QUICK ASSESSMENT OF INTRAABDOMINAL PRESSURE FOR BETTER DECISION
QUICK ASSESSMENT OF INTRA-ABDOMINAL PRESSURE FOR BETTER DECISION MAKING IN CASES OF ACUTE ABDOMEN IN RURAL SETUP Dr Sankalp Dwivedi Professor surgical discipline and Dean Academic Affairs MMIMSR, Maharishi Markandeshwar University Mullana, Ambala, India
INTRODUCTION § Intra-abdominal hypertension (IAH) is the steady-state pressure concealed within the abdominal cavity § Early recognition of IAH is of extreme importance to complications prevent devastating
§ In cases of critically ill adults, the IAP is around 5 -7 mm. Hg § In IAH cases, the IAP becomes greater than 12 mm Hg § In cases of Abdominal compartment syndrome (ACS) the IAP is usually ≥ 20 mm Hg With dysfunction of at least one thoraco-abdominal organ
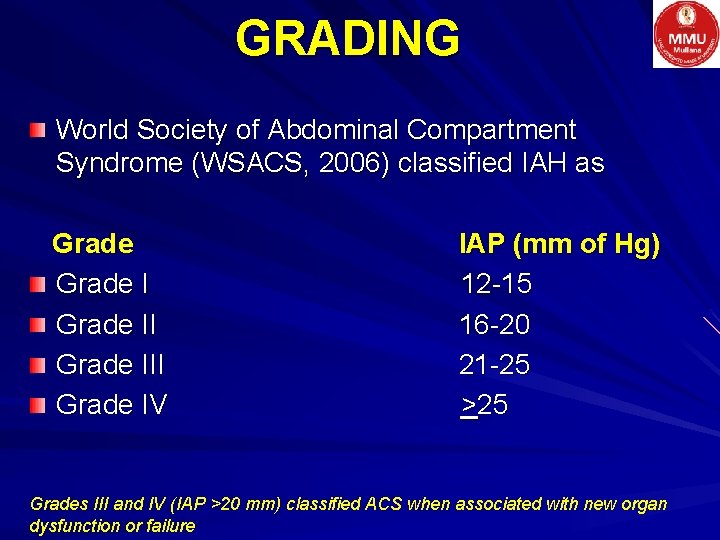
GRADING World Society of Abdominal Compartment Syndrome (WSACS, 2006) classified IAH as Grade III Grade IV IAP (mm of Hg) 12 -15 16 -20 21 -25 >25 Grades III and IV (IAP >20 mm) classified ACS when associated with new organ dysfunction or failure
Options available for IAP measurement
DIRECT MEASUREMENT § Intraperitoneal catheter inserted for ascites drainage peritoneal dialysis § Intraperitoneal pressure transducer § During laparoscopic surgery
INDIRECT MEASUREMENT § Intra-vesical pressure § Intra-gastric pressure § Inferior vena cava § Airway pressure measurements § Rectal pressure § Intra-uterine pressure
WHAT WE PREFERRED ? ? ? Intra-vesical pressure (IVP) monitoring through Foley's manometer
