Rangel QI Ironing out the kinks Improving Screening

- Slides: 18

Rangel QI Ironing out the kinks: Improving Screening and Treatment of Iron Deficiency Anemia Betty Reyes, Taina Sanchez, PFA Staff Michelle Coleman, Clara Paris, RN Staff Wendy Acosta, Jessie Soriano, MA Staff Evelyn Berger, Hetty Cunningham, Christine Krause Elshadey Bekele, Sandhya Brachio, Alicia Chang, Laura Perreta, Wee Chua, Kenny Mc. Kinley, Jen Cohen, Andrew Wehrman, Ashish Ankola, Nisha Broodie, Ashley Blanchard, Pooja Desai
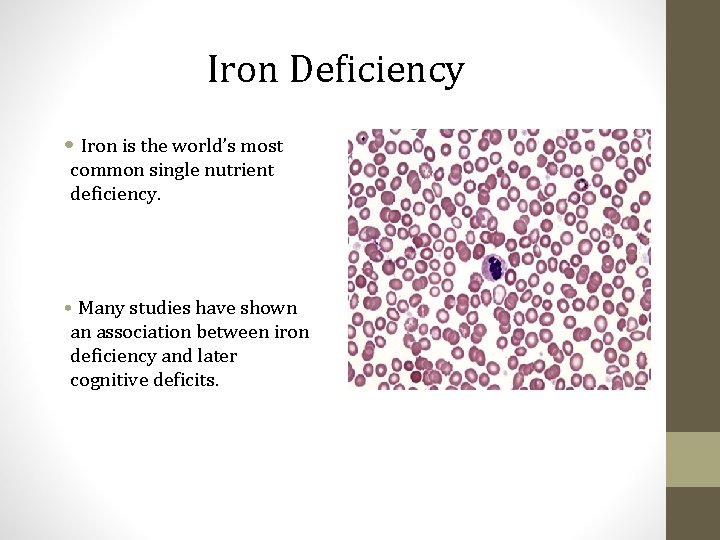
Iron Deficiency • Iron is the world’s most common single nutrient deficiency. • Many studies have shown an association between iron deficiency and later cognitive deficits.
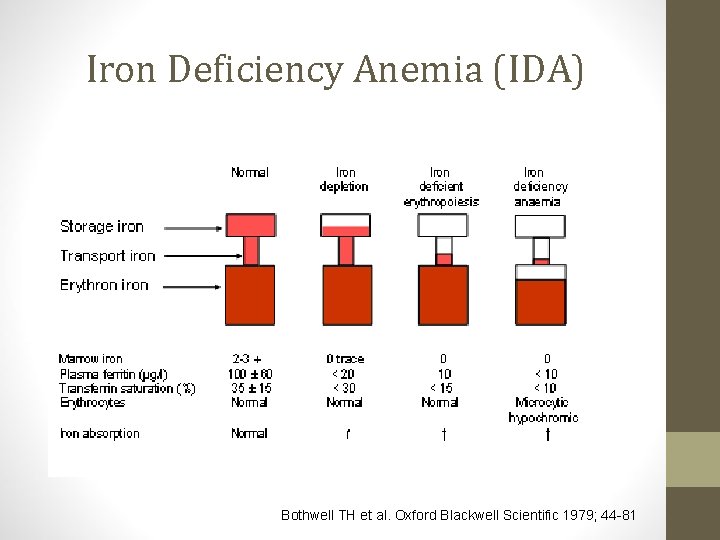
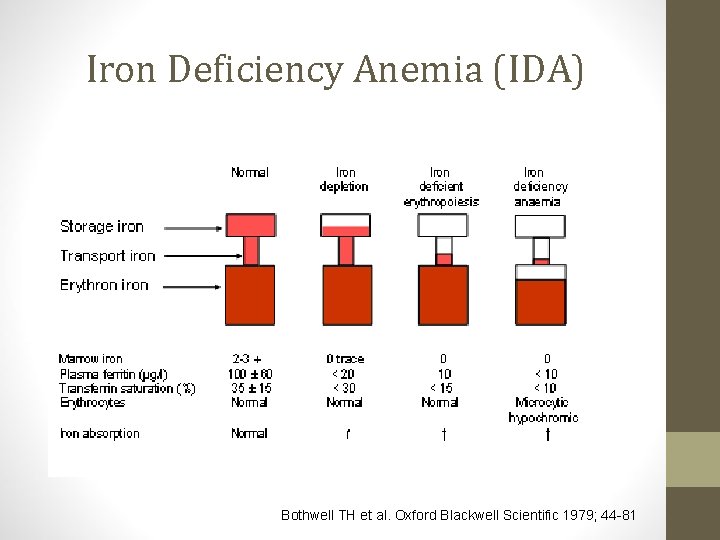
Iron Deficiency Anemia (IDA) Bothwell TH et al. Oxford Blackwell Scientific 1979; 44 -81
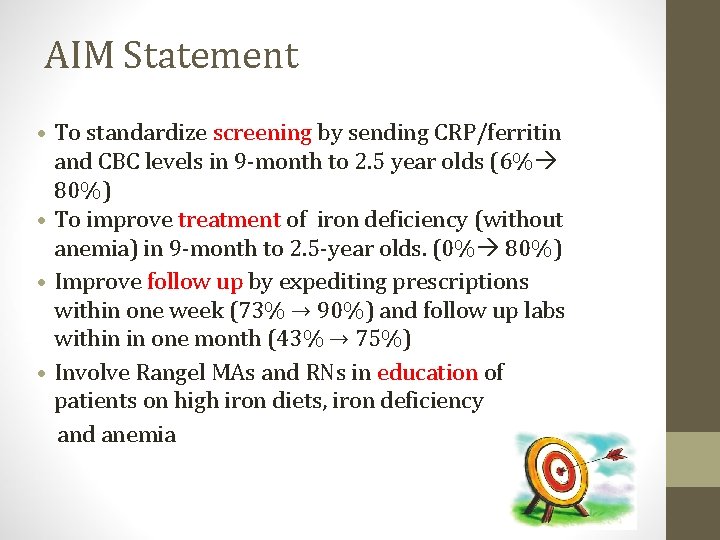
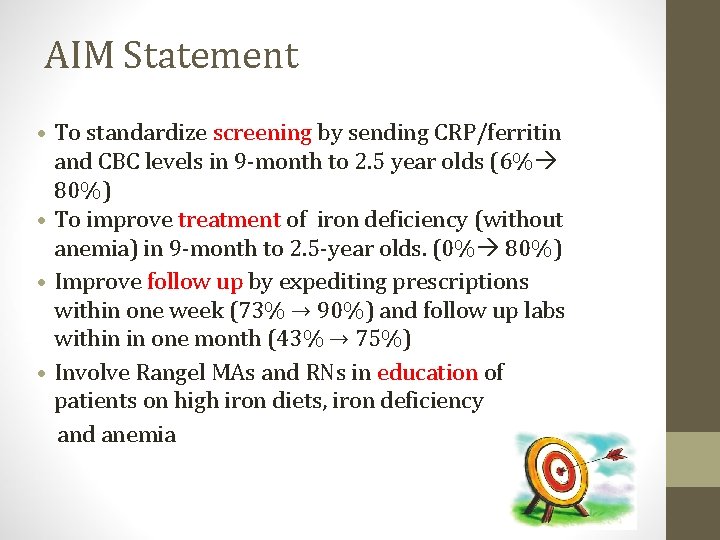
