Radiological Category Enter category here Principal Modality 1



- Slides: 22
Radiological Category: Enter category here Principal Modality (1): CT Principal Modality (2): Fluoroscopy Case Report 680 Submitted by: Joshua Franklin, M. D. Faculty reviewer: Venkateswar Surabhi, M. D The University of Texas Medical School at Houston Date accepted: 11 March 2010
Case History A 54 year old female presents to the emergency room with 3 day history of nausea, bilious vomiting, diarrhea, and severe abdominal pain. She has a past medical history of chronic abdominal pain and achalasia status post balloon dilatation in 2008. As part of her initial work up in the emergency room a CT of the abdomen and pelvis was performed. The patient was subsequently admitted during which time an Upper GI examination was also performed.
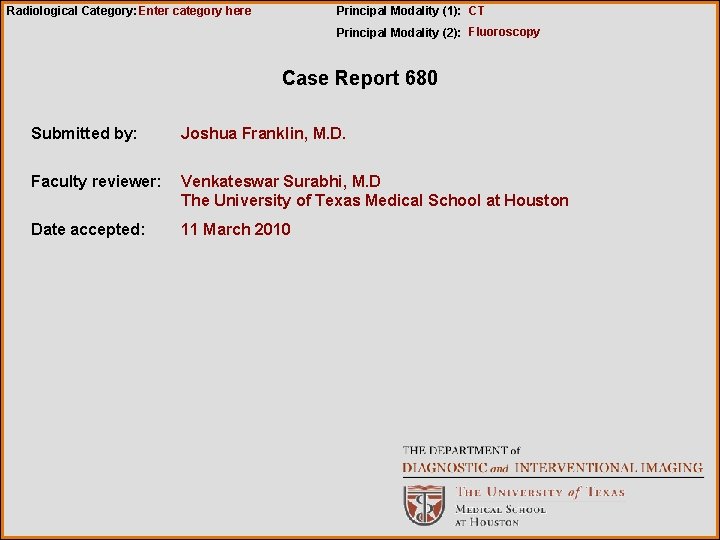
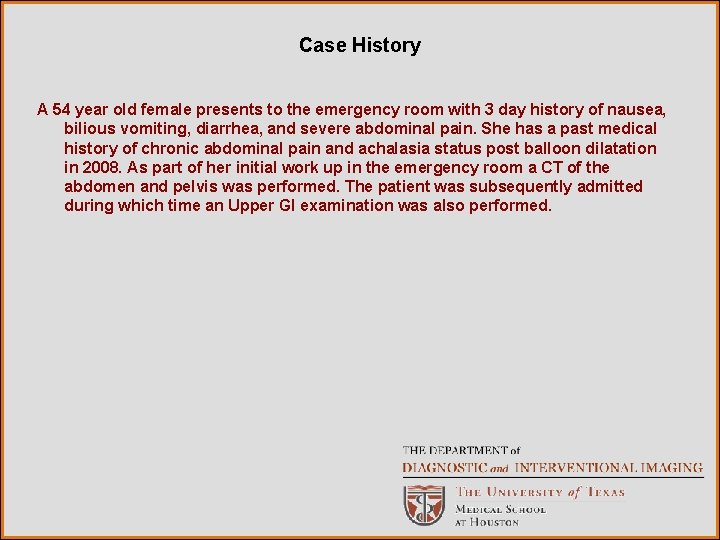
