Radiology Pathology Spinal Cord Tumors Before You Begin
Radiology - Pathology Spinal Cord Tumors
Before You Begin This module is intended primarily for pre-clinical students learning or reviewing pathophysiology. Please note that this series will focus on how pathology presents in imaging studies. It assumes familiarity with fundamental anatomy. If you need to learn or review this core concept, please visit the “Anatomy” section of our website. If material is repeated from another module, it will be outlined as this text is so that you are aware
Objectives • Review the anatomic compartments of the spinal canal • Identify the most common intramedullary spinal cord tumors with radiology and pathology correlation
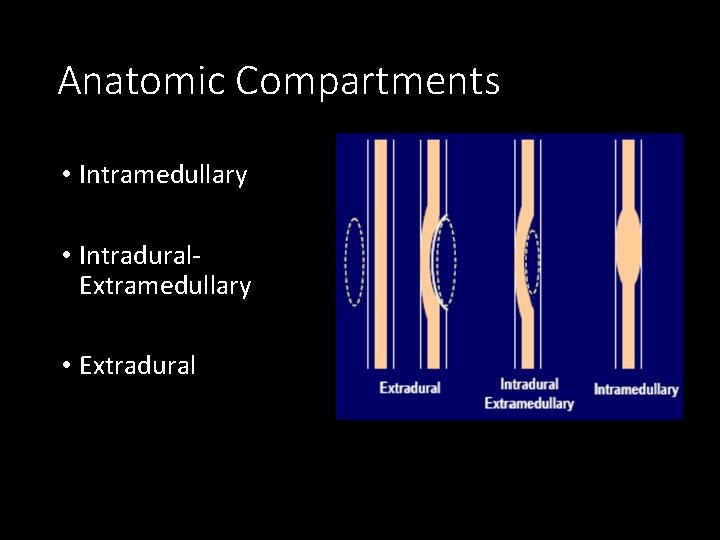
Anatomic Compartments • Intramedullary • Intradural. Extramedullary • Extradural
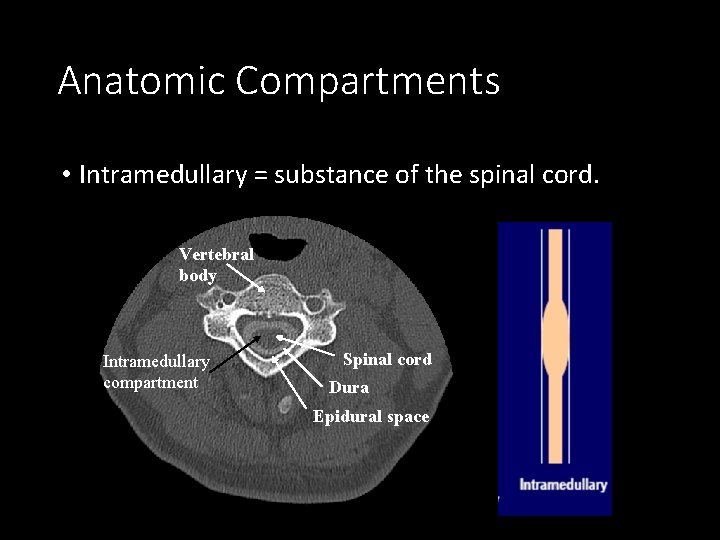
Anatomic Compartments • Intramedullary = substance of the spinal cord. Vertebral body Intramedullary compartment Spinal cord Dura Epidural space
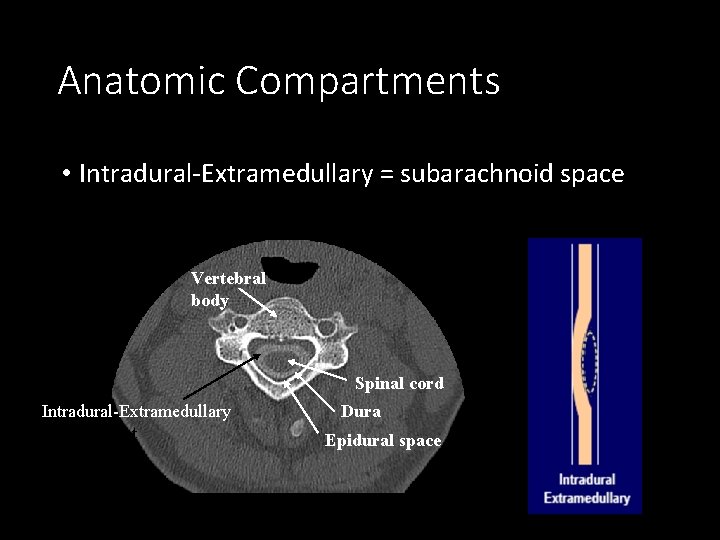
Anatomic Compartments • Intradural-Extramedullary = subarachnoid space Vertebral body Spinal cord Intradural-Extramedullary compartment Dura Epidural space
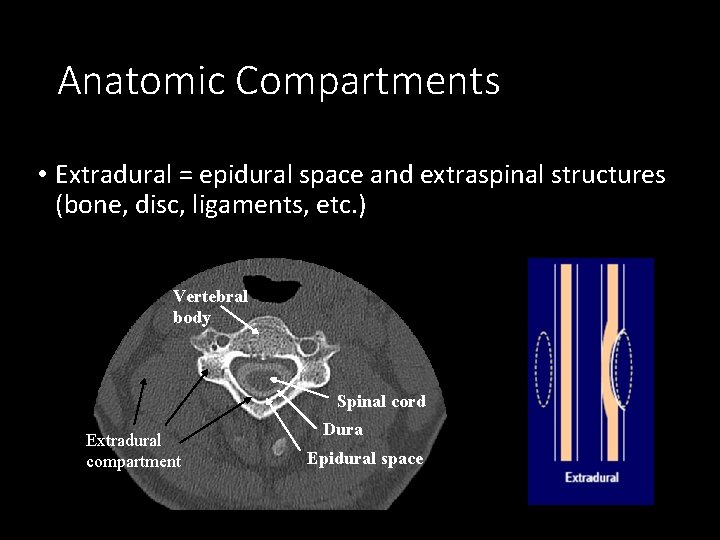
Anatomic Compartments • Extradural = epidural space and extraspinal structures (bone, disc, ligaments, etc. ) Vertebral body Spinal cord Extradural compartment Dura Epidural space
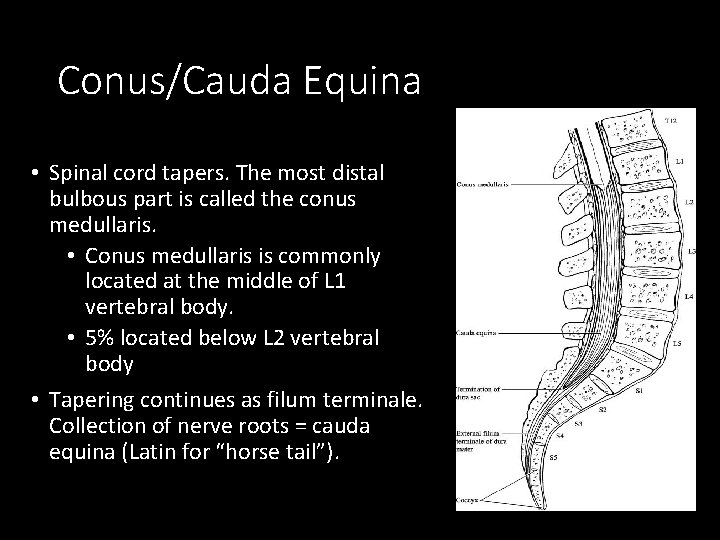
Conus/Cauda Equina • Spinal cord tapers. The most distal bulbous part is called the conus medullaris. • Conus medullaris is commonly located at the middle of L 1 vertebral body. • 5% located below L 2 vertebral body • Tapering continues as filum terminale. Collection of nerve roots = cauda equina (Latin for “horse tail”).
