Radiology Pathology Brain Pathology Before You Begin This
Radiology - Pathology Brain Pathology
Before You Begin This module is intended primarily for pre-clinical students learning or reviewing pathophysiology. Please note that this series will focus on how pathology presents in imaging studies. It assumes familiarity with fundamental anatomy. If you need to learn or review this core concept, please visit the “Anatomy” section of our website. If material is repeated from another module, it will be outlined as this text is so that you are aware
Structure and function of the brain • Layers of neurons and glial cells form the gray matter, which peripherally lines the gyri. Additional deep gray matter is present in the basal ganglia and thalami • Deeper white matter tracts are composed of glial cells and myelinated nerve fibers, and is less densely cellular than gray matter • Ventricles and subarachnoid space are filled with CSF. These spaces become more apparent with volume loss and some pathologic conditions • The posterior fossa, including the brainstem and cerebellum, contain highly organized white matter tracts as well as gray matter
CT appearance of the normal brain • Limited contrast resolution between gray and white matter; gray matter is hyperdense (whiter) compared to white matter due to cellularity • Contrast resolution also limits evaluation of smaller white matter lesions • X-rays must penetrate the calvarium, often leading to artifact, particularly at the skull base and in the posterior fossa • Good for the evaluation of intracranial hemorrhage, volume loss, hydrocephalus
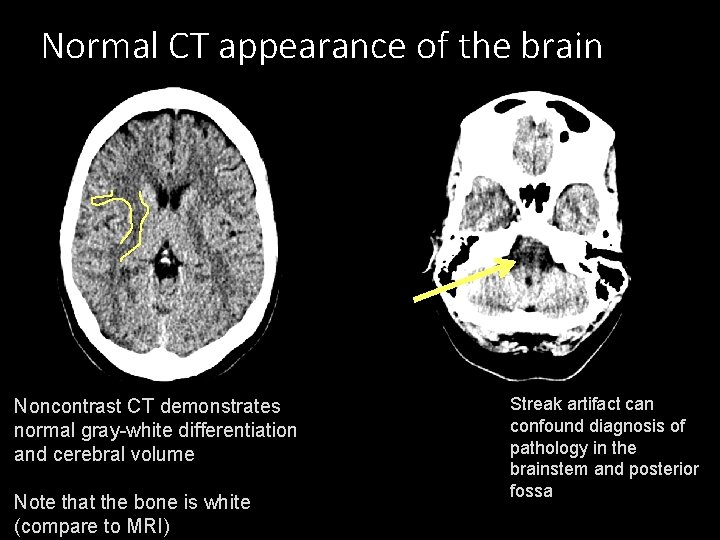
Normal CT appearance of the brain * * Noncontrast CT demonstrates normal gray-white differentiation and cerebral volume Note that the bone is white (compare to MRI) Streak artifact can confound diagnosis of pathology in the brainstem and posterior fossa
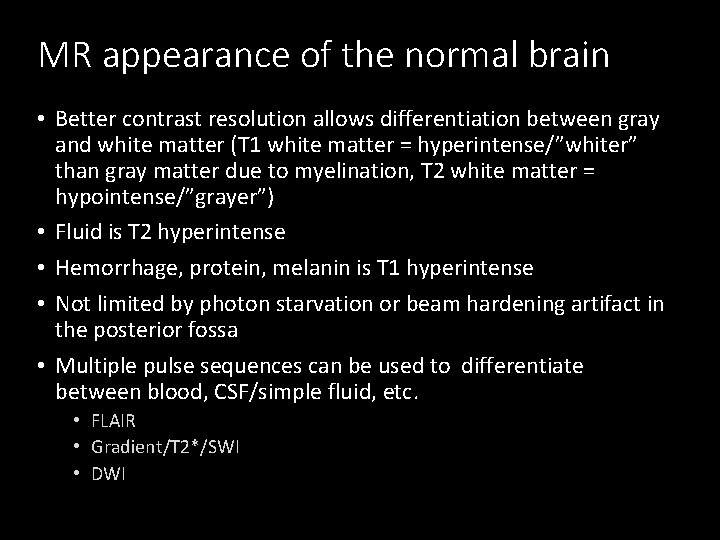
MR appearance of the normal brain • Better contrast resolution allows differentiation between gray and white matter (T 1 white matter = hyperintense/”whiter” than gray matter due to myelination, T 2 white matter = hypointense/”grayer”) • Fluid is T 2 hyperintense • Hemorrhage, protein, melanin is T 1 hyperintense • Not limited by photon starvation or beam hardening artifact in the posterior fossa • Multiple pulse sequences can be used to differentiate between blood, CSF/simple fluid, etc. • FLAIR • Gradient/T 2*/SWI • DWI
