Randomized Clinical Trials in Rheumatology Reporting Safety and















- Slides: 61
Randomized Clinical Trials in Rheumatology: Reporting Safety and Outcome Measures Yusuf Yazıcı, MD Assistant Professor of Medicine, NYU School of Medicine Director, Seligman Center for Advanced Therapeutics NYU Hospital for Joint Diseases 1
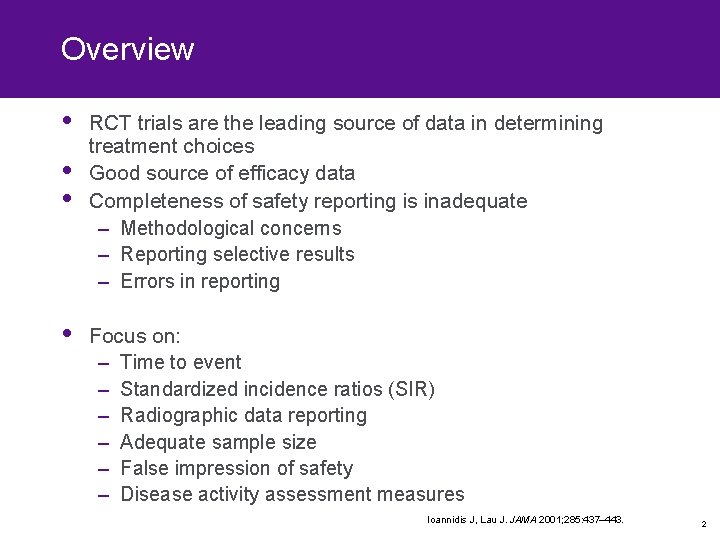
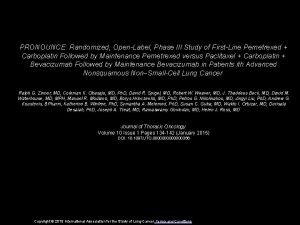
Overview • • RCT trials are the leading source of data in determining treatment choices Good source of efficacy data Completeness of safety reporting is inadequate – Methodological concerns – Reporting selective results – Errors in reporting Focus on: – Time to event – Standardized incidence ratios (SIR) – Radiographic data reporting – Adequate sample size – False impression of safety – Disease activity assessment measures Ioannidis J, Lau J. JAMA 2001; 285: 437– 443. 2
Time to adverse event 3
Time to adverse event • Problem in reporting AEs in RCT • Time to event – Clue to causality – When to expect AEs in clinical care • Instantaneous risk might be different for drugs, but the cumulative risk will be similar • ‘Average risk’ does not reflect the true risk faced by patients, especially when decisions are being made at the beginning of treatment 4

Risk of adverse effects related to drug exposure Collet JP, Bolvin JF. In: Pharmacoepidemiology, 3 rd Edn, Strom BL ed. 2000. 5
TNF inhibitors and lymphomas • An increased frequency of lymphomas, tuberculosis and demyelinating CNS disease has been associated TNF inhibitor use • SEER database • Based on annual incidence in the population, which is expected to be evenly distributed • If there is some skewing as to time of malignancies in the treatment arm, this would make comparisons based on an annual incidence inaccurate 1. Brown SL, et al. Arthritis Rheum 2002; 3151– 3158. 2. Yazici Y, Yazici H. Arthritis Rheum 2004; 50: S 302 6
TNF inhibitors and lymphomas • TNF inhibitor use and lymphoma development, as reported to the Federal Drug Administration (FDA)1 • Twenty-six lymphomas – Fourteen occurred within 2 months of use • Non-Hodgkin’s lymphoma (NHL) – Two-monthly incidence in normal population 3/100, 000 – Ten out of 16 occurred in 2 months 2 – Two-monthly NHL occurrence in etanercept users =10/100, 000 • Nearly 3 -4 times 1. Brown SL, et al. Arthritis Rheum 2002; 46: 3151– 3158; 2. Yazici H. Arthritis Rheum 2003; 48: 2389. 7
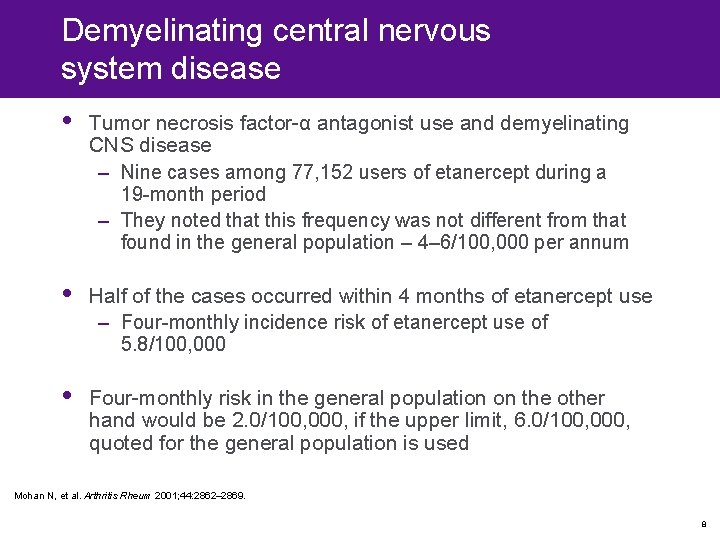
Demyelinating central nervous system disease • Tumor necrosis factor-α antagonist use and demyelinating CNS disease – Nine cases among 77, 152 users of etanercept during a 19 -month period – They noted that this frequency was not different from that found in the general population – 4– 6/100, 000 per annum • Half of the cases occurred within 4 months of etanercept use – Four-monthly incidence risk of etanercept use of 5. 8/100, 000 • Four-monthly risk in the general population on the other hand would be 2. 0/100, 000, if the upper limit, 6. 0/100, 000, quoted for the general population is used Mohan N, et al. Arthritis Rheum 2001; 44: 2862– 2869. 8

Coccidioidomycosis and TNF inhibitors • Risk of coccidioidomycosis in patients treated with TNF-α antagonists • Thirteen cases of coccidioidomycosis associated with TNF-α therapy were reported • Again seven out of 13 cases developed within 2 months of starting TNF-α therapy Bergstrom L, et al. Arthritis Rheum 2004; 50: 1959– 1966. 9
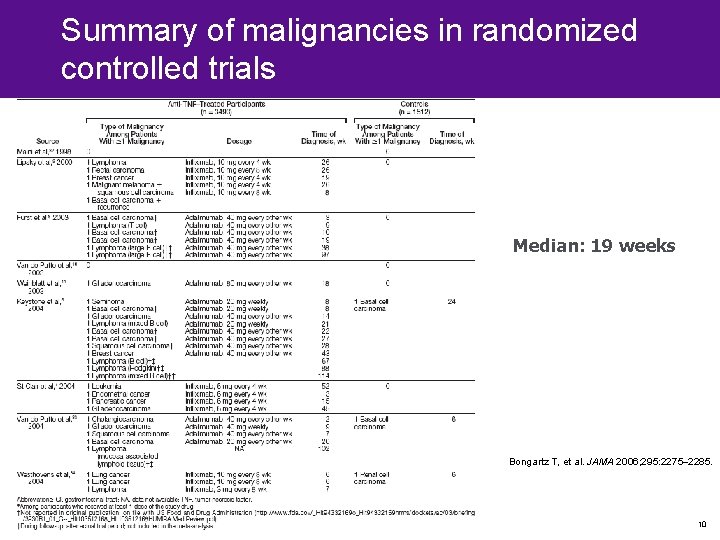
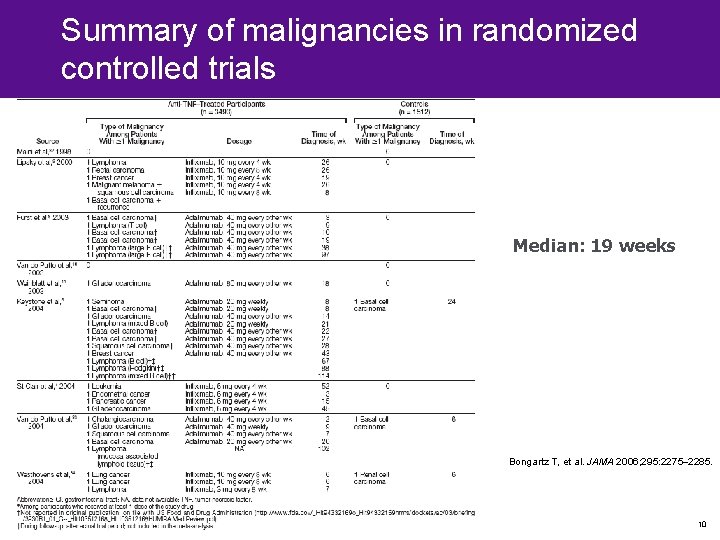
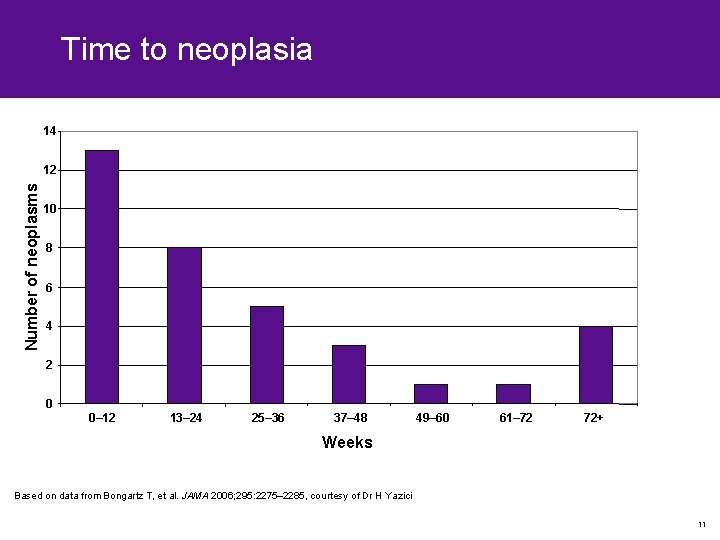
Summary of malignancies in randomized controlled trials Median: 19 weeks Bongartz T, et al. JAMA 2006; 295: 2275– 2285. 10
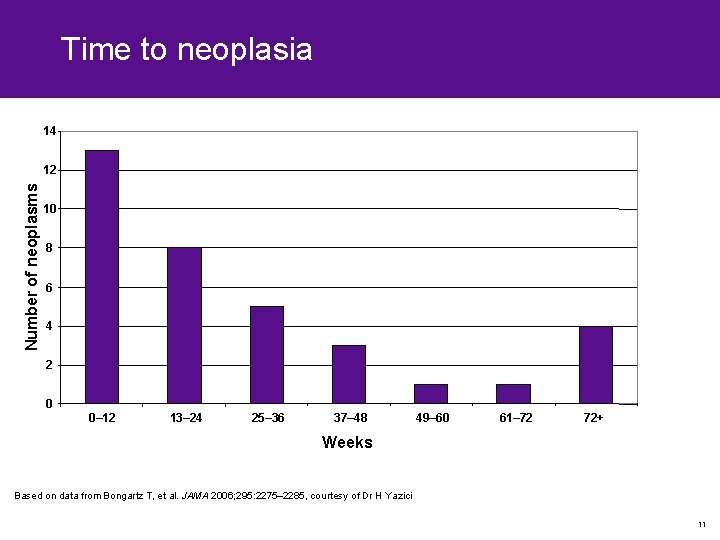
Time to neoplasia 14 Number of neoplasms 12 10 8 6 4 2 0 0– 12 13– 24 25– 36 37– 48 49– 60 61– 72 72+ Weeks Based on data from Bongartz T, et al. JAMA 2006; 295: 2275– 2285, courtesy of Dr H Yazici 11
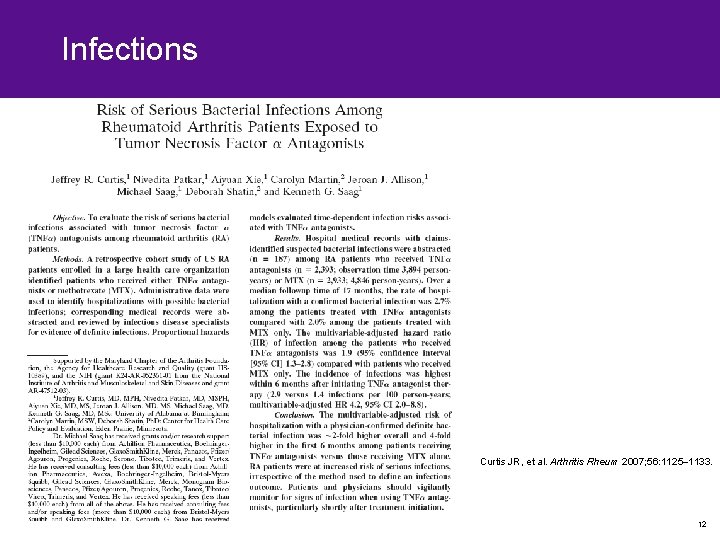
Infections Curtis JR, et al. Arthritis Rheum 2007; 56: 1125– 1133. 12
Infections • Hospital medical records with claims database reviewed – Median follow up of 17 months • Tumor necrosis factor-based treatment compared with MTX (or other DMARD-based) treatment • Reviewed 187 out of 217 suspected bacterial infections – TNF-α antagonist =65 in 2393 exposed persons (2. 7%) – DMARD =58 in 2933 exposed persons (2. 0%) – Number needed to harm =143 – Median time from exposure to medication to infection was <30 days for both groups – 93% occurred in 90 days • Multivariable adjustment approximately two times in TNF-α versus MTX Curtis JR, et al. Arthritis Rheum 2007; 56: 1125– 1133. 13

