Rapid Acting or Prandial Insulin H Delshad M


- Slides: 80

Rapid Acting or Prandial Insulin H. Delshad M. D Endocrinologist Research Institute For Endocrine Sciences
INSULIN Banting & Best 1921 The most powerful agent we have to control glucose
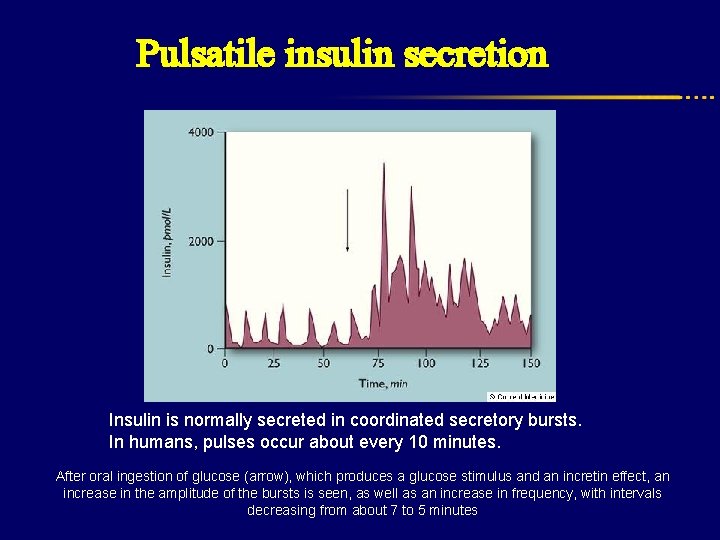
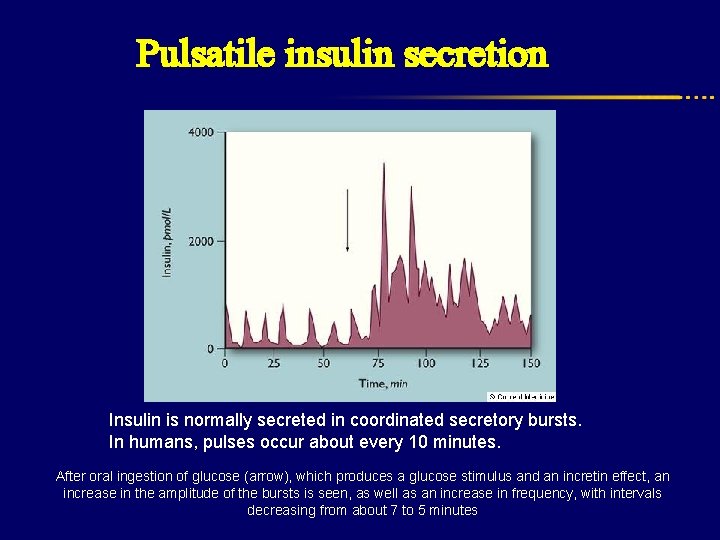
Pulsatile insulin secretion Insulin is normally secreted in coordinated secretory bursts. In humans, pulses occur about every 10 minutes. After oral ingestion of glucose (arrow), which produces a glucose stimulus and an incretin effect, an increase in the amplitude of the bursts is seen, as well as an increase in frequency, with intervals decreasing from about 7 to 5 minutes
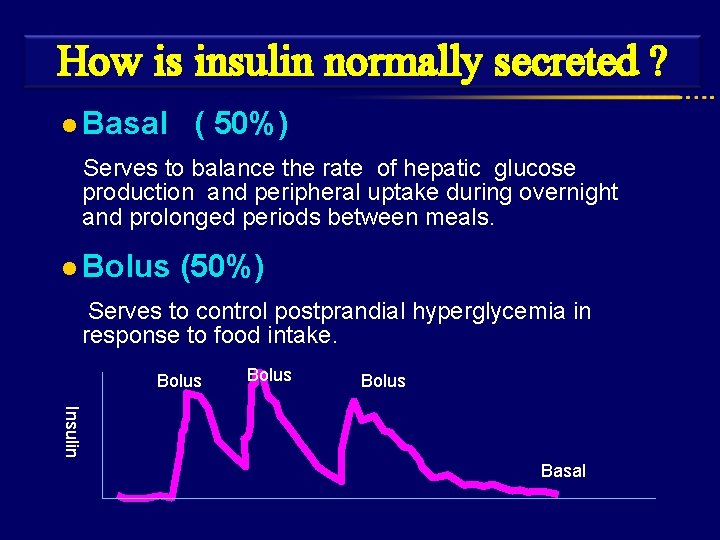
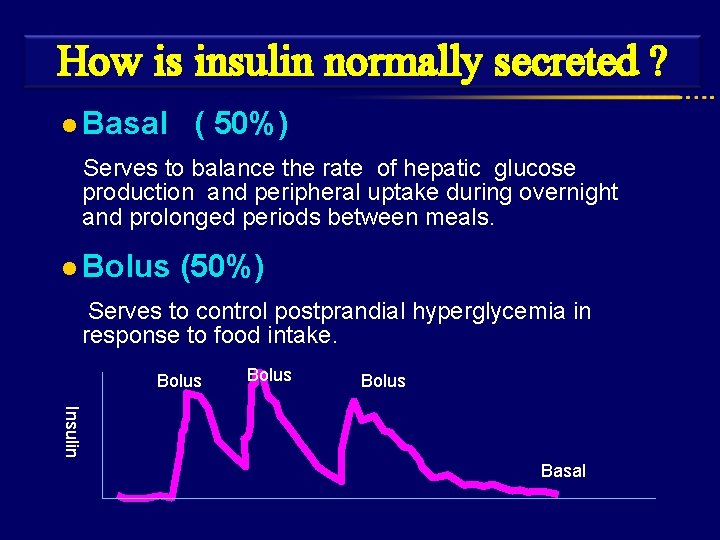
How is insulin normally secreted ? l Basal ( 50%) Serves to balance the rate of hepatic glucose production and peripheral uptake during overnight and prolonged periods between meals. l Bolus (50%) Serves to control postprandial hyperglycemia in response to food intake. Bolus Basal Bolus Insulin Basal
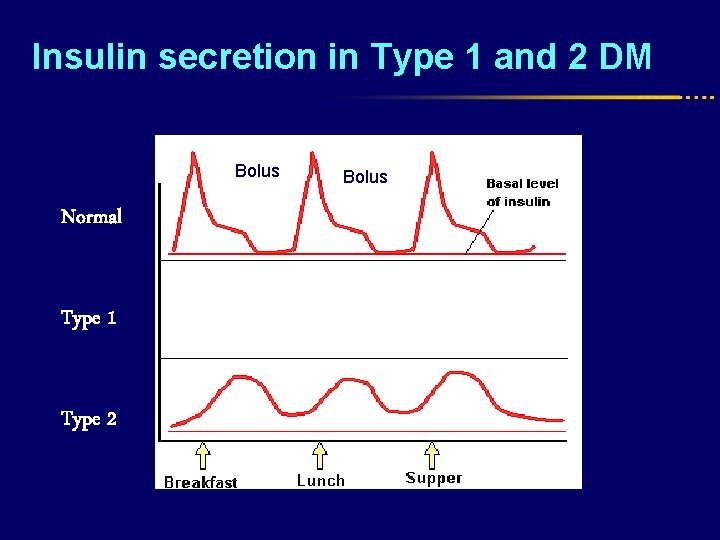
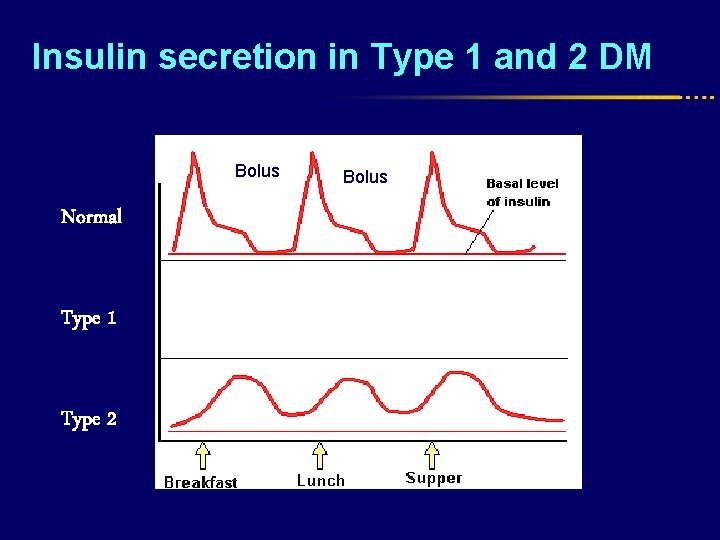
Insulin secretion in Type 1 and 2 DM Prandial Bolus Normal Type 1 Type 2 Bolus
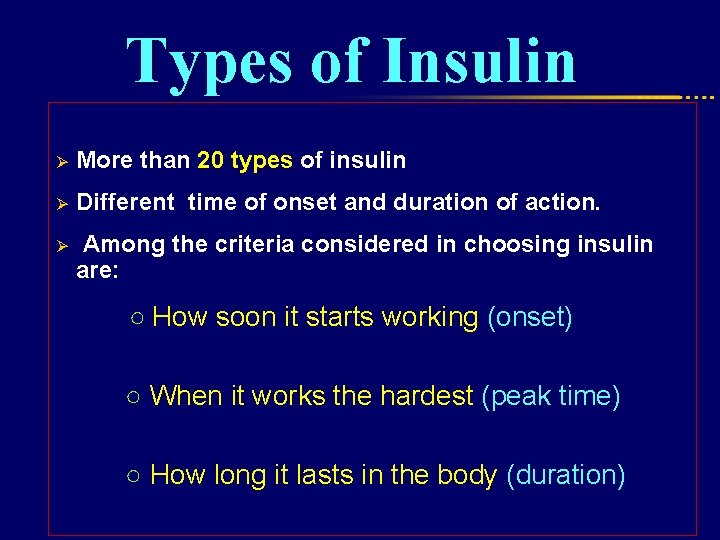
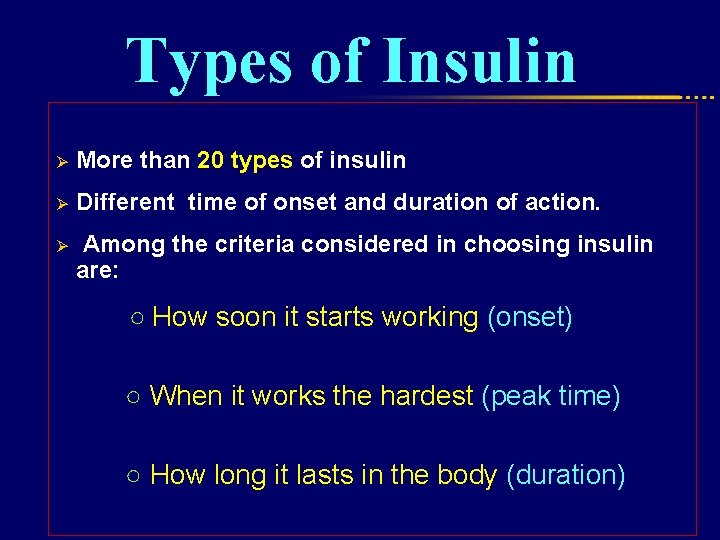
Types of Insulin Ø More than 20 types of insulin Ø Different time of onset and duration of action. Ø Among the criteria considered in choosing insulin are: ○ How soon it starts working (onset) ○ When it works the hardest (peak time) ○ How long it lasts in the body (duration)
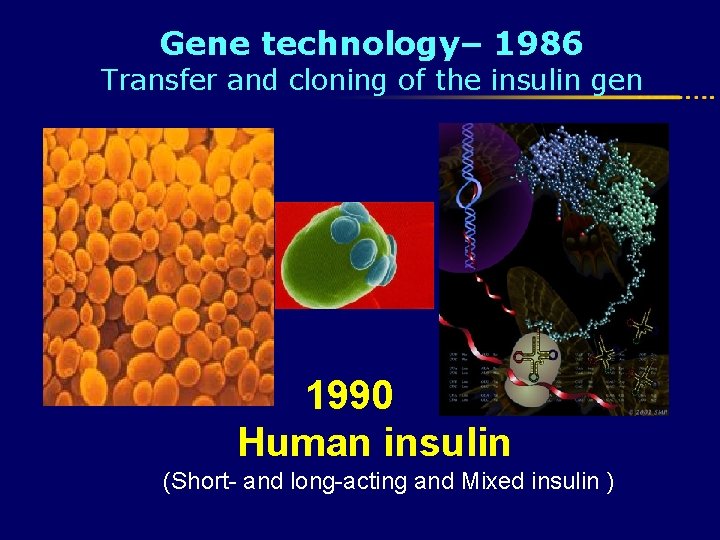
Gene technology– 1986 Transfer and cloning of the insulin gen 1990 Human insulin (Short- and long-acting and Mixed insulin )
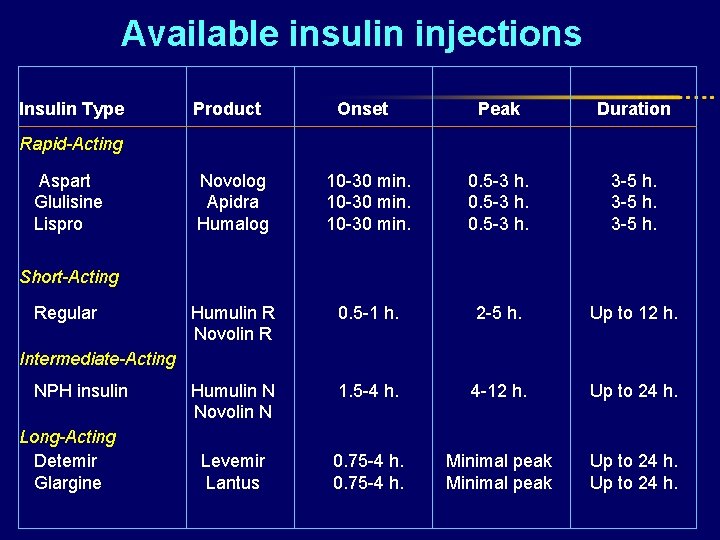
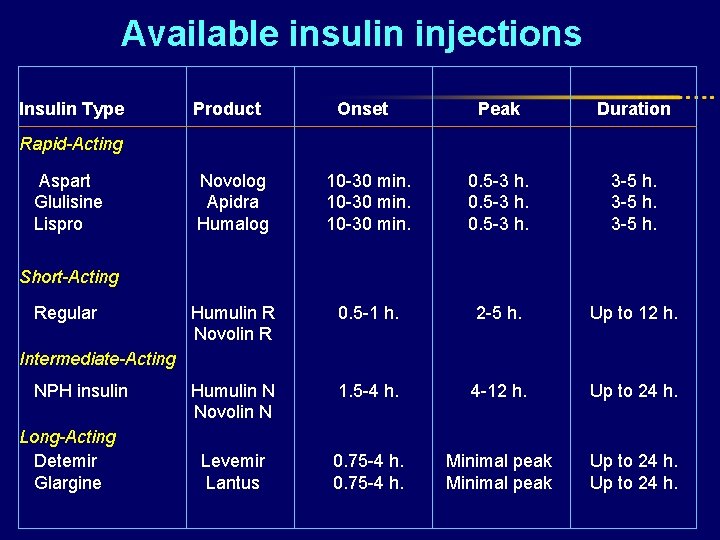
Available insulin injections Insulin Type Product Onset Peak Duration Novolog Apidra Humalog 10 -30 min. 0. 5 -3 h. 3 -5 h. Humulin R Novolin R 0. 5 -1 h. 2 -5 h. Up to 12 h. Humulin N Novolin N 1. 5 -4 h. 4 -12 h. Up to 24 h. Levemir Lantus 0. 75 -4 h. Minimal peak Up to 24 h. Rapid-Acting Aspart Glulisine Lispro Short-Acting Regular Intermediate-Acting NPH insulin Long-Acting Detemir Glargine
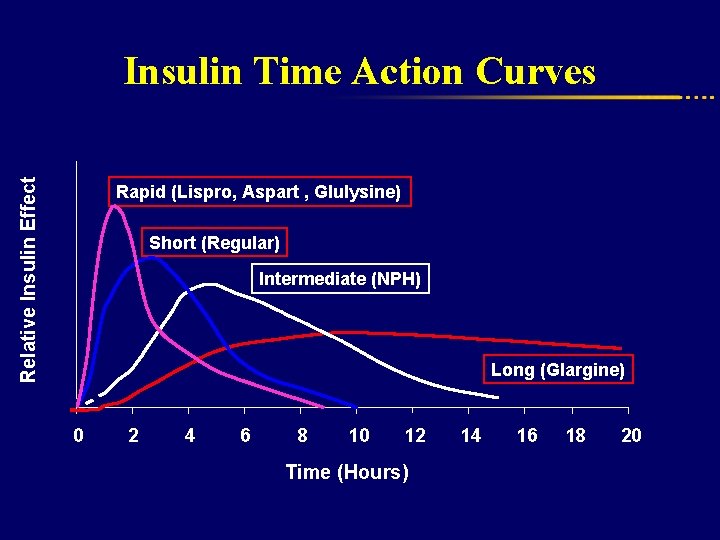
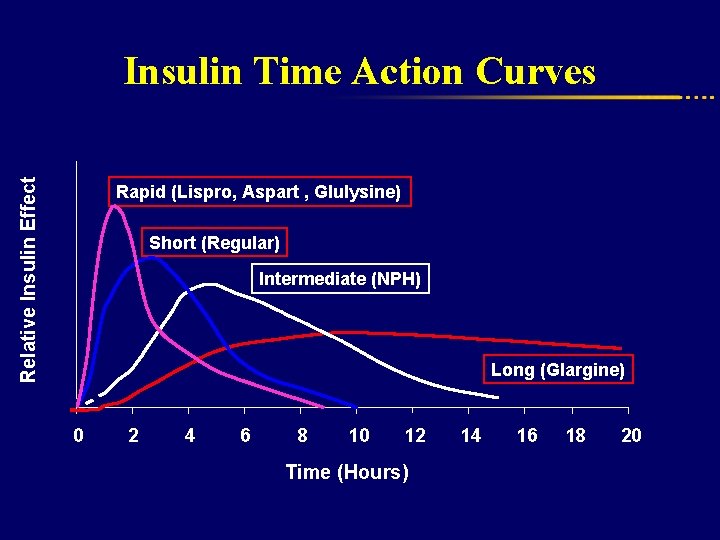
Relative Insulin Effect Insulin Time Action Curves Rapid (Lispro, Aspart , Glulysine) Short (Regular) Intermediate (NPH) Long (Glargine) 0 2 4 6 8 10 12 Time (Hours) 14 16 18 20
Insulin treatment regimens Conventional Advanced insulin regimen
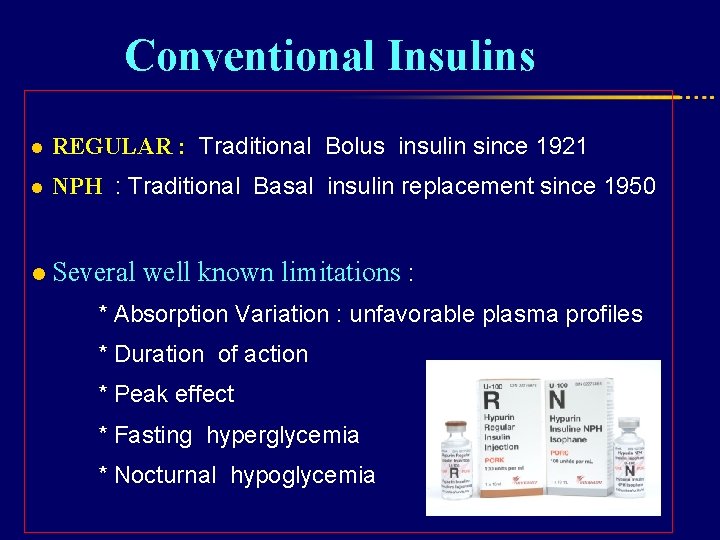
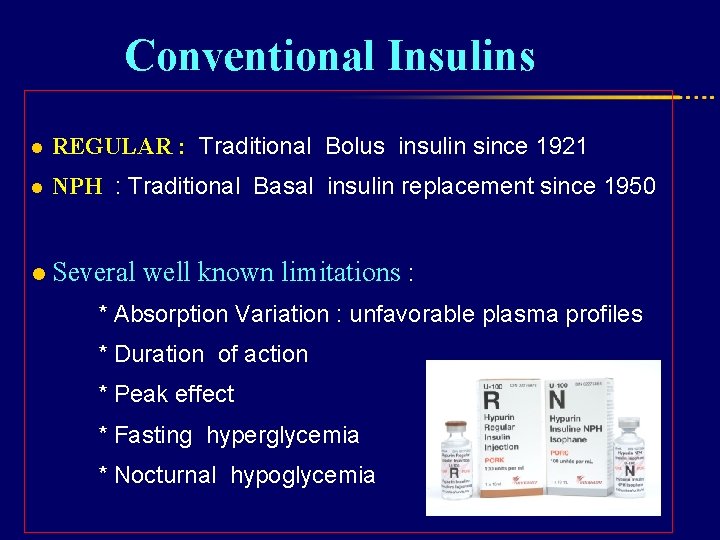
Conventional Insulins l REGULAR : Traditional Bolus insulin since 1921 l NPH : Traditional Basal insulin replacement since 1950 l Several well known limitations : * Absorption Variation : unfavorable plasma profiles * Duration of action * Peak effect * Fasting hyperglycemia * Nocturnal hypoglycemia
Advanced insulin regimen Physiologic, Multidose , Flexible, Functional , Basal-bolus
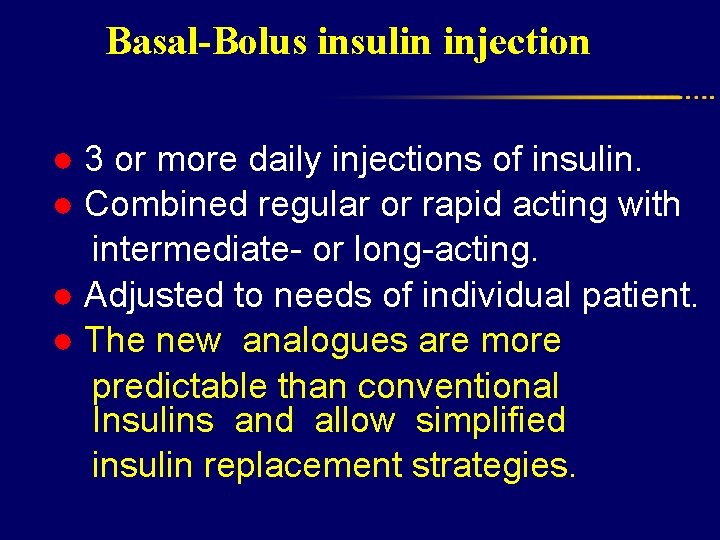
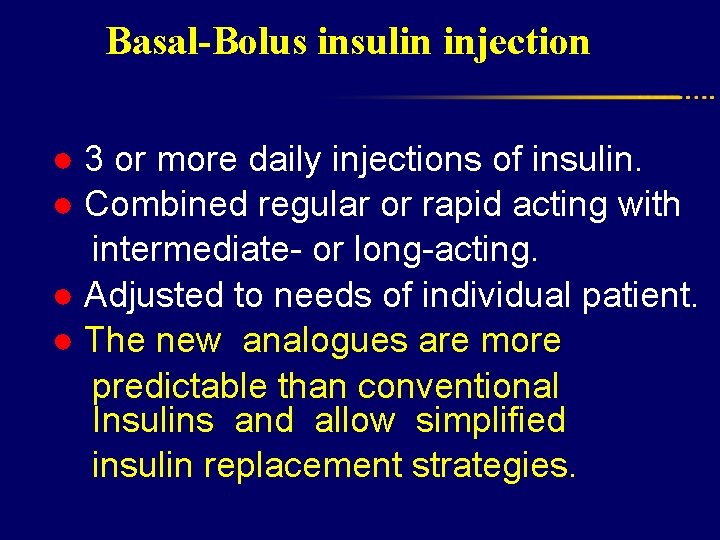
Basal-Bolus insulin injection ● 3 or more daily injections of insulin. ● Combined regular or rapid acting with intermediate- or long-acting. ● Adjusted to needs of individual patient. ● The new analogues are more predictable than conventional Insulins and allow simplified insulin replacement strategies.
