Radiological Category Mammography Principal Modality 1 Mammography Principal




- Slides: 23
Radiological Category: Mammography Principal Modality (1): Mammography Principal Modality (2): Nuclear Medicine Case # 787 Submitted by: Robert E. Klinglesmith, M. D. , Psy. D. Faculty reviewer: La. Verne Ingram, M. D. , The University of Texas Medical School at Houston Date accepted: 3 March, 2011 Special thanks to Laura Kidd, MD, Department of Pathology and Laboratory Medicine, University of Texas Medical School at Houston for assistance with histology.
Case History A 33 year old female presented for routine mammographic screening. She had previously undergone bilateral breast augmentation mammoplasty with no complications. She had no complaints at the time of presentation.
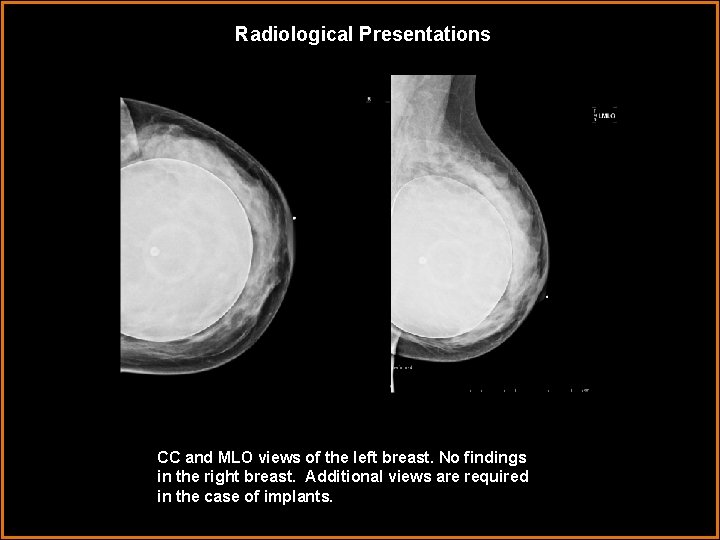
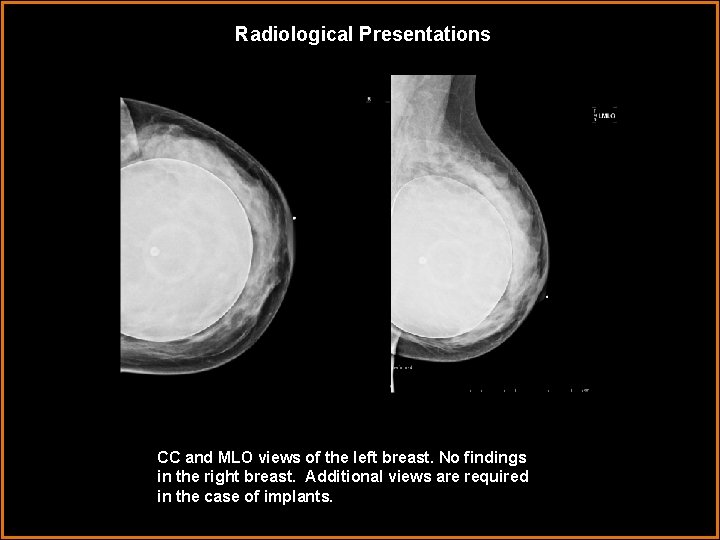
Radiological Presentations CC and MLO views of the left breast. No findings in the right breast. Additional views are required in the case of implants.