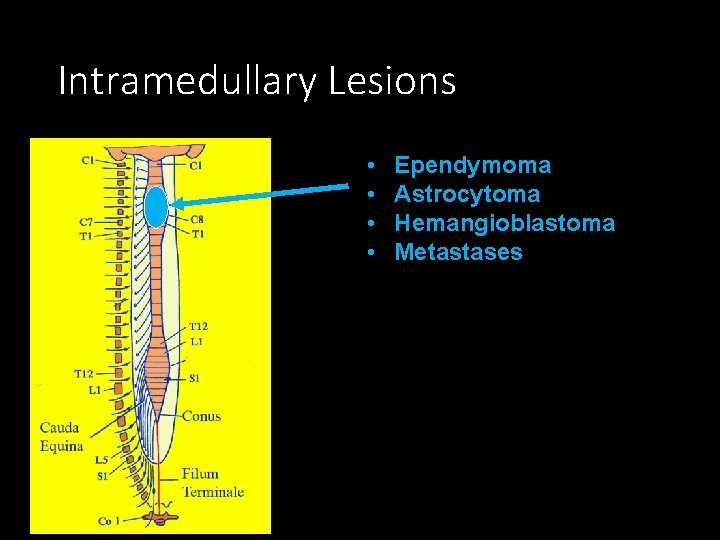
Intramedullary Lesions • • Ependymoma Astrocytoma Hemangioblastoma Metastases
Ependymoma • Most common primary spinal cord tumor in adults, second most common in children; typically present in 30 s-40 s. • 65% of cord gliomas • Cervical > thoracic > conus (myxopapillary ependymoma) • Typically 3 -4 vertebral body segments in length • Slow growing, well demarcated tumors that arise from the ependymal lining of central canal • Centrally located; cause fusiform expansion of the cord • Rarely metastasize • Most are WHO Grade II • Special category: myxopapillary ependymoma which occur at conus (discussed separately)
Ependymoma • MRI signal characteristics: • Isointense to normal cord on T 1 • Hyperintense to normal cord on T 2 • Homogenously and intensely enhancing on post-contrast sequences • Associations: • • Hemorrhage or hemosiderin cap is common finding Cystic changes often seen May have exophytic components May cause syrinx
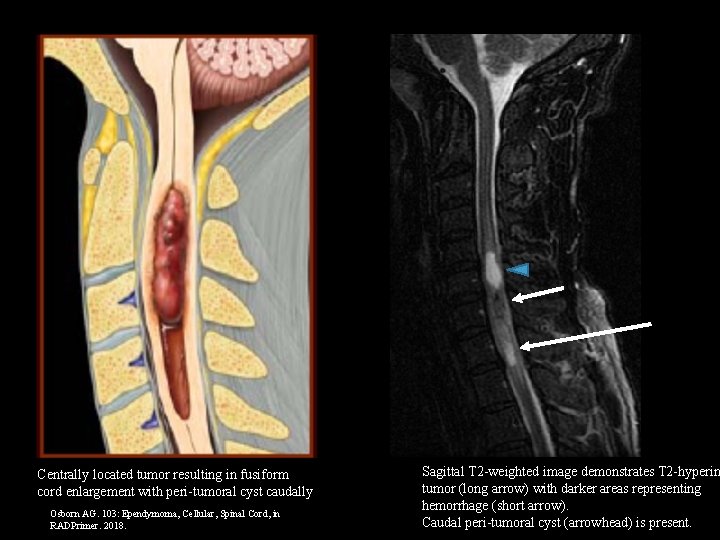
Centrally located tumor resulting in fusiform cord enlargement with peri-tumoral cyst caudally Osborn AG. 103: Ependymoma, Cellular, Spinal Cord, in RADPrimer. 2018. Sagittal T 2 -weighted image demonstrates T 2 -hyperin tumor (long arrow) with darker areas representing hemorrhage (short arrow). Caudal peri-tumoral cyst (arrowhead) is present.
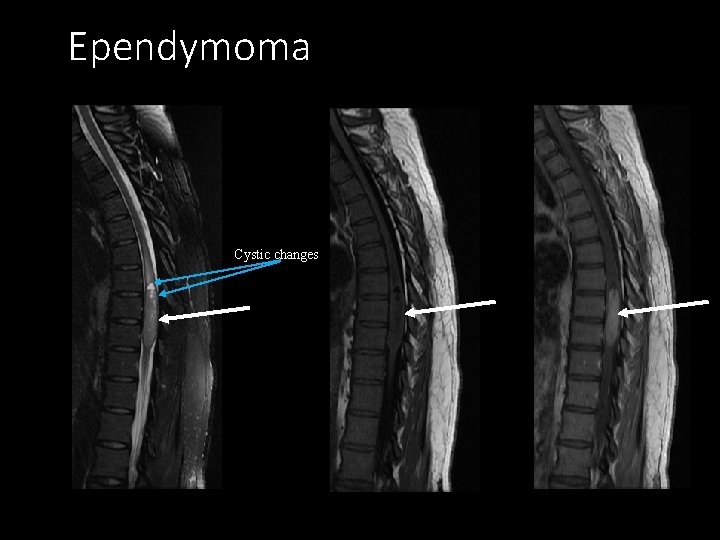
Ependymoma Cystic changes Sagittal T 2 Sagittal T 1 Post-contrast sagittal T 1

Axial T 1 -weighted post-contrast image confirms centrally located enhancing tumor. Sagittal T 1 -weighted post-contrast image shows heterogeneously enhancing tumor, without associated cysts.
