biliary stents. Once results of susceptibility testing become m available, treatment should be narrowed. Re em b r e
Liver transplant patients who develop cholangitis have high probability of Candida and/or Enterococcus
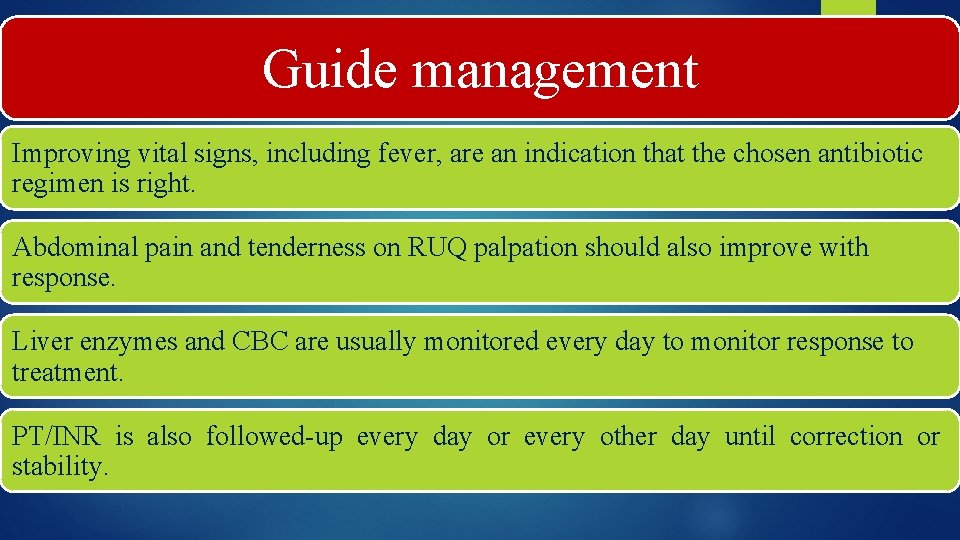
Guide management Improving vital signs, including fever, are an indication that the chosen antibiotic regimen is right. Abdominal pain and tenderness on RUQ palpation should also improve with response. Liver enzymes and CBC are usually monitored every day to monitor response to treatment. PT/INR is also followed-up every day or every other day until correction or stability.
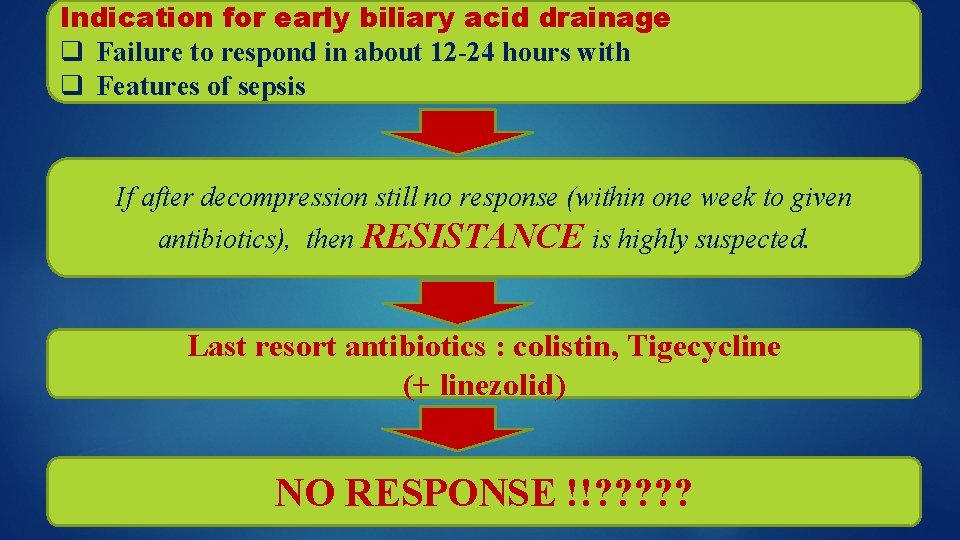
Indication for early biliary acid drainage q Failure to respond in about 12 -24 hours with q Features of sepsis If after decompression still no response (within one week to given antibiotics), then RESISTANCE is highly suspected. Last resort antibiotics : colistin, Tigecycline (+ linezolid) NO RESPONSE !!? ? ?