Radiological Presentations Figure 1 Figure 2 Figure 1, 2: Axial post contrast CT images
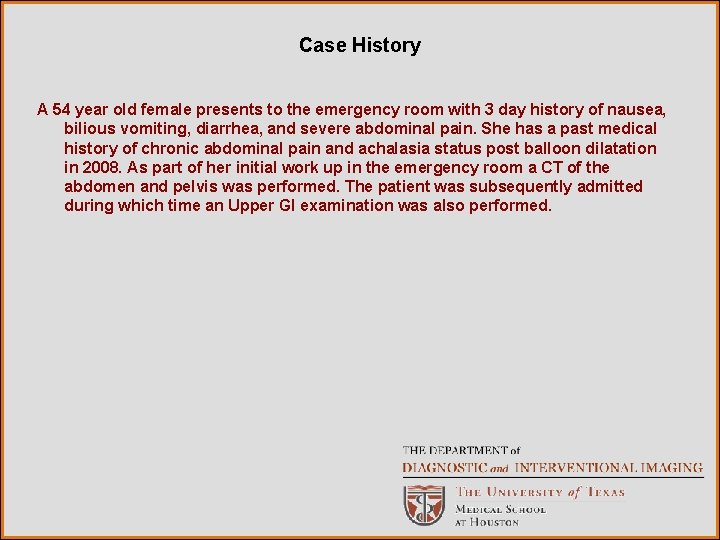
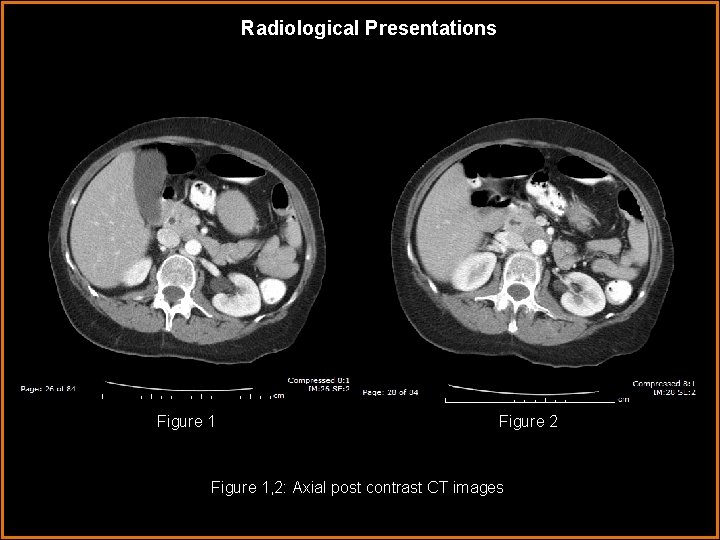
Radiological Presentations Figure 3 Figure 4 Figure 3, 4: Axial post contrast CT images
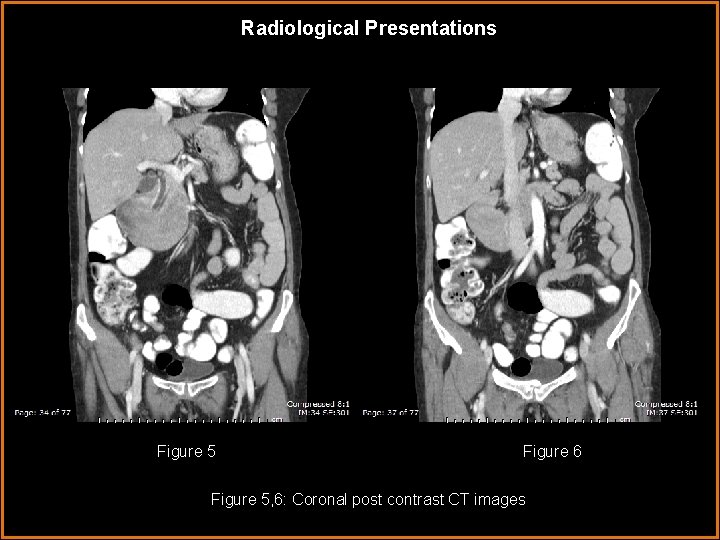
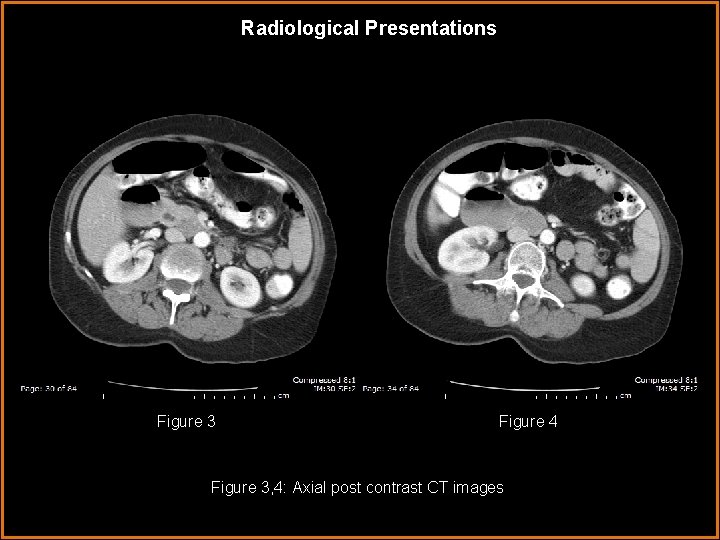
Radiological Presentations Figure 5 Figure 6 Figure 5, 6: Coronal post contrast CT images

Radiological Presentations Figure 7 Figure 8 Figure 7, 8 : Sagittal post contrast CT images

Radiological Presentations Figure 9: Double contrast upper GI Figure 10: Single contrast Upper GI
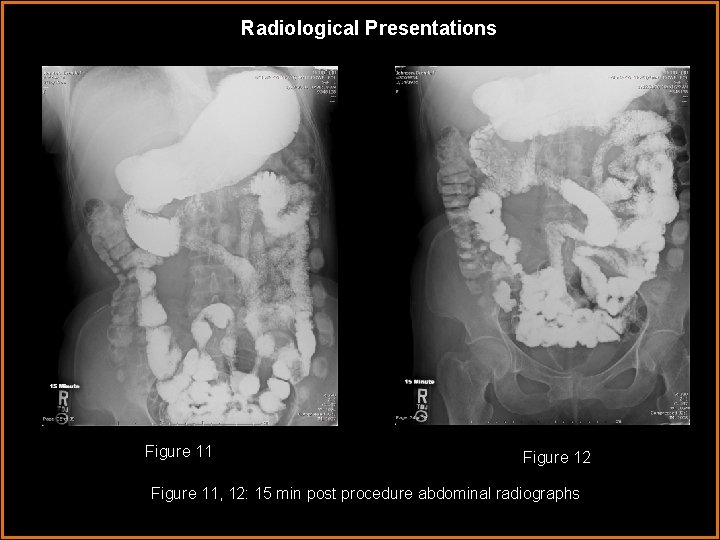
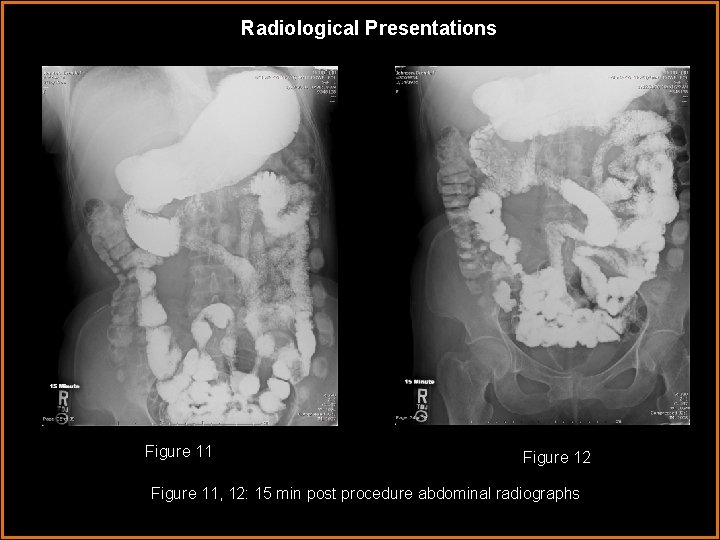
Radiological Presentations Figure 11 Figure 12 Figure 11, 12: 15 min post procedure abdominal radiographs
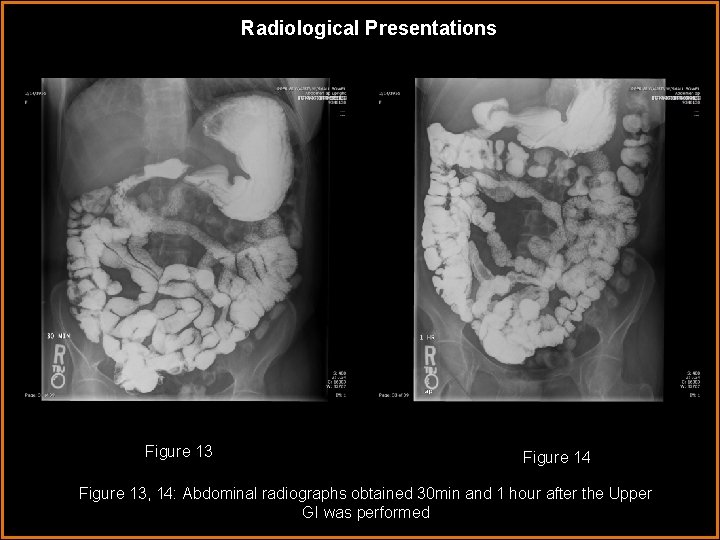
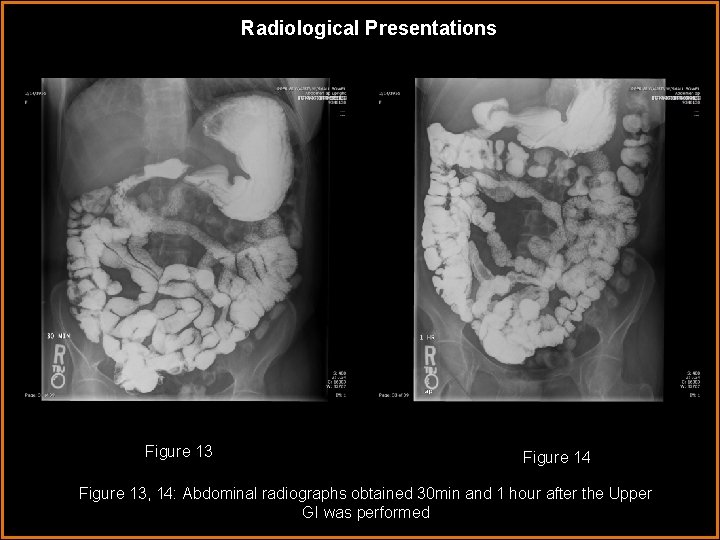