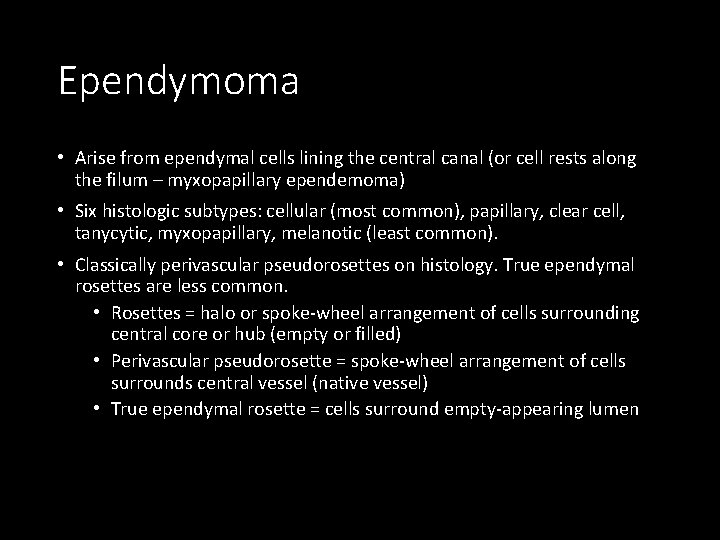
Ependymoma • Arise from ependymal cells lining the central canal (or cell rests along the filum – myxopapillary ependemoma) • Six histologic subtypes: cellular (most common), papillary, clear cell, tanycytic, myxopapillary, melanotic (least common). • Classically perivascular pseudorosettes on histology. True ependymal rosettes are less common. • Rosettes = halo or spoke-wheel arrangement of cells surrounding central core or hub (empty or filled) • Perivascular pseudorosette = spoke-wheel arrangement of cells surrounds central vessel (native vessel) • True ependymal rosette = cells surround empty-appearing lumen
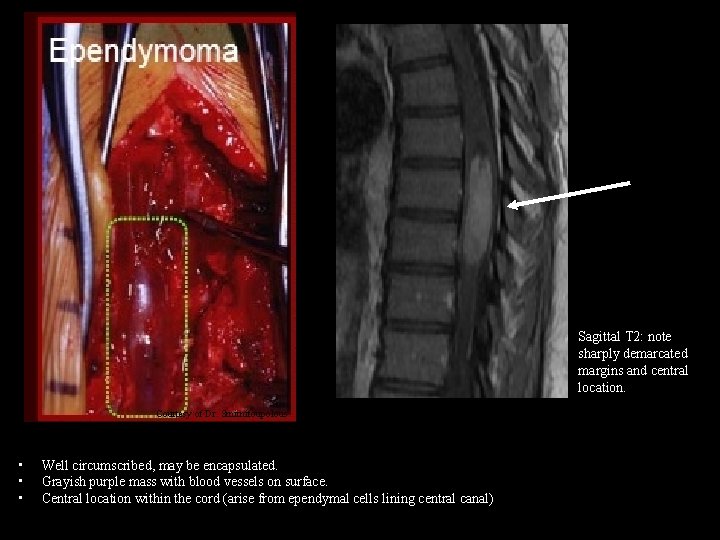
Sagittal T 2: note sharply demarcated margins and central location. Courtesy of Dr. Smirnitoupolous. • • • Well circumscribed, may be encapsulated. Grayish purple mass with blood vessels on surface. Central location within the cord (arise from ependymal cells lining central canal)
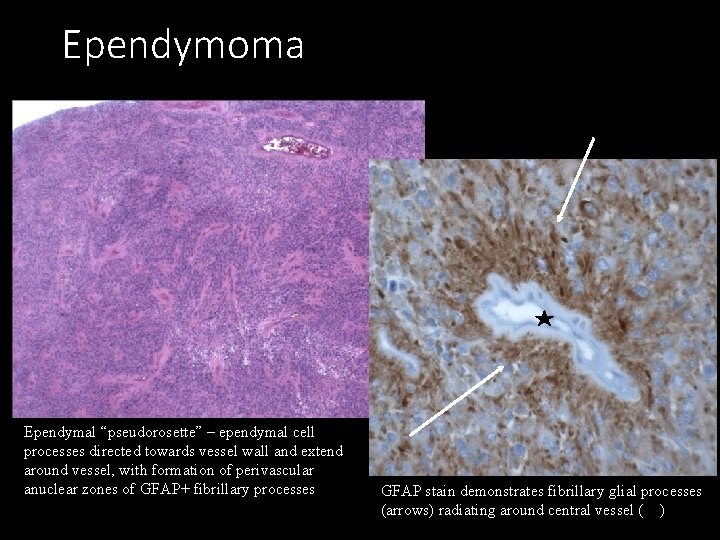
Ependymoma Ependymal “pseudorosette” – ependymal cell processes directed towards vessel wall and extend around vessel, with formation of perivascular anuclear zones of GFAP+ fibrillary processes GFAP stain demonstrates fibrillary glial processes (arrows) radiating around central vessel ( )
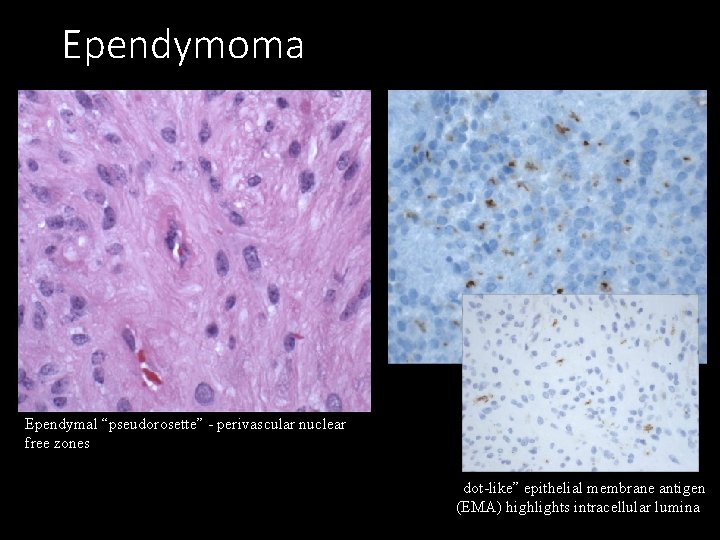
Ependymoma Ependymal “pseudorosette” - perivascular nuclear free zones “dot-like” epithelial membrane antigen (EMA) highlights intracellular lumina
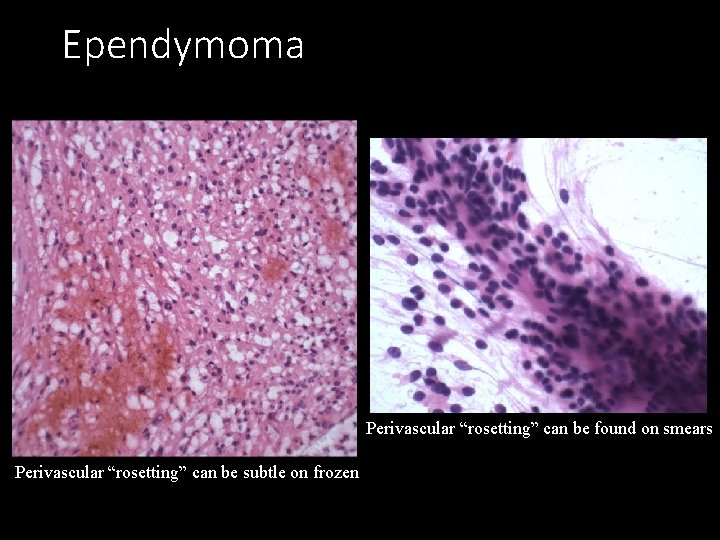
Ependymoma Perivascular “rosetting” can be found on smears Perivascular “rosetting” can be subtle on frozen
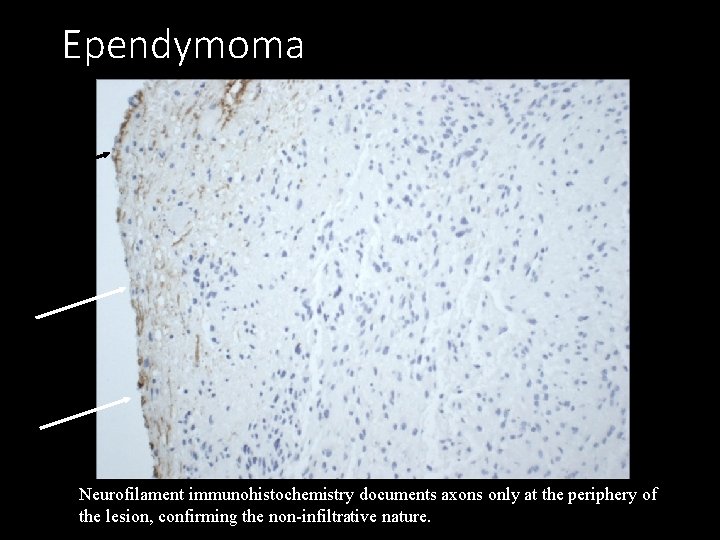
Ependymoma Neurofilament immunohistochemistry documents axons only at the periphery of the lesion, confirming the non-infiltrative nature.
