Rapamycin Analogs EVEROLIMUS SIROLIMUS O H H N













- Slides: 41

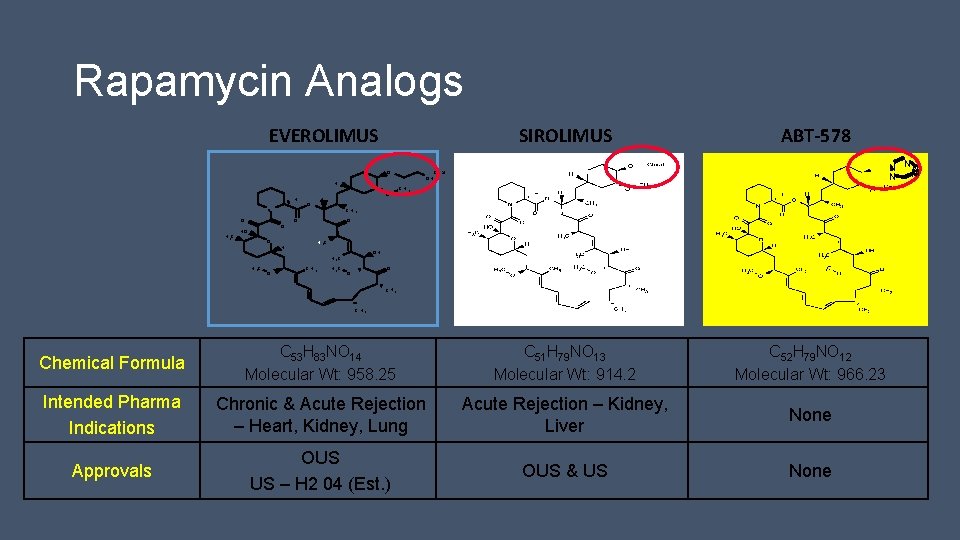
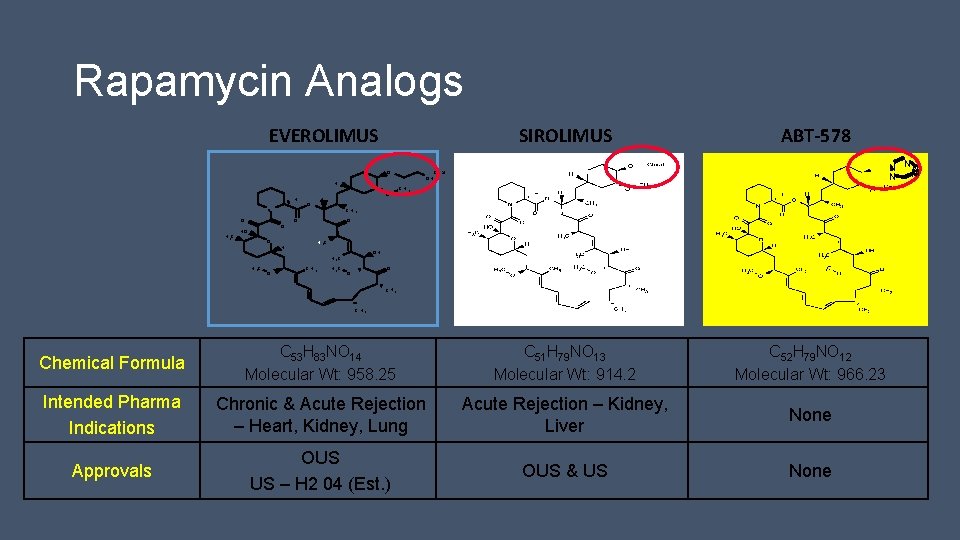
Rapamycin Analogs EVEROLIMUS SIROLIMUS O H H N O H 3 C O HO O H O N NN N Chiral C H 3 O O H 3 C H OH H 3 C OH ABT-578 C H 3 C O O C H 3 Chemical Formula C 53 H 83 NO 14 Molecular Wt: 958. 25 C 51 H 79 NO 13 Molecular Wt: 914. 2 C 52 H 79 NO 12 Molecular Wt: 966. 23 Intended Pharma Indications Chronic & Acute Rejection – Heart, Kidney, Lung Acute Rejection – Kidney, Liver None Approvals OUS US – H 2 04 (Est. ) OUS & US None



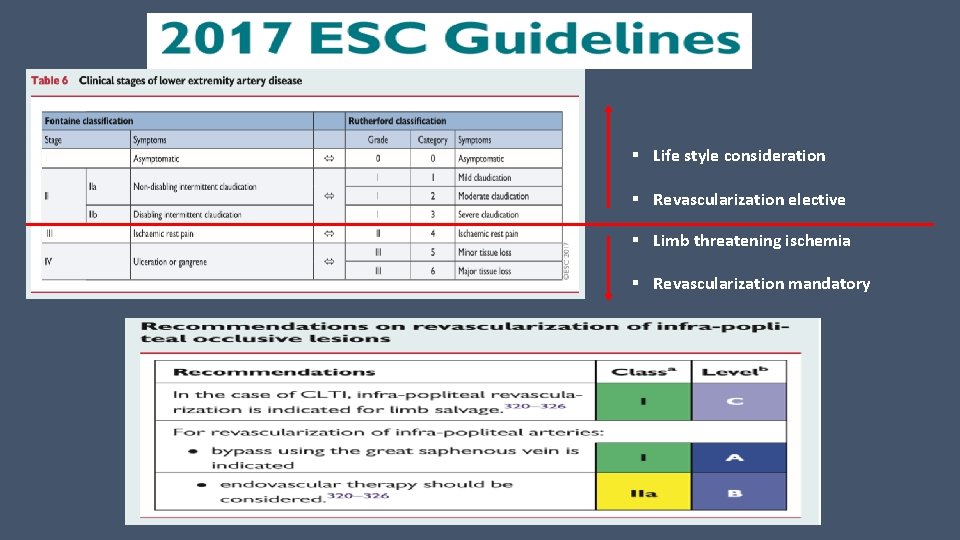
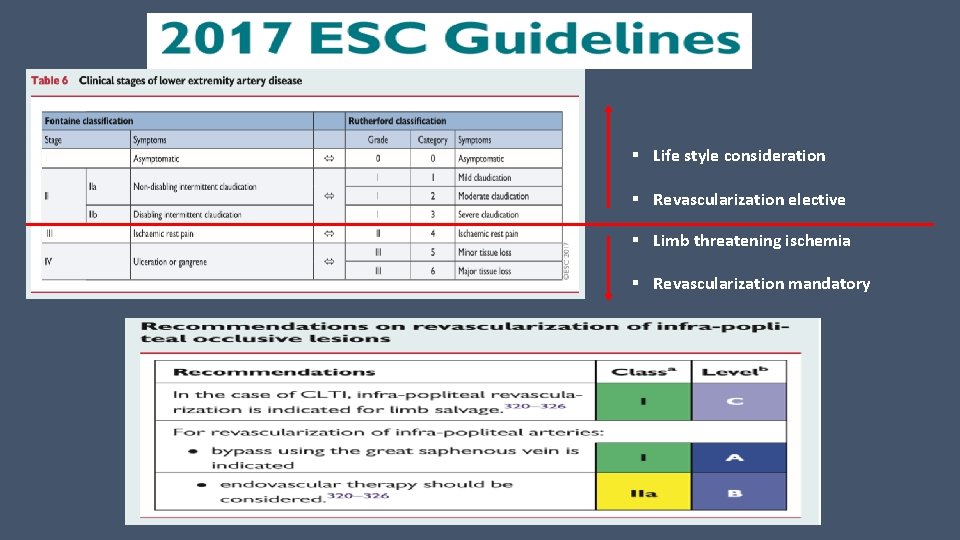
§ Life style consideration § Revascularization elective § Limb threatening ischemia § Revascularization mandatory


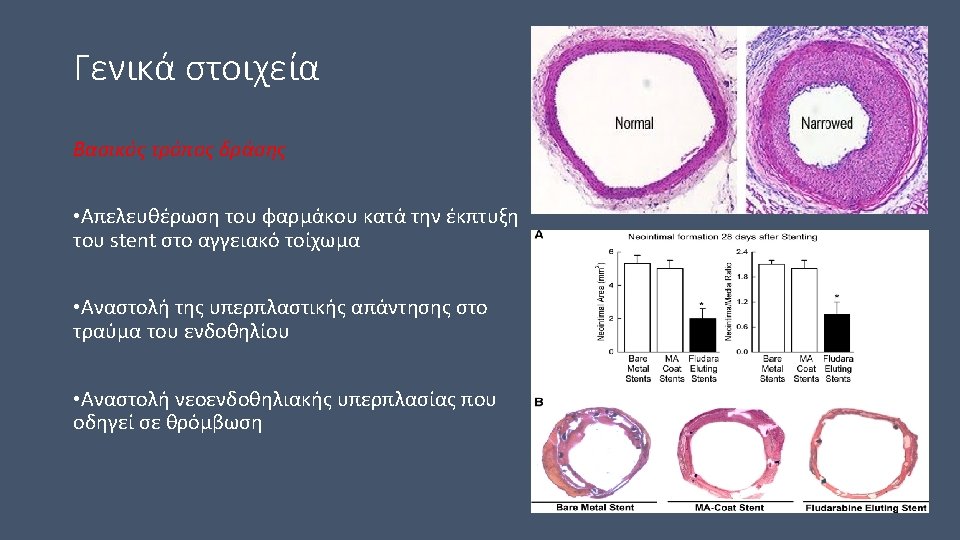
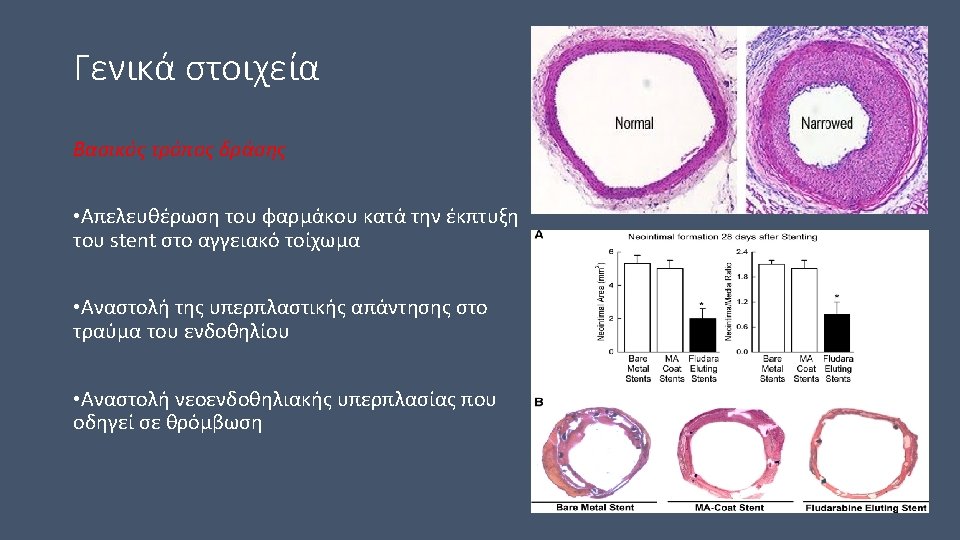
