RANGE OF MOTION AFTER A LATERAL ANKLE RECONSTRUCTION
- Slides: 35
RANGE OF MOTION AFTER A LATERAL ANKLE RECONSTRUCTION Sam De. Alto September 26 th 2016 Clinical Problem Solving II
Objectives Describe patient management of the demographic of interest To examine the evidence on ankle mobilizations as an effective intervention for patients status post lateral ankle reconstruction in an orthopedic setting To evaluate the implementation of ankle mobilizations in an orthopedic setting
Patient X: 38 -year old Caucasian male PMH: Bilateral chronic ankle instability/sprains since 1994 (L > R) L lateral ankle reconstruction April 2016 Premorbid Status: Full time in Air-force Recreational soccer Current Status: Lives alone in apartment � MOI: traumatic fall while Not working in the Air-force Unable to play recreational soccer PT Diagnosis: Plans to go to school in Spain Pain in L ankle and joints of foot (5/10 at worst) � ADLs: standing, squatting, walking, climbing stairs
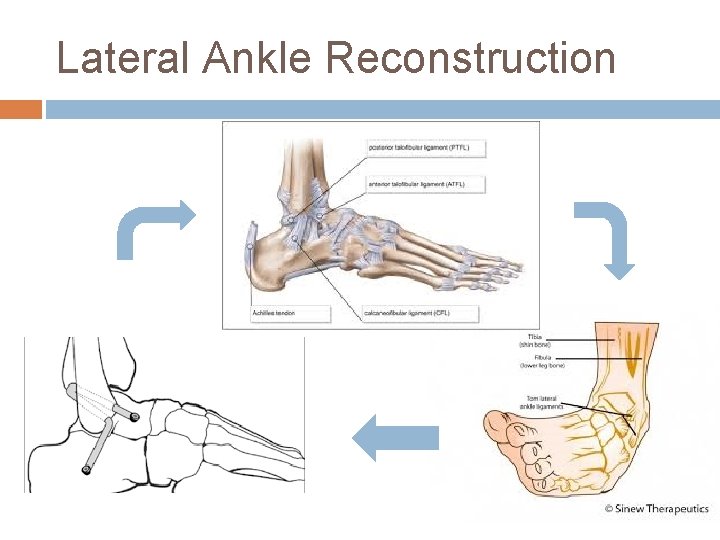
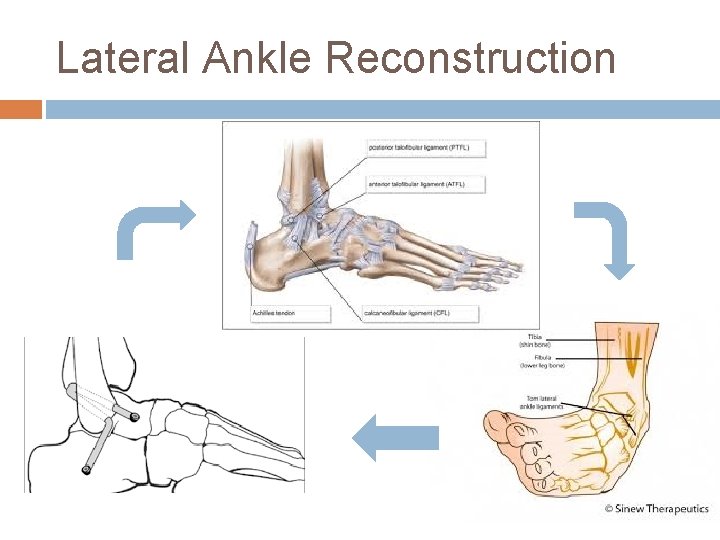
Lateral Ankle Reconstruction
