Radiology course PERIPHERAL VASCULAR STENOSIS AND THROMBOSIS Clinical
Radiology course PERIPHERAL VASCULAR STENOSIS AND THROMBOSIS Clinical cases Istituto di Radiologia Ilaria Fiorina
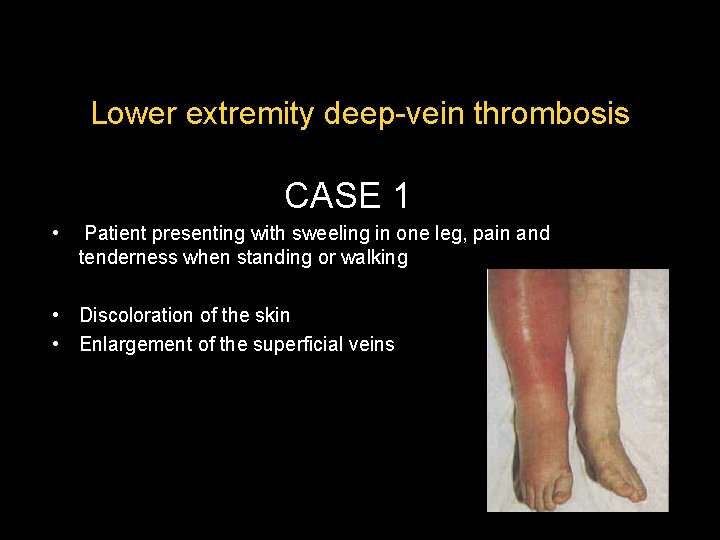
Lower extremity deep-vein thrombosis CASE 1 • Patient presenting with sweeling in one leg, pain and tenderness when standing or walking • Discoloration of the skin • Enlargement of the superficial veins
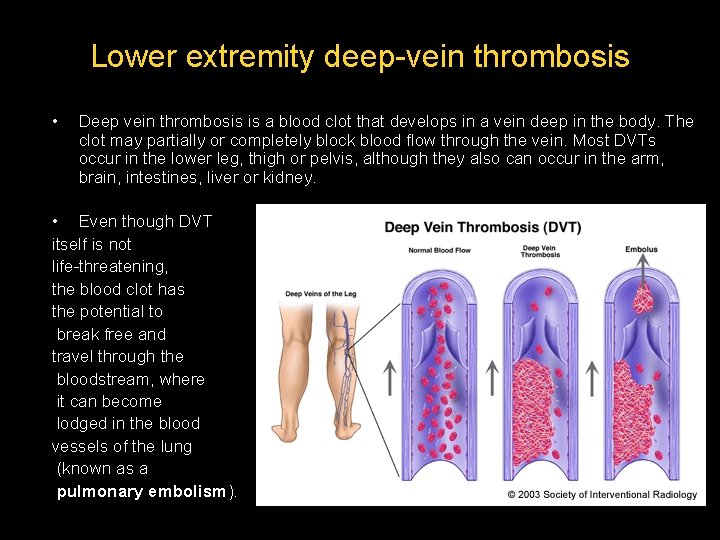
Lower extremity deep-vein thrombosis • Deep vein thrombosis is a blood clot that develops in a vein deep in the body. The clot may partially or completely block blood flow through the vein. Most DVTs occur in the lower leg, thigh or pelvis, although they also can occur in the arm, brain, intestines, liver or kidney. • Even though DVT itself is not life-threatening, the blood clot has the potential to break free and travel through the bloodstream, where it can become lodged in the blood vessels of the lung (known as a pulmonary embolism).
Case 1 • First study? – – US lower extremity with Doppler CT venography lower extremity with contrast MR venography lower extremity without contrast X-ray venography pelvis and lower extremity
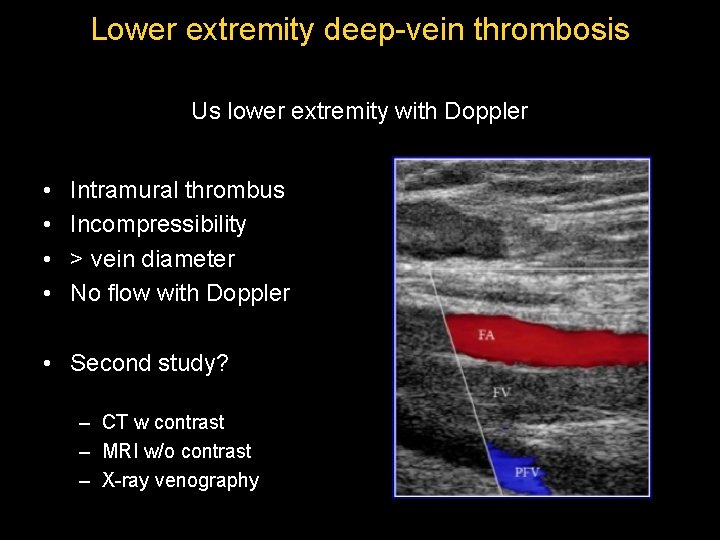
Lower extremity deep-vein thrombosis Us lower extremity with Doppler • • Intramural thrombus Incompressibility > vein diameter No flow with Doppler • Second study? – CT w contrast – MRI w/o contrast – X-ray venography
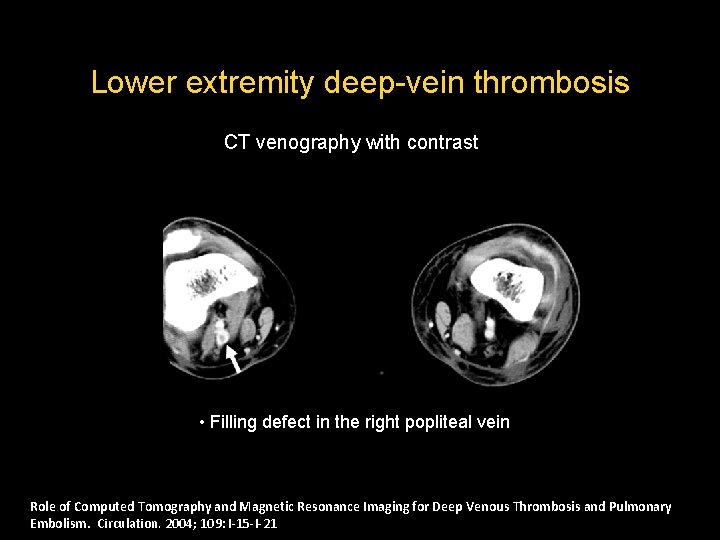
Lower extremity deep-vein thrombosis CT venography with contrast • Filling defect in the right popliteal vein Role of Computed Tomography and Magnetic Resonance Imaging for Deep Venous Thrombosis and Pulmonary Embolism. Circulation. 2004; 109: I-15 -I-21
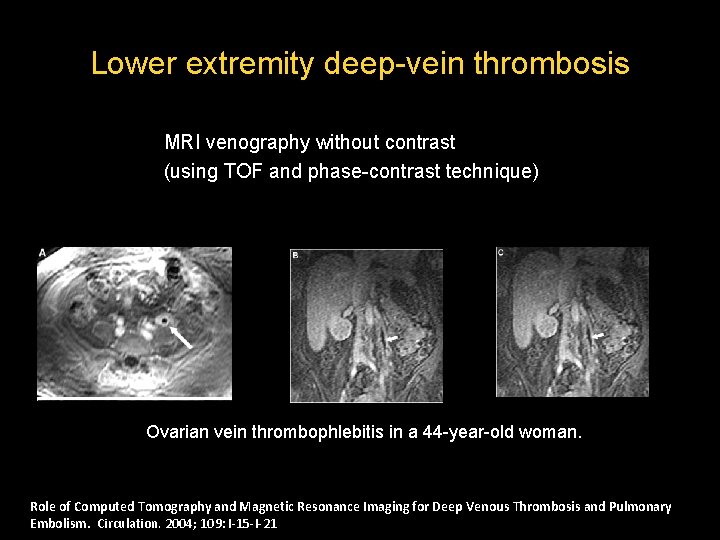
Lower extremity deep-vein thrombosis MRI venography without contrast (using TOF and phase-contrast technique) Ovarian vein thrombophlebitis in a 44 -year-old woman. Role of Computed Tomography and Magnetic Resonance Imaging for Deep Venous Thrombosis and Pulmonary Embolism. Circulation. 2004; 109: I-15 -I-21