There are three major components to a drug-eluting stent: S Type of stent that carries the drug coating S Method by which the drug is delivered (eluted) by the coating to the arterial wall (polymeric or other) S The drug itself – how does it act in the body to prevent restenosis? S Cordis CYPHER™ sirolimus-eluting stent S Boston Scientific TAXUS™ paclitaxel-eluting stent system, S Medtronic's Endeavor stent which uses ABT-578 S XIENCE PRIME Everolimus Eluting Coronary Stent System

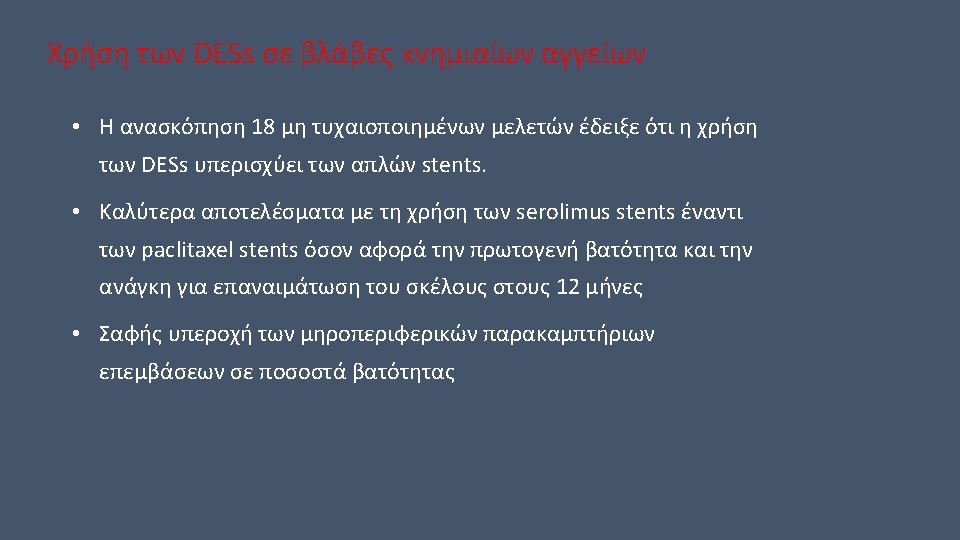
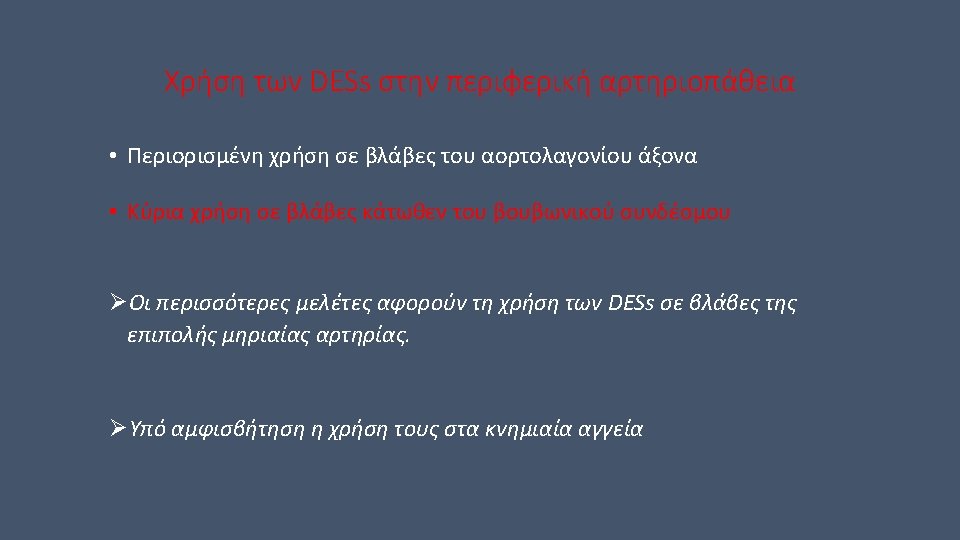
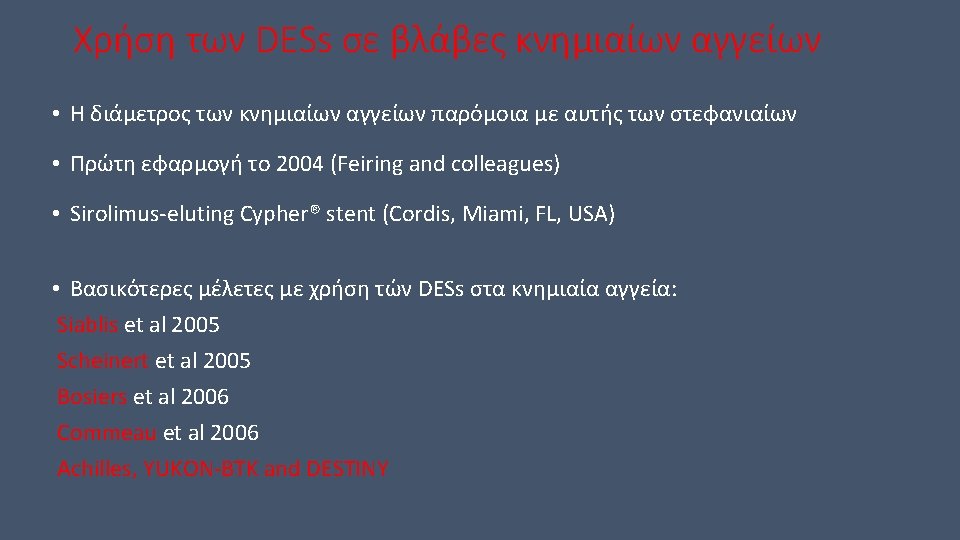
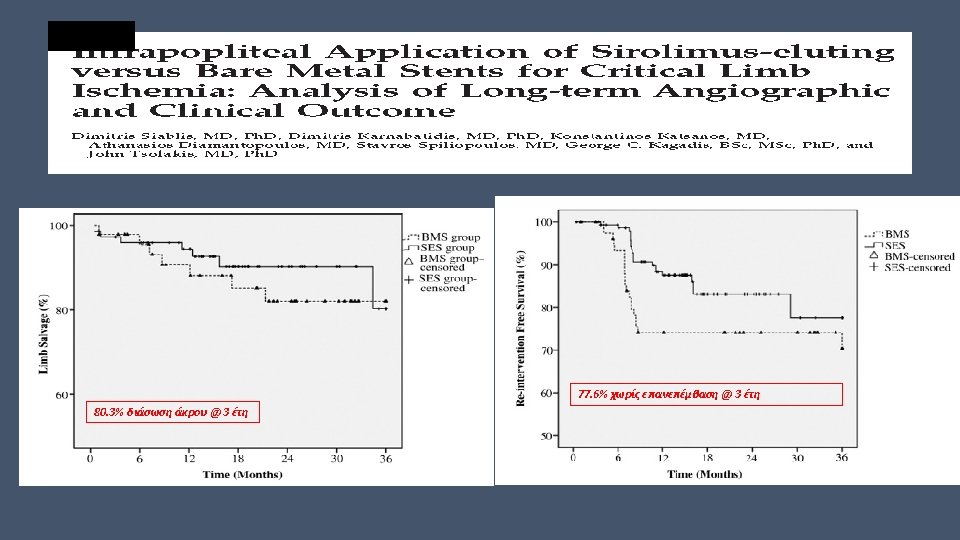
Τύποι drug-eluting stents με εφαρμογή στην αγγειοχειρουργική Sirolimus-eluting stents (SMART stents) Paclitaxel-eluting non– polymer-based stent (Zilver PTX) Self-expanding polymerbased everolimus-eluting stent (Dynalink-E)