Increased early risk • In the first 6 months – Thirty-two infections in TNF-α cohort – Nineteen infections in DMARD cohort • Adjusted hazard ratio of infection in the first 6 months after start of treatment – TNF-α compared with MTX controls was 4. 2 (95% confidence intervals [CI] 2. 0 -88. 8) • Similar to JAMA paper Curtis JR, et al. Arthritis Rheum 2007; 56: 1125– 1133. 14
Surveillance, epidemiology and end-results database (SEER) • If timing of a malignancy is not evenly distributed, we should not be using a yearly rate to compare incidence rates – SEER = 12 expected lymphomas in RA patients over 12 months, 1 per month – TNF-α = 12 seen in RCT • Conclusion is that there is no difference • TNF-α lymphoma – Eight in the first 4 months = 2/month – Four in the last 8 months = 0. 5/month • In the case of lymphoma development – Using annual incidence risk in the general population as a comparator is inappropriate – Development of such lymphomas within the few months after drug initiation in more than 50% of these patients 1 • The expected random occurrence of lymphomas in the general population would make the real risk look smaller 2 15

Tumor necrosis factor, time to AE • As more than half of these cases occur during the first months of therapy, quarterly or monthly (rather than annual) incidence risks in the normal population should be used for comparison • Increased incidence risks for TNF-α antagonist-related adverse events (AEs) would necessitate a reexamination of the screening protocols and patient selection criteria used for these therapies • Does not carry the same message for the practicing physician • Variable period comparison needs to be used – 2 -, 3 -, 4 -, 6 -monthly rates • Excluding events in the first 60– 180 days – Not done with other AEs – No strong evidence base for doing so 16

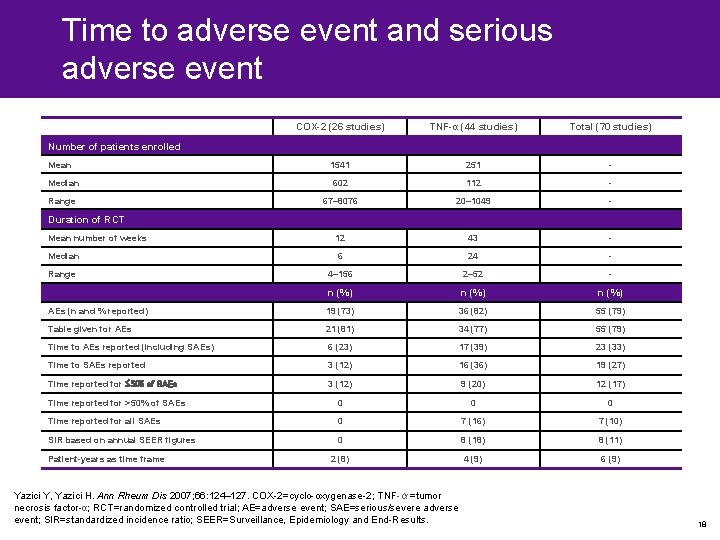
Time to adverse event reporting in randomized controlled trials • All RCT of cyclo-oxygenase-2 (COX-2) inhibitors and TNF-α inhibitors – Industry-sponsored RCTs (91%) – One-third gave time to AE in the report either as a table, text or Kaplan-Meier curve – No better reporting for serious adverse event (SAE) • Eight out of 17 RA–TNF-α trials reporting malignancy used the Surveillance, Epidemiology and End Results (SEER) database Yazici Y, Yazici H. Ann Rheum Dis 2007; 66: 124– 127. 17
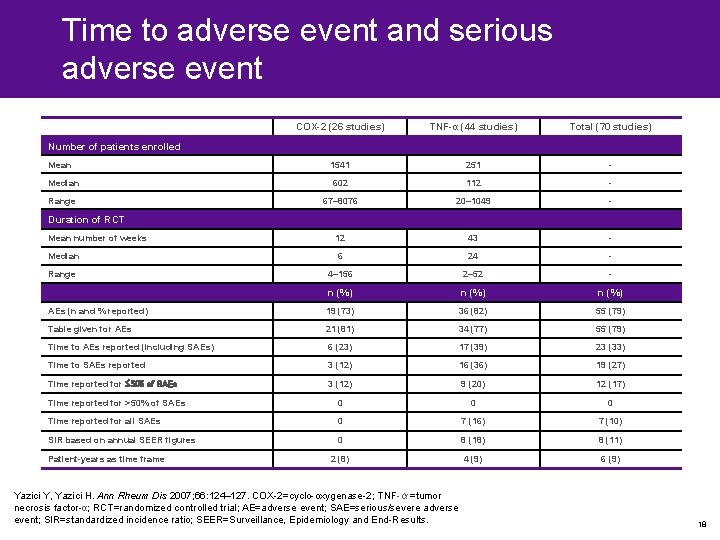
Time to adverse event and serious adverse event COX-2 (26 studies) TNF-α (44 studies) Total (70 studies) Mean 1541 251 - Median 602 112 - Range 67– 8076 20– 1049 - Mean number of weeks 12 43 - Median 6 24 - Range 4– 156 2– 52 - n (%) AEs (n and % reported) 19 (73) 36 (82) 55 (79) Table given for AEs 21 (81) 34 (77) 55 (79) Time to AEs reported (including SAEs) 6 (23) 17 (39) 23 (33) Time to SAEs reported 3 (12) 16 (36) 19 (27) Time reported for 50% of SAEs 3 (12) 9 (20) 12 (17) Time reported for >50% of SAEs 0 0 0 Time reported for all SAEs 0 7 (16) 7 (10) SIR based on annual SEER figures 0 8 (18) 8 (11) 2 (8) 4 (9) 6 (9) Number of patients enrolled Duration of RCT Patient-years as time frame Yazici Y, Yazici H. Ann Rheum Dis 2007; 66: 124– 127. COX-2=cyclo-oxygenase-2; TNF-α=tumor necrosis factor-α; RCT=randomized controlled trial; AE=adverse event; SAE=serious/severe adverse event; SIR=standardized incidence ratio; SEER=Surveillance, Epidemiology and End-Results. 18
Patient years 19
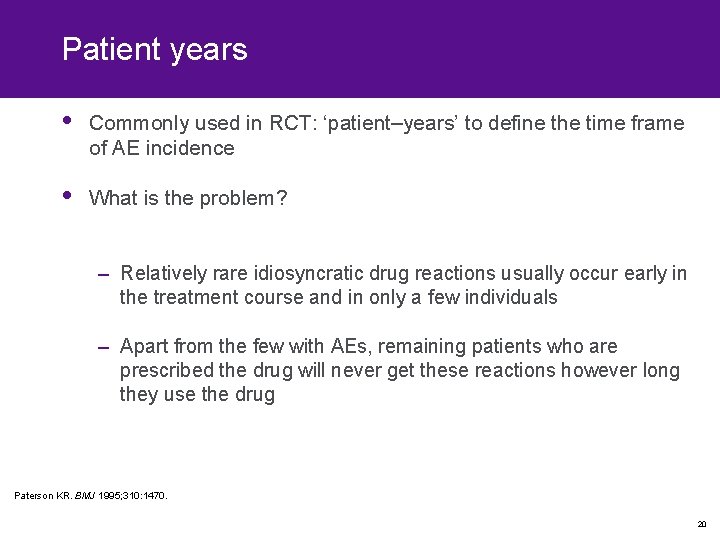
Patient years • Commonly used in RCT: ‘patient–years’ to define the time frame of AE incidence • What is the problem? – Relatively rare idiosyncratic drug reactions usually occur early in the treatment course and in only a few individuals – Apart from the few with AEs, remaining patients who are prescribed the drug will never get these reactions however long they use the drug Paterson KR. BMJ 1995; 310: 1470. 20
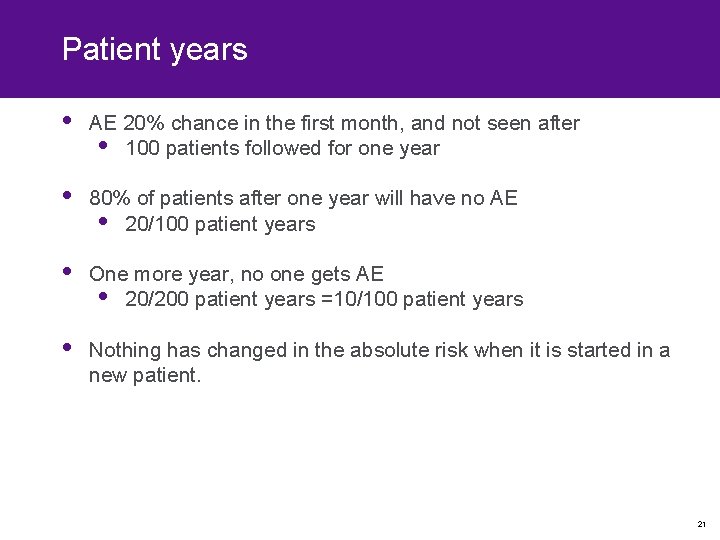
Patient years • AE 20% chance in the first month, and not seen after • 100 patients followed for one year • 80% of patients after one year will have no AE • 20/100 patient years • One more year, no one gets AE • 20/200 patient years =10/100 patient years • Nothing has changed in the absolute risk when it is started in a new patient. 21

Patient years (2) • Unduly inflate the denominator of the related incidence ratio; potential of under-representing AE – Late-onset AEs are also likely to be missed when we use patient–years • In short, only “…when an event is (or is believed to be) likely to occur at any stage during continuous treatment with a drug then an event rate with a time component (rate person year, etc) has a true meaning” • Not clear whether more than one event per patient goes into the numerator Paterson KR. BMJ 1995; 310: 1470. 22