Can we win our battle against MDR, XDR & even PDR? ? “Yes, but by no longer relying on discovery of new antibiotics” Slowing the evolution of antibiotic resistance can be MORE EFFECTIVE than developing new drugs 1. 2. 3. 4. 5. Rationalize use of antibiotics Look into the past and revive old antibiotics Appreciate individual differences between members of same AB group Optimize Antibiotic Dosing Strategies by proper utilization of PK/PDs Optimize use of drug combinations
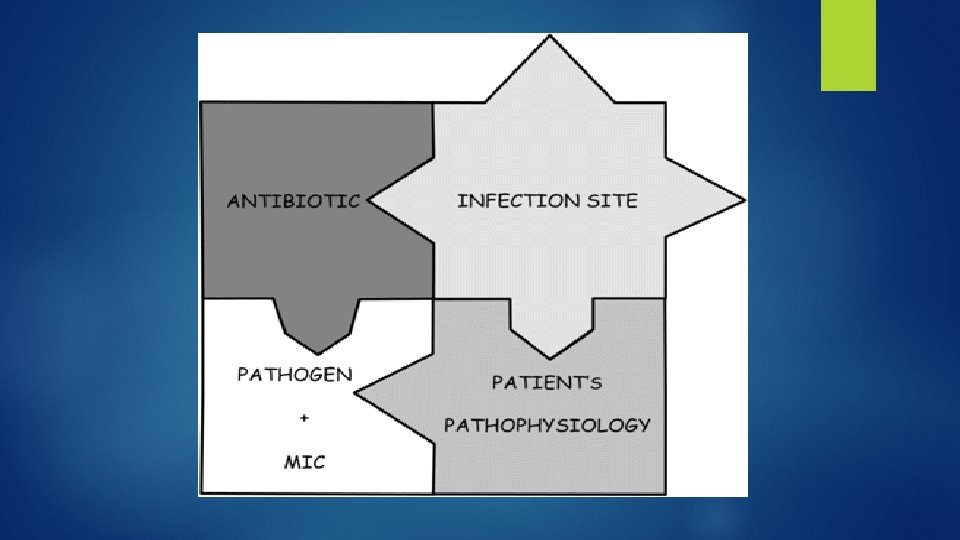
Antibiotic factors Tissue Penetration “Be sure that the antibiotic reaches the site of infection”
If cholangitis with bacteremia Choose Antibiotics that achieve good concentration in blood
Antibiotic factors Activity at the target site
II-Revival of old antibiotics -Carbapenems sparing ABs: cephalosporins, PTZ, AGs
III-Appreciate individual differences between members of the same group!!! Differences • Pharmacokinetic • Microbiological • Target tissue • Safety & DI • Resistance selection pressure (mutagenic potential)
Even BLIs differ!! If a βL-βLI is administered, does the type of β-LI matter (eg, tazobactam, sulbactam, clavulanic acid?
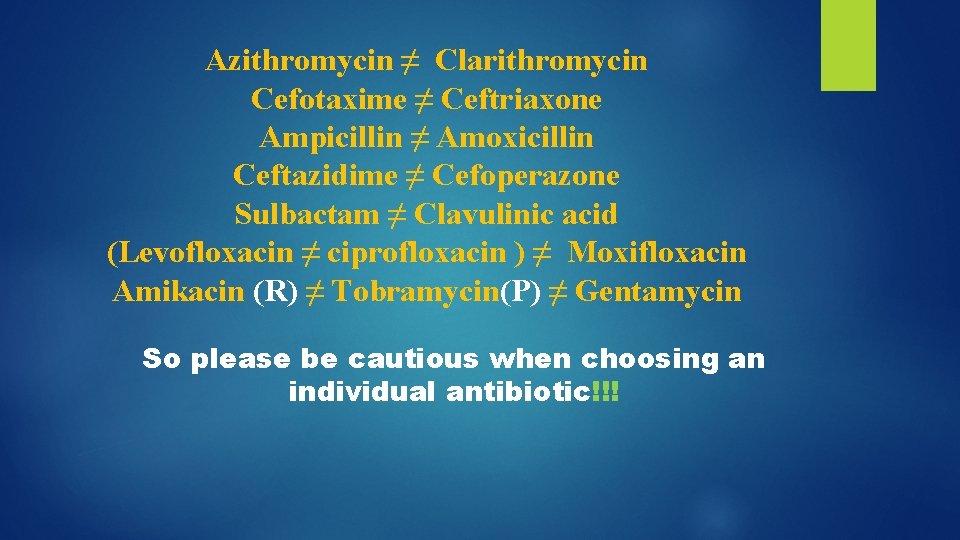
Azithromycin ≠ Clarithromycin Cefotaxime ≠ Ceftriaxone Ampicillin ≠ Amoxicillin Ceftazidime ≠ Cefoperazone Sulbactam ≠ Clavulinic acid (Levofloxacin ≠ ciprofloxacin ) ≠ Moxifloxacin Amikacin (R) ≠ Tobramycin(P) ≠ Gentamycin So please be cautious when choosing an individual antibiotic!!!