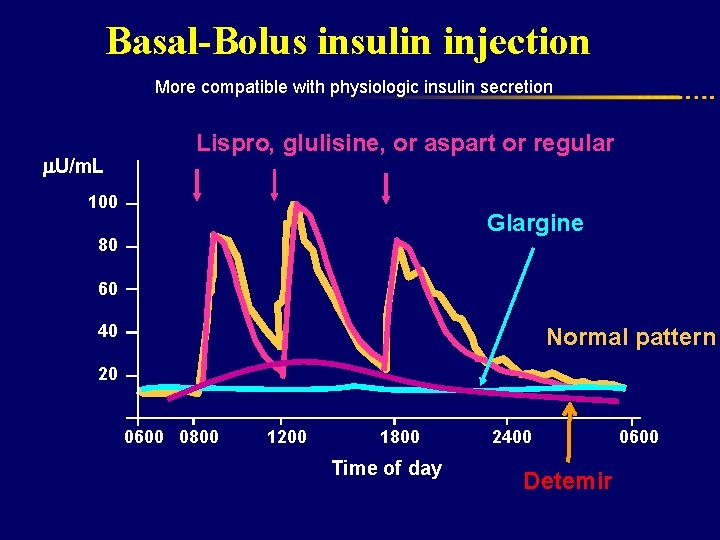
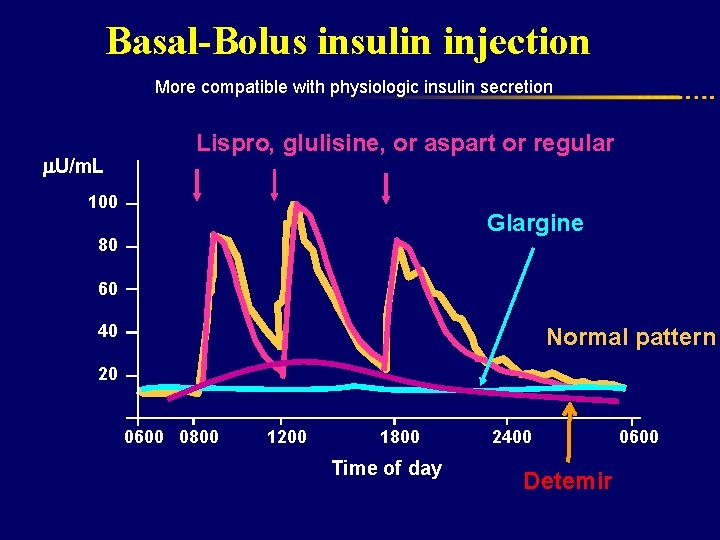
Basal-Bolus insulin injection More compatible with physiologic insulin secretion Lispro, glulisine, or aspart or regular U/m. L 100 Glargine 80 60 40 Normal pattern 20 0600 0800 1200 1800 Time of day 2400 Detemir 0600
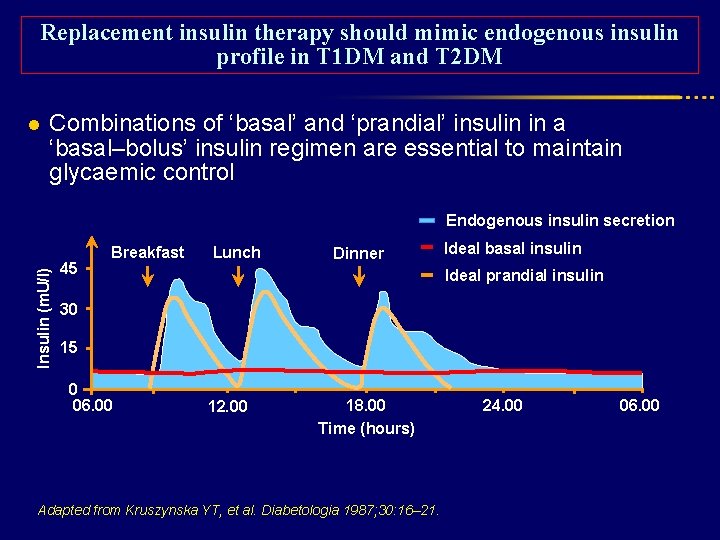
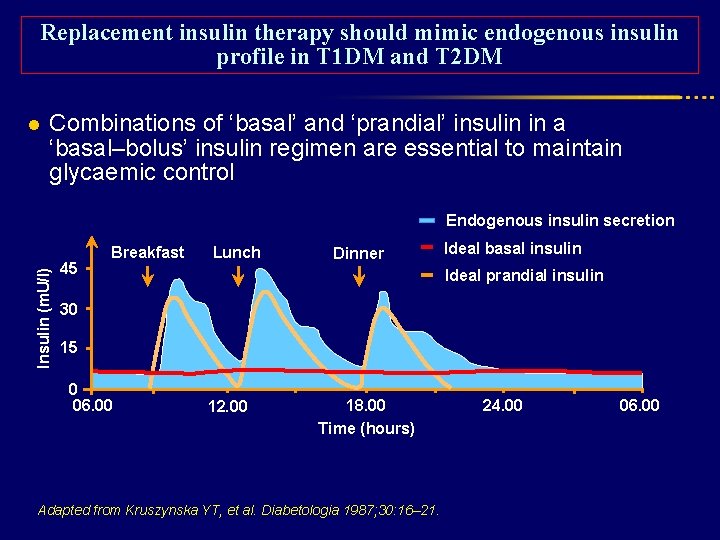
Replacement insulin therapy should mimic endogenous insulin profile in T 1 DM and T 2 DM l Combinations of ‘basal’ and ‘prandial’ insulin in a ‘basal–bolus’ insulin regimen are essential to maintain glycaemic control Insulin (m. U/l) Endogenous insulin secretion 45 Breakfast Lunch Dinner Ideal basal insulin Ideal prandial insulin 30 15 0 06. 00 12. 00 18. 00 Time (hours) Adapted from Kruszynska YT, et al. Diabetologia 1987; 30: 16– 21. 24. 00 06. 00
• FBS • PPBS Relative contribution to Hb. A 1 c
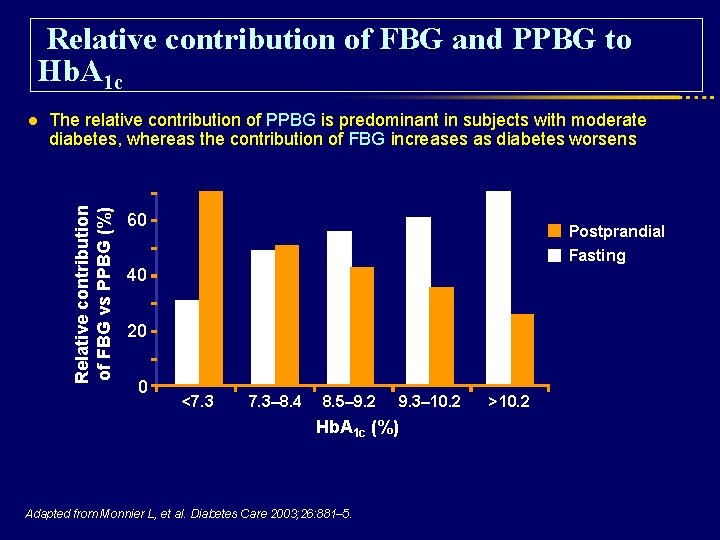
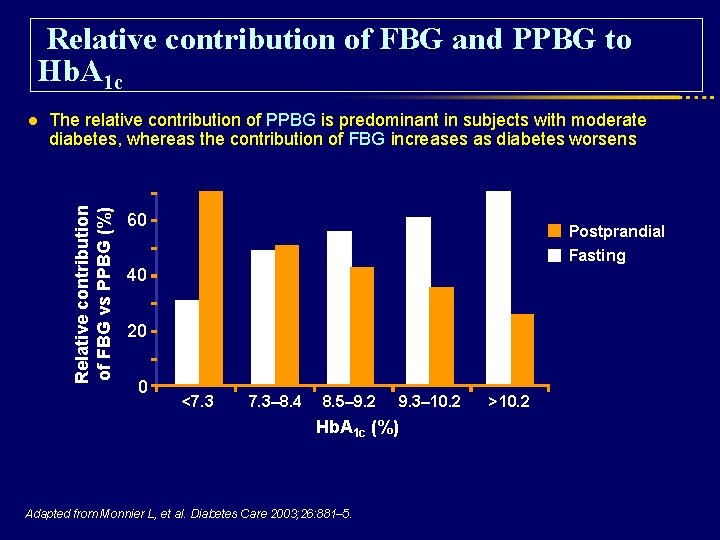
Relative contribution of FBG and PPBG to Hb. A 1 c The relative contribution of PPBG is predominant in subjects with moderate diabetes, whereas the contribution of FBG increases as diabetes worsens Relative contribution of FBG vs PPBG (%) l 60 Postprandial Fasting 40 20 0 <7. 3– 8. 4 8. 5– 9. 2 Hb. A 1 c (%) Adapted from Monnier L, et al. Diabetes Care 2003; 26: 881– 5. 9. 3– 10. 2 >10. 2
The Importance of intensive therapy: Controlling Fasting and Post Prandial Glucose
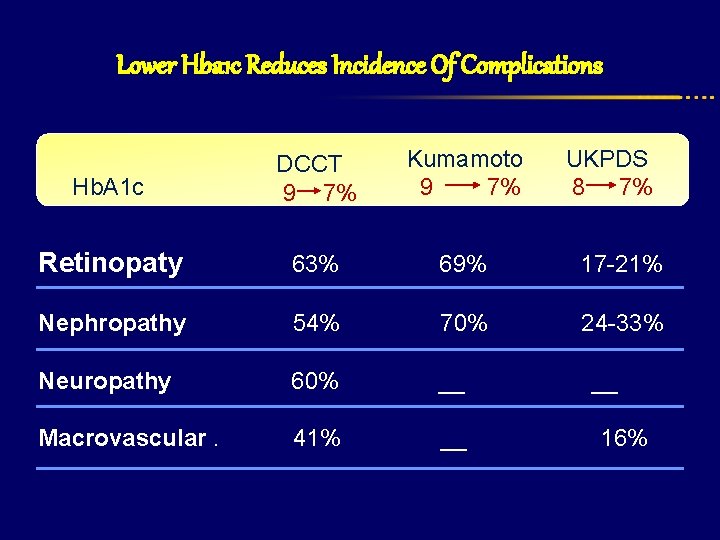
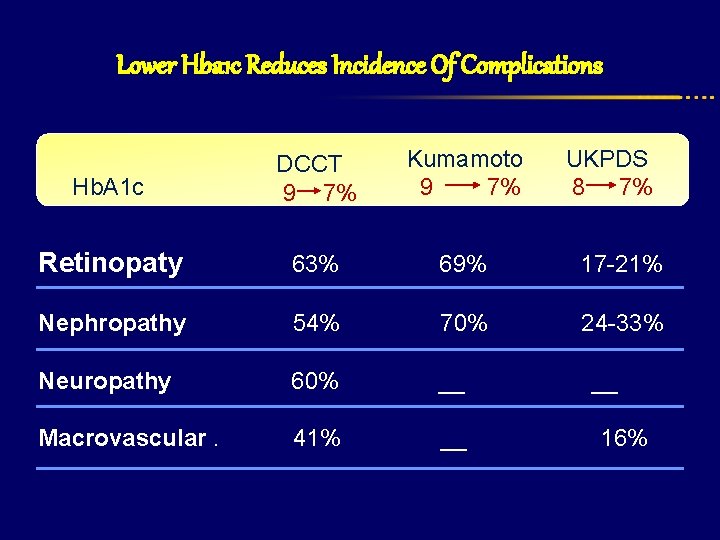
Lower Hba 1 c Reduces Incidence Of Complications Hb. A 1 c DCCT 9 7% Kumamoto 9 7% UKPDS 8 7% Retinopaty 63% 69% 17 -21% Nephropathy 54% 70% 24 -33% Neuropathy 60% __ Macrovascular. 41% __ 16%
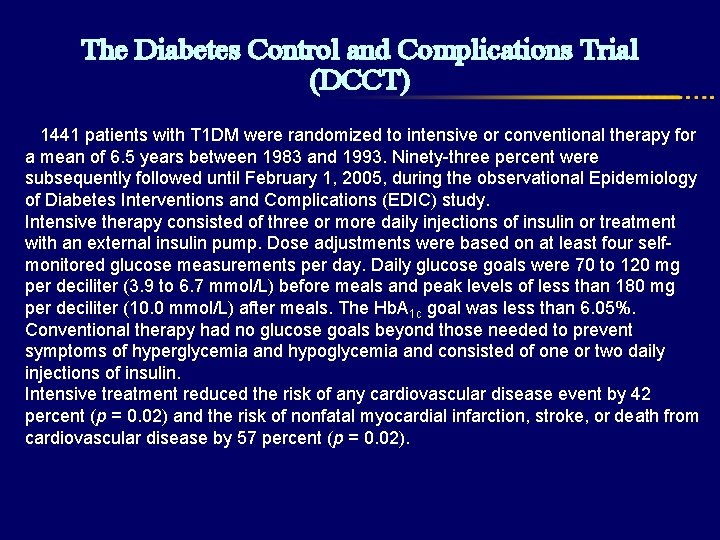
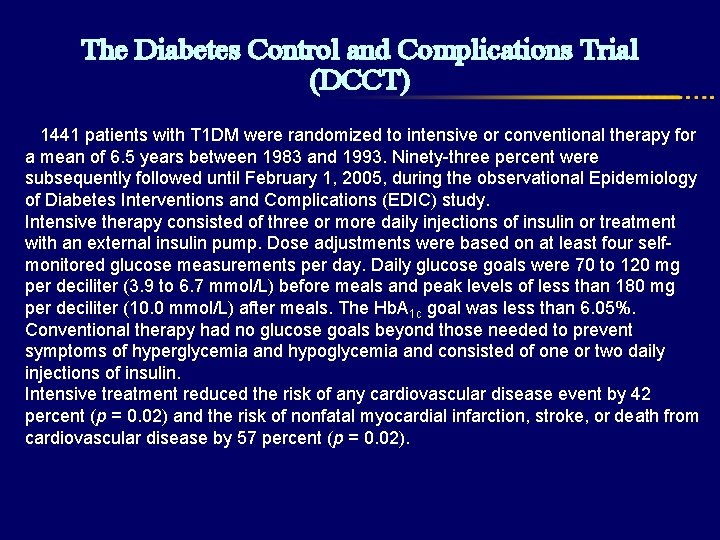
The Diabetes Control and Complications Trial (DCCT) 1441 patients with T 1 DM were randomized to intensive or conventional therapy for a mean of 6. 5 years between 1983 and 1993. Ninety-three percent were subsequently followed until February 1, 2005, during the observational Epidemiology of Diabetes Interventions and Complications (EDIC) study. Intensive therapy consisted of three or more daily injections of insulin or treatment with an external insulin pump. Dose adjustments were based on at least four selfmonitored glucose measurements per day. Daily glucose goals were 70 to 120 mg per deciliter (3. 9 to 6. 7 mmol/L) before meals and peak levels of less than 180 mg per deciliter (10. 0 mmol/L) after meals. The Hb. A 1 c goal was less than 6. 05%. Conventional therapy had no glucose goals beyond those needed to prevent symptoms of hyperglycemia and hypoglycemia and consisted of one or two daily injections of insulin. Intensive treatment reduced the risk of any cardiovascular disease event by 42 percent (p = 0. 02) and the risk of nonfatal myocardial infarction, stroke, or death from cardiovascular disease by 57 percent (p = 0. 02).