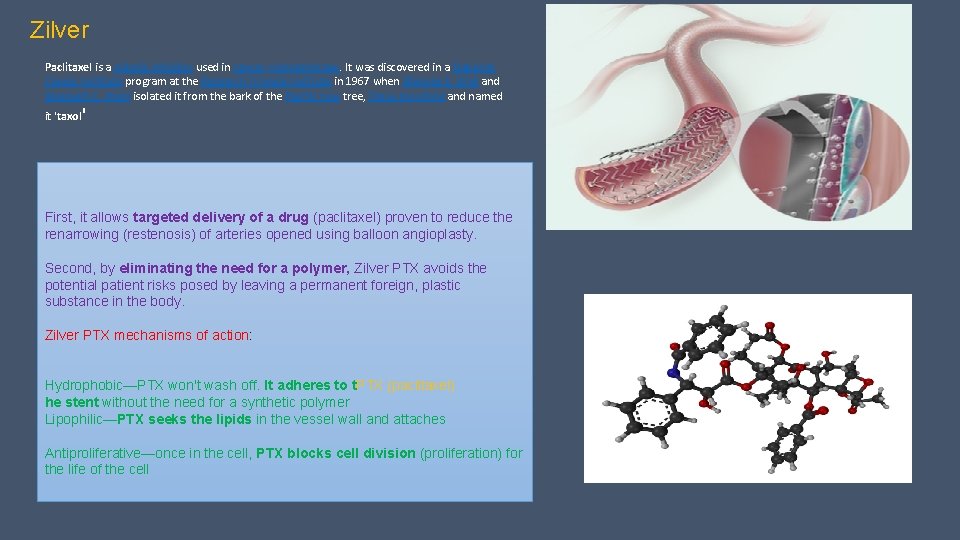
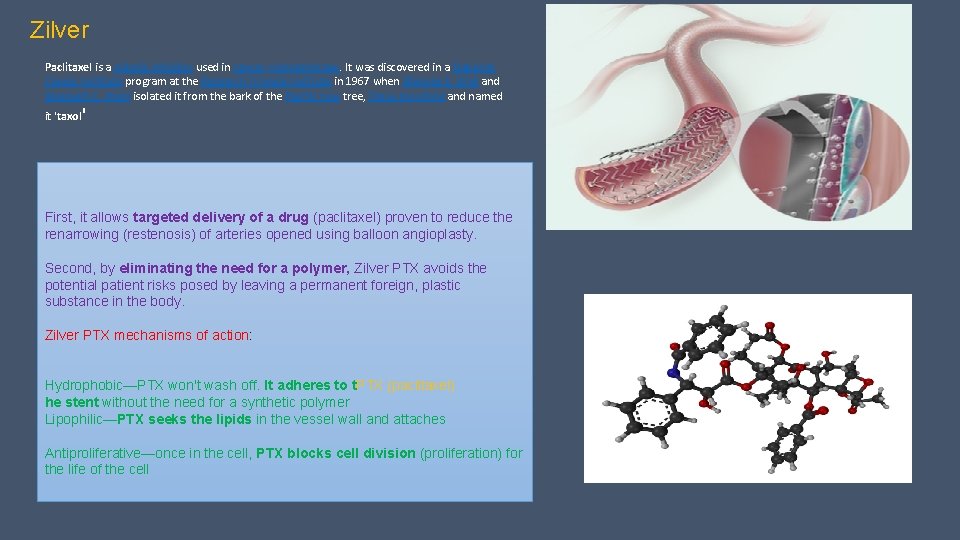
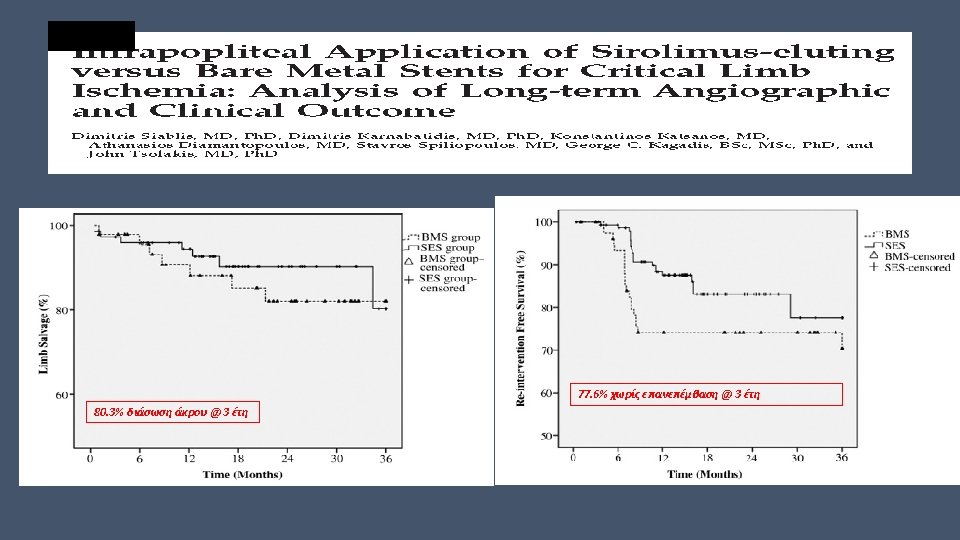
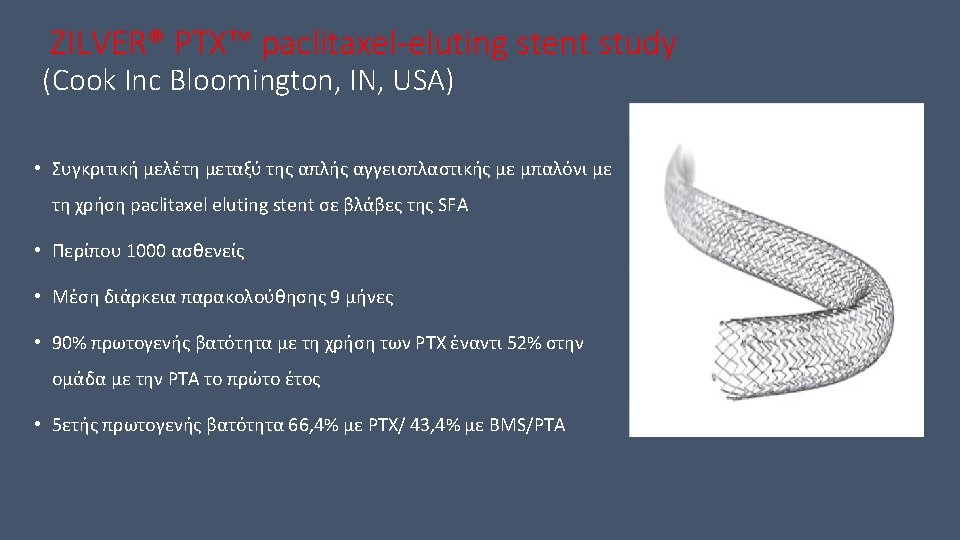
Zilver Paclitaxel is a mitotic inhibitor used in cancer chemotherapy. It was discovered in a National Cancer Institute program at the Research Triangle Institute in 1967 when Monroe E. Wall and Mansukh C. Wani isolated it from the bark of the Pacific Yew tree, Taxus brevifolia and named it 'taxol' First, it allows targeted delivery of a drug (paclitaxel) proven to reduce the renarrowing (restenosis) of arteries opened using balloon angioplasty. Second, by eliminating the need for a polymer, Zilver PTX avoids the potential patient risks posed by leaving a permanent foreign, plastic substance in the body. Zilver PTX mechanisms of action: Hydrophobic—PTX won't wash off. It adheres to t. PTX (paclitaxel) he stent without the need for a synthetic polymer Lipophilic—PTX seeks the lipids in the vessel wall and attaches Antiproliferative—once in the cell, PTX blocks cell division (proliferation) for the life of the cell



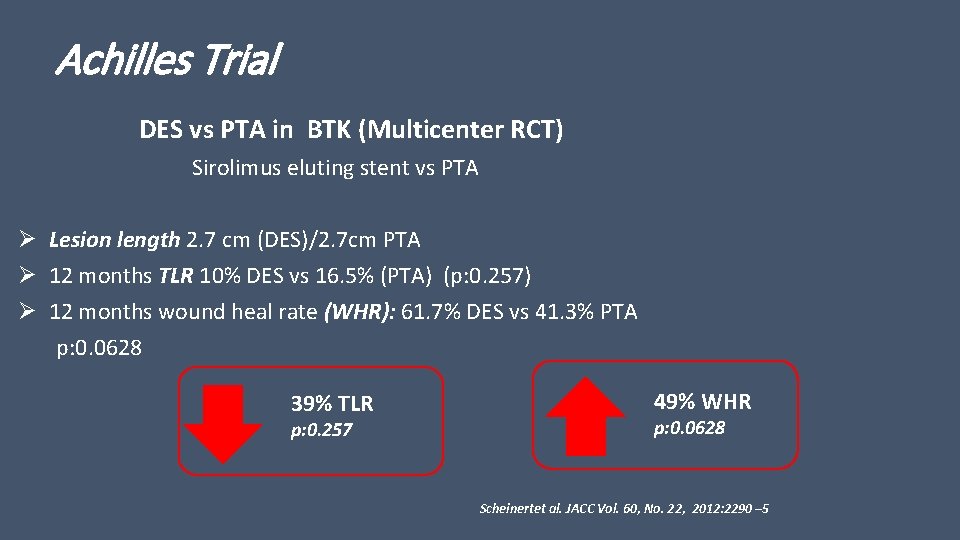
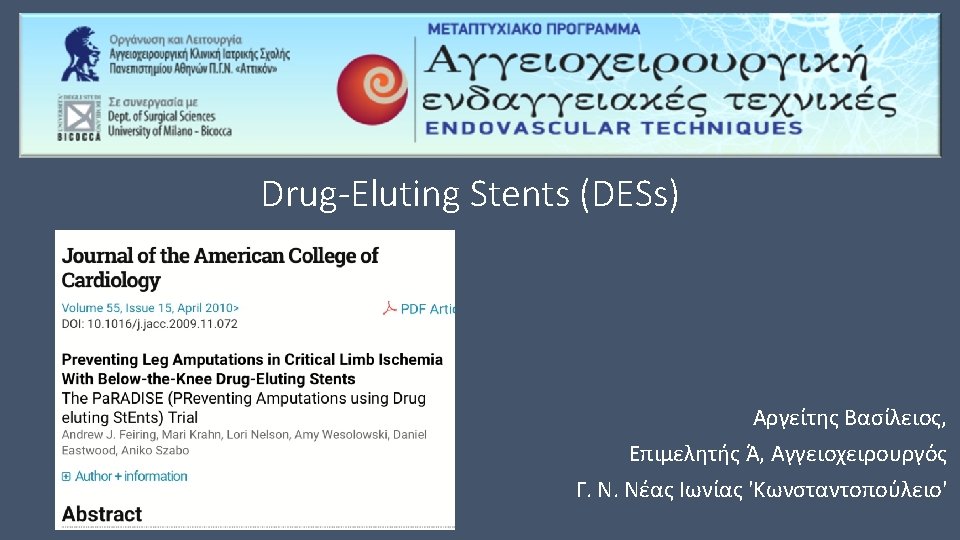
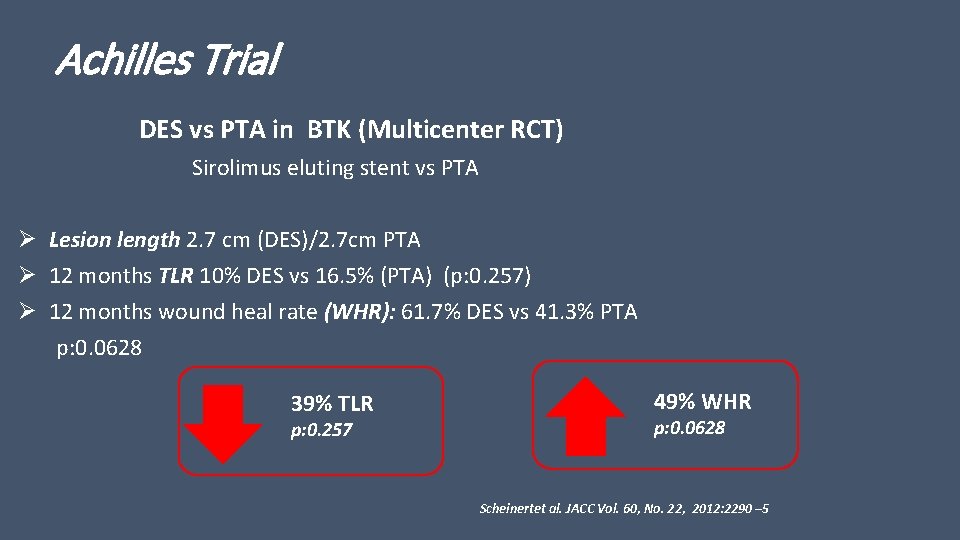
Achilles Trial DES vs PTA in BTK (Multicenter RCT) Sirolimus eluting stent vs PTA Ø Lesion length 2. 7 cm (DES)/2. 7 cm PTA Ø 12 months TLR 10% DES vs 16. 5% (PTA) (p: 0. 257) Ø 12 months wound heal rate (WHR): 61. 7% DES vs 41. 3% PTA p: 0. 0628 39% TLR p: 0. 257 49% WHR p: 0. 0628 Scheinertet al. JACC Vol. 60, No. 22, 2012: 2290 – 5
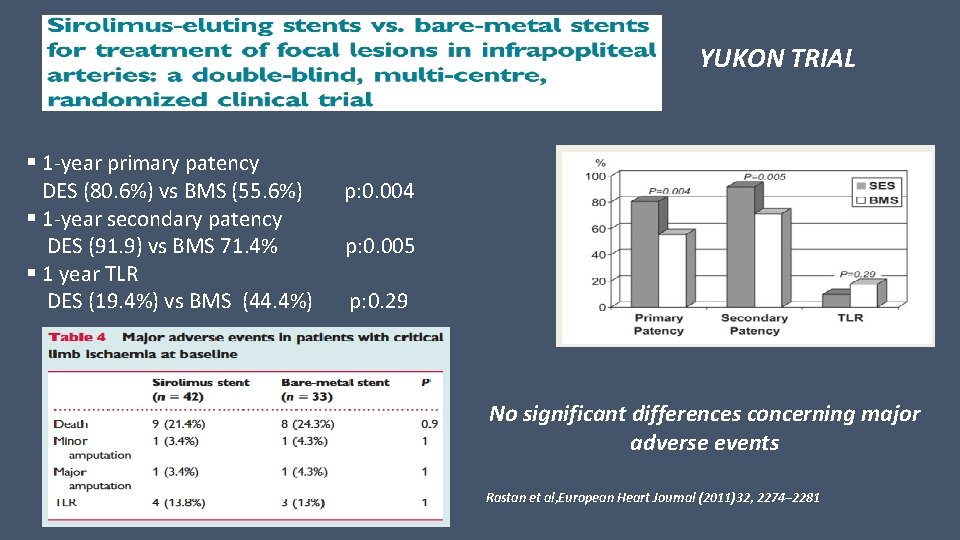
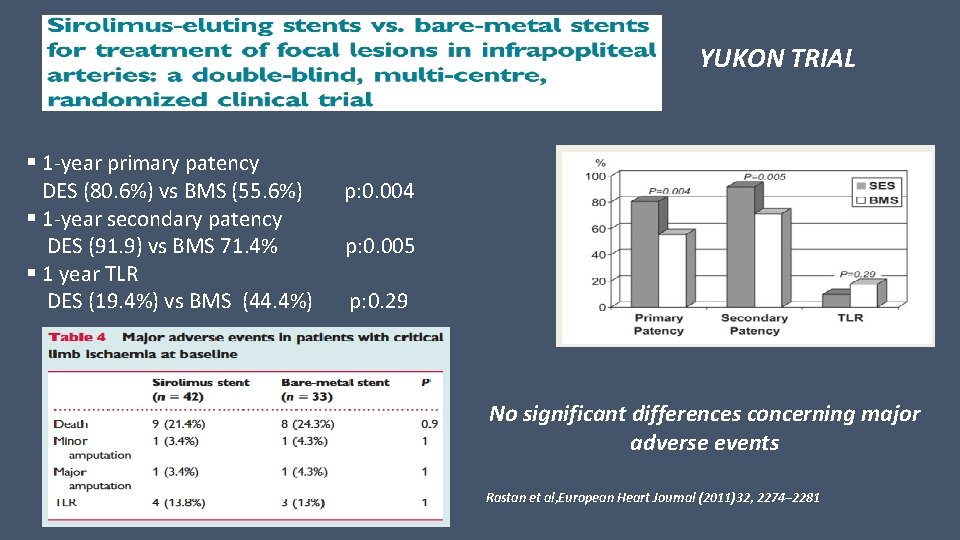