Radiological Presentations Figure 13 Figure 14 Figure 13, 14: Abdominal radiographs obtained 30 min and 1 hour after the Upper GI was performed
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Duodenal Ulcer • Intestinal pseudoobstruction • Pancreatic cancer • Superior Mesenteric Artery Syndrome • Duodenal Diverticulum
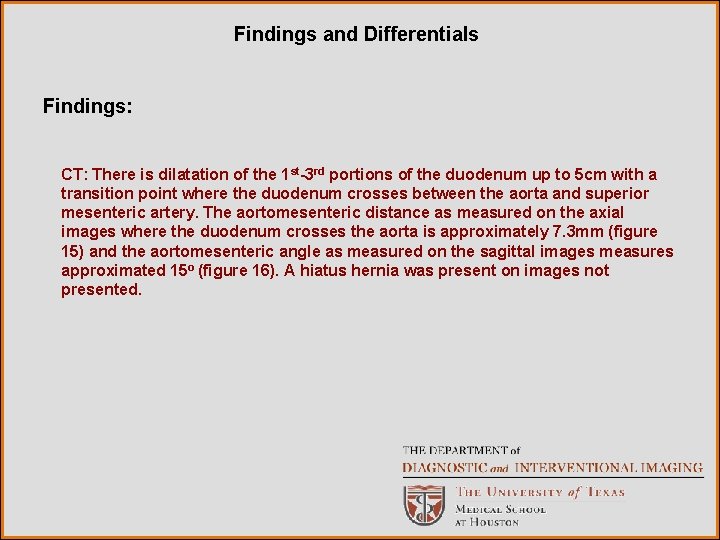
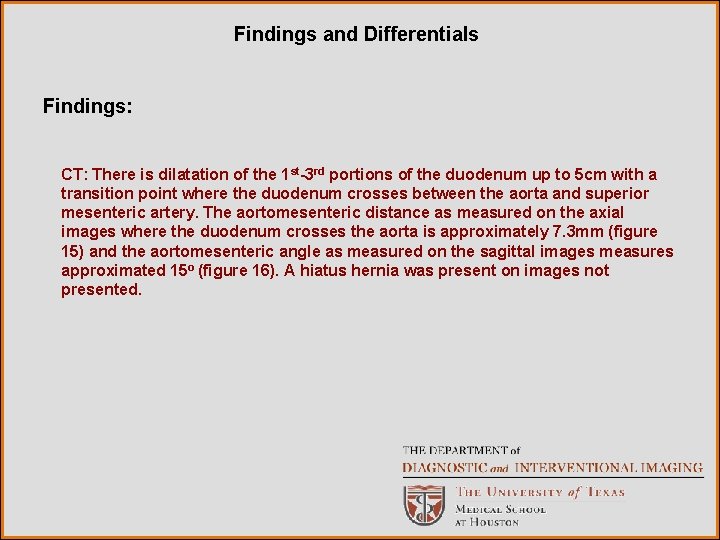
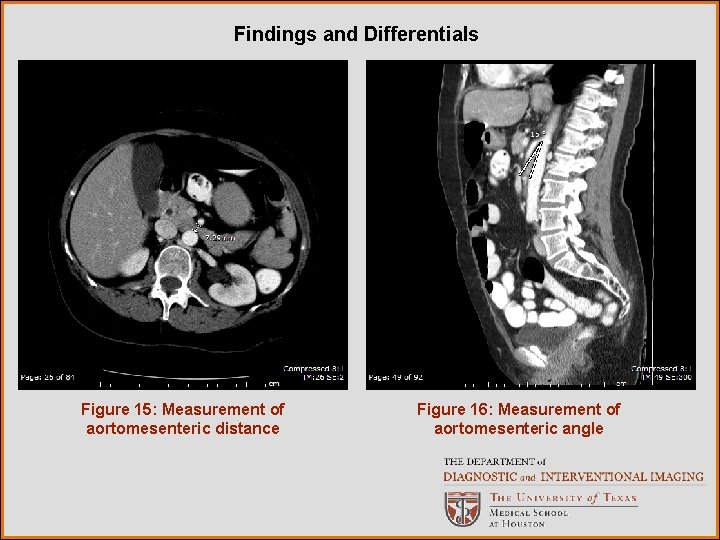
Findings and Differentials Findings: CT: There is dilatation of the 1 st-3 rd portions of the duodenum up to 5 cm with a transition point where the duodenum crosses between the aorta and superior mesenteric artery. The aortomesenteric distance as measured on the axial images where the duodenum crosses the aorta is approximately 7. 3 mm (figure 15) and the aortomesenteric angle as measured on the sagittal images measures approximated 15 o (figure 16). A hiatus hernia was present on images not presented.