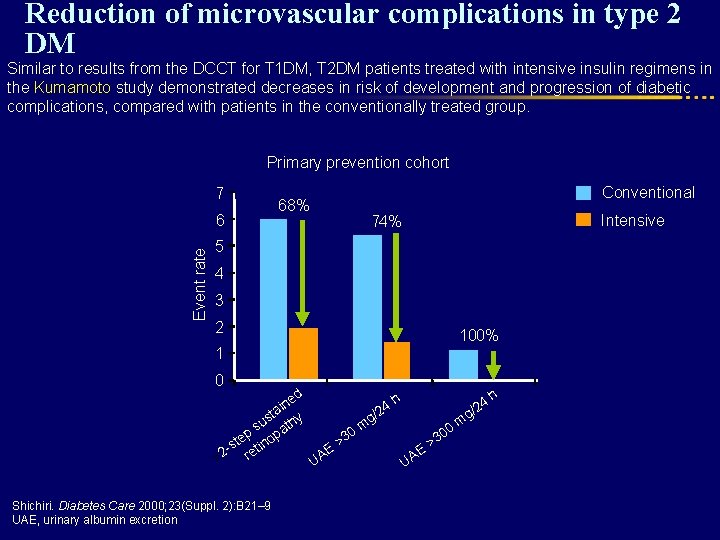
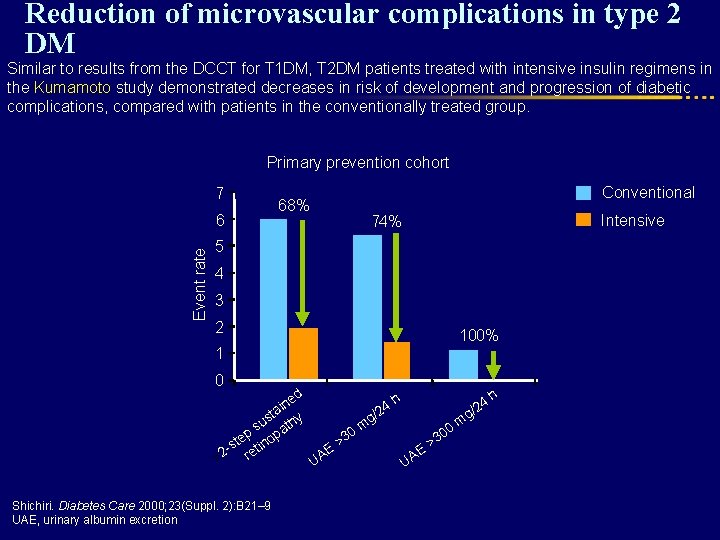
Reduction of microvascular complications in type 2 DM Similar to results from the DCCT for T 1 DM, T 2 DM patients treated with intensive insulin regimens in the Kumamoto study demonstrated decreases in risk of development and progression of diabetic complications, compared with patients in the conventionally treated group. Primary prevention cohort 7 Event rate 6 68% Conventional Intensive 74% 5 4 3 2 100% 1 0 h ed h 4 n i 4 2 / 2 g sta hy g/ m u t m s 0 00 p opa 3 3 e t > > -s tin E E A A >2 re U U Shichiri. Diabetes Care 2000; 23(Suppl. 2): B 21– 9 UAE, urinary albumin excretion
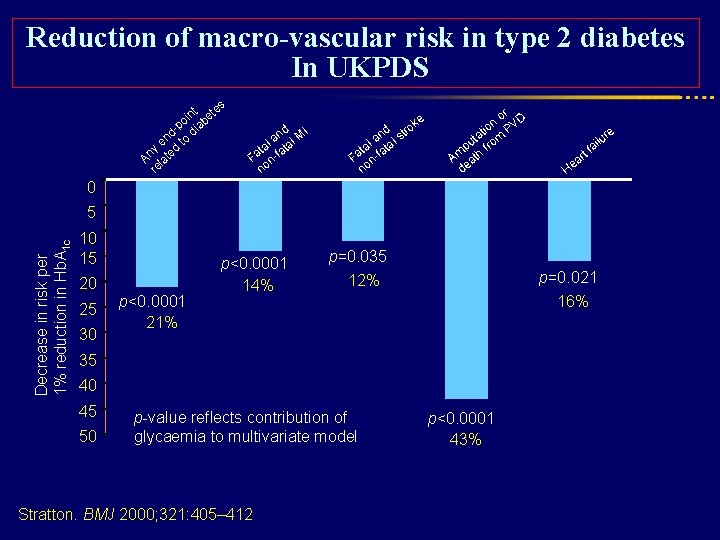
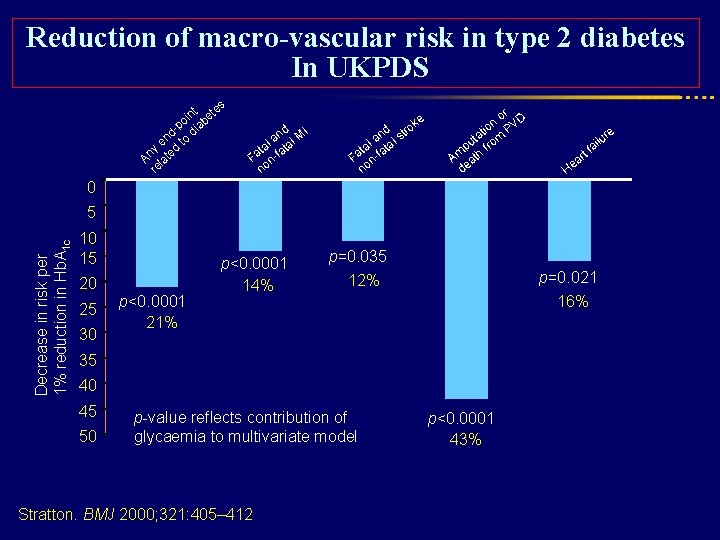
Reduction of macro-vascular risk in type 2 diabetes In UKPDS s nt ete i o b -p dia d en to y d An late re nd MI a l l ta fata a F nno ke d tro n a l s al ata t Fa n-f no r o VD n tio P ta om u p fr Am ath de rt a He 0 Decrease in risk per 1% reduction in Hb. A 1 c 5 10 15 20 25 30 p<0. 0001 21% p<0. 0001 14% p=0. 035 p=0. 021 12% 16% 35 40 45 50 p-value reflects contribution of glycaemia to multivariate model Stratton. BMJ 2000; 321: 405– 412 p<0. 0001 43% re lu i fa
Insulin treatment regimens Advanced insulin regimen -Basal : Long acting insulin -Bolus : Rapid acting insulin
Long acting analogous Glargine & Detemir • Were designed to provide a reliable, constant basal insulin concentration to control basal metabolism. • They are more predictable than conventional insulins and allow simplified insulin-replacement strategies
Rapid-acting or Prandial Insulins
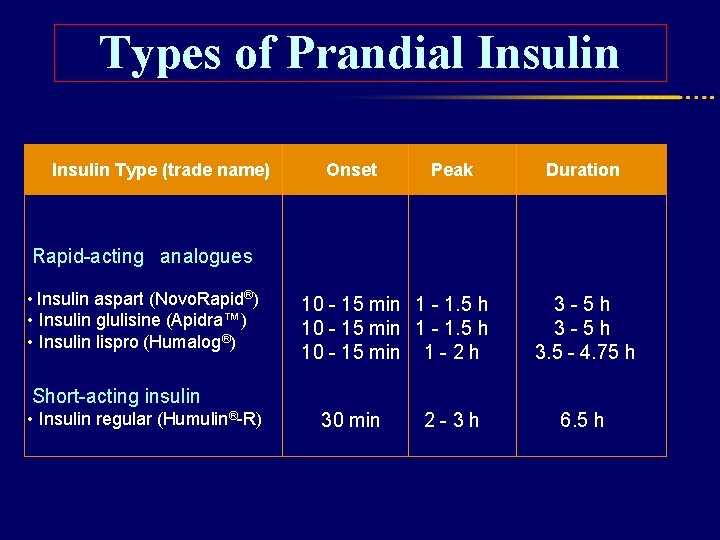
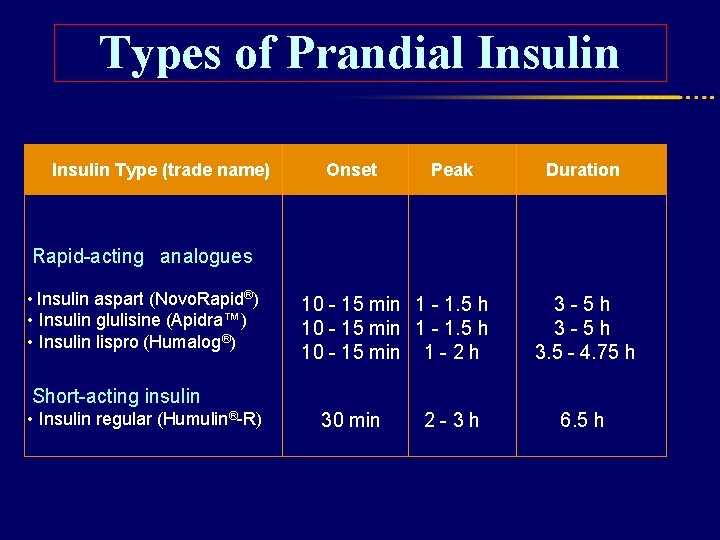
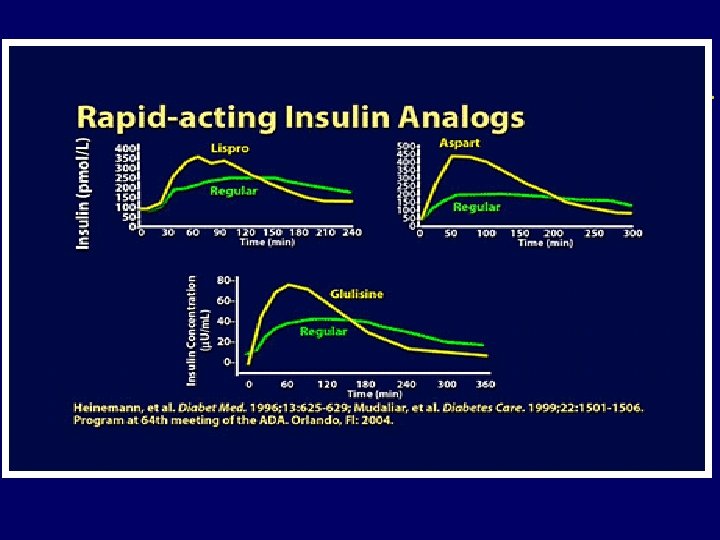
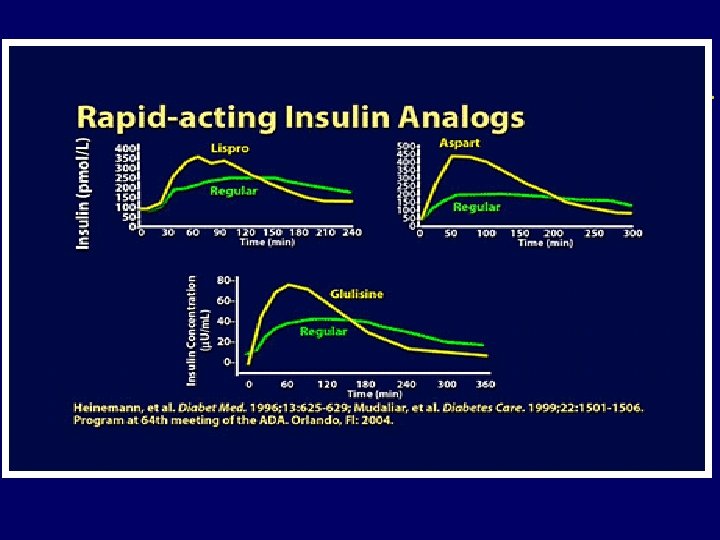
Types of Prandial Insulin Type (trade name) Onset Peak Duration Rapid-acting analogues • Insulin aspart (Novo. Rapid®) • Insulin glulisine (Apidra™) • Insulin lispro (Humalog®) 10 - 15 min 1 - 1. 5 h 10 - 15 min 1 - 2 h 3 - 5 h 3. 5 - 4. 75 h Short-acting insulin • Insulin regular (Humulin®-R) 30 min 2 - 3 h 6. 5 h
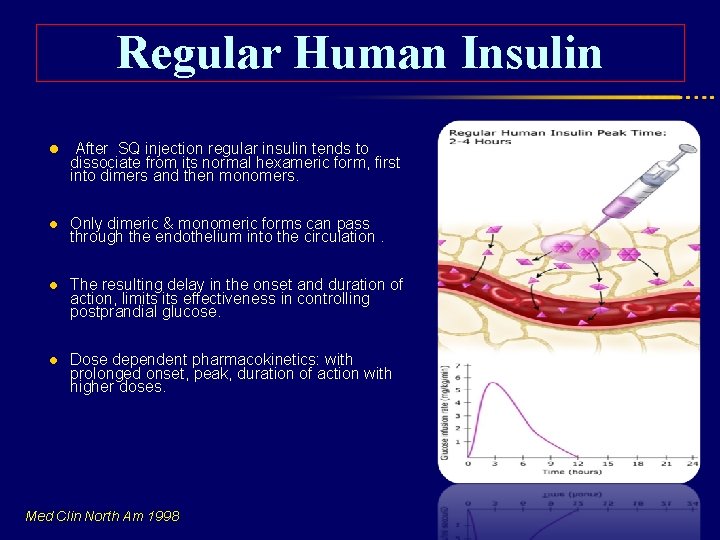
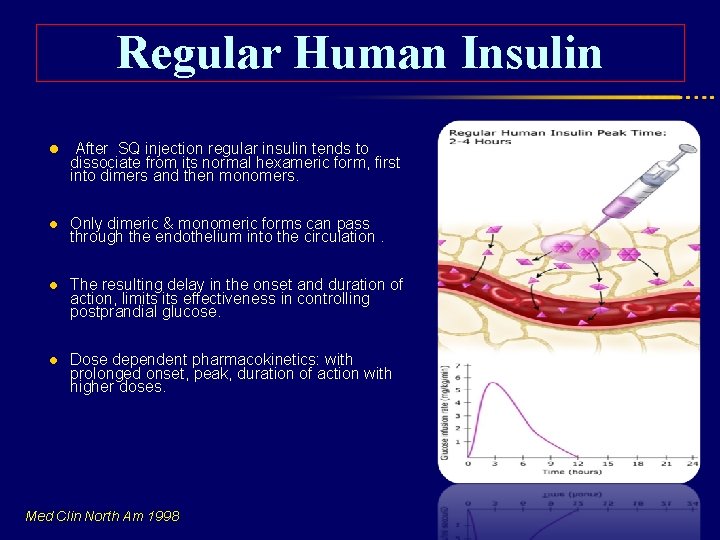
Regular Human Insulin l After SQ injection regular insulin tends to l Only dimeric & monomeric forms can pass through the endothelium into the circulation. l The resulting delay in the onset and duration of action, limits effectiveness in controlling postprandial glucose. l Dose dependent pharmacokinetics: with prolonged onset, peak, duration of action with higher doses. dissociate from its normal hexameric form, first into dimers and then monomers. Med Clin North Am 1998
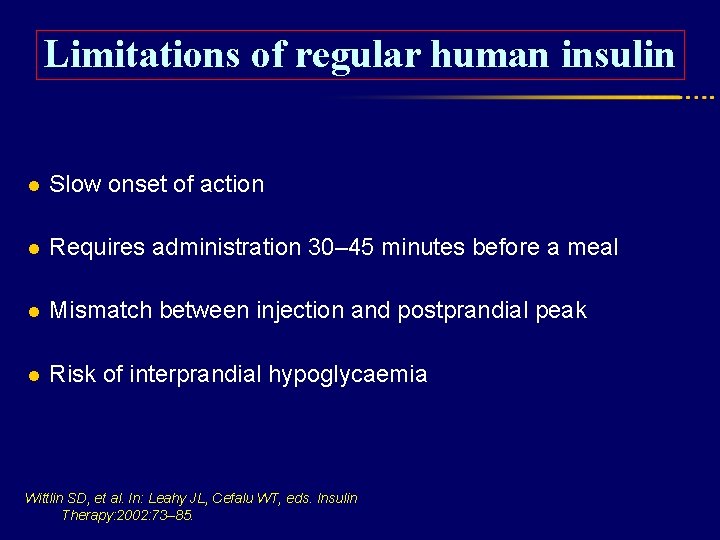
Limitations of regular human insulin l Slow onset of action l Requires administration 30– 45 minutes before a meal l Mismatch between injection and postprandial peak l Risk of interprandial hypoglycaemia Wittlin SD, et al. In: Leahy JL, Cefalu WT, eds. Insulin Therapy: 2002: 73– 85.