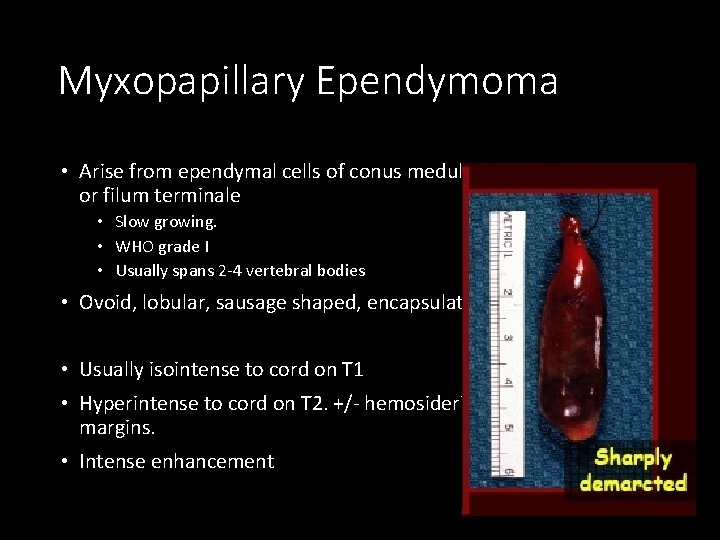
Myxopapillary Ependymoma • Arise from ependymal cells of conus medullaris or filum terminale • Slow growing. • WHO grade I • Usually spans 2 -4 vertebral bodies • Ovoid, lobular, sausage shaped, encapsulated. • Usually isointense to cord on T 1 • Hyperintense to cord on T 2. +/- hemosiderin at margins. • Intense enhancement Courtesy of Dr. Smirnitoupolous.
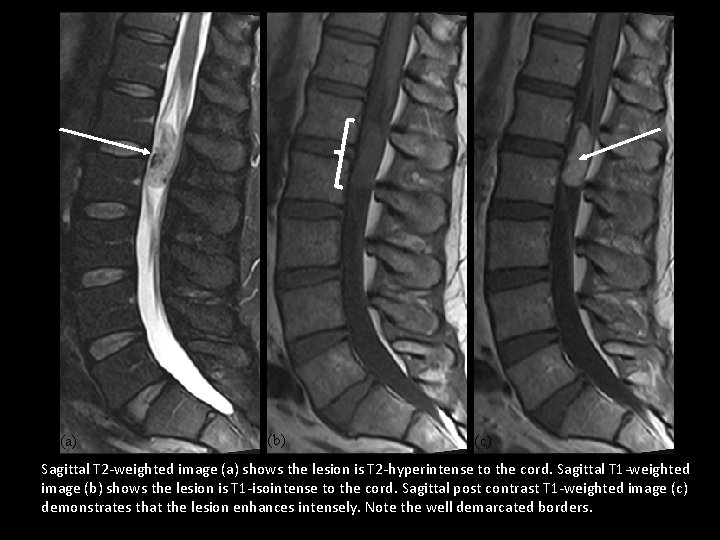
(a) (b) (c) Sagittal T 2 -weighted image (a) shows the lesion is T 2 -hyperintense to the cord. Sagittal T 1 -weighted image (b) shows the lesion is T 1 -isointense to the cord. Sagittal post contrast T 1 -weighted image (c) demonstrates that the lesion enhances intensely. Note the well demarcated borders.
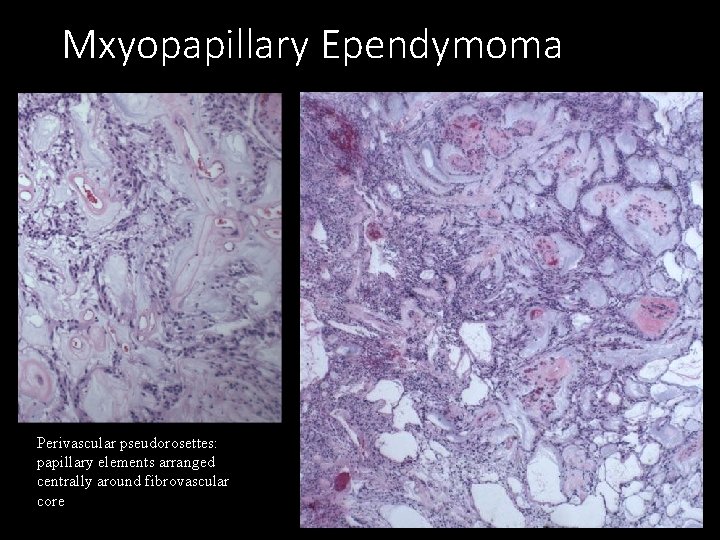
Mxyopapillary Ependymoma Perivascular pseudorosettes: papillary elements arranged centrally around fibrovascular core
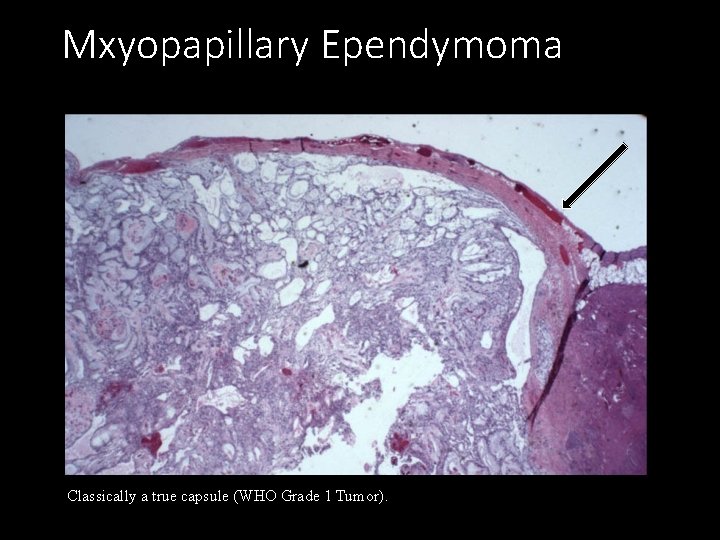
Mxyopapillary Ependymoma Classically a true capsule (WHO Grade 1 Tumor).
