Radiation Safety in Sentinel Node Biopsy Procedures 200416
Radiation Safety in Sentinel Node Biopsy Procedures 顏若芳 國立台灣大學醫學院附設醫院 核子醫學部 2004/1/6

Clinical Applications Breast ca Aggressive routine resection of draining lymphatic bed ? < 30% axillary node metastasis in T 1, T 2 lesion Melanoma If nodal positive stage III nodal dissection & immunotherapy

Sentinel Lymph Node 1 st node of regional lymphatic basin draining the primary tumor

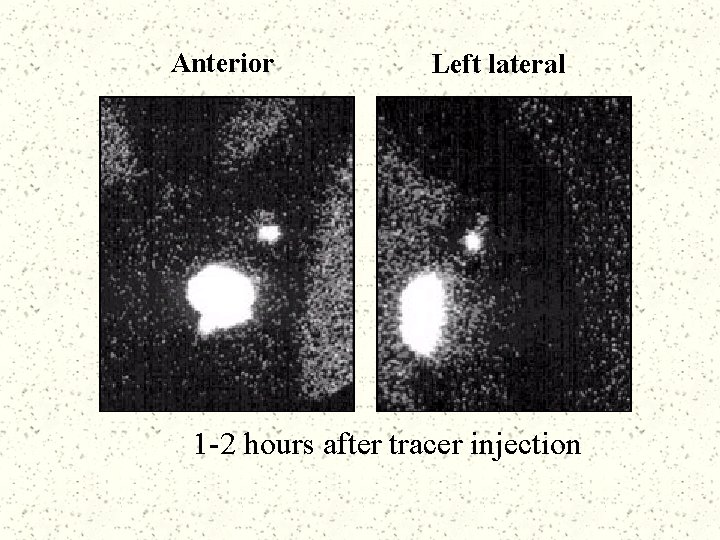
Anterior Left lateral 1 -2 hours after tracer injection

