Radiation Safety FOR HEALTHCARE PROFESSIONALS Ionizing Radiation Ionizing

- Slides: 14

Radiation Safety FOR HEALTHCARE PROFESSIONALS
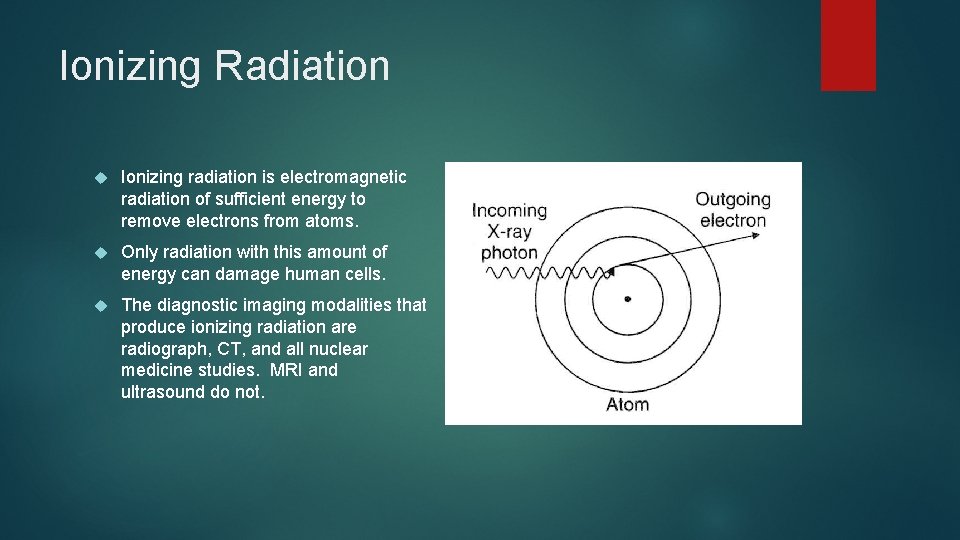
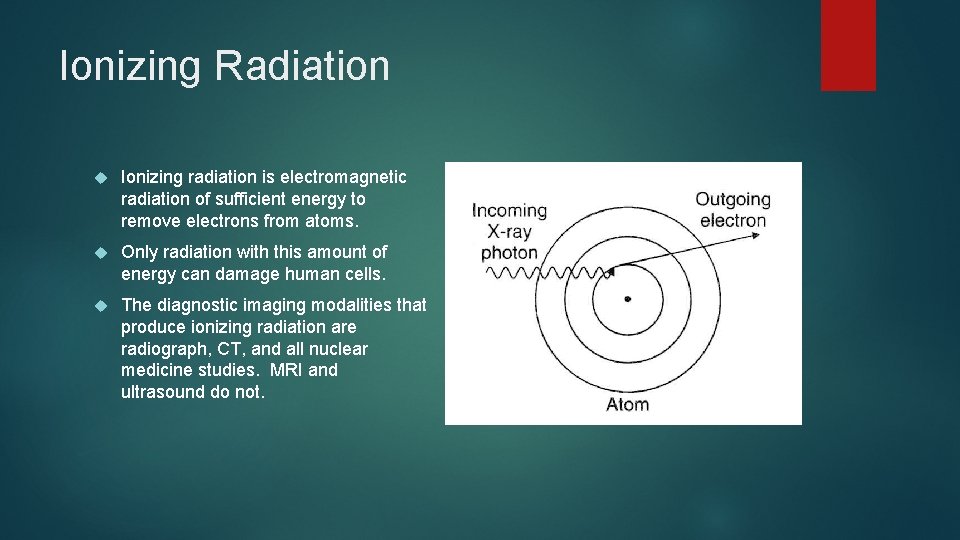
Ionizing Radiation Ionizing radiation is electromagnetic radiation of sufficient energy to remove electrons from atoms. Only radiation with this amount of energy can damage human cells. The diagnostic imaging modalities that produce ionizing radiation are radiograph, CT, and all nuclear medicine studies. MRI and ultrasound do not.
