Rapid Sequence Induction RSI What is RSI Administration

- Slides: 26
Rapid Sequence Induction (RSI)
What is RSI? Administration of an induction (anaesthetic) agent followed by a rapid-acting neuromuscular blocking agent Paralysis and sedation facilitate intubation Assumed the patient has a full stomach Risk of aspiration of gastric contents
Why intubate? Failure to protect/maintain airway Failure of oxygenation/ventiation What is the anticipated clinical course?
Roles of the team Airway assistance Drug preparation Circulation and monitoring assistant Drug administration: anaesthetic and emergency drugs Cricoid pressure Intubator In-line immobilisation if required
The seven Ps Preparation Pre-oxygenation Pre-treatment Paralysis and induction Protection and Positioning Placement with proof Post-intubation management
Preparation Environment Monitoring IV access Positioning of patient Drugs (drawn up & labelled)
Preparation Equipment ETT 8. 0/9. 0 Suction & catheters + Yankauer Laryngoscope with batteries; curved and long blades Bag, Valve Mask attached to Oxygen [15 litres flow rate] Bougie 10 ml syringe ETT tapes Stethoscope Catheter Mount & filter Lubrication jelly
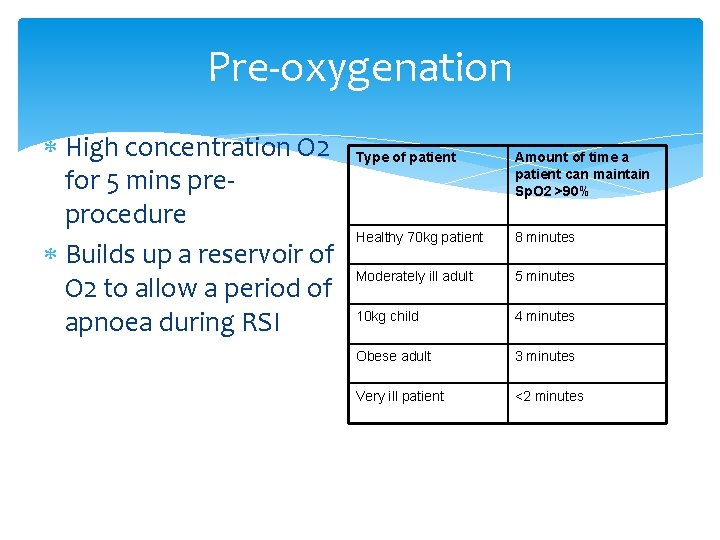
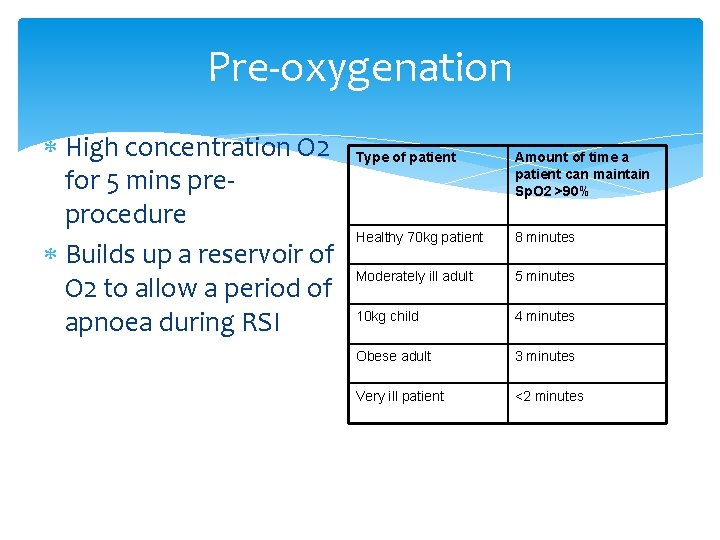
Pre-oxygenation High concentration O 2 for 5 mins preprocedure Builds up a reservoir of O 2 to allow a period of apnoea during RSI Type of patient Amount of time a patient can maintain Sp. O 2 >90% Healthy 70 kg patient 8 minutes Moderately ill adult 5 minutes 10 kg child 4 minutes Obese adult 3 minutes Very ill patient <2 minutes
Pre-treatment Some clinicians may choose to administer atropine or opiates to mitigate the effects of the procedure. Rapid fluid bolus