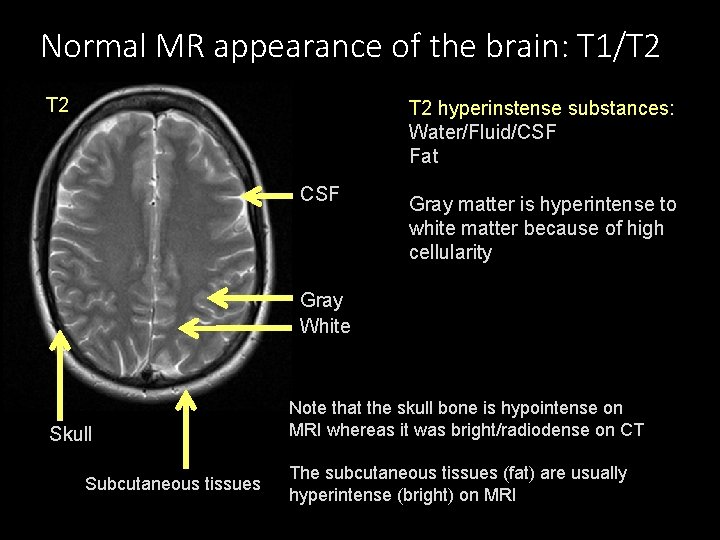
Normal MR appearance of the brain: T 1/T 2 T 2 hyperinstense substances: Water/Fluid/CSF Fat CSF * Gray matter is hyperintense to white matter because of high cellularity Gray White Skull Subcutaneous tissues Note that the skull bone is hypointense on MRI whereas it was bright/radiodense on CT The subcutaneous tissues (fat) are usually hyperintense (bright) on MRI
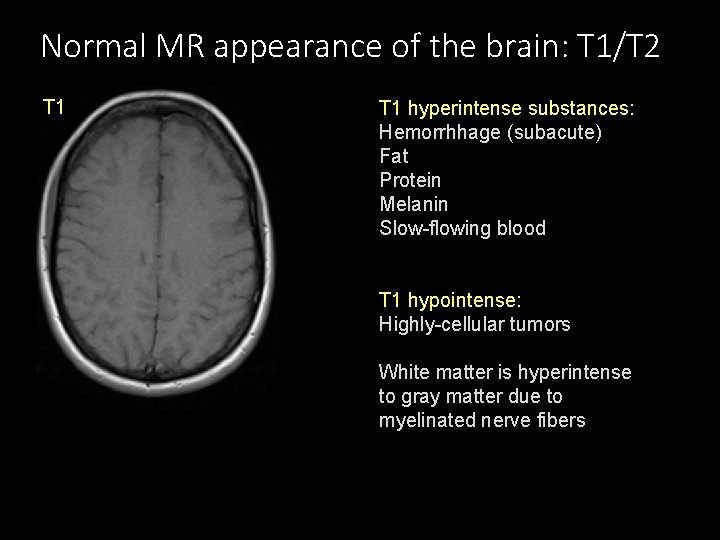
Normal MR appearance of the brain: T 1/T 2 T 1 hyperintense substances: Hemorrhhage (subacute) Fat Protein Melanin Slow-flowing blood * T 1 hypointense: Highly-cellular tumors White matter is hyperintense to gray matter due to myelinated nerve fibers
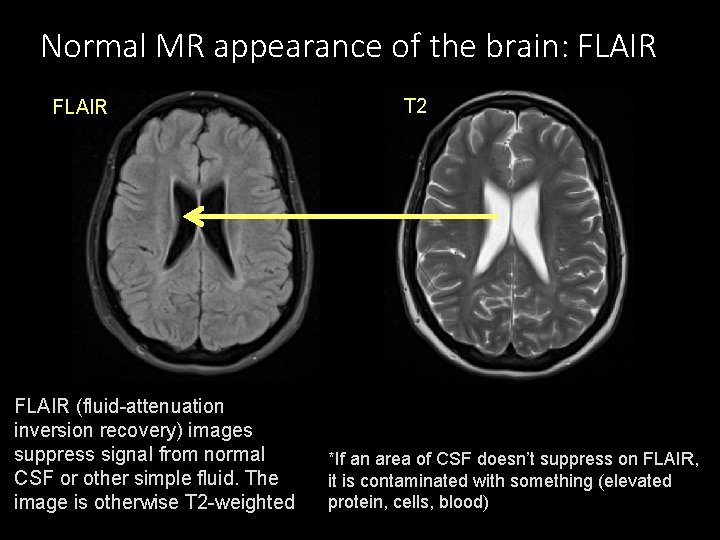
Normal MR appearance of the brain: FLAIR T 2 FLAIR * * FLAIR (fluid-attenuation inversion recovery) images suppress signal from normal CSF or other simple fluid. The image is otherwise T 2 -weighted *If an area of CSF doesn’t suppress on FLAIR, it is contaminated with something (elevated protein, cells, blood)

Normal MR appearance of the brain: T 2* * * Gradient or susceptibility weighted images (GRE/T 2*/SWI) exploit local magnetic field inhomogeneities, making calcifications, such as in the pineal gland, more conspicuous. Because T 2* images increase artifacts, things like aneurysm clips, VP shunts, etc. can obscure large portions of the image due to “blooming”

Normal MR appearance of the brain: DWI Abnormal: Restricted Diffusion * * DWI (diffusion-weighted imaging) evaluates the free flow of water. This is disrupted when there is: Intracellular water (cytotoxic edema) Hypercellular tumor or abscess Comparison is made with the ADC (apparent diffusion coefficient) image. True restricted diffusion is bright on DWI and dark on ADC
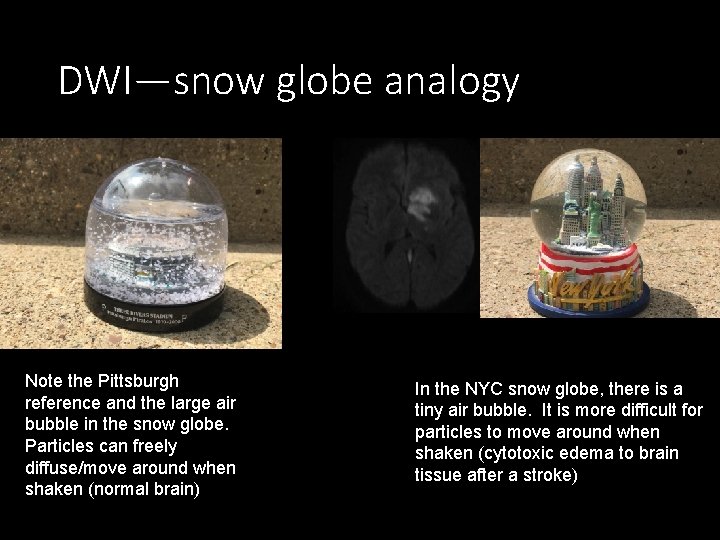
DWI—snow globe analogy Note the Pittsburgh reference and the large air bubble in the snow globe. Particles can freely diffuse/move around when shaken (normal brain) In the NYC snow globe, there is a tiny air bubble. It is more difficult for particles to move around when shaken (cytotoxic edema to brain tissue after a stroke)
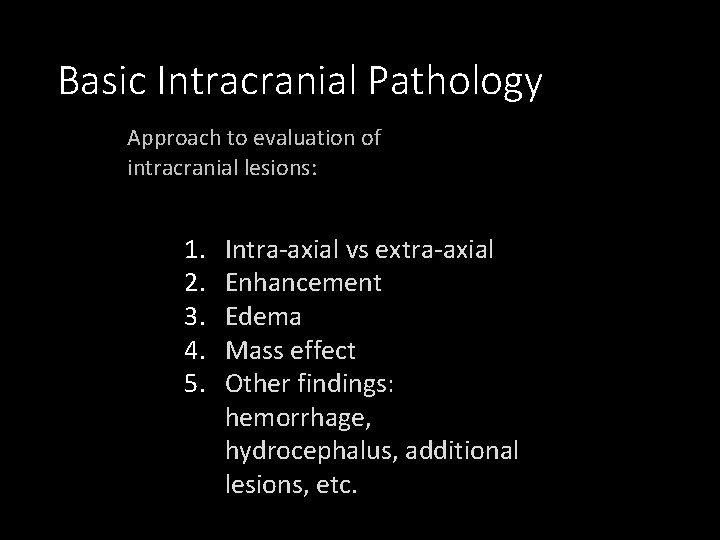
Basic Intracranial Pathology Approach to evaluation of intracranial lesions: 1. 2. 3. 4. 5. Intra-axial vs extra-axial Enhancement Edema Mass effect Other findings: hemorrhage, hydrocephalus, additional lesions, etc.