Why IVP? ? ? Validated and widely accepted for clinical use Feasible at ICU and normal ward for quick assessment Compliant Bladder wall functions as passive reservoir and transducer of IAP IVP measurements may not accurately reflect intra-abdominal pressure in neurogenic bladder, abdominal packing or adhesions
OBJECTIVES OF STUDY To measure intra abdominal pressure via IVP monitoring in acute surgical abdomen for early pick up of IAH/ACS
METHODOLOGY A Prospective Study planned after ethical clearance 30 patients of acute surgical abdomen who were suspected IAH/ACS selected randomly
INCLUSION CRITERIA All admitted patients of acute abdomen with suspected IAH/ACS due to § Perforation peritonitis § Acute intestinal obstruction § Acute Pancreatitis § Abdominal sepsis/ Septic Shock § Blunt trauma abdomen
EXCLUSION CRITERIA § Patients in whom Foley’s Catheter cannot be introduced § Diagnosed patients of non surgical Acute abdomen § Acute renal failure § Chronic renal failure § Abdominal packing or adhesions
KEY PARAMETERS § Intra-Vesical Pressure (IVP) § Abdominal perfusion pressure (APP) § CT Scan criteria
IVP § Foley Manometer method § The measuring tube inserted between the catheter and the collecting bag § The tube elevated with the base at the symphysis pubis § Maximum bladder instillation- 20 -25 m. L of sterile saline § The IAP/IVP § Expressed in millimeters of mercury (mm Hg) § Measured at end-expiration in the complete supine position § After ensuring that abdominal muscle contractions are absent § And that the transducer zeroed at the level of the mid-axillary line
APP = MAP – IAP More accurate predictor of visceral perfusion A potential endpoint for resuscitation