AIM Statement • To standardize screening by sending CRP/ferritin and CBC levels in 9 -month to 2. 5 year olds (6% 80%) • To improve treatment of iron deficiency (without anemia) in 9 -month to 2. 5 -year olds. (0% 80%) • Improve follow up by expediting prescriptions within one week (73% → 90%) and follow up labs within in one month (43% → 75%) • Involve Rangel MAs and RNs in education of patients on high iron diets, iron deficiency and anemia
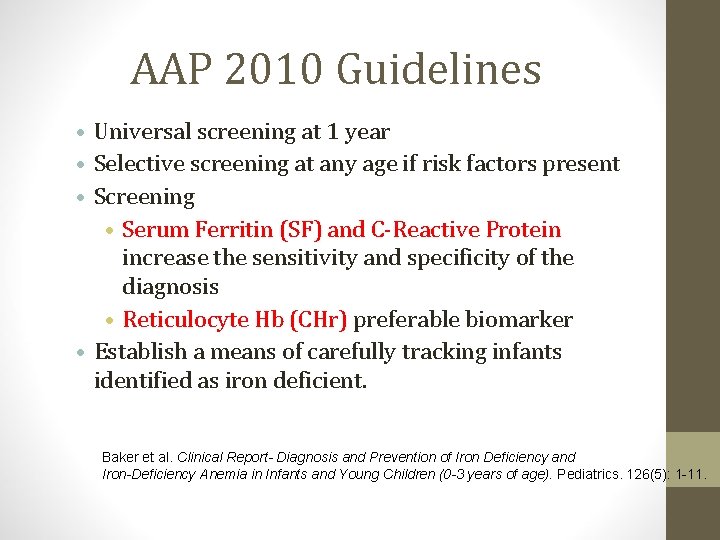
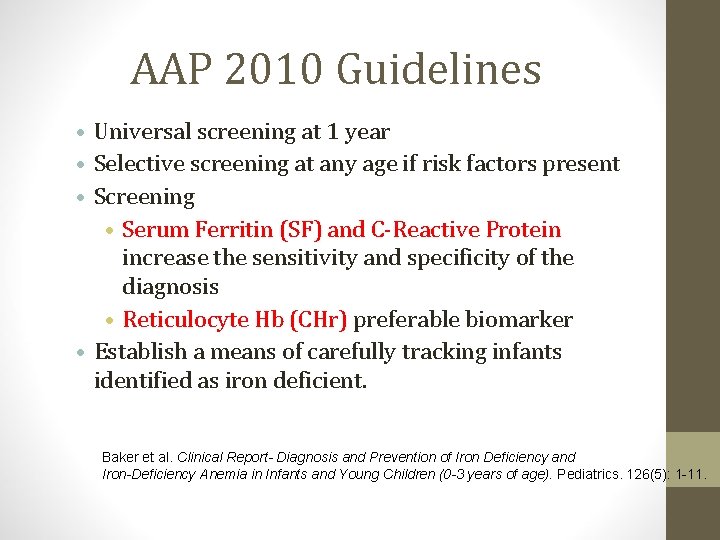
AAP 2010 Guidelines • Universal screening at 1 year • Selective screening at any age if risk factors present • Screening • Serum Ferritin (SF) and C-Reactive Protein increase the sensitivity and specificity of the diagnosis • Reticulocyte Hb (CHr) preferable biomarker • Establish a means of carefully tracking infants identified as iron deficient. Baker et al. Clinical Report- Diagnosis and Prevention of Iron Deficiency and Iron-Deficiency Anemia in Infants and Young Children (0 -3 years of age). Pediatrics. 126(5): 1 -11.