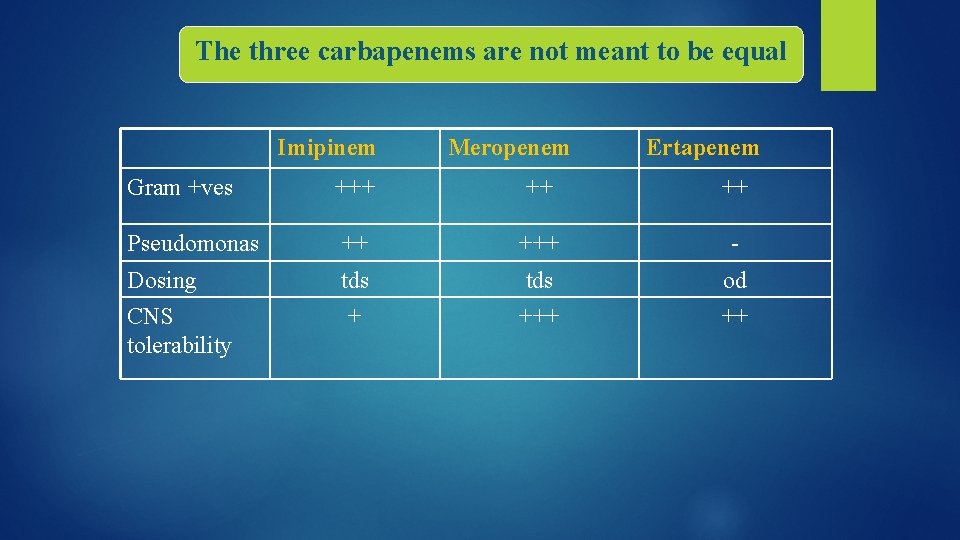
The three carbapenems are not meant to be equal Imipinem Meropenem Ertapenem Gram +ves +++ ++ ++ Pseudomonas ++ +++ - Dosing CNS tolerability tds +++ od ++
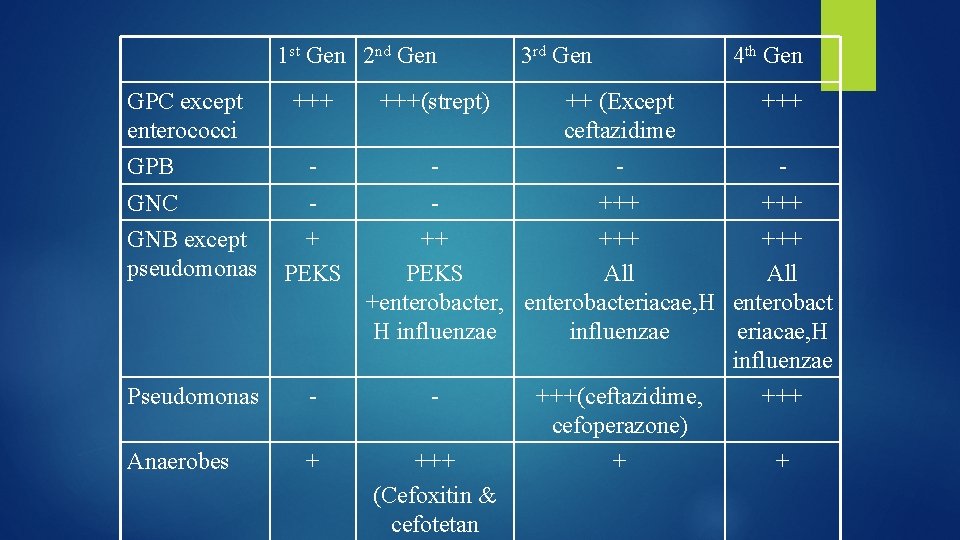
1 st Gen 2 nd Gen GPC except enterococci GPB 3 rd Gen 4 th Gen +++(strept) ++ (Except ceftazidime +++ - - GNC GNB except pseudomonas + PEKS +++ ++ +++ PEKS All +enterobacter, enterobacteriacae, H enterobact H influenzae eriacae, H influenzae Pseudomonas - - Anaerobes + +++ (Cefoxitin & cefotetan +++(ceftazidime, cefoperazone) + +++ +