PT Examination Integument Balance Functional Test: squat Gait ROM Strength FAAM ADL and Sport
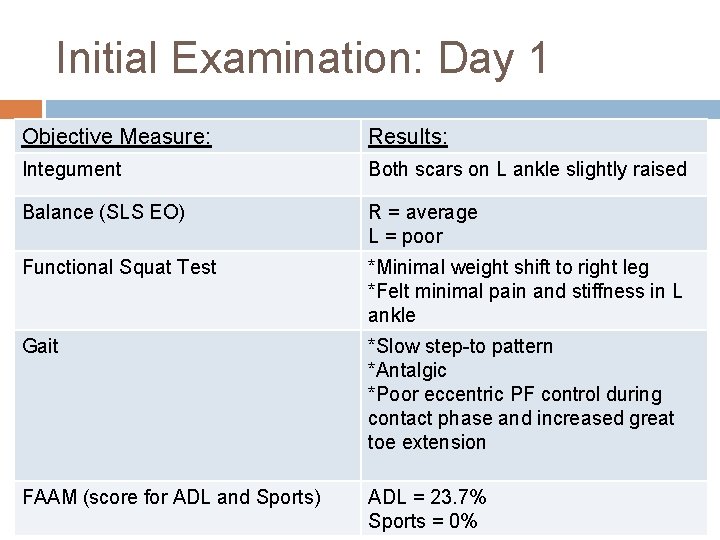
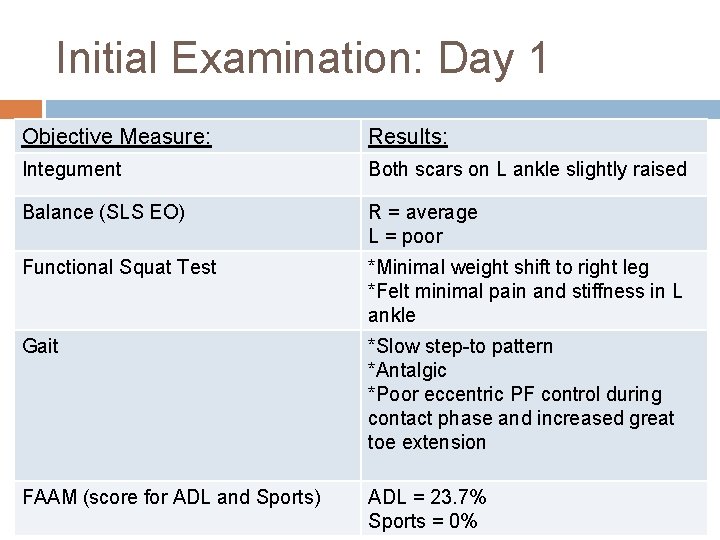
Initial Examination: Day 1 Objective Measure: Results: Integument Both scars on L ankle slightly raised Balance (SLS EO) R = average L = poor Functional Squat Test *Minimal weight shift to right leg *Felt minimal pain and stiffness in L ankle Gait *Slow step-to pattern *Antalgic *Poor eccentric PF control during contact phase and increased great toe extension FAAM (score for ADL and Sports) ADL = 23. 7% Sports = 0%
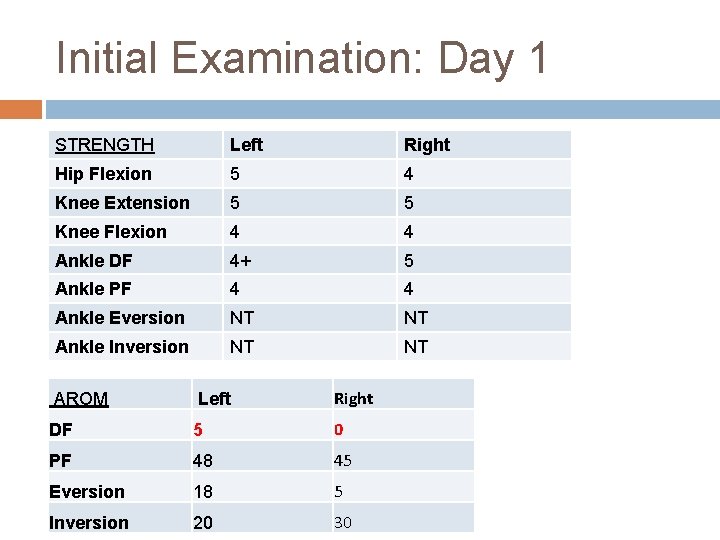
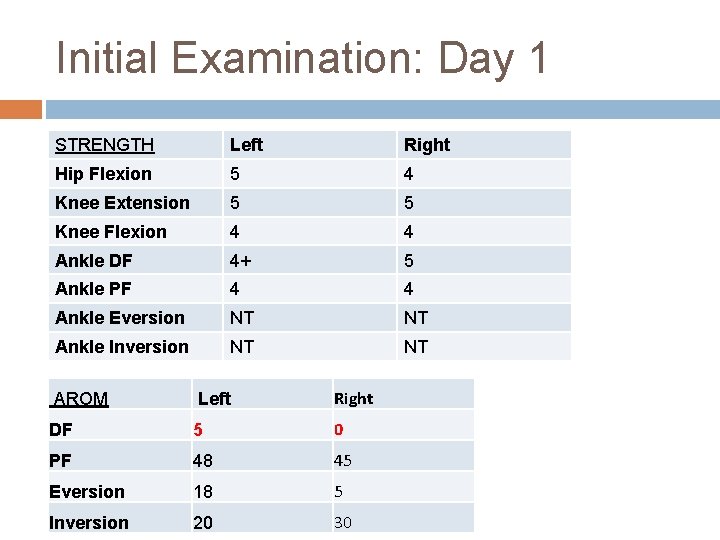
Initial Examination: Day 1 STRENGTH Left Right Hip Flexion 5 4 Knee Extension 5 5 Knee Flexion 4 4 Ankle DF 4+ 5 Ankle PF 4 4 Ankle Eversion NT NT Ankle Inversion NT NT AROM Left Right DF 5 0 PF 48 45 Eversion 18 5 Inversion 20 30
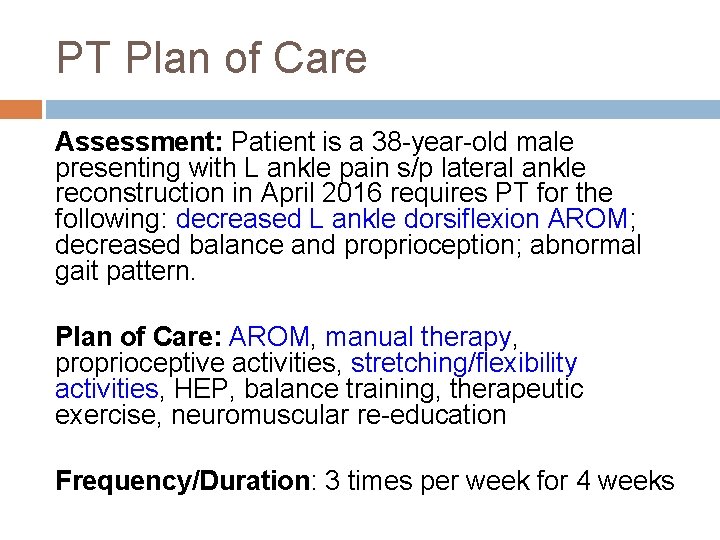
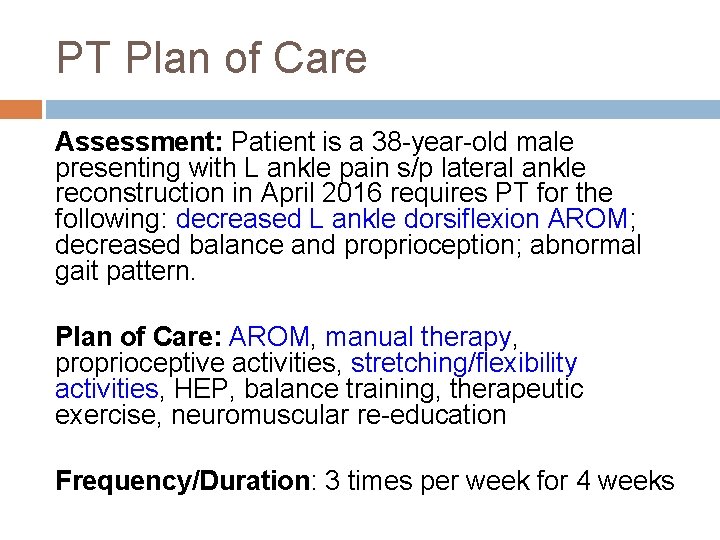
