Radiological Category Thoracic Principal Modality 1 General Radiology
- Slides: 15
Radiological Category: Thoracic Principal Modality (1): General Radiology Principal Modality (2): None Case Report 710 Submitted by: Robert E. Klinglesmith, M. D. Faculty reviewer: Sandra A. A. Oldham, M. D. , FACR, The University of Texas Medical School at Houston Date accepted: 16 March, 2010
Case History 25 year old female G 1 P 0 at 26. 3 weeks gestation presents to outside facility with fever, malaise and mildly productive cough. • Diagnosed with CAP, prescribed azithromycin and discharged. • Returned to facility the next day, was discharged with no change in management. • Returned to facility day 3 in respiratory distress, intubated and transferred to MHH by air ambulance. • On arrival to MHH, the patient was admitted to the ICU • Sonography diagnosed fetal demise, a stillborn fetus was delivered. • Respiratory distress worsened, requiring increased ventilatory and high dose pressor support. • On hospital 16, after severe multi-organ failure and clinical brain death, the family withdrew life support. The patient expired 15 minutes later.
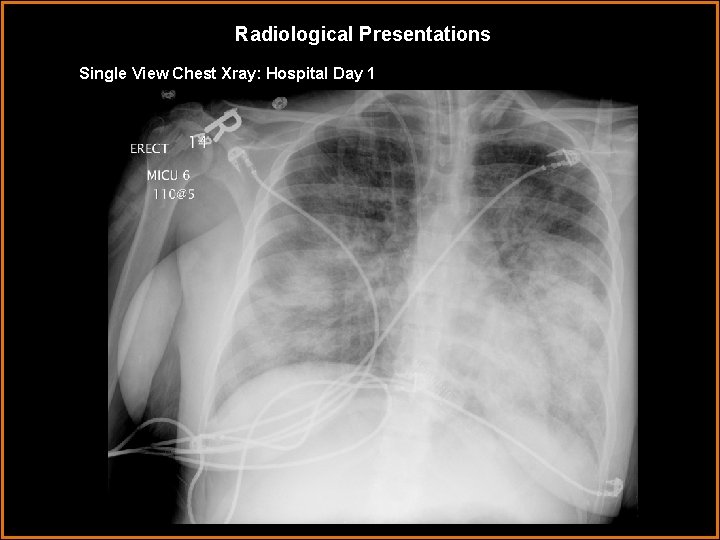
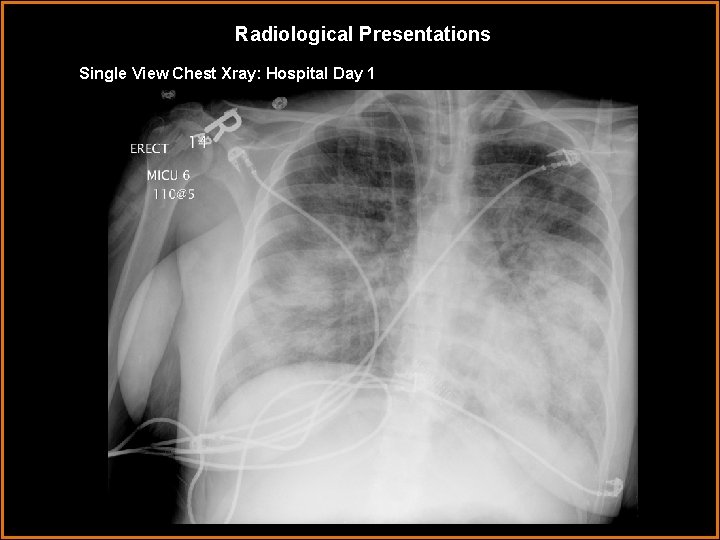
Radiological Presentations Single View Chest Xray: Hospital Day 1
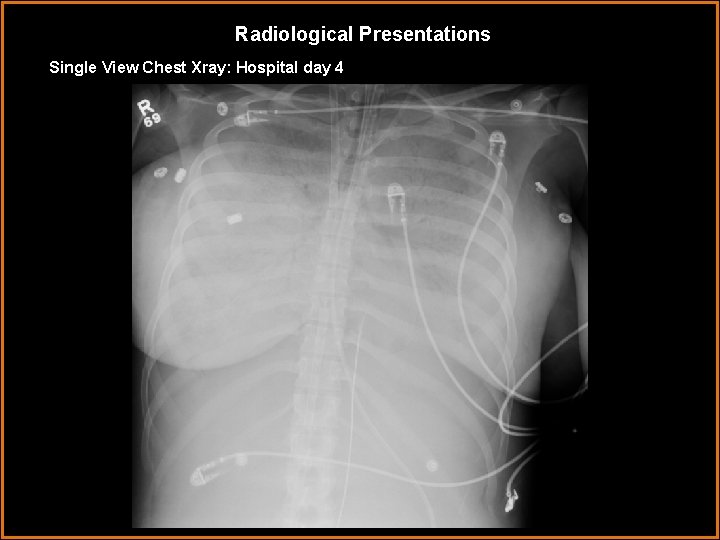
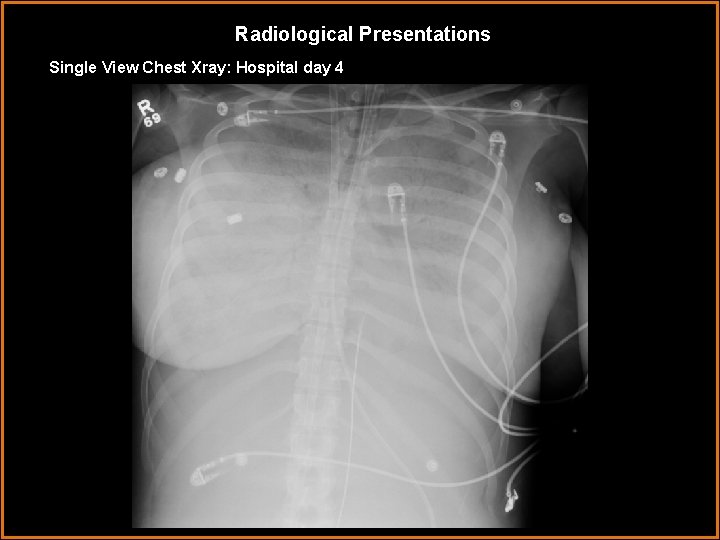
Radiological Presentations Single View Chest Xray: Hospital day 4
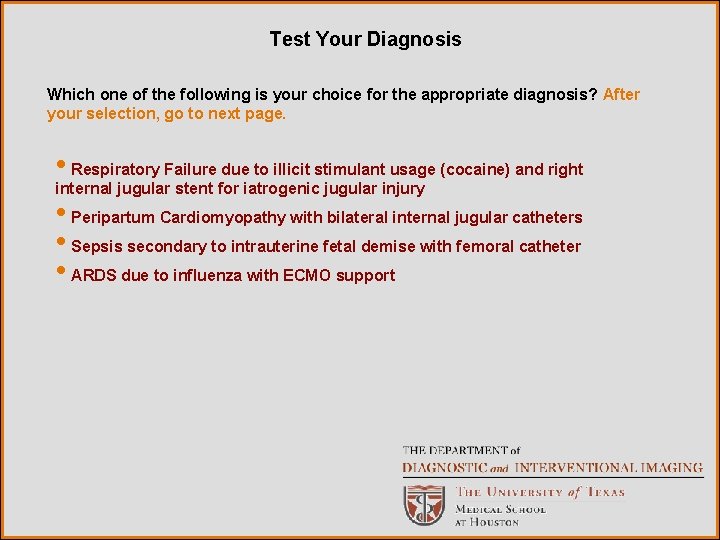
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Respiratory Failure due to illicit stimulant usage (cocaine) and right internal jugular stent for iatrogenic jugular injury • Peripartum Cardiomyopathy with bilateral internal jugular catheters • Sepsis secondary to intrauterine fetal demise with femoral catheter • ARDS due to influenza with ECMO support