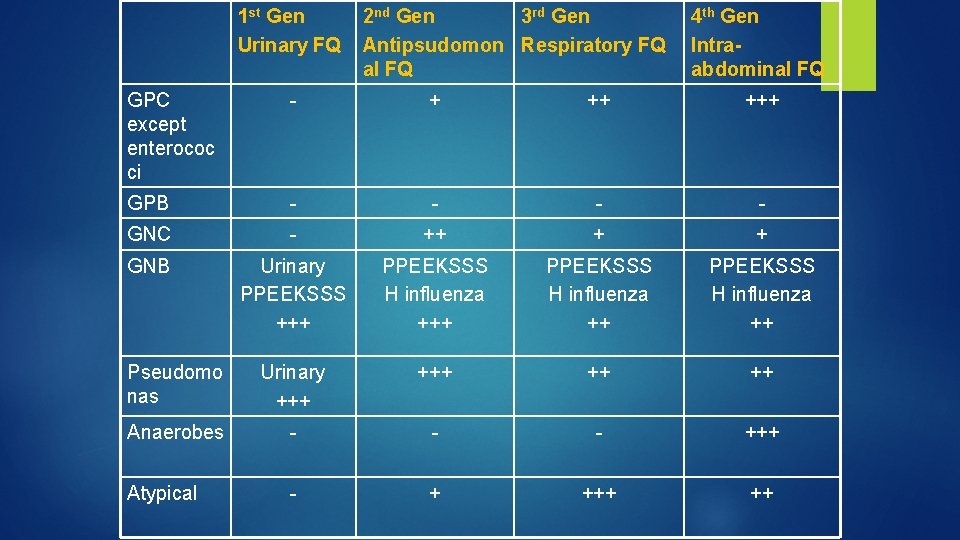
1 st Gen Urinary FQ 2 nd Gen 3 rd Gen Antipsudomon Respiratory FQ al FQ 4 th Gen Intraabdominal FQ GPC except enterococ ci - + ++ +++ GPB - - GNC - ++ + + GNB Urinary PPEEKSSS +++ PPEEKSSS H influenza ++ Pseudomo nas Urinary +++ ++ ++ Anaerobes - - - +++ Atypical - + ++
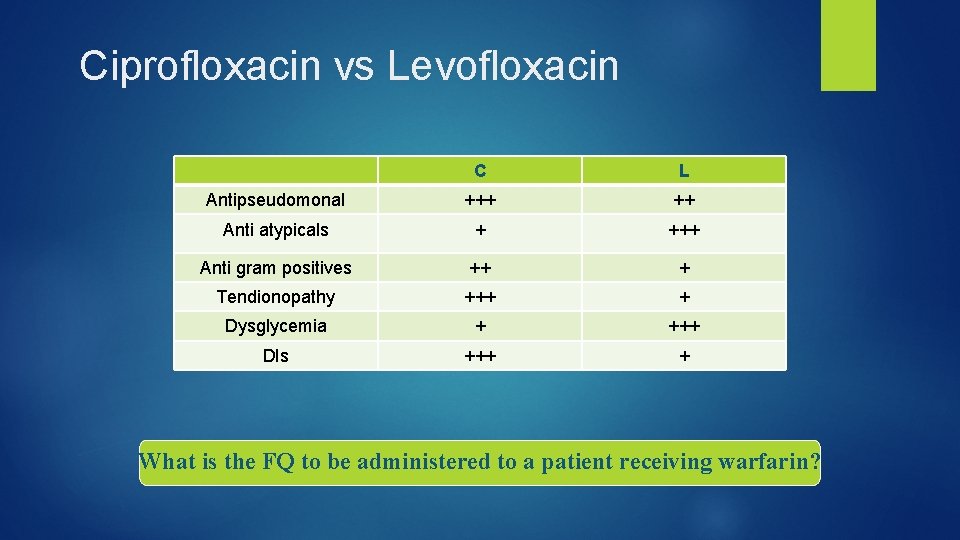
Ciprofloxacin vs Levofloxacin C L Antipseudomonal +++ ++ Anti atypicals + +++ Anti gram positives ++ + Tendionopathy +++ + Dysglycemia + +++ DIs +++ + What is the FQ to be administered to a patient receiving warfarin?