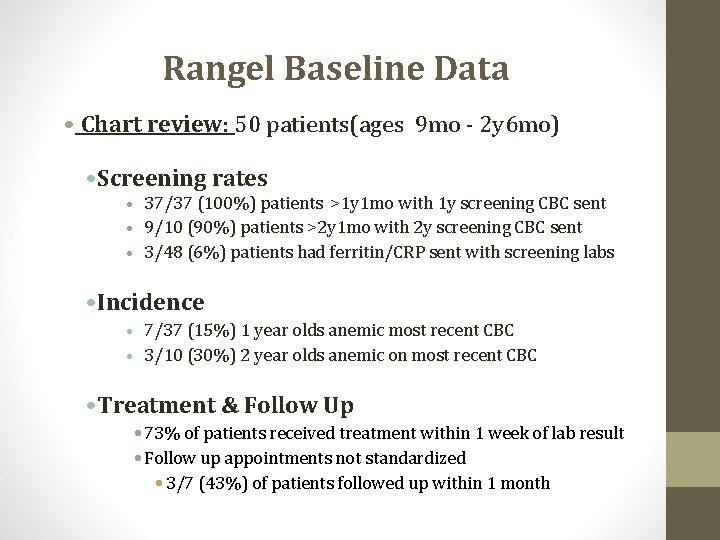
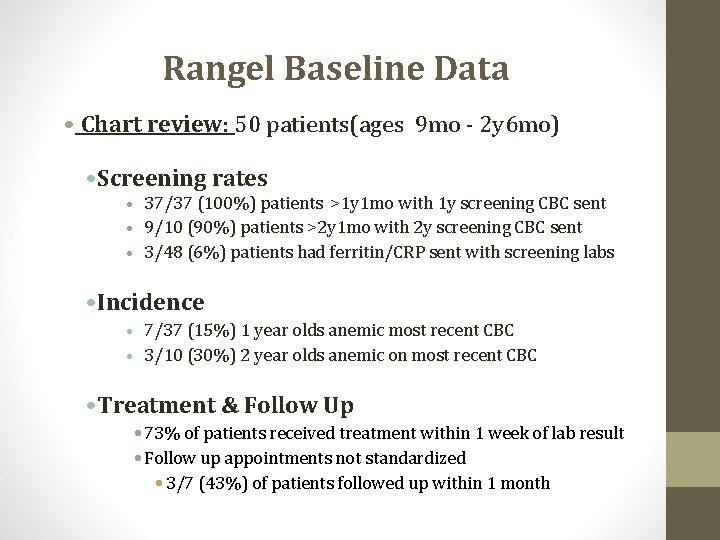
Rangel Baseline Data • Chart review: 50 patients(ages 9 mo - 2 y 6 mo) • Screening rates • 37/37 (100%) patients >1 y 1 mo with 1 y screening CBC sent • 9/10 (90%) patients >2 y 1 mo with 2 y screening CBC sent • 3/48 (6%) patients had ferritin/CRP sent with screening labs • Incidence • 7/37 (15%) 1 year olds anemic most recent CBC • 3/10 (30%) 2 year olds anemic on most recent CBC • Treatment & Follow Up • 73% of patients received treatment within 1 week of lab result • Follow up appointments not standardized • 3/7 (43%) of patients followed up within 1 month
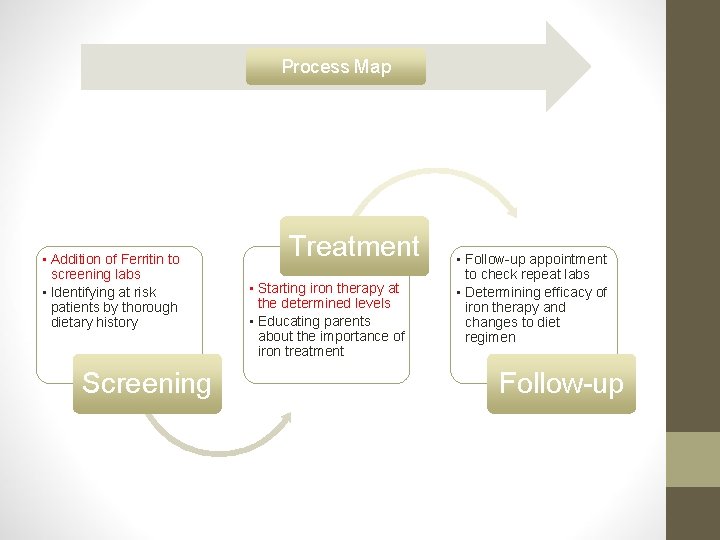
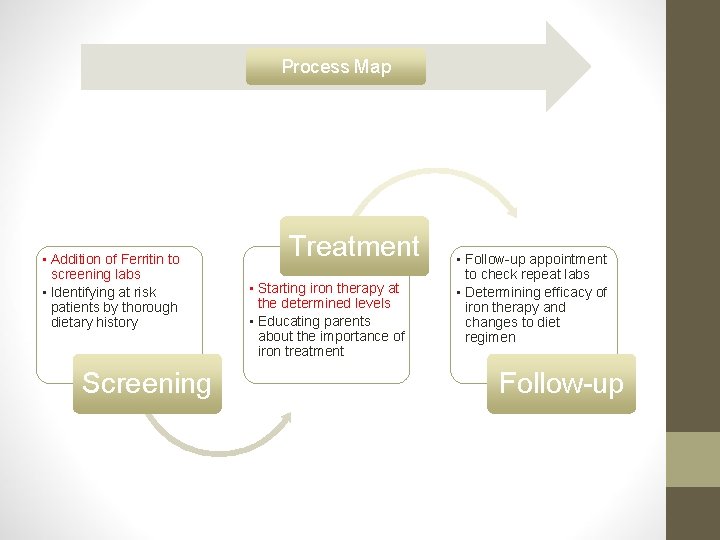
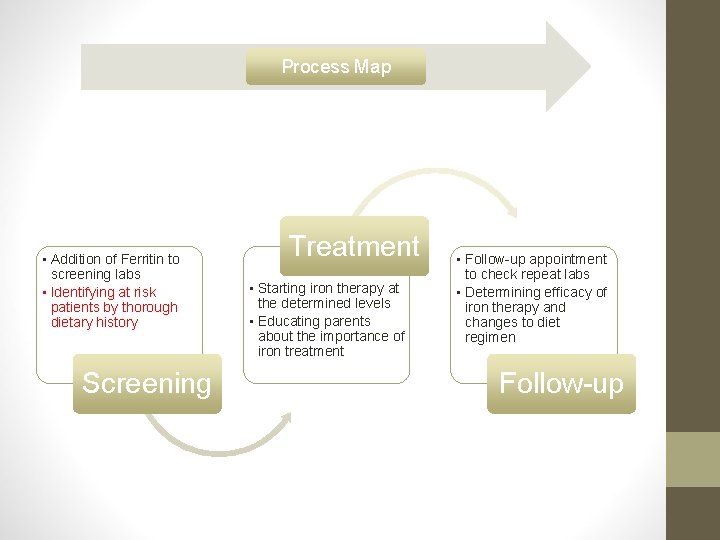