Patient years (3) • If more than one AE/patient is included in a numerator, statistics done with that incidence ratio will be erroneous • An AE can repeat itself, like skin rashes in TNF-α antagonist use in any one patient • This leads to over-representation of the said individual in tests of significance Paterson KR. BMJ 1995; 310: 1470. 23
“Statistics are like swimwear – what they reveal is suggestive but what they conceal is vital. ” –Ashish Mahajan, Lancet 2007 24
Reporting radiographic outcomes in RA RCTs 25
Conventional wisdom… Schett et al. Arthritis Rheum 2008
Conventional wisdom… • “…studies of anti-TNF therapy plus MTX, compared with the effect with MTX alone, have shown that although MTX is relatively effective at relieving clinical symptoms, it has little or no effect on underlying radiological progression. ” Emery P, Mc. Innes IB, van Vollenhoven R, Kraan MC. Rheumatology (Oxford) 2008
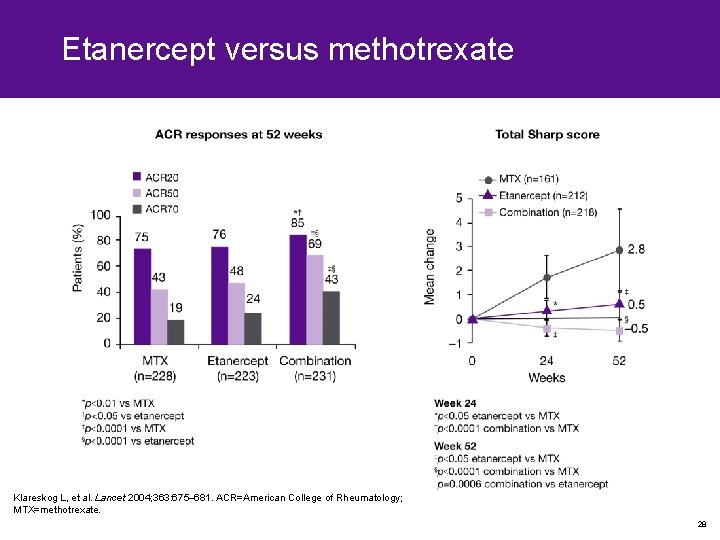
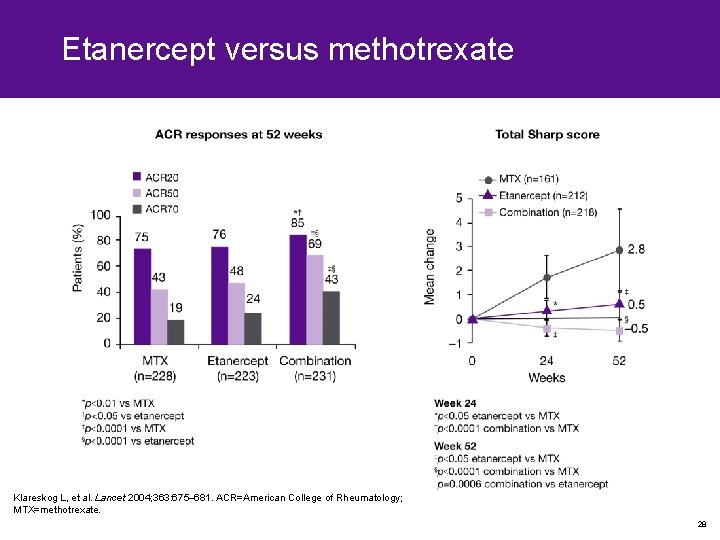
Etanercept versus methotrexate Klareskog L, et al. Lancet 2004; 363: 675– 681. ACR=American College of Rheumatology; MTX=methotrexate. 28

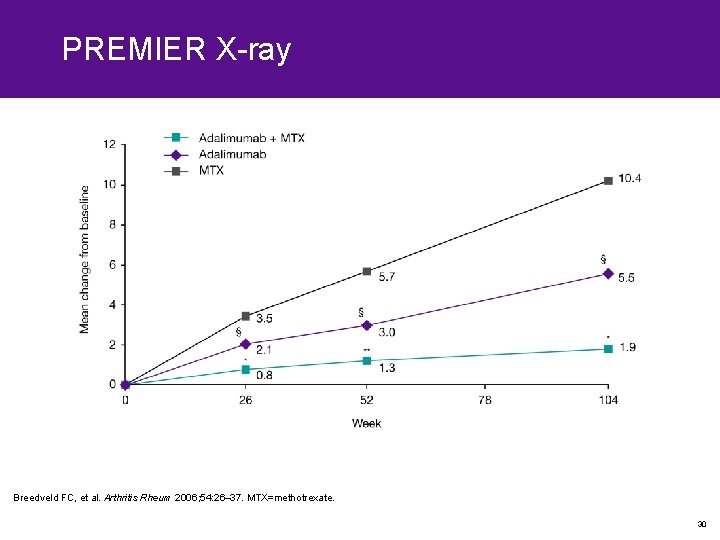
Adalimumab versus methotrexate Breedveld FC, et al. Arthritis Rheum 2006; 54: 26– 37. §p<0. 001 vs ADA alone and p=0. 022 vs MTX alone; †p<0. 001 vs ADA alone and p=0. 002 vs MTX alone; #p=0. 043 vs ADA alone; *p<0. 001 vs ADA alone and vs MTX alone; ACR=American College of Rheumatology; ADA=adalimumab; MTX=methotrexate. 29
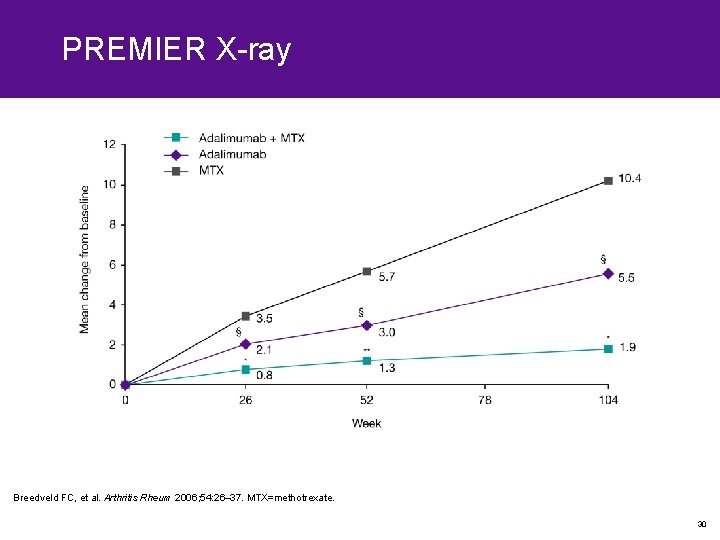
PREMIER X-ray Breedveld FC, et al. Arthritis Rheum 2006; 54: 26– 37. MTX=methotrexate. 30
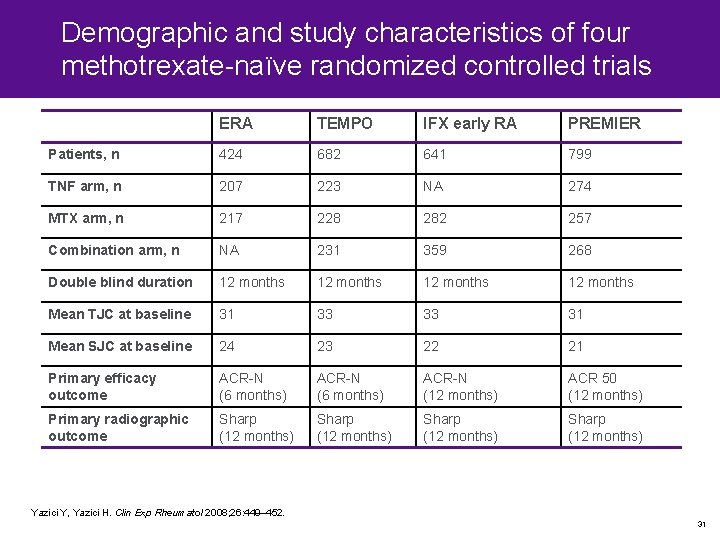
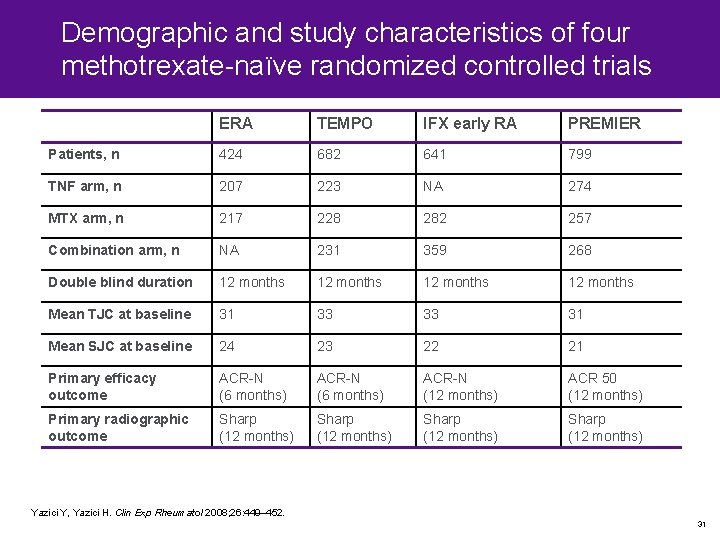
Demographic and study characteristics of four methotrexate-naïve randomized controlled trials ERA TEMPO IFX early RA PREMIER Patients, n 424 682 641 799 TNF arm, n 207 223 NA 274 MTX arm, n 217 228 282 257 Combination arm, n NA 231 359 268 Double blind duration 12 months Mean TJC at baseline 31 33 33 31 Mean SJC at baseline 24 23 22 21 Primary efficacy outcome ACR-N (6 months) ACR-N (12 months) ACR 50 (12 months) Primary radiographic outcome Sharp (12 months) Yazici Y, Yazici H. Clin Exp Rheumatol 2008; 26: 449– 452. 31

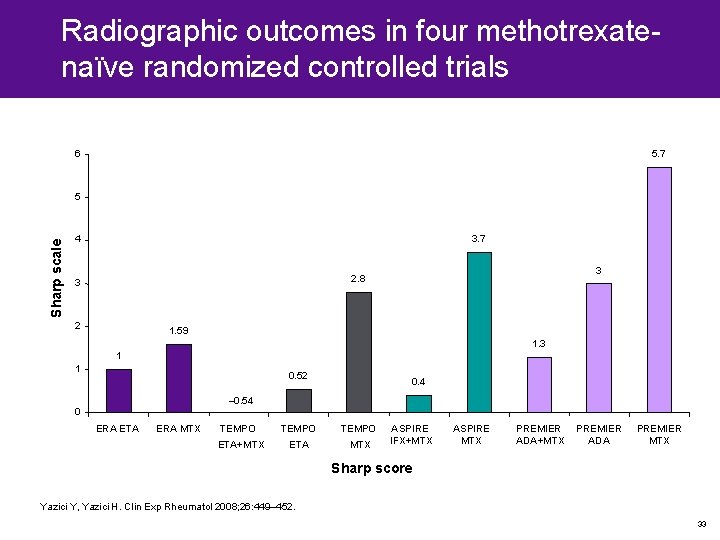
12 -month efficacy and radiographic outcomes in four methotrexate-naïve randomized controlled studies Study ACR 20 ACR 50 ACR 70 ACR N Sharp NNT ERA ETA 72 NR* NR* 1. 00 15 ERA MTX 65 NR* NR* 1. 59 - TEMPO combination 85 69 43 18. 3 – 0. 54 12 TEMPO ETA 75 48 24 14. 7 0. 52 - TEMPO MTX 76 43 19 12. 2 2. 8 - IFX combination 62. 4 45. 6 32. 5 38. 9 0. 4 13 IFX MTX 53. 6 32. 1 21. 2 26. 4 3. 7 - PREMIER combination 73 62 46 NR 1. 3 10 PREMIER ADA 54 41 26 NR 3. 0 - PREMIER MTX 63 46 28 NR 5. 7 - Yazici Y, Yazici H. Clin Exp Rheumatol 2008; 26: 449– 452. ACR=American College of Rheumatology, NNT=number needed to treat; ERA=Early RA; ETA=etanercept; NR=not reported; NR*=values not given, only depicted in graphic form; MTX=methotrexate; TNF=tumor necrosis factor inhibitor; TEMPO=Trial of Etanercept and MTX with radiographic Patient Outcomes; IFX=infliximab; ADA=adalimumab. 32
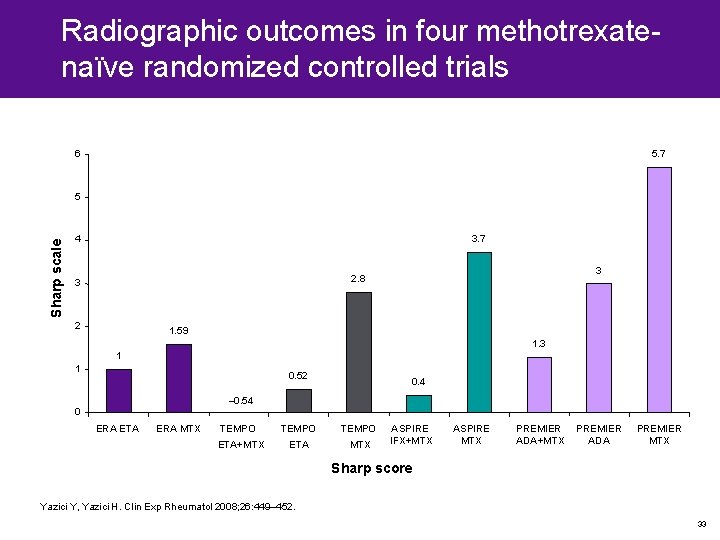
Radiographic outcomes in four methotrexatenaïve randomized controlled trials 6 5. 7 Sharp scale 5 4 3. 7 3 2. 8 3 2 1. 59 1. 3 1 1 0. 52 0. 4 – 0. 54 0 ERA ETA ERA MTX TEMPO ETA+MTX ETA MTX ASPIRE IFX+MTX ASPIRE MTX PREMIER ADA+MTX PREMIER ADA PREMIER MTX Sharp score Yazici Y, Yazici H. Clin Exp Rheumatol 2008; 26: 449– 452. 33