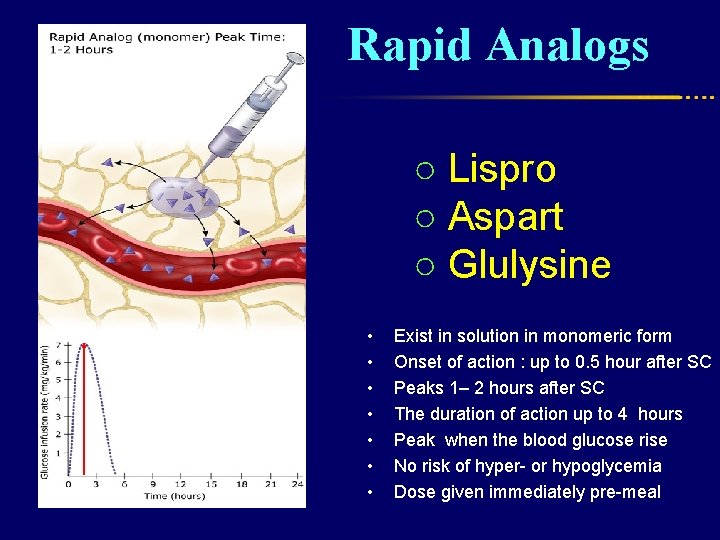
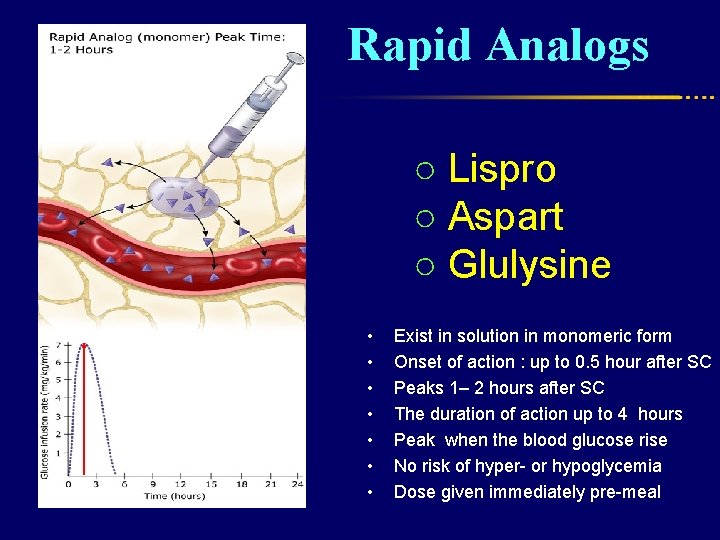
Rapid Analogs ○ Lispro ○ Aspart ○ Glulysine • • Exist in solution in monomeric form Onset of action : up to 0. 5 hour after SC Peaks 1– 2 hours after SC The duration of action up to 4 hours Peak when the blood glucose rise No risk of hyper- or hypoglycemia Dose given immediately pre-meal
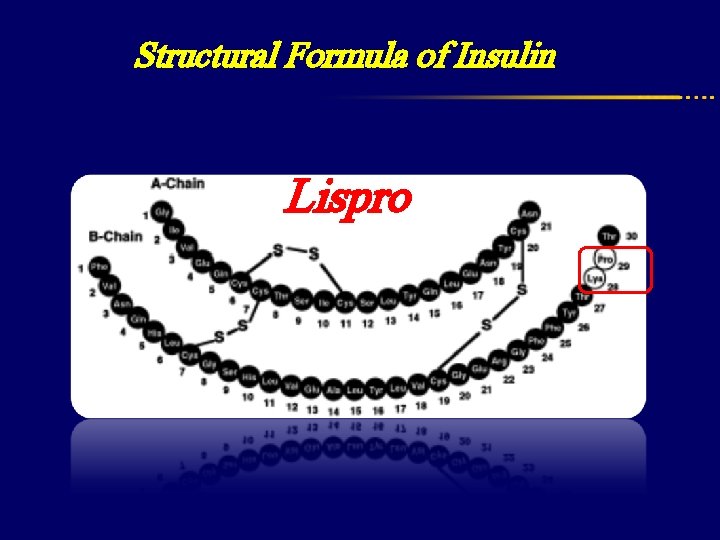
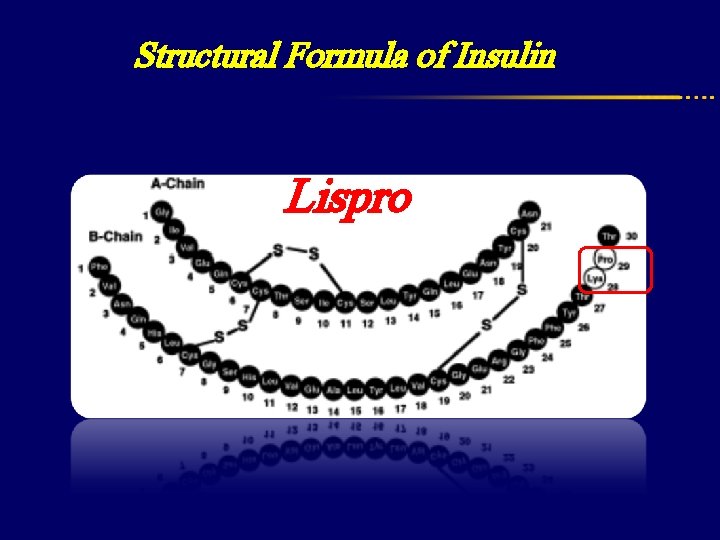
Structural Formula of Insulin Lispro
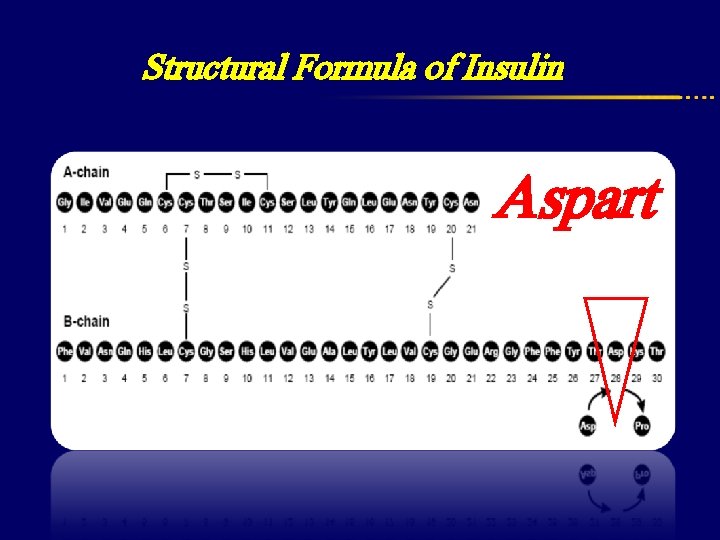
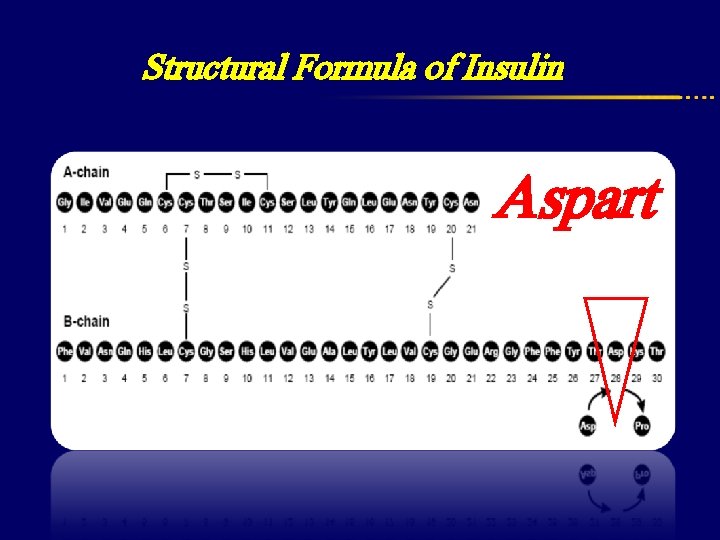
Structural Formula of Insulin Aspart
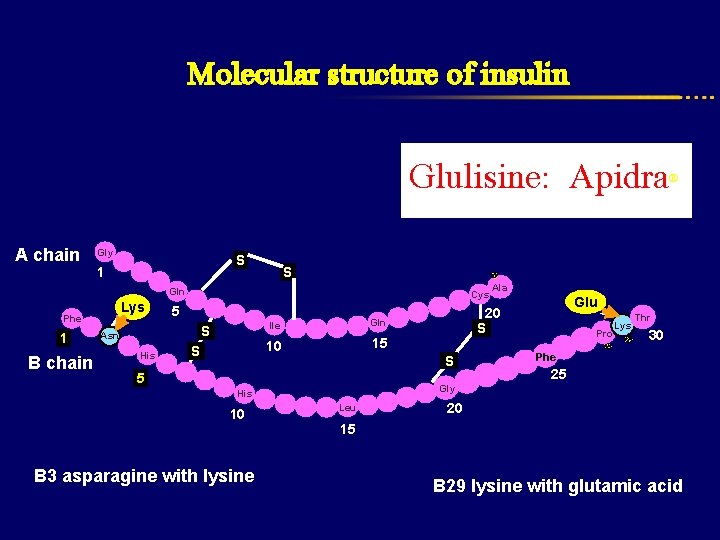
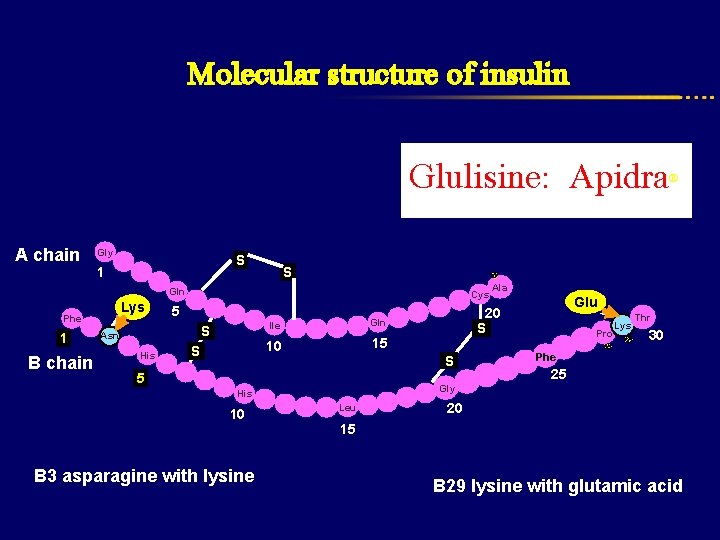
Molecular structure of insulin Glulisine: Apidra A chain Gly S 1 S Gln Lys Phe 1 B chain Cys 5 S Asn His S Ile Gln 10 15 Glu Pro Lys Thr 30 Phe 25 Gly His B 3 asparagine with lysine Ala 20 S S 5 10 ® Leu 20 15 B 29 lysine with glutamic acid
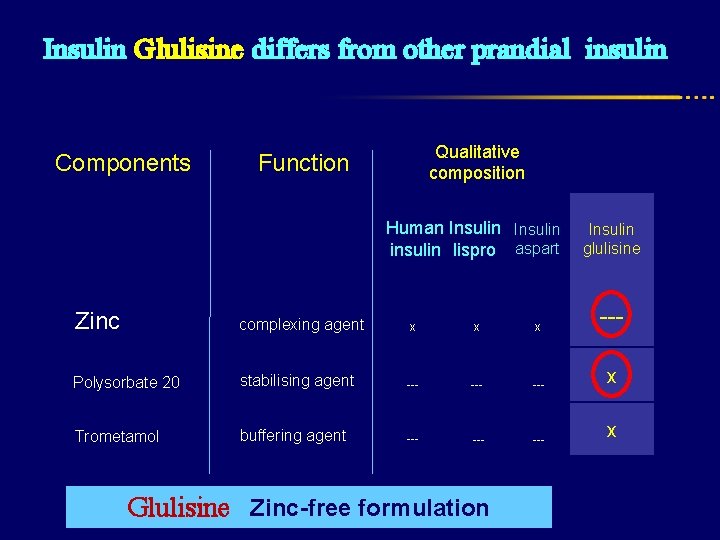
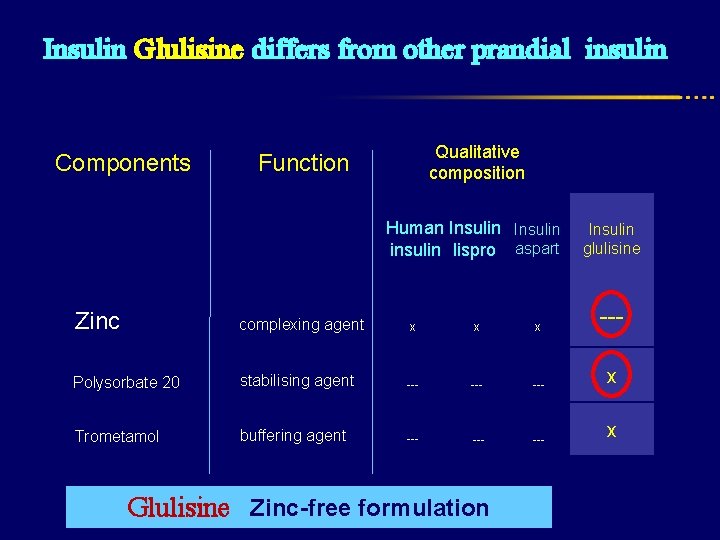
Insulin Glulisine differs from other prandial insulin Components Qualitative composition Function Human Insulin insulin lispro aspart glulisine Zinc complexing agent x x x --- Polysorbate 20 stabilising agent --- --- x Trometamol buffering agent --- --- x Glulisine Zinc-free formulation
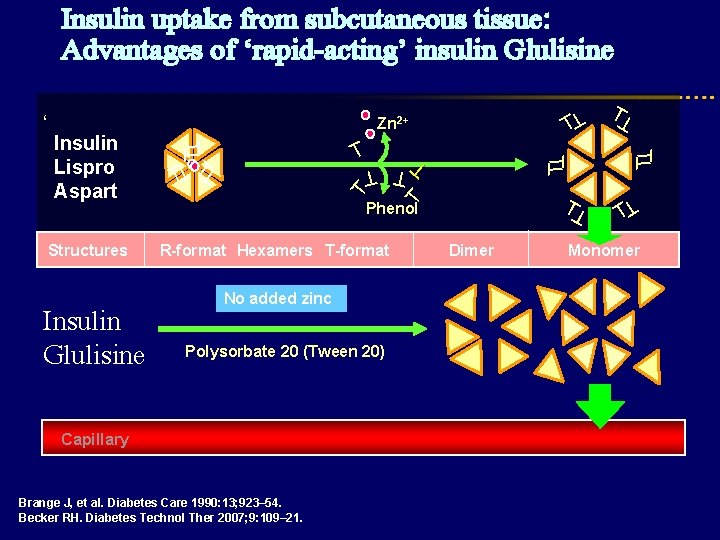
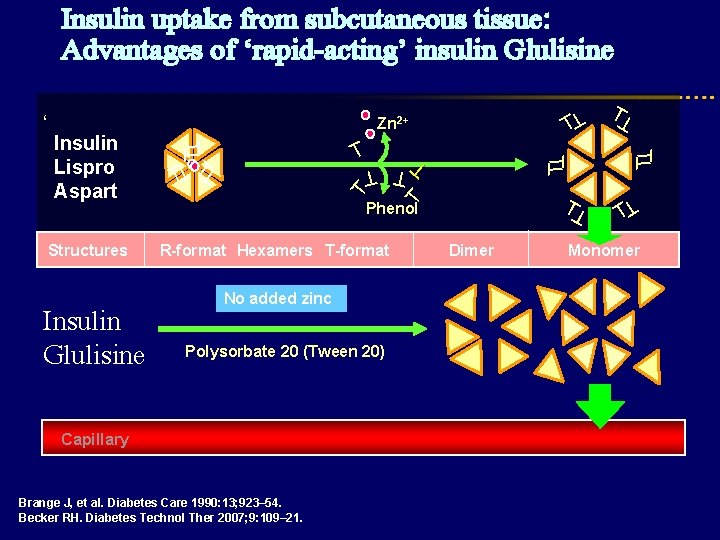
Insulin uptake from subcutaneous tissue: Advantages of ‘rapid-acting’ insulin Glulisine T T T Polysorbate 20 (Tween 20) Capillary Brange J, et al. Diabetes Care 1990: 13; 923– 54. Becker RH. Diabetes Technol Ther 2007; 9: 109– 21. T T T T No added zinc Dimer T T Phenol R-format Hexamers T-format T Insulin Glulisine T T T Structures T T Insulin Lispro Aspart T T Zn 2+ T ‘ T Monomer
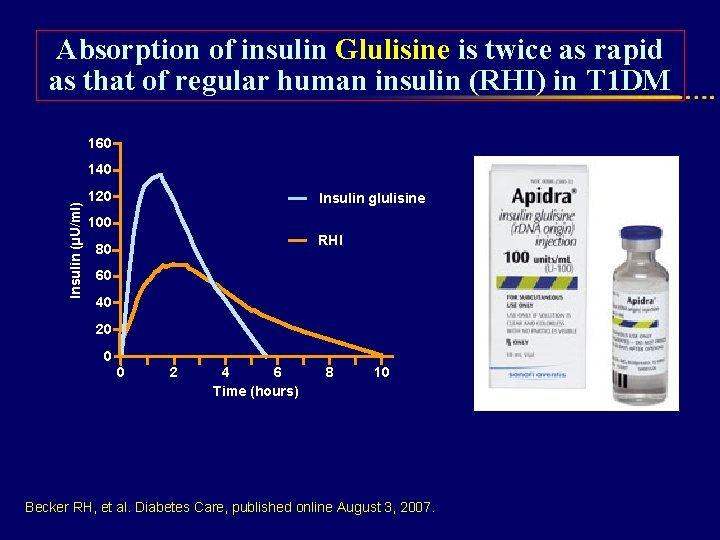
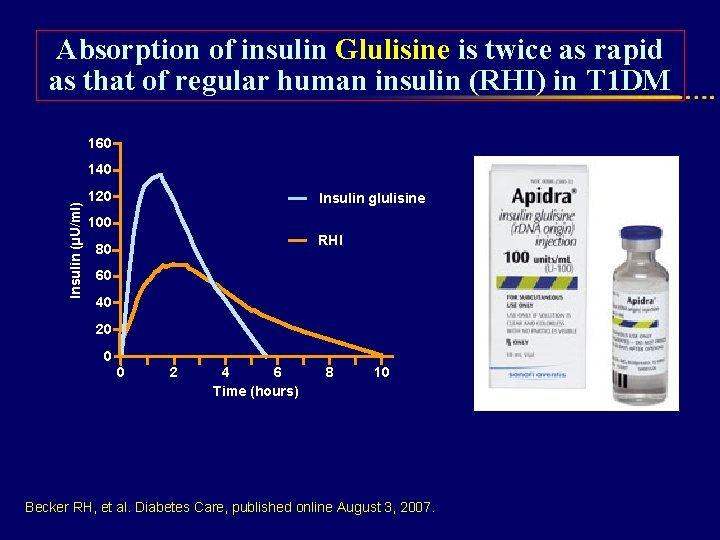
Absorption of insulin Glulisine is twice as rapid as that of regular human insulin (RHI) in T 1 DM 160 Insulin (µU/ml) 140 120 Insulin glulisine 100 RHI 80 60 40 20 0 0 2 4 6 Time (hours) 8 10 Becker RH, et al. Diabetes Care, published online August 3, 2007.
Efficacy of Prandial Insulin Analogues vs. Regular Insulin
Conclusion: Poland ; 2010 Analyses based on a systematic review showed that: ●Treatment with insulin Aspart in T 1 DM patients resulted in moderately better metabolic control and treatment satisfaction than Reg. insulin. ●In T 2 DM Patients, meta-analyses showed improvement in PPG, but not in any other outcomes.