Process Map • Addition of Ferritin to screening labs • Identifying at risk patients by thorough dietary history Screening Treatment • Starting iron therapy at the determined levels • Educating parents about the importance of iron treatment • Follow-up appointment to check repeat labs • Determining efficacy of iron therapy and changes to diet regimen Follow-up
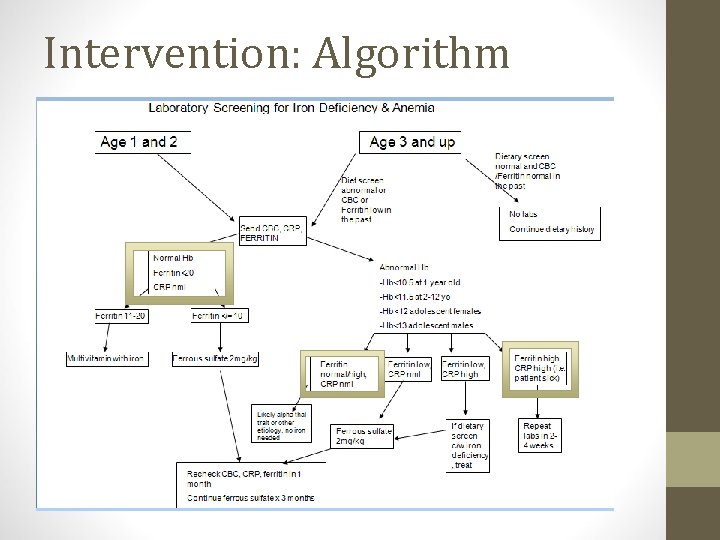
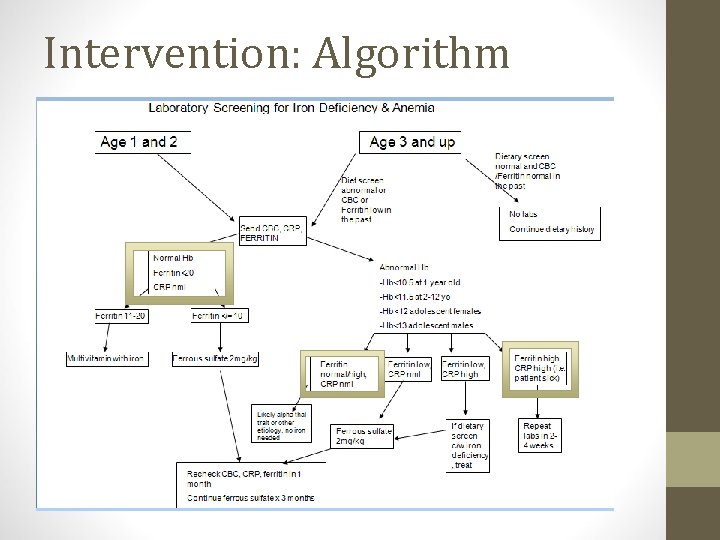
Intervention: Algorithm
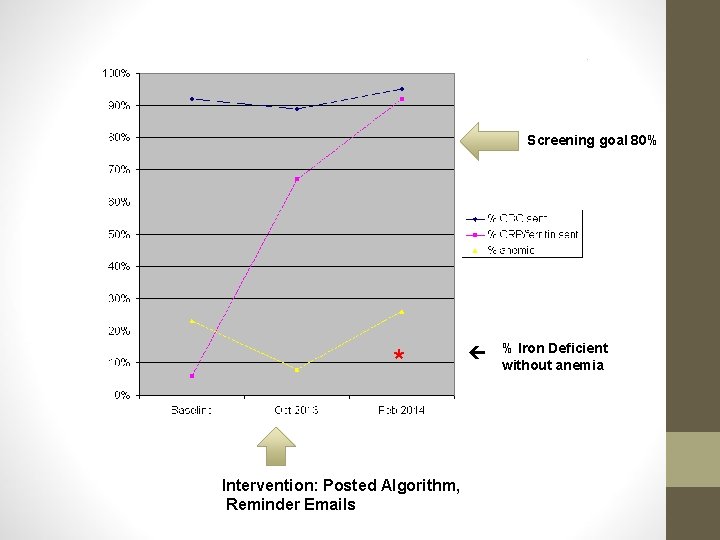
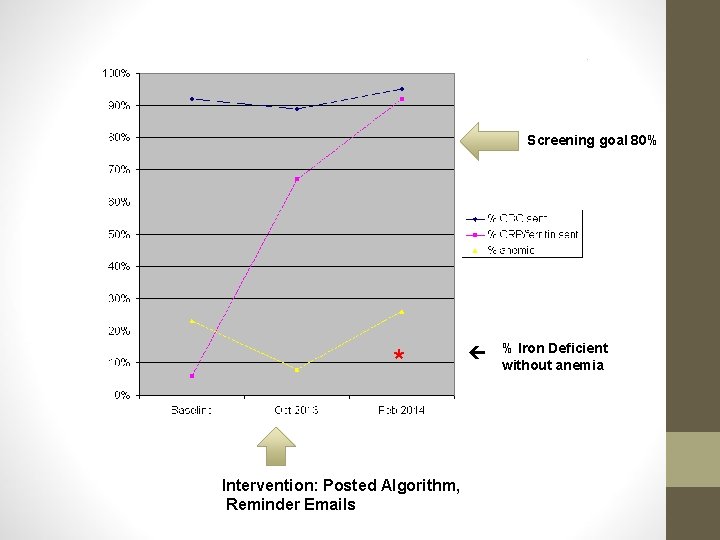
Screening goal 80% * Intervention: Posted Algorithm, Reminder Emails % Iron Deficient without anemia
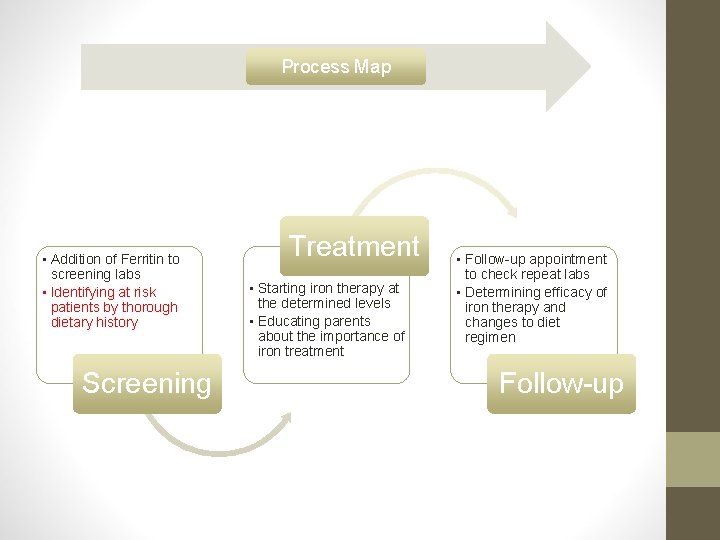
