Rapid sequence induction RSI Dr S Parthasarathy MD




- Slides: 38
Rapid sequence induction (RSI) Dr. S. Parthasarathy MD. , DA. , DNB, Dip. Diab. DCA, Dip. Software based statistics. Ph. D ( physiology), IDRA
• Rapid sequence induction (RSI) is a method of achieving rapid control of the airway whilst minimising the risk of regurgitation and aspiration of gastric contents. • What is the concept ?
• Time between loss of protective airway reflexes to insertion of cuffed endotracheal tube to be kept minimum • The scenario ? ? • Especially Unprepared patient with a risk of aspiration
What is the difference • • Sedate Mask ventilation sufficient – check Make them apneic Intubate Take that risk
What is the risk of aspiration ? ? • 1 in 2000 to 1 in 14000 • It varies • But the mortality – 1 in 72000 Obtunded patients – no RSI ? ? Intubate
History • Stept and Safar in 1970 • Conscious or unconscious patient with full stomach • Intracranial pathology and trauma • 15 step process for two years
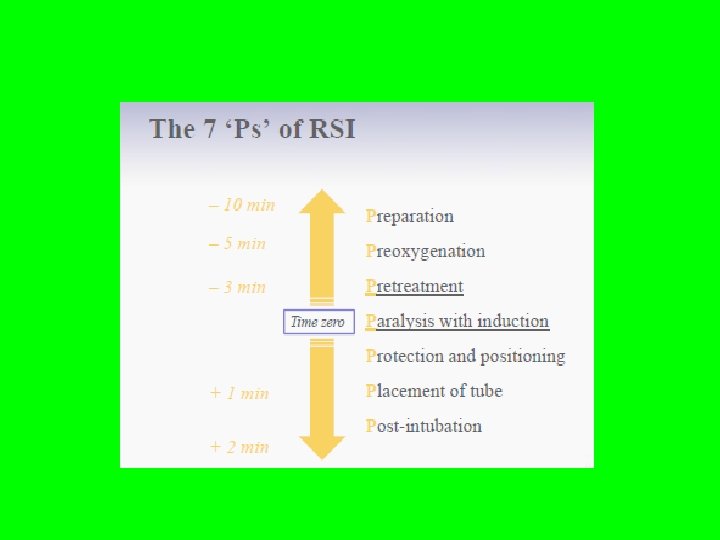
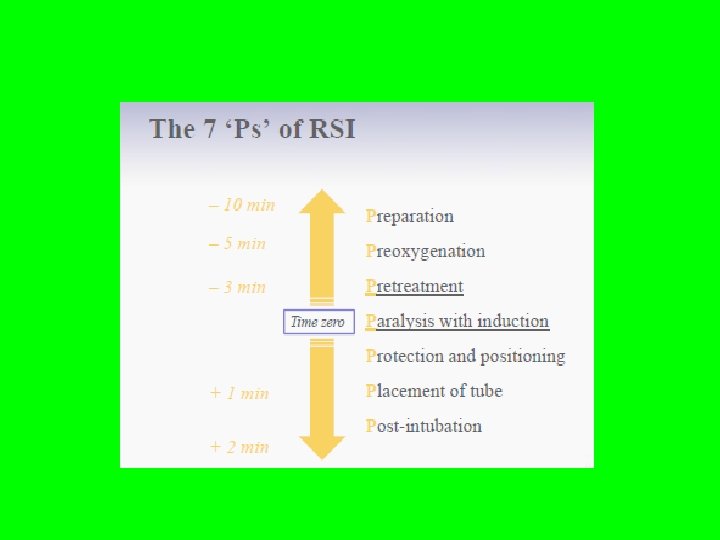
Evolved now as • Seven P s of RSI • • Preparation Pre oxygenation Pretreatment Paralyses Positioning Prove placement Post intubation management
Preparation • Equipment • Drugs and support staff • • SOAPME Suction oxygen airway evaluation pharmacology, monitors , equipment for difficult airway

Preoxygenation • 100 % oxygen for 3 -5 minutes • 4 vital capacity breaths • Pregnancy , obesity, cardio respiratory disease • Elderly and children desaturate earlier
Pretreatment • Atropine - ? Use. Only the second dose of succinyl choline • Opioids – the original drugs were long acting – but after fentanyl and analogues – OK • One tenth the dose of NDPs – but the dose of scoline – 2 mg/kg minimal – penetrating eye injury – distressing few seconds because 3 minutes is the ideal pre time – for not that emergent cases • Lignocaine 1 – 2 mg/kg – used prior to the advent of newer opioids
Paralyses with induction • Safar started with predetermined dose of thio and scoline • 150 and 100 respectively for a 70 kg patient • Intravenous induction facilitates loss of consciousness in one arm–brain circulation time, minimizing the time from loss of consciousness to intubation. Ideally, the chosen induction agent should provide a rapid onset and a rapid recovery from anaesthesia with minimal cardiovascular and systemic side effects.