Include 68 RCT for rapid acting analogues up to April 2007
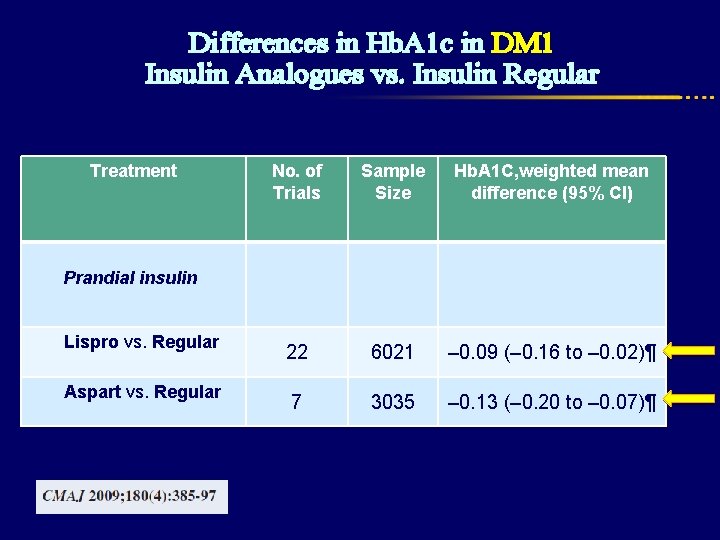
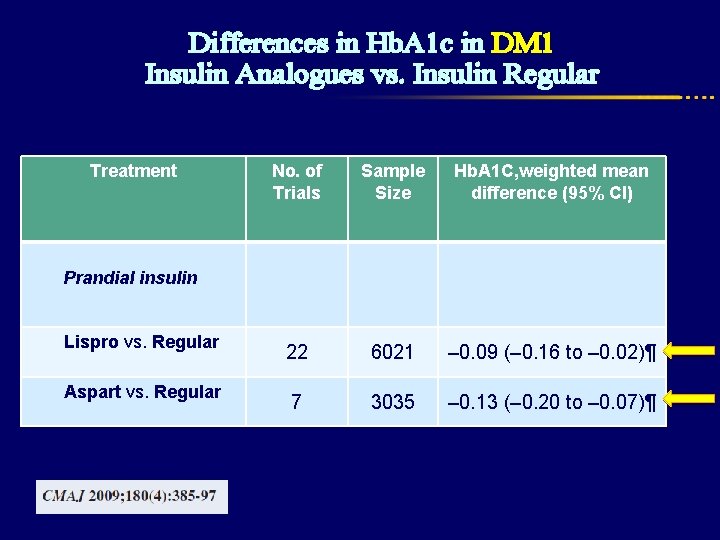
Differences in Hb. A 1 c in DM 1 Insulin Analogues vs. Insulin Regular Treatment No. of Trials Sample Size Hb. A 1 C, weighted mean difference (95% CI) 22 6021 – 0. 09 (– 0. 16 to – 0. 02)¶ 7 3035 – 0. 13 (– 0. 20 to – 0. 07)¶ Prandial insulin Lispro vs. Regular Aspart vs. Regular
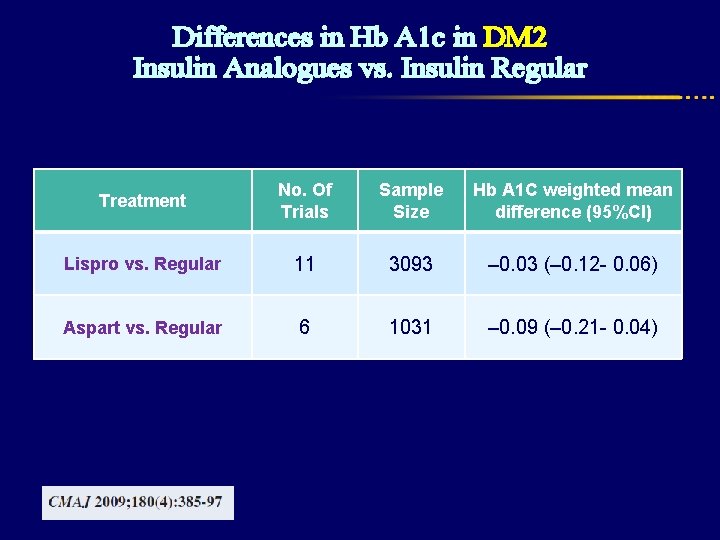
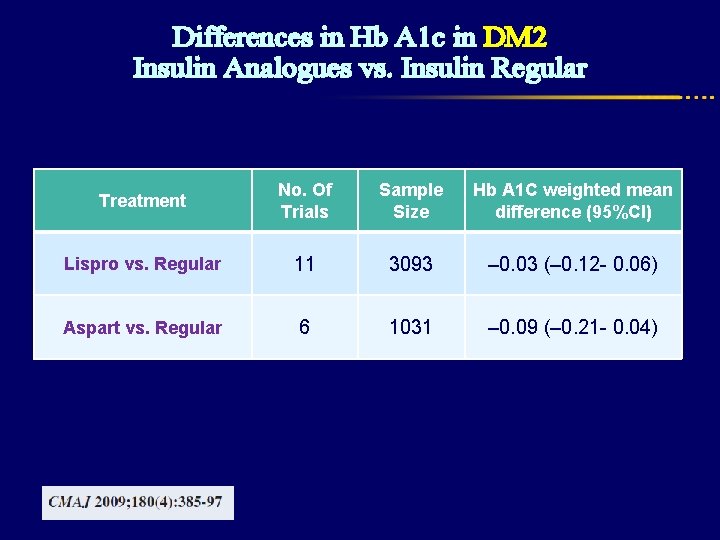
Differences in Hb A 1 c in DM 2 Insulin Analogues vs. Insulin Regular Treatment No. Of Trials Sample Size Hb A 1 C weighted mean difference (95%CI) Lispro vs. Regular 11 3093 – 0. 03 (– 0. 12 - 0. 06) Aspart vs. Regular 6 1031 – 0. 09 (– 0. 21 - 0. 04)
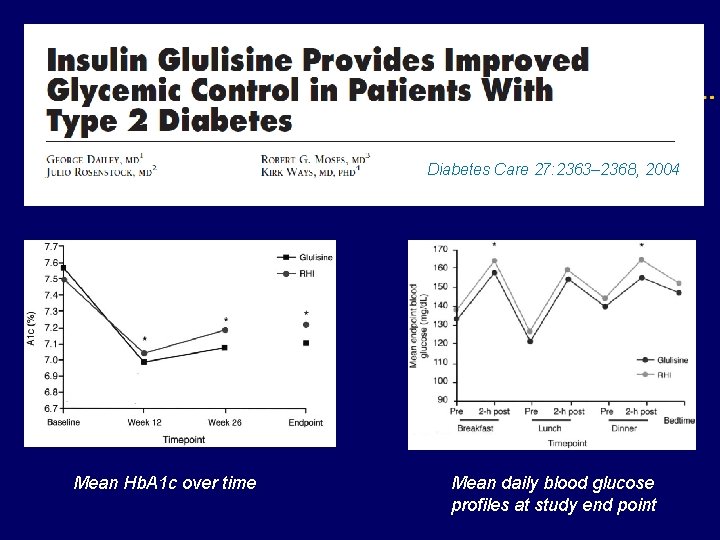
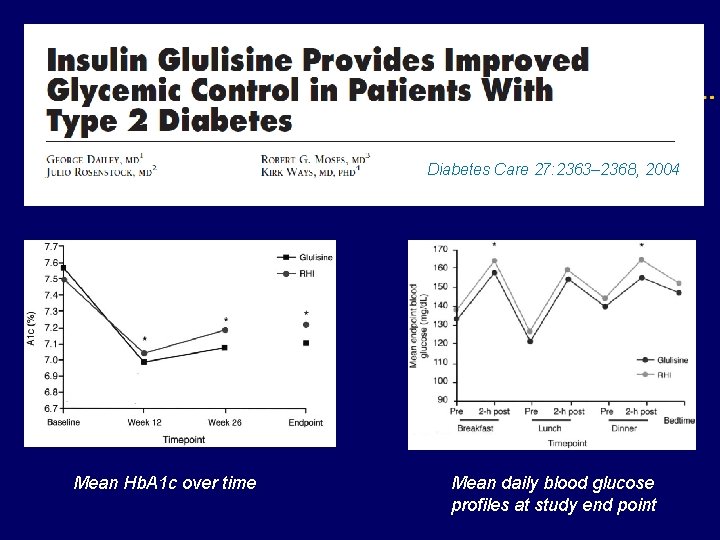
Diabetes Care 27: 2363– 2368, 2004 Mean Hb. A 1 c over time Mean daily blood glucose profiles at study end point
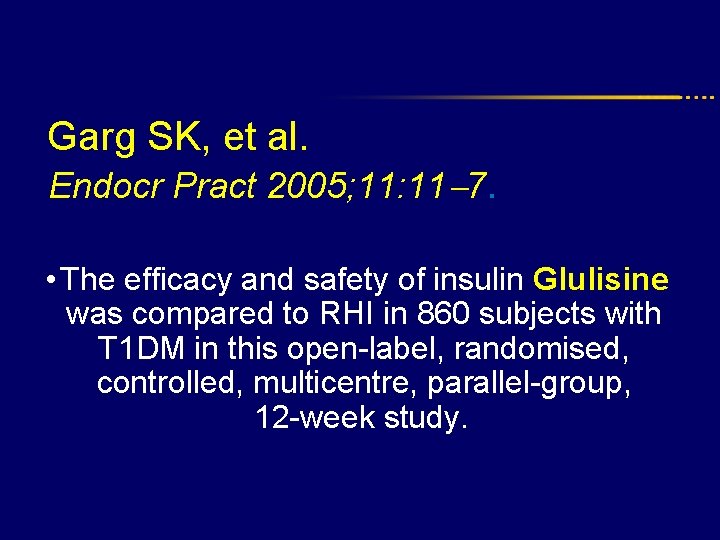
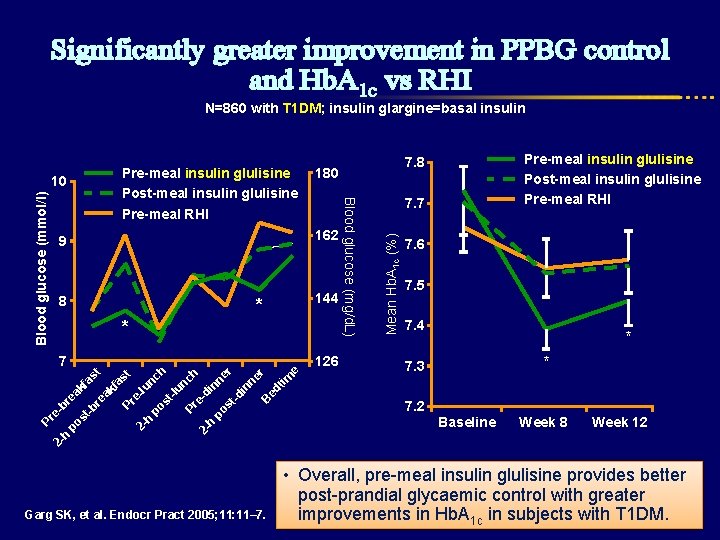
Garg SK, et al. Endocr Pract 2005; 11: 11 7. • The efficacy and safety of insulin Glulisine was compared to RHI in 860 subjects with T 1 DM in this open-label, randomised, controlled, multicentre, parallel-group, 12 -week study.
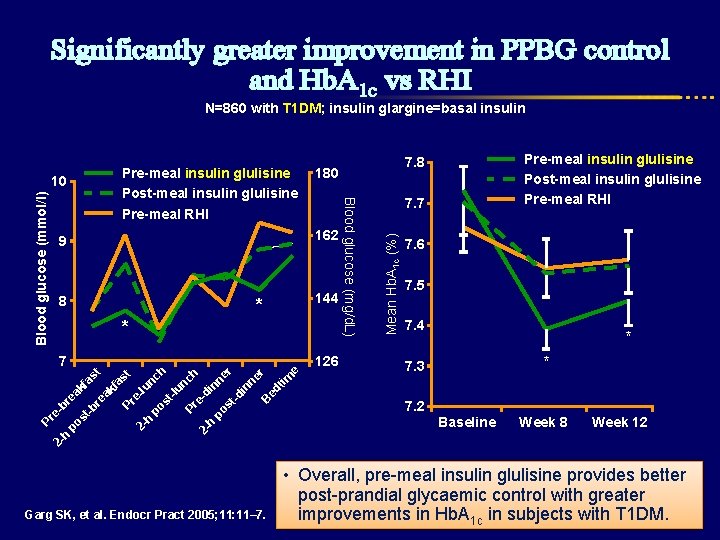
Significantly greater improvement in PPBG control and Hb. A 1 c vs RHI N=860 with T 1 DM; insulin glargine=basal insulin 180 9 162 8 144 * * 7 Pr e 2 b h po rea kf st as -b t re ak fa st Pr e 2 -lu h nc po h st -lu nc Pr h e 2 -d h in po ne st r -d in ne r B ed tim e 126 Garg SK, et al. Endocr Pract 2005; 11: 11– 7. 7 Mean Hb. A 1 c (%) Pre-meal insulin glulisine Post-meal insulin glulisine Pre-meal RHI Blood glucose (mg/d. L) Blood glucose (mmol/l) 10 Pre-meal insulin glulisine Post-meal insulin glulisine Pre-meal RHI 7. 8 7. 6 7. 5 7. 4 * * 7. 3 7. 2 Baseline Week 8 Week 12 • Overall, pre-meal insulin glulisine provides better post-prandial glycaemic control with greater improvements in Hb. A 1 c in subjects with T 1 DM.
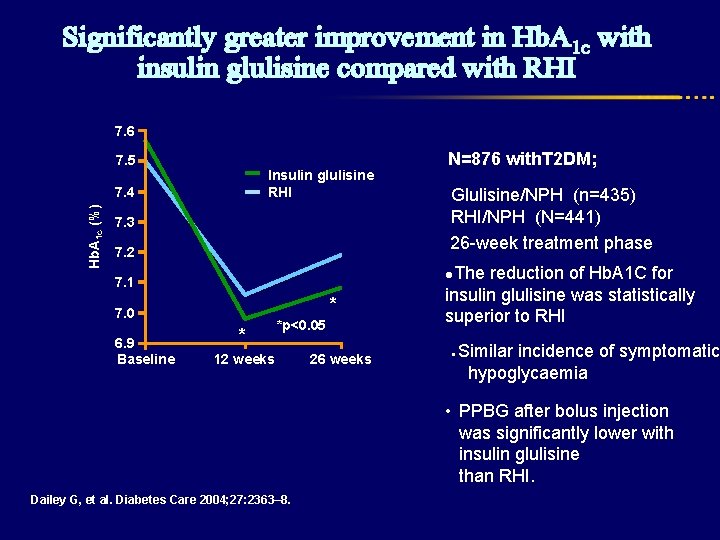
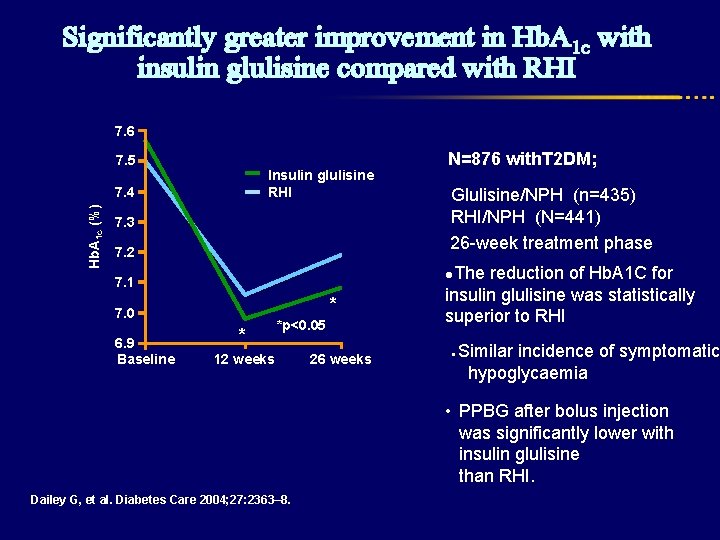
Significantly greater improvement in Hb. A 1 c with insulin glulisine compared with RHI 7. 6 7. 5 Insulin glulisine RHI Hb. A 1 c (%) 7. 4 N=876 with. T 2 DM; 7. 2 Glulisine/NPH (n=435) RHI/NPH (N=441) 26 -week treatment phase 7. 1 ●The reduction of Hb. A 1 C for 7. 3 * 7. 0 6. 9 Baseline * *p<0. 05 12 weeks Dailey G, et al. Diabetes Care 2004; 27: 2363– 8. 26 weeks insulin glulisine was statistically superior to RHI ● Similar incidence of symptomatic hypoglycaemia • PPBG after bolus injection was significantly lower with insulin glulisine than RHI.
Safety of Prandial Insulin Analogues vs. Regular Insulin
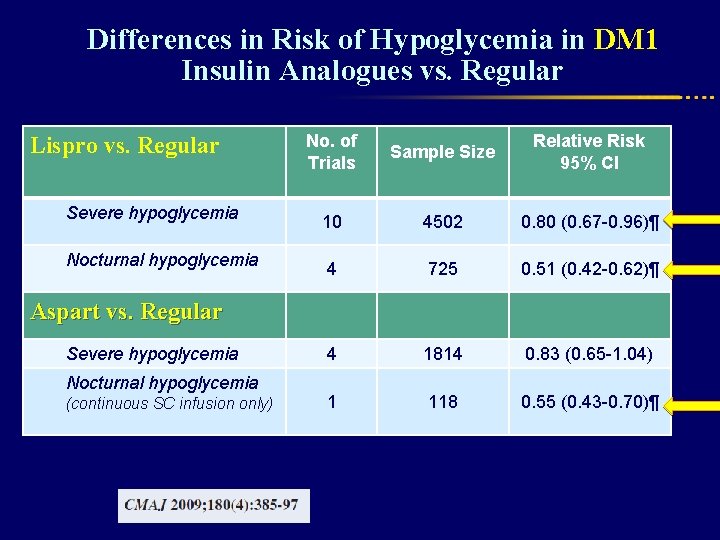
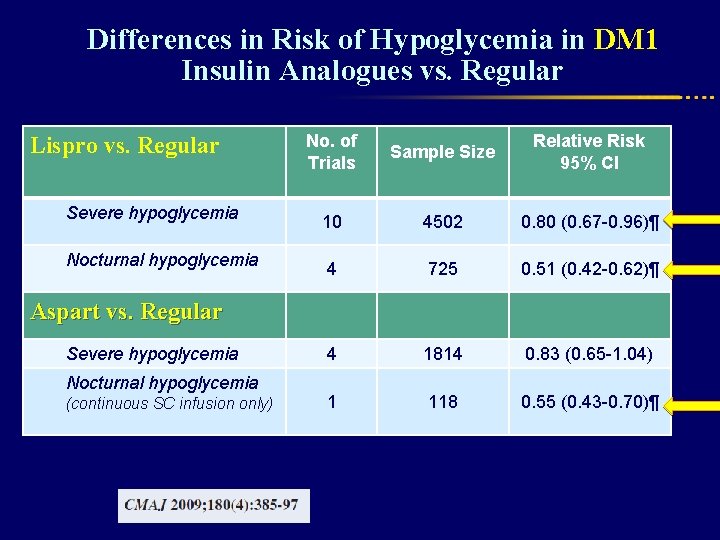
Differences in Risk of Hypoglycemia in DM 1 Insulin Analogues vs. Regular Lispro vs. Regular Severe hypoglycemia Nocturnal hypoglycemia No. of Trials Sample Size Relative Risk 95% CI 10 4502 0. 80 (0. 67 -0. 96)¶ 4 725 0. 51 (0. 42 -0. 62)¶ 4 1814 0. 83 (0. 65 -1. 04) 1 118 0. 55 (0. 43 -0. 70)¶ Aspart vs. Regular Severe hypoglycemia Nocturnal hypoglycemia (continuous SC infusion only)
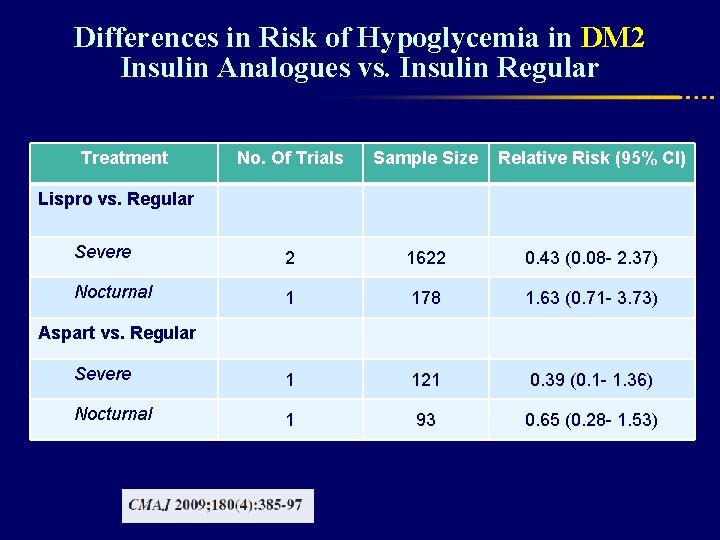
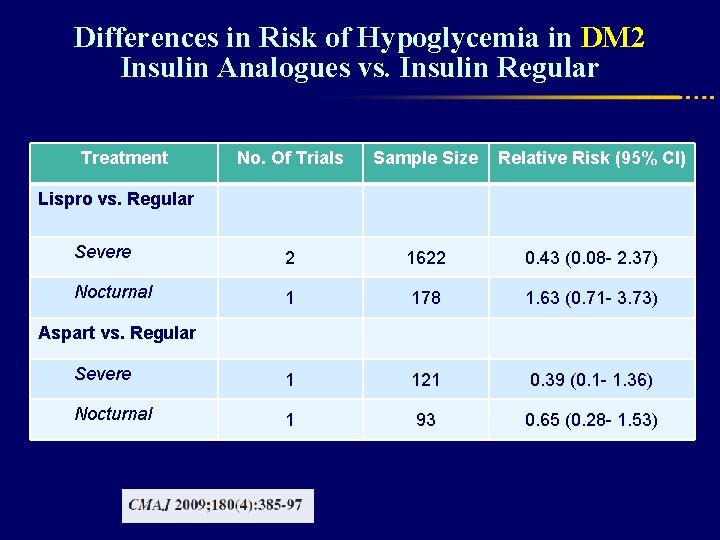
Differences in Risk of Hypoglycemia in DM 2 Insulin Analogues vs. Insulin Regular Treatment No. Of Trials Sample Size Relative Risk (95% CI) Severe 2 1622 0. 43 (0. 08 - 2. 37) Nocturnal 1 178 1. 63 (0. 71 - 3. 73) Severe 1 121 0. 39 (0. 1 - 1. 36) Nocturnal 1 93 0. 65 (0. 28 - 1. 53) Lispro vs. Regular Aspart vs. Regular
Differences in Risk of Hypoglycemia in DM 2 Insulin Analogues vs. Insulin Regular ● No statistical difference was detected between rapid-acting insulin analogues and regular human insulin with respect to the risk of severe hypoglycemia. ●The patients given insulin aspart had significantly fewer events of overall hypoglycemia than did those given regular human insulin.
