Radiological Incidents 1 Objectives To identify 4 radiation
Radiological Incidents 1
Objectives • To identify 4 radiation protection principles • To describe differences between radiological exposure and contamination • To identify key hospital contacts in the event of radiologically contaminated patients 2

Nuclear and Radiological Risks • Radiological Dispersal Device – Aka: Dirty Bomb • Greatest risk • Simple radiological sources – Transportation of radioactive material, – Likely-Not expected to be mass casualty event • Nuclear irradiation – Bomb (terrorism) – Leak (reactor) 3
Radiation Basics • Ionizing radiation is electromagnetic energy, or energy containing particles emitted from a source. • In living systems, this causes damage to cells and interrupt normal biological processes. 4
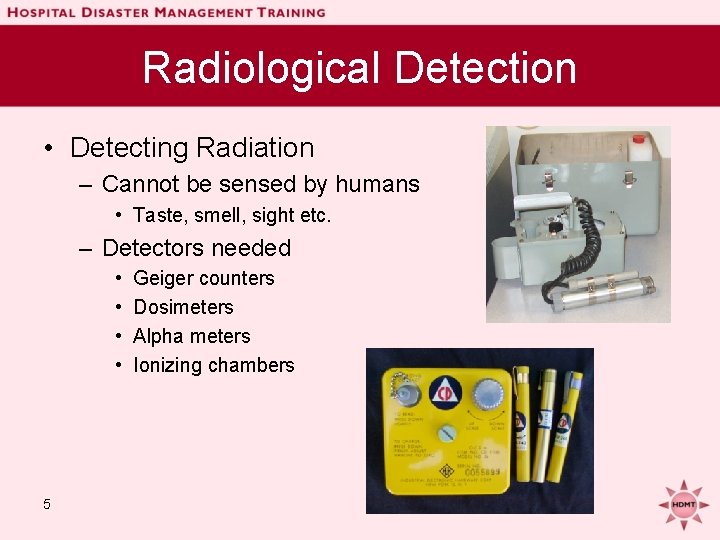
Radiological Detection • Detecting Radiation – Cannot be sensed by humans • Taste, smell, sight etc. – Detectors needed • • 5 Geiger counters Dosimeters Alpha meters Ionizing chambers
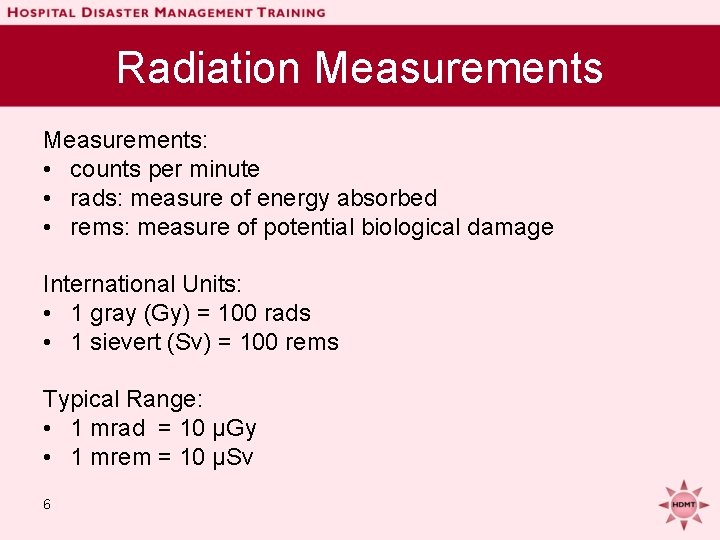
Radiation Measurements: • counts per minute • rads: measure of energy absorbed • rems: measure of potential biological damage International Units: • 1 gray (Gy) = 100 rads • 1 sievert (Sv) = 100 rems Typical Range: • 1 mrad = 10 μGy • 1 mrem = 10 μSv 6
Radiation Experts Hospitals are well prepared for a radiological event • Experts abound – Radiologists, Nuclear Med, Radiation Safety Officers, etc. • Detection methods already in place & they know how to use them! • • LA Co MAC 24/7 (866) 940 -4401 Contact LA Co Radiation Mgmt Office (213) 351 -7897 State (800) 852 -7550 • 7
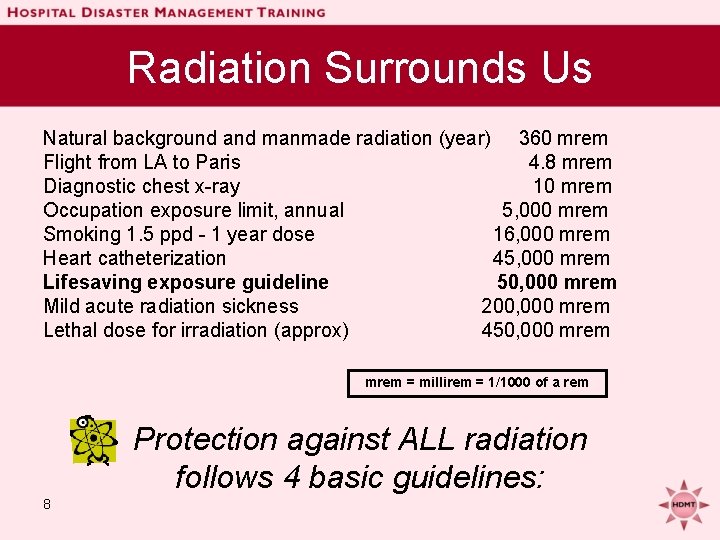
Radiation Surrounds Us Natural background and manmade radiation (year) 360 mrem Flight from LA to Paris 4. 8 mrem Diagnostic chest x-ray 10 mrem Occupation exposure limit, annual 5, 000 mrem Smoking 1. 5 ppd - 1 year dose 16, 000 mrem Heart catheterization 45, 000 mrem Lifesaving exposure guideline 50, 000 mrem Mild acute radiation sickness 200, 000 mrem Lethal dose for irradiation (approx) 450, 000 mrem = millirem = 1/1000 of a rem Protection against ALL radiation follows 4 basic guidelines: 8