Paralysis with induction Anaesthetic + NBA Sodium Thiopentone Etomidate Propofol Suxamethonium Rocuronium
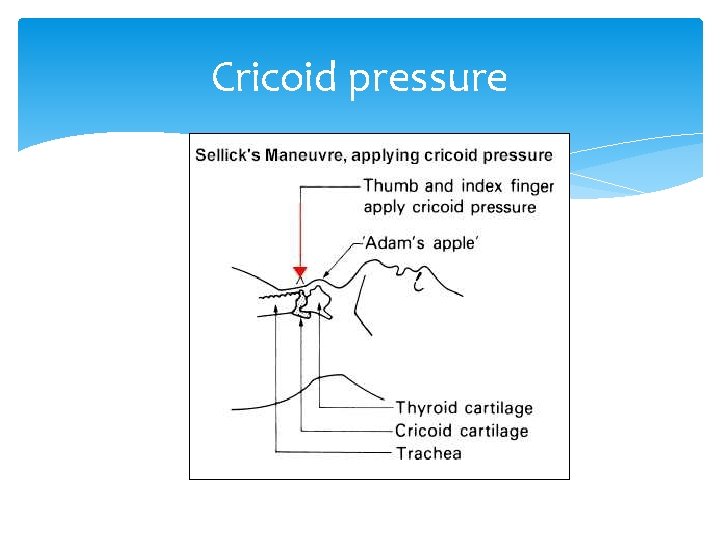
Protection & positioning Cricoid pressure Firm pressure @ 10 lbs applied to the cricoid cartilage Applied frojm when the patient loses consciousness until ETT position has been verified & cuff inflated Release when instructed by the Anaesthetist
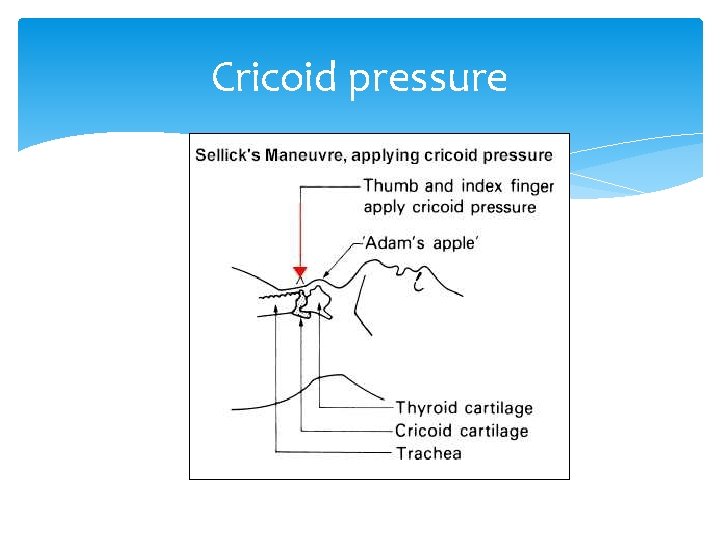
Cricoid pressure
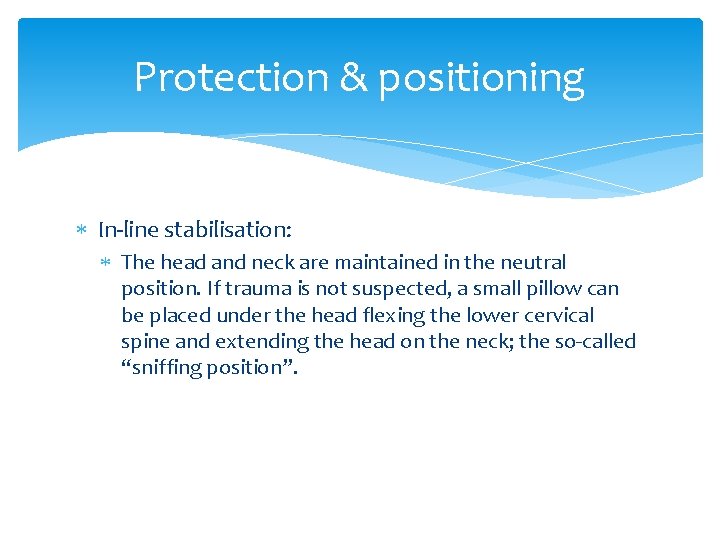
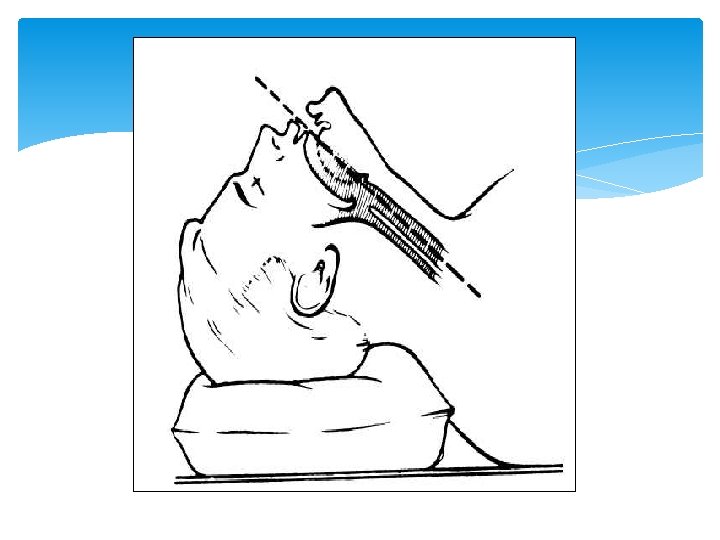
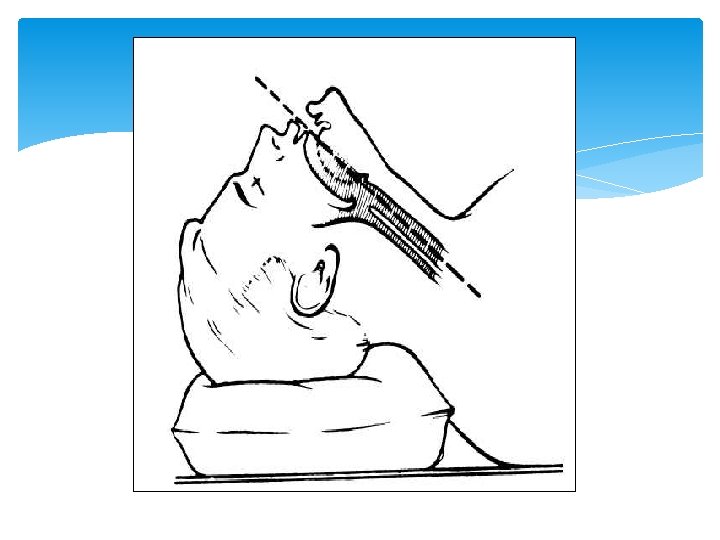
Protection & positioning In-line stabilisation: The head and neck are maintained in the neutral position. If trauma is not suspected, a small pillow can be placed under the head flexing the lower cervical spine and extending the head on the neck; the so-called “sniffing position”.