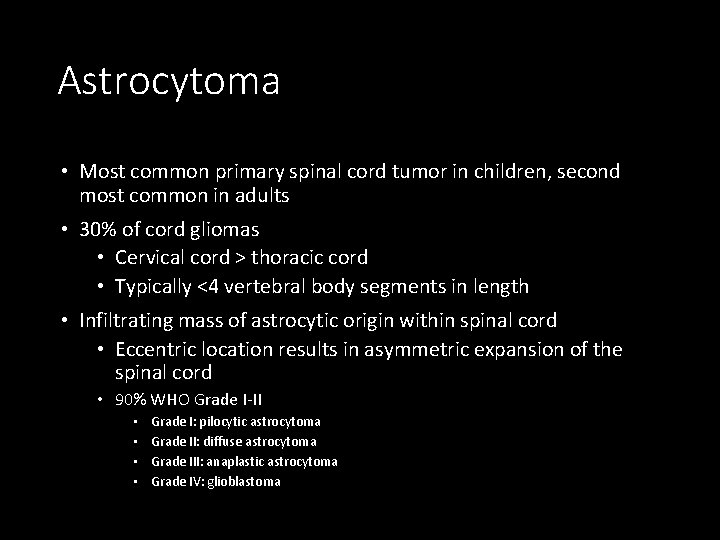
Astrocytoma • Most common primary spinal cord tumor in children, second most common in adults • 30% of cord gliomas • Cervical cord > thoracic cord • Typically <4 vertebral body segments in length • Infiltrating mass of astrocytic origin within spinal cord • Eccentric location results in asymmetric expansion of the spinal cord • 90% WHO Grade I-II • • Grade I: pilocytic astrocytoma Grade II: diffuse astrocytoma Grade III: anaplastic astrocytoma Grade IV: glioblastoma
Astrocytoma • Signal characteristics: • Hypo/isointense to normal cord on T 1 • Hyperintense to normal cord on T 2 • Almost always enhance on post-contrast sequences but can be patchy and irregular (enhancing regions are targets for biopsy) • Associations: • • Hemorrhage or hemosiderin cap is uncommon Cystic components May have exophytic components May cause syrinx
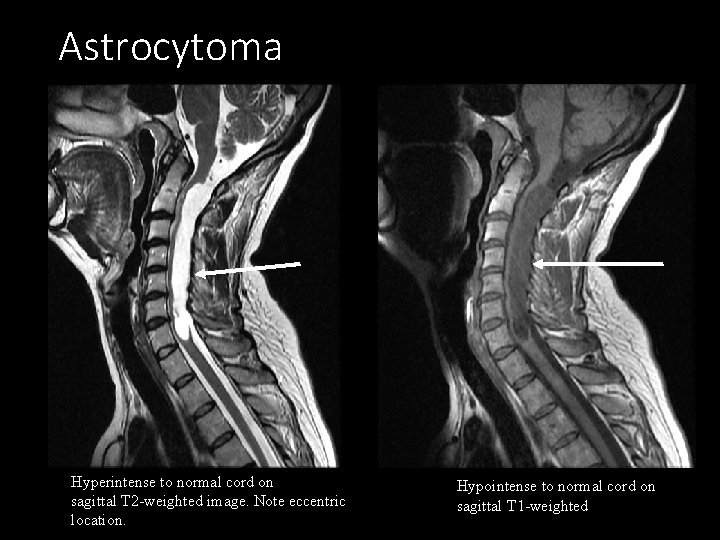
Astrocytoma Hyperintense to normal cord on sagittal T 2 -weighted image. Note eccentric location. Hypointense to normal cord on sagittal T 1 -weighted
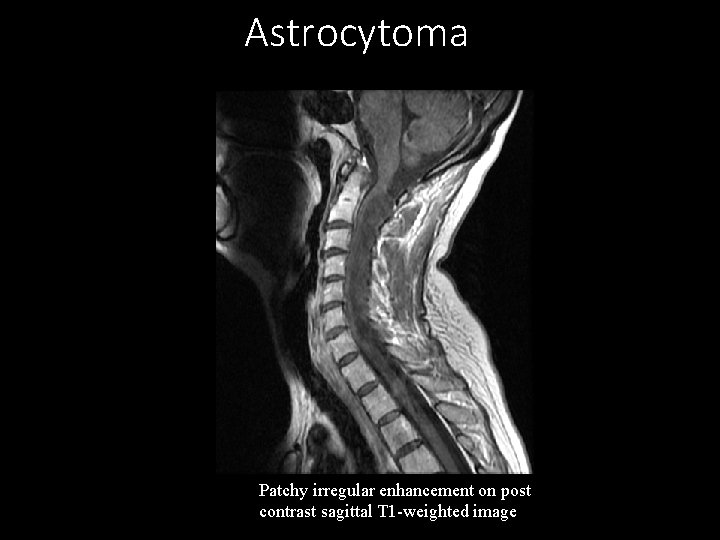
Astrocytoma Patchy irregular enhancement on post contrast sagittal T 1 -weighted image
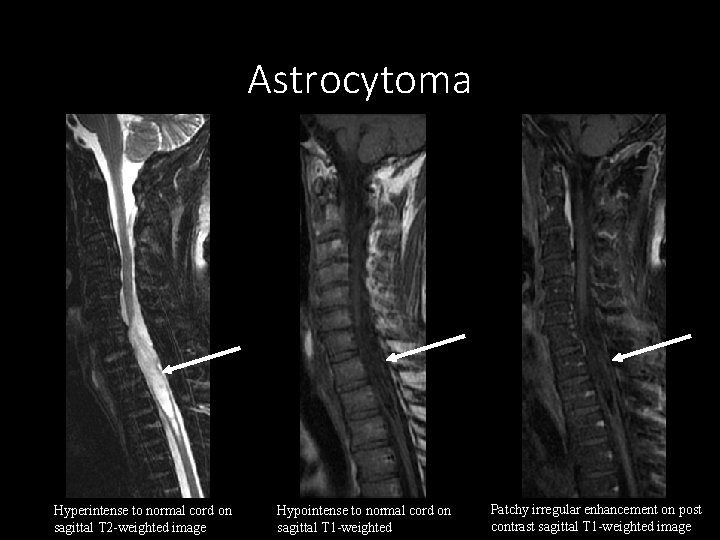
Astrocytoma Hyperintense to normal cord on sagittal T 2 -weighted image Hypointense to normal cord on sagittal T 1 -weighted Patchy irregular enhancement on post contrast sagittal T 1 -weighted image
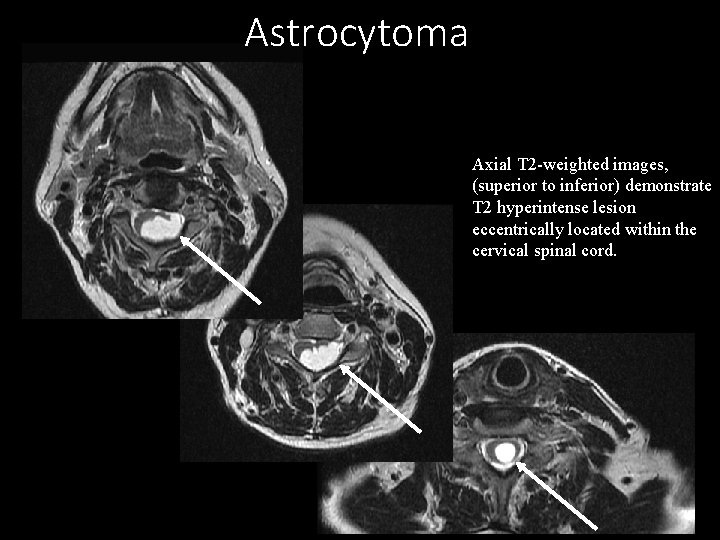
Astrocytoma Axial T 2 -weighted images, (superior to inferior) demonstrate T 2 hyperintense lesion eccentrically located within the cervical spinal cord.
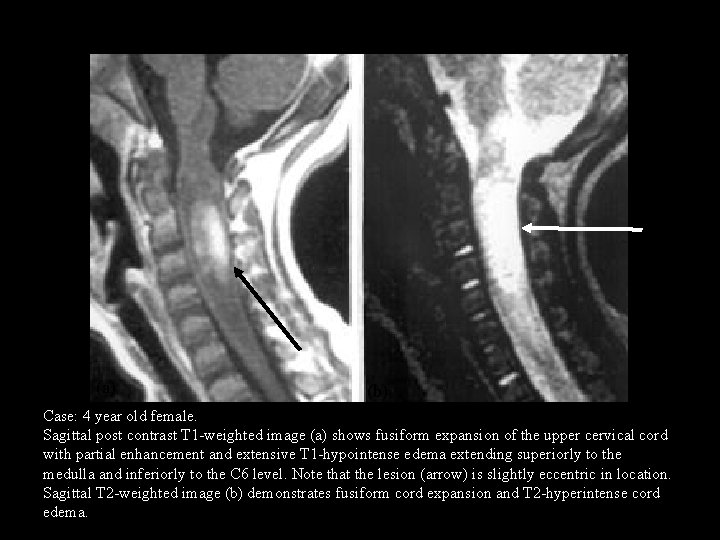
(a) (b) Case: 4 year old female. Sagittal post contrast T 1 -weighted image (a) shows fusiform expansion of the upper cervical cord with partial enhancement and extensive T 1 -hypointense edema extending superiorly to the medulla and inferiorly to the C 6 level. Note that the lesion (arrow) is slightly eccentric in location. Sagittal T 2 -weighted image (b) demonstrates fusiform cord expansion and T 2 -hyperintense cord edema.