Radiographic outcomes in four methotrexatenaïve randomized controlled trials 450 400 350 Sharp scale 300 250 200 150 100 50 1 1. 59 ERA ETA ERA MTX – 0. 54 0. 52 2. 8 TEMPO ETA+MTX ETA MTX 0. 4 3. 7 1. 3 3 5. 7 0 ASPIRE IFX+MTX ASPIRE MTX PREMIER ADA+MTX PREMIER ADA PREMIER MTX Sharp score Yazici Y, Yazici H. Clin Exp Rheumatol 2008; 26: 449– 452. 34
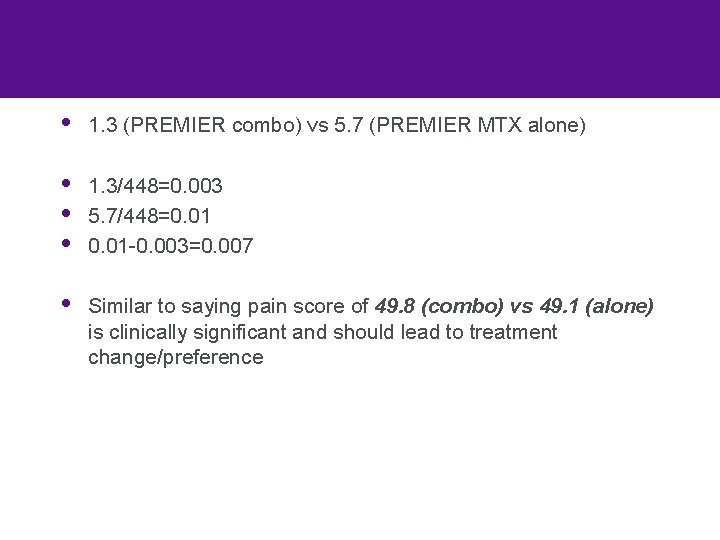
• 1. 3 (PREMIER combo) vs 5. 7 (PREMIER MTX alone) • • • 1. 3/448=0. 003 5. 7/448=0. 01 -0. 003=0. 007 • Similar to saying pain score of 49. 8 (combo) vs 49. 1 (alone) is clinically significant and should lead to treatment change/preference
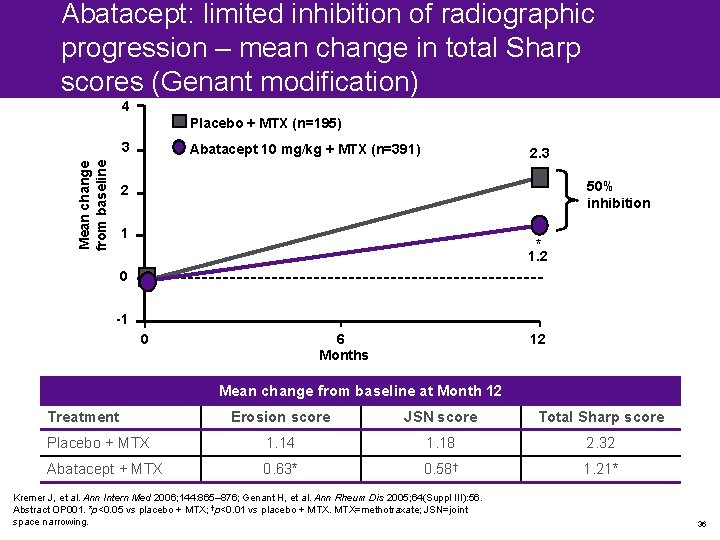
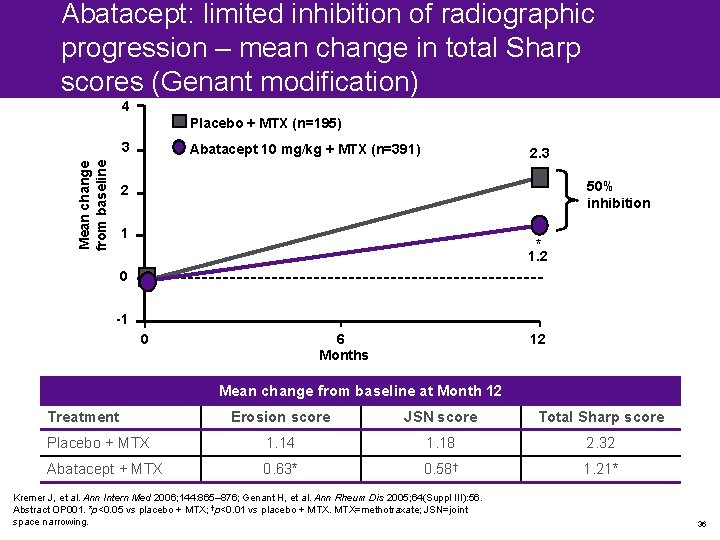
Abatacept: limited inhibition of radiographic progression – mean change in total Sharp scores (Genant modification) 4 Placebo + MTX (n=195) Mean change from baseline 3 Abatacept 10 mg/kg + MTX (n=391) 2. 3 50% inhibition 2 1 * 1. 2 0 -1 0 6 Months 12 Mean change from baseline at Month 12 Treatment Erosion score JSN score Total Sharp score Placebo + MTX 1. 14 1. 18 2. 32 Abatacept + MTX 0. 63* 0. 58† 1. 21* Kremer J, et al. Ann Intern Med 2006; 144: 865– 876; Genant H, et al. Ann Rheum Dis 2005; 64(Suppl III): 56. Abstract OP 001. *p<0. 05 vs placebo + MTX; †p<0. 01 vs placebo + MTX=methotraxate; JSN=joint space narrowing. 36
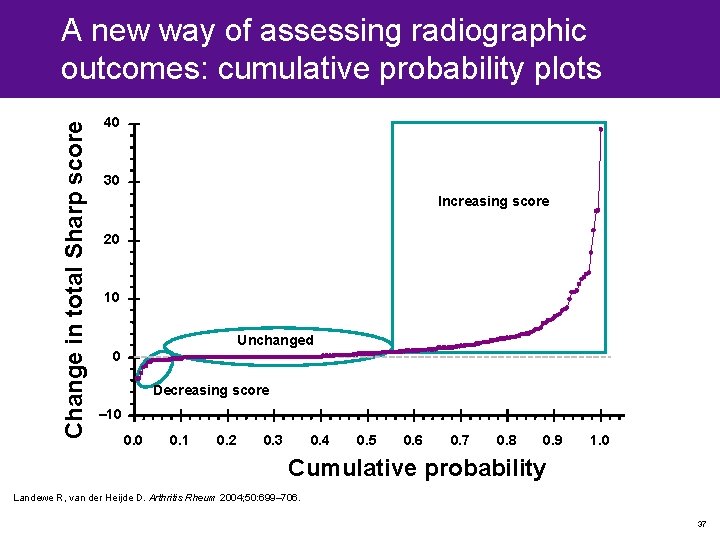
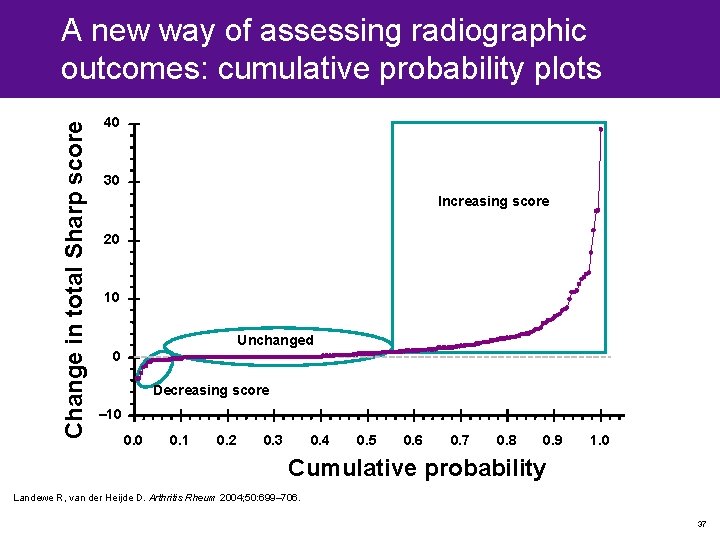
Change in total Sharp score A new way of assessing radiographic outcomes: cumulative probability plots 40 30 Increasing score 20 10 Unchanged 0 Decreasing score – 10 0. 1 0. 2 0. 3 0. 4 0. 5 0. 6 0. 7 0. 8 0. 9 1. 0 Cumulative probability Landewe R, van der Heijde D. Arthritis Rheum 2004; 50: 699– 706. 37