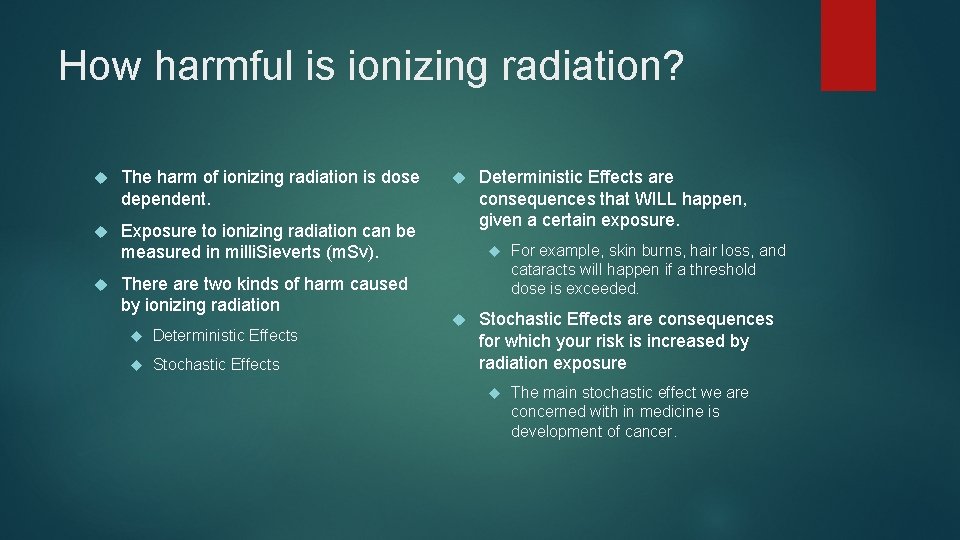
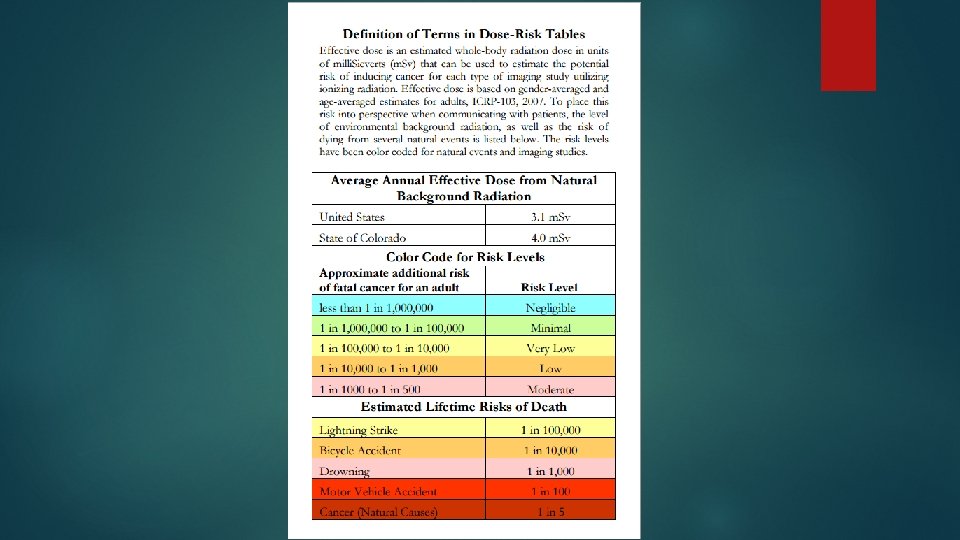
How harmful is ionizing radiation? The harm of ionizing radiation is dose dependent. Exposure to ionizing radiation can be measured in milli. Sieverts (m. Sv). There are two kinds of harm caused by ionizing radiation Deterministic Effects Stochastic Effects Deterministic Effects are consequences that WILL happen, given a certain exposure. For example, skin burns, hair loss, and cataracts will happen if a threshold dose is exceeded. Stochastic Effects are consequences for which your risk is increased by radiation exposure The main stochastic effect we are concerned with in medicine is development of cancer.