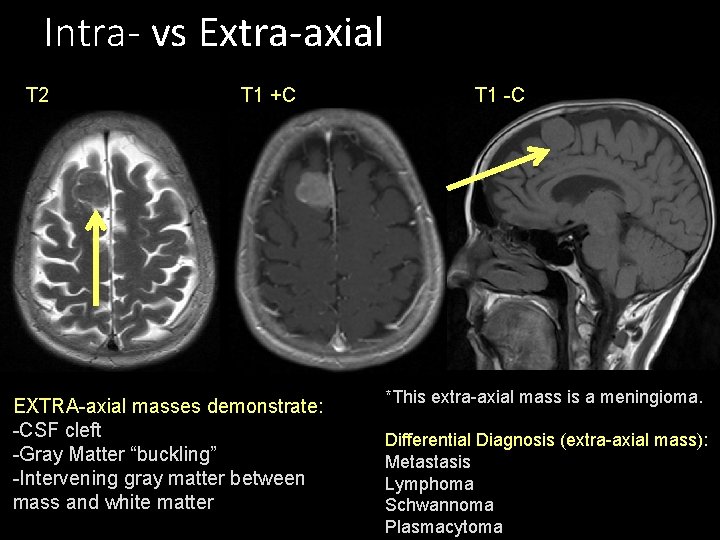
Intra- vs Extra-axial T 2 T 1 +C EXTRA-axial masses demonstrate: -CSF cleft -Gray Matter “buckling” -Intervening gray matter between mass and white matter T 1 -C *This extra-axial mass is a meningioma. Differential Diagnosis (extra-axial mass): Metastasis Lymphoma Schwannoma Plasmacytoma
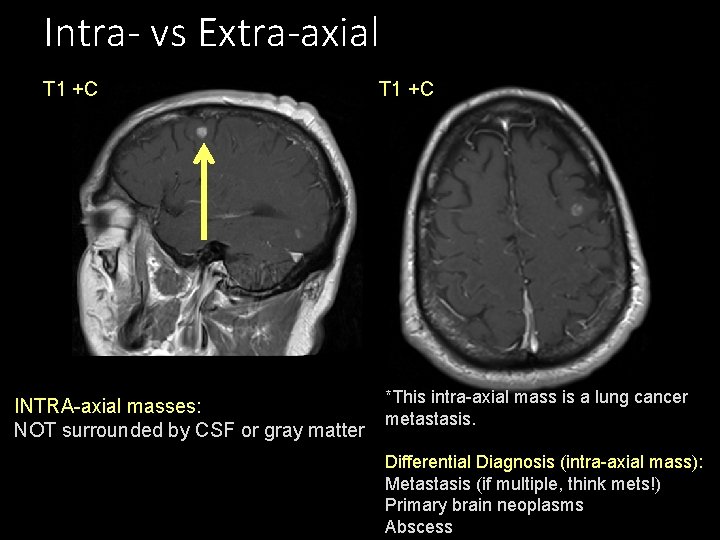
Intra- vs Extra-axial T 1 +C INTRA-axial masses: NOT surrounded by CSF or gray matter T 1 +C *This intra-axial mass is a lung cancer metastasis. Differential Diagnosis (intra-axial mass): Metastasis (if multiple, think mets!) Primary brain neoplasms Abscess
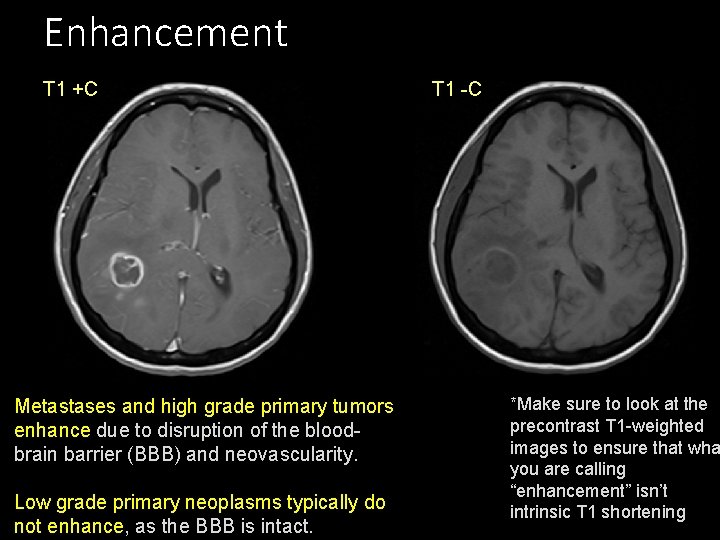
Enhancement T 1 +C Metastases and high grade primary tumors enhance due to disruption of the bloodbrain barrier (BBB) and neovascularity. Low grade primary neoplasms typically do not enhance, as the BBB is intact. T 1 -C *Make sure to look at the precontrast T 1 -weighted images to ensure that wha you are calling “enhancement” isn’t intrinsic T 1 shortening
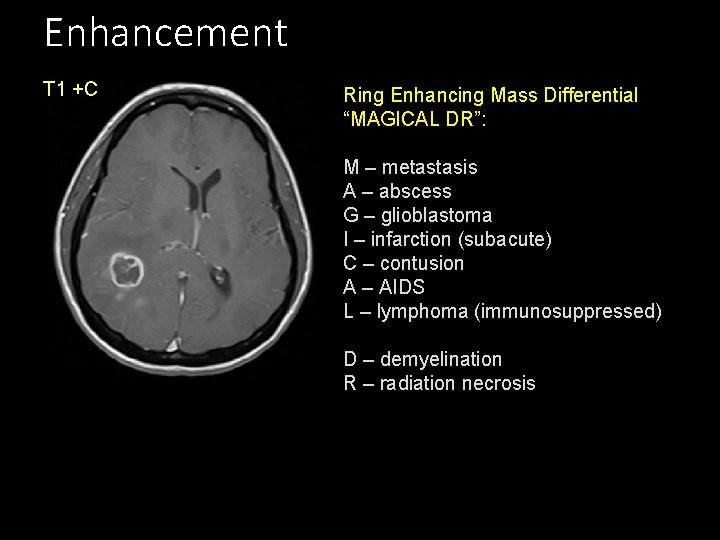
Enhancement T 1 +C Ring Enhancing Mass Differential “MAGICAL DR”: M – metastasis A – abscess G – glioblastoma I – infarction (subacute) C – contusion A – AIDS L – lymphoma (immunosuppressed) D – demyelination R – radiation necrosis
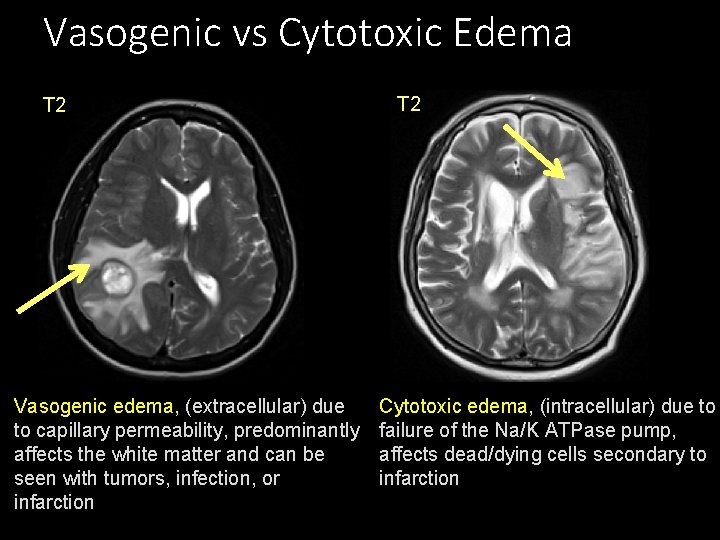
Vasogenic vs Cytotoxic Edema T 2 Vasogenic edema, (extracellular) due to capillary permeability, predominantly affects the white matter and can be seen with tumors, infection, or infarction T 2 Cytotoxic edema, (intracellular) due to failure of the Na/K ATPase pump, affects dead/dying cells secondary to infarction
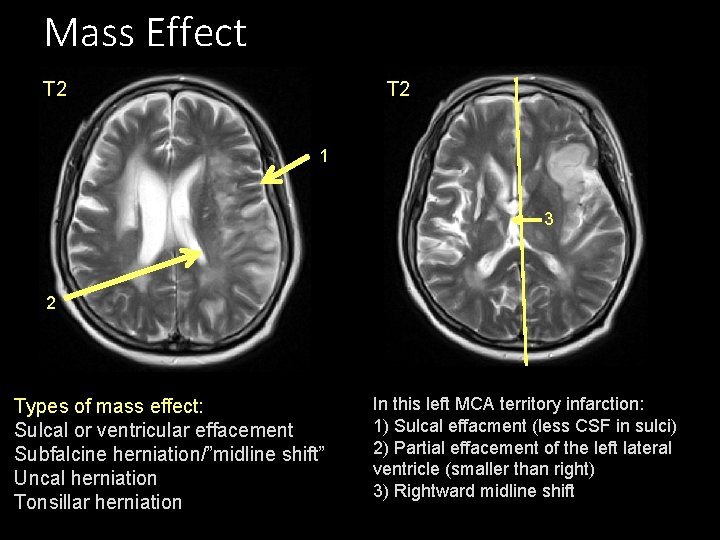