Radiation Protection Principles • Time • Shielding • Distance • Quantity 9
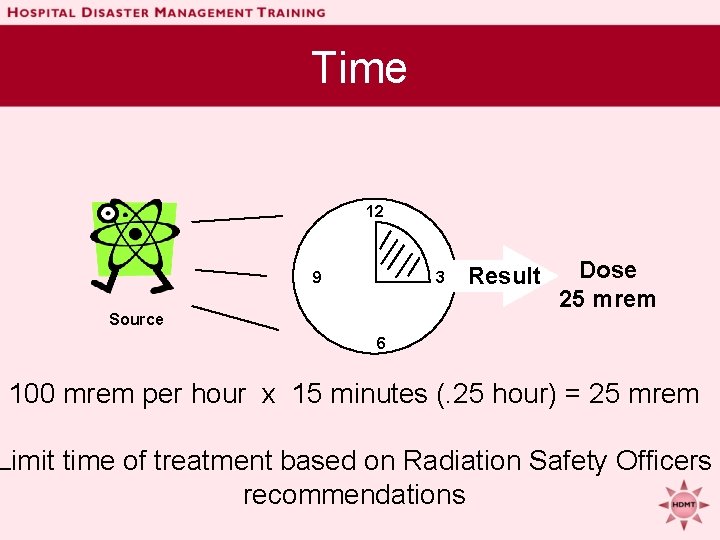
Time 12 9 3 Source Result Dose 25 mrem 6 100 mrem per hour x 15 minutes (. 25 hour) = 25 mrem Limit time of treatment based on Radiation Safety Officers recommendations
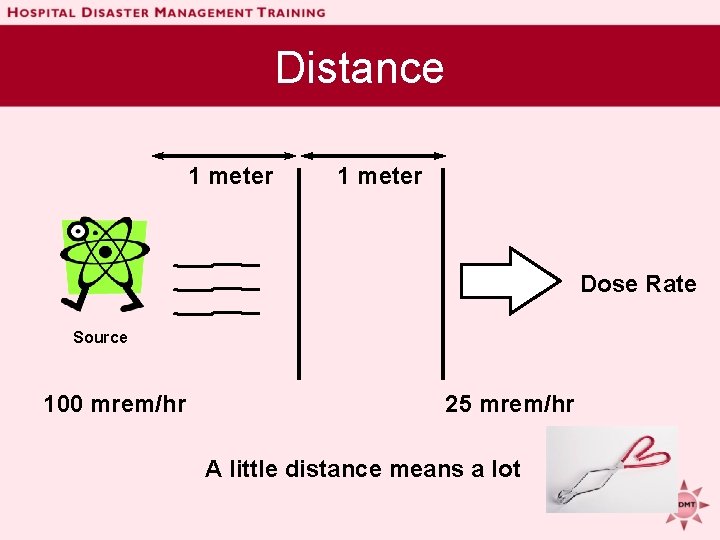
Distance 1 meter Dose Rate Source 100 mrem/hr 25 mrem/hr A little distance means a lot
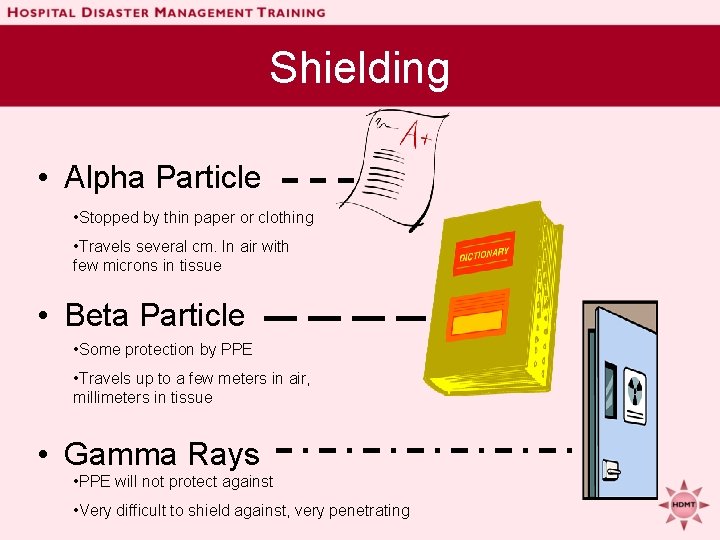
Shielding • Alpha Particle • Stopped by thin paper or clothing • Travels several cm. In air with few microns in tissue • Beta Particle • Some protection by PPE • Travels up to a few meters in air, millimeters in tissue • Gamma Rays • PPE will not protect against • Very difficult to shield against, very penetrating
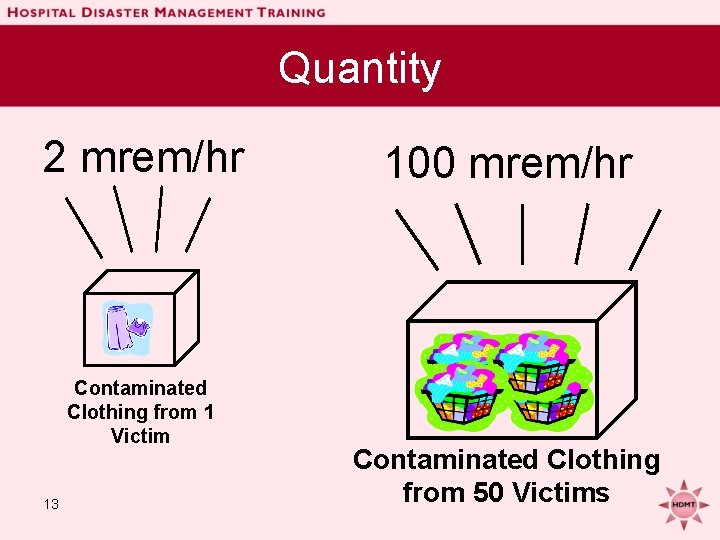
Quantity 2 mrem/hr Contaminated Clothing from 1 Victim 13 100 mrem/hr Contaminated Clothing from 50 Victims
Radiation Protection Principles • Practical applications of the 4 principles – If standard working PPE is inadequate as shielding, use the following to make a bad situation safer – Limit time in area • Decrease time dealing with the disaster – Increase working distances • Use long handled tools and grabbers – Don’t allow contaminated clothing bags to accumulate in quantity • Spread out contained materials over a large area 14
Exposure Vs. Contamination • Exposure to radiation does NOT necessarily make victims contaminated or radioactive! 15
Contamination • External Contamination – Material deposited on skin, clothes, hair • Dirty bomb – material exploded into air – Decontamination necessary – Victims are NOT radioactive, but the ‘dust’ is • Internal Contamination – Material becomes integral part of the body • Ingestion-DO NOT lick lips • Absorption from mucous membrane – DO NOT touch eyes, mouth nose 16 – Nuclear imaging or therapy
Management of Radiation Victims • Immediately – Secure hospital entrances and perimeter – Establish triage area outside of hospital if possible – Control ventilation – Issue protective clothing & dosimeters to staff – Establish area for contaminated waste/clothes 17