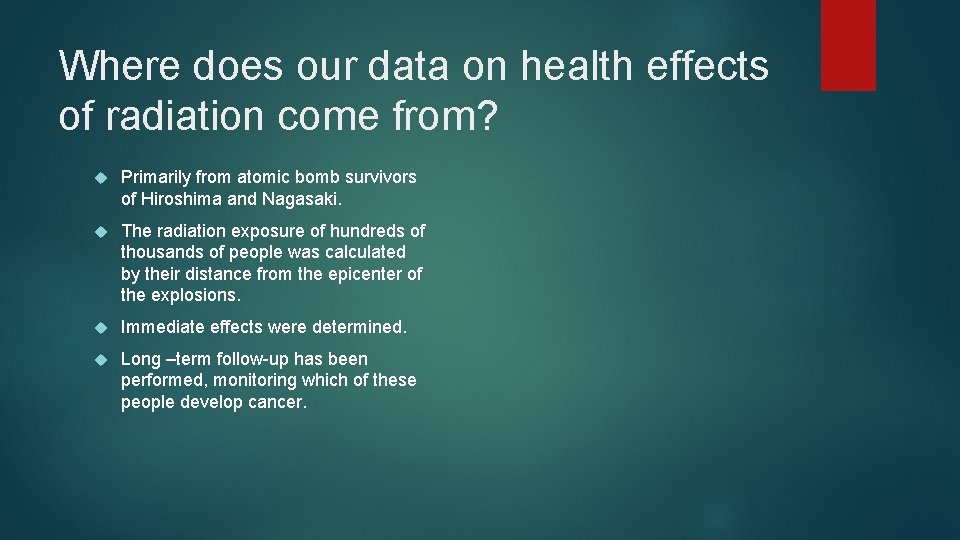
Where does our data on health effects of radiation come from? Primarily from atomic bomb survivors of Hiroshima and Nagasaki. The radiation exposure of hundreds of thousands of people was calculated by their distance from the epicenter of the explosions. Immediate effects were determined. Long –term follow-up has been performed, monitoring which of these people develop cancer.
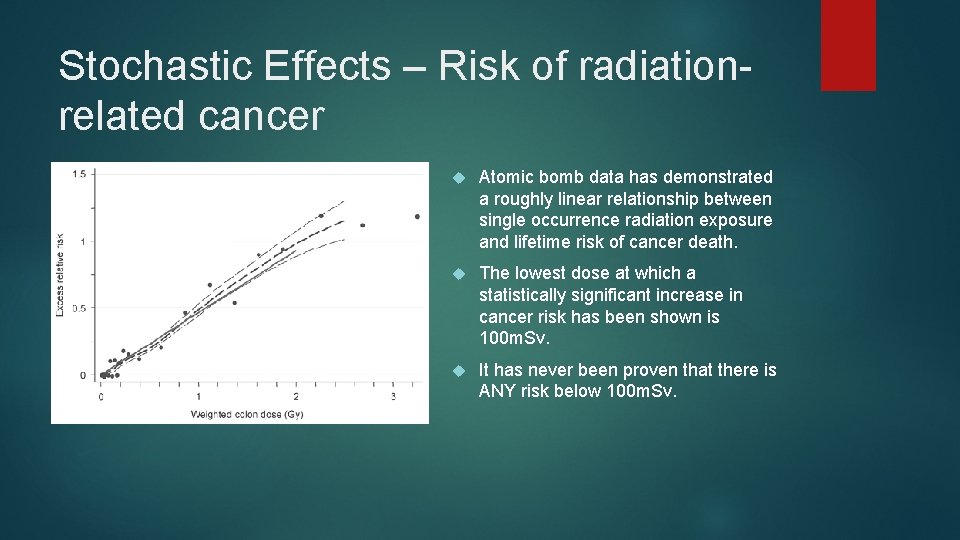