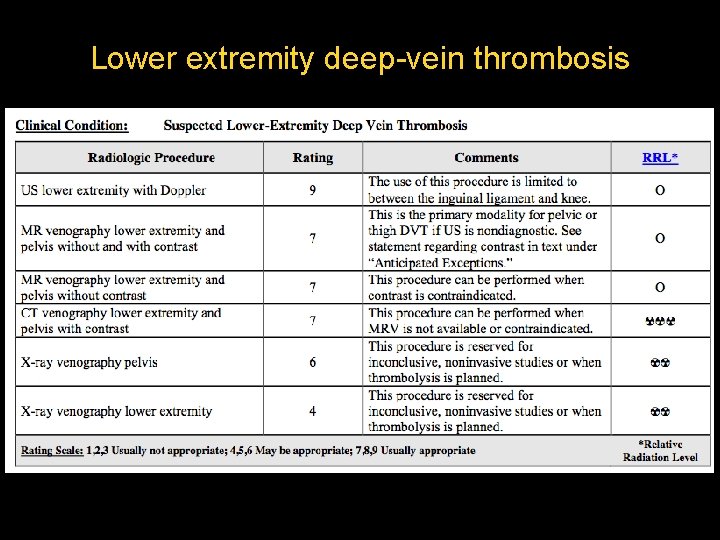
Lower extremity deep-vein thrombosis
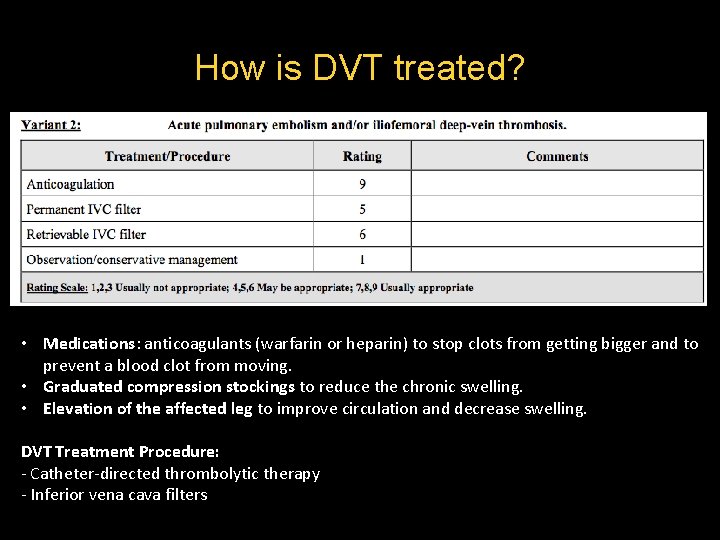
How is DVT treated? • Medications: anticoagulants (warfarin or heparin) to stop clots from getting bigger and to prevent a blood clot from moving. • Graduated compression stockings to reduce the chronic swelling. • Elevation of the affected leg to improve circulation and decrease swelling. DVT Treatment Procedure: - Catheter-directed thrombolytic therapy - Inferior vena cava filters
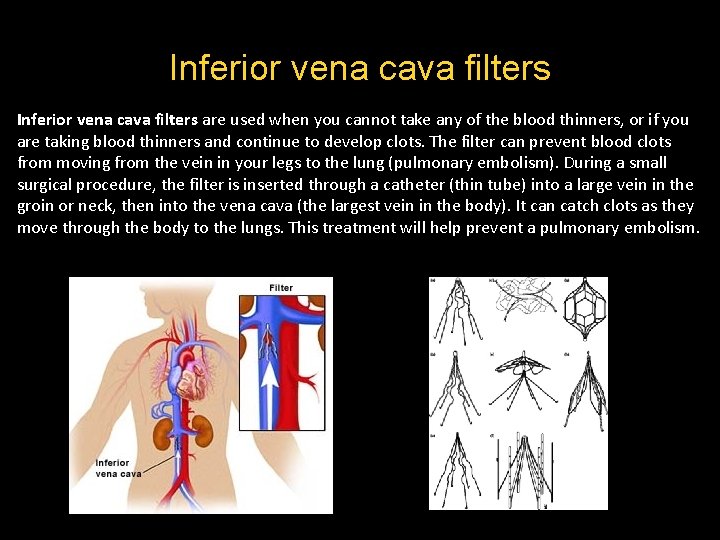
Inferior vena cava filters are used when you cannot take any of the blood thinners, or if you are taking blood thinners and continue to develop clots. The filter can prevent blood clots from moving from the vein in your legs to the lung (pulmonary embolism). During a small surgical procedure, the filter is inserted through a catheter (thin tube) into a large vein in the groin or neck, then into the vena cava (the largest vein in the body). It can catch clots as they move through the body to the lungs. This treatment will help prevent a pulmonary embolism.
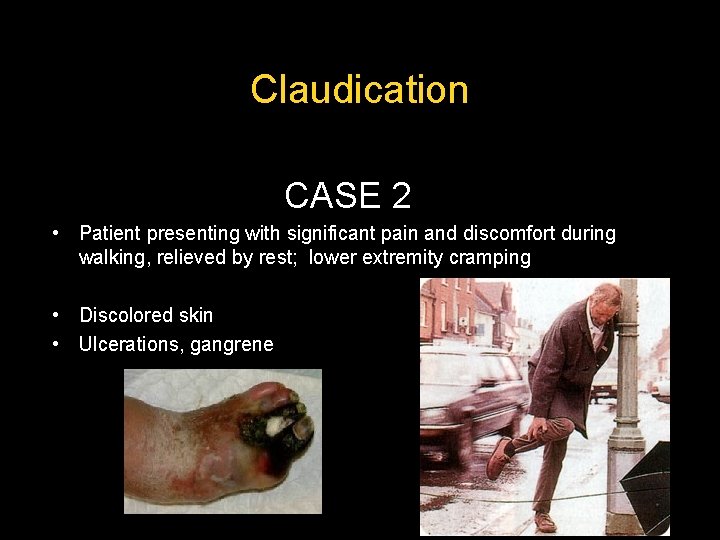
Claudication CASE 2 • Patient presenting with significant pain and discomfort during walking, relieved by rest; lower extremity cramping • Discolored skin • Ulcerations, gangrene
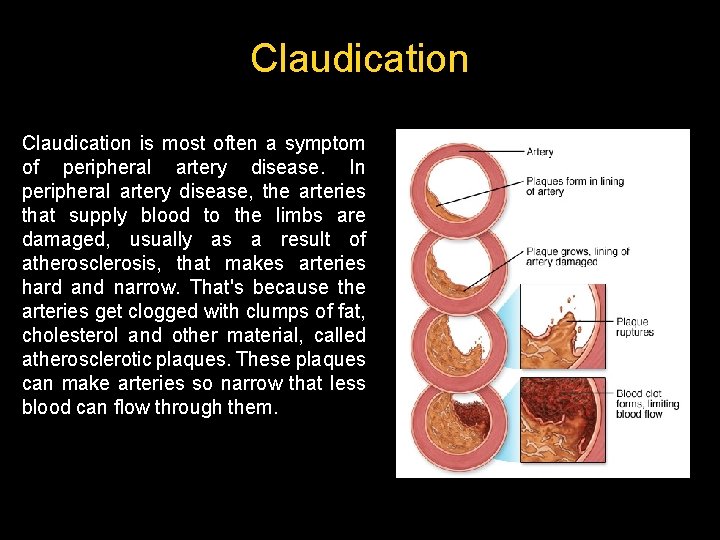
Claudication is most often a symptom of peripheral artery disease. In peripheral artery disease, the arteries that supply blood to the limbs are damaged, usually as a result of atherosclerosis, that makes arteries hard and narrow. That's because the arteries get clogged with clumps of fat, cholesterol and other material, called atherosclerotic plaques. These plaques can make arteries so narrow that less blood can flow through them.