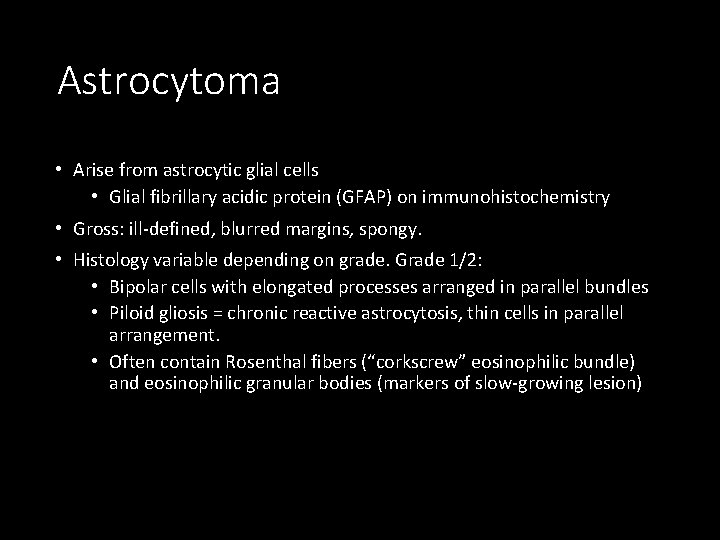
Astrocytoma • Arise from astrocytic glial cells • Glial fibrillary acidic protein (GFAP) on immunohistochemistry • Gross: ill-defined, blurred margins, spongy. • Histology variable depending on grade. Grade 1/2: • Bipolar cells with elongated processes arranged in parallel bundles • Piloid gliosis = chronic reactive astrocytosis, thin cells in parallel arrangement. • Often contain Rosenthal fibers (“corkscrew” eosinophilic bundle) and eosinophilic granular bodies (markers of slow-growing lesion)
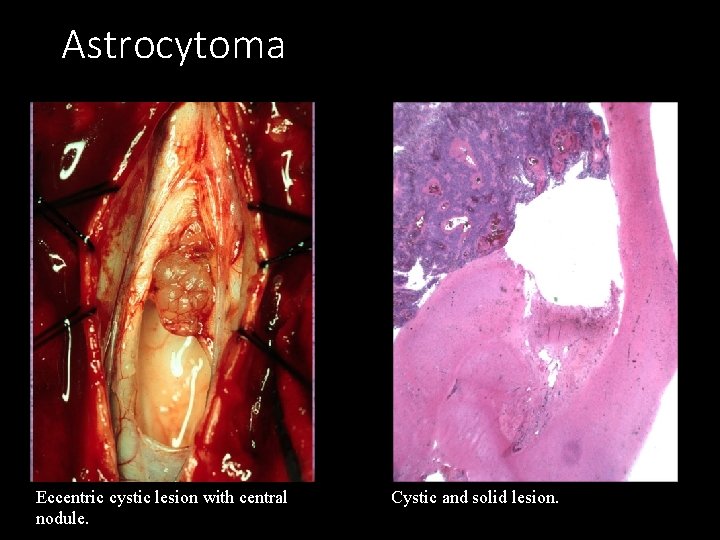
Astrocytoma Eccentric cystic lesion with central nodule. Cystic and solid lesion.
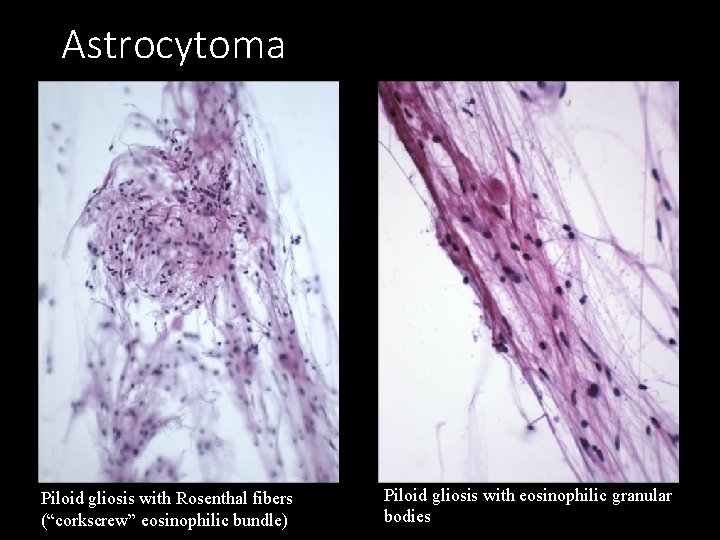
Astrocytoma Piloid gliosis with Rosenthal fibers (“corkscrew” eosinophilic bundle) Piloid gliosis with eosinophilic granular bodies
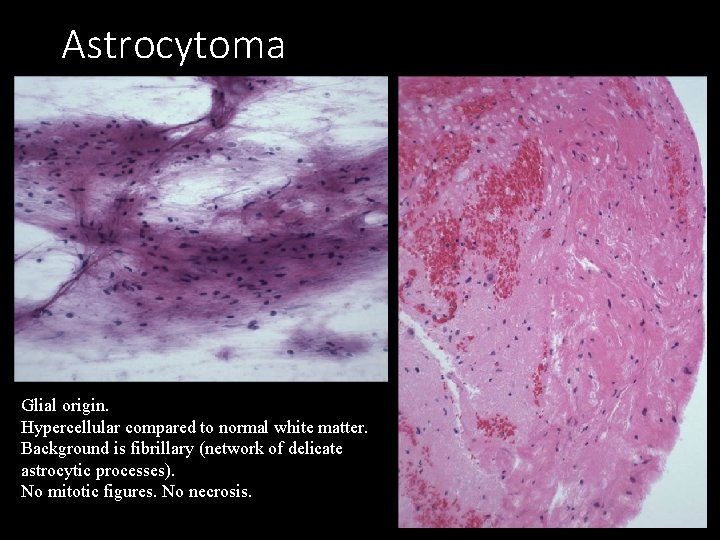
Astrocytoma Glial origin. Hypercellular compared to normal white matter. Background is fibrillary (network of delicate astrocytic processes). No mitotic figures. No necrosis.
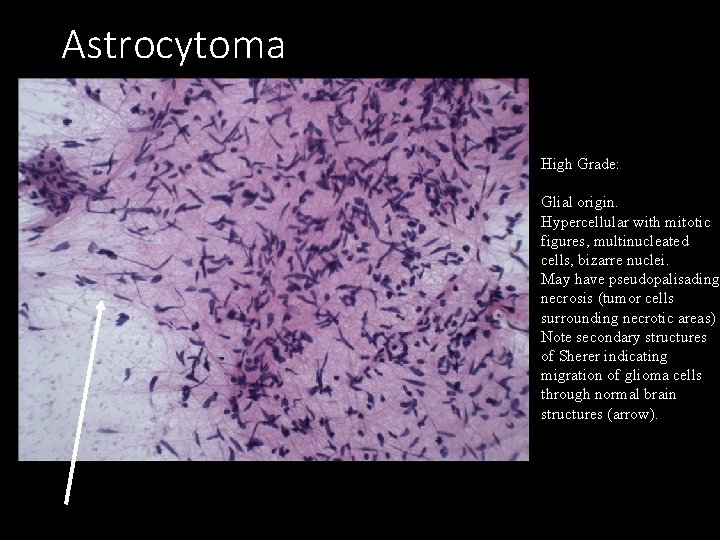
Astrocytoma High Grade: Glial origin. Hypercellular with mitotic figures, multinucleated cells, bizarre nuclei. May have pseudopalisading necrosis (tumor cells surrounding necrotic areas) Note secondary structures of Sherer indicating migration of glioma cells through normal brain structures (arrow).