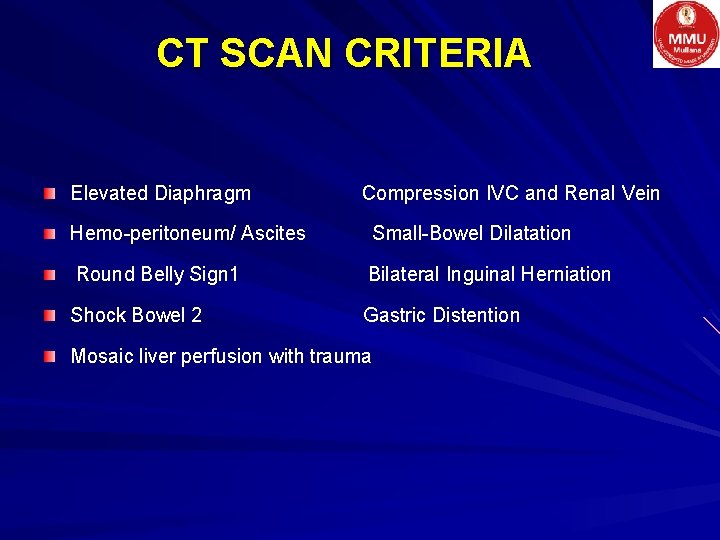
CT SCAN CRITERIA Elevated Diaphragm Compression IVC and Renal Vein Hemo-peritoneum/ Ascites Small-Bowel Dilatation Round Belly Sign 1 Bilateral Inguinal Herniation Shock Bowel 2 Gastric Distention Mosaic liver perfusion with trauma

OBSERVATION
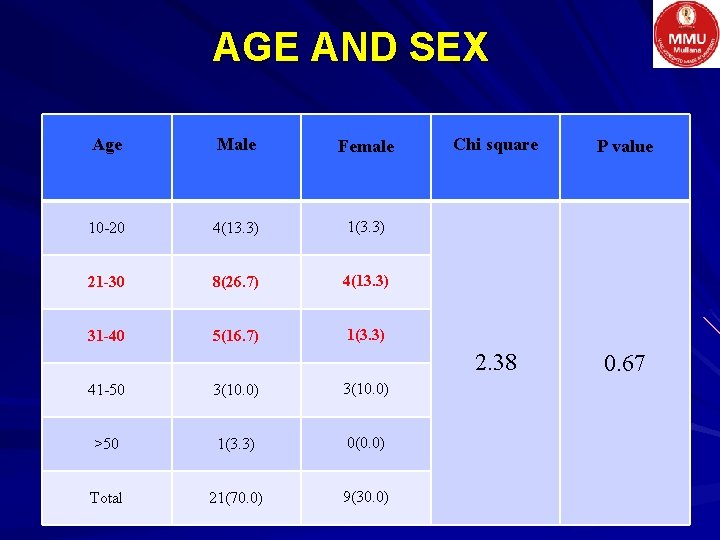
AGE AND SEX Age Male Female 10 -20 4(13. 3) 1(3. 3) 21 -30 8(26. 7) 4(13. 3) 31 -40 5(16. 7) 1(3. 3) 41 -50 3(10. 0) >50 1(3. 3) 0(0. 0) Total 21(70. 0) 9(30. 0) Chi square P value 2. 38 0. 67
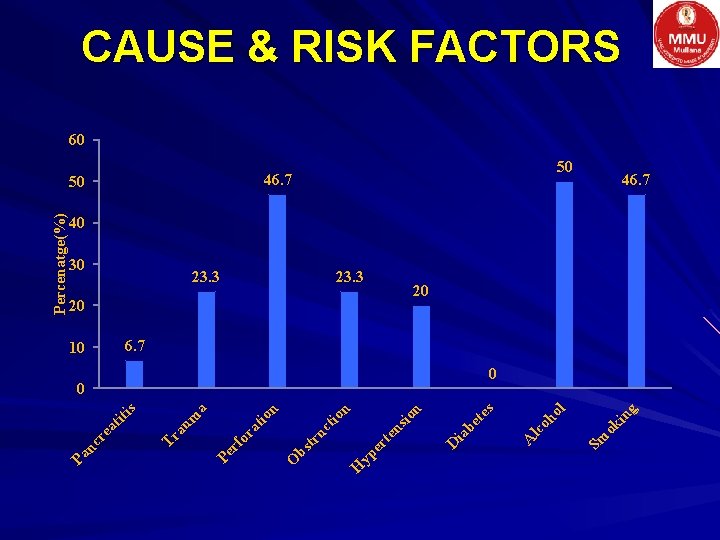
g in 46. 7 Sm ok oh ol lc 0 A s te be 20 ia 23. 3 D n sio en rt yp e n 23. 3 H tio uc tr bs 50 O n tio rf or a Percenatge(%) 30 Pe m a au 10 Tr is ea tit nc r Pa CAUSE & RISK FACTORS 60 50 46. 7 40 20 6. 7 0
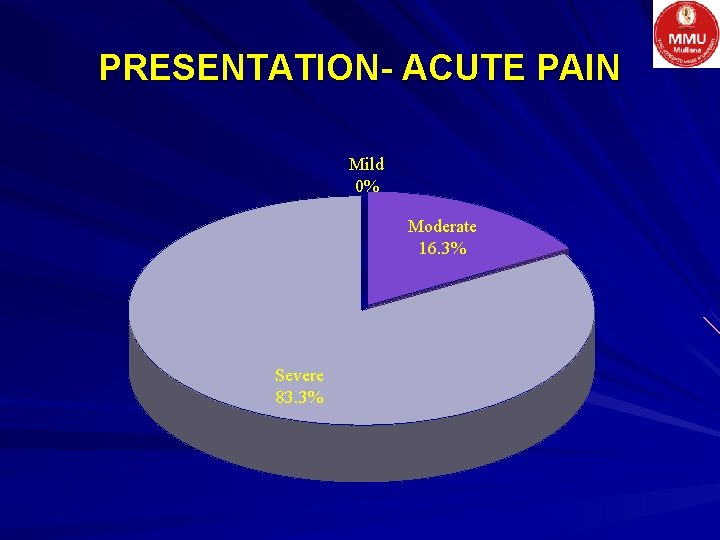
PRESENTATION- ACUTE PAIN Mild 0% Moderate 16. 3% Severe 83. 3%
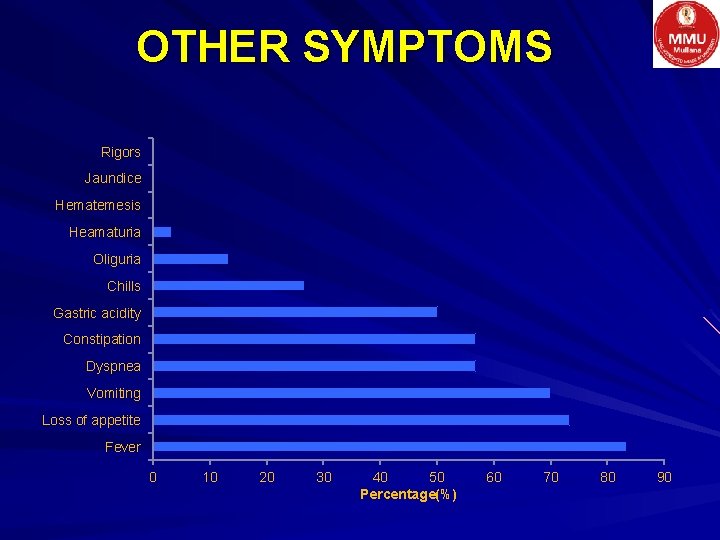
OTHER SYMPTOMS Rigors Jaundice Hematemesis Heamaturia Oliguria Chills Gastric acidity Constipation Dyspnea Vomiting Loss of appetite Fever 0 10 20 30 40 50 Percentage(%) 60 70 80 90
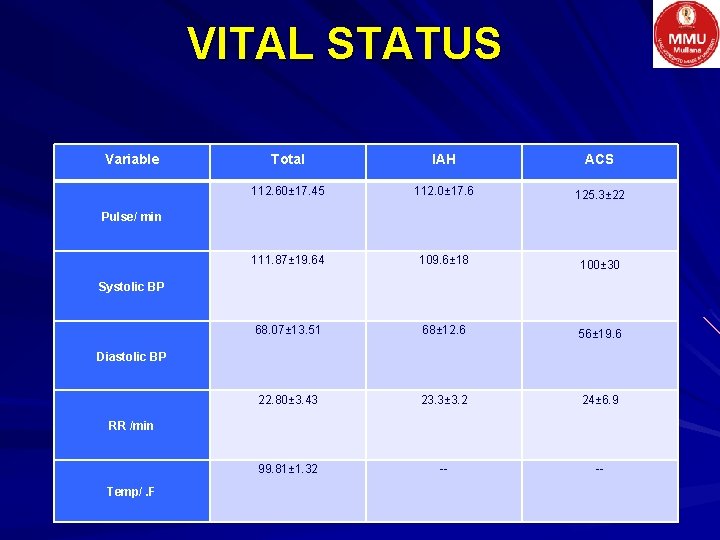
VITAL STATUS Variable Pulse/ min Systolic BP Diastolic BP RR /min Temp/. F Total IAH ACS 112. 60± 17. 45 112. 0± 17. 6 125. 3± 22 111. 87± 19. 64 109. 6± 18 68. 07± 13. 51 68± 12. 6 22. 80± 3. 43 23. 3± 3. 2 24± 6. 9 99. 81± 1. 32 -- -- 100± 30 56± 19. 6
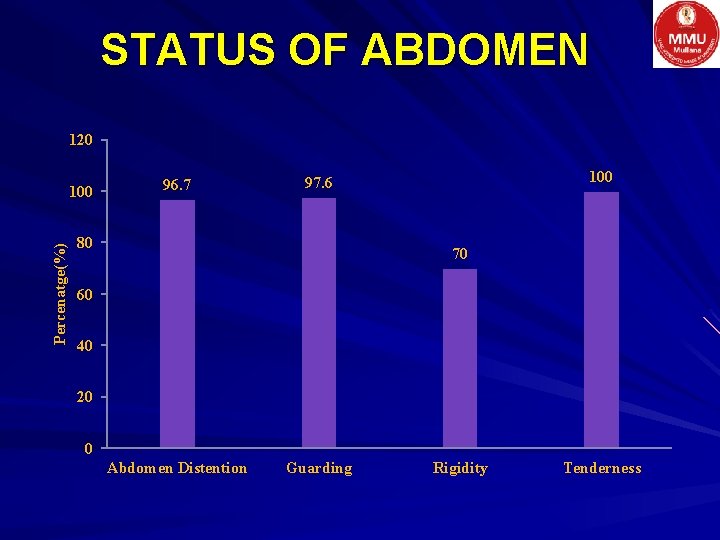
STATUS OF ABDOMEN 120 Percenatge(%) 100 96. 7 100 97. 6 80 70 60 40 20 0 Abdomen Distention Guarding Rigidity Tenderness
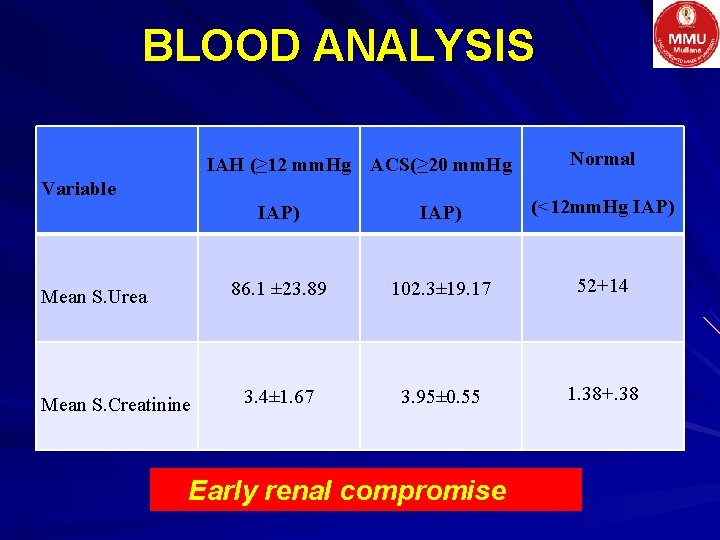