Claudication • First study? – – US lower extremity with Doppler CT angiography lower extremity with contrast MR angiography lower extremity w/o contrast X-ray angiography pelvis and lower extremity
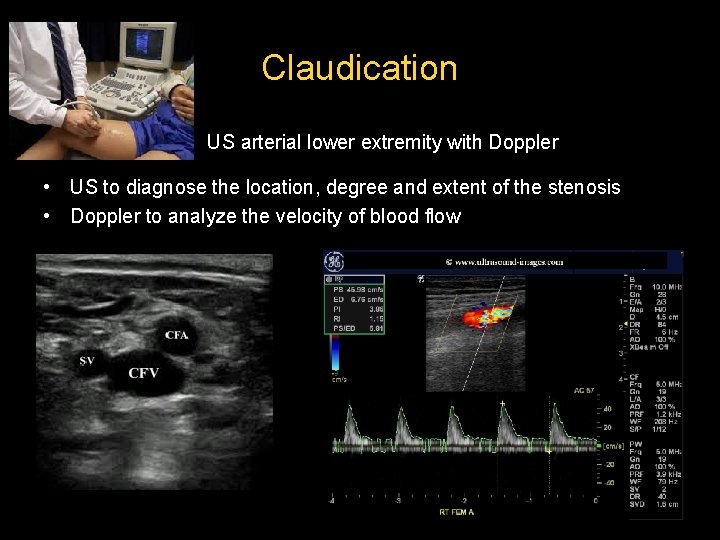
Claudication US arterial lower extremity with Doppler • US to diagnose the location, degree and extent of the stenosis • Doppler to analyze the velocity of blood flow
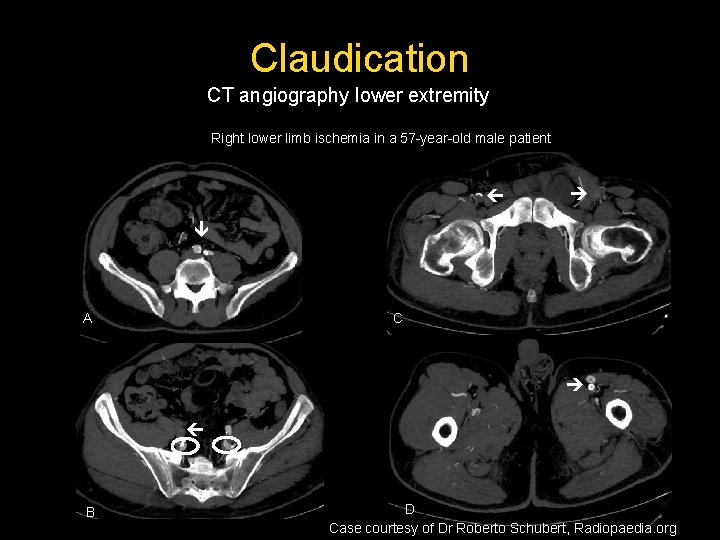
Claudication CT angiography lower extremity Right lower limb ischemia in a 57 -year-old male patient A C B D Case courtesy of Dr Roberto Schubert, Radiopaedia. org
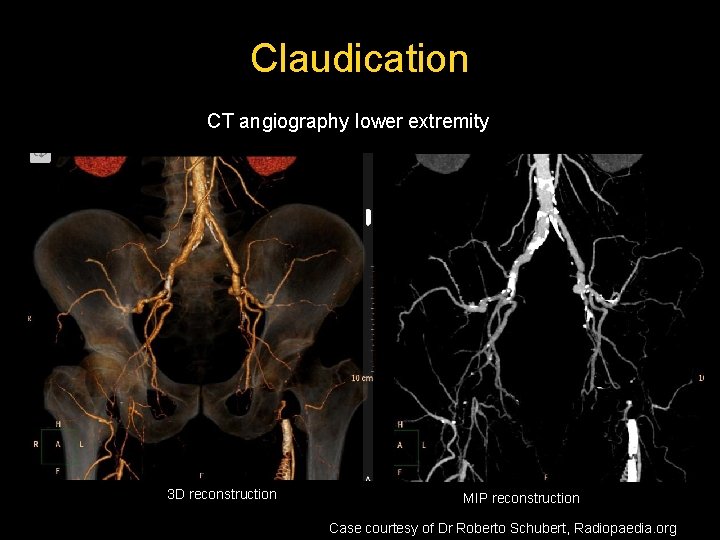
Claudication CT angiography lower extremity 3 D reconstruction MIP reconstruction Case courtesy of Dr Roberto Schubert, Radiopaedia. org
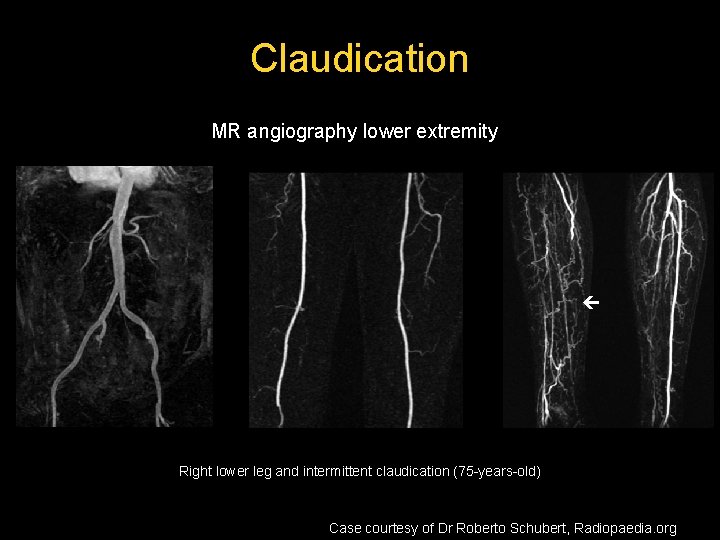
Claudication MR angiography lower extremity Right lower leg and intermittent claudication (75 -years-old) Case courtesy of Dr Roberto Schubert, Radiopaedia. org
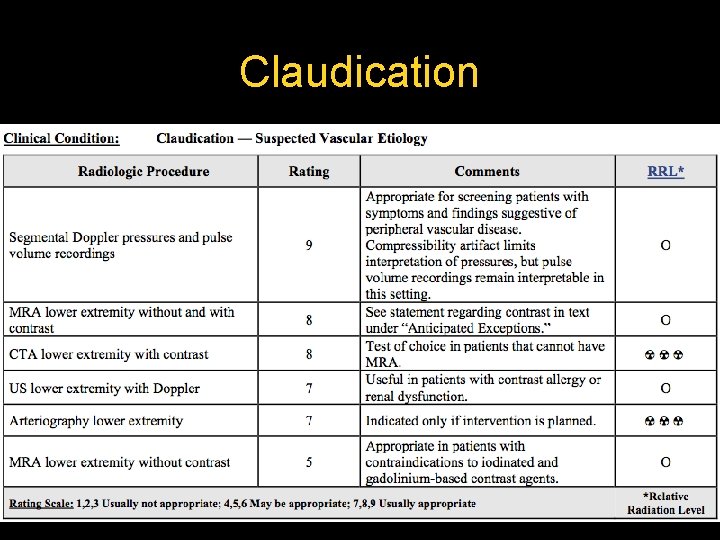
Claudication
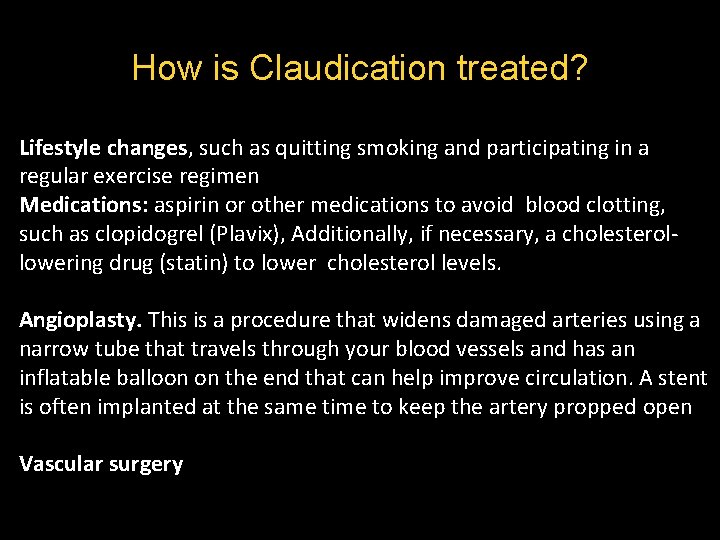
How is Claudication treated? Lifestyle changes, such as quitting smoking and participating in a regular exercise regimen Medications: aspirin or other medications to avoid blood clotting, such as clopidogrel (Plavix), Additionally, if necessary, a cholesterollowering drug (statin) to lower cholesterol levels. Angioplasty. This is a procedure that widens damaged arteries using a narrow tube that travels through your blood vessels and has an inflatable balloon on the end that can help improve circulation. A stent is often implanted at the same time to keep the artery propped open Vascular surgery