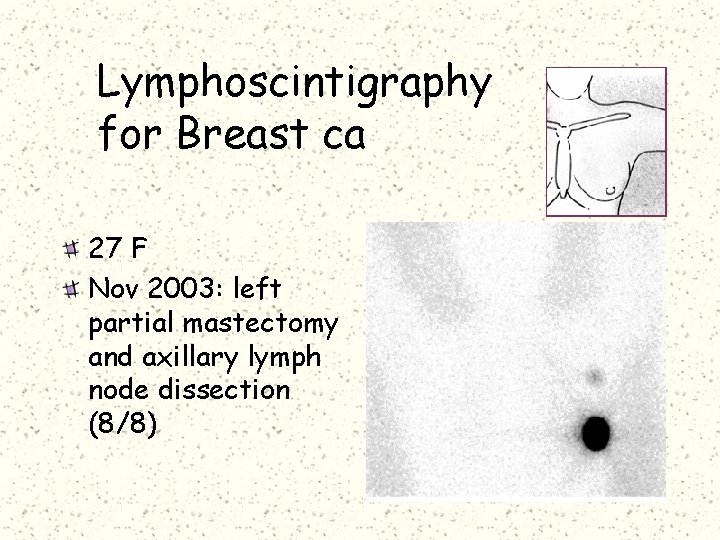
Lymphoscintigraphy for Breast ca 27 F Nov 2003: left partial mastectomy and axillary lymph node dissection (8/8)
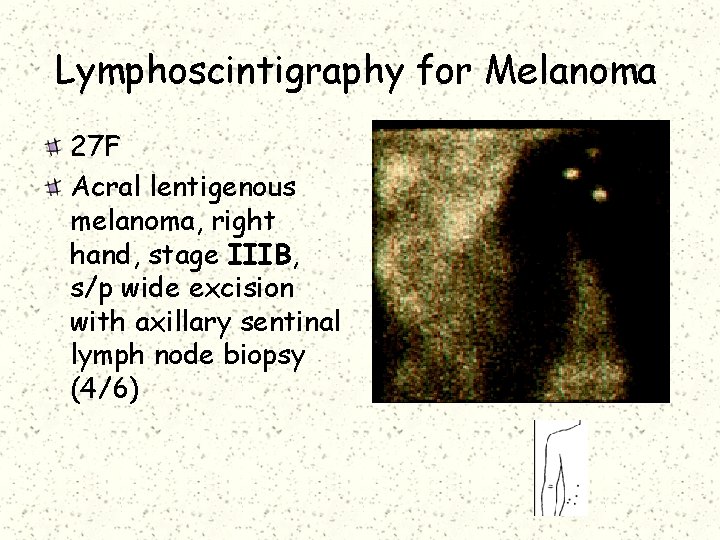
Lymphoscintigraphy for Melanoma 27 F Acral lentigenous melanoma, right hand, stage IIIB, s/p wide excision with axillary sentinal lymph node biopsy (4/6)
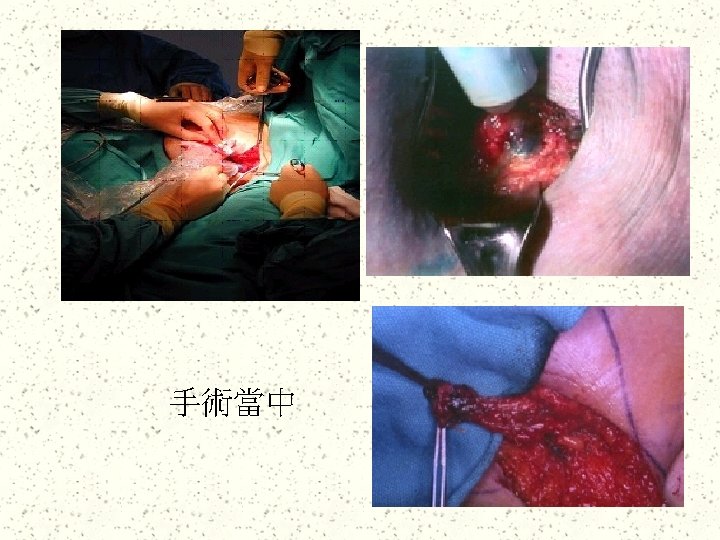
Personnel Involved in SNB Procedure Surgeon / Assistant surgeons Theatre nurse Anesthetist /Assistant anesthetist Pathologist / Pathologist-assistant
Sentinel Lymph Node Biopsy Radiopharmaceutical Tc-99 m filtered sulfur colloid Dose Next-day procedure : 2 m. Ci 16 hours before surgery Same-day procedure : 1 m. Ci 4 hours before surgery
Tracer Distribution 70% tracer activity at administered site at 16 hours Small amount in the sentinel node Almost no radioactivity detectable in blood-contaminated gauze and other garbage No radiation detectable by film batches Jap J Nucl Med 2001; 38: 47 -52
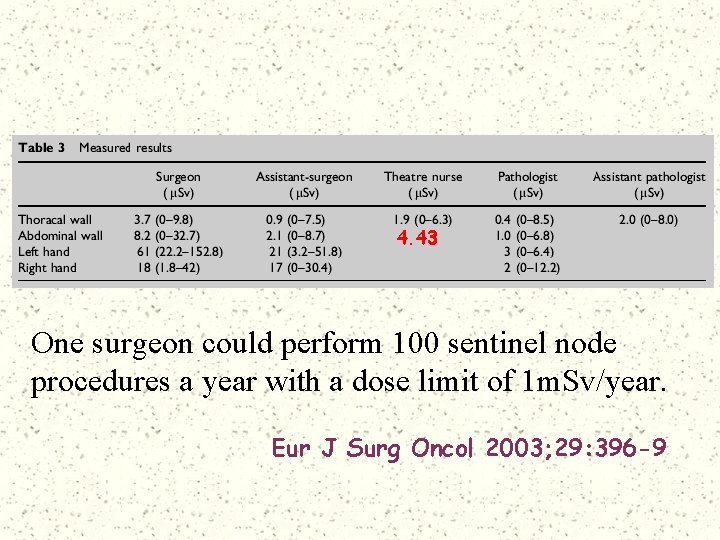
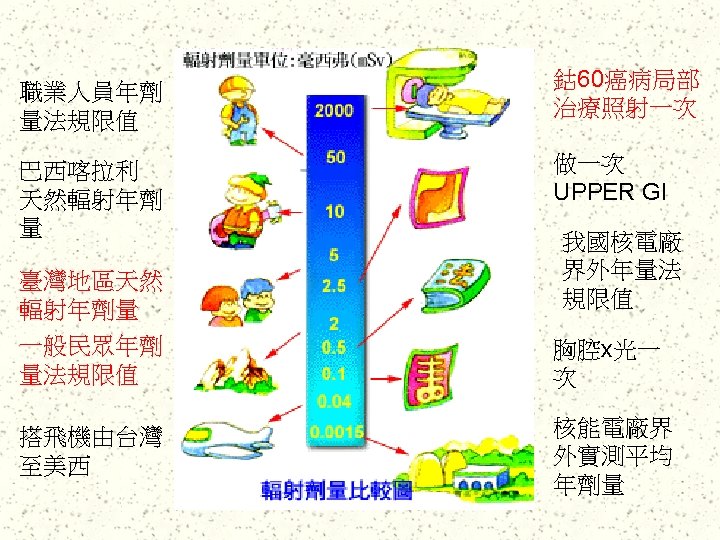
4. 43 One surgeon could perform 100 sentinel node procedures a year with a dose limit of 1 m. Sv/year. Eur J Surg Oncol 2003; 29: 396 -9
Dose at worst 2 Sv per case 30 min air journey Br J Radiol 2003; 76: 117 -122
Staffs who are Pregnant Regulation The equivalent dose to the fetus shall be no more than 1 m. Sv for the remainder of the pregnancy = 1. 3 m. Sv to the surface of abdominal wall 300 cases Minimal risk
SLN in Malignant Melanoma Lower than those in breast cancer surgery Anesthetist & Assistant Anesthetist : < 1 Sv Avoidance of direct contact with the radiopharmaceutical injection sites Dermatol Surg 2003; 29: 141 -145
“Sentinel lymph node biopsy using Tc-99 m represents a safe technique for both operating room personnel and pathology personnel. ”
References: Dermatol Surg 2003; 29: 141 -145 Br J Radiol 2003; 76: 117 -122 Eur J Surg Oncol 2003; 29: 396 -399 Jap J Nucl Med 2001; 38: 47 -52 Am J Surg 1999; 78: 454 -45730
- Slides: 33