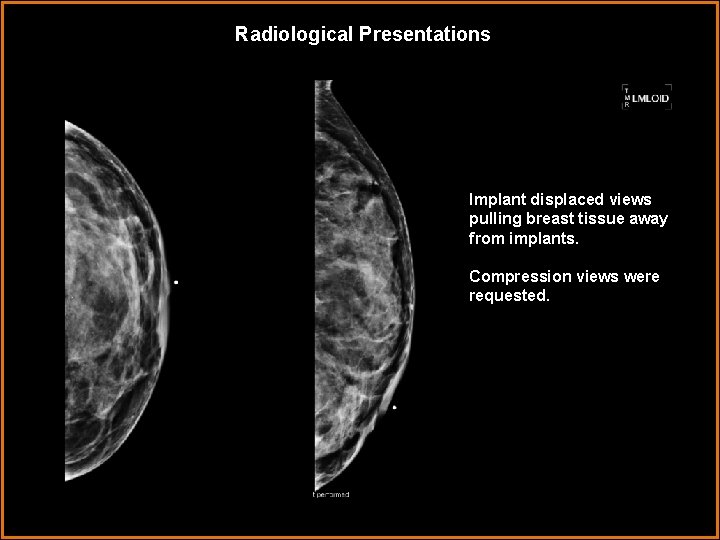
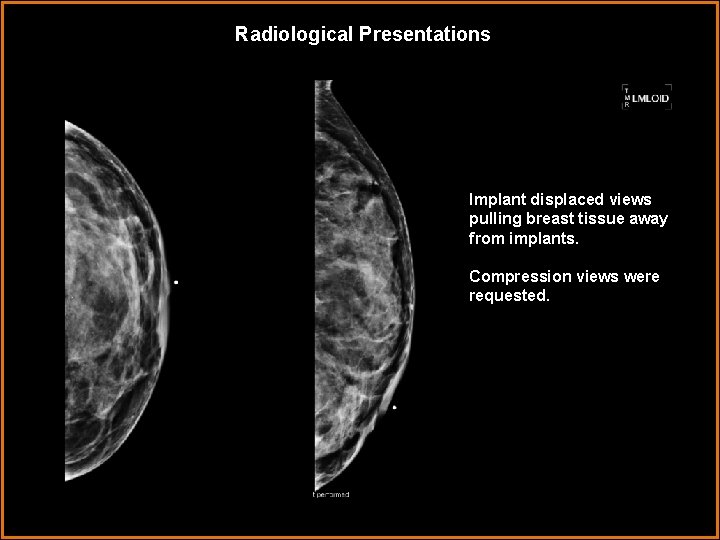
Radiological Presentations Implant displaced views pulling breast tissue away from implants. Compression views were requested.
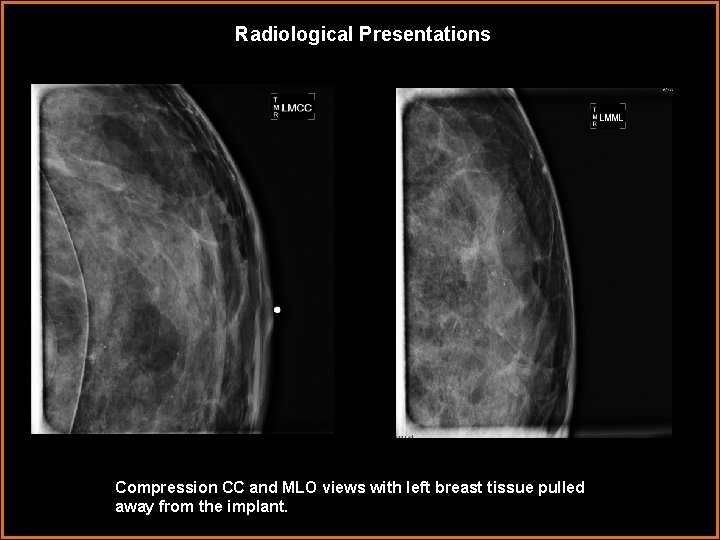
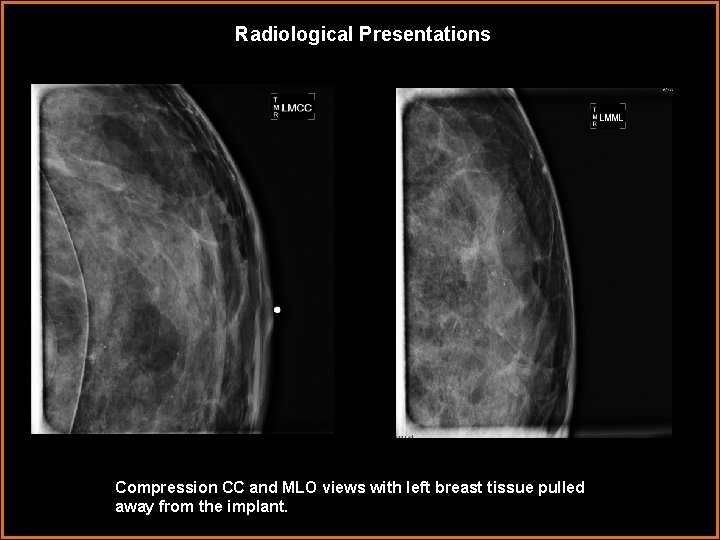
Radiological Presentations Compression CC and MLO views with left breast tissue pulled away from the implant.