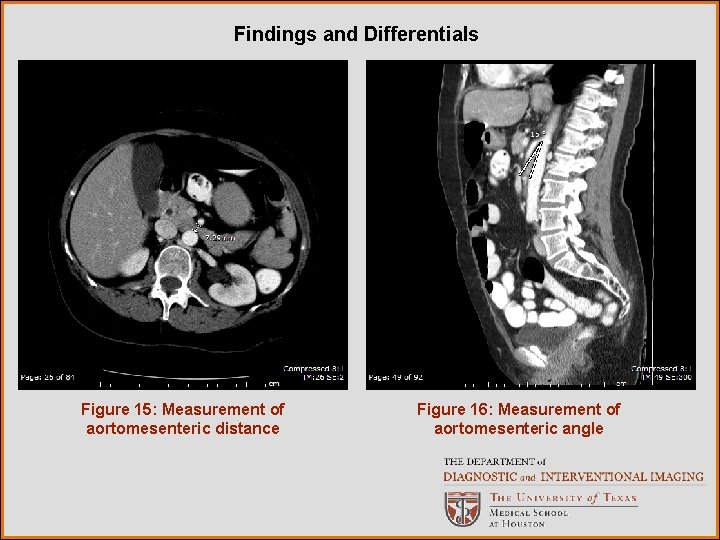
Findings and Differentials Figure 15: Measurement of aortomesenteric distance Figure 16: Measurement of aortomesenteric angle

Findings and Differentials Findings: Upper GI: The duodenum is dilated and hypokinetic. On several of the delayed images there is the appearance of an abrupt vertical cutoff at the distal 2 nd portion of the duodenum; however, there is no obstruction with contrast promptly flowing into the jejunum. Esophageal motility is normal. Small bowel transit time is normal with contrast reaching the colon by the 30 minute post examination radiograph. Other than the duodenum, there are no other dilated loops of bowel. Differentials: • Megaduodenum • Superior mesenteric artery syndrome
Discussion In the most general sense, megaduodenum is a term that applies to dilatation of the duodenum. Causes of megaduodenum are numerous and may be obstructive or non-obstrutive. The obstructive causes include tumors, intraluminal foreign bodies, adhesions, aortic aneurysms, intramural hematomas, and superior mesenteric artery syndrome amongst others. Non-obstructive megaduodenum, which can be considered a form of localized intestinal pseudoobstruction, also has a long differential that includes, but is not limited to collagen vascular diseases, visceral myopathies, and visceral neuropathies. 1, 2 One of the most commonly discussed, and likely over diagnosed etiologies for megaduodenum is superior mesenteric artery syndrome. 3 SMA syndrome, also known as Wilkie’s syndrome and chronic intermittent arteriomesenteric occlusion of the duodenum, is a rare condition in which the 3 rd part of the duodenum is compressed and occluded by a narrowed distance between the superior mesenteric artery and aorta.