Findings and Differentials Findings: Hospital Day 1: Bilateral airspace opacification with lower lobe predominance and air bronchograms. Endotracheal intubation, right internal jugular central venous catheter. Hospital Day 4: Interval progression diffuse opacification of the lungs bilaterally with air bronchograms. ET, nasogastric tubes in appropriate positioning. Left internal jugular central venous catheter terminating in the left subclavian vein. Right internal jugular catheter and IVC catheter. Differentials: • Cocaine-related acute respiratory failure with right venous stent for iatrogenic injury to jugular vein • Peripartum Cardiomyopathy and bilateral internal jugular venous access • Sepsis secondary to intrauterine fetal demise with femoral catheter • ARDS with ECMO support
Discussion Extracorporeal Membrane Oxygenation (ECMO), is a method of providing gas exchange through a modified cardiopulmonary bypass circuit. It is indicated for patients with severe but reversible respiratory or cardiac compromise. The circuit was most commonly used to assist in support of neonates with hyaline membrane disease. The external circuit provided not only gas exchange, but also protection from iatrogenic injury. Patients who required high end-expiratory pressures with conventional ventilator support were susceptible to barotrauma. Examples include pneumothoraces and pneumomediastinum, depending on the location of eruption [1, 5]. ECMO support directly improves oxygenation without the need for increasing ventilator pressures. Barotrauma risk is thus reduced. Use of ECMO in adult populations was sporadic until the outbreak of the novel Influenza A (H 1 N 1) virus in 2009. The rapid progression of respiratory distress in pregnant or otherwise at-risk adults required an aggressive approach to support, [2], The CESAR trial [3], demonstrated that ECMO was superior to conventional ventilatory support in selected patients with severe respiratory distress. Common complications include thromboembolism/coagulopathy, infection, need for pressor support, physiologic increase in lung opacity and limb ischemia [1, 4, 6]. Benefits of ECMO use include vital oxygenation support without barotraumas such pneumomediastinum and pneumothorax seen in conventional mechanical ventilation.