Findings and Differentials Findings: When compared to prior, outside facility films, there is a new area of grouped heterogeneous calcifications in the left breast at 12 o'clock middle depth. Suspicious of malignancy. Stereotactic biopsy is recommended.

Radiological Presentations Review of implant displaced views with the concerning calcifications highlighted.
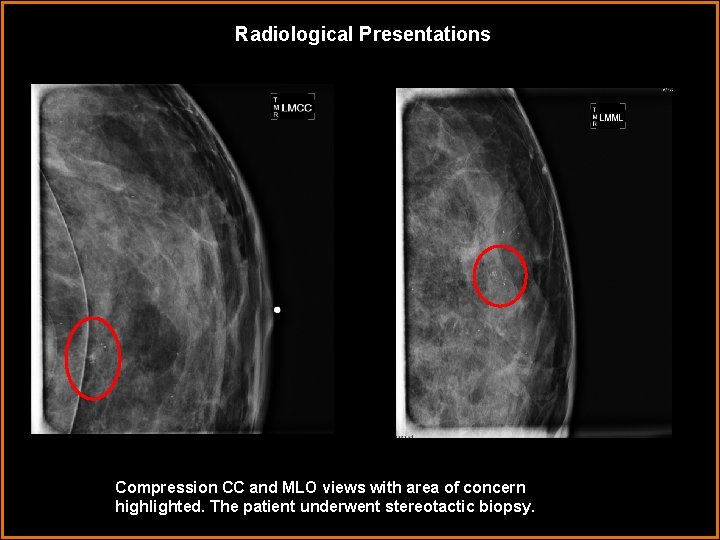
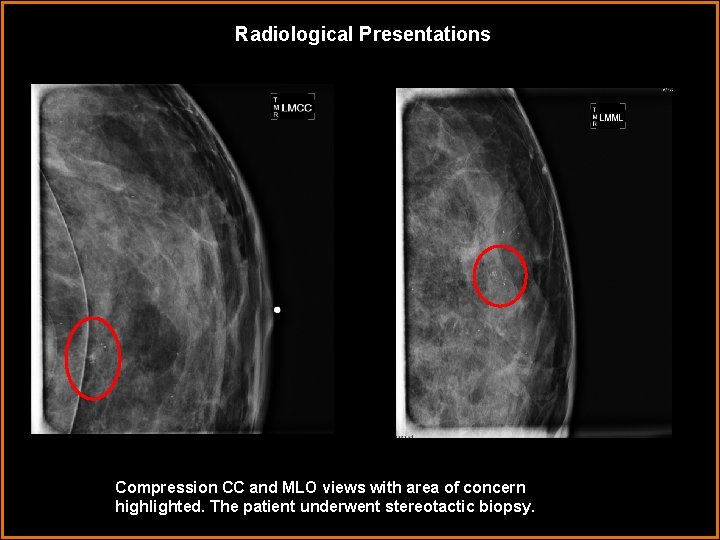
Radiological Presentations Compression CC and MLO views with area of concern highlighted. The patient underwent stereotactic biopsy.