Mass Effect T 2 1 3 2 Types of mass effect: Sulcal or ventricular effacement Subfalcine herniation/”midline shift” Uncal herniation Tonsillar herniation In this left MCA territory infarction: 1) Sulcal effacment (less CSF in sulci) 2) Partial effacement of the left lateral ventricle (smaller than right) 3) Rightward midline shift
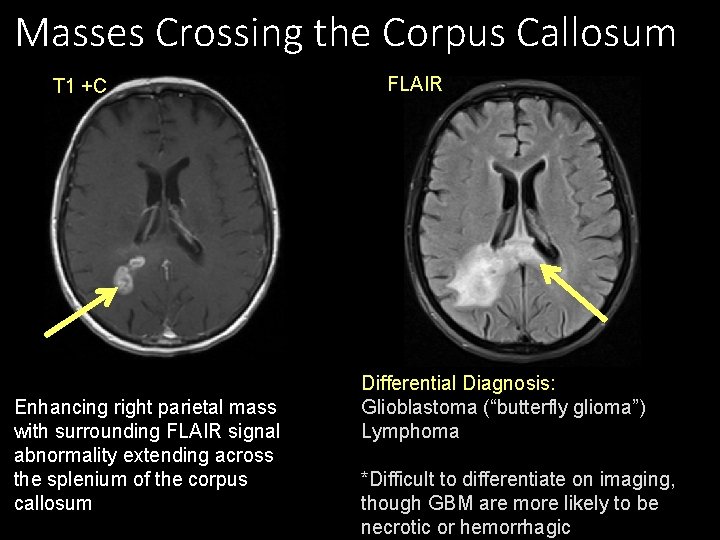
Masses Crossing the Corpus Callosum T 1 +C Enhancing right parietal mass with surrounding FLAIR signal abnormality extending across the splenium of the corpus callosum FLAIR Differential Diagnosis: Glioblastoma (“butterfly glioma”) Lymphoma *Difficult to differentiate on imaging, though GBM are more likely to be necrotic or hemorrhagic
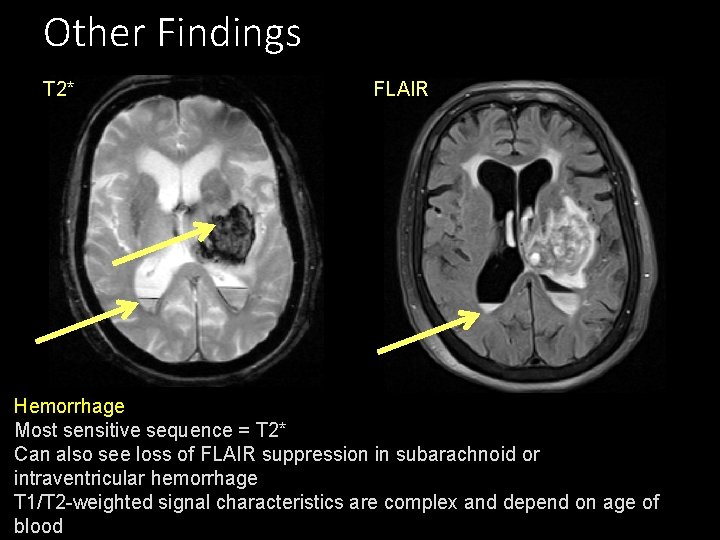
Other Findings T 2* FLAIR Hemorrhage Most sensitive sequence = T 2* Can also see loss of FLAIR suppression in subarachnoid or intraventricular hemorrhage T 1/T 2 -weighted signal characteristics are complex and depend on age of blood
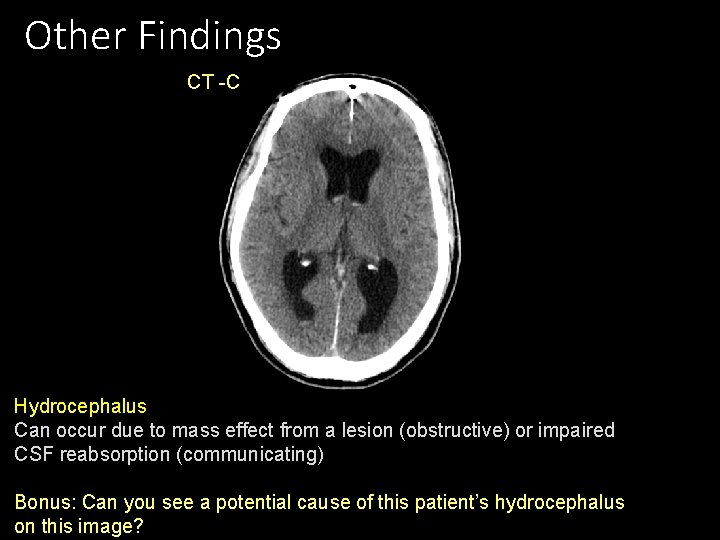
Other Findings CT -C Hydrocephalus Can occur due to mass effect from a lesion (obstructive) or impaired CSF reabsorption (communicating) Bonus: Can you see a potential cause of this patient’s hydrocephalus on this image?
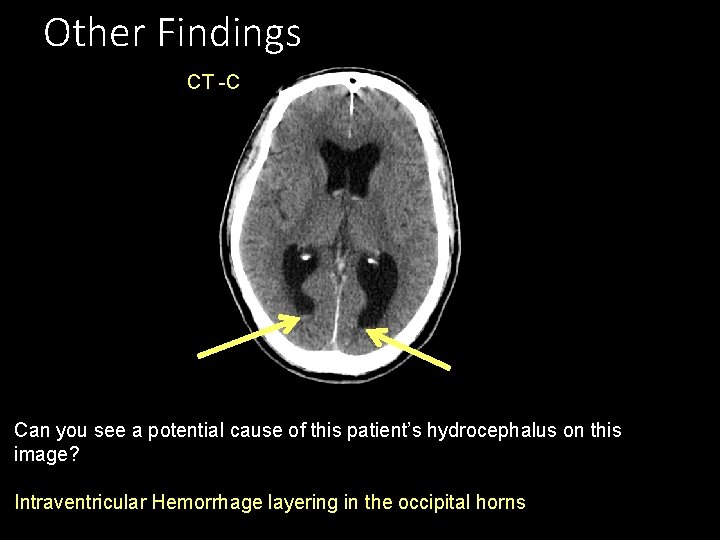
Other Findings CT -C Can you see a potential cause of this patient’s hydrocephalus on this image? Intraventricular Hemorrhage layering in the occipital horns
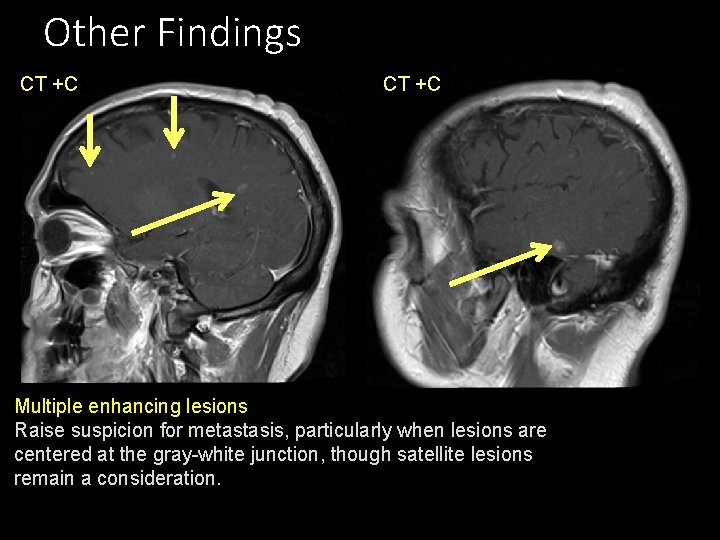
Other Findings CT +C Multiple enhancing lesions Raise suspicion for metastasis, particularly when lesions are centered at the gray-white junction, though satellite lesions remain a consideration.