Paralyses - continued • Thiopentone 3 - 5 mg / kg – fast • Propofol 1 mg/ kg but depression of reflexes better • Midaz and ketamine for shocked patients and • Etomidate for hemodynamic stability • Acidic relaxants and alkaline thio – precipitate – loss of IV lines
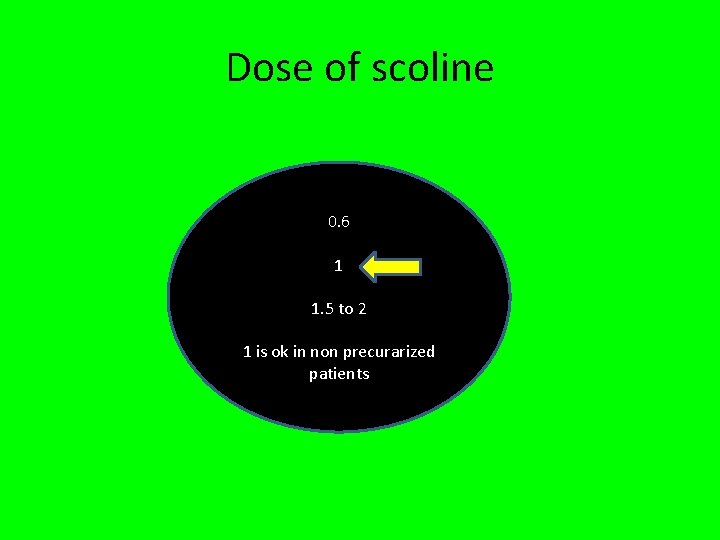
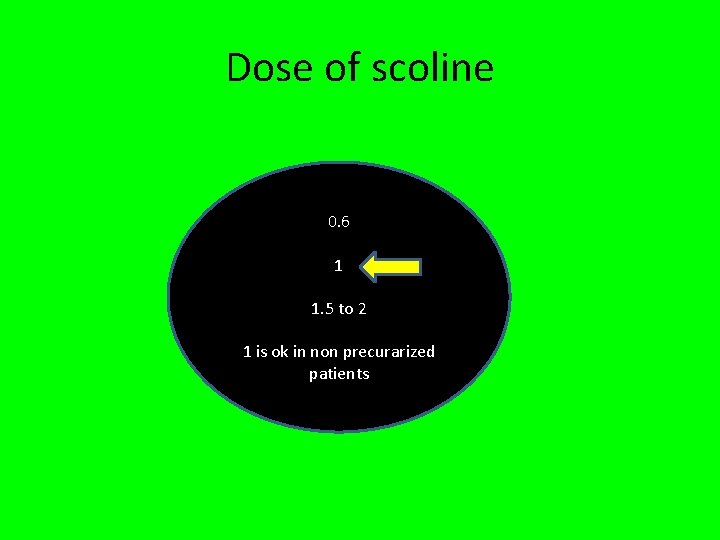
Dose of scoline 0. 6 1 1. 5 to 2 1 is ok in non precurarized patients
Non depolarizers • Rocuronium comes nearer • Crush injury , raised ICP or IOP , hyperkalemia • 0. 6 mg / kg – ok intubating conditions in 1 minute • But 0. 9 – 1. 2 means – excellent – long acting but want to reverse in CICV, suggamadex
Priming and timing • One tenth of the nondepolarizer is given prior three minutes to original dose • Partial weakness problem • Timing – means give the full dose just prior to thiopentone

Positioning • Sniffing position
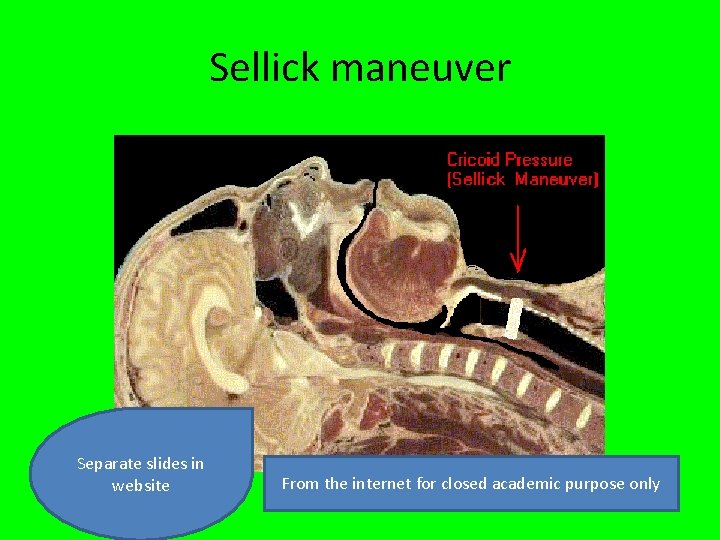
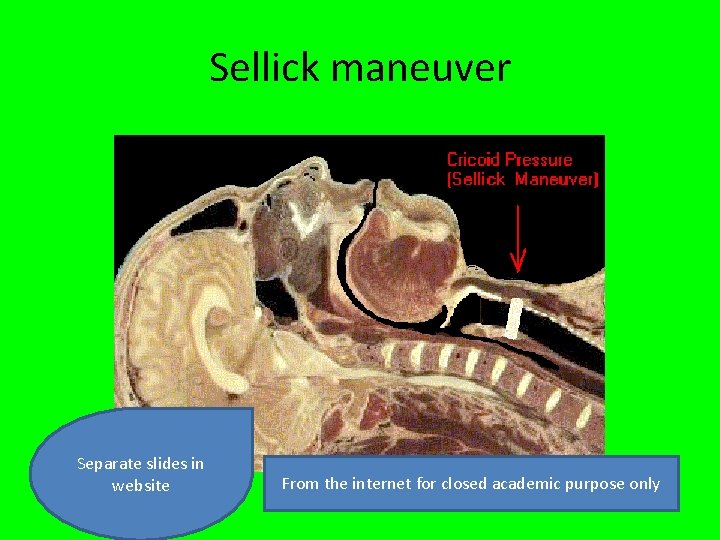
Sellick maneuver Separate slides in website From the internet for closed academic purpose only
Prove • Confirm and prove placement of endotracheal tube in the correct position • Visual • Stethoscope • Capnograph
Post intubation managemant • Need for mechanical ventilation • Monitoring • Vital signs
Modified rapid sequence induction • Trial of mask ventilation • Use of nondepolarizers • Proseal LMA Rapid sequence induction (RSI) or Rapid sequence airway
• Name • Rapid sequence induction (RSI) ? • Actually • Rapid sequence intubation ? !
Clinical implications • • Emergency surgical procedures Special – peritonitis Ryles tube Abdominal distension insertion may not Opioids eliminate the risks Trauma alcohol Pain
Pregnancy • Physical and physiological changes – prone • Elective LSCS is RSI ( 95 % anesthesiologists prefer) • Thio and scoline obvious choice • Rocuronium, difficult cricoid pressure , possible proseal ? ?