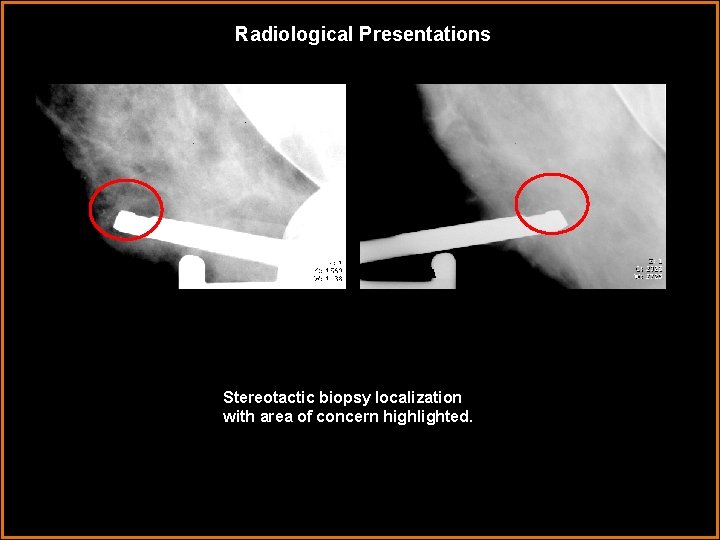
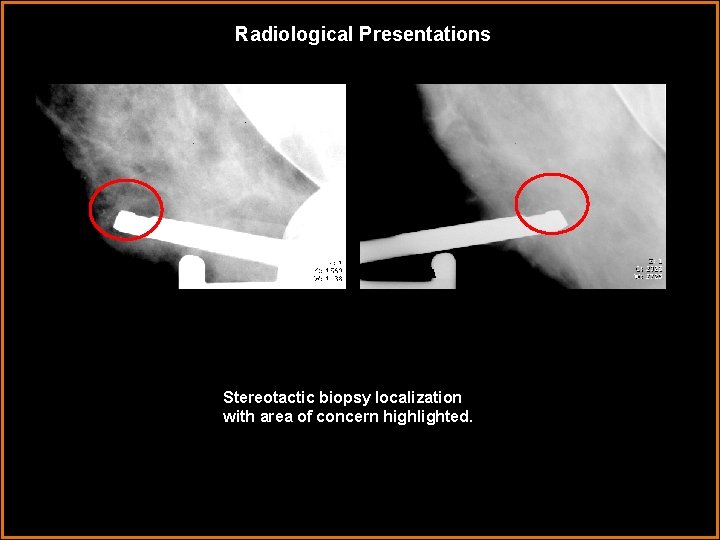
Radiological Presentations Stereotactic biopsy localization with area of concern highlighted.
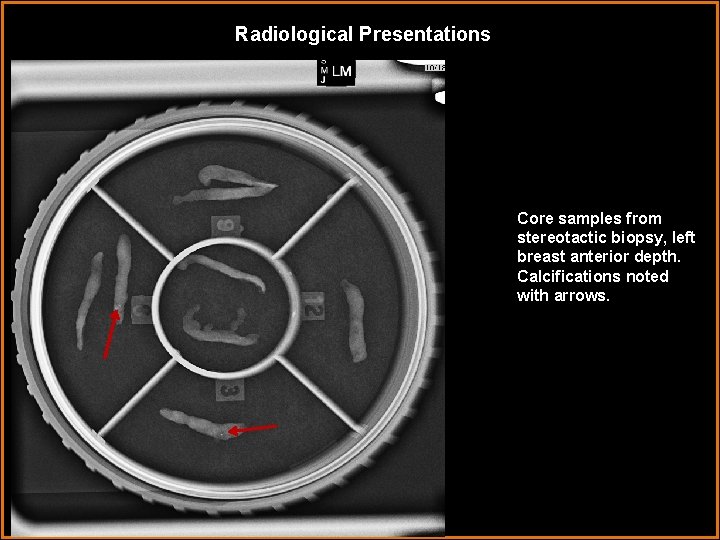
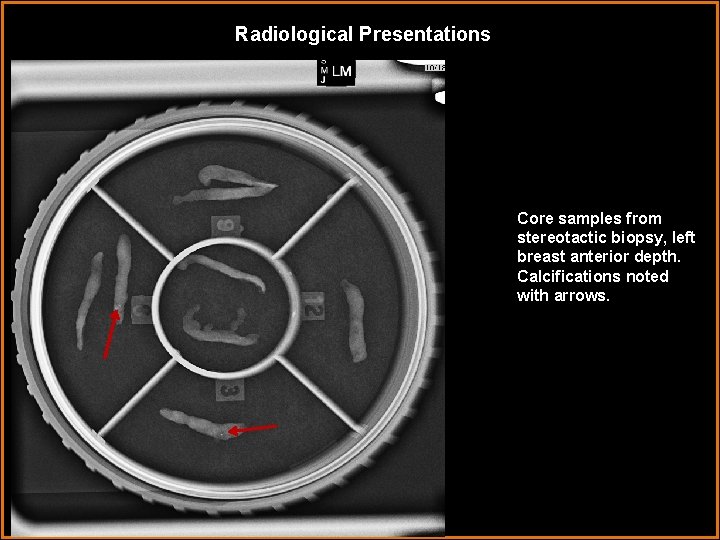
Radiological Presentations Core samples from stereotactic biopsy, left breast anterior depth. Calcifications noted with arrows.