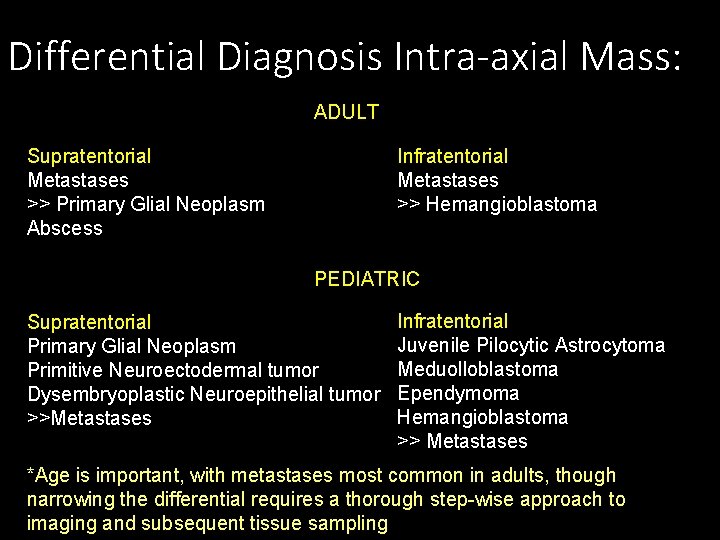
Differential Diagnosis Intra-axial Mass: ADULT Supratentorial Metastases >> Primary Glial Neoplasm Abscess Infratentorial Metastases >> Hemangioblastoma PEDIATRIC Supratentorial Primary Glial Neoplasm Primitive Neuroectodermal tumor Dysembryoplastic Neuroepithelial tumor >>Metastases Infratentorial Juvenile Pilocytic Astrocytoma Meduolloblastoma Ependymoma Hemangioblastoma >> Metastases *Age is important, with metastases most common in adults, though narrowing the differential requires a thorough step-wise approach to imaging and subsequent tissue sampling
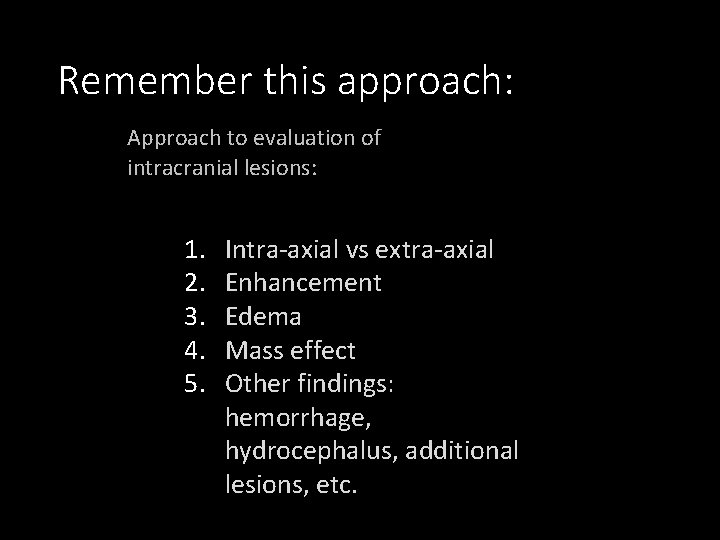
Remember this approach: Approach to evaluation of intracranial lesions: 1. 2. 3. 4. 5. Intra-axial vs extra-axial Enhancement Edema Mass effect Other findings: hemorrhage, hydrocephalus, additional lesions, etc.
Cases Use this approach to try to make the following diagnoses
Case 1 57 M with dizziness, intermittent left sided paresthesia, and cognitive decline
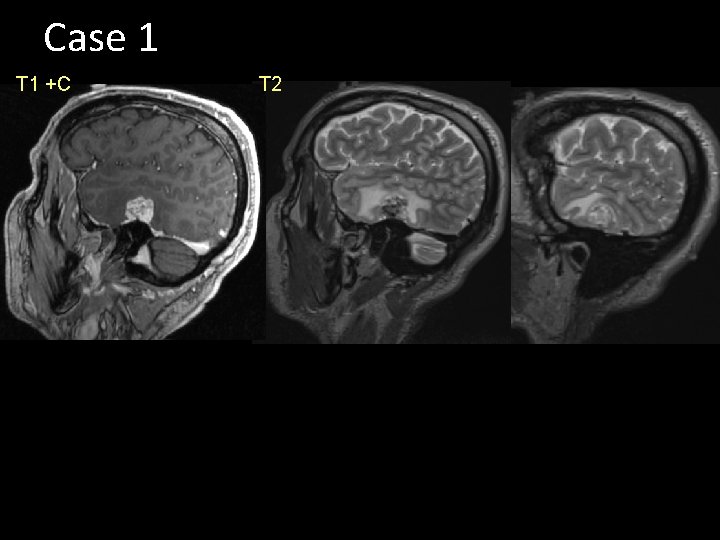
Case 1 T 1 +C T 2
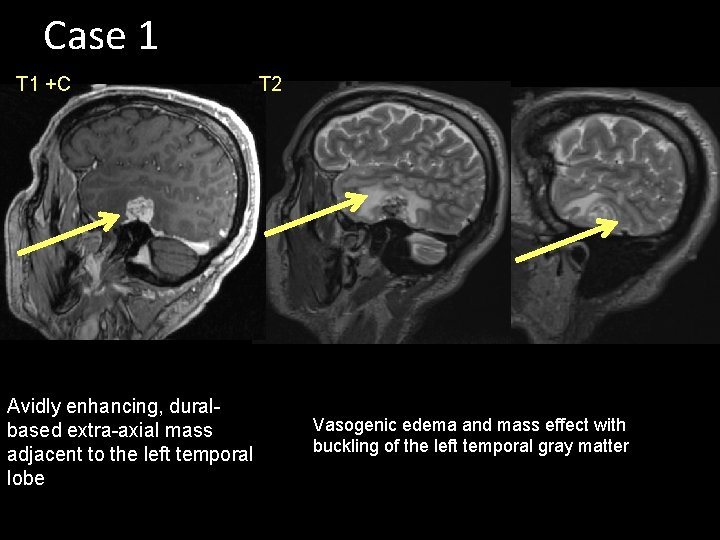
Case 1 T 1 +C Avidly enhancing, duralbased extra-axial mass adjacent to the left temporal lobe T 2 Vasogenic edema and mass effect with buckling of the left temporal gray matter
Meningioma • Avidly enhancing extra-axial, dural-based mass • Dural tail • May see susceptibility artifact if calcified • Benign WHO grade 1, but can have substantial mass effect and vasogenic edema in adjacent parenchyma, which is typically the reason for symptoms and resection.