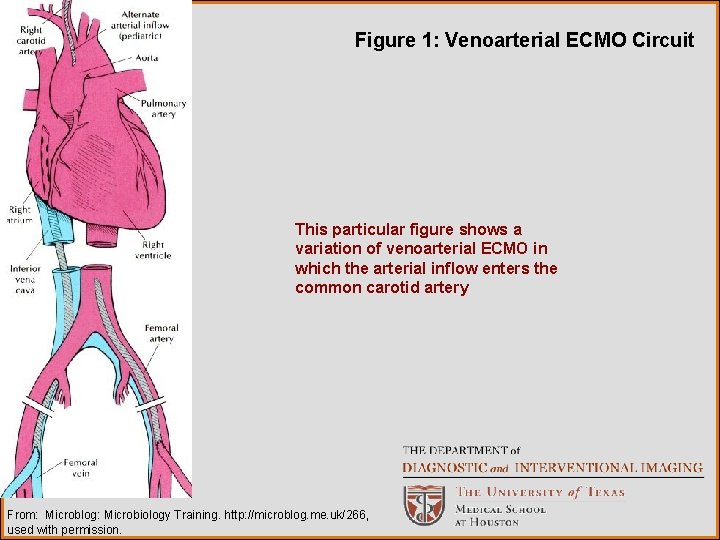
Discussion Venoarterial circuits provide more cardiac support, and are thus used in patients after cardiac surgery or failure [4, 6]. Correct catheter position for venous circuits include the tip of the draining catheter in the right atrium and the returning catheter in the common femoral or axillary veins. The venoarterial circuits include a draining cannula in the right internal jugular vein and return to the right common carotid artery, respectively [6]. This case demonstrates an adult venous circuit with the draining catheter in the right atrium and the returning catheter in the IVC. Conventional radiography of the chest in H 1 N 1 influenza patients may initially show predominantly lower and middle lobe consolidation with progression to diffuse, extensive bilateral consolidation [5].
Discussion The radiologist plays a central role in assisting the surveillance of ECMO line placement and progression of disease. Among the contributions of the radiologist are evaluation of the severity of pulmonary disease – including vigilance for cavitation, pleural effusion, barotrauma or pneumatocele formation – and assessment of cannula and catheter placement [6].
Discussion DIFFERENTIAL DIAGNOSES: Cocaine related lung injury would more commonly give the appearance of cardiogenic pulmonary edema [7]. Jugular vein stents are metal density and wire or wire basket appearance [10]. It would not account for the IVC line. Although peripartum cardiomyopathy may create a picture of cardiogenic pulmonary edema, there would be prominence of the cardiac silhouette and perihilar dominance in the initial film. Bilateral IJ access is not unheard of, but again does not address the appearance of a line in the inferior vena cava. Of note, ECMO has been successfully used in the treatment of peripartum cardiomyopathy [8] Intrauterine fetal demise was a contributing factor in this case. Sepsis was a subsequent complication Chest roentgenogram findings following sepsis typically present an ARDS pattern [9]. It does not tend to progress to diffuse bilateral opacification, as seen in this case. A femoral catheter is indeed placed, but is only half of the venous circuit.