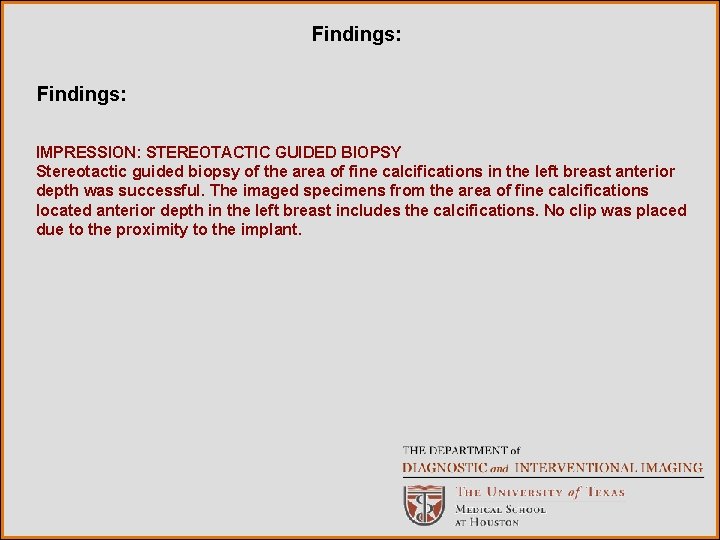
Findings: IMPRESSION: STEREOTACTIC GUIDED BIOPSY Stereotactic guided biopsy of the area of fine calcifications in the left breast anterior depth was successful. The imaged specimens from the area of fine calcifications located anterior depth in the left breast includes the calcifications. No clip was placed due to the proximity to the implant.
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Post traumatic calcifications secondary to implantation scarring • Degenerating fibroadenoma • Fibrocystic change • Ductal carcinoma in situ (DCIS) • Implant rupture with leak
Discussion Evaluation of breast with implants is complicated by the distortion of normal tissue distribution by the implant and by difficulty in positioning. This is less common with sub pectoral implants. In order to complete a screening mammogram in the presence of retroglandular (or pre-pectoral) implants, the breast tissue is manually displaced anteriorly. The sequelae of augmentation implants includes rupture and calcification. Calcification tends to be coarse and dense or ringlike in a pattern more like fat necrosis. Calcifications tend to be most coarse, and breast parenchyma most dense, in the case of direct injection of silicone. Although this is not currently approved in the US, some patients have had augmentation done remotely or overseas [1]. The current case involves retroglandular placement of saline implants. This is identifiable by the presence of a valve and relatively lower density/attenuation than expected for a silicone implant. Had such an implant ruptured, the loss of symmetry would have been rapid [1]. Diffused saline in the breast parenchyma would likely have been resorbed. Therefore, implant rupture could not be the cause of the findings. Similarly, a focal area of heterogeneous cacifications is not consistent with either capsular calcification or scarring, making the choice of post-traumatic/post-surgical sequelae incorrect.
Discussion Fibroadenomas tend to be palpable lesions. The calcifications can become large and bizarre. In their early stages, the calcifications may be mistaken for carcinoma [2]. Microscopically, the fibroadenoma is well circumscribed [3]. The current case included a new cluster of heterogeneous calcifications, which is not consistent with degenerating fibroadenoma. Although less prognostic, the patient denied palpable masses. Given the history of augmentation, a fibroadenoma may arguably have been more readily palpable given the limited tissue anterior to the implant. Fibrocystic change is the term preferred when describing benign evolution of intraand extralobar stroma and prominent lobules. This change may or may not present as a palpable mass [4]. On mammography, fibrocystic change may appear focal and well defined or even ill-defined. In the latter case, this is difficult to differentiate from malignancy. Associated, benign appearing calcifications are common [5].