Management of Radiation Victims • At patient arrival – Treat life-threatening conditions first! – Consider irradiation/contamination second – Survey patient for radiation ASAP – Use usual triage methods based on complaints – Remove and bag victim’s clothing 18
Management of Radiation Victims • Decontamination – If there is an open wound decontaminate first, then rest of skin – Cover wound with sterile dressing – Soap/water decon (including hair) – Re-survey patient for radiation • If radiation present, send back through decon – Refer for needed surgery 19
Management of Internal Contamination • Various medications available for limiting uptake or facilitate removal of radioactive material – – KI Radiogardase (Prussian blue) DTPA Bicarbonate • Now part of response stockpiles 20
Why Radiation Makes You Sick • Some cells in your body have a short life cycle (they reproduce and die rapidly). • Radiation most affects the rapidly reproducing cells which are in the gut, bone marrow and skin/hair. • Once these cells are damaged by radiation, they are unable to reproduce. 21
Acute Radiation Syndrome (ARS) • Follows a predictable course over a few hours to several weeks • Group of symptoms that develop after total body irradiation (> 100 rems) • Patients are classified in three categories based on signs and symptoms: – Survival probable: < 100 rems – Survival possible: 200 - 800 rems – Survival improbable: > 800 rems 22
ARS - Phases Prodromal Phase - occurs in the first 48 to 72 hours postexposure and is characterized by nausea, vomiting, and anorexia. At doses below about 500 rems this lasts 2 to 4 days. Latent Phase - follows the prodromal phase and lasts for approximately 2 to 2 1/2 weeks. During this time, predisposed to infection due to decrease of infection fighting cells. Illness Phase - period when overt illness develop such as infection, electrolyte imbalances, diarrhea and shock. Recovery or Death Phase - may take weeks or months 23

Phases of Rad Syndrome & Trauma • Radiation + Trauma = áMortality • Surgical procedures that are not done in the first 48 hours generally are delayed for 2 to 3 months • Major use of hospital resources due to increased risk for infection, bleeding and time in the hospital Emergency Surgery 24 - 48 Hours 24 No Surgery 3 Months Surgery Permitted After 3 Months