PT Plan of Care Assessment: Patient is a 38 -year-old male presenting with L ankle pain s/p lateral ankle reconstruction in April 2016 requires PT for the following: decreased L ankle dorsiflexion AROM; decreased balance and proprioception; abnormal gait pattern. Plan of Care: AROM, manual therapy, proprioceptive activities, stretching/flexibility activities, HEP, balance training, therapeutic exercise, neuromuscular re-education Frequency/Duration: 3 times per week for 4 weeks
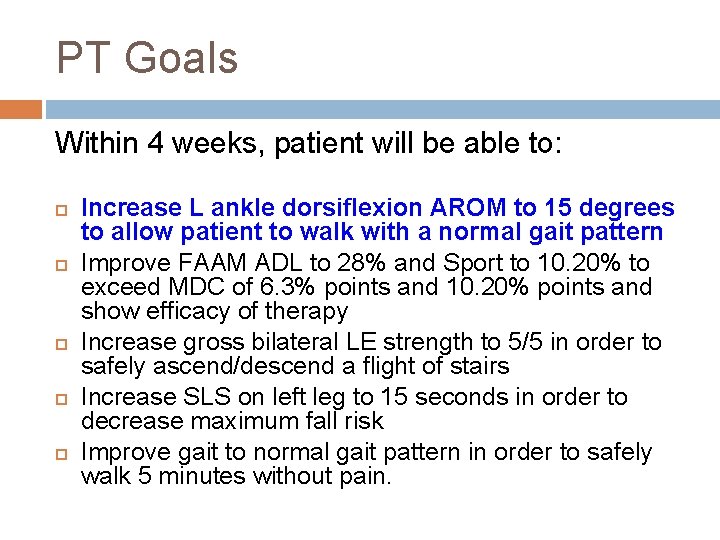
PT Goals Within 4 weeks, patient will be able to: Increase L ankle dorsiflexion AROM to 15 degrees to allow patient to walk with a normal gait pattern Improve FAAM ADL to 28% and Sport to 10. 20% to exceed MDC of 6. 3% points and 10. 20% points and show efficacy of therapy Increase gross bilateral LE strength to 5/5 in order to safely ascend/descend a flight of stairs Increase SLS on left leg to 15 seconds in order to decrease maximum fall risk Improve gait to normal gait pattern in order to safely walk 5 minutes without pain.
Clinical Question For a 38 -year-old male status-post lateral ankle reconstruction, is weight-bearing mobilization with movement an effective intervention for increasing ankle dorsiflexion range of motion?