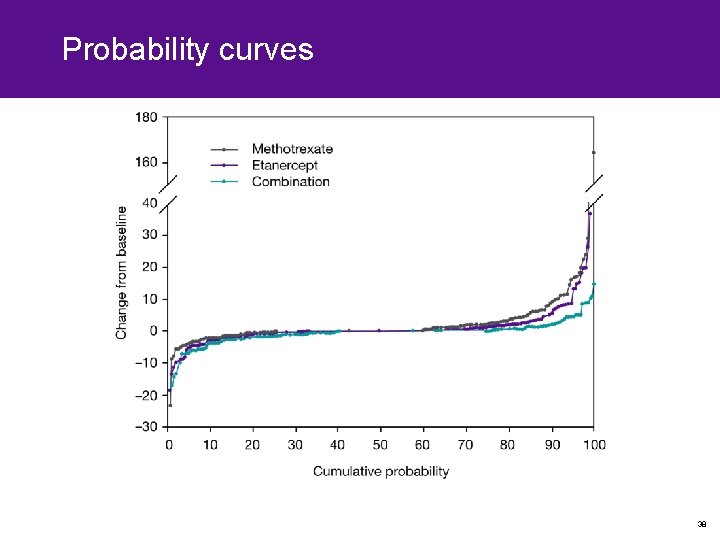
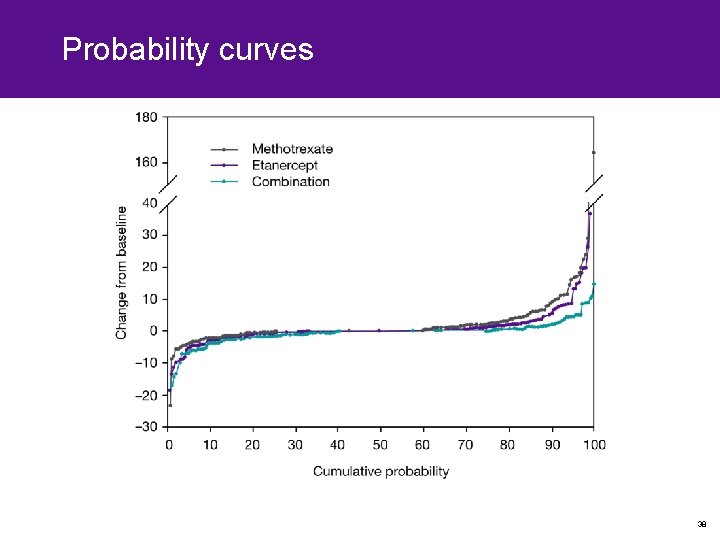
Probability curves 38
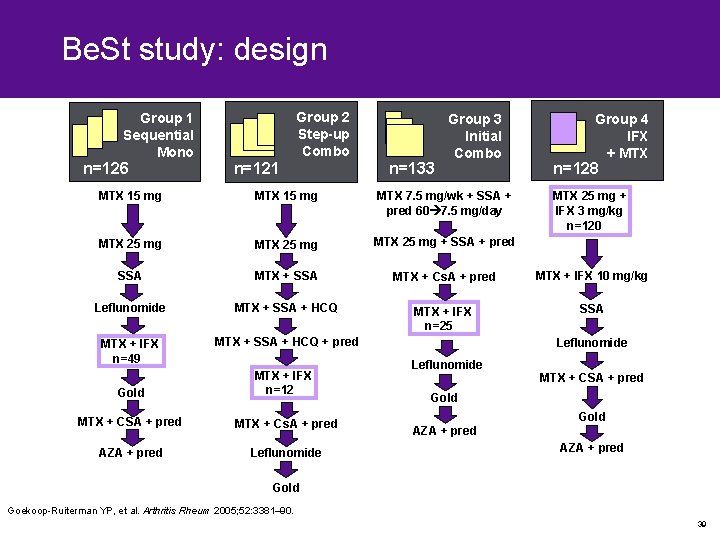
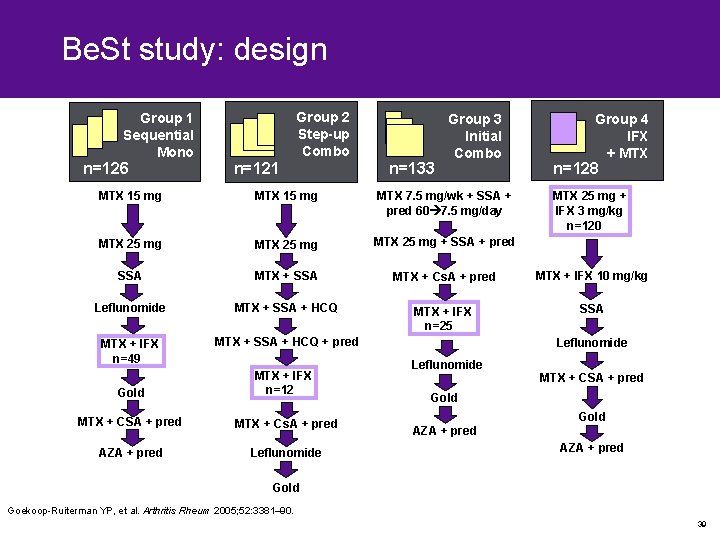
Be. St study: design Group 1 Sequential Mono n=126 Group 2 Step-up Combo n=121 n=133 Group 3 Initial Combo Group 4 IFX + MTX n=128 MTX 15 mg MTX 7. 5 mg/wk + SSA + pred 60 7. 5 mg/day MTX 25 mg + SSA + pred SSA MTX + Cs. A + pred MTX + IFX 10 mg/kg Leflunomide MTX + SSA + HCQ MTX + IFX n=25 SSA MTX + IFX n=49 MTX + SSA + HCQ + pred Gold MTX + IFX n=12 MTX + CSA + pred MTX + Cs. A + pred AZA + pred Leflunomide MTX 25 mg + IFX 3 mg/kg n=120 Leflunomide MTX + CSA + pred Gold AZA + pred Gold Goekoop-Ruiterman YP, et al. Arthritis Rheum 2005; 52: 3381– 90. 39
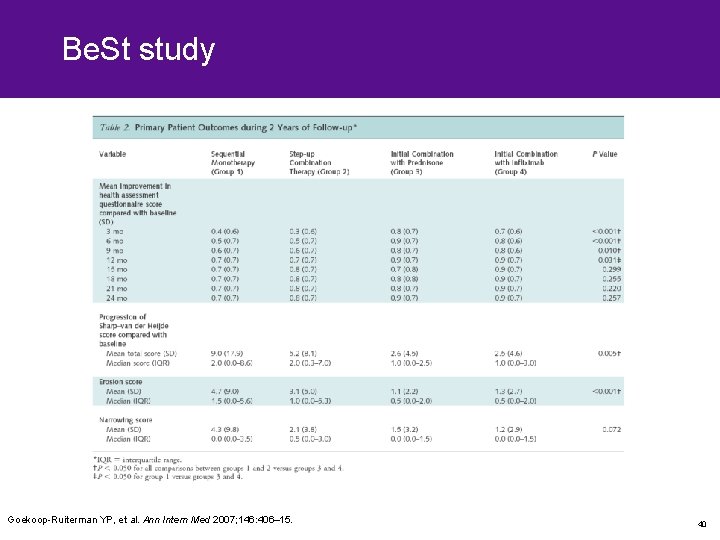
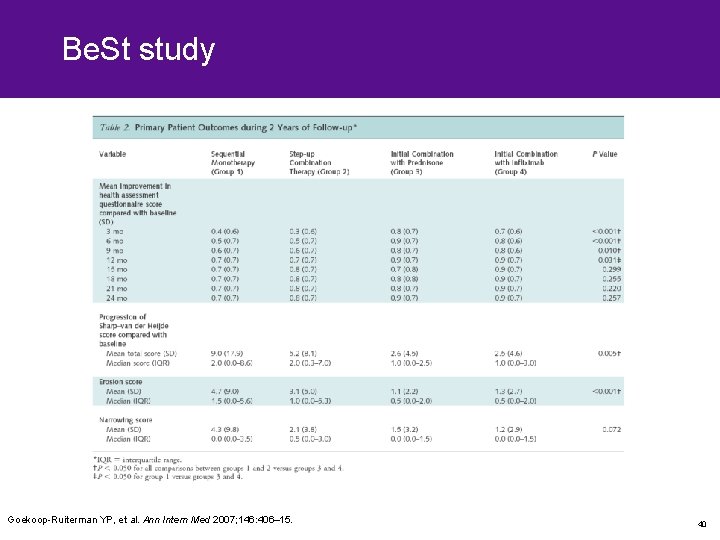
Be. St study Goekoop-Ruiterman YP, et al. Ann Intern Med 2007; 146: 406– 15. 40
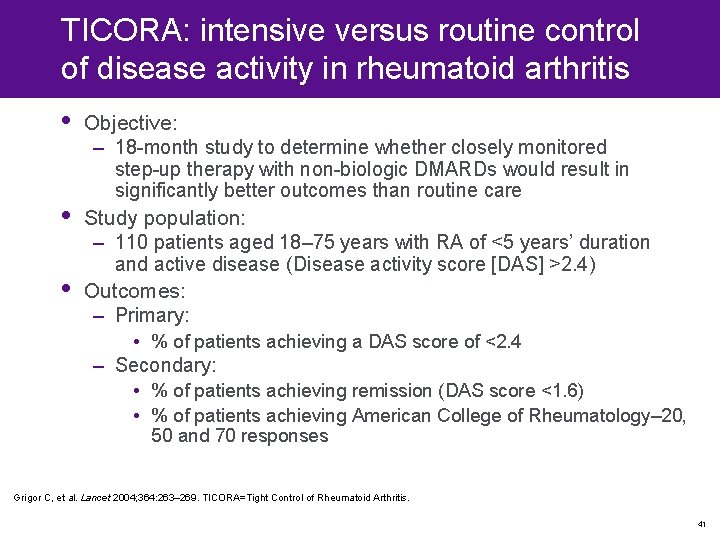
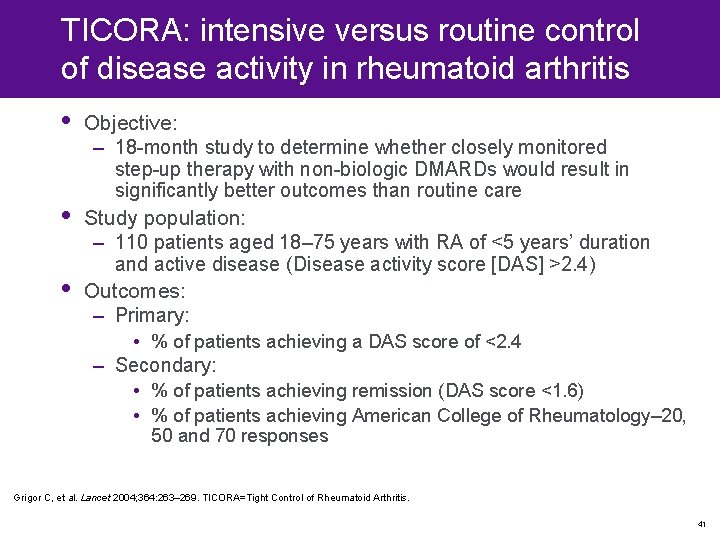
TICORA: intensive versus routine control of disease activity in rheumatoid arthritis • • • Objective: – 18 -month study to determine whether closely monitored step-up therapy with non-biologic DMARDs would result in significantly better outcomes than routine care Study population: – 110 patients aged 18– 75 years with RA of <5 years’ duration and active disease (Disease activity score [DAS] >2. 4) Outcomes: – Primary: • % of patients achieving a DAS score of <2. 4 – Secondary: • % of patients achieving remission (DAS score <1. 6) • % of patients achieving American College of Rheumatology– 20, 50 and 70 responses Grigor C, et al. Lancet 2004; 364: 263– 269. TICORA=Tight Control of Rheumatoid Arthritis. 41