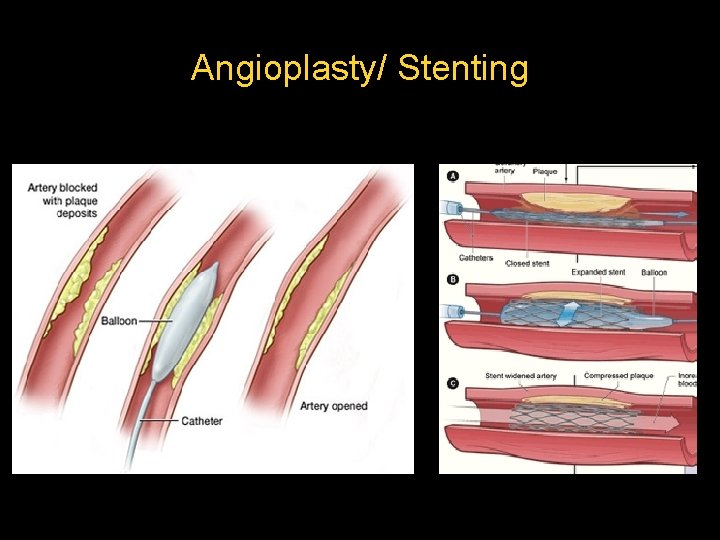
Angioplasty/ Stenting
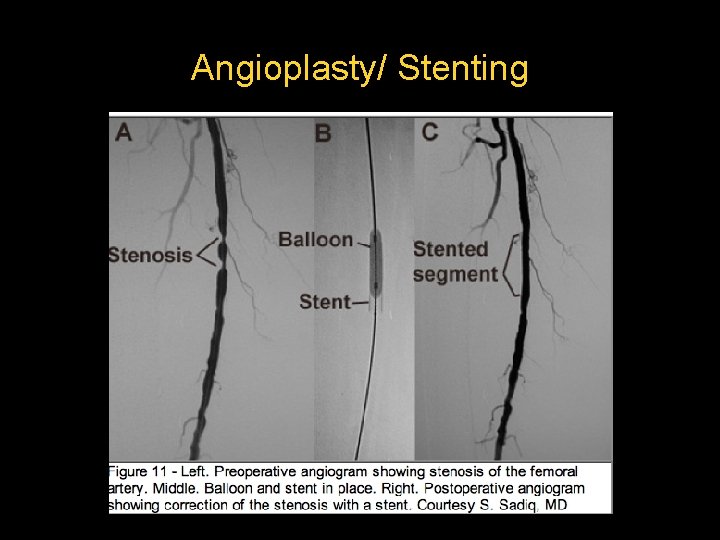
Angioplasty/ Stenting
Renovascular hypertension CASE 3 • Patient (generally young woman) presenting with hypertension refractory to antihypertensive medication. • Diminished kidney function
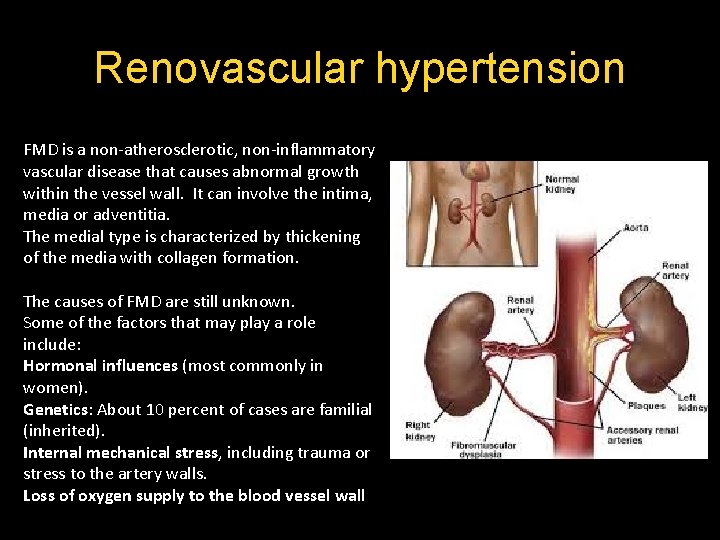
Renovascular hypertension FMD is a non-atherosclerotic, non-inflammatory vascular disease that causes abnormal growth within the vessel wall. It can involve the intima, media or adventitia. The medial type is characterized by thickening of the media with collagen formation. The causes of FMD are still unknown. Some of the factors that may play a role include: Hormonal influences (most commonly in women). Genetics: About 10 percent of cases are familial (inherited). Internal mechanical stress, including trauma or stress to the artery walls. Loss of oxygen supply to the blood vessel wall
Renovascular hypertension • First study? – – Renal duplex US with Doppler CT angiography with contrast MR angiography w/o contrast Renal angiography
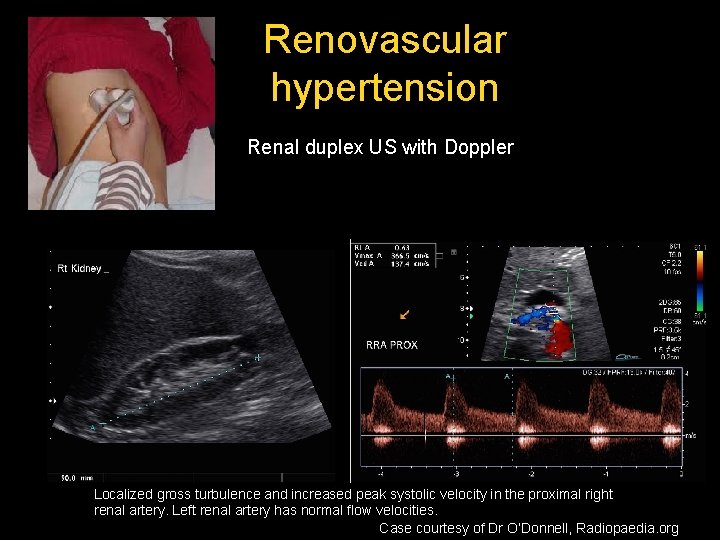
Renovascular hypertension Renal duplex US with Doppler Localized gross turbulence and increased peak systolic velocity in the proximal right renal artery. Left renal artery has normal flow velocities. Case courtesy of Dr O’Donnell, Radiopaedia. org
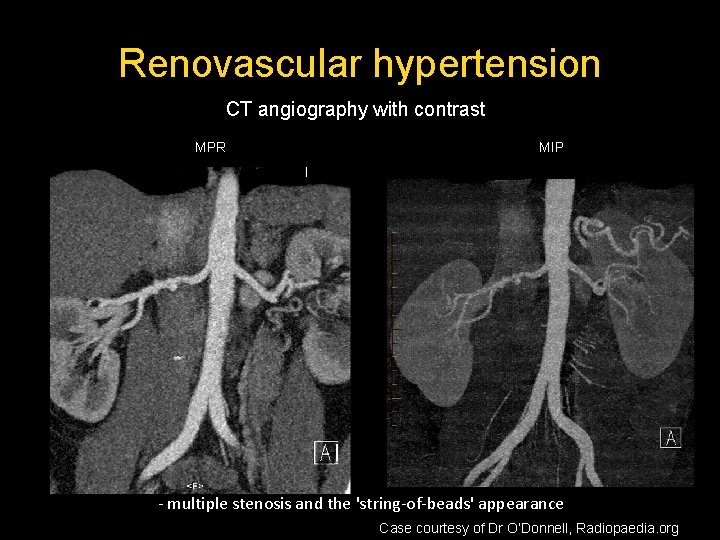
Renovascular hypertension CT angiography with contrast MPR MIP - multiple stenosis and the 'string-of-beads' appearance Case courtesy of Dr O’Donnell, Radiopaedia. org