Initial Changes in Posterior Talar Glide and Dorsiflexion of the Ankle after Mobilization with Movement in Individuals with Recurrent Ankle Sprain (Vicenzino, et al. 2006)
Vicenzino, et al. 2006 Study Design: Double blind, randomized crossover experimental study with repeated measures, including control group Purpose: Evaluate the initial effect of mobilization with movement (MWM) in weight-bearing and non-weight bearing on posterior talar glide and talocrural dorsiflexion in individuals with recurrent lateral ankle sprain
Vicenzino, et al. 2006 16 individuals: 8 female, 8 male Age: 18 to 27 Inclusion Criteria: History of recurrent lateral ankle sprains (2 -6) > 20 mm asymmetry on the Weight-bearing Lunge Test No history of lateral ankle sprain on the contralateral side Exclusion criteria: Acute ankle sprain within the past 6 months Previous injury or surgery to the back, hip, or knee or major injury or fracture to the ankle or distal leg
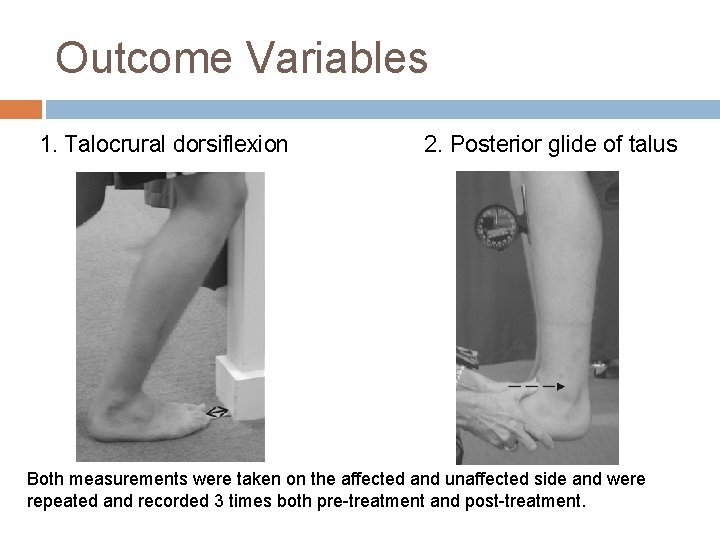
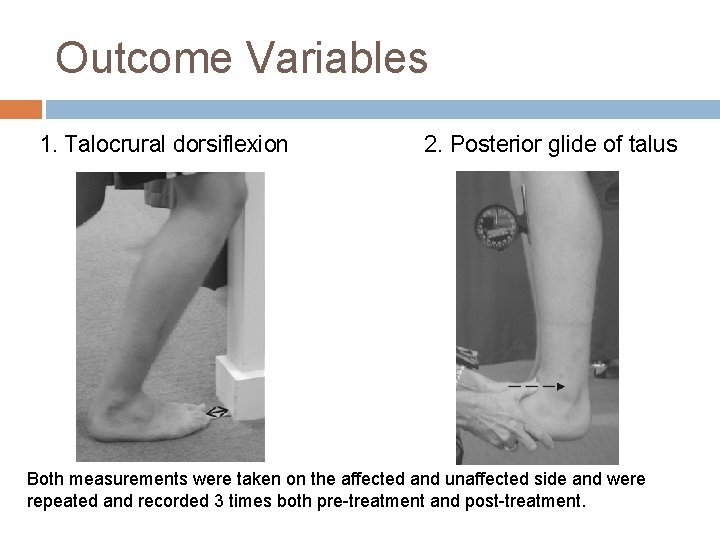
Outcome Variables 1. Talocrural dorsiflexion 2. Posterior glide of talus Both measurements were taken on the affected and unaffected side and were repeated and recorded 3 times both pre-treatment and post-treatment.
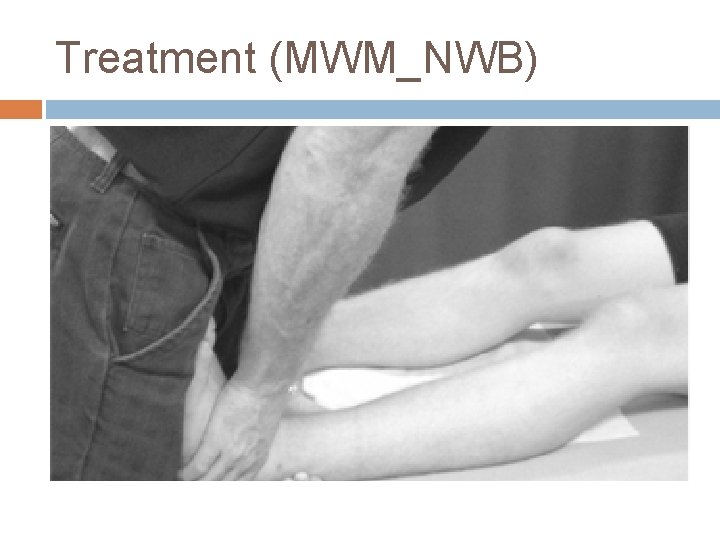
Treatment Groups Treatment sessions: 4 sets of 4 glides held for 10 seconds with 20 seconds rest period 1. Weight-Bearing MWM (MWM_WB) 2. Non-Weight-Bearing MWM (MWM_NWB) 3. No Treatment (control)
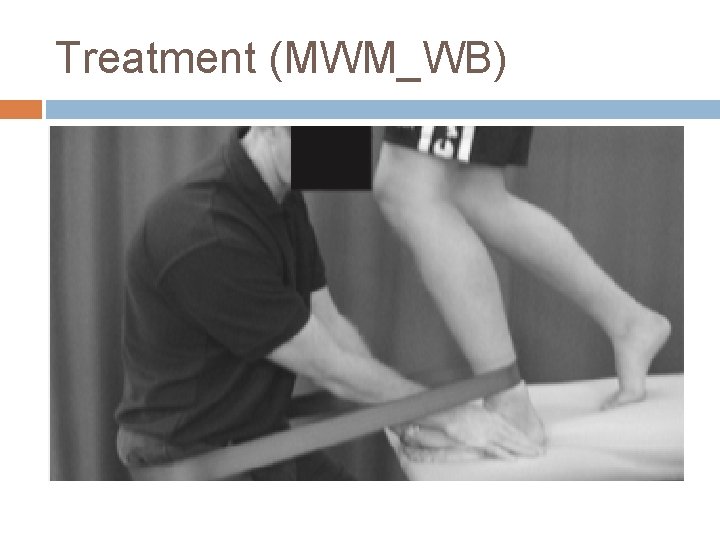
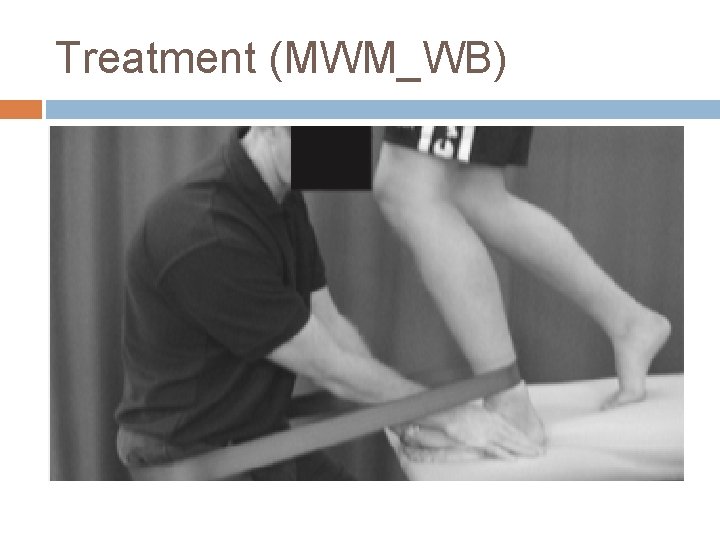
Treatment (MWM_WB)
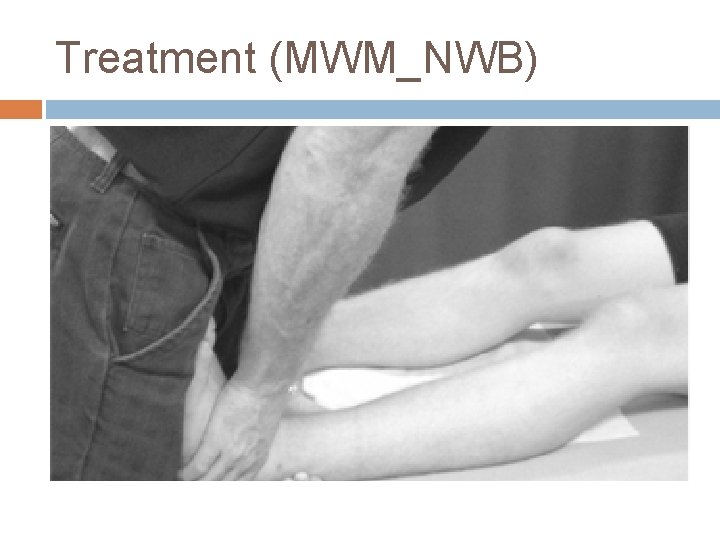
Treatment (MWM_NWB)
Conclusions Both MWM groups improved posterior talar glide and DF ROM immediately after application greater than that of the control group There is little difference in treatment effect between both MWM groups � MWM_WB joint may improve coupling at the talocrural