Discussion Clinically, patients with SMA syndrome will present with symptoms of high intestinal obstruction, bilious emesis, postprandial discomfort and weight loss. The distance between the aorta and SMA is narrowed and the angle formed by the aorta and SMA is decreased in these patients. If SMA syndrome is seriously being considered over other forms of megaduodenum a history for risk factors that may lead to a decreased aortomesenteric angle should be obtained. These risk factors inlcude: Severe weight loss with depletion of mesenteric fat (as in cancer and burn patients), exaggerated lumbar lordosis, eating disorders such as anorexia, malabsorption, trauma, spinal deformity, and rapid growth without compensatory weight gain as seen in adolescents. 4 The syndrome is also much more common in young patients, with 2/3 between the ages of 10 and 39. 5 Traditionally, the radiologic diagnosis of SMA syndrome was made with a combination of fluoroscopic duodenography and conventional angiography. Since the late 1980 s and early 1990 s the use of cross sectional imaging, especially CT, in combination with fluoroscopy has become the method of choice for diagnosing SMA syndrome. 5 -7
Discussion Radiographically, the classic picture is a dilated duodenum with abrupt cut off of the duodenum in its 3 rd portion. This appearance, however, is nonspecific and is also seen in non-obstructive forms of megaduodenum. Strict radiographic criteria have been developed for the diagnosis of SMA syndrome to avoid this confusion. The 5 radiographic criteria for diagnosis of SMA syndrome are: 1) Dilatation of the 1 st and 2 nd portions of the duodenum with or without gastric dilatation. 2) Abrupt vertical and oblique compression of the duodenal mucosal folds 3) Antiperistaltic flow of contrast proximal to the obstruction resulting in to-andfro movements 4) 4 -6 hour delay in transit of contrast through the gastroduodenal region. 5) Relief of obstruction in a prone, knee-chest, or left lateral decubitus position, which decrease the drag on the small bowel mesentery 3 -5
Discussion As previously mentioned, the aortomesenteric angle and distance are decreased in patients with SMA syndrome. Patients with SMA syndrome have aortomesenteric distances of 2 -8 mm whereas the normal range is 10 -28 mm. Similarly, patients with SMA syndrome have decreased aortomesenteric angles of 6 -22 o whereas the normal range is 25 -60 o. 3 -7 These measurements have traditionally been obtained with angiography, but today they are more commonly obtained with CT. CT is noninvasive and is more effective at evaluating for other causes of duodenal dilation than conventional angiography. Also, if the SMA is anterolateral rather than directly anterior to the aorta, lateral projection angiography may underestimate the true aortomesenteric distance. 6 -7 In the presented case, many of the radiographic and clinical features of SMA syndrome are present. The patient presented with symptoms of high intestinal obstruction including bilious vomiting. On CT the duodenum was dilated with a transition point at the 3 rd portion and both the aortomesenteric distance and aortomesenteric angle were decreased measuring 7. 3 mm and 15 o respectively. On upper GI there was also a dilated duodenum with the suggestion of an abrupt vertical cutoff of contrast at the 3 rd portion just to the right of the spine.