ARS - Hemopoietic Syndrome • Radiation dose > 100 rems • Nausea, vomiting and anorexia start within 12 hrs & lasts 1 -2 days. • Bone marrow depression - lymphocyte count at 48 hours indicates severity • Complications - sepsis, hemorrhage, anemia, impaired wound healing 25
ARS - Gastrointestinal Syndrome • Radiation dose > 600 rems • Damages intestinal lining • Nausea and vomiting within the first 2 - 4 hours • May develop diarrhea • Associated with severe infections • Bloody diarrhea and persistent high fever are an ominous sign 26
ARS - Central Nervous System • Radiation dose > 1, 000 rems • Brain bleeding and swelling • Very disoriented or unconsciousness • Death within hours 27
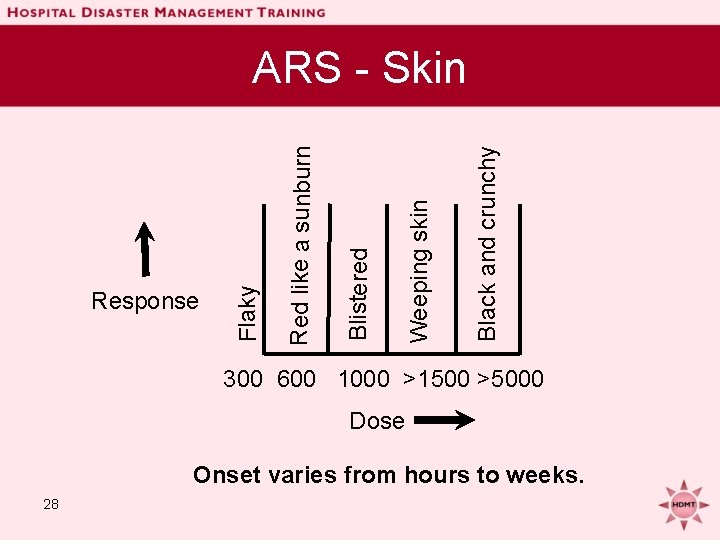
Black and crunchy Weeping skin Blistered Red like a sunburn Response Flaky ARS - Skin 300 600 1000 >1500 >5000 Dose Onset varies from hours to weeks. 28
Hospital Considerations • Utilize radiation experts in your facility • Call MAC if you suspect a radiologically contaminated patient has arrived at hospital – Phone 24/7 (866) 940 -4401 • Contact LA County Radiation Management Office (213) 351 -7897 • State (800) 852 -7550 29
Hospital Considerations • Time-Distance-Shielding-Dose • Do not delay treatment for life threatening injuries or illnesses for decontamination • Universal fear of radiation can lead to panic & misunderstandings – Accurate public information essential! 30
Hospital Considerations • Long-term care and resources may be needed to care for these patients • Internally contaminated victims may need to be isolated from other patients • Most victims will be able to be decontaminated, treated and sent home 31
Additional Resources • H&HS: Radiation Event Medical Management: remm. nlm. gov • Oak Ridge Institute for Science and Education orise. orau. gov • CDC bt. cdc. gov/radiation • Los Angeles County: MARRP (Multi-Agency Radiation Response Plan) 32
Summary • Radiation Protection: Time. Distance, Shielding, Quantity • Radiation exposure alone does not usually result in contamination. • Do not delay life-saving treatment to decontaminate radiologically contaminated victims. • Identify your local radiological experts. 33
Questions ? 34
- Slides: 34