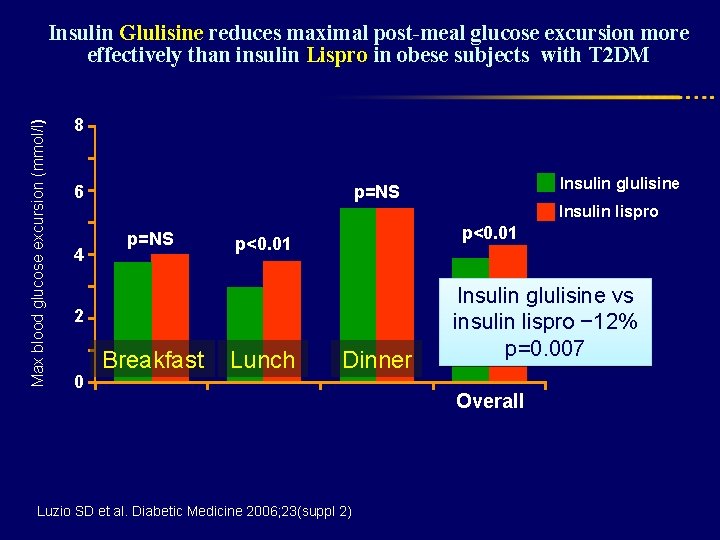
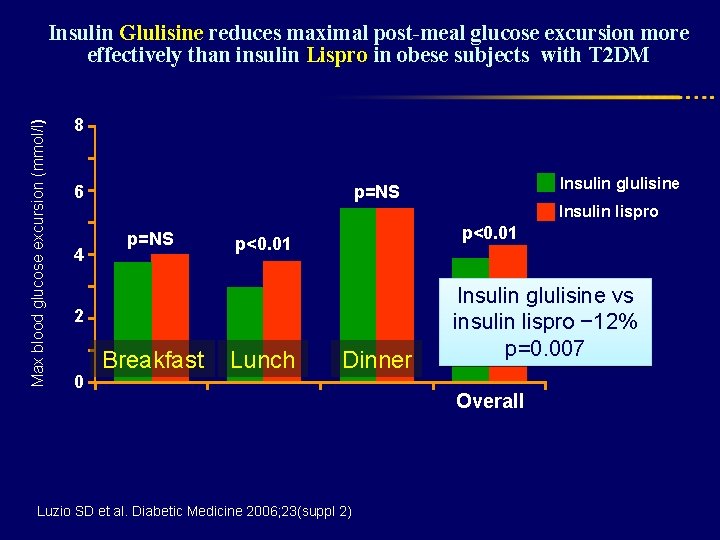
Max blood glucose excursion (mmol/l) Insulin Glulisine reduces maximal post-meal glucose excursion more effectively than insulin Lispro in obese subjects with T 2 DM 8 Insulin glulisine p=NS 6 Insulin lispro 4 p=NS p<0. 01 2 0 Breakfast Lunch Dinner Luzio SD et al. Diabetic Medicine 2006; 23(suppl 2) Insulin glulisine vs insulin lispro − 12% p=0. 007 Overall
Quality of Life with Prandial Insulin Analogues vs. Regular Insulin
Quality of Life in DM 1 l Patients generally preferred rapid-acting insulin analogues over regular insulin because of flexibility in dosing relative to mealtimes. l Some studies that assessed quality of life and patient satisfaction reported statistically significant improvements with the use of rapid –acting insulin compared with regular insulin.
Quality of Life in DM 2 Two studies comparing insulin Lispro with regular human insulin reported data on quality of life and patient satisfaction. ●They found that “worry related to diabetes” was significantly improved with insulin lispro in one of the studies ● None of the studies of insulin Aspart in type 2 diabetes reported data on quality of life or patient satisfaction.
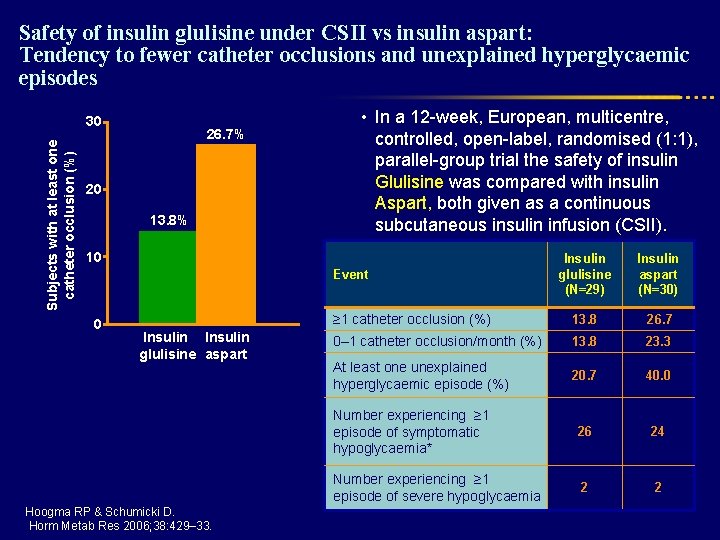
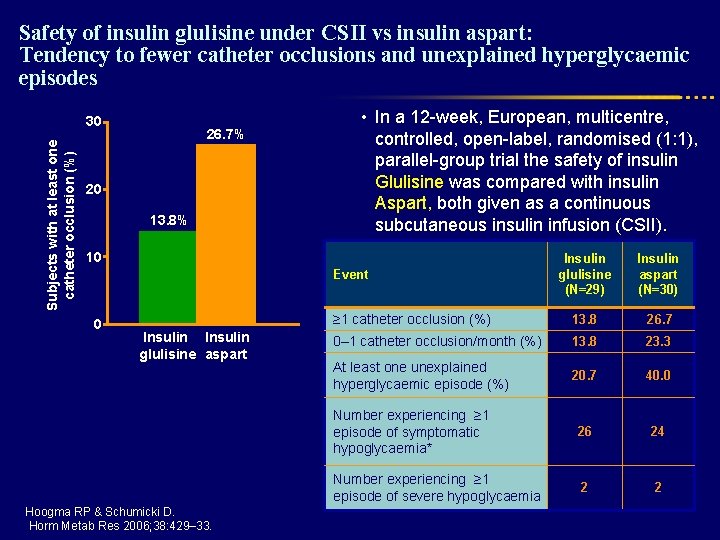
Safety of insulin glulisine under CSII vs insulin aspart: Tendency to fewer catheter occlusions and unexplained hyperglycaemic episodes Subjects with at least one catheter occlusion (%) 30 26. 7% 20 13. 8% • In a 12 -week, European, multicentre, controlled, open-label, randomised (1: 1), parallel-group trial the safety of insulin Glulisine was compared with insulin Aspart, both given as a continuous subcutaneous insulin infusion (CSII). 10 Insulin glulisine (N=29) Insulin aspart (N=30) ≥ 1 catheter occlusion (%) 13. 8 26. 7 0– 1 catheter occlusion/month (%) 13. 8 23. 3 At least one unexplained hyperglycaemic episode (%) 20. 7 40. 0 Number experiencing ≥ 1 episode of symptomatic hypoglycaemia* 26 24 Number experiencing ≥ 1 episode of severe hypoglycaemia 2 2 Event 0 Insulin glulisine aspart Hoogma RP & Schumicki D. Horm Metab Res 2006; 38: 429– 33.
Special Population
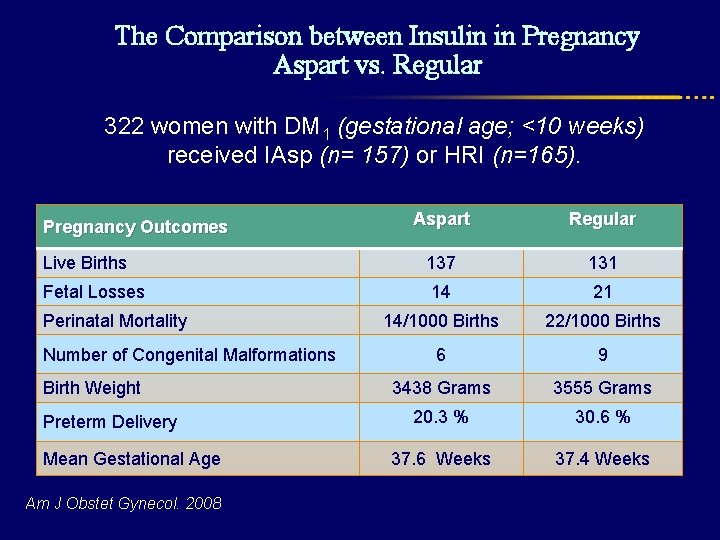
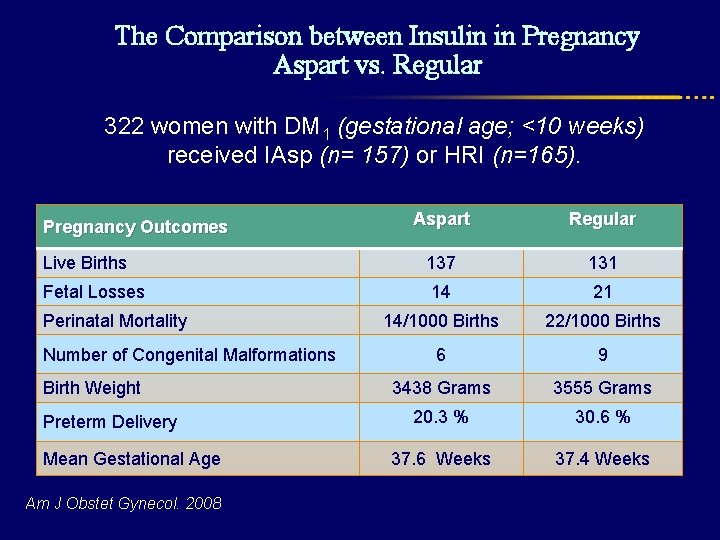
The Comparison between Insulin in Pregnancy Aspart vs. Regular 322 women with DM 1 (gestational age; <10 weeks) received IAsp (n= 157) or HRI (n=165). Aspart Regular Live Births 137 131 Fetal Losses 14 21 14/1000 Births 22/1000 Births 6 9 3438 Grams 3555 Grams 20. 3 % 30. 6 % 37. 6 Weeks 37. 4 Weeks Pregnancy Outcomes Perinatal Mortality Number of Congenital Malformations Birth Weight Preterm Delivery Mean Gestational Age Am J Obstet Gynecol. 2008
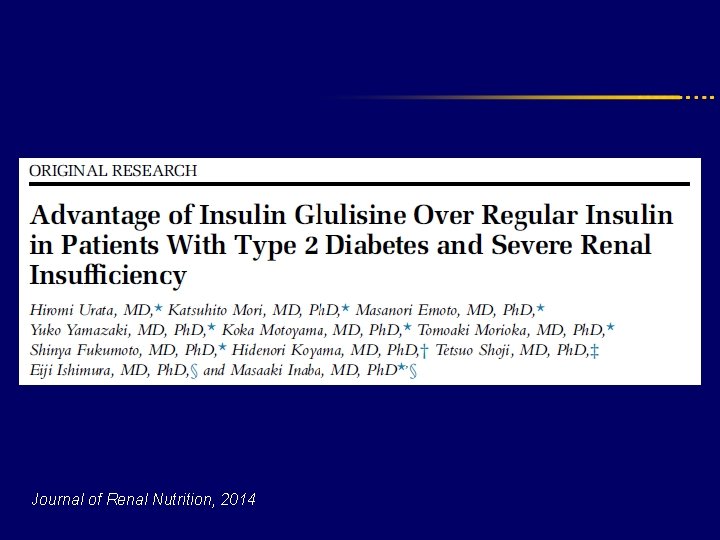
Journal of Renal Nutrition, 2014
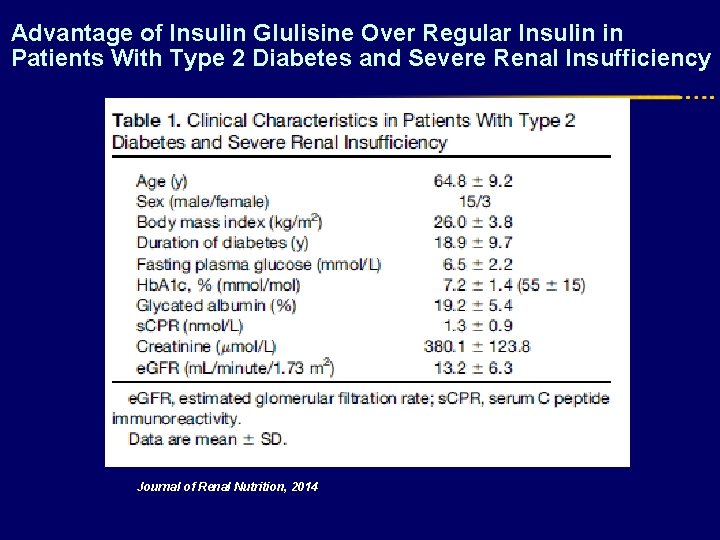
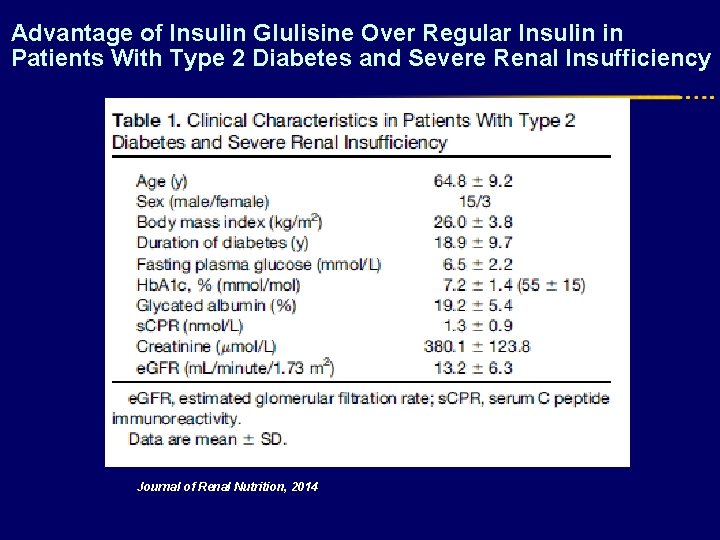
Advantage of Insulin Glulisine Over Regular Insulin in Patients With Type 2 Diabetes and Severe Renal Insufficiency Journal of Renal Nutrition, 2014
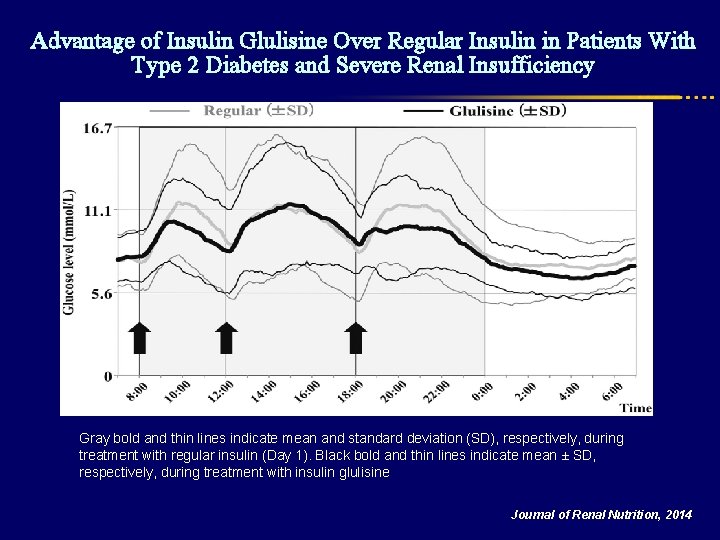
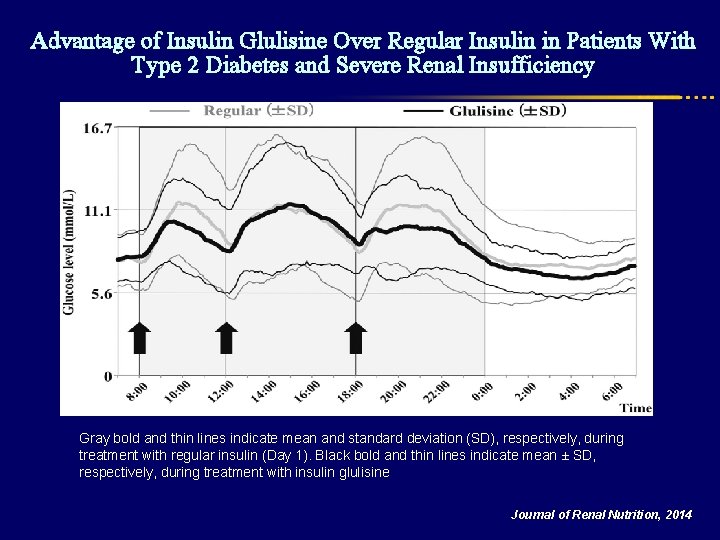
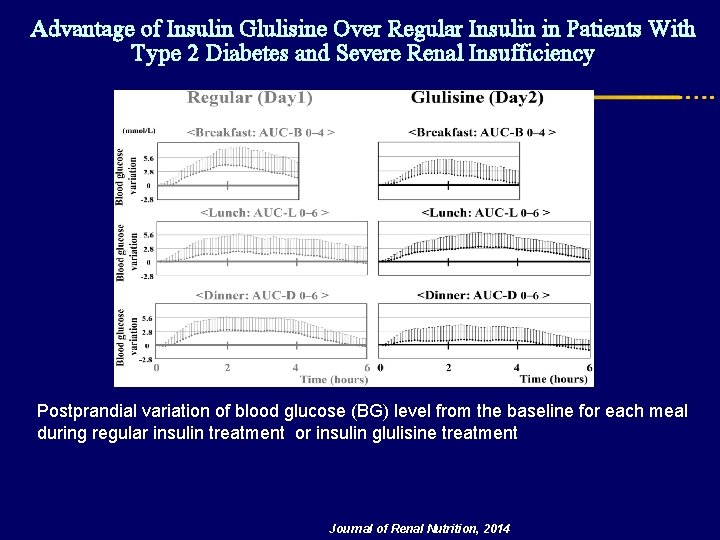