Process Map • Addition of Ferritin to screening labs • Identifying at risk patients by thorough dietary history Screening Treatment • Starting iron therapy at the determined levels • Educating parents about the importance of iron treatment • Follow-up appointment to check repeat labs • Determining efficacy of iron therapy and changes to diet regimen Follow-up
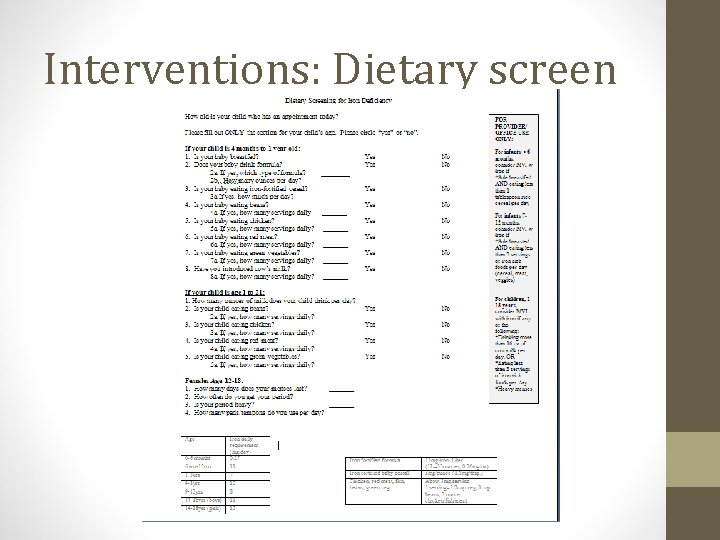
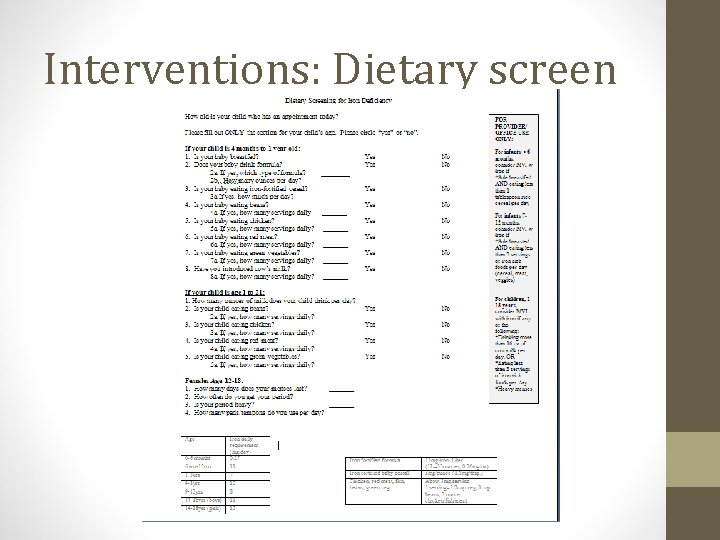
Interventions: Dietary screen
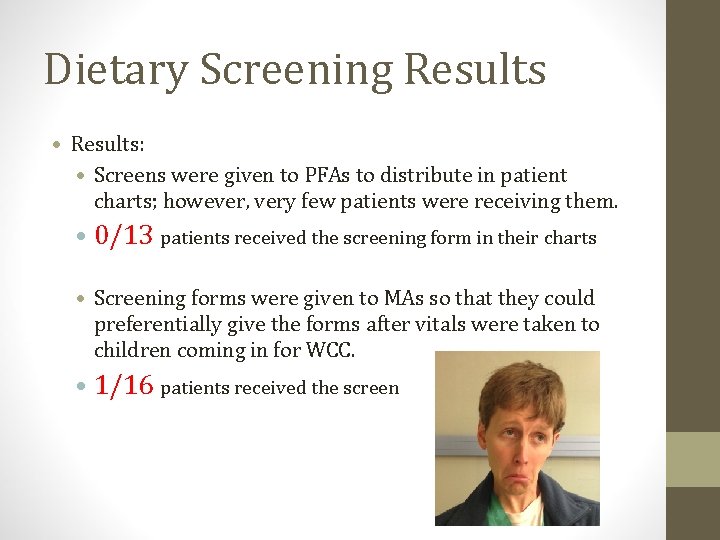
Dietary Screening Results • Results: • Screens were given to PFAs to distribute in patient charts; however, very few patients were receiving them. • 0/13 patients received the screening form in their charts • Screening forms were given to MAs so that they could preferentially give the forms after vitals were taken to children coming in for WCC. • 1/16 patients received the screen