Case 2 51 M with vertigo and ataxia
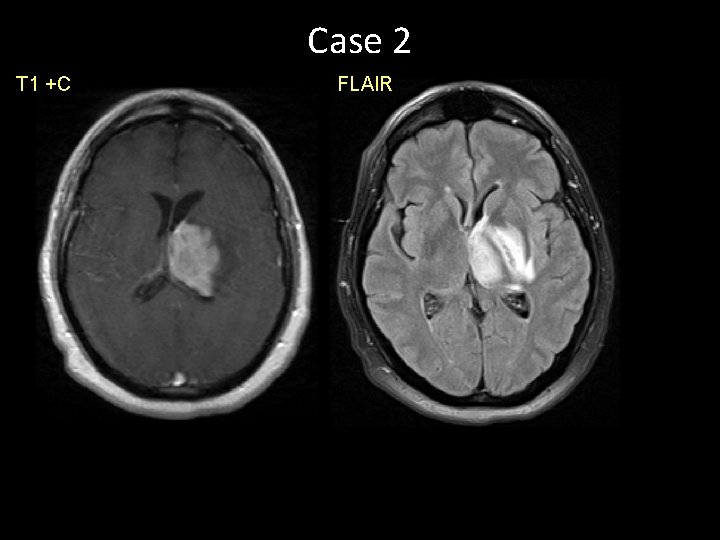
Case 2 T 1 +C FLAIR
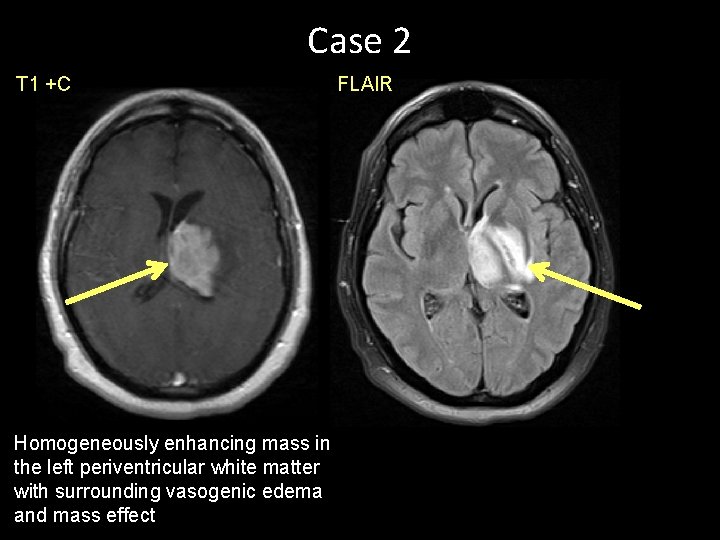
Case 2 T 1 +C Homogeneously enhancing mass in the left periventricular white matter with surrounding vasogenic edema and mass effect FLAIR
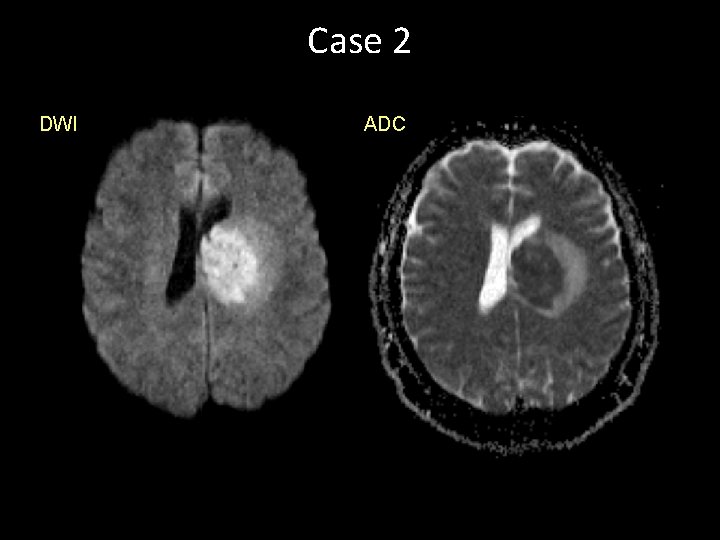
Case 2 DWI ADC
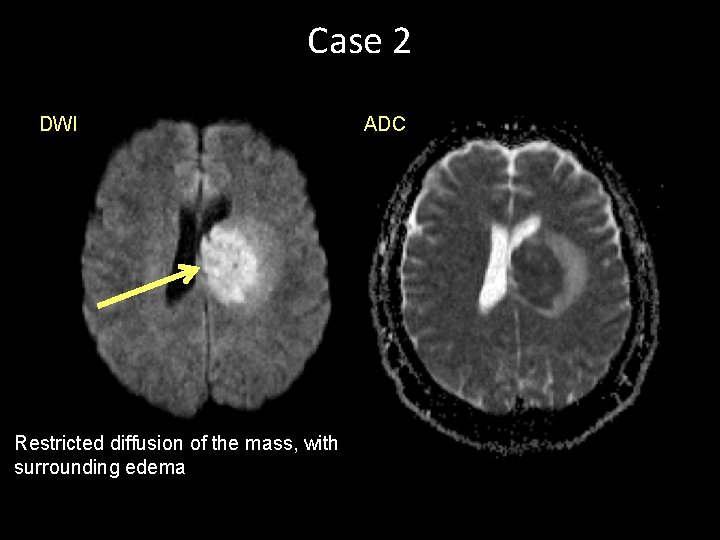
Case 2 DWI Restricted diffusion of the mass, with surrounding edema ADC
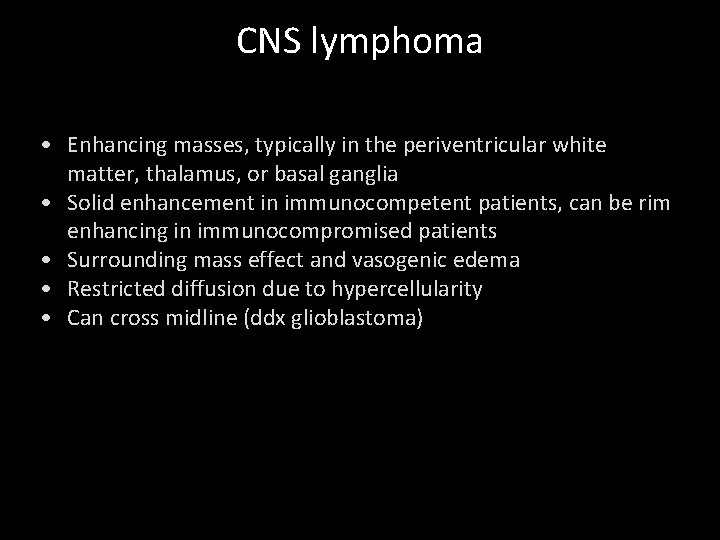
CNS lymphoma • Enhancing masses, typically in the periventricular white matter, thalamus, or basal ganglia • Solid enhancement in immunocompetent patients, can be rim enhancing in immunocompromised patients • Surrounding mass effect and vasogenic edema • Restricted diffusion due to hypercellularity • Can cross midline (ddx glioblastoma)
Case 3 65 M with lung cancer and altered mental status
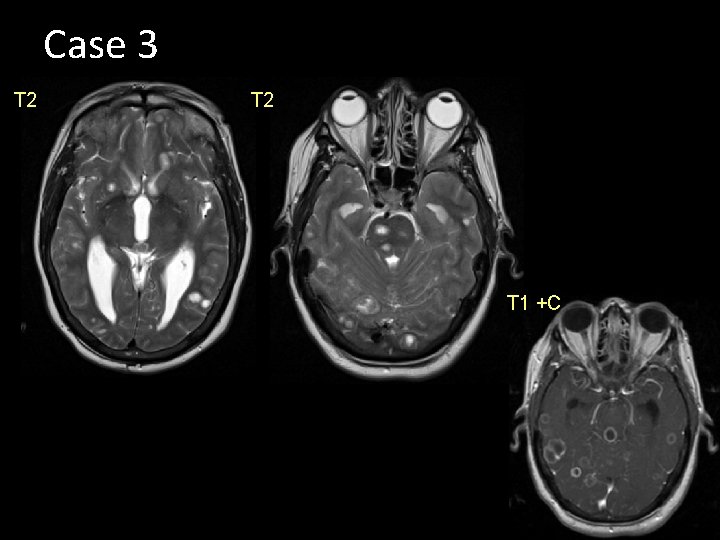
Case 3 T 2 T 1 +C
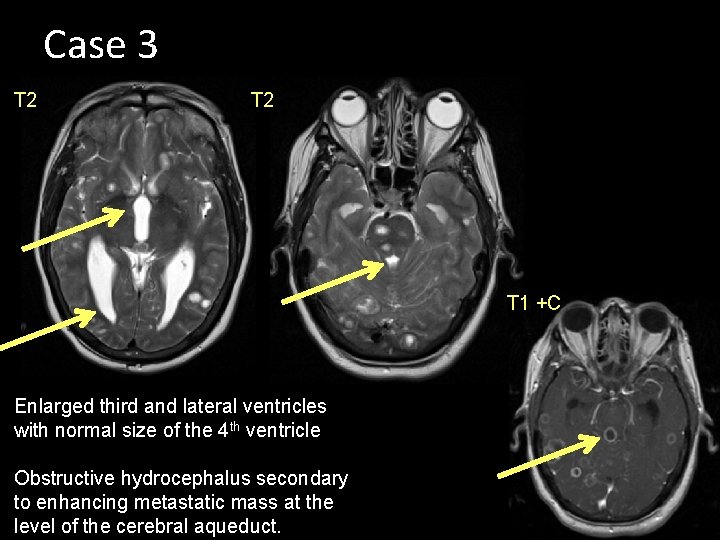
Case 3 T 2 T 1 +C Enlarged third and lateral ventricles with normal size of the 4 th ventricle Obstructive hydrocephalus secondary to enhancing metastatic mass at the level of the cerebral aqueduct.