BLOOD ANALYSIS IAH (≥ 12 mm. Hg ACS(≥ 20 mm. Hg Variable Mean S. Urea Mean S. Creatinine Normal IAP) (<12 mm. Hg IAP) 86. 1 ± 23. 89 102. 3± 19. 17 52+14 3. 4± 1. 67 3. 95± 0. 55 1. 38+. 38 Early renal compromise
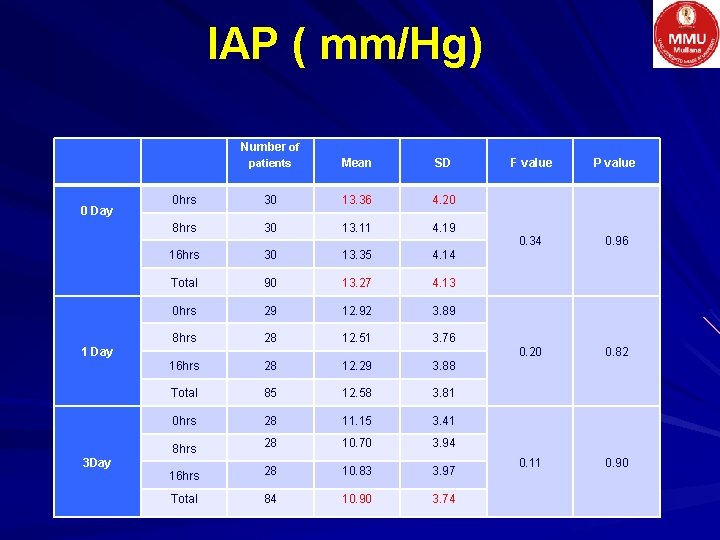
IAP ( mm/Hg) Number of 0 Day patients Mean SD 0 hrs 30 13. 36 4. 20 8 hrs 30 13. 11 4. 19 16 hrs 30 13. 35 4. 14 Total 90 13. 27 4. 13 0 hrs 29 12. 92 3. 89 8 hrs 28 12. 51 3. 76 16 hrs 28 12. 29 3. 88 Total 85 12. 58 3. 81 0 hrs 28 11. 15 3. 41 8 hrs 28 10. 70 3. 94 16 hrs 28 10. 83 3. 97 Total 84 10. 90 3. 74 1 Day 3 Day F value P value 0. 34 0. 96 0. 20 0. 82 0. 11 0. 90
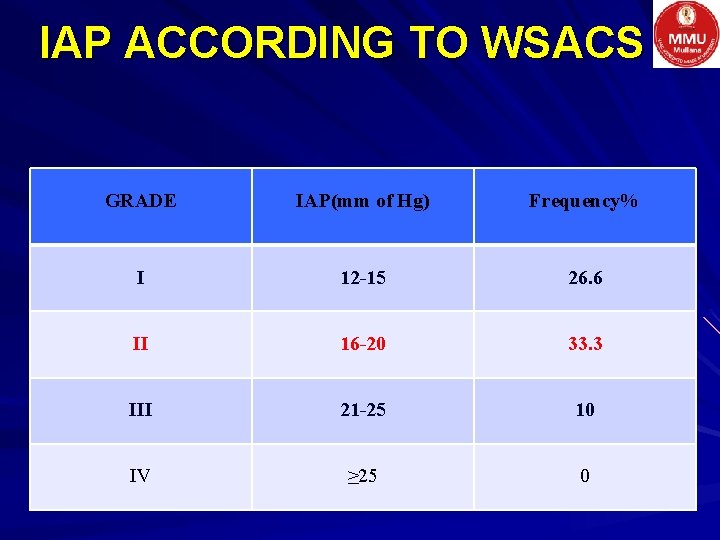
IAP ACCORDING TO WSACS GRADE IAP(mm of Hg) Frequency% I 12 -15 26. 6 II 16 -20 33. 3 III 21 -25 10 IV ≥ 25 0
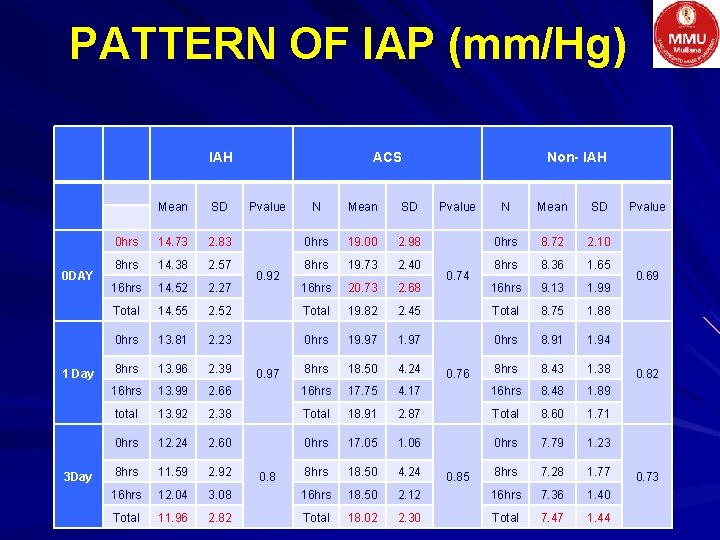
PATTERN OF IAP (mm/Hg) IAH 0 DAY 1 Day 3 Day Mean SD 0 hrs 14. 73 2. 83 8 hrs 14. 38 2. 57 16 hrs 14. 52 2. 27 Total 14. 55 0 hrs ACS Pvalue N Mean SD 0 hrs 19. 00 2. 98 8 hrs 19. 73 2. 40 16 hrs 20. 73 2. 68 2. 52 Total 19. 82 13. 81 2. 23 0 hrs 8 hrs 13. 96 2. 39 16 hrs 13. 99 total Non- IAH N Mean SD 0 hrs 8. 72 2. 10 8 hrs 8. 36 1. 65 16 hrs 9. 13 1. 99 2. 45 Total 8. 75 1. 88 19. 97 1. 97 0 hrs 8. 91 1. 94 8 hrs 18. 50 4. 24 8 hrs 8. 43 1. 38 2. 66 16 hrs 17. 75 4. 17 16 hrs 8. 48 1. 89 13. 92 2. 38 Total 18. 91 2. 87 Total 8. 60 1. 71 0 hrs 12. 24 2. 60 0 hrs 17. 05 1. 06 0 hrs 7. 79 1. 23 8 hrs 11. 59 2. 92 8 hrs 18. 50 4. 24 8 hrs 7. 28 1. 77 16 hrs 12. 04 3. 08 16 hrs 18. 50 2. 12 16 hrs 7. 36 1. 40 Total 11. 96 2. 82 Total 18. 02 2. 30 Total 7. 47 1. 44 0. 92 0. 97 0. 8 Pvalue 0. 74 0. 76 0. 85 Pvalue 0. 69 0. 82 0. 73