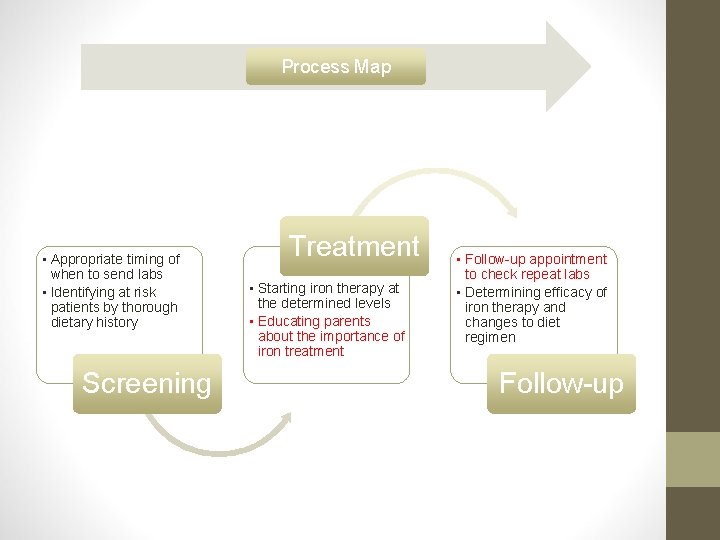
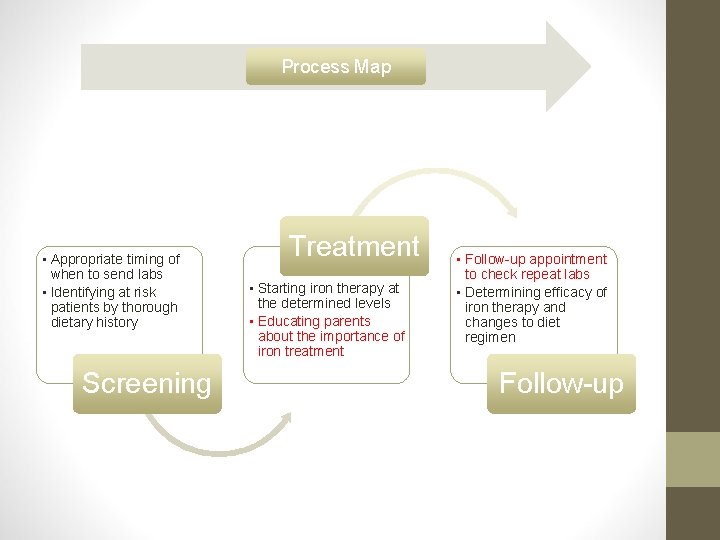
Process Map • Appropriate timing of when to send labs • Identifying at risk patients by thorough dietary history Screening Treatment • Starting iron therapy at the determined levels • Educating parents about the importance of iron treatment • Follow-up appointment to check repeat labs • Determining efficacy of iron therapy and changes to diet regimen Follow-up
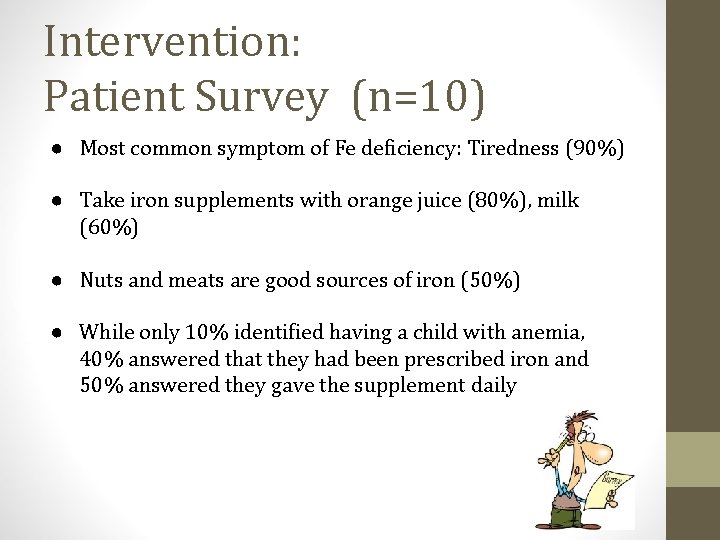
Intervention: Patient Survey (n=10) ● Most common symptom of Fe deficiency: Tiredness (90%) ● Take iron supplements with orange juice (80%), milk (60%) ● Nuts and meats are good sources of iron (50%) ● While only 10% identified having a child with anemia, 40% answered that they had been prescribed iron and 50% answered they gave the supplement daily