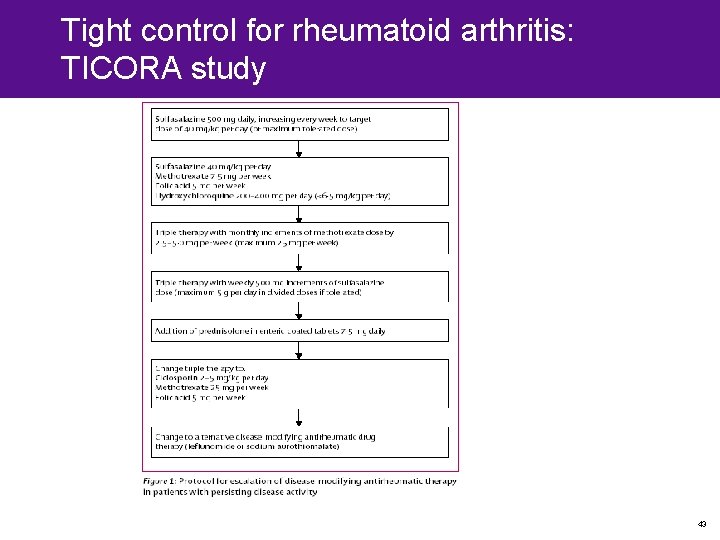
TICORA: intensive versus routine control of disease activity in rheumatoid arthritis (2) • • Intensive care group: – Monthly review of disease activity and measurement of DAS – Intra-articular corticosteroid injection of swollen joints as required – Intramuscular corticosteroid injection given as ‘bridge therapy’ during first 3 months of a new DMARD – Structured escalation of therapy if DAS >2. 4 after 3 months of a new DMARD: SSZ MTX + SSZ + HCQ MTX (up to 25 mg/wk); SSZ (up to 5 g/d) prednisolone 7. 5 mg/d switch to MTX + CSA switch to leflunomide Routine care group: – Review every 3 months (with no measure of DAS) – Management at the discretion of attending rheumatologist (i. e. DMARD therapy; intra-articular, intramuscular and/or oral corticosteroids) Grigor C, et al. Lancet 2004; 364: 263– 269. TICORA=Tight Control of Rheumatoid Arthritis. 42
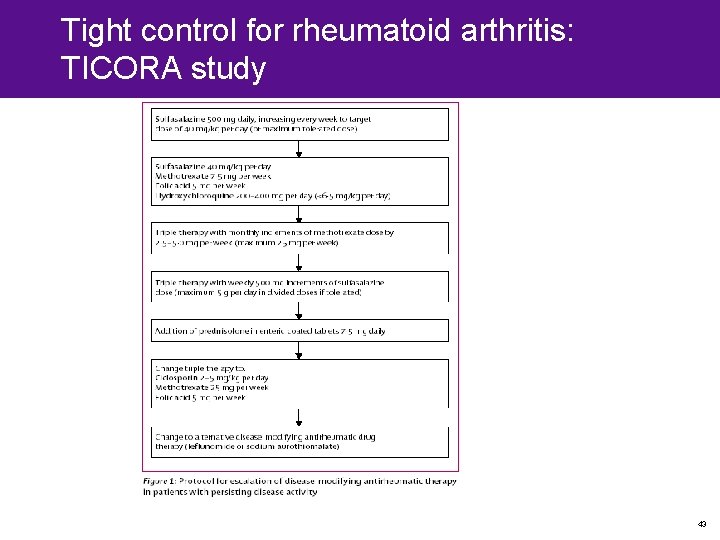
Tight control for rheumatoid arthritis: TICORA study 43
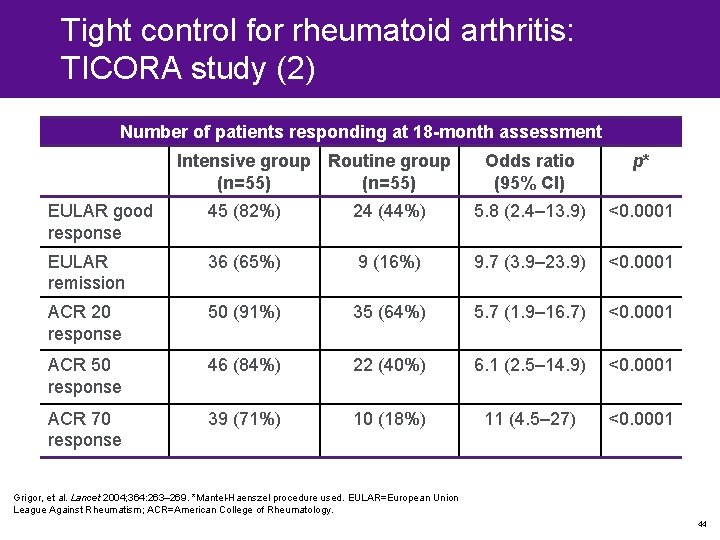
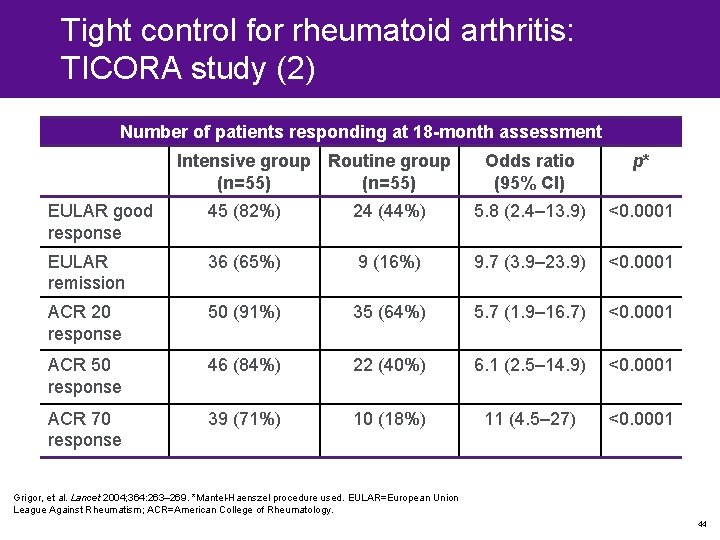
Tight control for rheumatoid arthritis: TICORA study (2) Number of patients responding at 18 -month assessment Intensive group Routine group (n=55) Odds ratio (95% CI) p* EULAR good response 45 (82%) 24 (44%) 5. 8 (2. 4– 13. 9) <0. 0001 EULAR remission 36 (65%) 9 (16%) 9. 7 (3. 9– 23. 9) <0. 0001 ACR 20 response 50 (91%) 35 (64%) 5. 7 (1. 9– 16. 7) <0. 0001 ACR 50 response 46 (84%) 22 (40%) 6. 1 (2. 5– 14. 9) <0. 0001 ACR 70 response 39 (71%) 10 (18%) 11 (4. 5– 27) <0. 0001 Grigor, et al. Lancet 2004; 364: 263– 269. *Mantel-Haenszel procedure used. EULAR=European Union League Against Rheumatism; ACR=American College of Rheumatology. 44
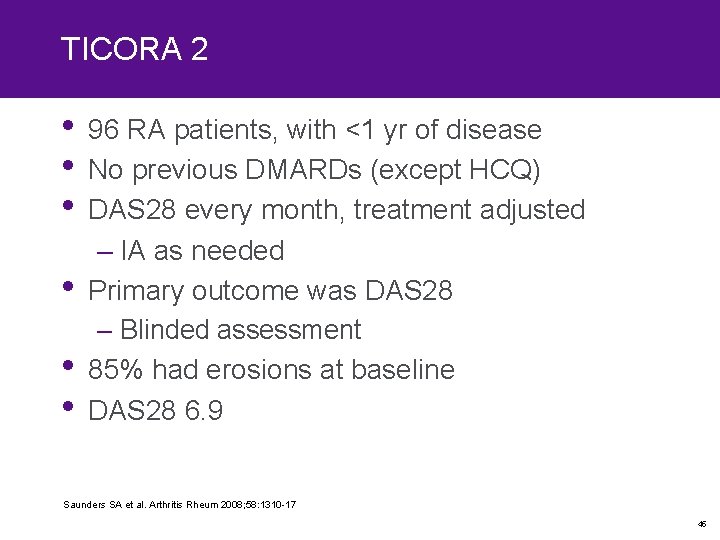
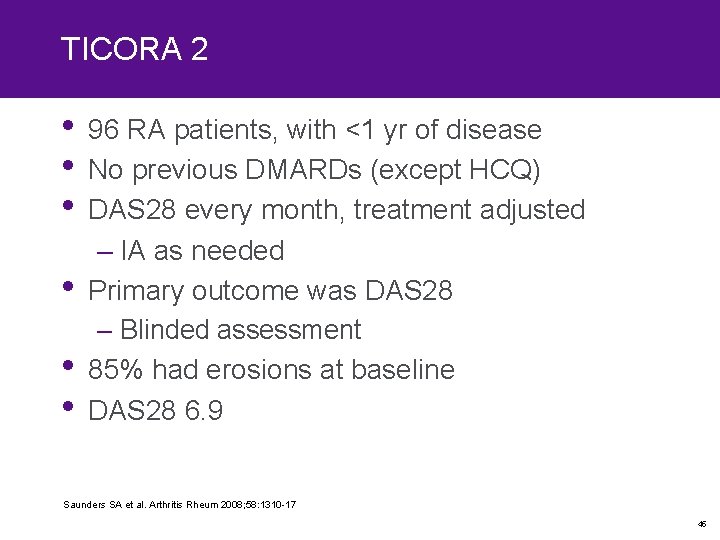
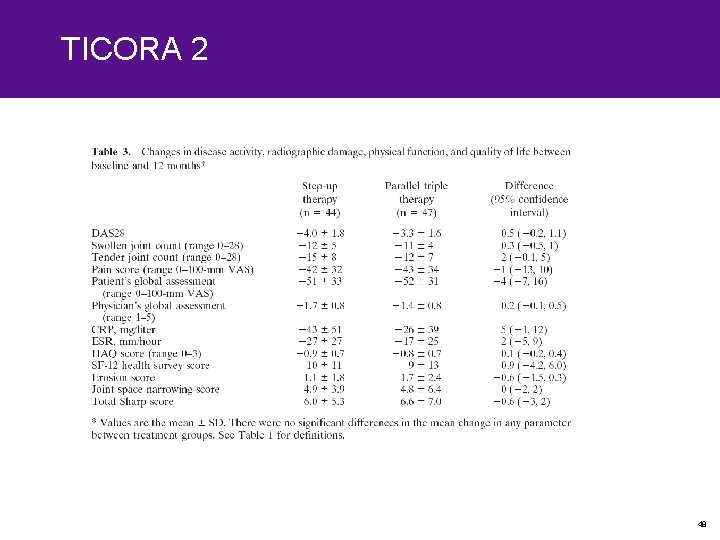
TICORA 2 • 96 RA patients, with <1 yr of disease • No previous DMARDs (except HCQ) • DAS 28 every month, treatment adjusted • • • – IA as needed Primary outcome was DAS 28 – Blinded assessment 85% had erosions at baseline DAS 28 6. 9 Saunders SA et al. Arthritis Rheum 2008; 58: 1310 -17 45
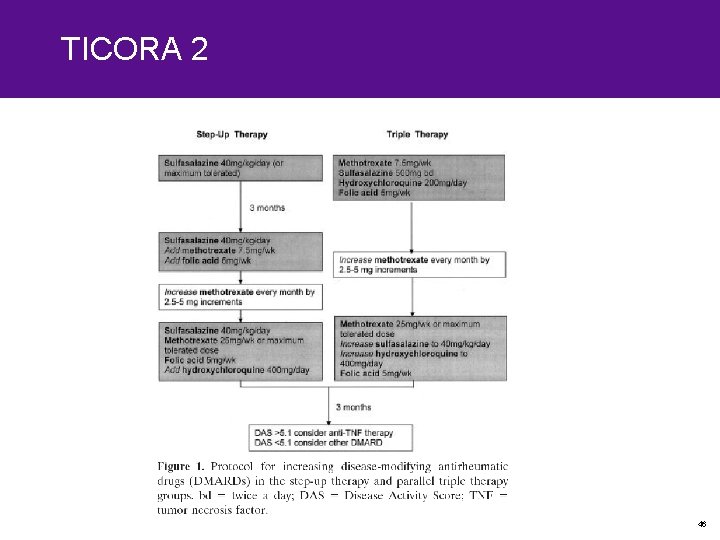
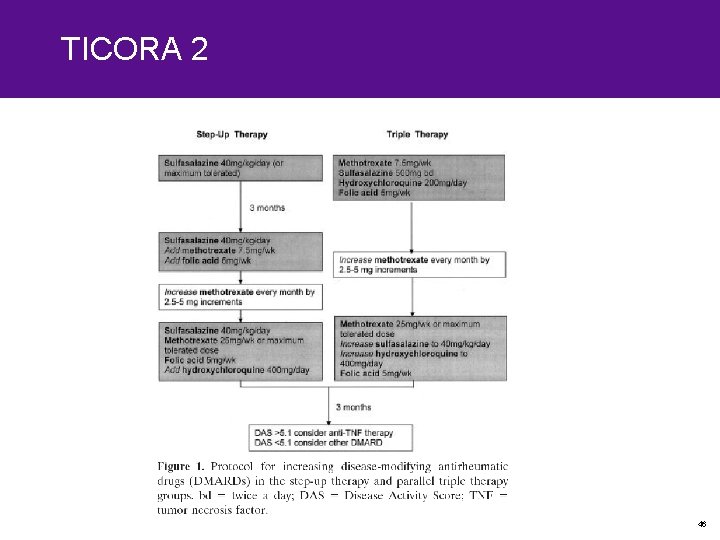
TICORA 2 46
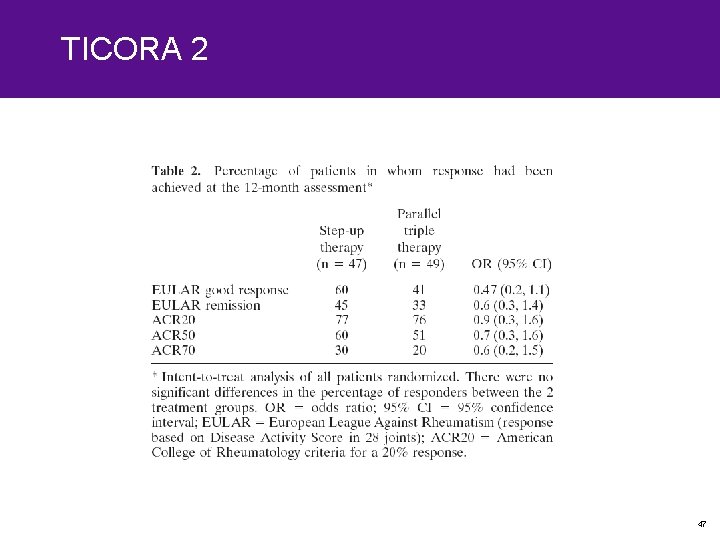
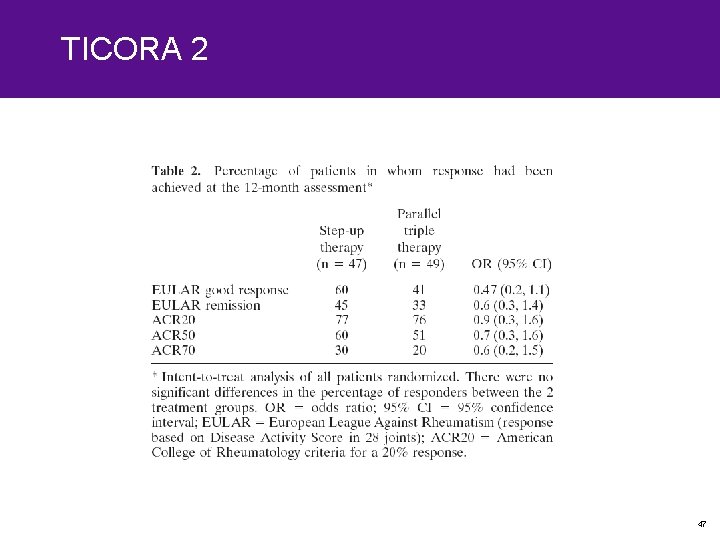
TICORA 2 47
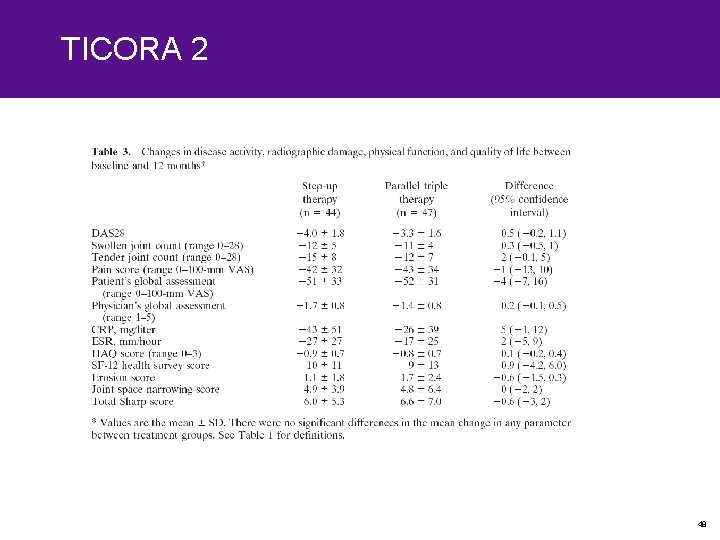
TICORA 2 48