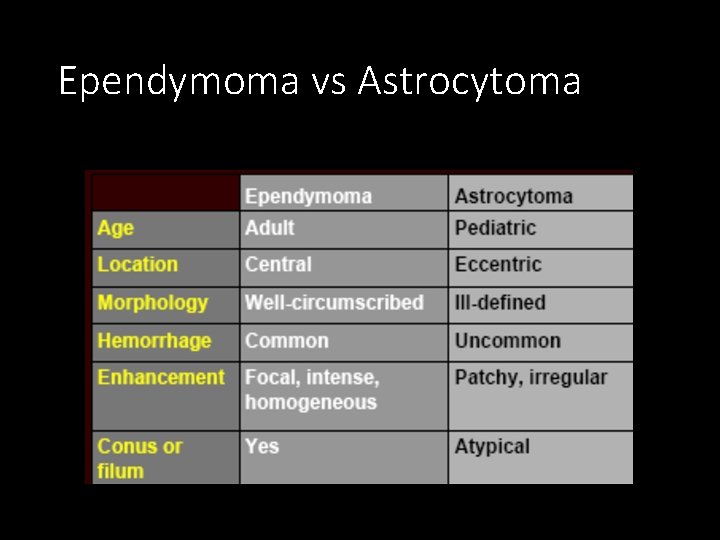
Ependymoma vs Astrocytoma Koeller et al, Radio. Graphics 2000; 20: 1721 -1749.
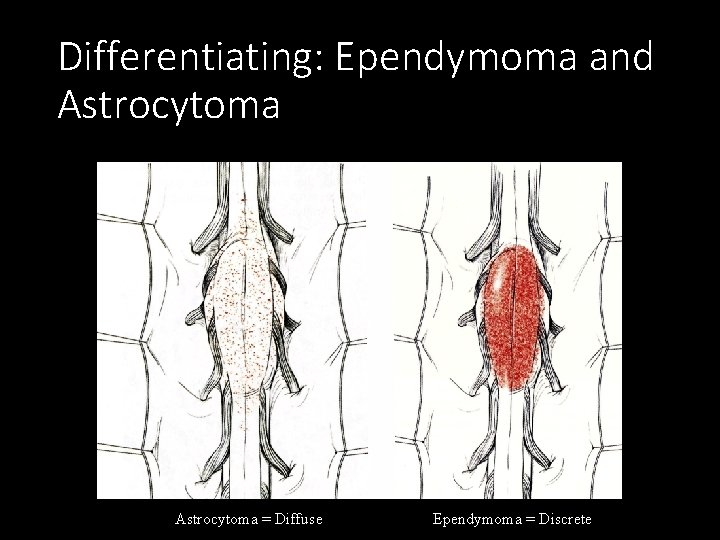
Differentiating: Ependymoma and Astrocytoma = Diffuse Ependymoma = Discrete
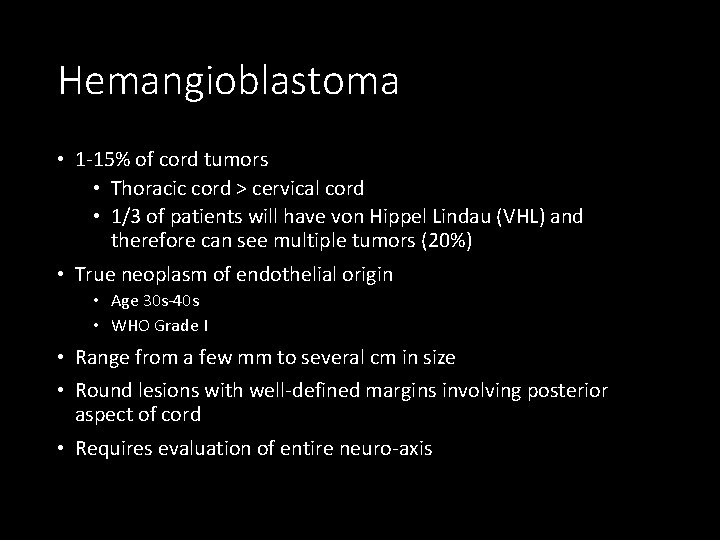
Hemangioblastoma • 1 -15% of cord tumors • Thoracic cord > cervical cord • 1/3 of patients will have von Hippel Lindau (VHL) and therefore can see multiple tumors (20%) • True neoplasm of endothelial origin • Age 30 s-40 s • WHO Grade I • Range from a few mm to several cm in size • Round lesions with well-defined margins involving posterior aspect of cord • Requires evaluation of entire neuro-axis
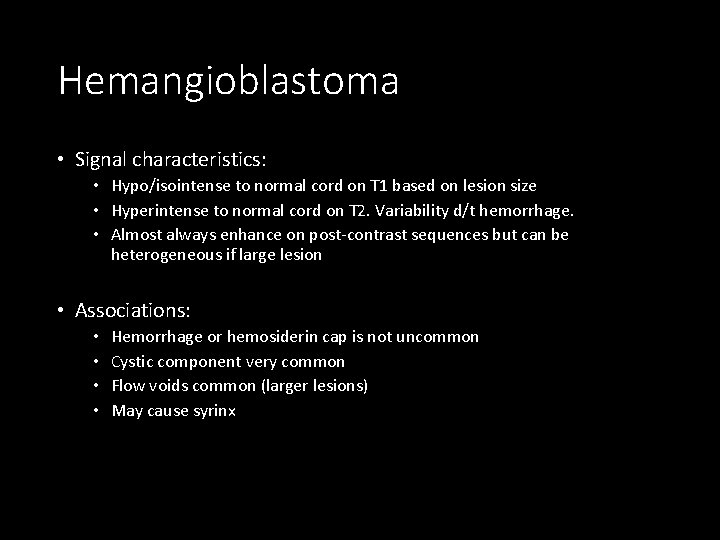
Hemangioblastoma • Signal characteristics: • Hypo/isointense to normal cord on T 1 based on lesion size • Hyperintense to normal cord on T 2. Variability d/t hemorrhage. • Almost always enhance on post-contrast sequences but can be heterogeneous if large lesion • Associations: • • Hemorrhage or hemosiderin cap is not uncommon Cystic component very common Flow voids common (larger lesions) May cause syrinx
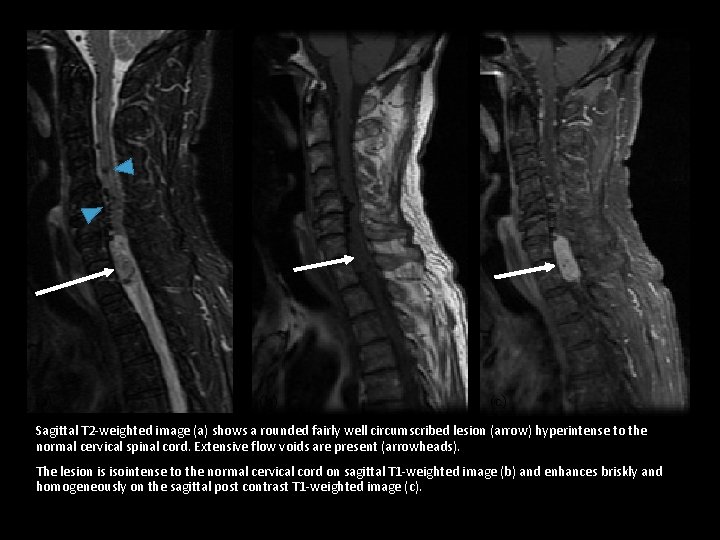
(a) (b) (c) Sagittal T 2 -weighted image (a) shows a rounded fairly well circumscribed lesion (arrow) hyperintense to the normal cervical spinal cord. Extensive flow voids are present (arrowheads). The lesion is isointense to the normal cervical cord on sagittal T 1 -weighted image (b) and enhances briskly and homogeneously on the sagittal post contrast T 1 -weighted image (c).