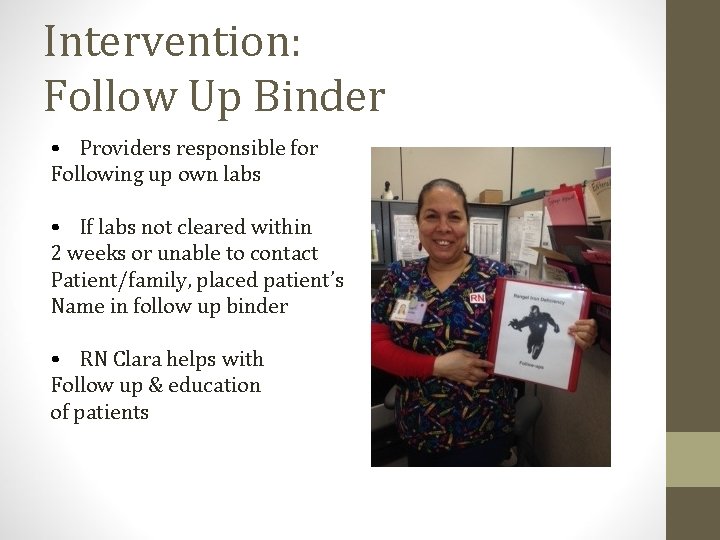
Intervention: Follow Up Binder • Providers responsible for Following up own labs • If labs not cleared within 2 weeks or unable to contact Patient/family, placed patient’s Name in follow up binder • RN Clara helps with Follow up & education of patients
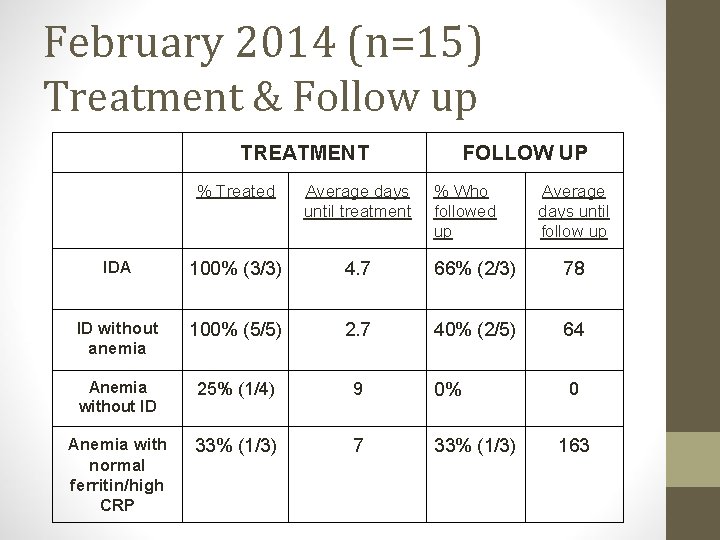
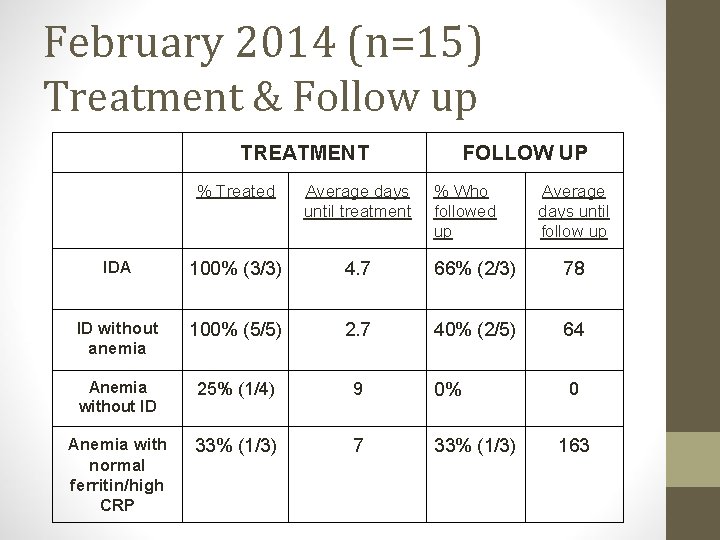
February 2014 (n=15) Treatment & Follow up TREATMENT FOLLOW UP % Treated Average days until treatment % Who followed up Average days until follow up IDA 100% (3/3) 4. 7 66% (2/3) 78 ID without anemia 100% (5/5) 2. 7 40% (2/5) 64 Anemia without ID 25% (1/4) 9 0% Anemia with normal ferritin/high CRP 33% (1/3) 7 33% (1/3) 0 163