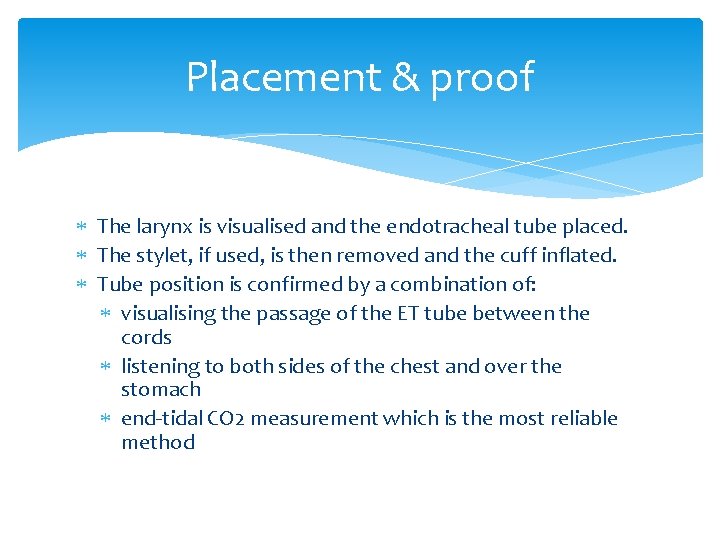
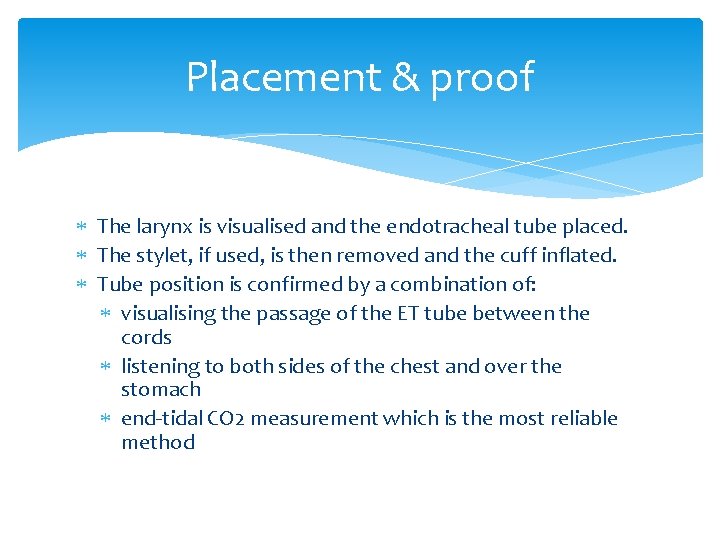
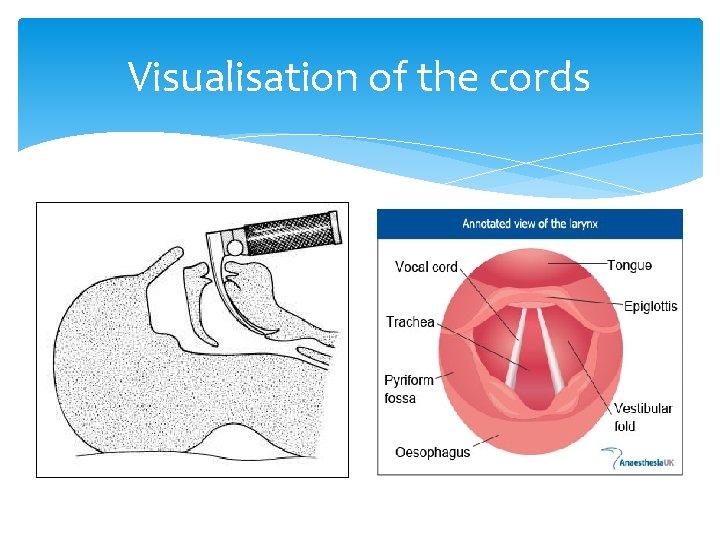
Placement & proof The larynx is visualised and the endotracheal tube placed. The stylet, if used, is then removed and the cuff inflated. Tube position is confirmed by a combination of: visualising the passage of the ET tube between the cords listening to both sides of the chest and over the stomach end-tidal CO 2 measurement which is the most reliable method
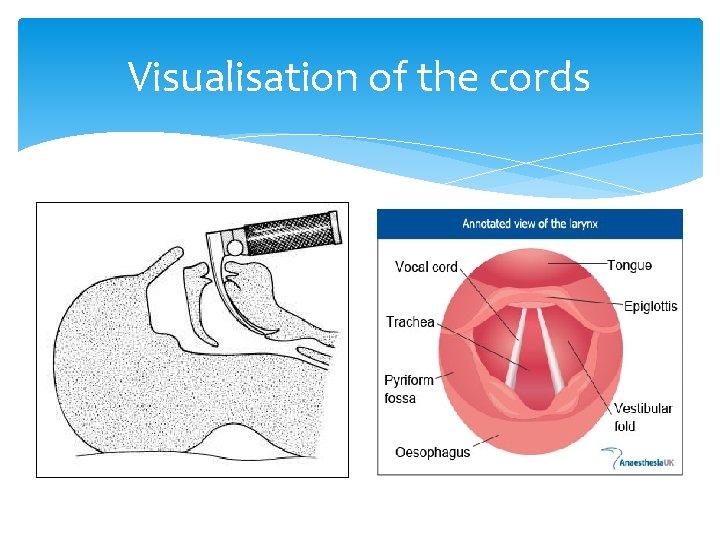
Visualisation of the cords
Difficult & failed airway How do we anticipate which patients will be difficult to intubate? Look externally and internally Obstruction Neck mobility