‘Efficacy versus safety versus efficacy and safety trials’ 49

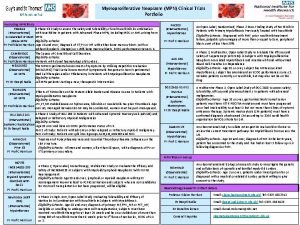
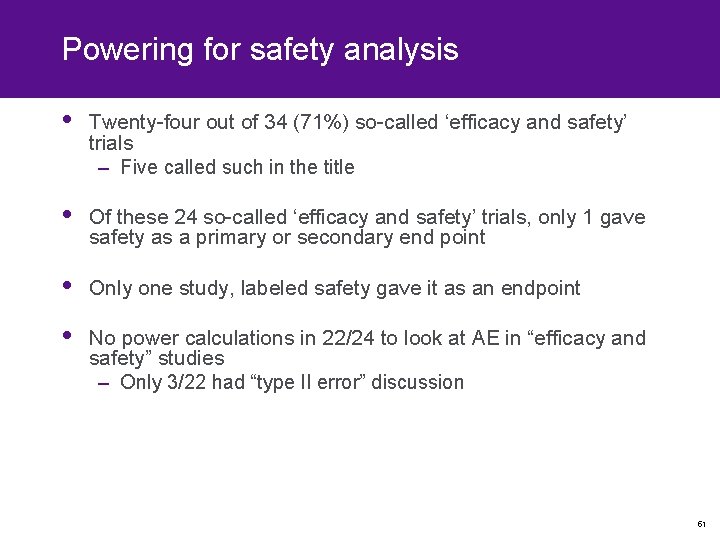
‘Efficacy and safety’ randomized controlled trials • Trend of increasing number of RCT called ‘efficacy and safety’ trials • All RCT of TNF-α inhibitors in RA, psoriatic arthritis (Ps. A) and ankylosing spondylitis (AS) • Only original reports – ‘Efficacy’, ‘safety’ or ‘efficacy and safety’ – Power for safety and efficacy – Type II error • Power – Alpha – Beta – Expected treatment effects in both arms Yazici Y, et al. Rheumatology 2008; 47: 1054– 1057. 50
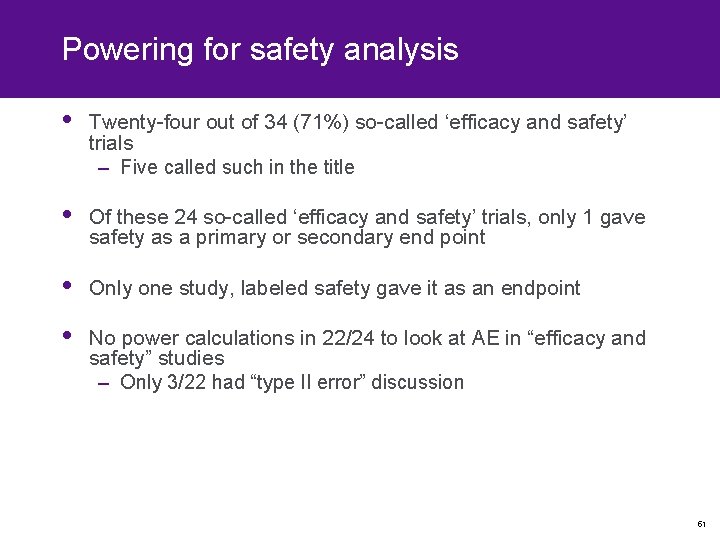
Powering for safety analysis • Twenty-four out of 34 (71%) so-called ‘efficacy and safety’ trials – Five called such in the title • Of these 24 so-called ‘efficacy and safety’ trials, only 1 gave safety as a primary or secondary end point • Only one study, labeled safety gave it as an endpoint • No power calculations in 22/24 to look at AE in “efficacy and safety” studies – Only 3/22 had “type II error” discussion 51
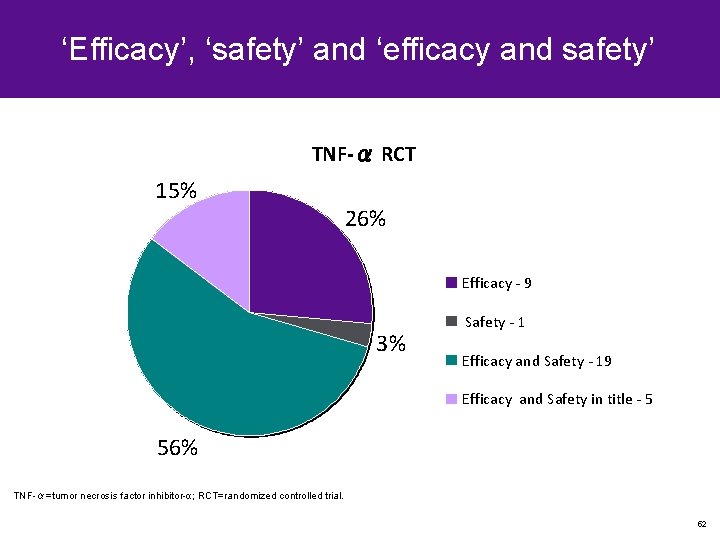
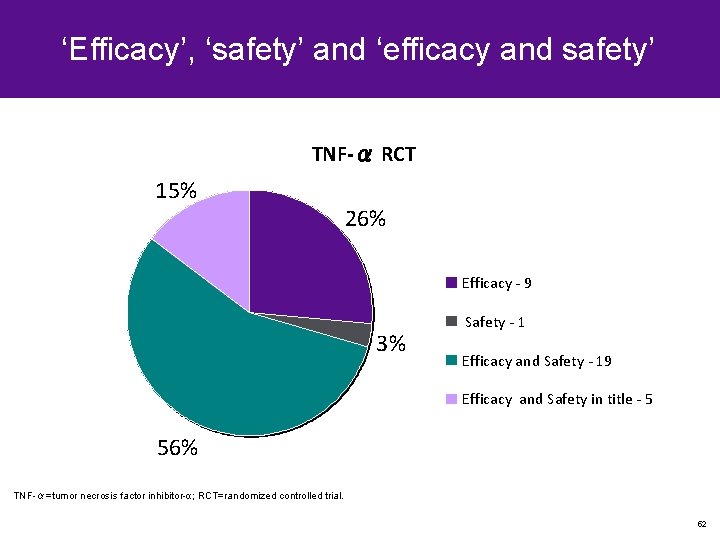
‘Efficacy’, ‘safety’ and ‘efficacy and safety’ TNF-α RCT 15% 26% Efficacy - 9 3% Safety - 1 Efficacy and Safety - 19 Efficacy and Safety in title - 5 56% TNF-α=tumor necrosis factor inhibitor-α; RCT=randomized controlled trial. 52
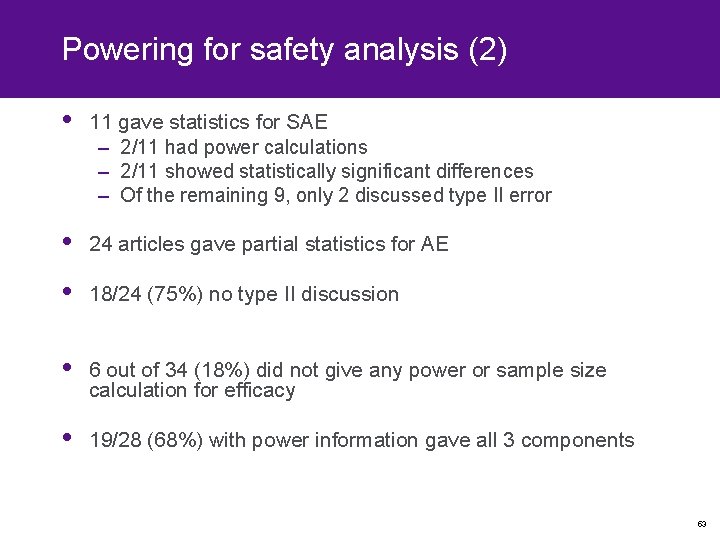
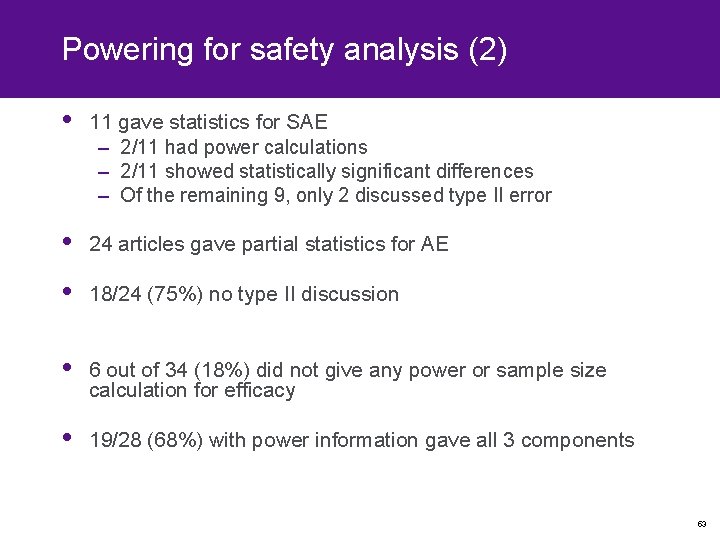
Powering for safety analysis (2) • 11 gave statistics for SAE – 2/11 had power calculations – 2/11 showed statistically significant differences – Of the remaining 9, only 2 discussed type II error • 24 articles gave partial statistics for AE • 18/24 (75%) no type II discussion • 6 out of 34 (18%) did not give any power or sample size calculation for efficacy • 19/28 (68%) with power information gave all 3 components 53
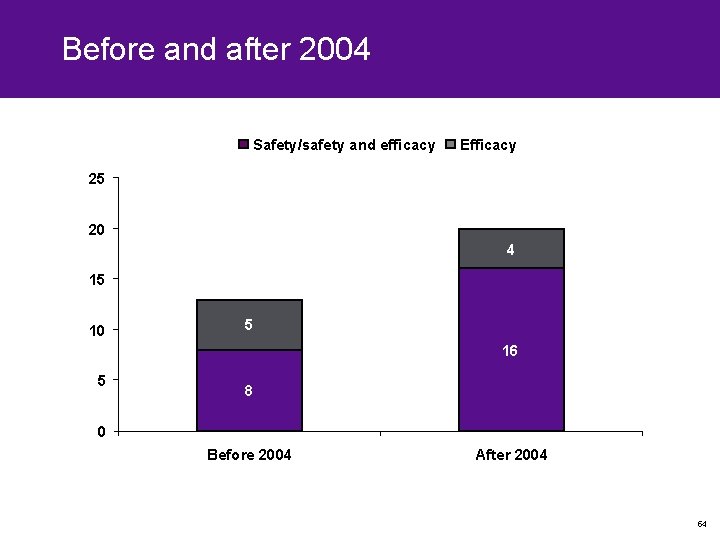
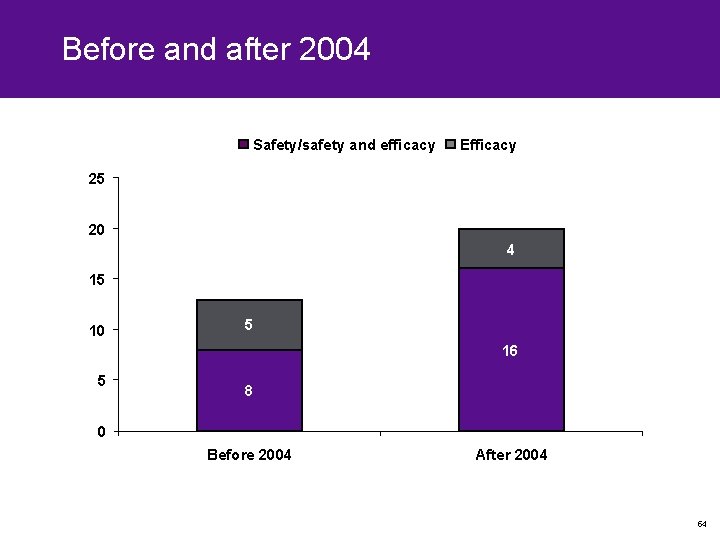
Before and after 2004 Safety/safety and efficacy Efficacy 25 20 4 15 10 5 16 5 8 0 Before 2004 After 2004 54