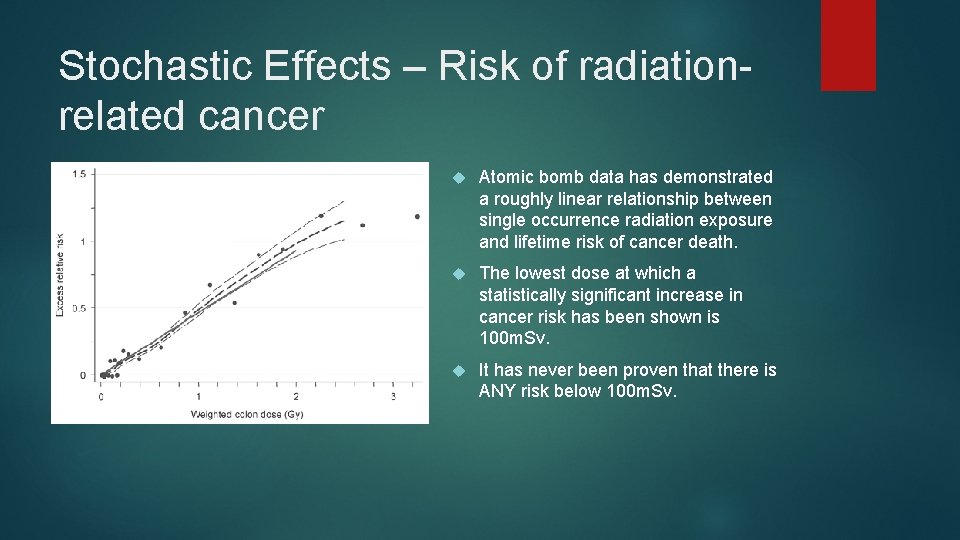
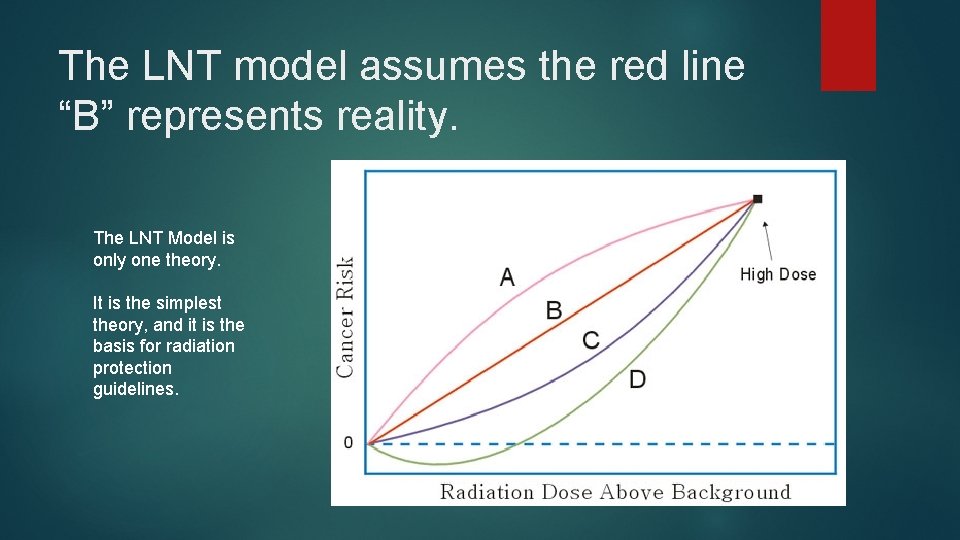
Stochastic Effects – Risk of radiationrelated cancer Atomic bomb data has demonstrated a roughly linear relationship between single occurrence radiation exposure and lifetime risk of cancer death. The lowest dose at which a statistically significant increase in cancer risk has been shown is 100 m. Sv. It has never been proven that there is ANY risk below 100 m. Sv.