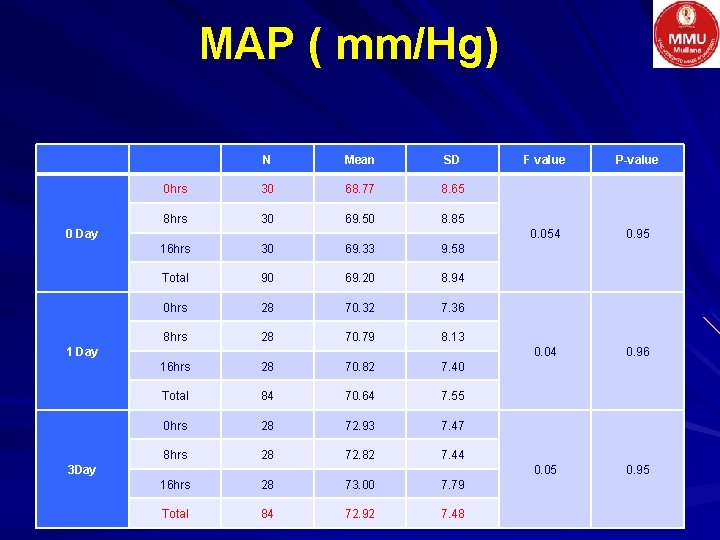
MAP ( mm/Hg) N Mean SD 0 hrs 30 68. 77 8. 65 8 hrs 30 69. 50 8. 85 0 Day 16 hrs 30 69. 33 9. 58 Total 90 69. 20 8. 94 0 hrs 28 70. 32 7. 36 8 hrs 28 70. 79 8. 13 1 Day 16 hrs 28 70. 82 7. 40 Total 84 70. 64 7. 55 0 hrs 28 72. 93 7. 47 8 hrs 28 72. 82 7. 44 3 Day 16 hrs 28 73. 00 7. 79 Total 84 72. 92 7. 48 F value P-value 0. 054 0. 95 0. 04 0. 96 0. 05 0. 95
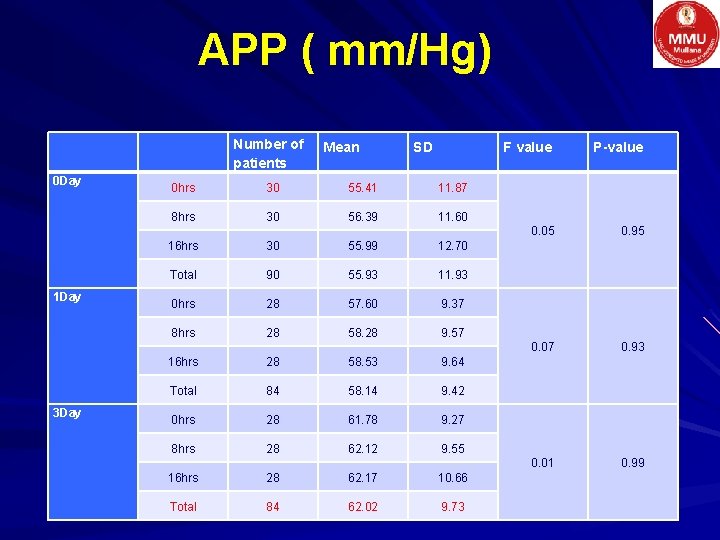
APP ( mm/Hg) 0 Day 1 Day 3 Day Number of patients 0 hrs 30 55. 41 11. 87 8 hrs 30 56. 39 11. 60 Mean SD 16 hrs 30 55. 99 12. 70 Total 90 55. 93 11. 93 0 hrs 28 57. 60 9. 37 8 hrs 28 58. 28 9. 57 16 hrs 28 58. 53 9. 64 Total 84 58. 14 9. 42 0 hrs 28 61. 78 9. 27 8 hrs 28 62. 12 9. 55 16 hrs 28 62. 17 10. 66 Total 84 62. 02 9. 73 F value P-value 0. 05 0. 95 0. 07 0. 93 0. 01 0. 99
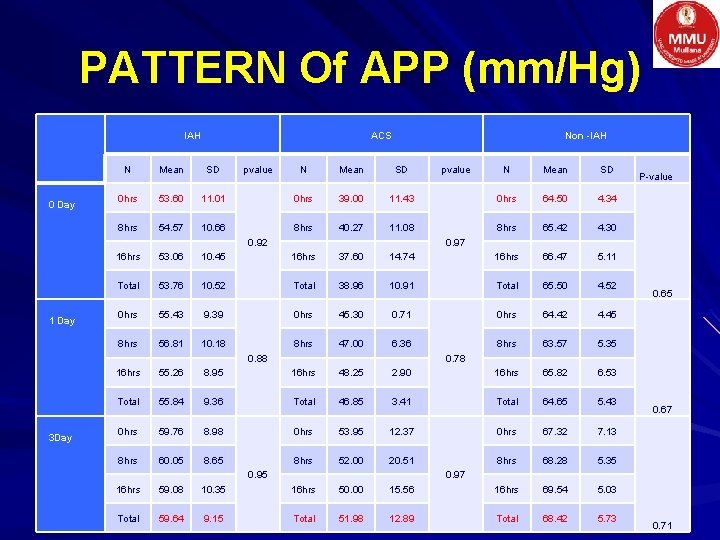
PATTERN Of APP (mm/Hg) IAH 0 Day ACS N Mean SD 0 hrs 53. 60 8 hrs 54. 57 pvalue Non -IAH N Mean SD 11. 01 0 hrs 39. 00 10. 66 8 hrs 40. 27 N Mean SD 11. 43 0 hrs 64. 50 4. 34 11. 08 8 hrs 65. 42 4. 30 0. 92 1 Day 3 Day pvalue P-value 0. 97 16 hrs 53. 06 10. 45 16 hrs 37. 60 14. 74 16 hrs 66. 47 5. 11 Total 53. 76 10. 52 Total 38. 96 10. 91 Total 65. 50 4. 52 0 hrs 55. 43 9. 39 0 hrs 45. 30 0. 71 0 hrs 64. 42 4. 45 8 hrs 56. 81 10. 18 8 hrs 47. 00 6. 36 8 hrs 63. 57 5. 35 0. 88 0. 65 0. 78 16 hrs 55. 26 8. 95 16 hrs 48. 25 2. 90 16 hrs 65. 82 6. 53 Total 55. 84 9. 36 Total 46. 85 3. 41 Total 64. 65 5. 43 0 hrs 59. 76 8. 98 0 hrs 53. 95 12. 37 0 hrs 67. 32 7. 13 8 hrs 60. 05 8. 65 8 hrs 52. 00 20. 51 8 hrs 68. 28 5. 35 0. 95 0. 67 0. 97 16 hrs 59. 08 10. 35 16 hrs 50. 00 15. 56 16 hrs 69. 54 5. 03 Total 59. 64 9. 15 Total 51. 98 12. 89 Total 68. 42 5. 73 0. 71