IV- Optimize dosing regimens “Optimal antibiotic therapy” should be used and is meant to indicate that not only is the correct antibiotic selected, but also that the dosage is sufficient to obtain the maximal exposure threshold determined from pharmacodynamic studies. An interesting observation relevant to optimal antibiotic therapy is that the pathogen need not be “Susceptible” to the drug in question, as long as the exposure of the agent is sufficient to kill that organism (Aggressive dosing regimen). . Avoid failure to meet necessary pharmacodynamic targets due to inadequate dosing and/or interval schedule
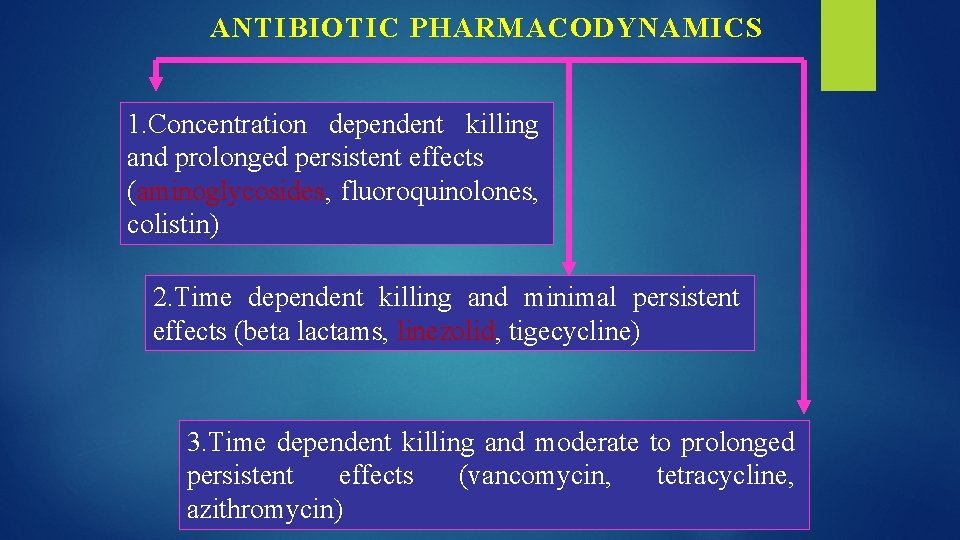
ANTIBIOTIC PHARMACODYNAMICS 1. Concentration dependent killing and prolonged persistent effects (aminoglycosides, fluoroquinolones, colistin) 2. Time dependent killing and minimal persistent effects (beta lactams, linezolid, tigecycline) 3. Time dependent killing and moderate to prolonged persistent effects (vancomycin, tetracycline, azithromycin)
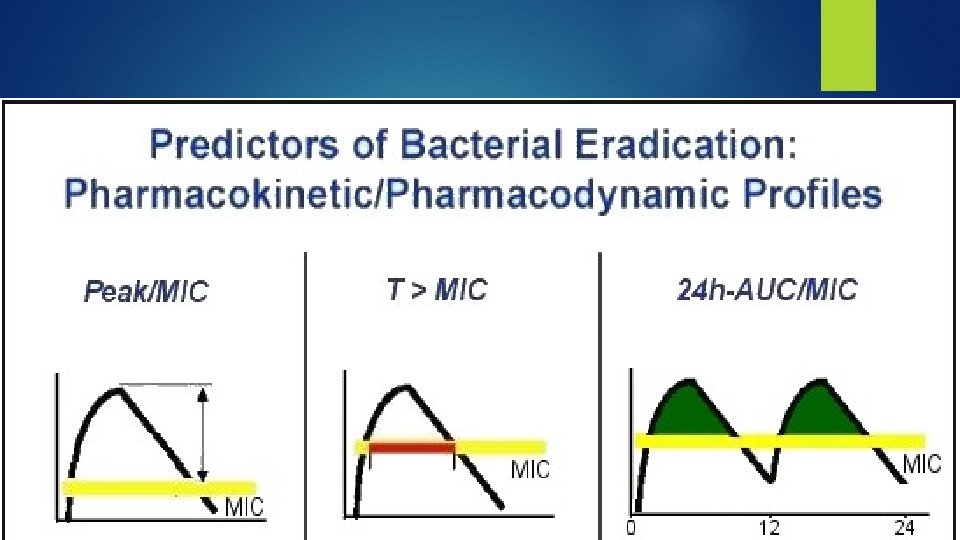
Dosing Regimens According To PK/PD The ideal dosing regimen for category “ 1” would maximize concentration, because the higher the concentration, the more extensive and faster the degree of killing. ( eg ODD aminoglycoside) The ideal dosing regimen for category “ 2”, would maximize time of exposure because t >MIC is the parameter that best correlates with efficacy. (eg extend infusion time for meropenem) The ideal dosing regimen for category “ 3” is to maximize the amount received.