YUKON TRIAL § 1 -year primary patency DES (80. 6%) vs BMS (55. 6%) § 1 -year secondary patency DES (91. 9) vs BMS 71. 4% § 1 year TLR DES (19. 4%) vs BMS (44. 4%) p: 0. 004 p: 0. 005 p: 0. 29 No significant differences concerning major adverse events Rastan et al, European Heart Journal (2011)32, 2274– 2281
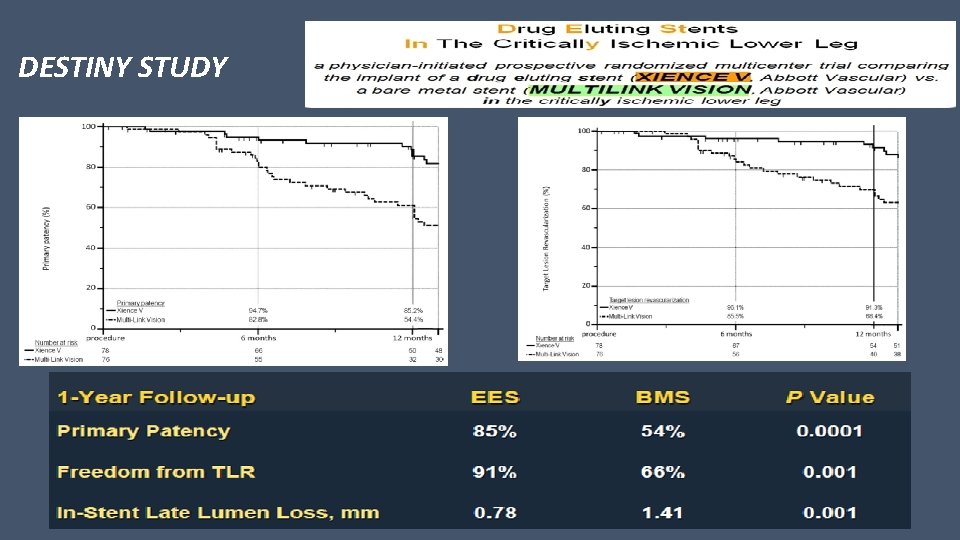
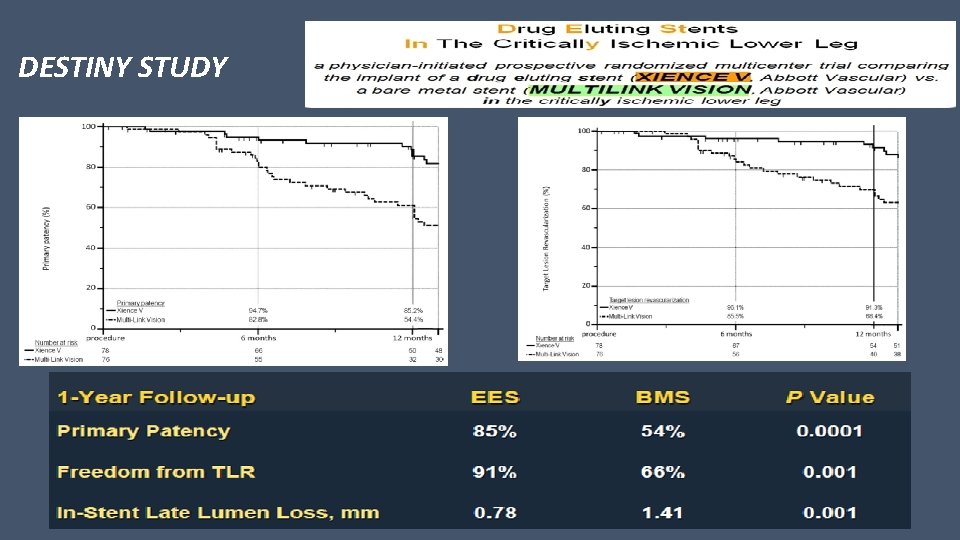
DESTINY STUDY
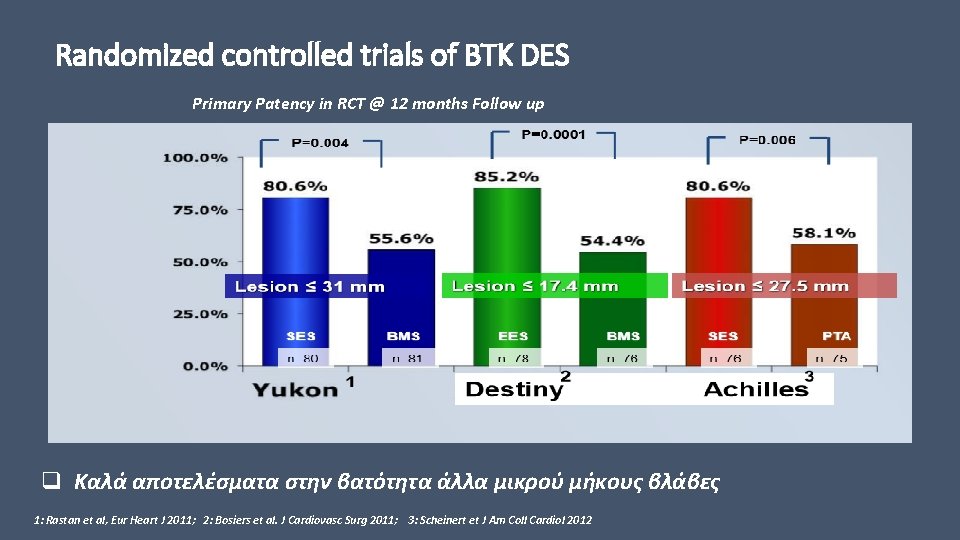
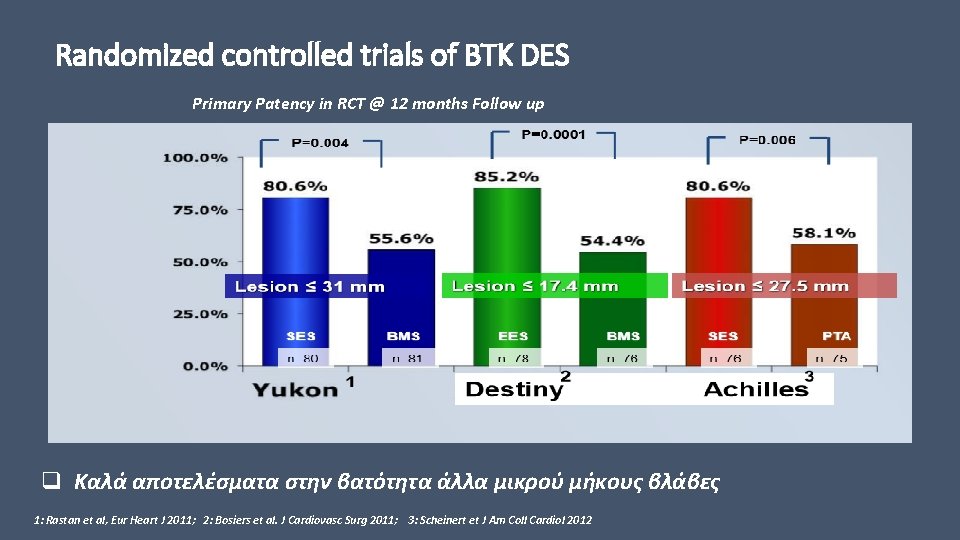
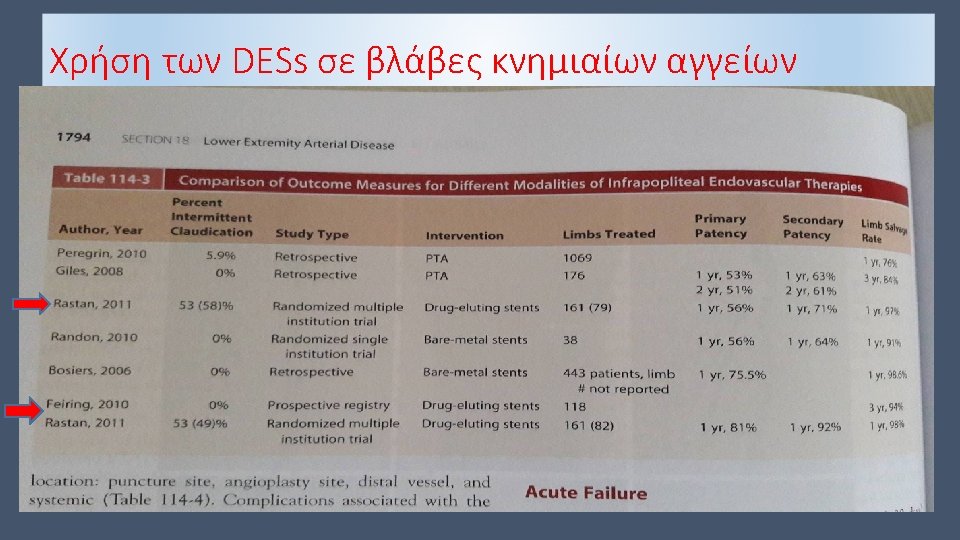
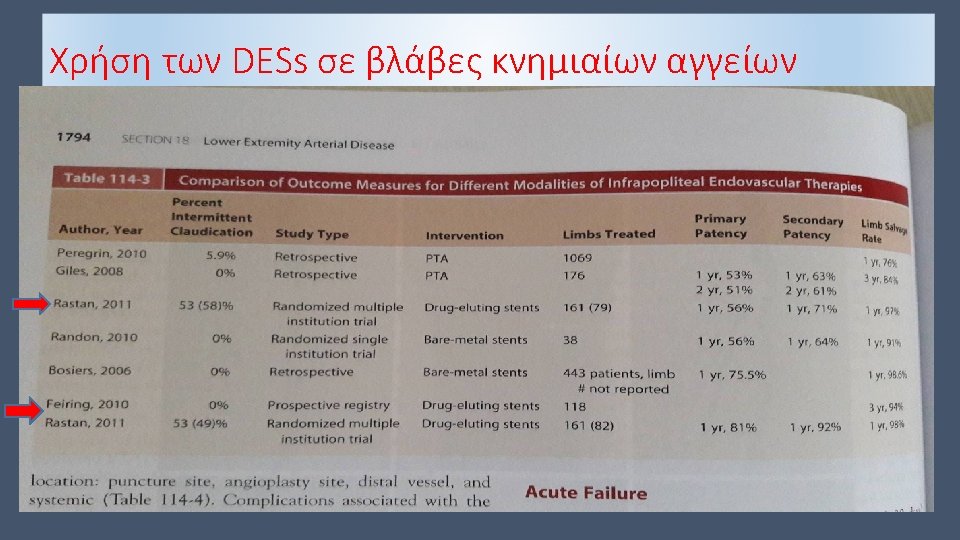
Randomized controlled trials of BTK DES Primary Patency in RCT @ 12 months Follow up q Καλά αποτελέσματα στην βατότητα άλλα μικρού μήκους βλάβες 1: Rastan et al, Eur Heart J 2011; 2: Bosiers et al. J Cardiovasc Surg 2011; 3: Scheinert et J Am Coll Cardiol 2012

DESTINY 2 § Prospective, non-randomized, multi-center study § Lesions between 30 mm and 100 mm 12 months -75, 4% 12 months -84, 9% Bosiers et al, Journal of Cardiovascular surgery 2017 february; 58(1): 49 -54