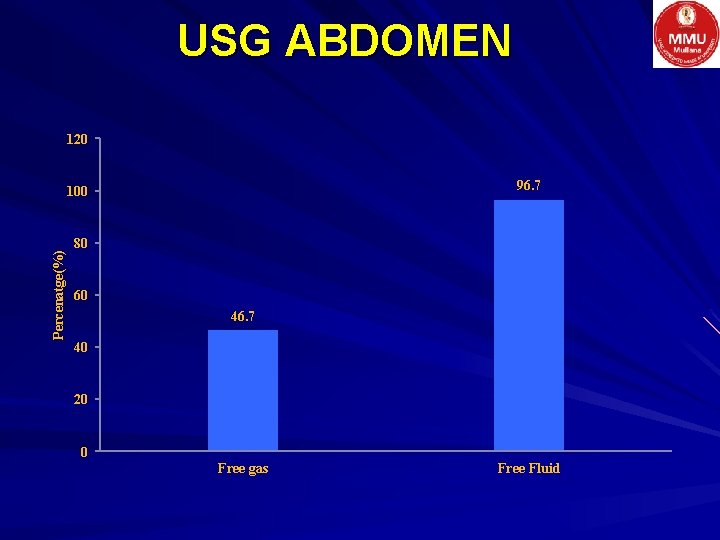
USG ABDOMEN 120 96. 7 Percenatge(%) 100 80 60 46. 7 40 20 0 Free gas Free Fluid
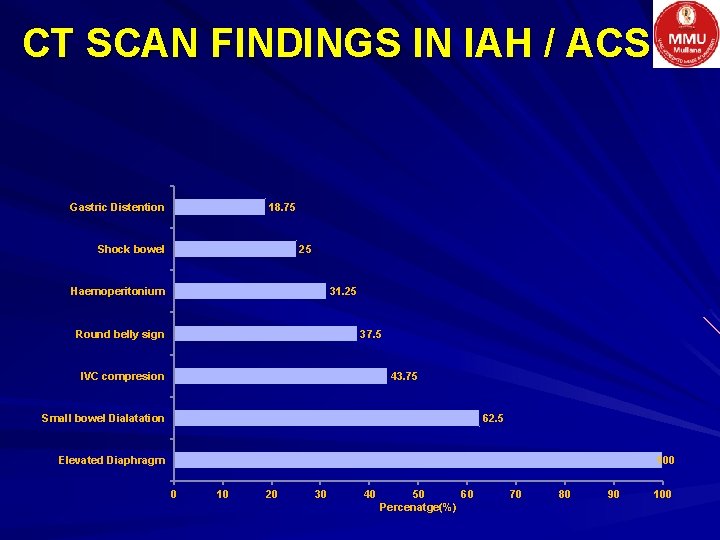
CT SCAN FINDINGS IN IAH / ACS Gastric Distention 18. 75 Shock bowel 25 Haemoperitonium 31. 25 Round belly sign 37. 5 IVC compresion 43. 75 Small bowel Dialatation 62. 5 100 Elevated Diaphragm 0 10 20 30 40 50 60 Percenatge(%) 70 80 90 100
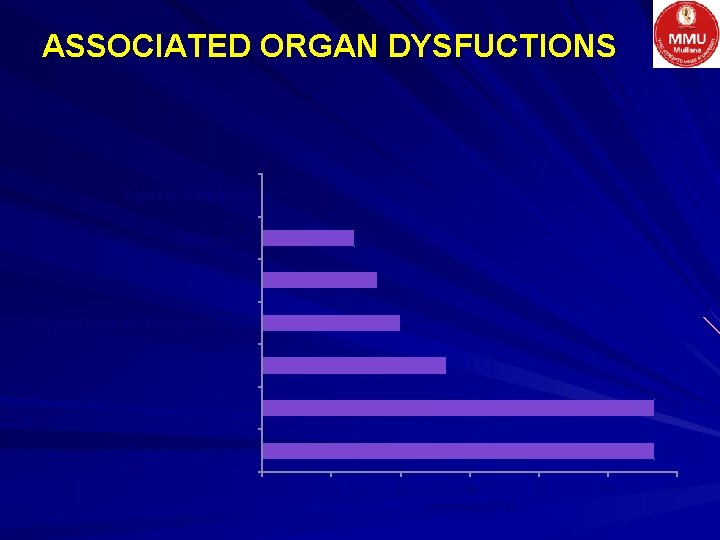
ASSOCIATED ORGAN DYSFUCTIONS Reperfusion syndrome 0 Cardiac arrest 13. 3 Respiratory failure 16. 7 Hypervolumea and Pulmonary Edema 20 Wound Dehesience 26. 7 Renal failure 56. 7 Hypotension & shock 56. 7 0 10 20 30 Percentage(%) 40 50 60
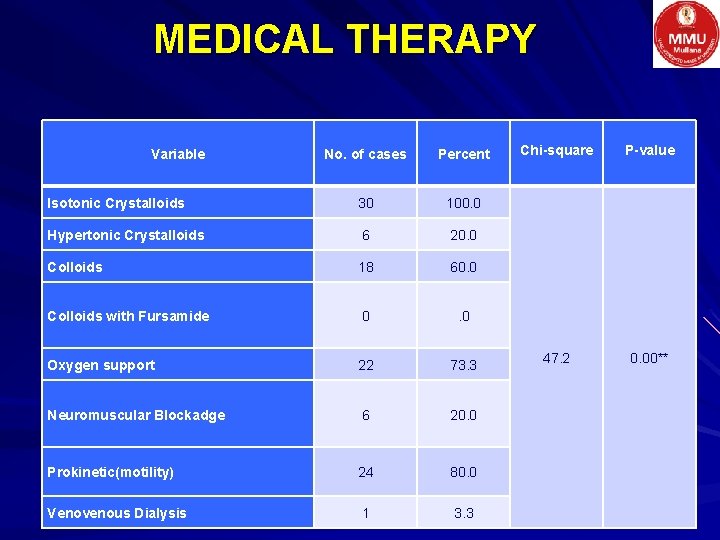
MEDICAL THERAPY Variable No. of cases Percent Isotonic Crystalloids 30 100. 0 Hypertonic Crystalloids 6 20. 0 Colloids 18 60. 0 Colloids with Fursamide 0 . 0 Oxygen support 22 73. 3 Neuromuscular Blockadge 6 20. 0 Prokinetic(motility) 24 80. 0 Venovenous Dialysis 1 3. 3 Chi-square P-value 47. 2 0. 00**
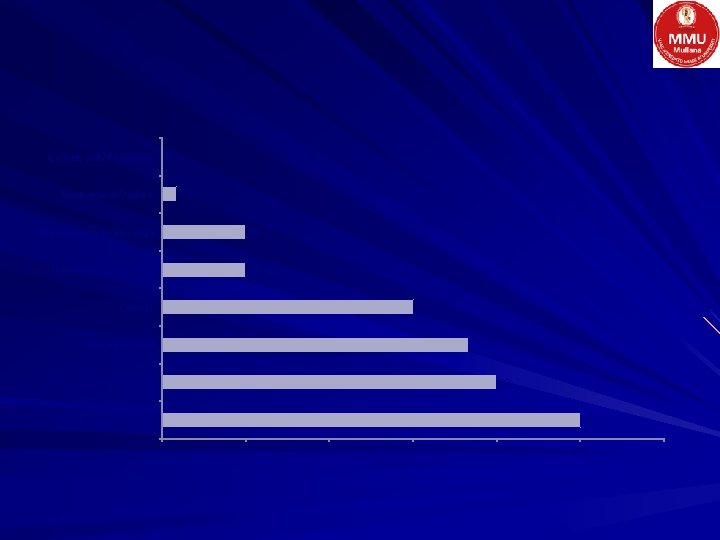
0 Colloids with Frusamide Venovenous Dialysis 3. 3 Neuromuscular Blocadge 20 Hypertonic Crystelloids 20 Colloids 60 Oxygen support 73. 3 Prokinetic 80 Isotonic Crystelloids 100 0 20 40 60 Percentage(%) 80 100 120
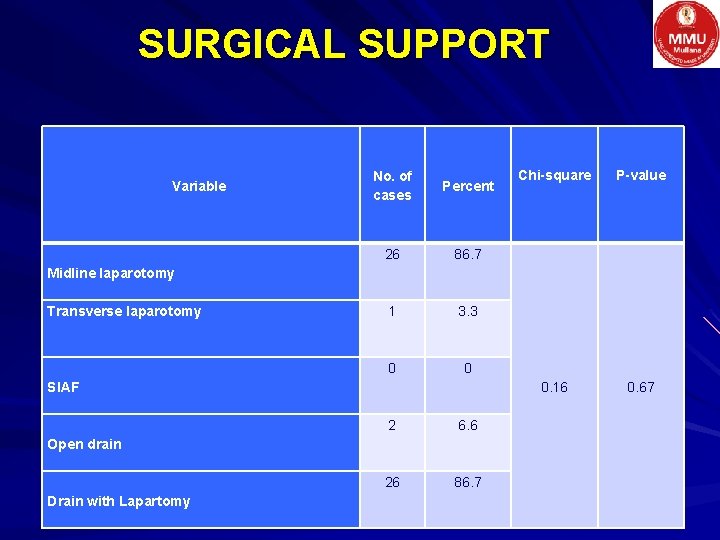
SURGICAL SUPPORT Variable No. of cases Percent 26 86. 7 1 3. 3 0 0 Chi-square P-value 0. 16 0. 67 Midline laparotomy Transverse laparotomy Sl. AF 2 6. 6 26 86. 7 Open drain Drain with Lapartomy