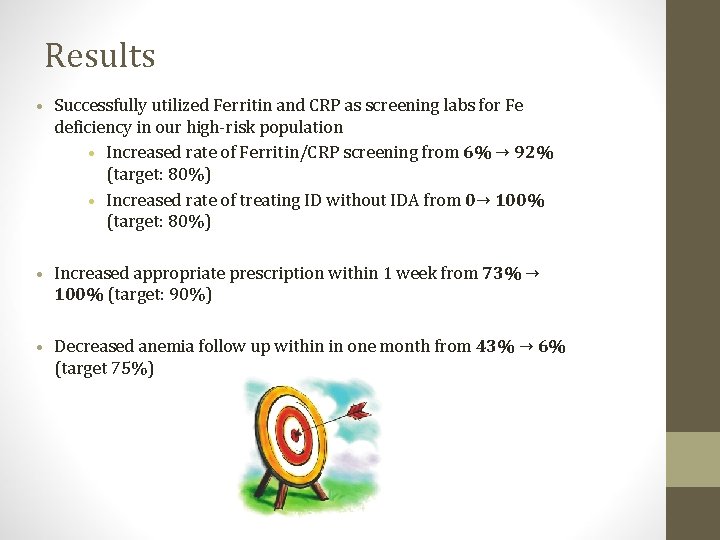
Results • Successfully utilized Ferritin and CRP as screening labs for Fe deficiency in our high-risk population • Increased rate of Ferritin/CRP screening from 6% → 92% (target: 80%) • Increased rate of treating ID without IDA from 0→ 100% (target: 80%) • Increased appropriate prescription within 1 week from 73% → 100% (target: 90%) • Decreased anemia follow up within in one month from 43% → 6% (target 75%)
Lessons We Learned…. • Barriers to Change • Screening tools hard to incorporate into work flow, Follow up hurdles, time (PDSA cycles) • Applicable to Other ACN Clinics? • YES! • Next Steps… • Patient Survey and Education, System changes to improve follow up, Other possible tests Thank You!!!