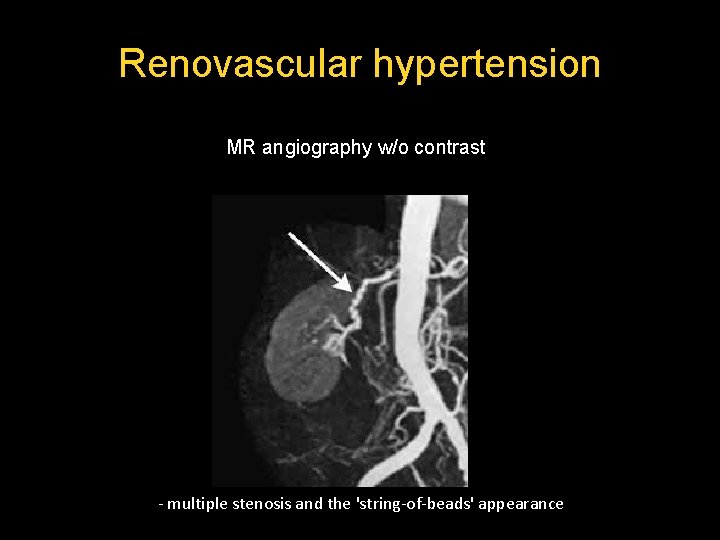
Renovascular hypertension MR angiography w/o contrast - multiple stenosis and the 'string-of-beads' appearance
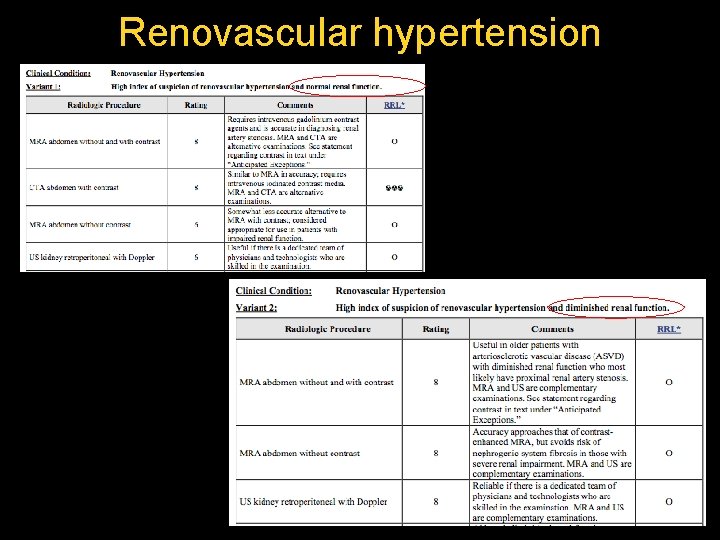
Renovascular hypertension
How is renovascular hypertension treated? - Lifestyle changes: control high blood pressure, cholesterol, diabetes, and heart disease. Imaging study (duplex ultrasound, MRA or CTA) performed at regular intervals, generally every year, to monitor disease progression. - Medications: antiplatelet (aspirin) - Treatment procedures: Percutaneous angioplasty of the renal arteries is recommended. Similar to the procedure used to treat blockages in the heart arteries, renal angioplasty involves placement of a balloon-mounted catheter inside the artery at the site of the narrowing or blockage. The catheter is guided through the blood vessel with the aid of a special x-ray machine. The balloon is inflated to re-open the blood vessel, and then the balloon and the catheter are withdrawn.
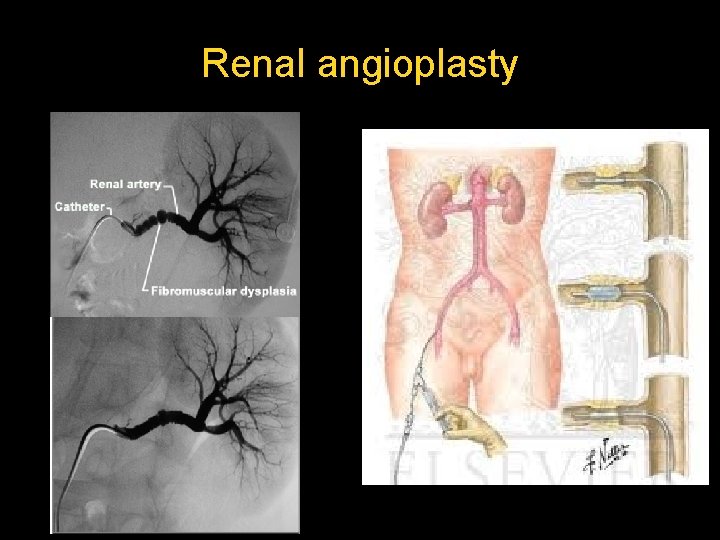
Renal angioplasty
CAD/CAS CASE 4 • Patient presenting with TIA (Transient Ischemic Attack) • Smoking, hypertension • Diabetes, obesity
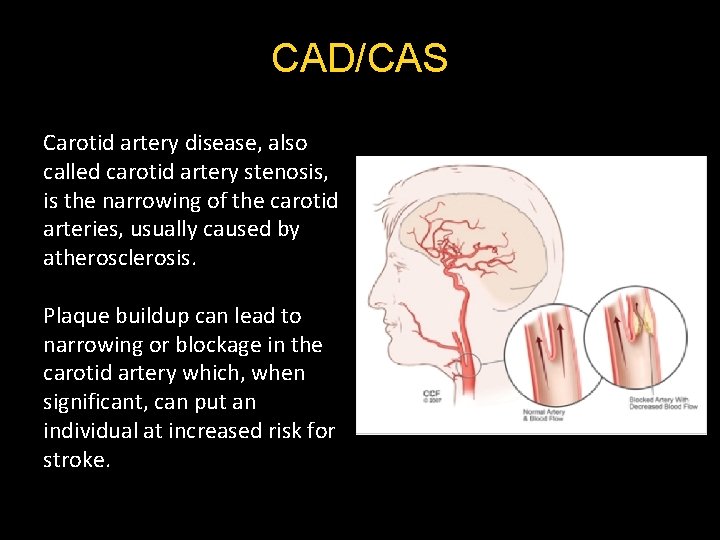
CAD/CAS Carotid artery disease, also called carotid artery stenosis, is the narrowing of the carotid arteries, usually caused by atherosclerosis. Plaque buildup can lead to narrowing or blockage in the carotid artery which, when significant, can put an individual at increased risk for stroke.