OUTCOME
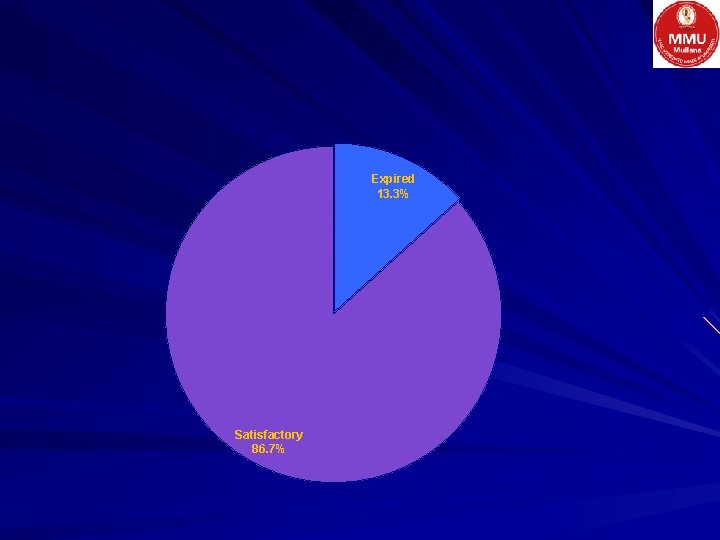
Expired 13. 3% Satisfactory 86. 7%
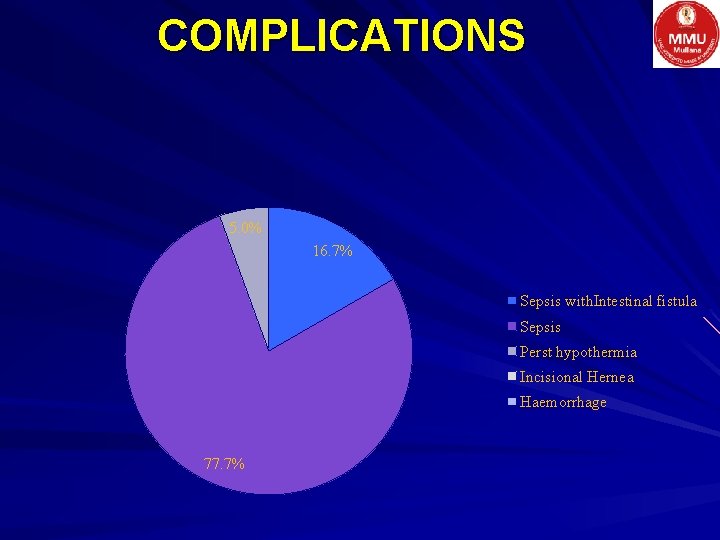
COMPLICATIONS 5. 0% 16. 7% Sepsis with. Intestinal fistula Sepsis Perst hypothermia Incisional Hernea Haemorrhage 77. 7%
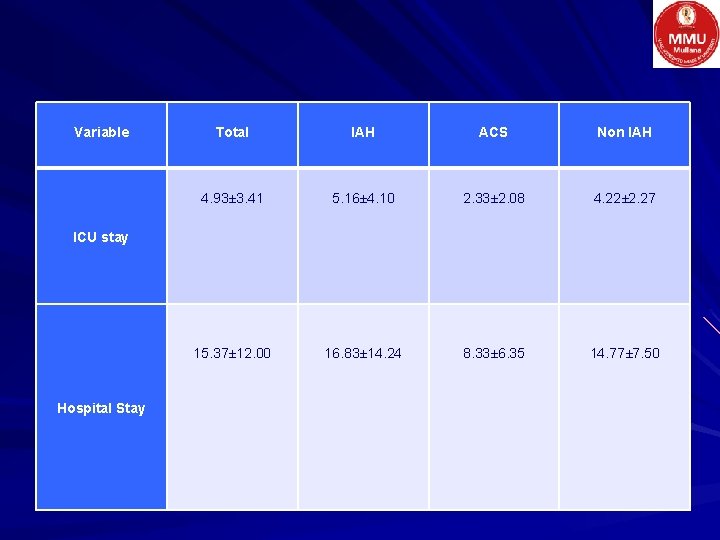
Variable Total IAH ACS Non IAH 4. 93± 3. 41 5. 16± 4. 10 2. 33± 2. 08 4. 22± 2. 27 15. 37± 12. 00 16. 83± 14. 24 8. 33± 6. 35 14. 77± 7. 50 ICU stay Hospital Stay
CONCLUSION Raised IAP is a hidden threat to acute surgical abdomen Majority of IAH/ACS cases are abdominal sepsis due to gut perforation or obstruction Measurement of IAP may be the quick help in such chases to pick up IAH/ACS and treat them appropriately
REFERENCES Manu Malbrain; Abdominal compartment syndrome; F 1000 Medicine Reports 2009, 1: 86 Dariusz Onichimowski 1, 2, Iwona Podlińska 1, Sebastian Sobiech 1, Robert Ropiak 3 Measurement of intra-abdominal pressure in clinical practice; Anaesthesiology Intensive Therapy, 2010, XLII, 2; 96 -101 D. Turnbull 1*, S. Webber 2, C. H. Hamnegard 3 and G. H. Mills 2 Intra-abdominal pressure measurement: validation of intragastric pressure as a measure of intra-abdominal pressure British Journal of Anaesthesia 98 (5): 628– 34 (2007) Jens Otto*1, Daniel Kaemmer 1, Marcel Binnebösel 1, Marc Jansen 1, Rolf Dembinski 2, Volker Schumpelick 1 and Alexander Schachtrupp 1; Direct intra-abdominal pressure monitoring via piezoresistive pressure measurement: a technical note; BMC Surgery 2009, 9: 5 Malbrain ML, Deeren DH. Effect of bladder volume on measured intravesical