Limitations Small sample size (16 subjects) Only looked at immediate effects Measurement reliability � Validity of the assessment of the posterior talar glide Relevance to Patient X
Effects of Joint Mobilization on Chronic Ankle Instability: a Randomized Controlled Trial (Cruz-Diaz, et al. 2015)
Cruz-Diaz, et al. 2015 Study Design: Randomized clinical trial with control group Purpose: Evaluate short- and long-term effects of mobilization with movement in weight bearing on ankle dorsiflexion range of motion, dynamic postural control and self reported instability in individuals with chronic ankle instability
Subject Characteristics 81 subjects: 47 male, 34 female � Age: 20 to 34 � Inclusion criteria: History of ankle sprains on the same side in the last 2 years � Asymmetry > 2 cm on weight-bearing lunge test � Self-reported instability of “giving-way” � Not receiving any other PT treatment during the study � Exclusion criteria: � Acute ankle sprain within 6 months � History of bilateral ankle sprains � Bony injury associated with ankle sprain � Previous injury or surgery to back, hip or knee
Methods Outcomes Assessed: measured pre-treatment, after first session, 3 weeks and 6 months Weight Bearing Lunge Test to measure ankle DF � Cumberland Ankle Instability Tool (CAIT) to measure selfreported ankle instability � Star Excursion Balance Test (SEBT) to measure dynamic postural control � 3 Groups Tested: received 2 sessions/week for 3 weeks � Weight-bearing mobilization with movement (MWM_WB) � Sham treatment for placebo group � 2 sets of 10 repetitions with 2 minutes rest Same as MWM_WB Control group No treatment received
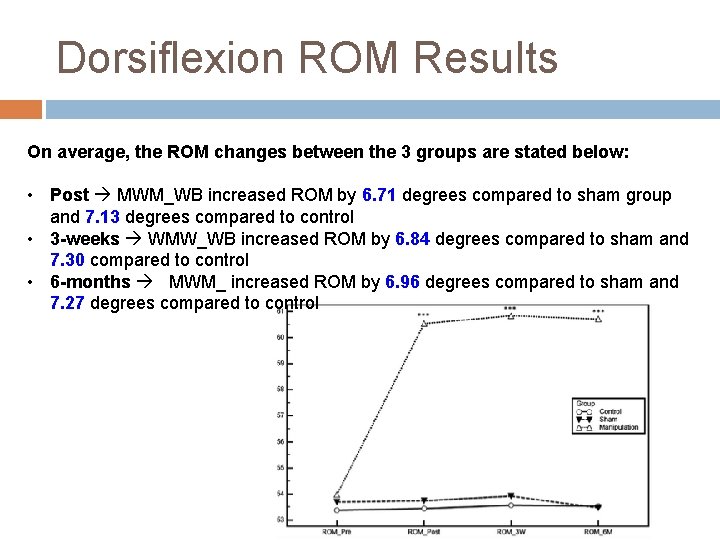
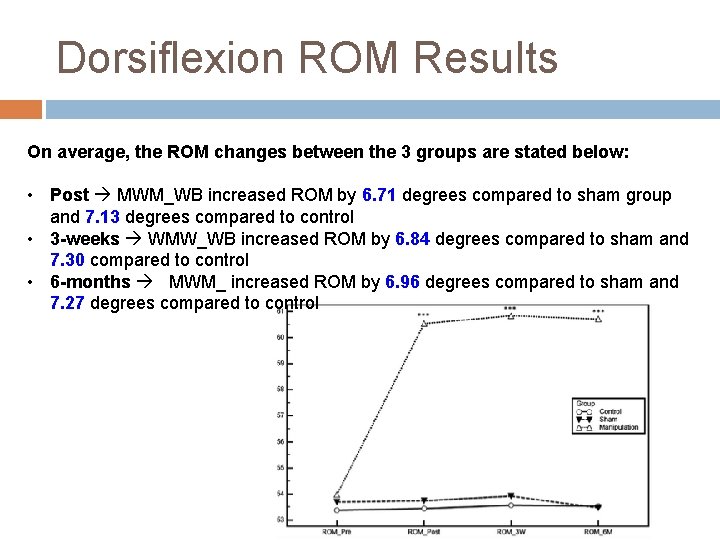