Discussion Ductal carcinoma in situ is the most frequent breast cancer identified by mammography, and most often by its appearance as a group of calcifications [6]. These calcifications can actually be stable for up to 2 years, forcing biopsy of any suspicious lesion regardless of stability [1]. The development of DCIS results in rapid outstripping of the vascular supply, leading to necrosis and ultimately the calcifications that make its presence visible on mammography [6]. The current case demonstrates new suspicious calcifications. Mastectomy is curative in 95% of cases. Surgical advances have improved breast conservation surgery. However, subtotal resection continues to have a higher rate of recurrence [7]. The BI-RADS lexicon for describing calcifications includes intermediate suspicion in the case of amorphous, heterogeneous or indistinct calcifications (Category 4) [8].

Discussion Low and medium power fields, respectively, demonstrating DCIS. Hematoxylin and eosin staining. Area of comedonecrosis is highlighted with arrow.
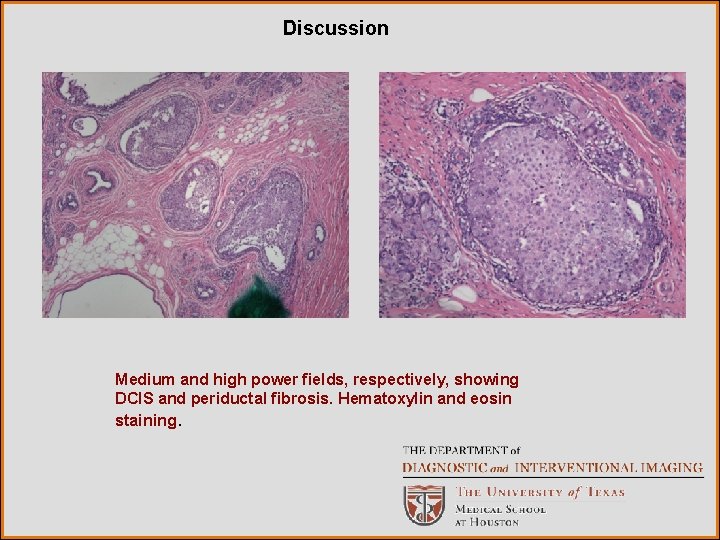
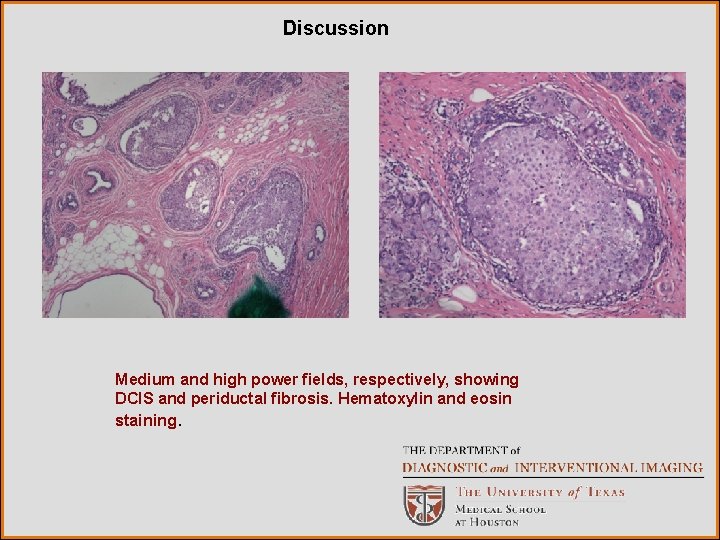
Discussion Medium and high power fields, respectively, showing DCIS and periductal fibrosis. Hematoxylin and eosin staining.
