Randomized prospective evaluation of surgical trainees in warm


- Slides: 17
Randomized prospective evaluation of surgical trainees in 'warm up' simulations of laparoscopic ventral hernia repair Richardson, C MD, St. Hill, C MD, MSc, Baynosa, J MD, Bregg, J MD, Cassinelli, S, Chino, J, Tsuda, S MD Department of Surgery University of Nevada School of Medicine
Introduction • The effective training of surgical residents in operative techniques requires that residents have repeated experience performing the involved maneuvers on multiple occasions • Optimally, this experience is gained and techniques are mastered in a controlled setting prior to being performed on patients • Any method which enhances the resident competence prior to undertaking surgical procedures in patients would therefore be of value
Introduction • Laparoscopic ventral hernia repair is particularly difficult for novice surgeons, given that the camera angle relative to movement of the instruments can often be counter-intuitive and fine motor control is essential in performing an adequate repair • We postulated that having novice surgical trainees perform a specific set of “warm-up” exercises immediately prior to these procedures will result in better performances during live surgery
Methods • Novice surgical trainees (PGY 1 and 2, 4 th year med students) were randomized into test and control groups • All participants were given an instructional session about the technical aspects of the procedure to be performed – Session included an explanation of the procedure, use of instruments, introduction to mesh, and video demonstration
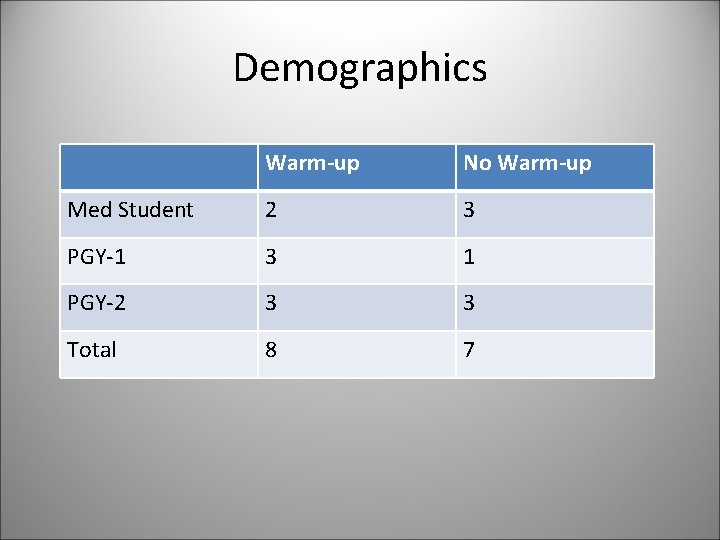
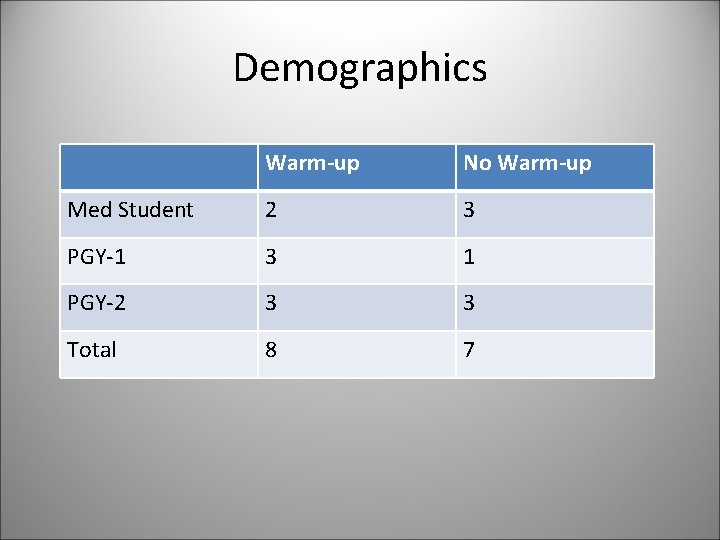
Demographics Warm-up No Warm-up Med Student 2 3 PGY-1 3 1 PGY-2 3 3 Total 8 7

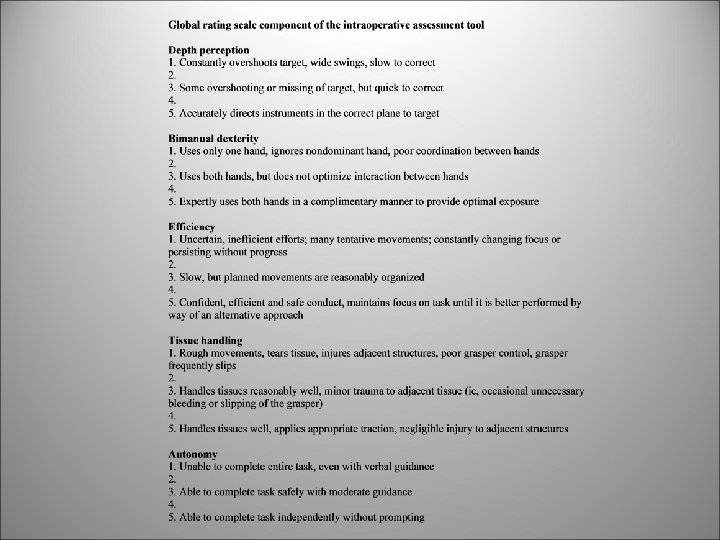
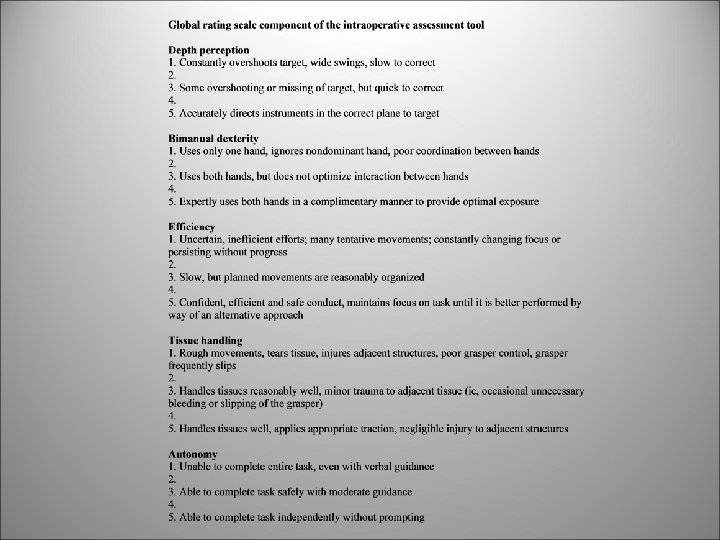
Methods • The control group then proceeded to the live animal lab where they performed the assigned tasks and were timed and scored using the Global Operative Assessment of Laparoscopic Skills (GOALS) rating scale as well as a novel checklist specific to the laparoscopic ventral hernia exercise
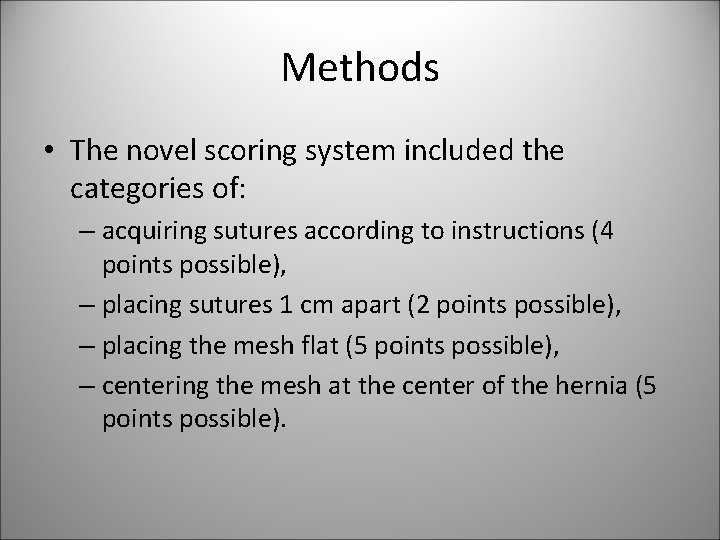
Methods • The novel scoring system included the categories of: – acquiring sutures according to instructions (4 points possible), – placing sutures 1 cm apart (2 points possible), – placing the mesh flat (5 points possible), – centering the mesh at the center of the hernia (5 points possible).