Advantage of Insulin Glulisine Over Regular Insulin in Patients With Type 2 Diabetes and Severe Renal Insufficiency Gray bold and thin lines indicate mean and standard deviation (SD), respectively, during treatment with regular insulin (Day 1). Black bold and thin lines indicate mean ± SD, respectively, during treatment with insulin glulisine Journal of Renal Nutrition, 2014
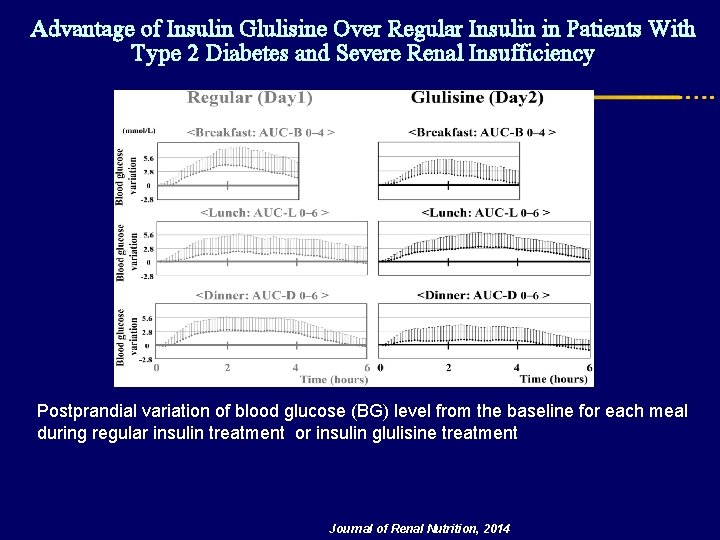
Advantage of Insulin Glulisine Over Regular Insulin in Patients With Type 2 Diabetes and Severe Renal Insufficiency Postprandial variation of blood glucose (BG) level from the baseline for each meal during regular insulin treatment or insulin glulisine treatment Journal of Renal Nutrition, 2014
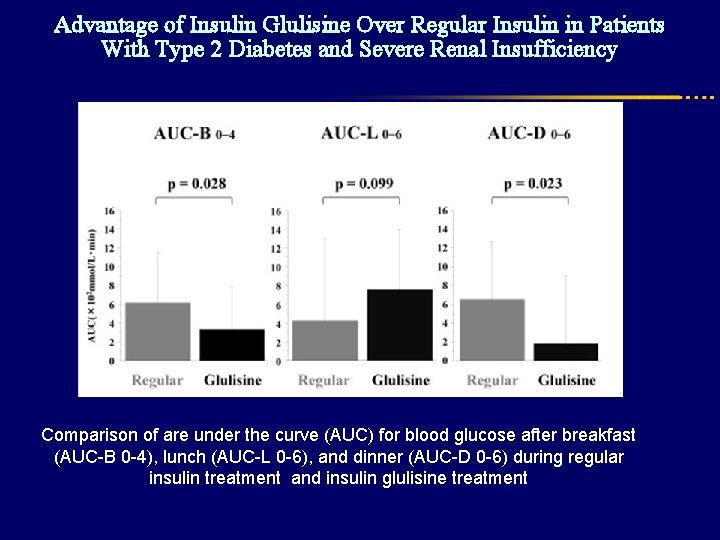
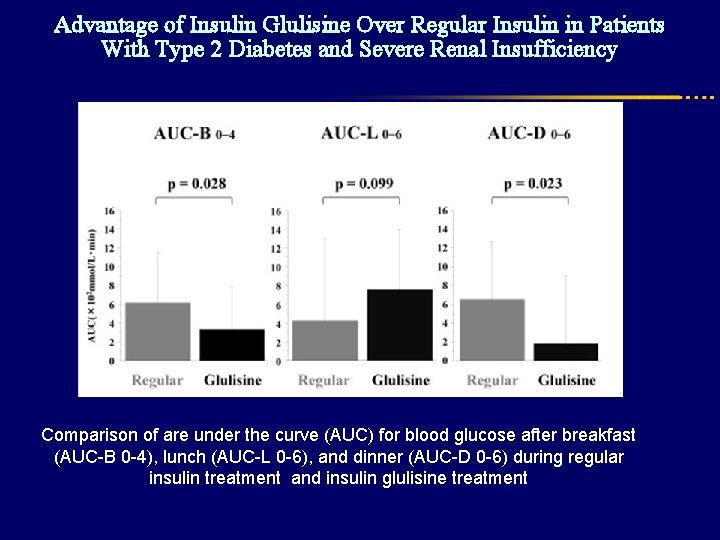
Advantage of Insulin Glulisine Over Regular Insulin in Patients With Type 2 Diabetes and Severe Renal Insufficiency Comparison of are under the curve (AUC) for blood glucose after breakfast (AUC-B 0 -4), lunch (AUC-L 0 -6), and dinner (AUC-D 0 -6) during regular insulin treatment and insulin glulisine treatment
Advantage of Insulin Glulisine Over Regular Insulin in Patients With Type 2 Diabetes and Severe Renal Insufficiency Conclusions Insulin glulisine effectively suppressed postprandial hyperglycemia, whereas regular insulin caused a prolonged hypoglycemic action These findings support the effectiveness and safety of insulin glulisine in patients with type 2 diabetes and severe renal insufficiency
Urakami T, et al. J Diabetes Investig. 2015 Jan; 6(1): 87– 90.
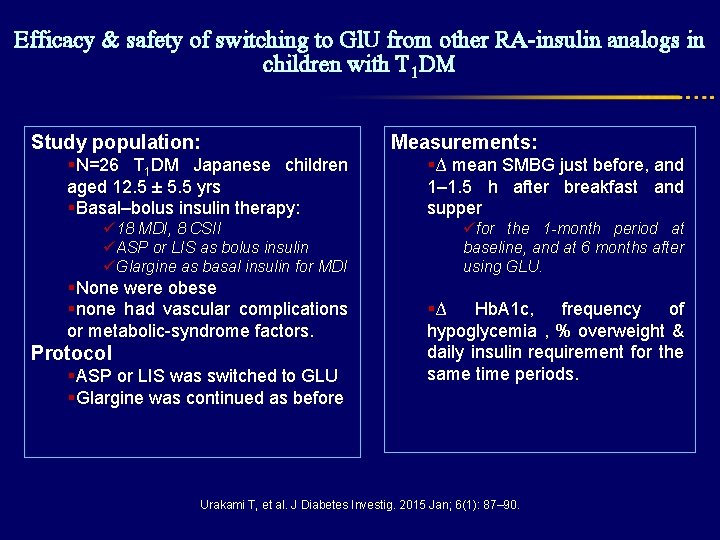
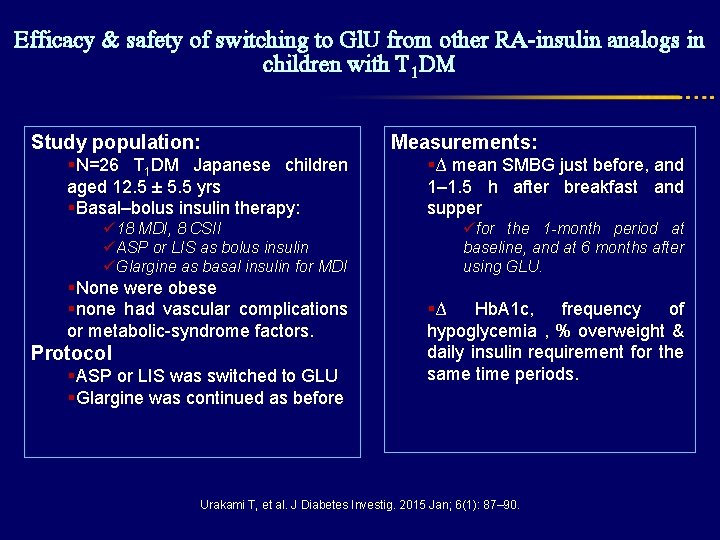
Efficacy & safety of switching to Gl. U from other RA-insulin analogs in children with T 1 DM Study population: §N=26 T 1 DM Japanese children aged 12. 5 ± 5. 5 yrs §Basal–bolus insulin therapy: ü 18 MDI, 8 CSII üASP or LIS as bolus insulin üGlargine as basal insulin for MDI §None were obese §none had vascular complications or metabolic-syndrome factors. Protocol §ASP or LIS was switched to GLU §Glargine was continued as before Measurements: §∆ mean SMBG just before, and 1– 1. 5 h after breakfast and supper üfor the 1 -month period at baseline, and at 6 months after using GLU. §∆ Hb. A 1 c, frequency of hypoglycemia , % overweight & daily insulin requirement for the same time periods. Urakami T, et al. J Diabetes Investig. 2015 Jan; 6(1): 87– 90.
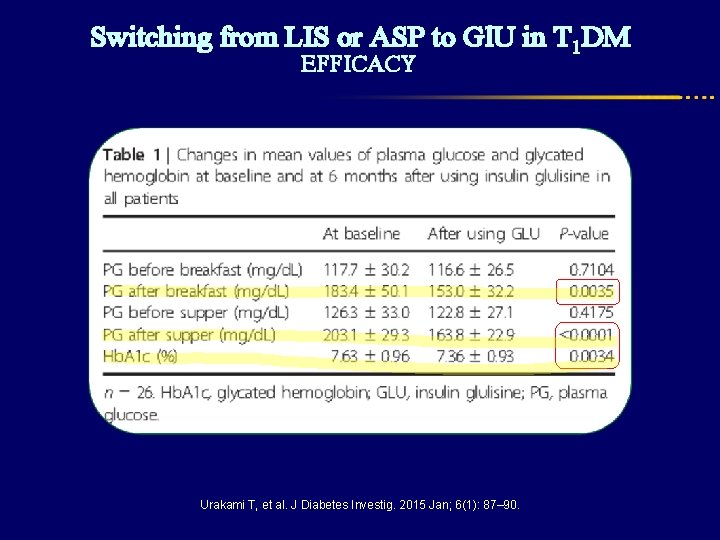
Switching from LIS or ASP to Gl. U in T 1 DM EFFICACY Urakami T, et al. J Diabetes Investig. 2015 Jan; 6(1): 87– 90.
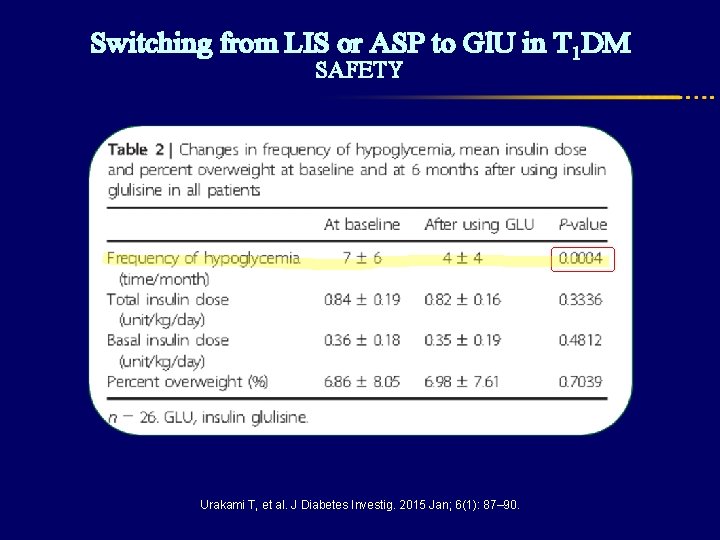
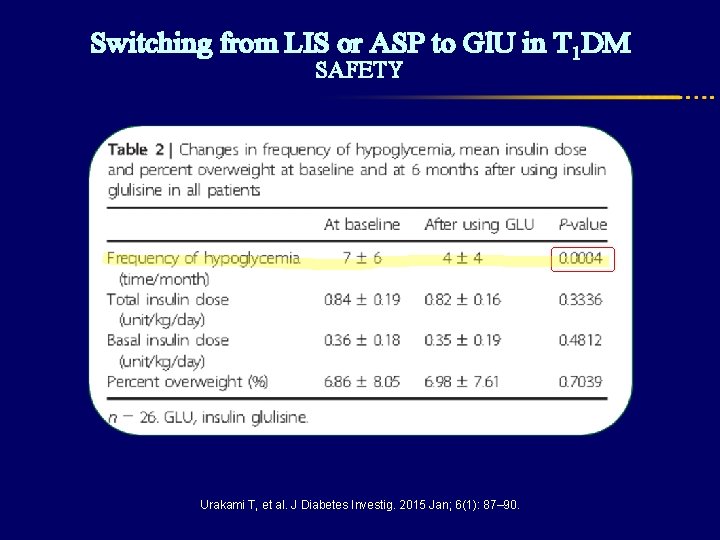
Switching from LIS or ASP to Gl. U in T 1 DM SAFETY Urakami T, et al. J Diabetes Investig. 2015 Jan; 6(1): 87– 90.
Summary Rapid-acting insulin in DM 1 l Reduces Hb. A 1 c l Reduces rate of hypoglycemia specially nocturnal type l Improves quality of life Rapid-acting insulin in DM 2 l Comparable efficacy (Hb. A 1 C) with RHI l Reduces overall hypoglycemia l “worry related to diabetes” was significantly improved Special population l May cause lower fetal losses & preterm delivery l May improve glycemic control with a decreased risk of hypoglycemia in patients with severe renal insufficiency.