Morbid obesity and RSI • • Weight and drug dosage CVS and RS changes Fatty neck Comorbidities Prone for aspiration And go ahead with RSI
Neonates • Inhalational agents or without it also • Prone for arrhythmias , desaturation, intra ventricular hemorhage, vocal cord injuries and a longer time ? ? • RSI is acceptable when there are no facial or airway anomalies
So many !! • inadvertent esophageal intubation, • esophageal perforation, and trauma to the lips, gums, or tongue. • Vocal folds edema, ulcerations of the arytenoids, ulcerations of the posterior glottis, and ulcerations of the main stem bronchus have been described in the literature
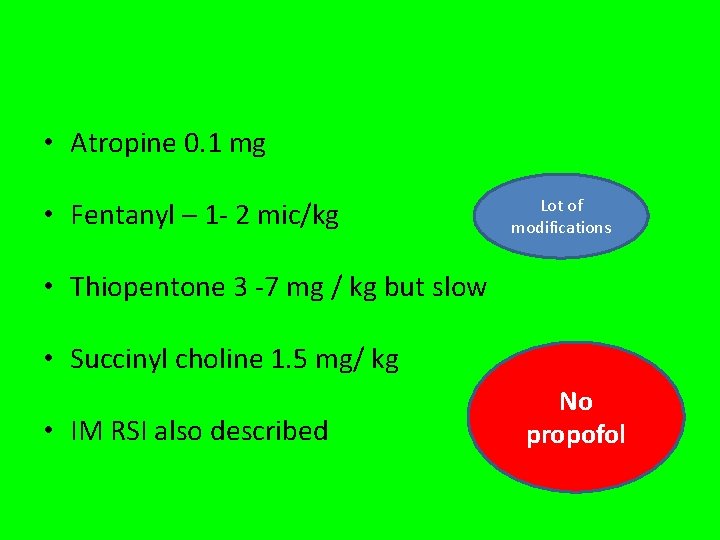
• Atropine 0. 1 mg • Fentanyl – 1 - 2 mic/kg Lot of modifications • Thiopentone 3 -7 mg / kg but slow • Succinyl choline 1. 5 mg/ kg • IM RSI also described No propofol
Outside the operation theatre – ER • • • Can be done by non anesthesiologists also Can be done by technicians also Urgent – no 100 % oxygen also Only with sedatives Sedative facilitated intubation (SFI) – midaz and ketamine with atropine is used for that purpose
ICU • Hypoxic acidotic and collapsed stage • RSI decreased the morbidity by 50% • Two operators • Experienced staff
• • • Preoxygenation – must 500 ml crystalloids – vasopressors Minimum diastolic – 35 mm. Hg preferable Newer short acting opioids Etomidate Scoline

Prehospital RSI • • Arrest Trauma Hypoxic Unstable patients • Gagging , uncooperative patients made failure common • Hence RSI
Extubation also important • In patients for whom an RSI was indicated due to aspiration risk, emergence remains a high-risk time for further aspiration events. • Awake patient with intact reflexes • Left lateral head-down positioning may further reduce the chance of aspiration, at the expense of reduced access to the airway.
Complications of RSI • Drugs • Cricoid pressure • Due to intubation or due to “cant do it”

CICV • Release CP • Insert LMA • Keep CP again • Try to ventilate • Still no – means – take out CP and try
• • • Difficult airway 2 % Hypoxia – 2% Hypotension – 0. 7 % Hypertension - ? Arrhythmias -? Scoline and arrhythmias !!
Rupture of esophagus • Clear cut vomiting during RSI, relax CP and suck • 20 or 30 40 N pressure • Possible but rare cricoid fractures • Awareness – worst may be upto 50 % • Think of high doses of Thio – 7 mg/kg in fit individuals
Summary • • What is it ? And the concept – name ? Preparation , Pre oxygenation , Pretreatment Paralyses, Positioning , Prove placement Post intubation management Outside the OR Neonates Complications