CAD/CAS • First study? – – – Carotid duplex US with Doppler Cerebral CT without contrast Cerebral CT angiography with contrast Cerebral MR angiography w/o contrast Carotid angiography
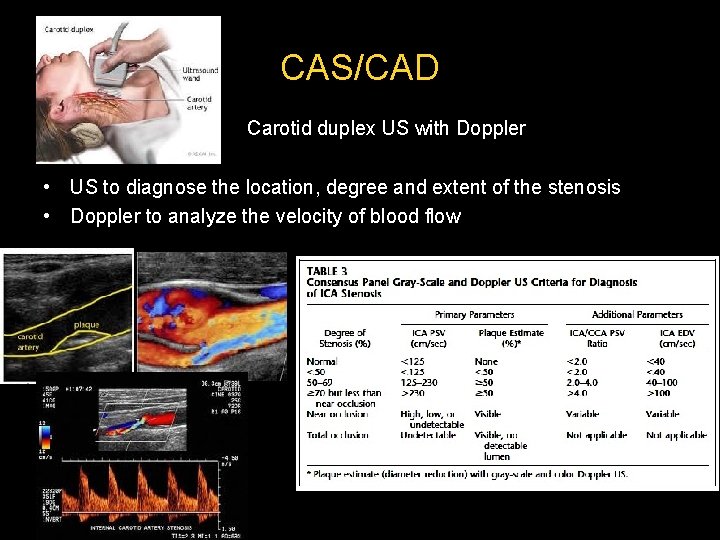
CAS/CAD Carotid duplex US with Doppler • US to diagnose the location, degree and extent of the stenosis • Doppler to analyze the velocity of blood flow
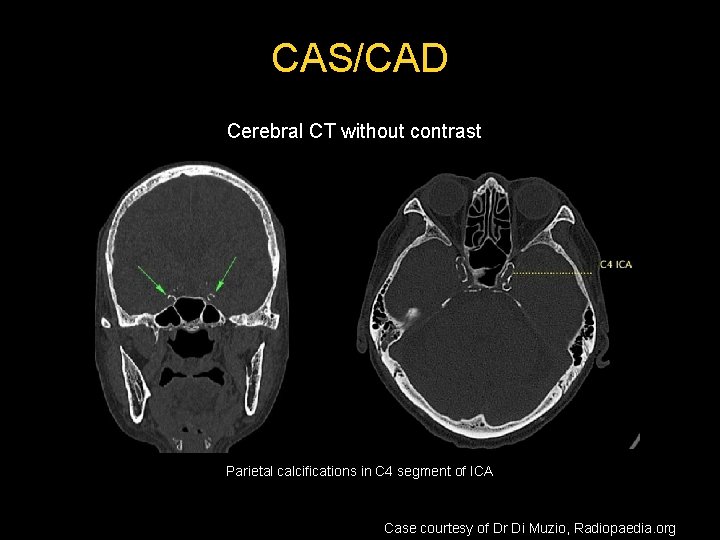
CAS/CAD Cerebral CT without contrast Parietal calcifications in C 4 segment of ICA Case courtesy of Dr Di Muzio, Radiopaedia. org
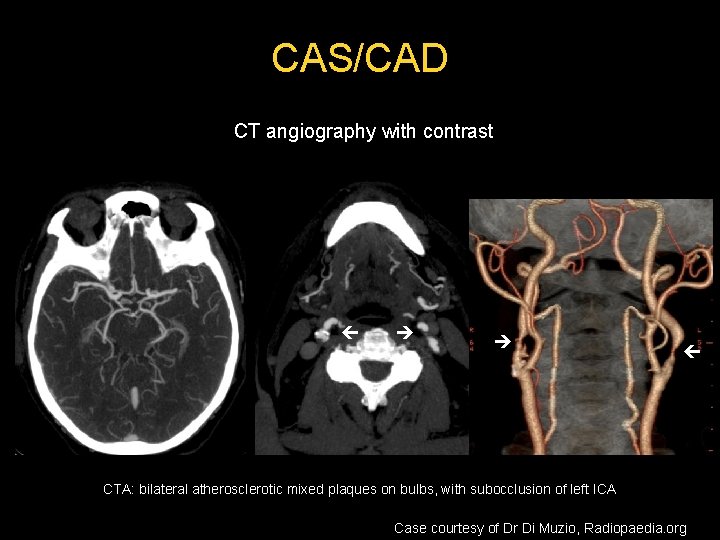
CAS/CAD CT angiography with contrast CTA: bilateral atherosclerotic mixed plaques on bulbs, with subocclusion of left ICA Case courtesy of Dr Di Muzio, Radiopaedia. org
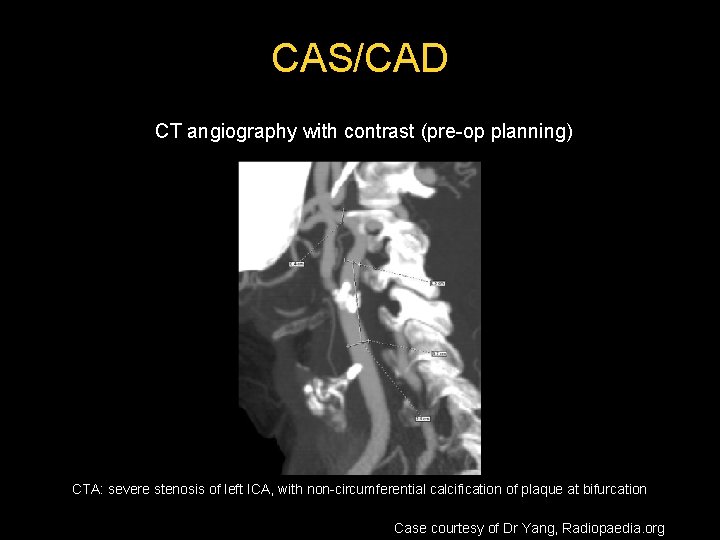
CAS/CAD CT angiography with contrast (pre-op planning) CTA: severe stenosis of left ICA, with non-circumferential calcification of plaque at bifurcation Case courtesy of Dr Yang, Radiopaedia. org
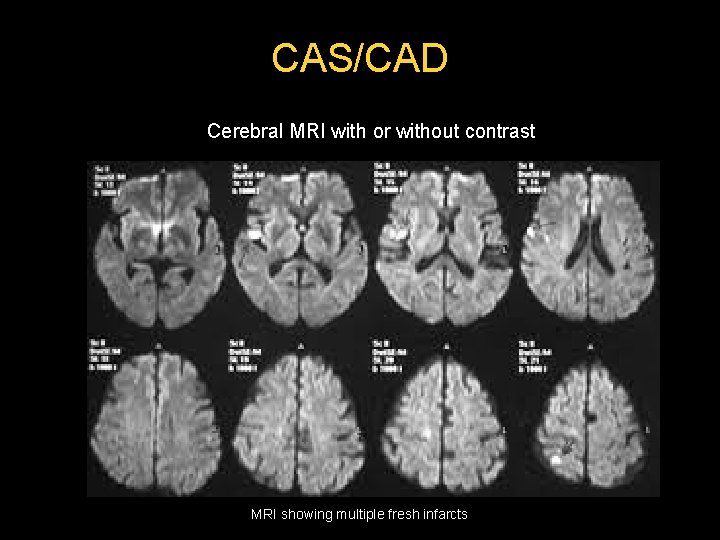
CAS/CAD Cerebral MRI with or without contrast MRI showing multiple fresh infarcts
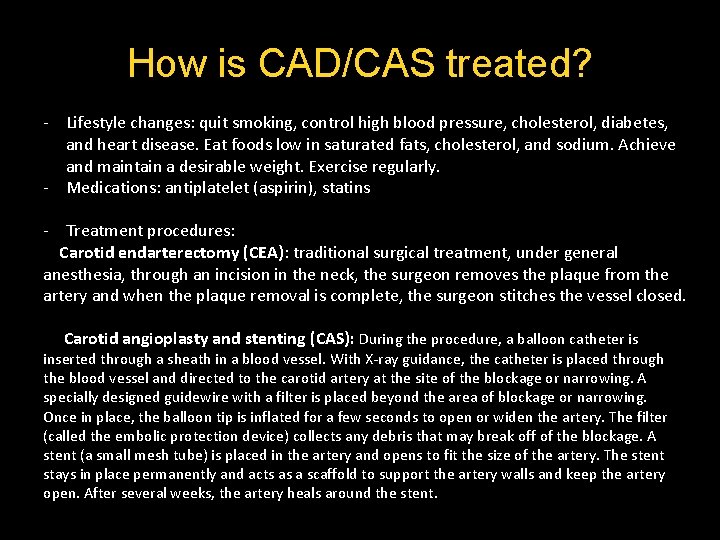
How is CAD/CAS treated? - Lifestyle changes: quit smoking, control high blood pressure, cholesterol, diabetes, and heart disease. Eat foods low in saturated fats, cholesterol, and sodium. Achieve and maintain a desirable weight. Exercise regularly. - Medications: antiplatelet (aspirin), statins - Treatment procedures: Carotid endarterectomy (CEA): traditional surgical treatment, under general anesthesia, through an incision in the neck, the surgeon removes the plaque from the artery and when the plaque