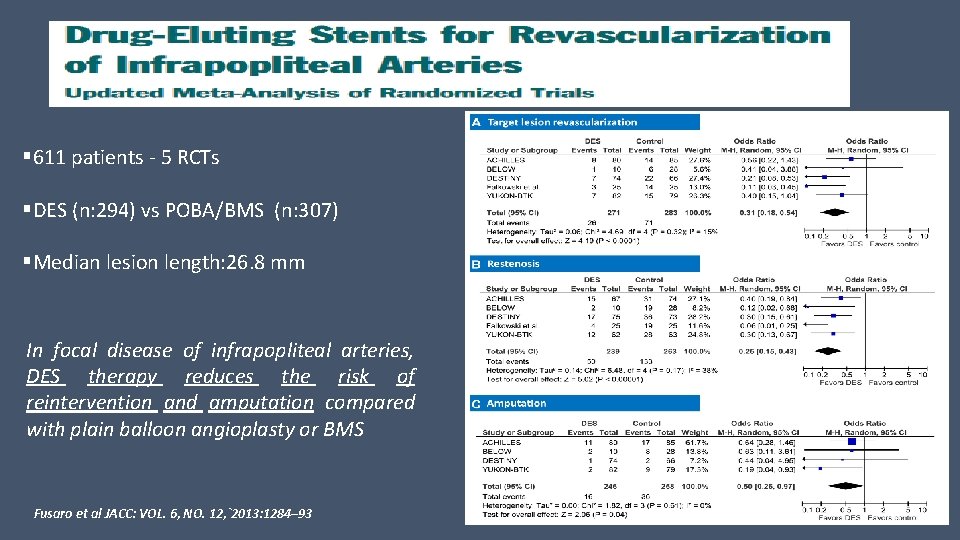
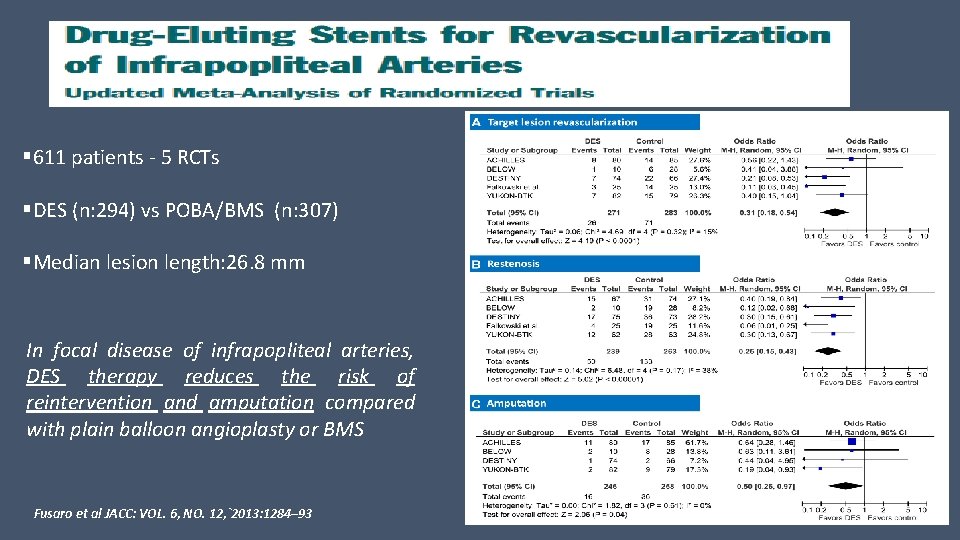
§ 611 patients - 5 RCTs §DES (n: 294) vs POBA/BMS (n: 307) §Median lesion length: 26. 8 mm In focal disease of infrapopliteal arteries, DES therapy reduces the risk of reintervention and amputation compared with plain balloon angioplasty or BMS Fusaro et al JACC: VOL. 6, NO. 12, `2013: 1284– 93
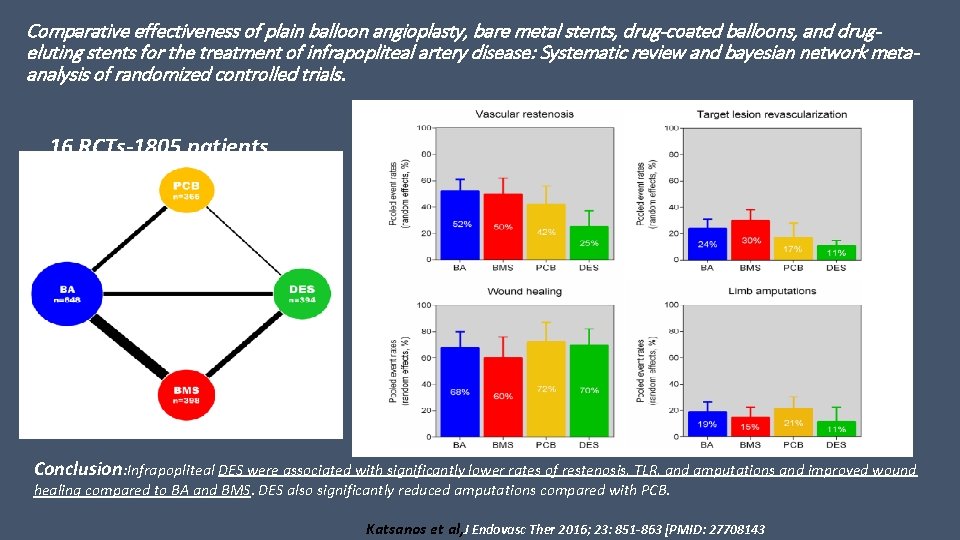
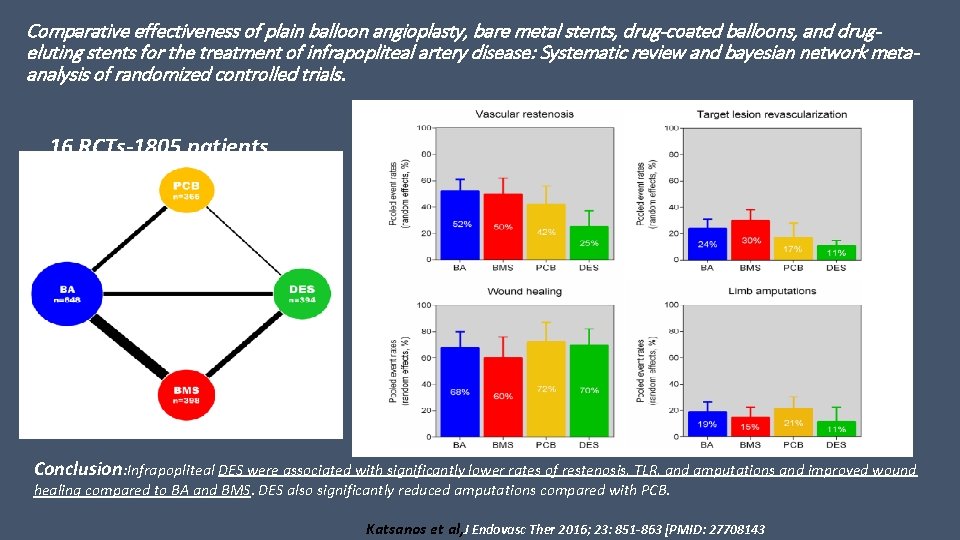
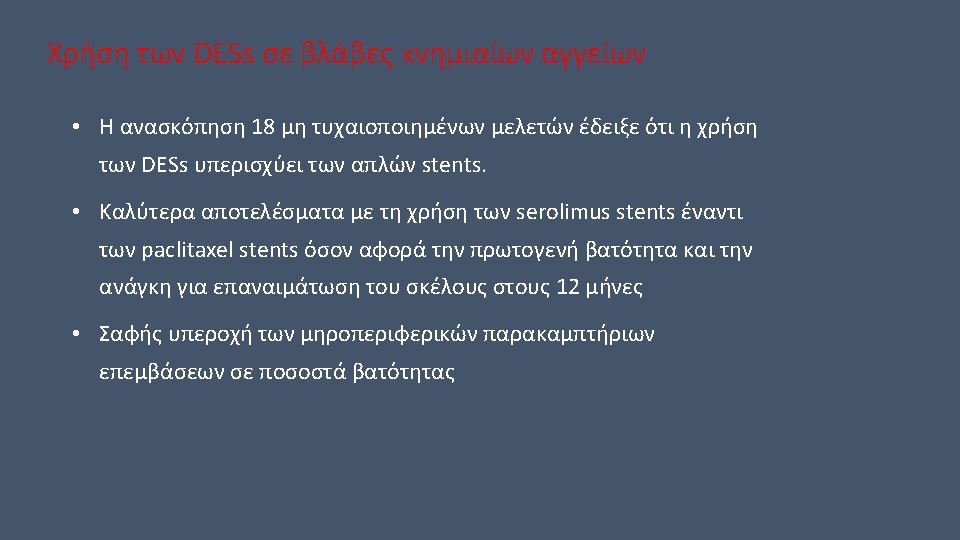
Comparative effectiveness of plain balloon angioplasty, bare metal stents, drug-coated balloons, and drugeluting stents for the treatment of infrapopliteal artery disease: Systematic review and bayesian network metaanalysis of randomized controlled trials. 