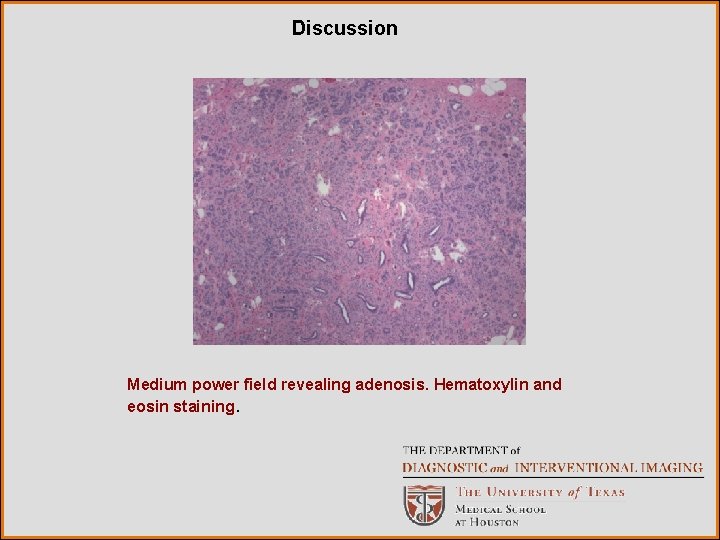
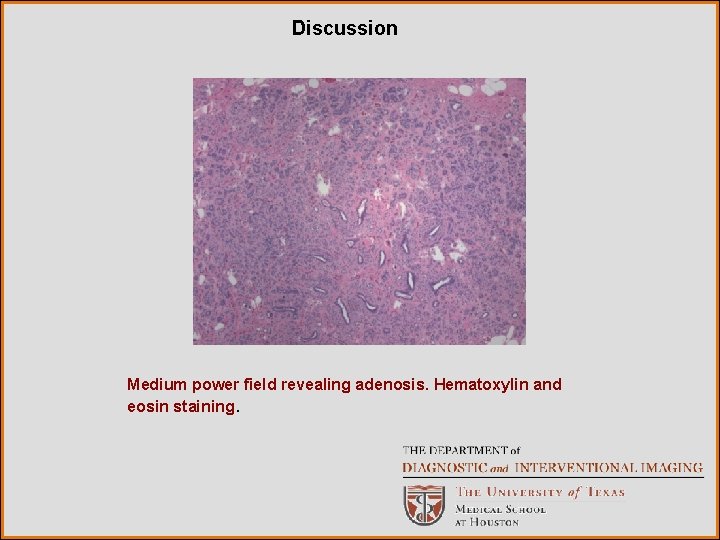
Discussion Medium power field revealing adenosis. Hematoxylin and eosin staining.
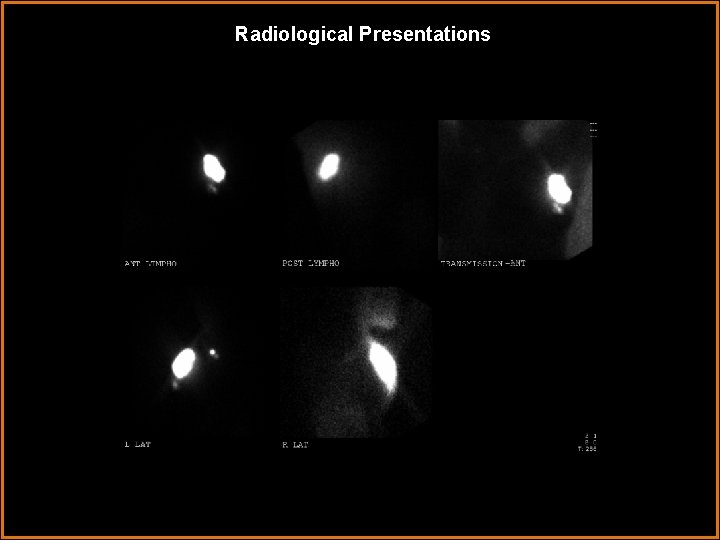
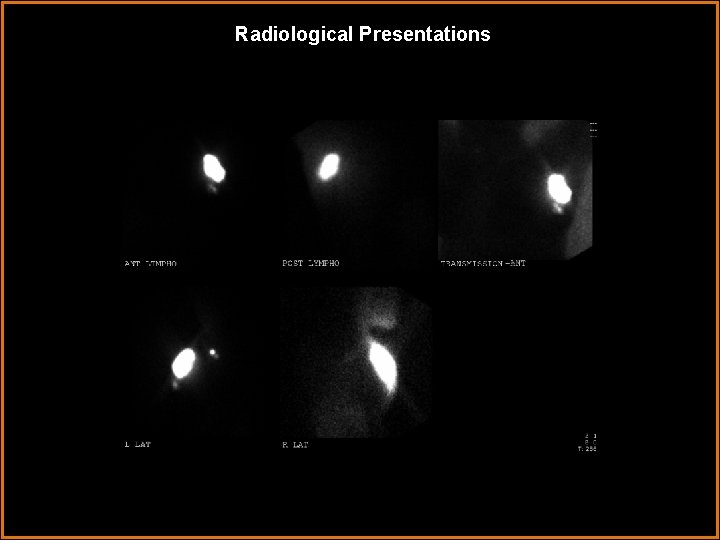
Radiological Presentations
Findings: Lymphoscintigraphy: There is focal tracer uptake in the left axilla, consistent with sentinel node. Injection site is visualized.