Discussion Radiologically, the aortomesenteric distance and angle are decreased and the duodenum is dilated, but the other radiographic criteria are not met. Most importantly, no obstruction was demonstrated on upper GI. The duodenum was hypokinetic on upper GI, but there was no antiperistaltic flow of barium resulting in to-and-fro movements. Also, transit through the gastroduodenal region, although only followed to 1 hour, was noticeably delayed. Clinically, the presentation is atypical in that the patient is older than expected and does not have any of the previously described risk factors, such as recent and severe weight loss. While this case may not demonstrate SMA syndrome, it certainly could represent a form of non-obstructive megaduodenum. An interesting note is that although no esophageal motility disorder was noted on the upper GI, the patient has a history of achalasia status post balloon dilatation in 2008. Also of note is the history of chronic abdominal pain. The possible discovery of a 2 nd form of GI motility disorder in patient with chronic symptoms could indicate a chronic underlying systemic process.
Discussion Unfortunately, without more information, we can only speculate as to the etiology of this patient’s findings. One consideration is systemic sclerosis, which is commonly associated with achalasia and esophageal motility disorders as well as abnormalities of the small bowel. Systemic sclerosis is a known cause of both generalized and localized intestinal pseudo-obstruction, which includes megaduodenum. 2, 8, 9 There is no history of skin involvement in this patient, however, an entity called systemic sclerosis sine scleroderma exists in which there are visceral manifestations of the disease without skin manifestations. Kudoh et. al, recently reported a case of megaduodenum in systemic sclerosis sine scleroderma. 9 While we may not be able to make a specific diagnosis in this case, it is important for the radiologist to recognize the features of megaduodenum and to attempt to differentiate between obstructive and non-obstructive causes. Megaduodenum has a large differential and the management strategies vary from conservative management to invasive sugery depending on the severity and etiology.
Diagnosis At this point the diagnosis is non-obstructive megaduodenum of unspecified etiology. The patient spent 5 days in the hospital and was discharged after she began tolerating PO. Fecal cultures, fecal ova and parasites, and fecal wbc labs were normal. Scheduled follow up appointments with surgery and GI are pending at the time this presentation was written.
References 1. Anderson JR, Earnshaw PM, Fraser GM. Extrinsic compression of the third part of the duodenum. Clinical Radiology 1982; 33: 75 -81. 2. Anderson FH. Megaduodenum: A case report and literature review. American journal of gastroenterology 1974; 62: 509 -515. 3. Hines JR, Gore RM, Balantyne GH. Superior mesenteric artery syndrome: Diagnostic criteria and therapeutic approaches. American journal of surgery 1984; 148: 630 -632. 4. Plesa A, Constantinescu C, Crumpei F, Cotea E. Superior mesenteric artery syndrome: An unusual case of intestinal obstruction. J Gastrointest Liver 2006; 15: 69 -72. 5. Welsch T, Buchler MW, Kienle P. Recalling superior mesenteric artery syndrome. Dig Surg 2007; 24: 149– 1566.
References 6. Applegate GR, Cohen AJ. Dynamic CT in superior mesenteric artery syndrome. J Comput Assist Tomogr 1988; 12: 976 -980. 7. Konen E, Amitai M, Apter S, Garniek A, Gayer G, Nass S, Itzchak Y. CT Angiography of Superior Mesenteric Artery Syndrome. AJR 1998; 171: 1279 -1281. 8. Rohrmann CA, Ricci MT, Krishnamurthy S, Schuffler MD. Radiologic and Histologic Differentiation of Neuromuscular Disorders of the Gastrointestinal Tract: Visceral Myopathies, Visceral Neuropathies, and Progressive Systemic Sclerosis. AJR 1981; 143: 933 -941. 9. Kudoh K, Shibata C, Funayama Y, Fukushima K, Takahashi K, Ogawa H, Sagami Y, Hirabayashi Y, Moriya T, Sasaki I. Gastrojejunostomy and duodenojejunostomy for megaduodenum in systemic sclerosis sine scleroderma: Report of a case. Dig Dis Sci (2007) 52: 2257– 2260.