Methods • The test group completed a specific warm-up routine designed to practice the more technically difficult aspects of a lap ventral hernia repair on teaching models in a dry lab before proceeding to the live animal lab • They were then timed and scored in the same manner as the control group • All participants completed a self-assessment survey at the conclusion of the exercise
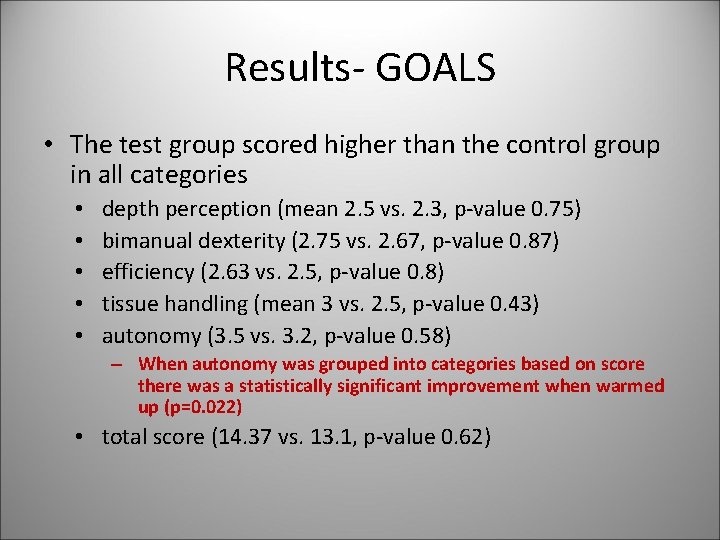
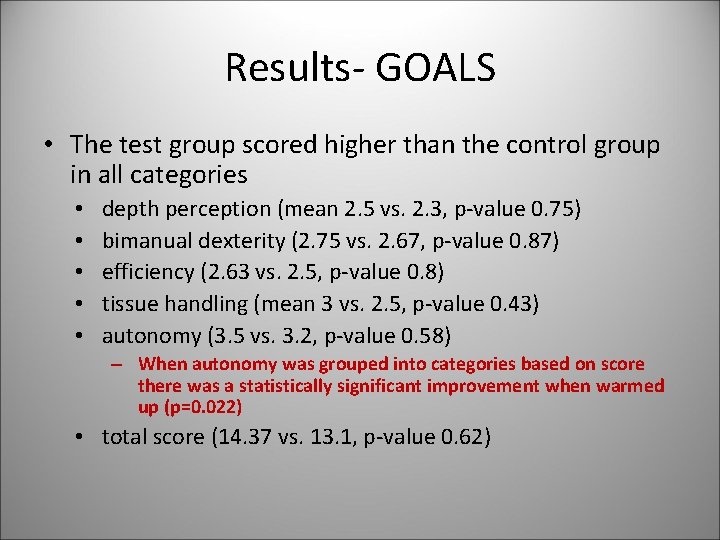
Results- GOALS • The test group scored higher than the control group in all categories • • • depth perception (mean 2. 5 vs. 2. 3, p-value 0. 75) bimanual dexterity (2. 75 vs. 2. 67, p-value 0. 87) efficiency (2. 63 vs. 2. 5, p-value 0. 8) tissue handling (mean 3 vs. 2. 5, p-value 0. 43) autonomy (3. 5 vs. 3. 2, p-value 0. 