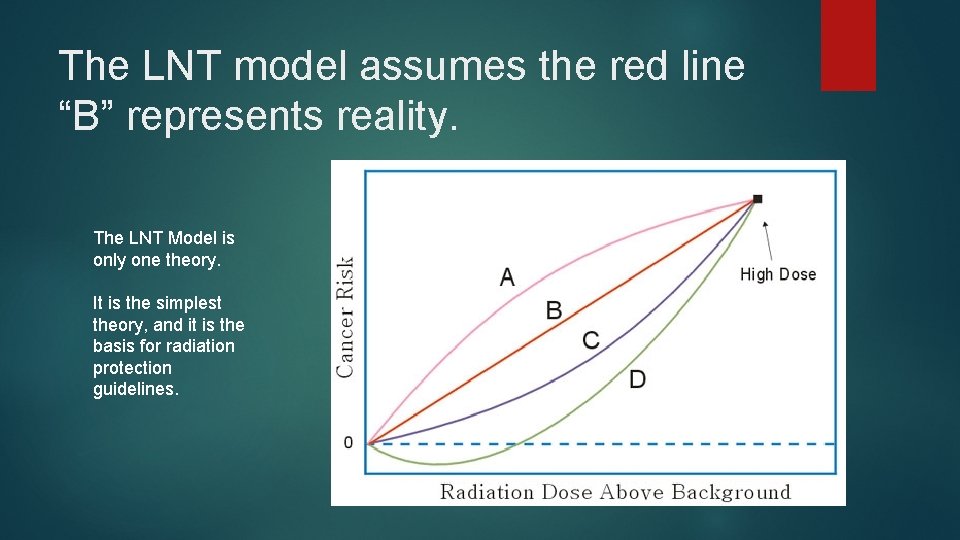
The LNT model assumes the red line “B” represents reality. The LNT Model is only one theory. It is the simplest theory, and it is the basis for radiation protection guidelines.
Age and Radiation Risk For a given radiation dose, the risk of cancer is higher for younger individuals. 1. There are decades of delay between exposure to a carcinogen and development of cancer, and even more delay between development of cancer and death from cancer. 2. Worrying about the radiation dose either to terminally ill patients or to the very old is rarely warranted. DNA is most susceptible to radiation-induced mutation during mitosis/meiosis. The young have more mitotic cells. There is no precise data on the effects of specific radiation doses in the young, particularly fetuses. It is therefore reasonable to simply reduce radiation to these patients as much as possible.
Some Perspective on Low Doses The American Association of physicists in medicine says: Risks of medical imaging at effective doses below 50 m. Sv for single