DOSING OPTIMIZATION “One of the inviting factors to AMR is under-dosing” It is time to move away from the “one dose fits all” strategy that has been traditionally applied in clinical medicine towards a "more personalized antibiotic dosing"
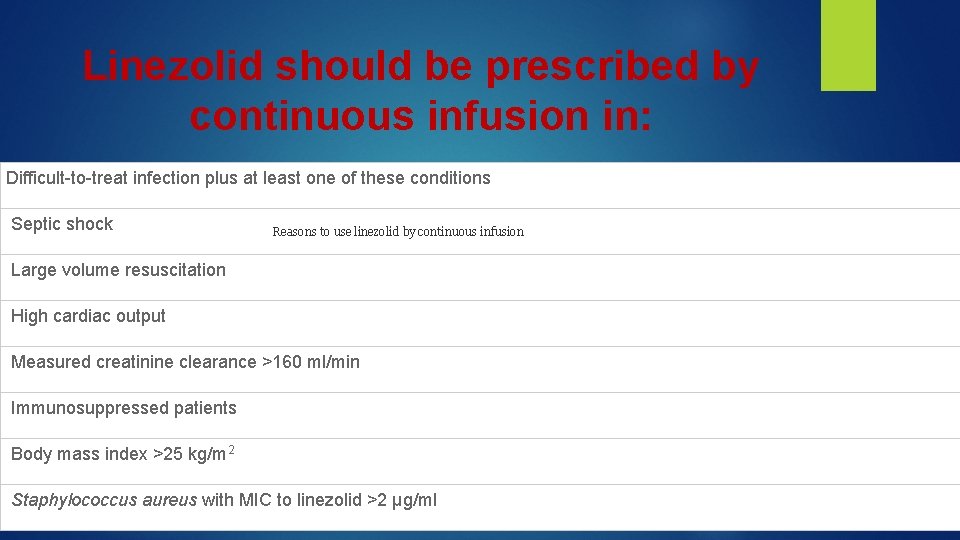
Linezolid should be prescribed by continuous infusion in: Difficult-to-treat infection plus at least one of these conditions Septic shock Reasons to use linezolid by continuous infusion Large volume resuscitation High cardiac output Measured creatinine clearance >160 ml/min Immunosuppressed patients Body mass index >25 kg/m 2 Staphylococcus aureus with MIC to linezolid >2 µg/ml
Even timing of antibiotic administration has an impact “Chronotherapy” Administer SDD of AG according to circadian variation in GFR. !!
Be cautious from Under dosing 1 - Obesity causes a number of changes in PKs, including increase in Vd In general, lipophilic antibiotics usually require TBW dosing . In contrast, hydrophilic antibiotics usually require IBW or ABW dosing. BUT NEVER give a child a dose exceeding recommended adult dose