Metastases with hydrocephalus • Most metastases are parenchymal and frequently centered at the gray-white junction due to highlybranching vasculature • Multiple enhancing masses high suspicion for metastatic disease • Will enhance due to BBB disruption and neovascularity • Mass effect with vasogenic edema in this case, resulting in effacement of the cerebral aqueduct and hydrocephalus
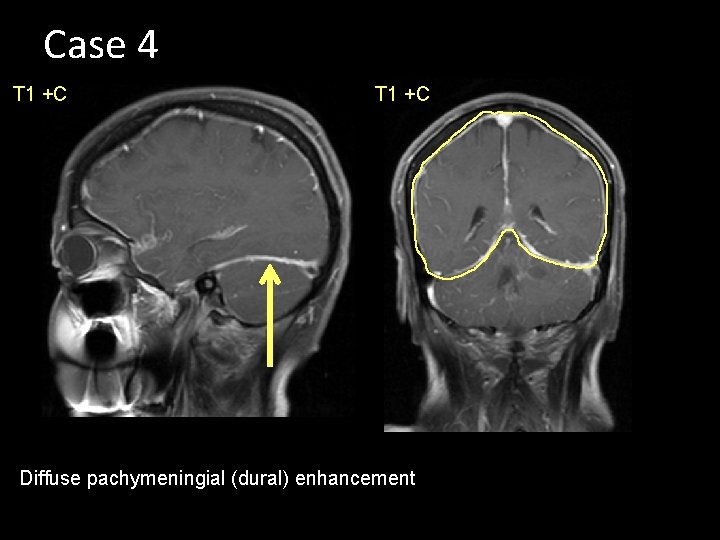
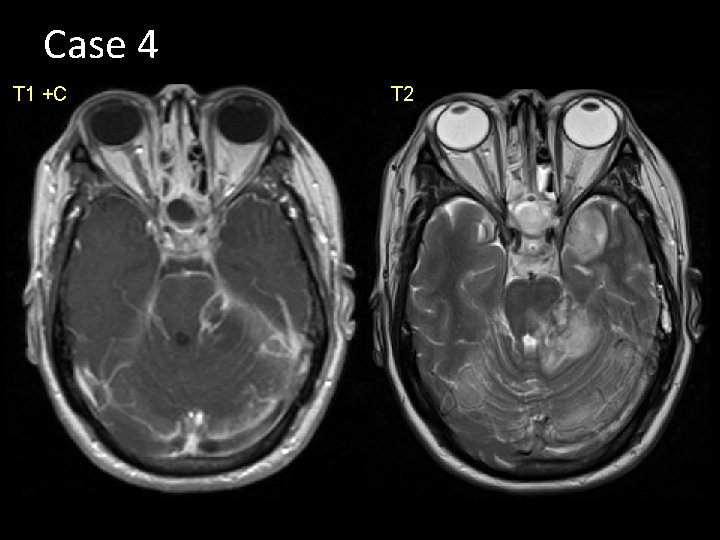
Case 4 44 yo F with altered mental status, left facial droop, and weakness
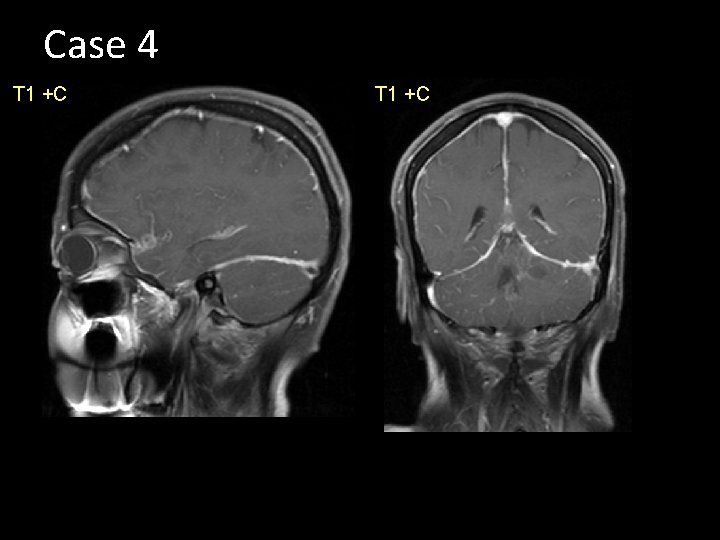
Case 4 T 1 +C
Case 4 T 1 +C Diffuse pachymeningial (dural) enhancement
Case 4 T 1 +C T 2
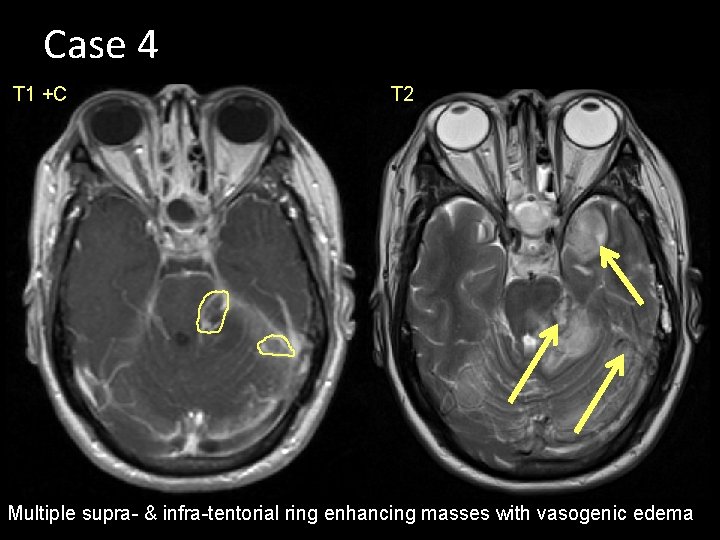
Case 4 T 1 +C T 2 Multiple supra- & infra-tentorial ring enhancing masses with vasogenic edema
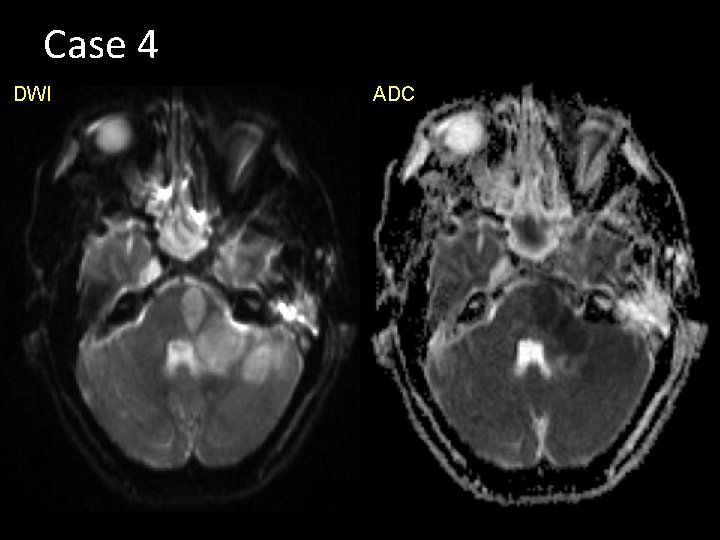
Case 4 DWI ADC
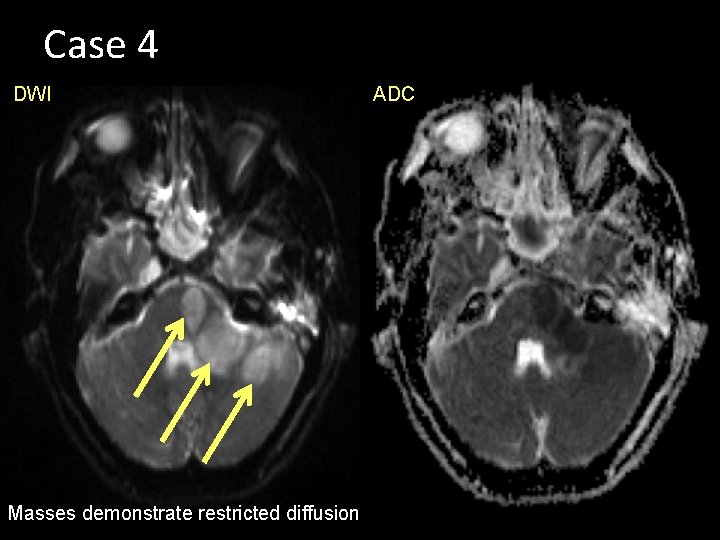
Case 4 DWI Masses demonstrate restricted diffusion ADC