procedures or 100 m. Sv for multiple procedures over short time periods are too low to be detectable and may be nonexistent. Predictions of hypothetical cancer incidence and deaths in patient populations exposed to such low doses are highly speculative and should be discouraged. These predictions are harmful because they lead to sensationalistic articles in the public media that cause some patients and parents to refuse medical imaging procedures, placing them at substantial risk by not receiving the clinical benefits of the prescribed procedures. The Health Physics Society says: In accordance with current knowledge of radiation health risks, the Health Physics Society recommends against quantitative estimation of health risks below an individual dose of 50 m. Sv in one year or a lifetime dose of 100 m. Sv above that received from natural sources. The International Organization for Medical Physics says: Prospective estimates of cancers and cancer deaths induced by medical radiation should include a statement that the estimates are highly speculative because of various random and systematic uncertainties embedded in them.
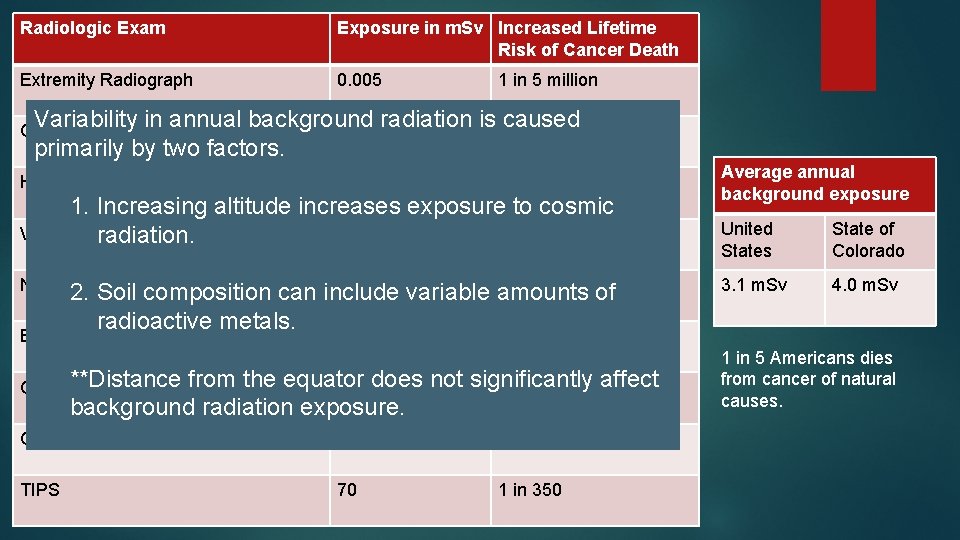
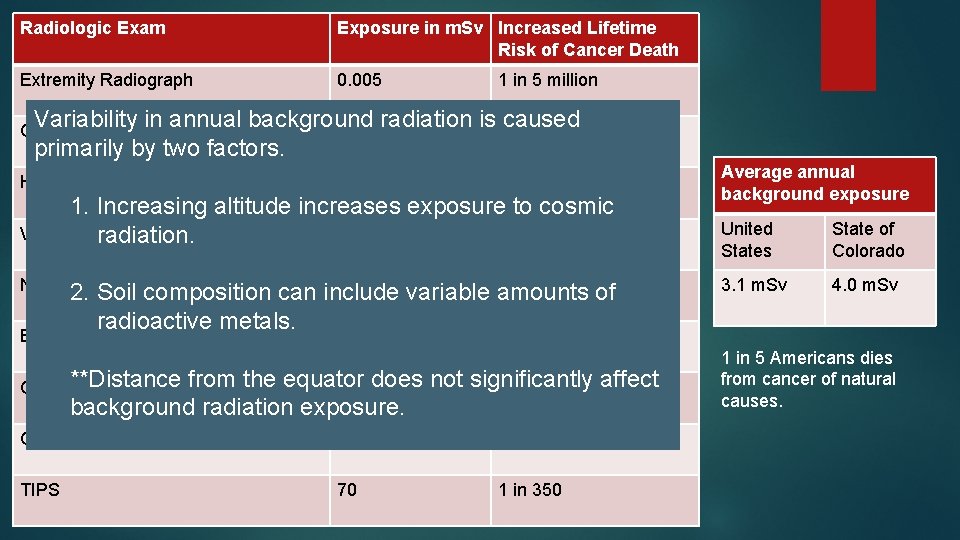
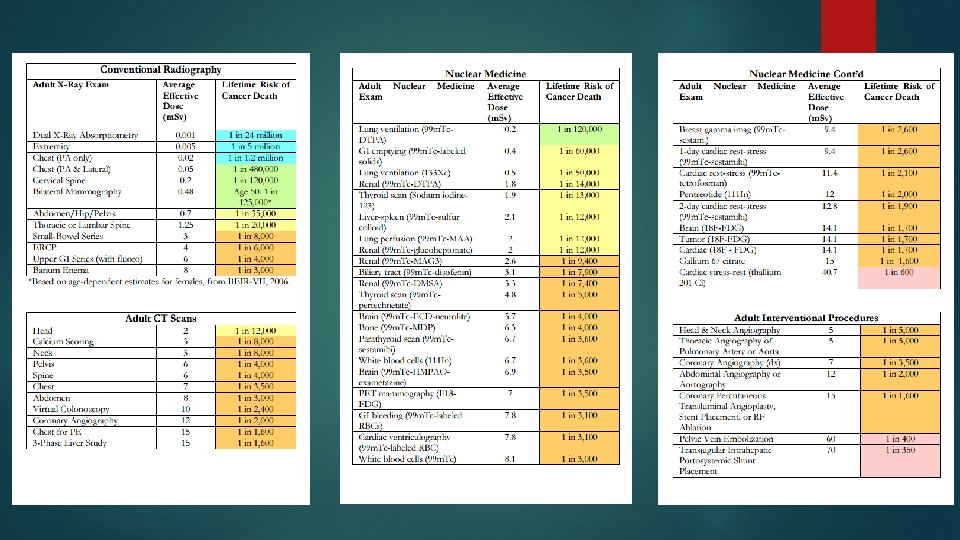
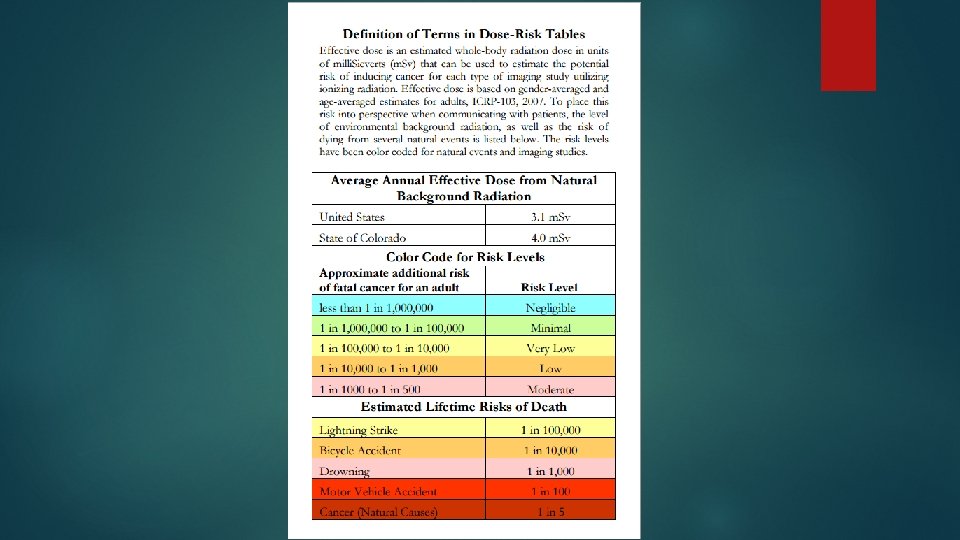
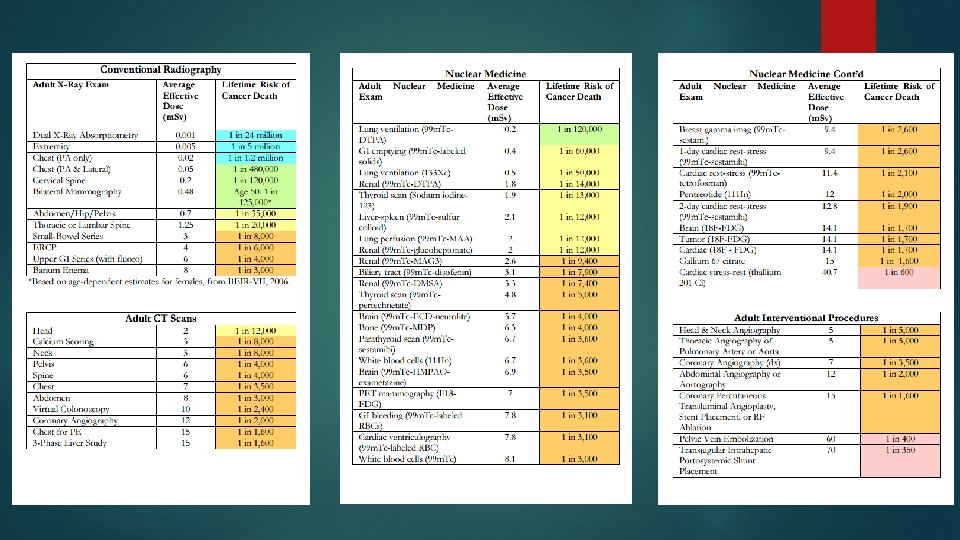
Radiologic Exam Exposure in m. Sv Increased Lifetime Risk of Cancer Death Extremity Radiograph 0. 005 1 in 5 million Variability in annual background radiation is 1 caused 0. 05 in 480, 000 primarily by two factors. Chest Radiograph (Two View) Head CT 2 1 in 12, 000 1. Increasing altitude increases exposure to cosmic V/Q Scanradiation. 2. 2 1 in 11, 000 Neck CT 3 1 in 8, 000 2. Soil composition can include variable amounts of radioactive metals. Barium Enema 8 Average annual background exposure United States State of Colorado 3. 1 m. Sv 4. 0 m. Sv 1 in 3, 000 CT PE**Distance from the equator 15 does not significantly 1 in 1, 600 affect background radiation exposure. Cardiac Stress Test with Thallium 40. 7 1 in 600 TIPS 70 1 in 350 1 in 5 Americans dies from cancer of natural causes.