Failure to intubate Can’t oxygenate, can’t ventilate 3 failed attempts Immediate priorities: Oxygenate Call for senior help See DAS guidance
Other optionss when intubation is anticipated to be difficult: Fibreoptic laryngoscope Bougie Stylet Aintree catheter (cook)
Post-intubation management Secure the tube Ventilate Monitoring (ECG, BP, Sp. O 2, ETCO 2) CXR ABG Maintenance of sedation
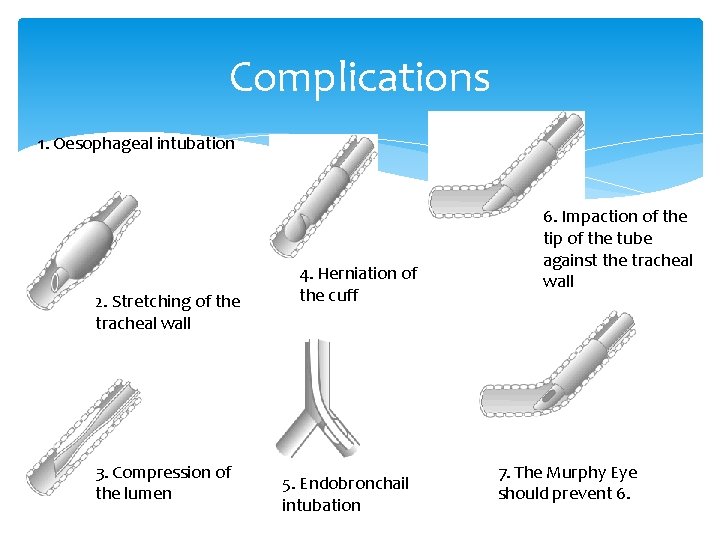
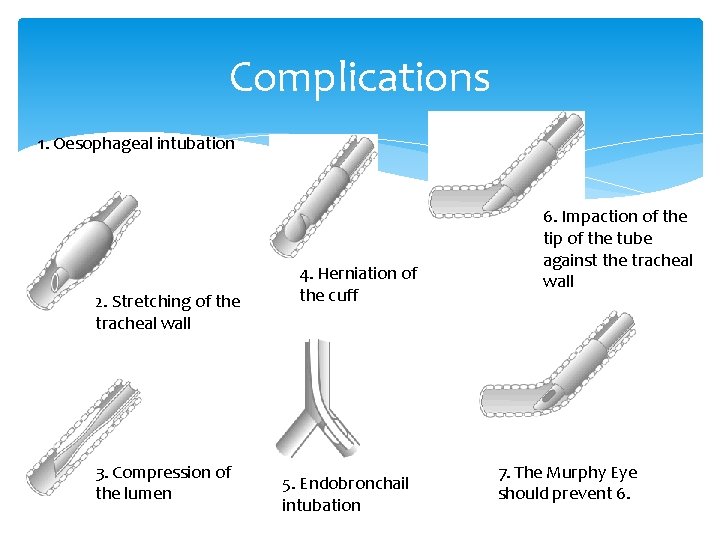
Complications 1. Oesophageal intubation 2. Stretching of the tracheal wall 3. Compression of the lumen 4. Herniation of the cuff 5. Endobronchail intubation 6. Impaction of the tip of the tube against the tracheal wall 7. The Murphy Eye should prevent 6.