Meningitis with abscess • CT: usually normal, may see hyperdensity in basilar cisterns or sylvian fissures. If +C, may see meningeal enhancement • MR: loss of FLAIR suppression in sulci, meningeal enhancement • Complications: sinus thrombosis, abscess, empyema
Challenge Case Don’t fall victim to satisfaction of search!

Challenge Case FLAIR
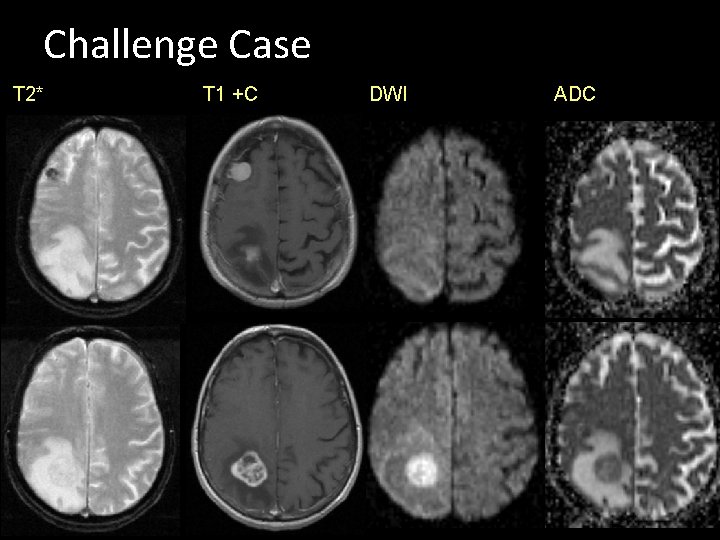
Challenge Case T 2* T 1 +C DWI ADC
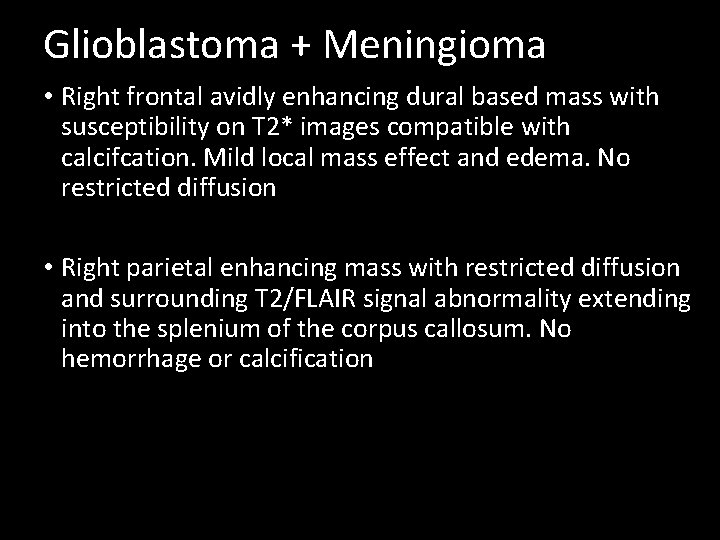
Glioblastoma + Meningioma • Right frontal avidly enhancing dural based mass with susceptibility on T 2* images compatible with calcifcation. Mild local mass effect and edema. No restricted diffusion • Right parietal enhancing mass with restricted diffusion and surrounding T 2/FLAIR signal abnormality extending into the splenium of the corpus callosum. No hemorrhage or calcification
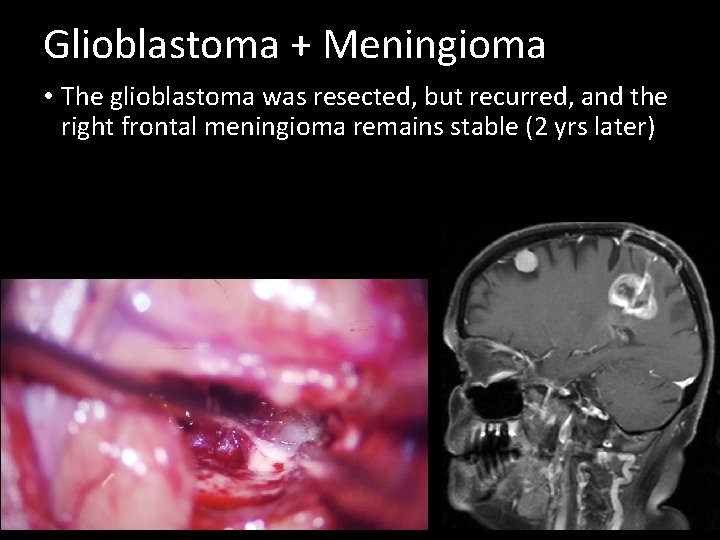
Glioblastoma + Meningioma • The glioblastoma was resected, but recurred, and the right frontal meningioma remains stable (2 yrs later)
Conclusion Imaging findings and localization can help narrow the differential diagnosis of intracranial pathologies, though tissue sampling is frequently necessary
END
- Slides: 56