58) – When autonomy was grouped into categories based on score there was a statistically significant improvement when warmed up (p=0. 022) • total score (14. 37 vs. 13. 1, p-value 0. 62)
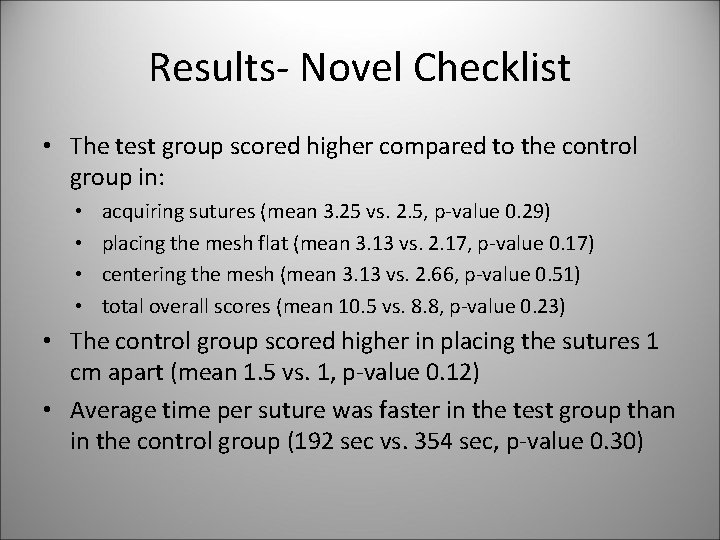
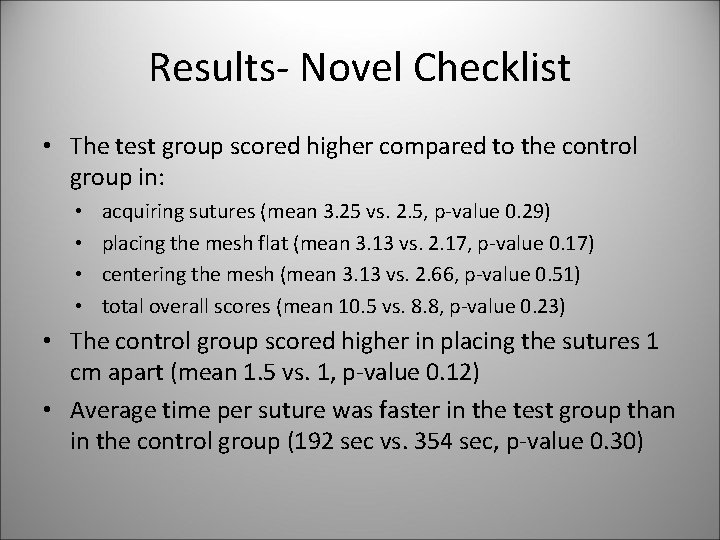
Results- Novel Checklist • The test group scored higher compared to the control group in: • • acquiring sutures (mean 3. 25 vs. 2. 5, p-value 0. 29) placing the mesh flat (mean 3. 13 vs. 2. 17, p-value 0. 17) centering the mesh (mean 3. 13 vs. 2. 66, p-value 0. 51) total overall scores (mean 10. 5 vs. 8. 8, p-value 0. 23) • The control group scored higher in placing the sutures 1 cm apart (mean 1. 5 vs. 1, p-value 0. 12) • Average time per suture was faster in the test group than in the control group (192 sec vs. 354 sec, p-value 0. 30)
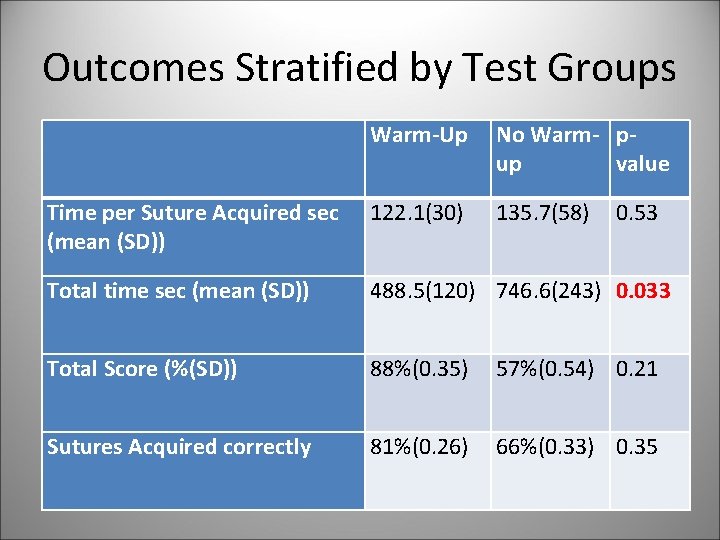