16 RCTs-1805 patients Conclusion: Infrapopliteal DES were associated with significantly lower rates of restenosis, TLR, and amputations and improved wound healing compared to BA and BMS. DES also significantly reduced amputations compared with PCB. Katsanos et al, J Endovasc Ther 2016; 23: 851 -863 [PMID: 27708143
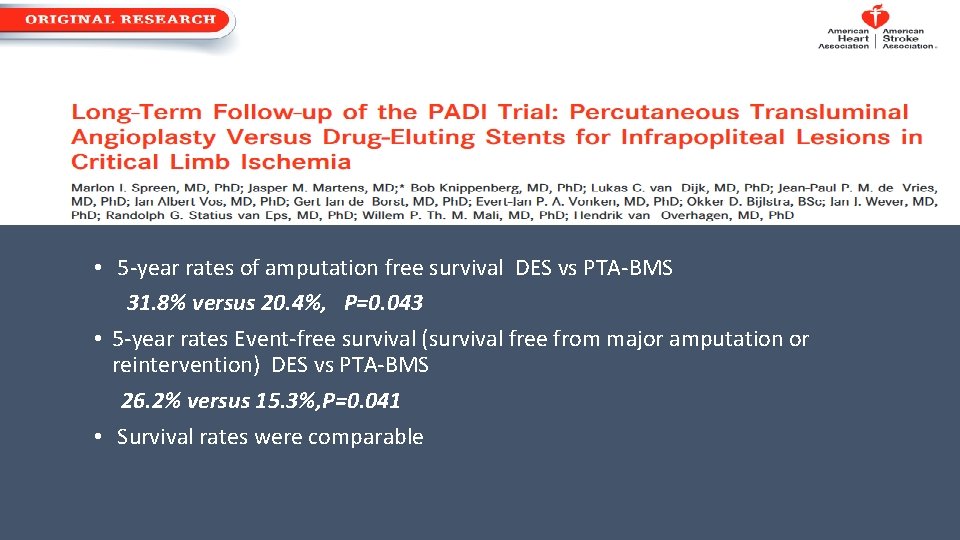
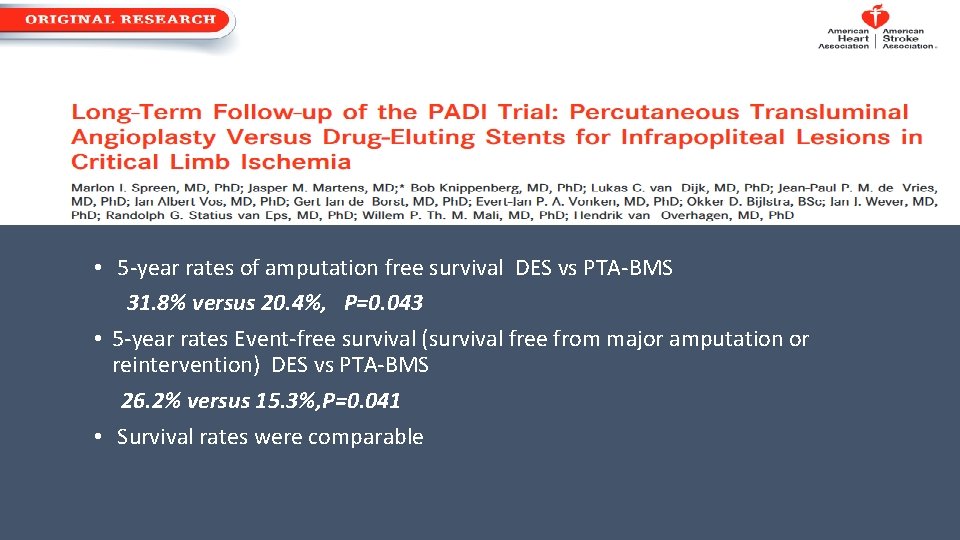
• 5 -year rates of amputation free survival DES vs PTA-BMS 31. 8% versus 20. 4%, P=0. 043 • 5 -year rates Event-free survival (survival free from major amputation or reintervention) DES vs PTA-BMS 26. 2% versus 15. 3%, P=0. 041 • Survival rates were comparable
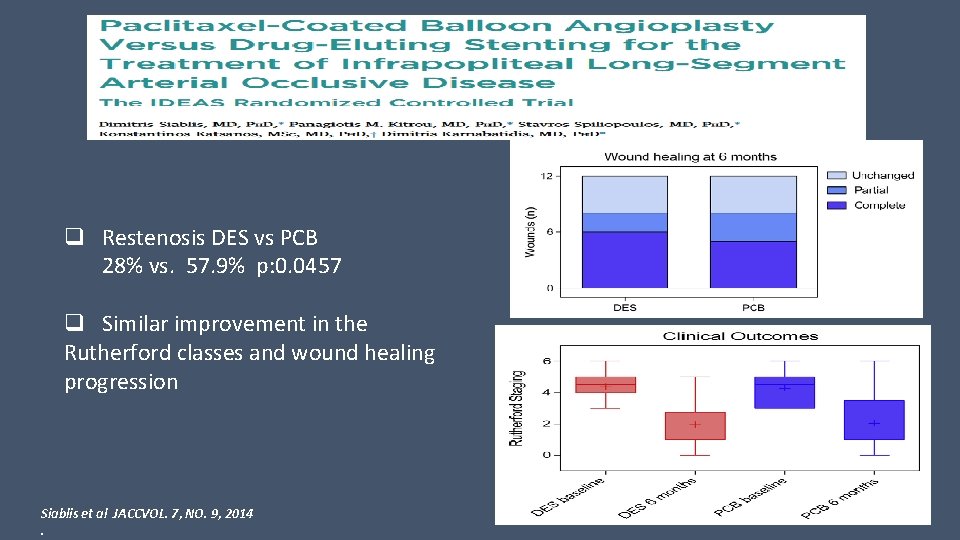
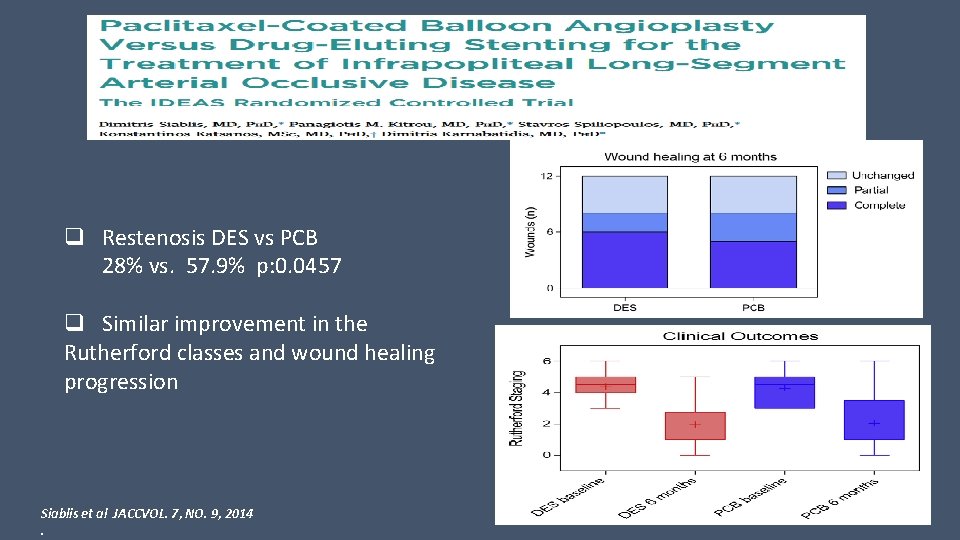
q Restenosis DES vs PCB 28% vs. 57. 9% p: 0. 0457 q Similar improvement in the Rutherford classes and wound healing progression Siablis et al JACCVOL. 7, NO. 9, 2014.