Initiation and Titration
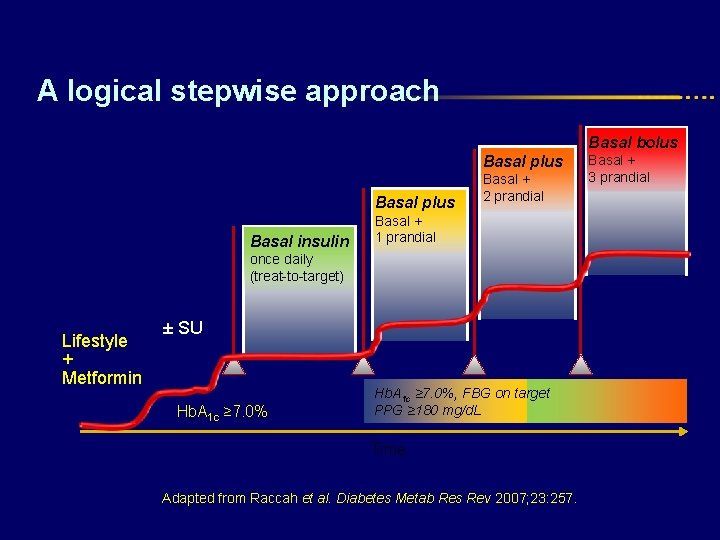
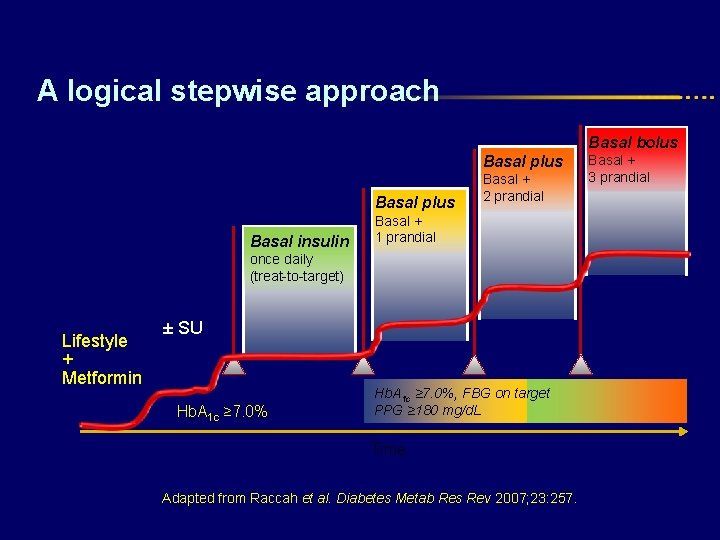
A logical stepwise approach Basal bolus Basal plus Basal insulin Basal + 2 prandial Basal + 1 prandial once daily (treat-to-target) Lifestyle + Metformin ± SU Hb. A 1 c ≥ 7. 0%, FBG on target PPG ≥ 180 mg/d. L Time Adapted from Raccah et al. Diabetes Metab Res Rev 2007; 23: 257. Basal + 3 prandial
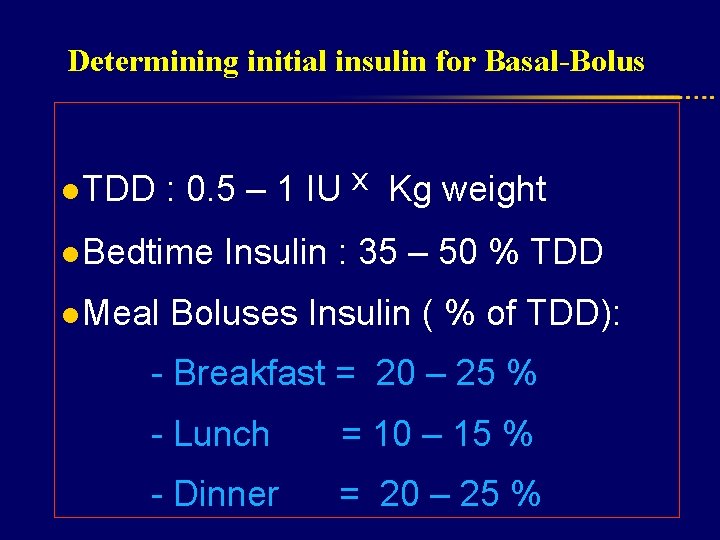
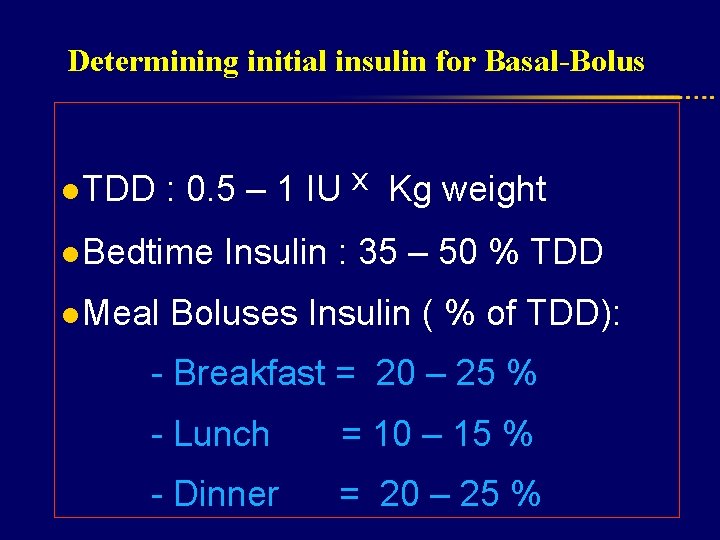
Determining initial insulin for Basal-Bolus l TDD : 0. 5 – 1 IU ˣ Kg weight l Bedtime Insulin : 35 – 50 % TDD l Meal Boluses Insulin ( % of TDD): - Breakfast = 20 – 25 % - Lunch = 10 – 15 % - Dinner = 20 – 25 %
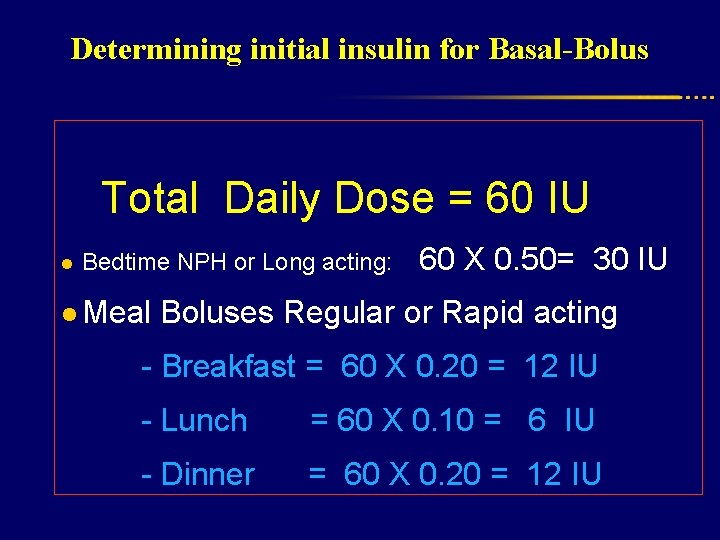
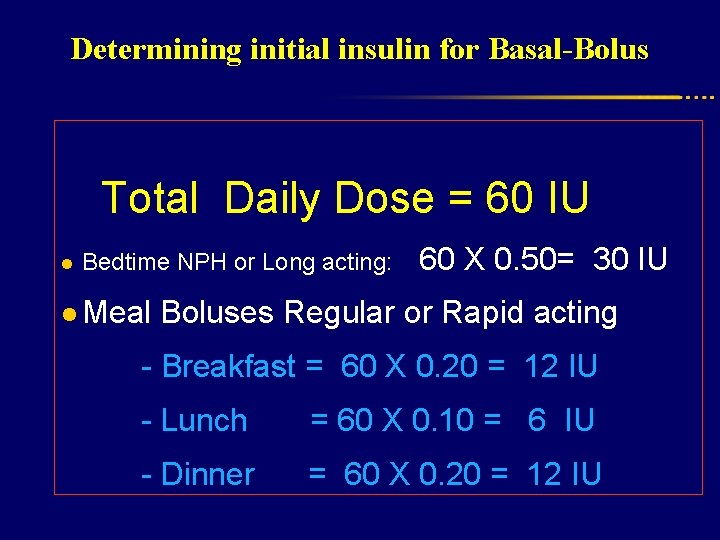
Determining initial insulin for Basal-Bolus l Total Daily Dose = 60 IU Bedtime NPH or Long acting: 60 X 0. 50= 30 IU l Meal Boluses Regular or Rapid acting - Breakfast = 60 X 0. 20 = 12 IU - Lunch = 60 X 0. 10 = 6 IU - Dinner = 60 X 0. 20 = 12 IU
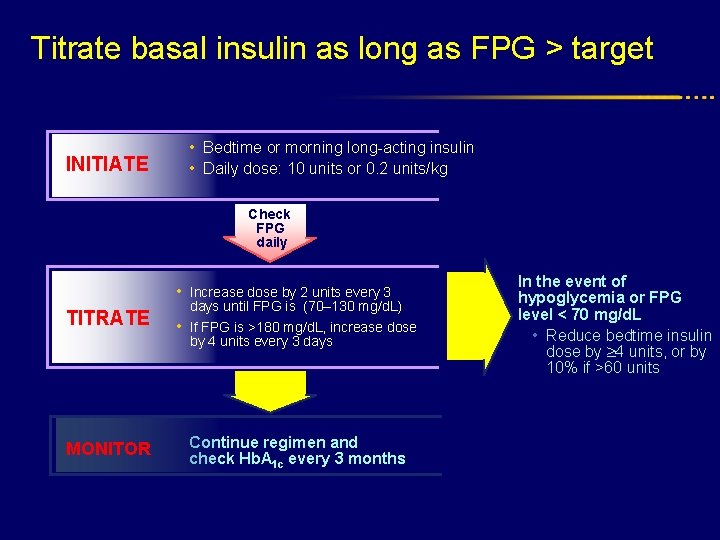
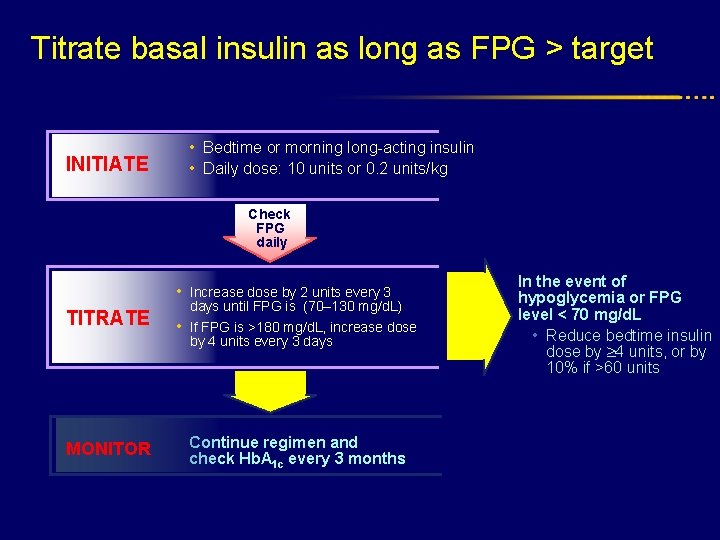
Titrate basal insulin as long as FPG > target INITIATE • Bedtime or morning long-acting insulin • Daily dose: 10 units or 0. 2 units/kg Check FPG daily • Increase dose by 2 units every 3 TITRATE days until FPG is (70– 130 mg/d. L) • If FPG is >180 mg/d. L, increase dose by 4 units every 3 days MONITOR Continue regimen and check Hb. A 1 c every 3 months In the event of hypoglycemia or FPG level < 70 mg/d. L • Reduce bedtime insulin dose by 4 units, or by 10% if >60 units
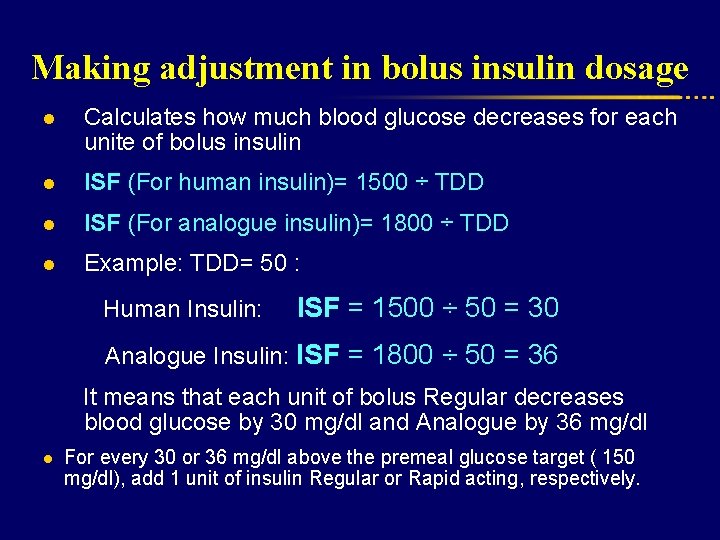
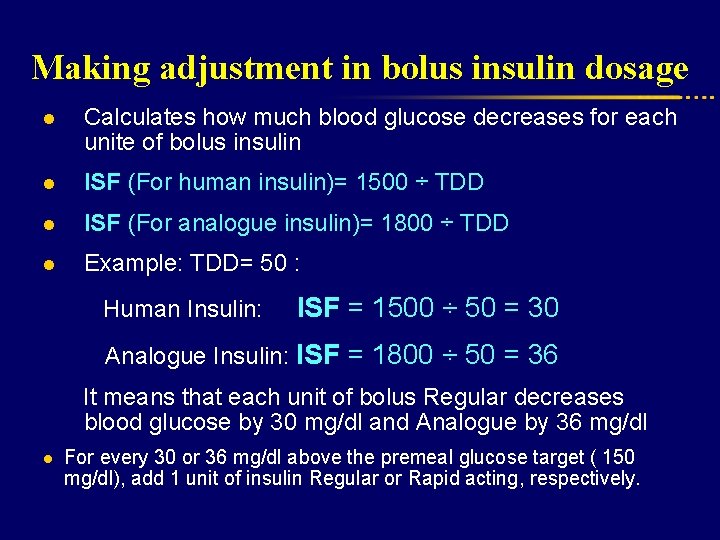
Making adjustment in bolus insulin dosage l Calculates how much blood glucose decreases for each unite of bolus insulin l ISF (For human insulin)= 1500 ÷ TDD l ISF (For analogue insulin)= 1800 ÷ TDD l Example: TDD= 50 : Human Insulin: ISF = 1500 ÷ 50 = 30 Analogue Insulin: ISF = 1800 ÷ 50 = 36 It means that each unit of bolus Regular decreases blood glucose by 30 mg/dl and Analogue by 36 mg/dl l For every 30 or 36 mg/dl above the premeal glucose target ( 150 mg/dl), add 1 unit of insulin Regular or Rapid acting, respectively.
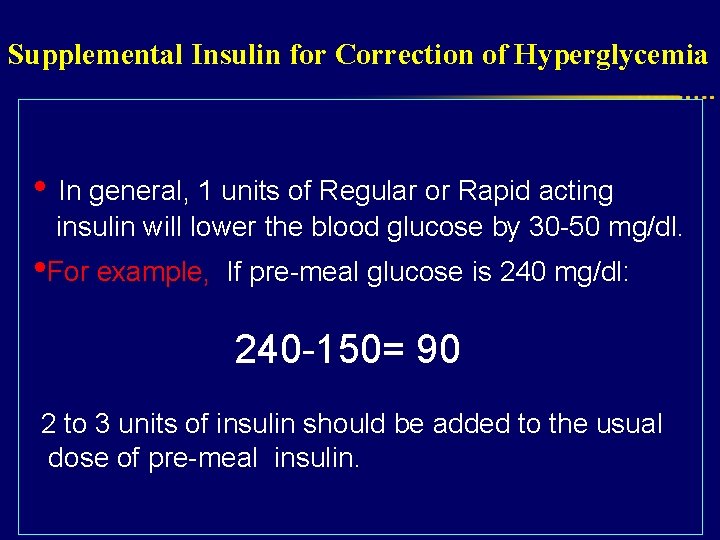
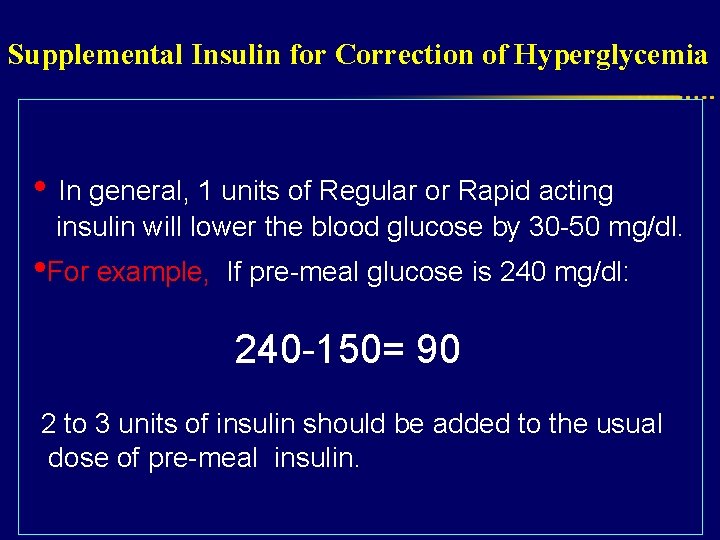
Supplemental Insulin for Correction of Hyperglycemia • In general, 1 units of Regular or Rapid acting insulin will lower the blood glucose by 30 -50 mg/dl. • For example, If pre-meal glucose is 240 mg/dl: 240 -150= 90 2 to 3 units of insulin should be added to the usual dose of pre-meal insulin.
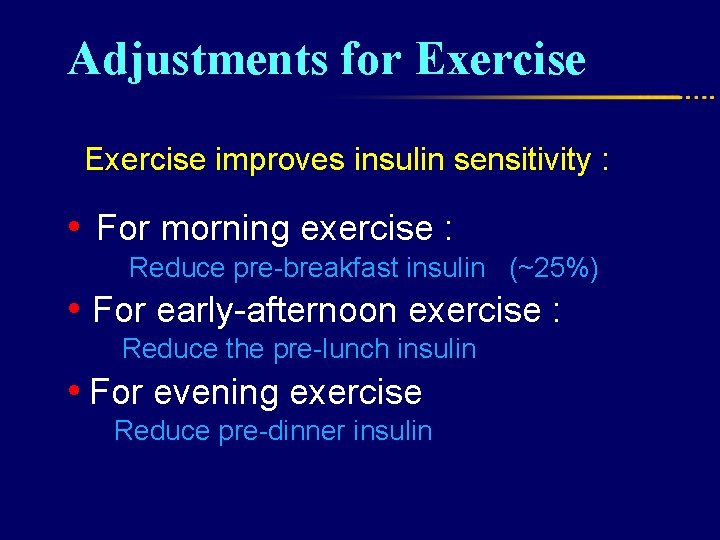
Adjustments for Exercise improves insulin sensitivity : • For morning exercise : Reduce pre-breakfast insulin (~25%) • For early-afternoon exercise : Reduce the pre-lunch insulin • For evening exercise Reduce pre-dinner insulin
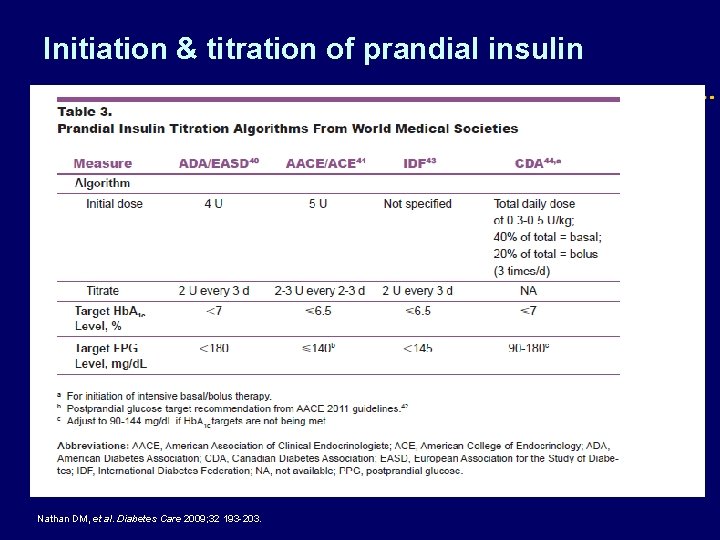
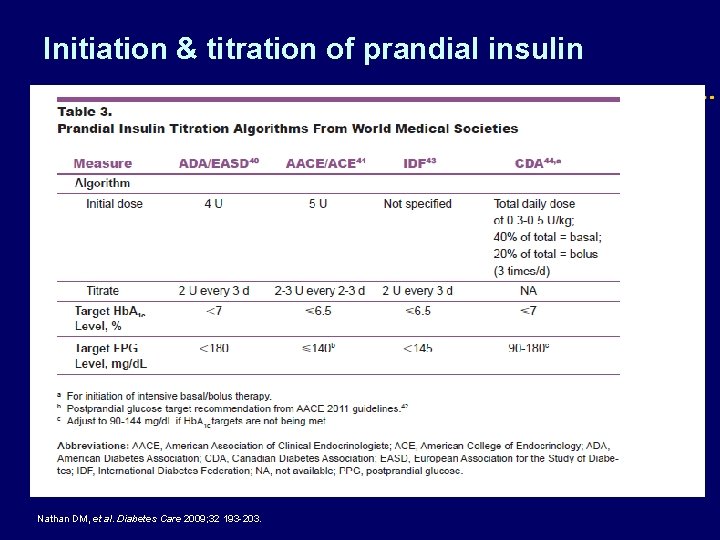
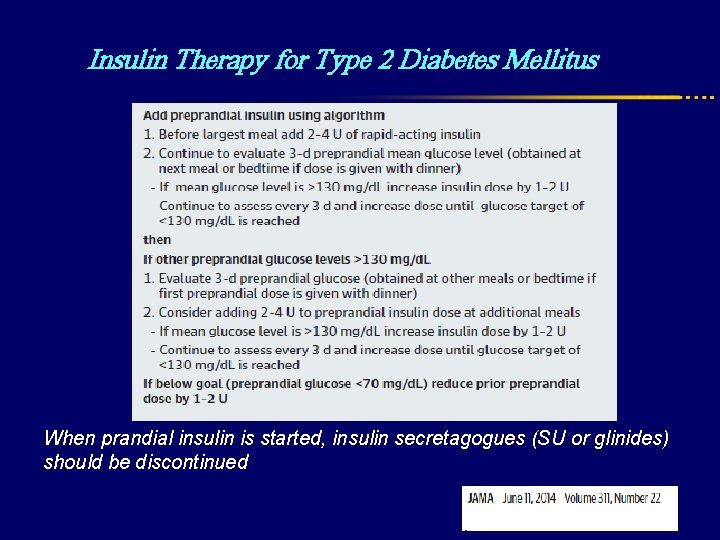
Initiation & titration of prandial insulin PPG Nathan DM, et al. Diabetes Care 2009; 32 193 -203.
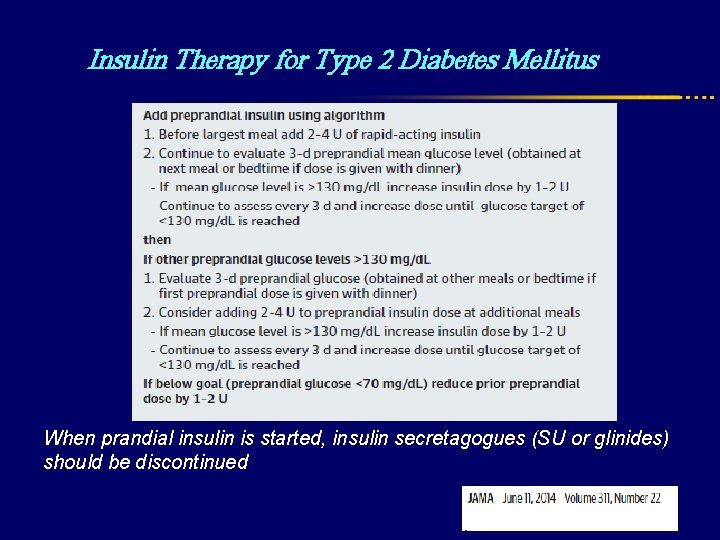
Insulin Therapy for Type 2 Diabetes Mellitus When prandial insulin is started, insulin secretagogues (SU or glinides) should be discontinued
Conclusion Insulin treatment has always been as much an art as a science. ●The proper use of insulin analogues allows people with diabetes greater flexibility in the timing of meals, snacks, and exercise, which in turn enhances their ability to lead normal lives. ●When choosing between insulin analogues and RHI, not only should their differences in glycaemic control and treatment flexibility be considered, but also their cost of treatment, type of diet and patients’ preferences.