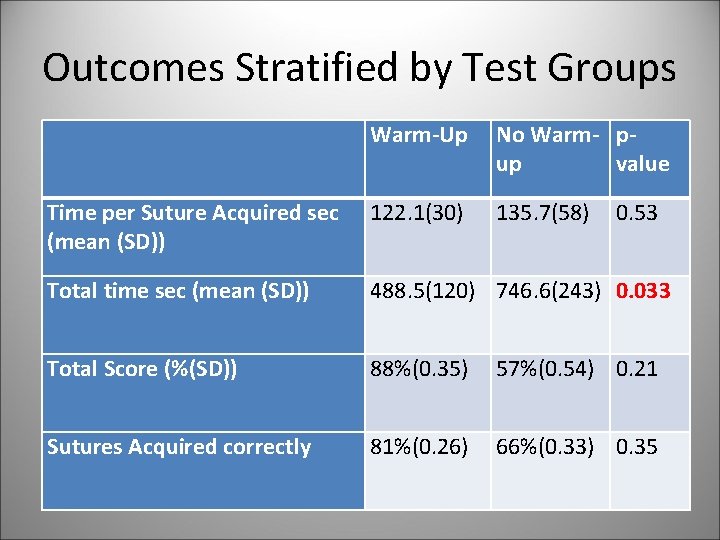
Outcomes Stratified by Test Groups Warm-Up No Warm- pup value Time per Suture Acquired sec (mean (SD)) 122. 1(30) 135. 7(58) Total time sec (mean (SD)) 488. 5(120) 746. 6(243) 0. 033 Total Score (%(SD)) 88%(0. 35) 57%(0. 54) 0. 21 Sutures Acquired correctly 81%(0. 26) 66%(0. 33) 0. 35 0. 53
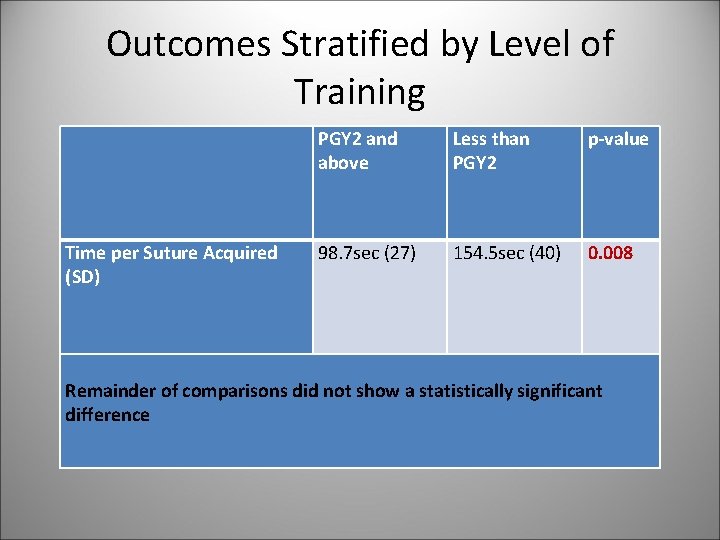
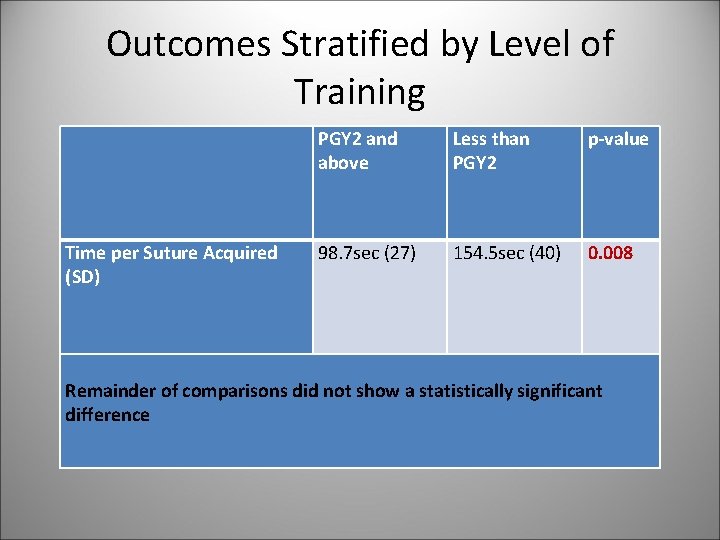
Outcomes Stratified by Level of Training PGY 2 and above Less than PGY 2 p-value Time per Suture Acquired (SD) 98. 7 sec (27) 154. 5 sec (40) 0. 008 Remainder of comparisons did not show a statistically significant difference
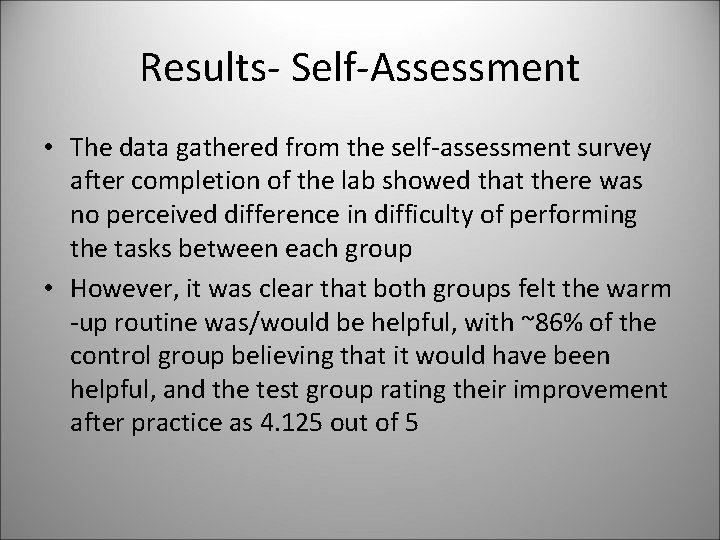
Results- Self-Assessment • The data gathered from the self-assessment survey after completion of the lab showed that there was no perceived difference in difficulty