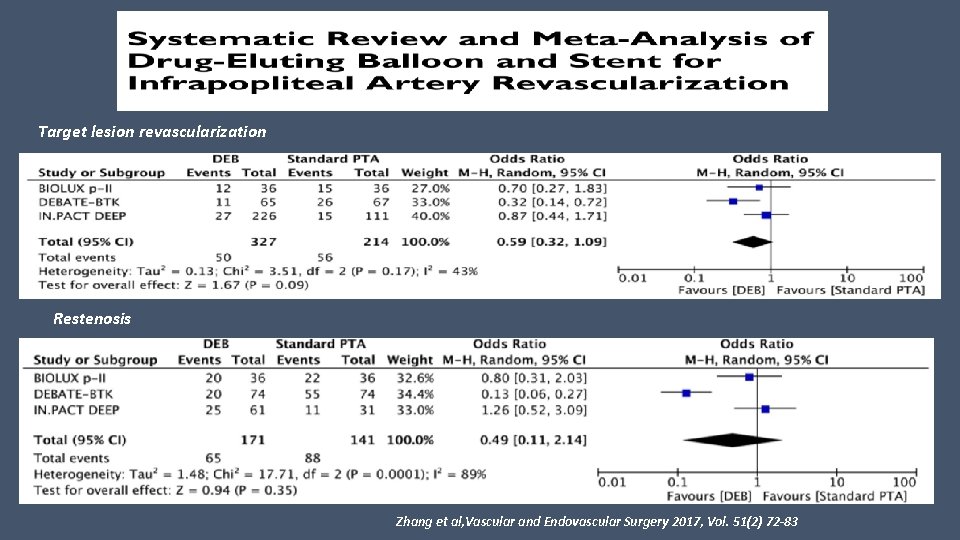
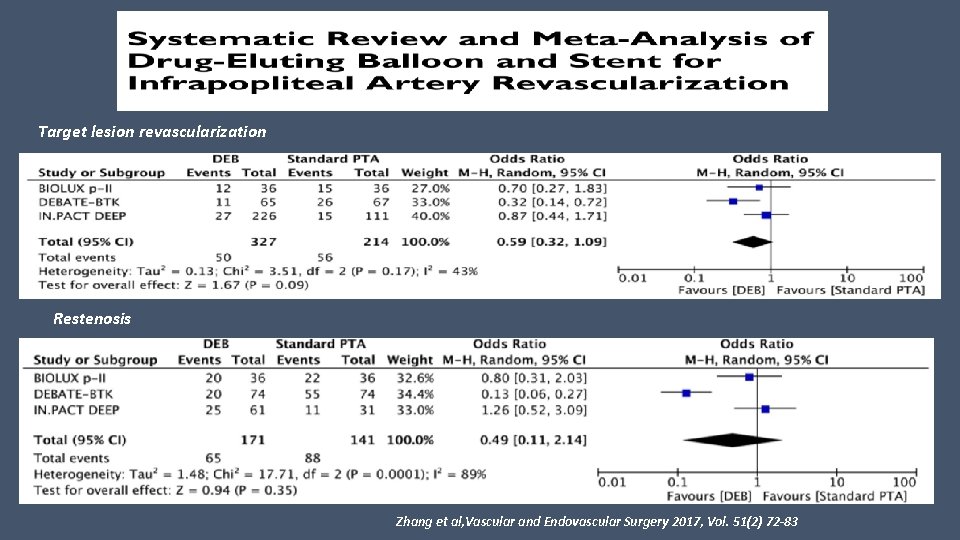
Target lesion revascularization Restenosis Zhang et al, Vascular and Endovascular Surgery 2017, Vol. 51(2) 72 -83
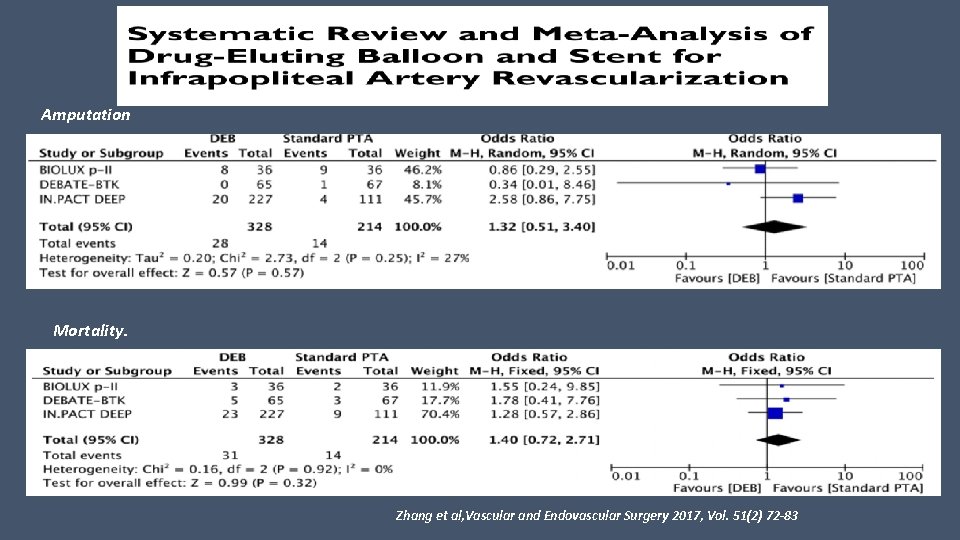
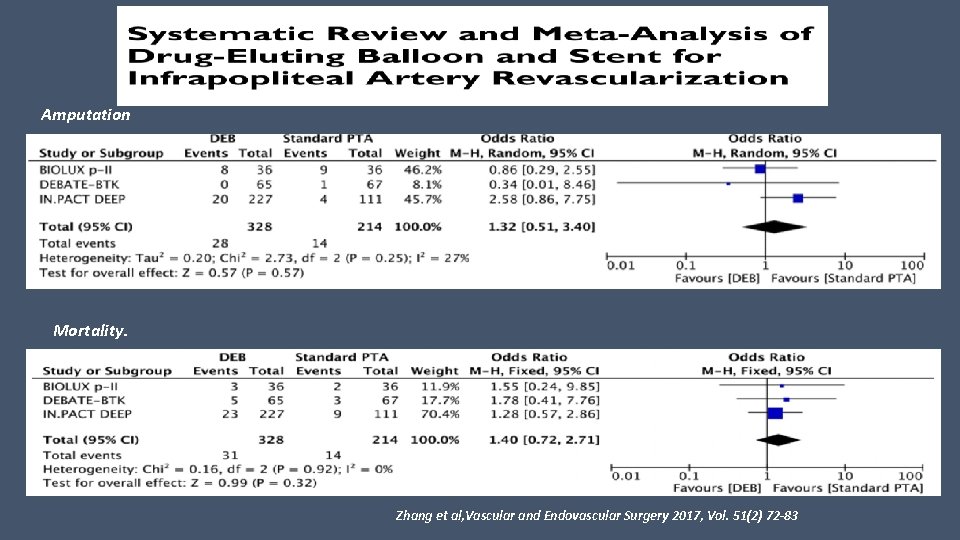
Amputation Mortality. Zhang et al, Vascular and Endovascular Surgery 2017, Vol. 51(2) 72 -83
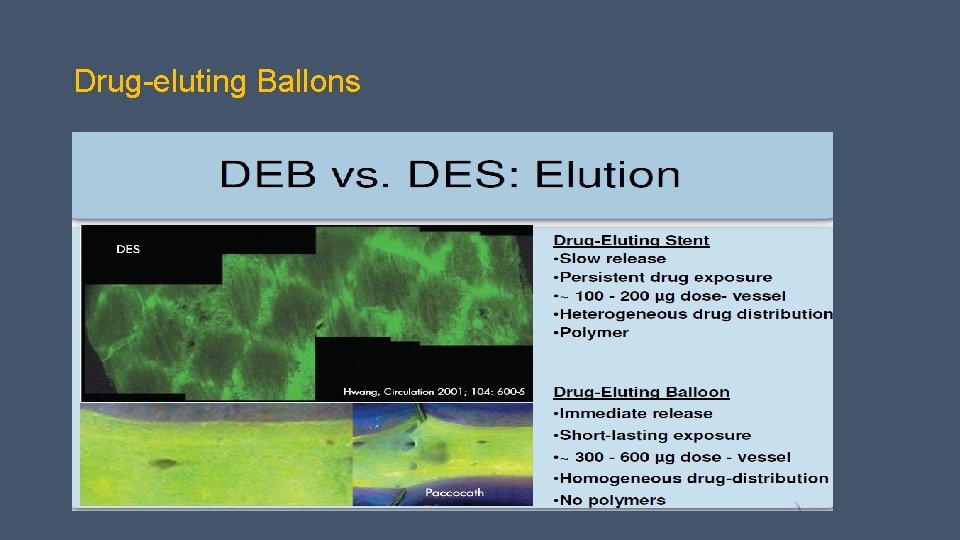
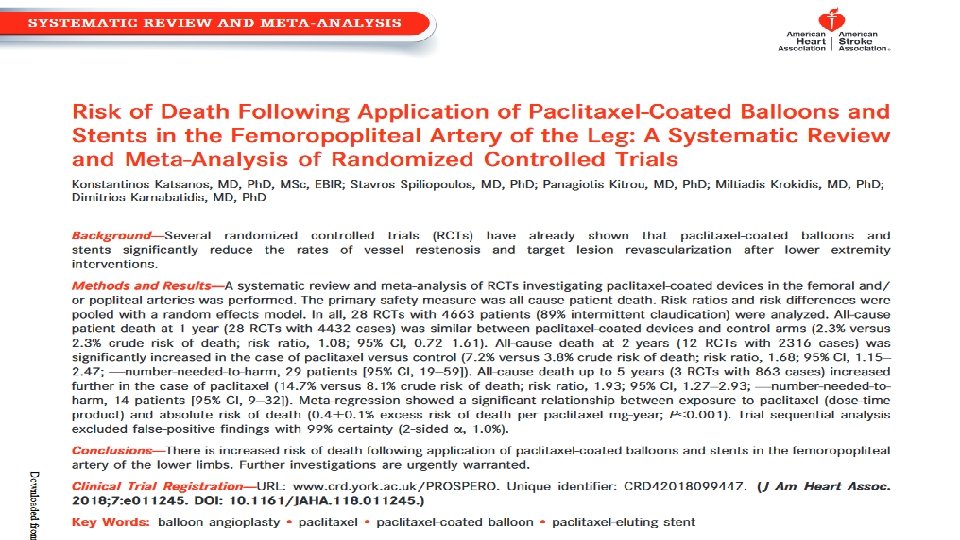
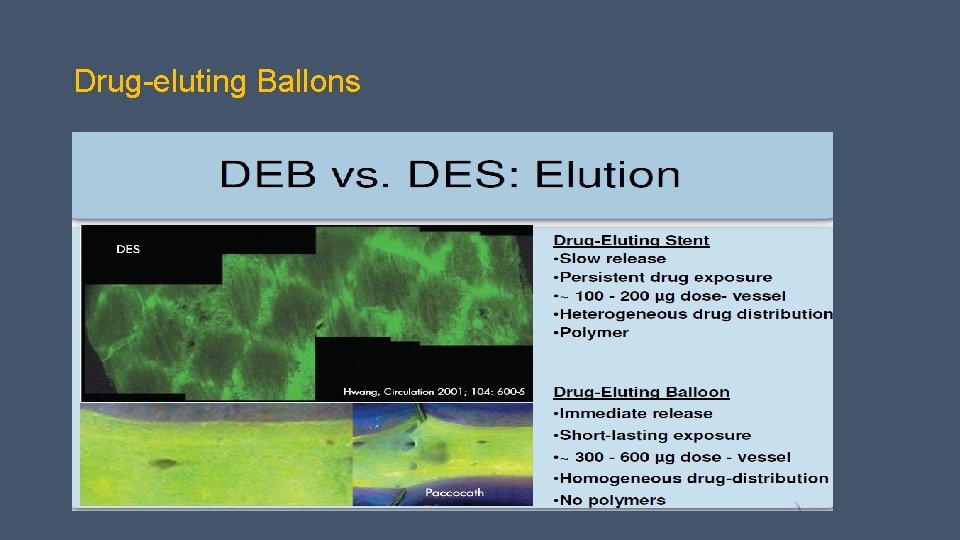
Drug-eluting Ballons