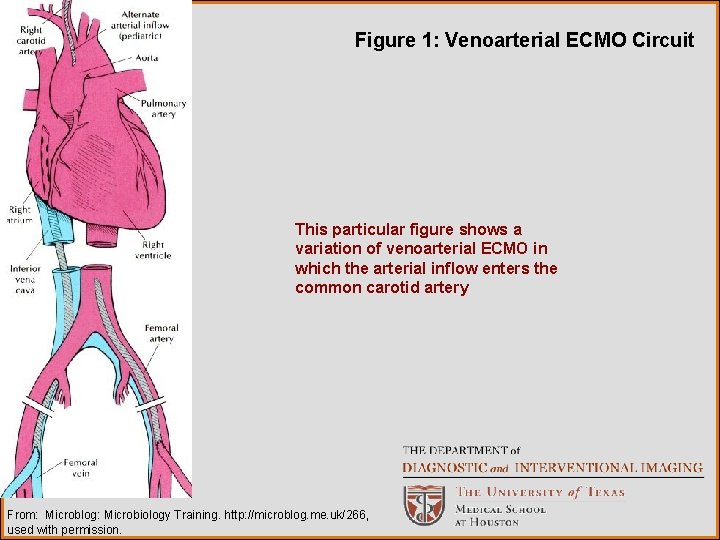
Figure 1: Venoarterial ECMO Circuit This particular figure shows a variation of venoarterial ECMO in which the arterial inflow enters the common carotid artery From: Microblog: Microbiology Training. http: //microblog. me. uk/266, used with permission.
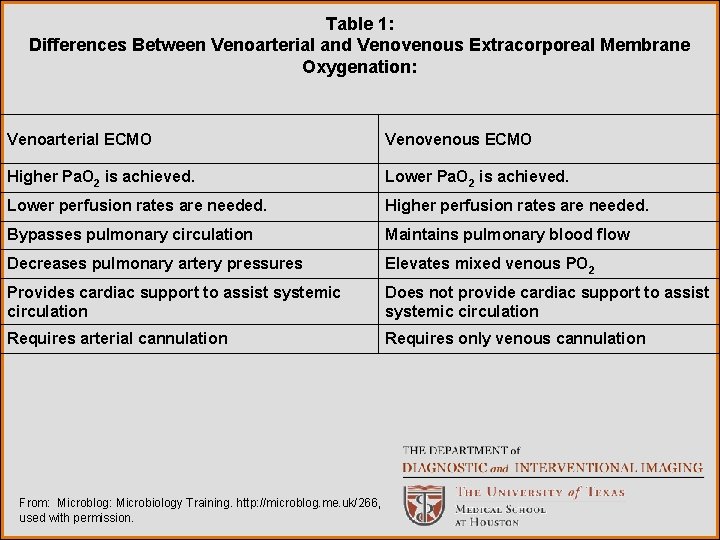
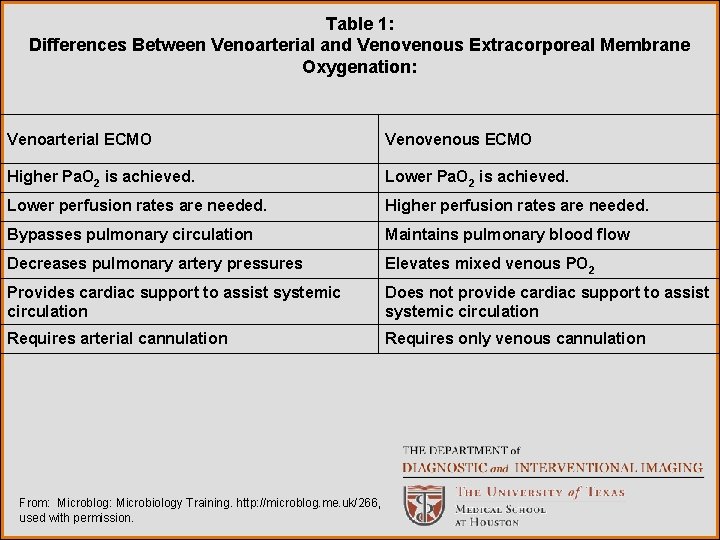
Table 1: Differences Between Venoarterial and Venovenous Extracorporeal Membrane Oxygenation: Venoarterial ECMO Venovenous ECMO Higher Pa. O 2 is achieved. Lower perfusion rates are needed. Higher perfusion rates are needed. Bypasses pulmonary circulation Maintains pulmonary blood flow Decreases pulmonary artery pressures Elevates mixed venous PO 2 Provides cardiac support to assist systemic circulation Does not provide cardiac support to assist systemic circulation Requires arterial cannulation Requires only venous cannulation From: Microblog: Microbiology Training. http: //microblog. me. uk/266, used with permission.