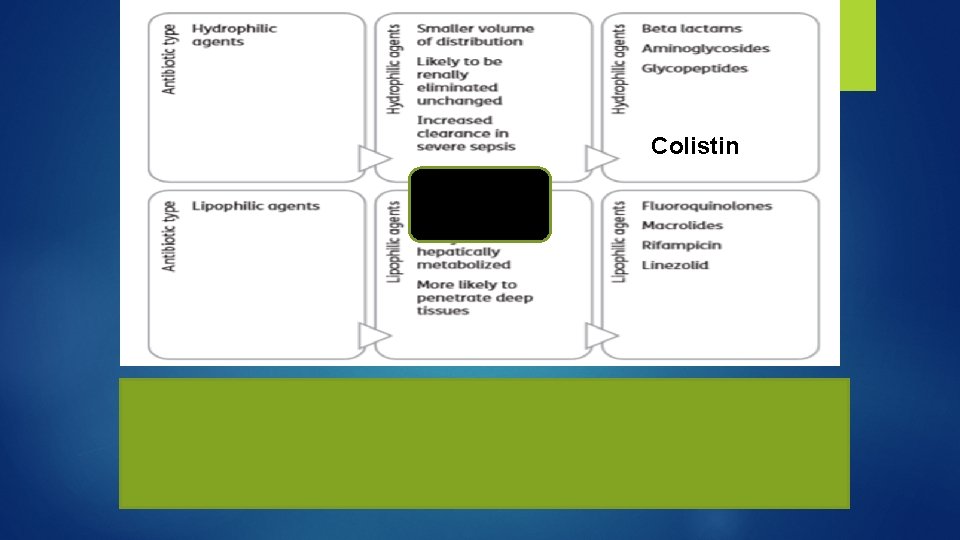
Colistin
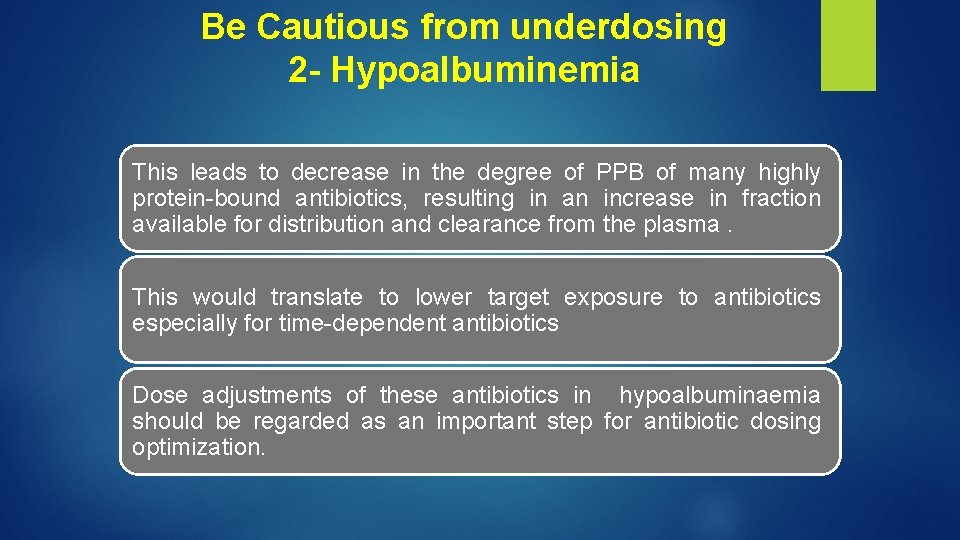
Be Cautious from underdosing 2 - Hypoalbuminemia This leads to decrease in the degree of PPB of many highly protein-bound antibiotics, resulting in an increase in fraction available for distribution and clearance from the plasma. This would translate to lower target exposure to antibiotics especially for time-dependent antibiotics Dose adjustments of these antibiotics in hypoalbuminaemia should be regarded as an important step for antibiotic dosing optimization.
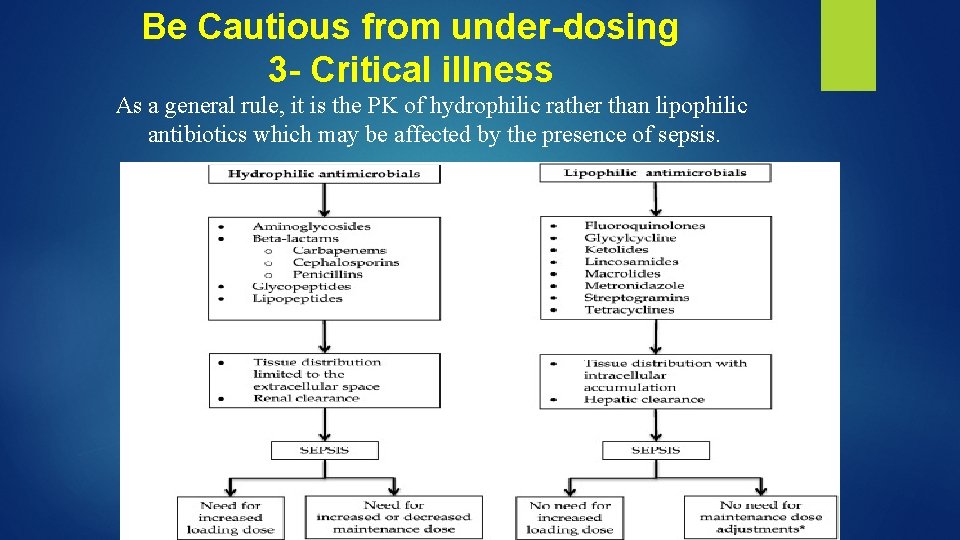
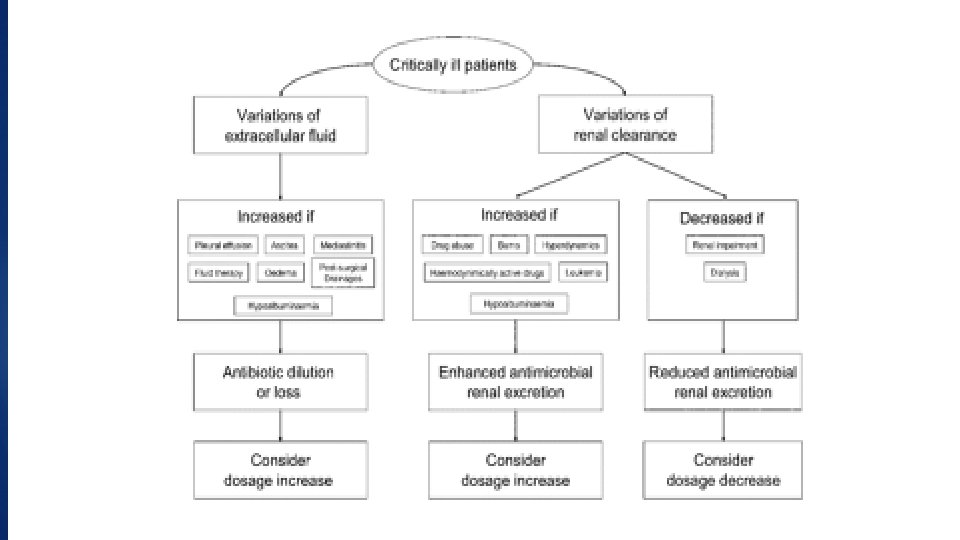
Be Cautious from under-dosing 3 - Critical illness As a general rule, it is the PK of hydrophilic rather than lipophilic antibiotics which may be affected by the presence of sepsis.