Diagnosis Radiologic diagnosis: New group of heterogeneous calcifications in the left breast, suspicious for malignancy. BI-RADS 4. Pathologic diagnosis: Ductal carcinoma in situ (DCIS), high grade, solid type with comedonecrosis and pagetoid spread into lobules. Microcalcifications identified in benign and malignant profiles. Estrogen and progesterone receptors positive. Areas of adenosis. Outcome: The patient went on to have the implant removed with simultaneous partial mastectomy. Surgical pathology of the mastectomy sample yielded DCIS with comedonecrosis and atypical ductal hyperplasia. Surgical margins were negative. The implant capsule was intact. Sentinel lymph node biopsy was negative.
References 1. De. Paredes AS. Analysis of calcifications. In De. Paredes AS, ed Atlas of mammography 3 rd ed. Lippincott Williams and Wilkins 2007, online edition. 2. De. Paredes AS. Circumscribed masses. In De. Paredes AS, ed Atlas of mammography 3 rd ed. Lippincott Williams and Wilkins 2007, online edition. 3. Stricker TP, Kumar V. Characteristics of benign and malignant disease. In Kumar V, Abbas AK, Fausto N, Aster JC. Eds. Robbins and Cotran’s pathological basis for disease 8 th ed. Philadelphia, PA: Saunders Elselvier 2010, online edition. 4. Santen RJ, Mansel R. Benign Breast Disorders N Engl J Med 2005; 353: 275 -285 5. Lindfors KK, Le-Petross HT. Breast imaging. In: Brant WE & Helms CA eds. Fundamentals of diagnostic imaging 3 rd ed Lippincott Williams and Wilkins 2006 564601. 6. Lester SC. Carcinoma of the breast. In Kumar V, Abbas AK, Fausto N, Aster JC. Eds. Robbins and Cotran’s pathological basis for disease 8 th ed. Philadelphia, PA: Saunders Elselvier 2010, online edition.
References 7. Copeland EM, Hunt KK, Newman LA The breast. In Brunicardi FC, Andersen DK, Billiar TR, et al, eds. Schwartz’s principles of surgery 9 th ed. Mc. Graw Hill 2010, online edition. 8. American College of Radiolog (ACR). ACR BI-RADS-Mammography 4 th ed. In: ACR Breast imaging reporting and data system, Breast imaging atlas. Reston, VA. American College of Radiology; 2003.
 Erate category 2 eligible equipment
Erate category 2 eligible equipment Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Mammo qc
Mammo qc Cscc medical imaging
Cscc medical imaging Mammography
Mammography Mqsa requirements for mammography checklist
Mqsa requirements for mammography checklist Mcq breast anatomy
Mcq breast anatomy Breast ultrasound
Breast ultrasound Htc grid mammography
Htc grid mammography Hologic contrast enhanced mammography
Hologic contrast enhanced mammography Components of mammography machine
Components of mammography machine Lateral decentering grid
Lateral decentering grid Standard screening tomohd
Standard screening tomohd Sensory modality examples
Sensory modality examples Epistemic modality
Epistemic modality High modality examples
High modality examples Modality in software engineering
Modality in software engineering Cardinality and modality
Cardinality and modality Lexical vs auxiliary verbs
Lexical vs auxiliary verbs Modality microsoft services
Modality microsoft services Epistemic modality
Epistemic modality