Dorsiflexion ROM Results On average, the ROM changes between the 3 groups are stated below: • Post MWM_WB increased ROM by 6. 71 degrees compared to sham group and 7. 13 degrees compared to control • 3 -weeks WMW_WB increased ROM by 6. 84 degrees compared to sham and 7. 30 compared to control • 6 -months MWM_ increased ROM by 6. 96 degrees compared to sham and 7. 27 degrees compared to control
CAIT and SEBT Results CAIT MWM_WB group showed a significant improvement in self-reported feeling of “giving way” after 3 -weeks while the sham and control maintained similar scores from baseline SEBT MWM_WB group showed greater significant improvements after 3 -weeks in all reach distances compared to the sham and control groups
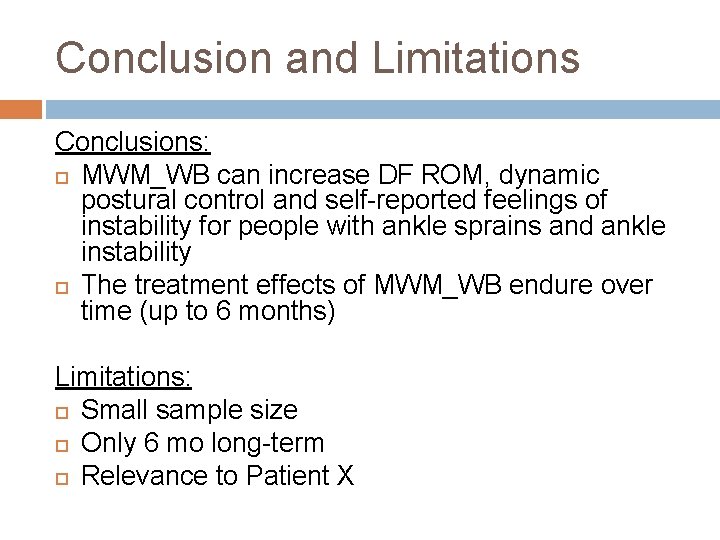
Conclusion and Limitations Conclusions: MWM_WB can increase DF ROM, dynamic postural control and self-reported feelings of instability for people with ankle sprains and ankle instability The treatment effects of MWM_WB endure over time (up to 6 months) Limitations: Small sample size Only 6 mo long-term Relevance to Patient X
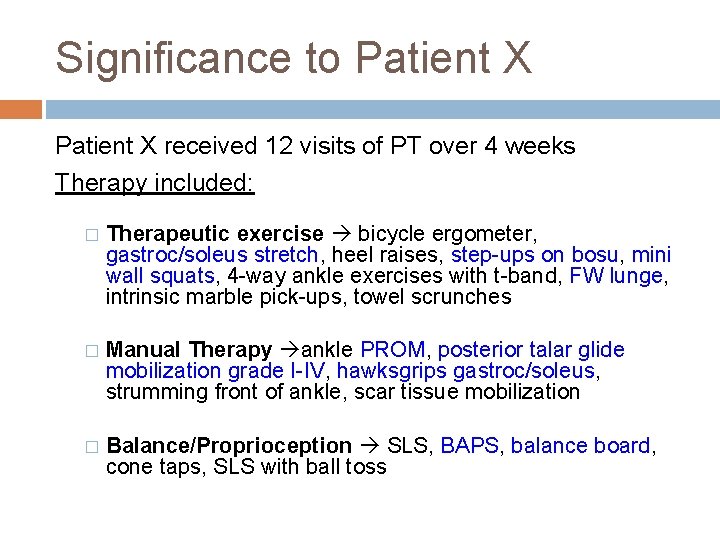
Significance to Patient X received 12 visits of PT over 4 weeks Therapy included: � Therapeutic exercise bicycle ergometer, gastroc/soleus stretch, heel raises, step-ups on bosu, mini wall squats, 4 -way ankle exercises with t-band, FW lunge, intrinsic marble pick-ups, towel scrunches � Manual Therapy ankle PROM, posterior talar glide mobilization grade I-IV, hawksgrips gastroc/soleus, strumming front of ankle, scar tissue mobilization � Balance/Proprioception SLS, BAPS, balance board, cone taps, SLS with ball toss
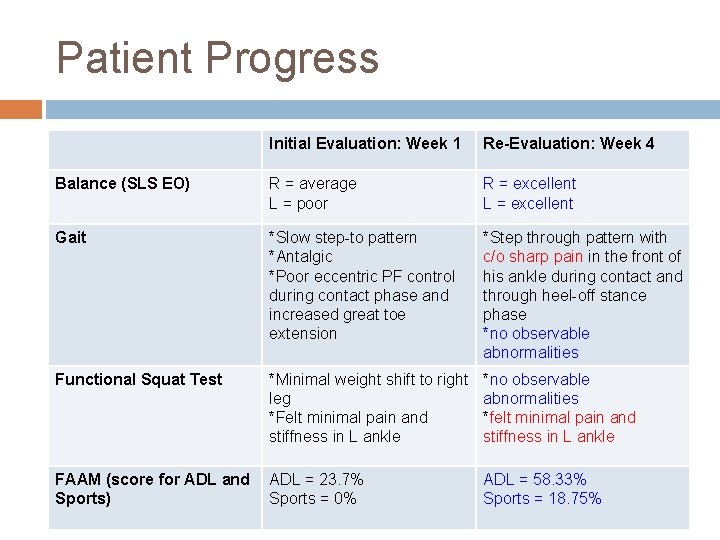
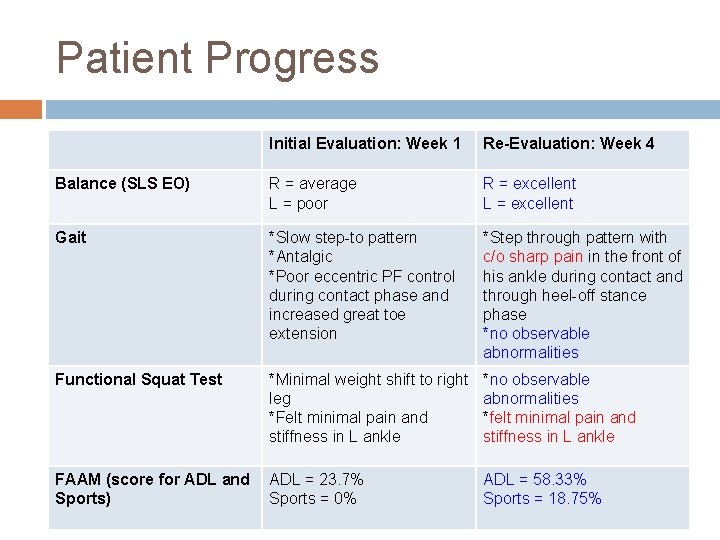
Patient Progress Initial Evaluation: Week 1 Re-Evaluation: Week 4 Balance (SLS EO) R = average L = poor R = excellent L = excellent Gait *Slow step-to pattern *Antalgic *Poor eccentric PF control during contact phase and increased great toe extension *Step through pattern with c/o sharp pain in