Trolley contents aka – What the heck is this?

What is this?
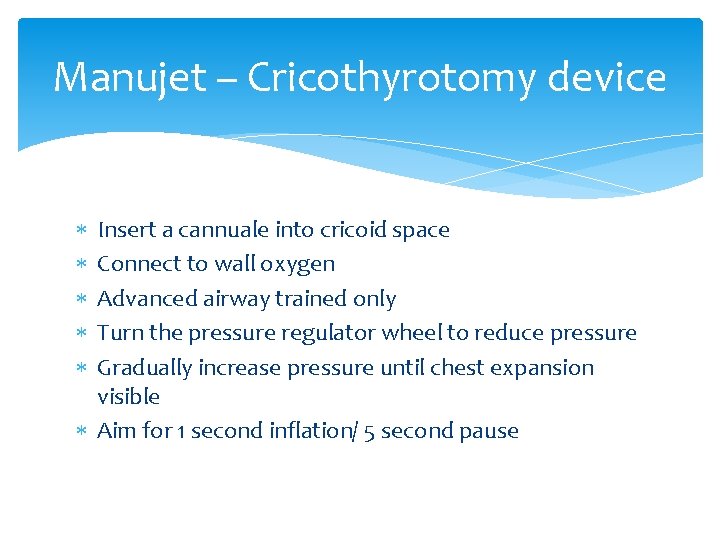
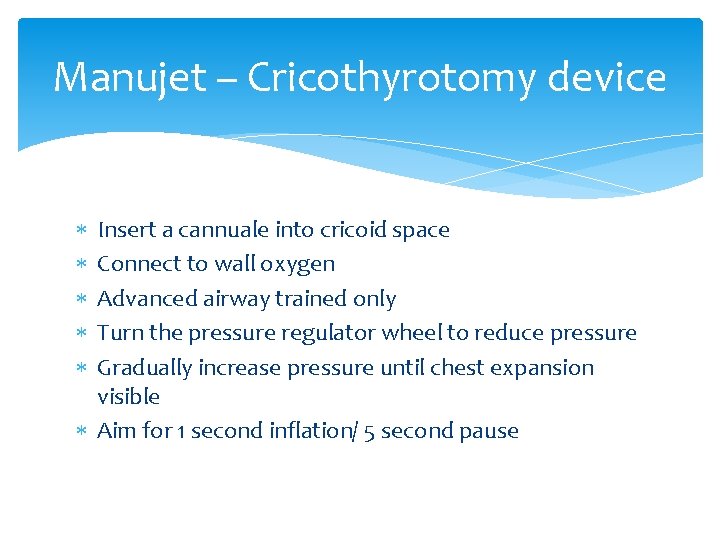
Manujet – Cricothyrotomy device Insert a cannuale into cricoid space Connect to wall oxygen Advanced airway trained only Turn the pressure regulator wheel to reduce pressure Gradually increase pressure until chest expansion visible Aim for 1 second inflation/ 5 second pause
What is this?
Cricothyrotomy Kit Incision is made through the skin and cricothyroid membrane to esablish an airway. Useful in patients with aiways obstructed due to trauma and foreign bodies. Easier and quicker then a tracheostomy Last resort?