removal is complete, the surgeon stitches the vessel closed. Carotid angioplasty and stenting (CAS): During the procedure, a balloon catheter is inserted through a sheath in a blood vessel. With X-ray guidance, the catheter is placed through the blood vessel and directed to the carotid artery at the site of the blockage or narrowing. A specially designed guidewire with a filter is placed beyond the area of blockage or narrowing. Once in place, the balloon tip is inflated for a few seconds to open or widen the artery. The filter (called the embolic protection device) collects any debris that may break off of the blockage. A stent (a small mesh tube) is placed in the artery and opens to fit the size of the artery. The stent stays in place permanently and acts as a scaffold to support the artery walls and keep the artery open. After several weeks, the artery heals around the stent.
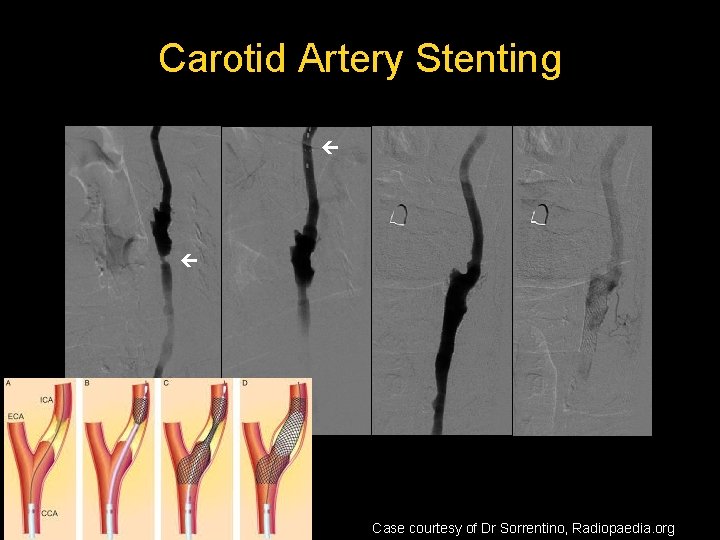
Carotid Artery Stenting Case courtesy of Dr Sorrentino, Radiopaedia. org
CMI CASE 5 • Patient presenting with abdominal pain after meals, weight loss, fear of eating, nausea and/or vomiting • • Smoking Hypertension Diabetes History of cardiovascular disease
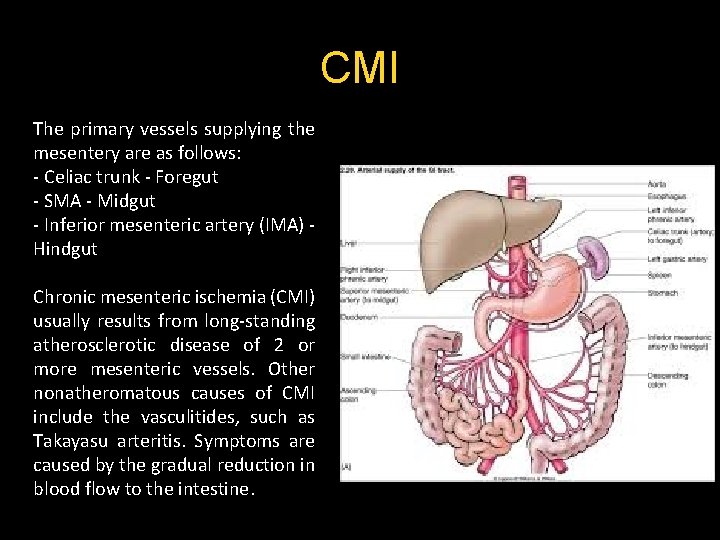
CMI The primary vessels supplying the mesentery are as follows: - Celiac trunk - Foregut - SMA - Midgut - Inferior mesenteric artery (IMA) - Hindgut Chronic mesenteric ischemia (CMI) usually results from long-standing atherosclerotic disease of 2 or more mesenteric vessels. Other nonatheromatous causes of CMI include the vasculitides, such as Takayasu arteritis. Symptoms are caused by the gradual reduction in blood flow to the intestine.