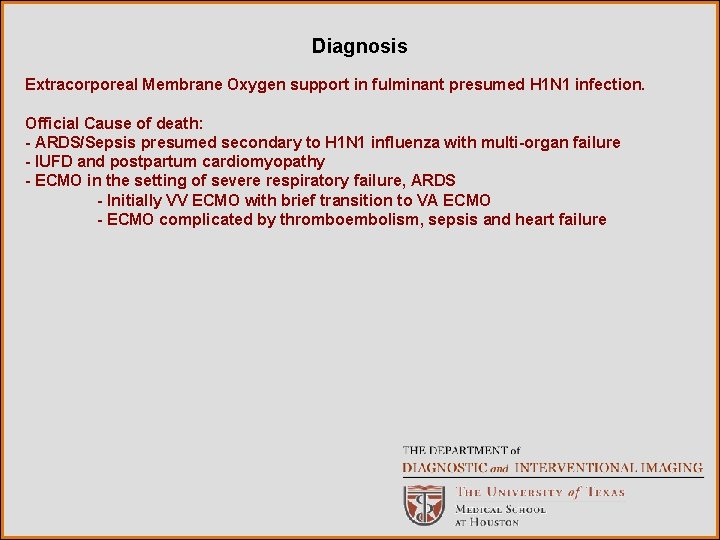
Diagnosis Extracorporeal Membrane Oxygen support in fulminant presumed H 1 N 1 infection. Official Cause of death: - ARDS/Sepsis presumed secondary to H 1 N 1 influenza with multi-organ failure - IUFD and postpartum cardiomyopathy - ECMO in the setting of severe respiratory failure, ARDS - Initially VV ECMO with brief transition to VA ECMO - ECMO complicated by thromboembolism, sepsis and heart failure
References 1. Hermans G, Meersseman A, Wilmer B, Meyns H, Bobbaers H. Extracorporeal Membrane Oxygenation: Experience in an adult medical ICU. Thorac Cardiov Surg 2007; 55: 223 -228. 2. Bishop JF, Murnane MP, Owen R. Australia’s winter with the 2009 pandemic Influenza A (H 1 N 1) virus. N Engl J Med 2009; 361: 2591 -2594. 3. Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assement of conventional ventilatory support versus extracorporeal membrane oxygentation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 2009; 374: 351 -1363. 4 Marasco SF, Lukas G, Mc. Donald M, Mc. Millan J, Ihle B. Review of ECMO (Extracorporeal Membrane Oxygenation) support in critically ill adult patients. Heart, Lung and Circulation 2009; 17 S: S 41 -S 47. 5. Hui DS, Lee N, Chan PKS. Clinical management of pandemic (H 1 N 1) infection. Chest 2009 December 18, prepublished ahead of print 1 -41.
References 6. Jamadar DA, Kazerooni EA, Cascade PN, Fazzalari FL, Vydareny KH, Bartlett RH. Extracoporeal Membrane Oxygenation in adults: Radiographic findings and correlation of lung opacity with patient mortality. Radiology 1996; 198: 693 -698. 7. Gotway MB, Marder SR, Hanks DK, et al. Thoracic complications of illicit drug use: An organ system approach. Radiographics 2002; 22: 119 -S 135. 8. Palanzo DA, Baer LD, El-Banayosy A, et al. Successful treatment of postpartum cardiomyopathy with extra corporeal membrane oxygenation. Perfusion 2009; 24: 75 -79. 9. Webb WR. Pulmonary edema, the acute respiratory distress syndrome, and radiology in the intensive care unit. In: Webb WR, Higgins CB, eds. Thoracic imaging: Pulmonary and cardiovascular radiology. Philadelphia, PA: Lippincott Williams & Wilkins 2005: 331355. 10. Wright KC, Wallace S, Charnsangavej C, Carrasco CH, Gianturco C. Percutaneous endovascular stents: An experimental evaluation. Radiology 1985; 156: 69 -72.