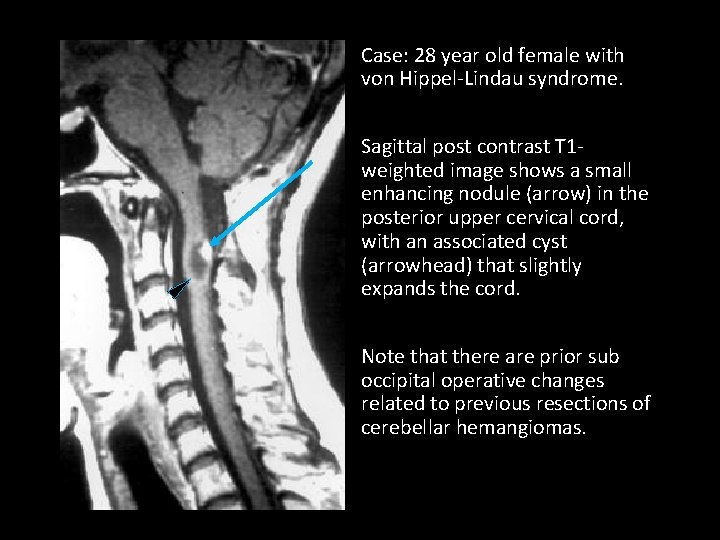
Case: 28 year old female with von Hippel-Lindau syndrome. Sagittal post contrast T 1 weighted image shows a small enhancing nodule (arrow) in the posterior upper cervical cord, with an associated cyst (arrowhead) that slightly expands the cord. Note that there are prior sub occipital operative changes related to previous resections of cerebellar hemangiomas.
Hemangioblastoma • Benign. • Highly vascular. • Frequently associated with cysts. • Well circumscribed. • On histology, large pale stromal cells (neoplastic cells with clear cytoplasm) between blood vessels.
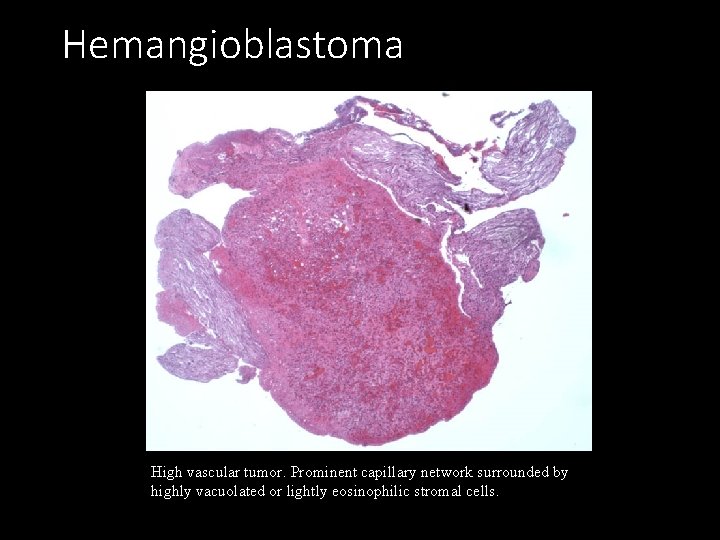
Hemangioblastoma High vascular tumor. Prominent capillary network surrounded by highly vacuolated or lightly eosinophilic stromal cells.
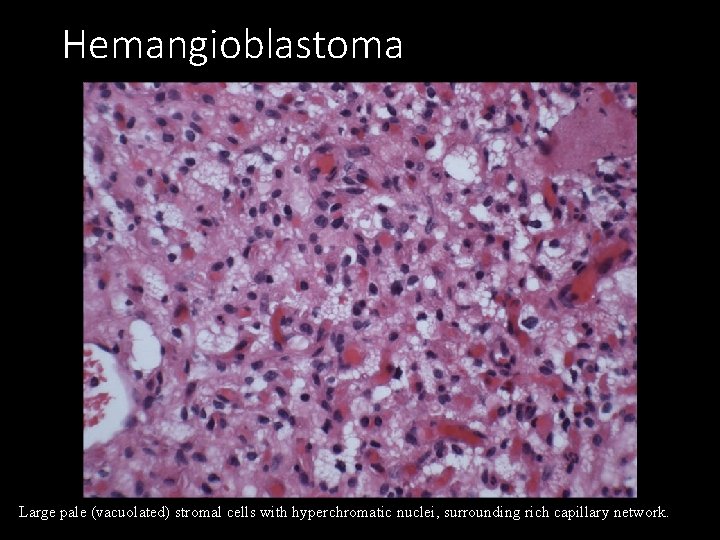
Hemangioblastoma Large pale (vacuolated) stromal cells with hyperchromatic nuclei, surrounding rich capillary network.
Metastatic Disease • Rare (<1% of general autopsies) • Typically seen in advanced cancer cases but as patients are living longer, there is increased prevalence • Median survival if treated 4 -6 months; without 4 -6 weeks • May be the first presentation of cancer in 20% of patients • Full craniospinal imaging for evaluation • MRI more sensitive than CSF cytology which can be falsely negative in up to 40% cases
Metastatic Disease • CNS metastases more commonly vertebral, leptomeningeal carcinomatosis, drop metastases • Represent ~4% of CNS metastases • Hematogenous dissemination (lung, breast, melanoma) • Lung, breast two most common primaries • Primary CNS tumors (GBM, ependymoma, anaplastic astrocytoma) • Leukemia/lymphoma
Metastatic Disease • Well circumscribed small enhancing lesion with extensive edema on MRI. • Smooth or nodular enhancement along spinal cord, including the conus medullaris, and/or the cauda equina • +/- syrinx

Metastatic Disease (a) (b) (c) Metastatic Breast Cancer: Sagittal T 2 -weighted image (a) show small well-circumscribed intramedullary lesion with extensive edema in the mid-thoracic spine. The lesion is iso-intense to normal spinal cord on sagittal T 1 (b) and demonstrates enhancement on the sagittal post contrast T 1 -weighted image (c).
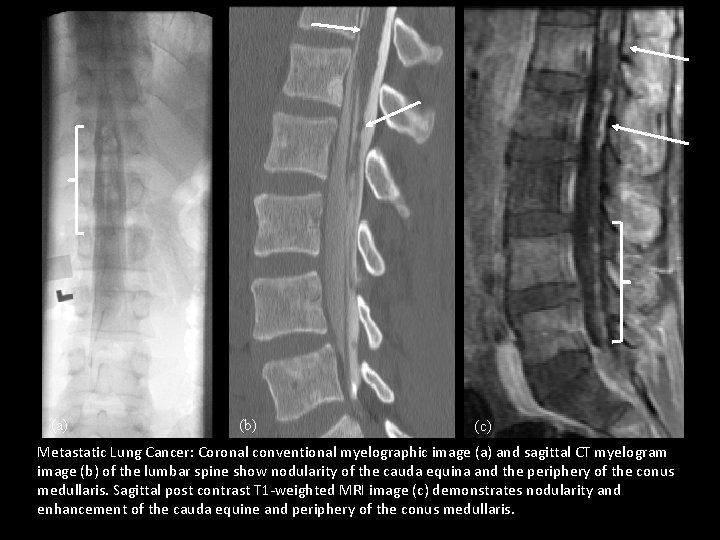
(a) (b) (c) Metastatic Lung Cancer: Coronal conventional myelographic image (a) and sagittal CT myelogram image (b) of the lumbar spine show nodularity of the cauda equina and the periphery of the conus medullaris. Sagittal post contrast T 1 -weighted MRI image (c) demonstrates nodularity and enhancement of the cauda equine and periphery of the conus medullaris.
Metastatic Disease • Will correlate with the primary malignancy.
Summary • Geography is destiny. • Try to localize the spinal tumor: • Intramedullary • Intradural-extramedullary • Extradural • Is the lesion solid or cystic? • Is the lesion single or multiple?
END
- Slides: 53