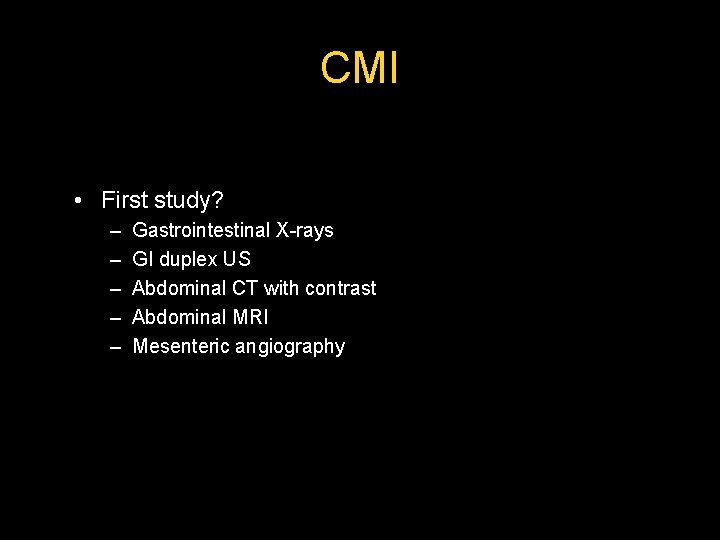
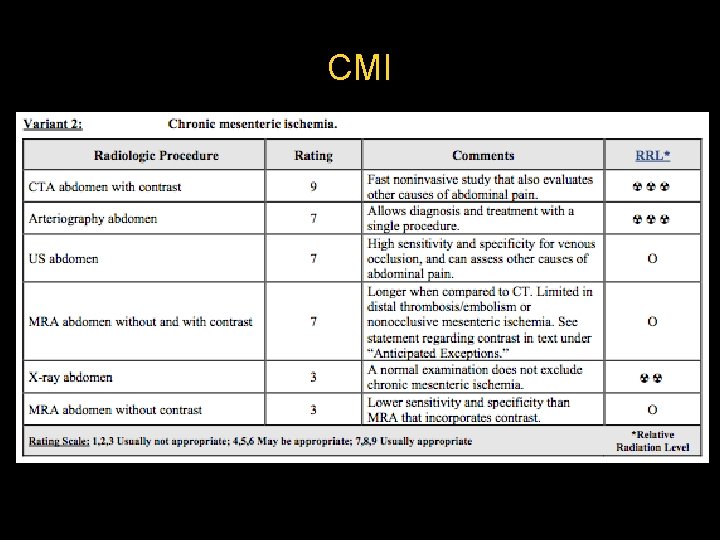
CMI • First study? – – – Gastrointestinal X-rays GI duplex US Abdominal CT with contrast Abdominal MRI Mesenteric angiography
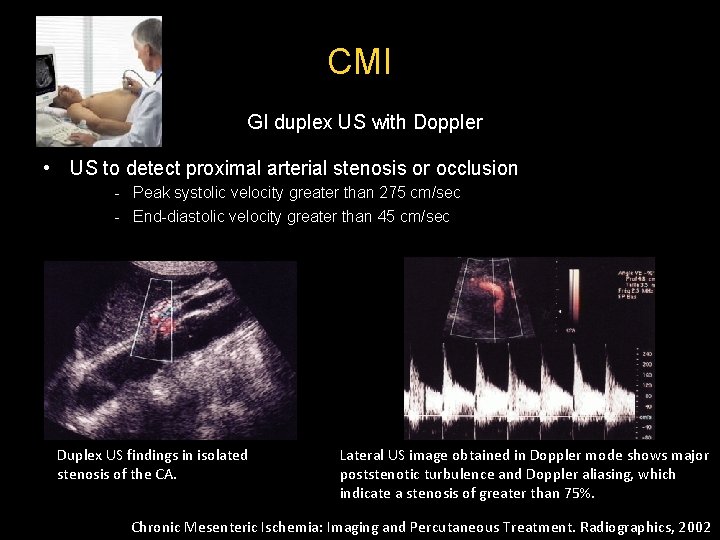
CMI GI duplex US with Doppler • US to detect proximal arterial stenosis or occlusion - Peak systolic velocity greater than 275 cm/sec - End-diastolic velocity greater than 45 cm/sec Duplex US findings in isolated stenosis of the CA. Lateral US image obtained in Doppler mode shows major poststenotic turbulence and Doppler aliasing, which indicate a stenosis of greater than 75%. Chronic Mesenteric Ischemia: Imaging and Percutaneous Treatment. Radiographics, 2002
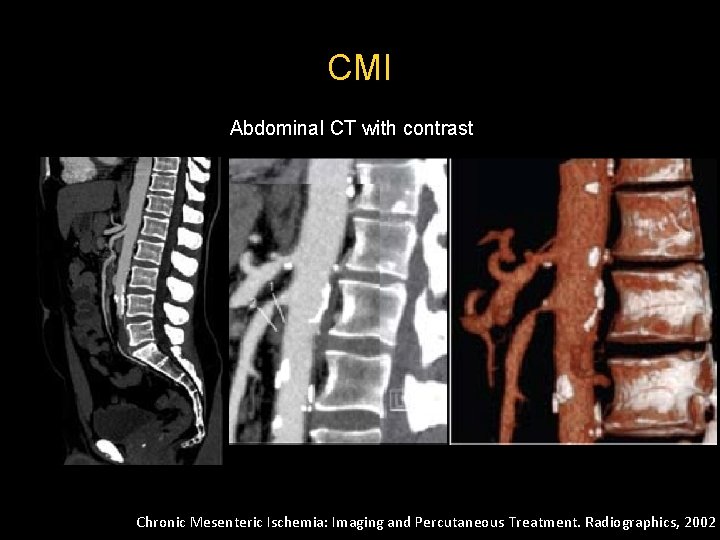
CMI Abdominal CT with contrast Chronic Mesenteric Ischemia: Imaging and Percutaneous Treatment. Radiographics, 2002
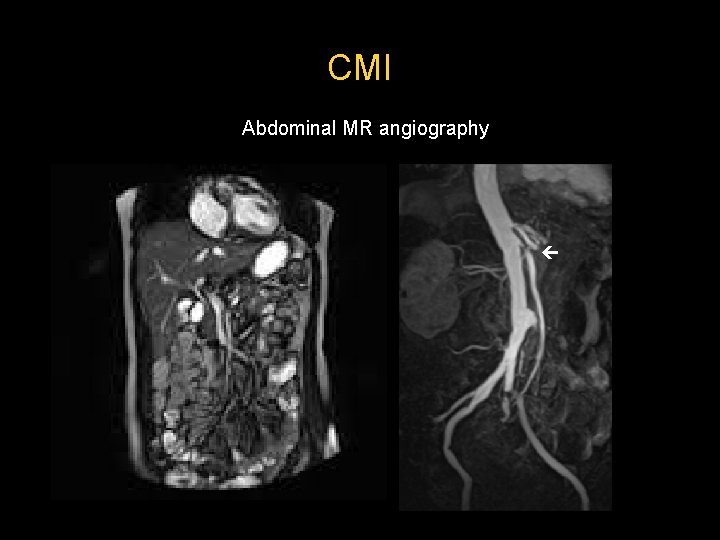
CMI Abdominal MR angiography
CMI
How is CMI treated? Anticoagulant medications, such as Coumadin (warfarin - a bloodthinner), to reduce the risk of blood clots. Angioplasty and stenting: A balloon catheter is used to attempt to open the artery and a small stent is placed inside the artery to keep it open. Surgery may be performed to remove plaque (endarterectomy), bypass the blocked vessel to restore blood flow to the intestines, or remove or repair an aneurysm. The surgeon may use autologous bypass grafts (patient’s own blood vessels) or artificial grafts during the bypass procedure.
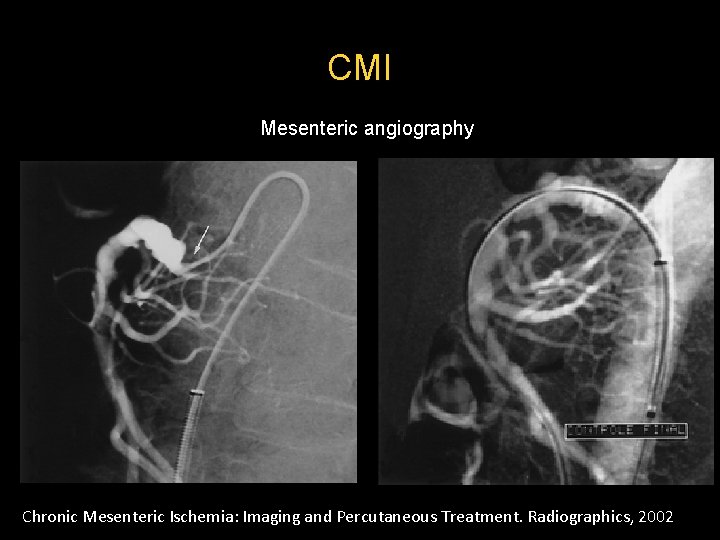
CMI Mesenteric angiography Chronic Mesenteric Ischemia: Imaging and Percutaneous Treatment. Radiographics, 2002
Thank you
- Slides: 51