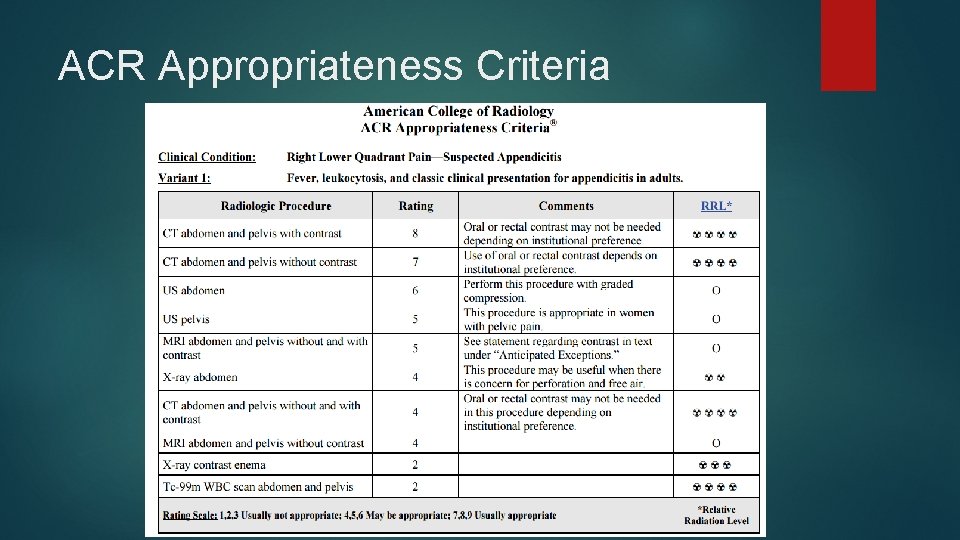
Tips for appropriate use of radiologic testing. When deciding on an appropriate exam… 1. Order the exam that will answer the clinical question. Don’t waste time, expense, and radiation exposure on suboptimal exams. Not answering the clinical question will delay diagnosis, and often will actually increase total patient dose. 2. Perform only essential tests. 3. When appropriate, use alternative imaging, such as ultrasound or MRI. 4. Consult with a radiologist. 5. Consult the ACR appropriateness criteria.
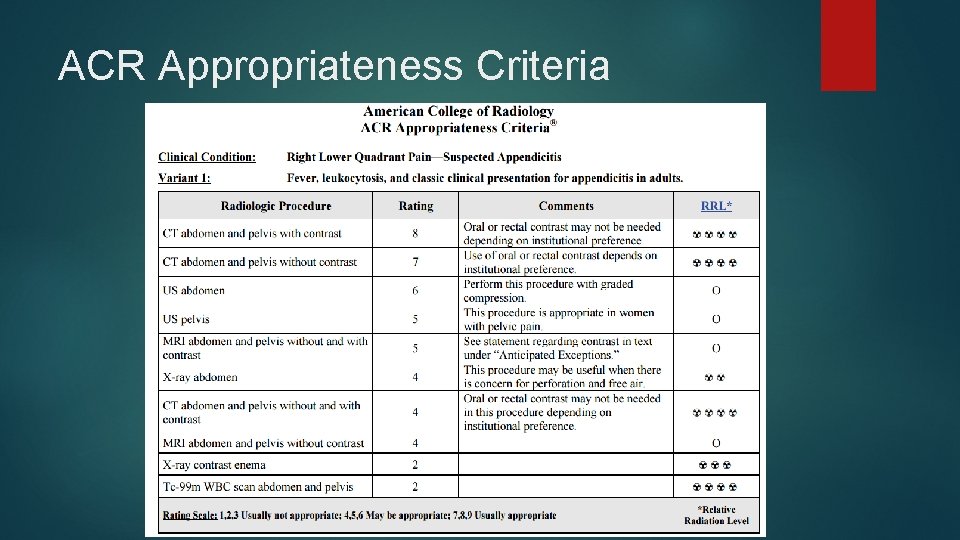
ACR Appropriateness Criteria