the front of his ankle during contact and through heel-off stance phase *no observable abnormalities Functional Squat Test *Minimal weight shift to right leg *Felt minimal pain and stiffness in L ankle *no observable abnormalities *felt minimal pain and stiffness in L ankle FAAM (score for ADL and Sports) ADL = 23. 7% Sports = 0% ADL = 58. 33% Sports = 18. 75%
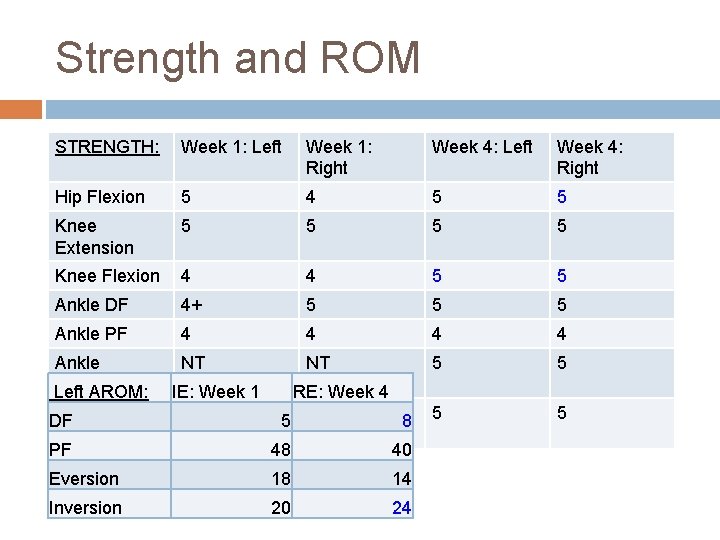
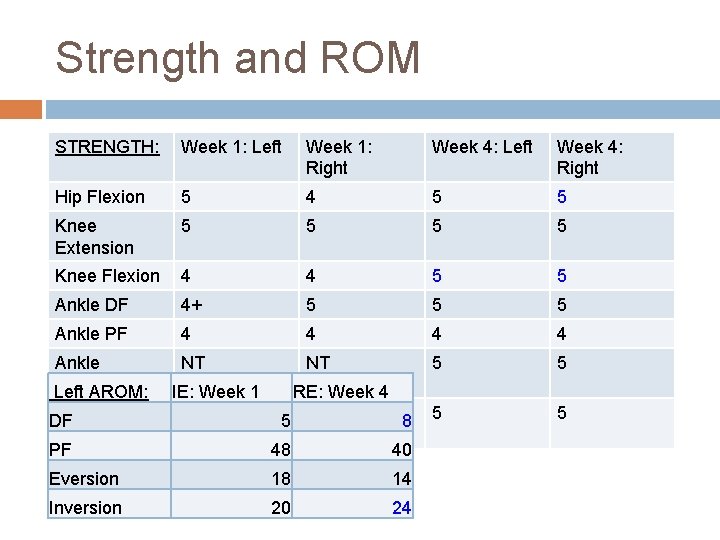
Strength and ROM STRENGTH: Week 1: Left Week 1: Right Week 4: Left Week 4: Right Hip Flexion 5 4 5 5 Knee Extension 5 5 Knee Flexion 4 4 5 5 Ankle DF 4+ 5 5 5 Ankle PF 4 4 Ankle Eversion Left AROM: NT NT 5 5 Ankle DF Inversion PF IE: Week 1 NT RE: Week 4 5 NT 8 48 40 Eversion 18 14 Inversion 20 24
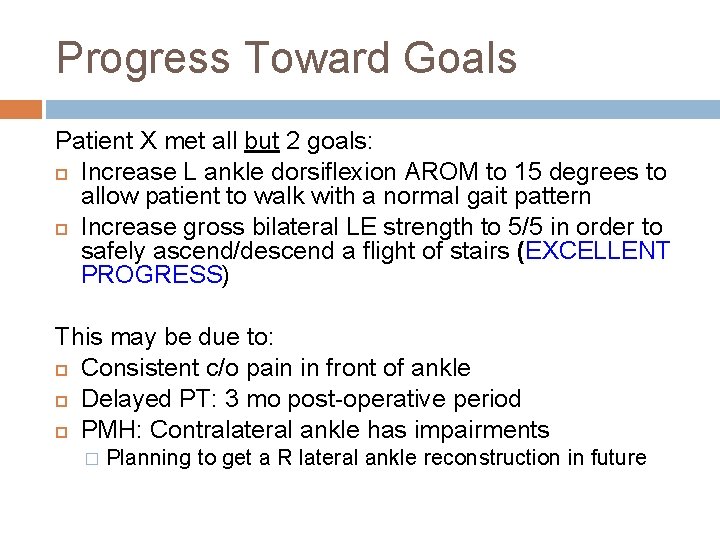
Progress Toward Goals Patient X met all but 2 goals: Increase L ankle dorsiflexion AROM to 15 degrees to allow patient to walk with a normal gait pattern Increase gross bilateral LE strength to 5/5 in order to safely ascend/descend a flight of stairs (EXCELLENT PROGRESS) This may be due to: Consistent c/o pain in front of ankle Delayed PT: 3 mo post-operative period PMH: Contralateral ankle has impairments � Planning to get a R lateral ankle reconstruction in future
Research Relevance to Patient X Hard to find studies with the following: � Lateral ankle reconstruction, bilateral ankle sprain, MWM_WB and ankle DF ROM Patient X did not perform MWM_WB but did perform posterior talar glides in supine as well as therapeutic exercise to increase DF
What would I do differently? After looking at the research, I would consider doing MWM_WB for patients s/p lateral ankle reconstruction based on the following: Surgeon protocol Patient impairments Lateral Ankle Reconstruction procedures and ROM � Modified Brostrom Evans Procedure – no significant difference in ROM b/t surgical side and non-surgical side