‘Efficacy and safety’ • Designating RCT as ‘safety’ as well as ‘efficacy’ has the potential to give false impressions that lack of AE increase is evidence of overall safety of the medication tested • Only one of these trials was powered to look at safety • In addition, RCT are highly selective for lack of major comorbidities – So even if they were powered to look at safety, results need to be interpreted with caution – Phase IV trials • Randomized controlled trials report on AEs, but these efficacy trials cannot provide any conclusive evidence about safety; these shortcomings should be reported and required by journals and reviewers 55

Disease activity measurement in RA 56
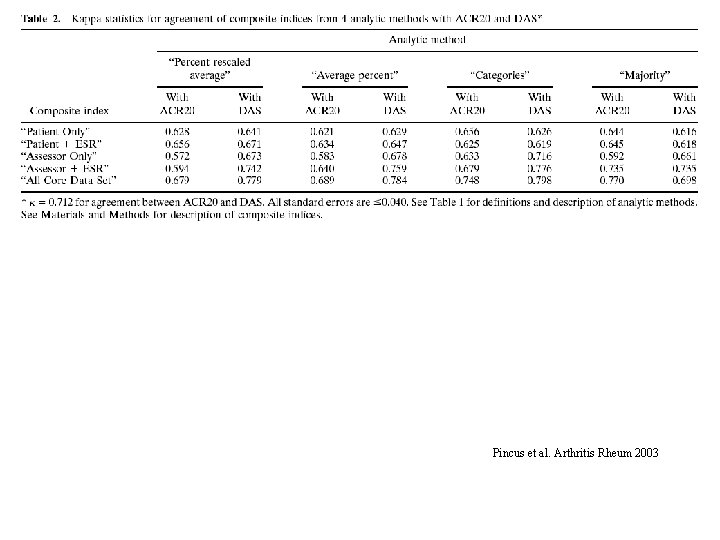
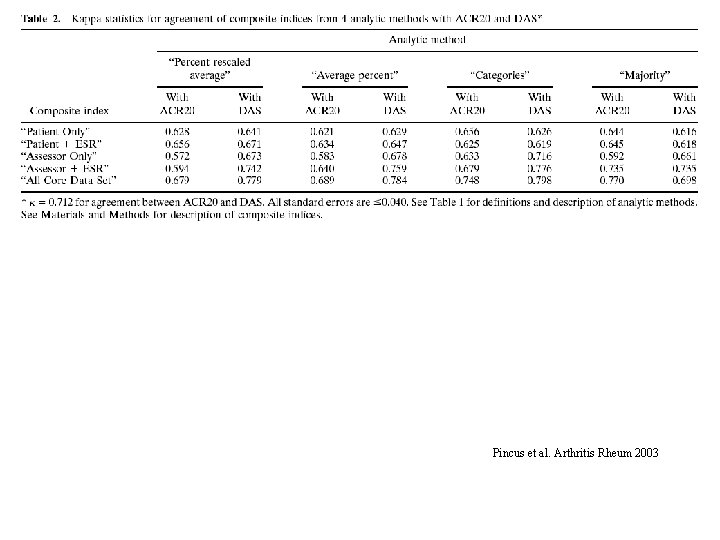
Pincus et al. Arthritis Rheum 2003
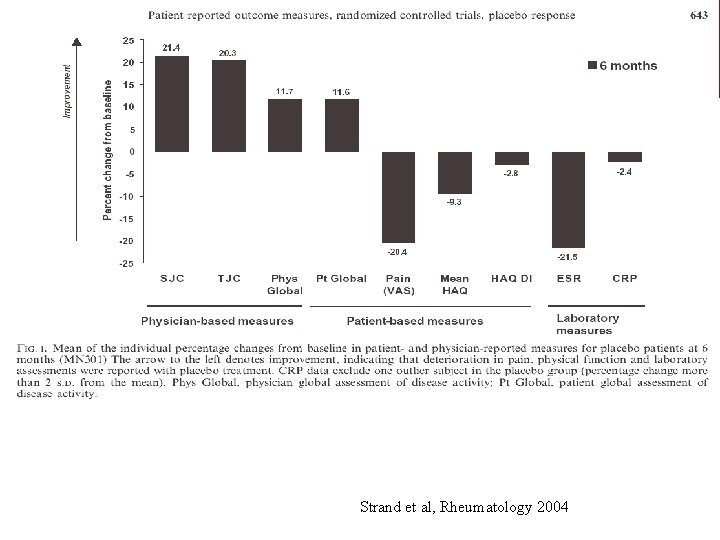
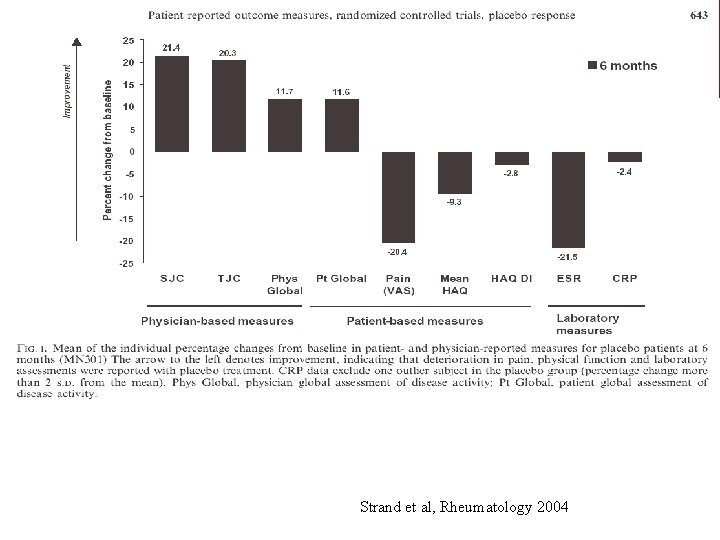
Patient–reported outcomes Strand et al, Rheumatology 2004
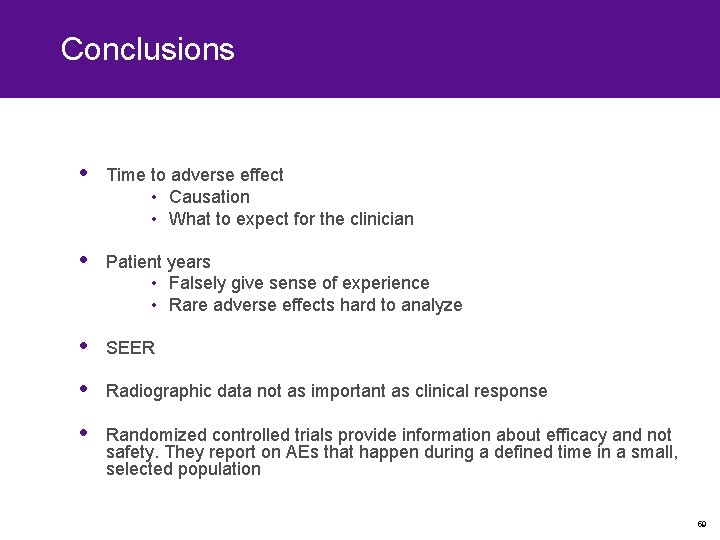
Conclusions • Time to adverse effect • Causation • What to expect for the clinician • Patient years • Falsely give sense of experience • Rare adverse effects hard to analyze • SEER • Radiographic data not as important as clinical response • Randomized controlled trials provide information about efficacy and not safety. They report on AEs that happen during a defined time in a small, selected population 59
“We become confident in our educated guesswork to the point where it is easy to confuse personal opinion with evidence, or personal ignorance with scientific uncertainty” –David Naylor, MD, Ph. D (1954–) 60
Esra & Leyla
 Phs human subjects and clinical trials information
Phs human subjects and clinical trials information Difference between inspection and audit
Difference between inspection and audit Nida clinical trials network
Nida clinical trials network Site initiation visit powerpoint presentation
Site initiation visit powerpoint presentation Clinicaltrials.gov api
Clinicaltrials.gov api Clinical research statistician
Clinical research statistician Andrew nunn
Andrew nunn Randomization
Randomization Mpn clinical trials
Mpn clinical trials Clinicaltrials gov prs
Clinicaltrials gov prs Clinical trials
Clinical trials Clinical trials quality by design
Clinical trials quality by design Mpn clinical trials
Mpn clinical trials Dhl bishkek
Dhl bishkek Clinical hysteria salem witch trials
Clinical hysteria salem witch trials Ohsu clinical trials office
Ohsu clinical trials office Protocol registration system
Protocol registration system Clinical trials.gov login
Clinical trials.gov login Clinical trial iwr
Clinical trial iwr York clinical trials unit
York clinical trials unit Ind safety report
Ind safety report Vbpm rheumatology
Vbpm rheumatology Rheumatology
Rheumatology Symmetryical
Symmetryical Rheumatology org
Rheumatology org Gregory gardner md
Gregory gardner md Alberto rios zertuche caceres
Alberto rios zertuche caceres Ps suite emr cost
Ps suite emr cost Enthesitis
Enthesitis Colin tench rheumatology
Colin tench rheumatology Probabilistic analysis and randomized algorithms
Probabilistic analysis and randomized algorithms Do we our life done
Do we our life done Design and analysis of cross-over trials
Design and analysis of cross-over trials Duke safety reporting system
Duke safety reporting system Patient safety incident policy
Patient safety incident policy Randomized polynomial time
Randomized polynomial time Completely randomized design
Completely randomized design Randomized skip list
Randomized skip list Randomized group design
Randomized group design Duncan's multiple range test
Duncan's multiple range test Example of rcbd
Example of rcbd Rcbd design layout
Rcbd design layout Types of randomized algorithms
Types of randomized algorithms Rbal
Rbal Example of crd
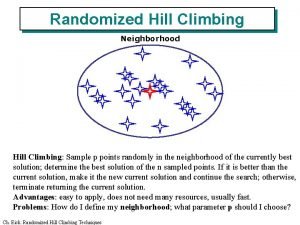
Example of crd Randomized hill climbing
Randomized hill climbing Experimental design
Experimental design Expected running time of randomized algorithm
Expected running time of randomized algorithm Completely randomized design
Completely randomized design Randomized hill climbing
Randomized hill climbing Contoh rancangan acak kelompok
Contoh rancangan acak kelompok Statistical model for crd
Statistical model for crd Factorial randomized block design
Factorial randomized block design Randomized polynomial time
Randomized polynomial time Advantage of randomized controlled trial
Advantage of randomized controlled trial Symantha melemed
Symantha melemed Randomized algorithm in daa
Randomized algorithm in daa Anova table
Anova table Salem witch trials discovery education
Salem witch trials discovery education National geographic salem witch trials
National geographic salem witch trials Malta football trials
Malta football trials Bernoulli trials formula
Bernoulli trials formula