of performing the tasks between each group • However, it was clear that both groups felt the warm -up routine was/would be helpful, with ~86% of the control group believing that it would have been helpful, and the test group rating their improvement after practice as 4. 125 out of 5
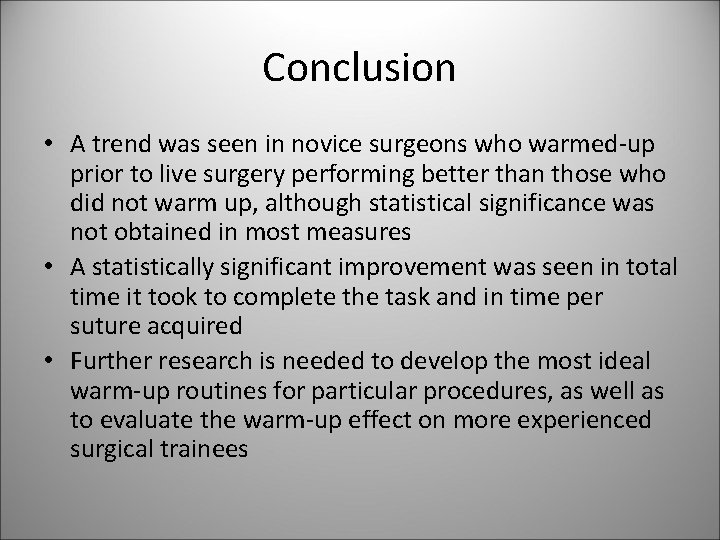
Conclusion • A trend was seen in novice surgeons who warmed-up prior to live surgery performing better than those who did not warm up, although statistical significance was not obtained in most measures • A statistically significant improvement was seen in total time it took to complete the task and in time per suture acquired • Further research is needed to develop the most ideal warm-up routines for particular procedures, as well as to evaluate the warm-up effect on more experienced surgical trainees