Overall Conclusion MWM_WB in order to increase ankle DF ROM in individuals s/p lateral ankle reconstruction is uncertain; HOWEVER, MWM_WB can increase ankle DF in patients with chronic ankle instability in short and long-term MWM_WB may be more effective functionally for patients with history of chronic ankle sprains More research needed to compare MWM_WB on bilateral chronic ankle instability and lateral ankle reconstruction More research needed to look at therapeutic exercise
Questions
References Cruz-Díaz, David, Rafael Lomas Vega, Maria Catalina Osuna-Pérez, Fidel Hita. Contreras, and Antonio Martínez-Amat. "Effects of Joint Mobilization on Chronic Ankle Instability: A Randomized Controlled Trial. " Disability and Rehabilitation 37. 7 (2014): 60110. Web. Hsu, A. R. , G. T. Ardoin, W. H. Davis, and R. B. Anderson. "Intermediate and Long-Term Outcomes of the Modified Brostrom-Evans Procedure for Lateral Ankle Ligament Reconstruction. " Foot & Ankle Specialist 9. 2 (2015): 131 -39. Web. "Lateral Ankle Sprain. " Related Keywords & Suggestions. N. p. , n. d. Web. 21 Sept. 2016. Schmidt, R. , E. Cordier, C. Bertsch, E. Eils, S. Neller, S. Benesch, A. Herbst, D. Rosenbaum, and L. Claes. "Reconstruction of the Lateral Ligaments: Do the Anatomical Procedures Restore Physiologic Ankle Kinematics? " Foot Ankle Int Foot & Ankle International 25. 1 (2004): 31 -36. Web. "Surgical Treatment of Chronic Ankle Lateral Instability: Reconstruction with Tenodesis or Tendon Graft. " Http: //dx. doi. org/10. 4055/jkoa. 2014. 49. 1. 22. N. p. , n. d. Web. 21 Sept. 2016. Vicenzino, Bill, Michelle Branjerdporn, Pam Teys, and Kate Jordan. "Initial Changes in Posterior Talar Glide and Dorsiflexion of the Ankle After Mobilization With Movement in Individuals with Recurrent Ankle Sprain. " J Orthop Sports Phys Ther Journal of Orthopaedic & Sports Physical Therapy 36. 7 (2006): 464 -71. Web