V- Antibiotic combinations “Our new coming players that can play a role against MDR” BUT
Antibiotic combination efficacy networks Antibiotic combinations are not always the magic stick Synergistic effects Collateral sensitivity
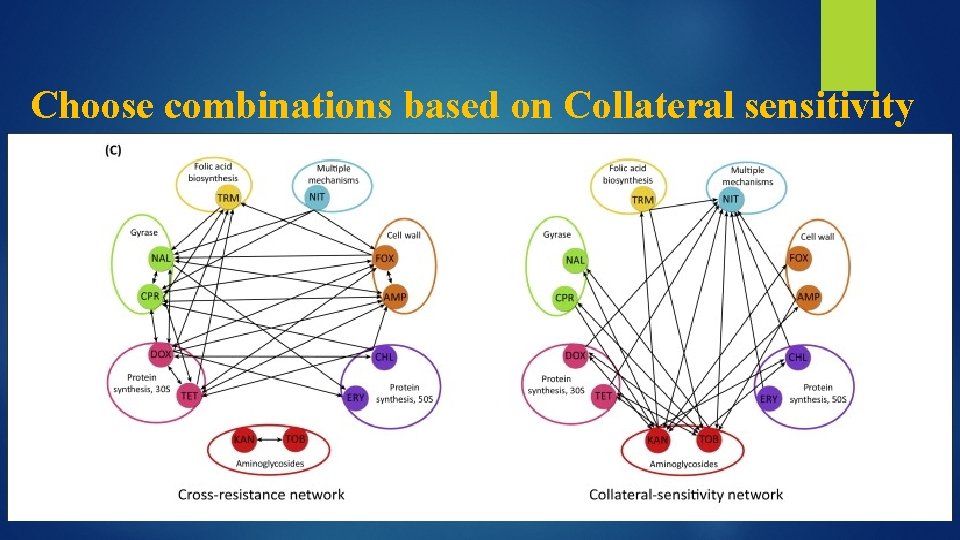
Choose combinations based on Collateral sensitivity
Synergistic Antibiotic Combinations against MDR positives 1. Anti staphylococcal Beta lactams plus Vancomycin against VISA 2. Penicillin plus Aminoglycosides or cephalosporin against Enterococci 3. Meropenem plus piperacillin plus tazobactam : against MRSA via reciprocal collateral sensitivity of its constituents.
Synergistic Antibiotic Combinations against MDR negatives 1. Carbapenem based Combinations: § Double carbapenems ( imipinem or meropenem/ ertapenem), Colistin/ meropenem against CPE § Triple combinations (double carbapenems /tigecycline (colistin) ) , (carbapenem / rifampin / colistin) against CPE 2. Colisitin/Vancomycin (linezolid) or Colistin /tigecyclin (rifampicin) in MDR Acinetobacter
ii-Antagonistic antibiotic combinations 1. Some Bacteriostatic/ bactericidal combinations The stasis produced by bacteriostatic, likely inhibits the activity of bactericidal, which works best on actively-dividing bacteria. Examples: linezolid/vancomycin against MRSA
Antagonistic Antibiotic Combinations (Cont. . ) 2. Double -lactam Antagonism in SPACE/SPICE: Induction of B-lactamase by one agent, renders the second agent ineffective. ( especially combining 3 rd GCs).
3 - DO NOT Combine Clavulanic acid and cephalosporins Clavulanic acid is a Potent inducer of the Amp. C beta-lactamase ( cephalosporinase) that confers resistance against cephalosporins. For this reason , sulbactam ( which is not reported to induce such Amp. C beta lactamases, is the preferred beta lactamases inhibitor to be combined with cephalosporins ( eg combination between cefoperazone and sulbactam)
TAKE HOME MESSAGE “THE REAL WORRY IS NOT FROM AMR BUT FROM BRAIN RESISTANCE TO CHANGE” “when fighting an evolving enemy, it is NOT right to rely on prior victories to continue. There is a glimmer of hope for winning the battle of AMR”.
- Slides: 54