pressure: a prospective cohort study. Crit Care 2006; 10(4): 98. Zhao-Xi Sun, Hai-Rong Huang, Hong Zhou; Indwelling catheter and conservative measures in the treatment of abdominal compartment syndrome in fulminant acute pancreatitis; World J Gastroenterol 2006 August 21; 12(31) Jens Otto, Daniel Kaemmer, Marcel Binnebösel, Marc Jansen, Rolf Dembinski, Volker Schumpelick and Alexander Schachtrupp Direct intra-abdominal pressure monitoring via piezoresistive pressure measurement: a technical note; BMC Surgery 2009, 9: 5 Jian-cang Hong-chen Kong-han Qiu-ping Current recognition and management of intra-abdominal hypertension and abdominal compartment syndrome among tertiary Chinese intensive care physicians J Zhejiang Univ-Sci B (Biomed & Biotechnol) 2011 12(2): 156 -162 Mentula P, Hienonen P, Kemppainen E, Lippaniemi A. Surgical Decompression for Abdominal Compartment Syndrome in severe acute pancreatitis. Arch Surg 2010; 145(8): 764 -769. Lee RK. Intraabdominal hypertension and abdominal compartment syndrome: a comprehensive review. Crit Care Nurse 2012; 32(1): 19 -32. Kim IB, Prowle J, Baldwin I, Bellomo R. Incidence, risk factors and outcome associations of intra-abdominal hypertension in critically ill patients. Anaesth Int Care 2012; 40: 79 -89. Zhou JC, Zhau HC, Pan KH, Zu QP. Current recognition and management of intra-abdominal hypertension and abdominal compartment syndrome among tertiary Chinese intensive care physicians. J Zhejiang Univ 2011; 12(2): 156 -162. Hill L, Hill B, Miller M, Michell WL. The effect of intra-abdominal hypertension on gastrointestinal function. South Afr J Crit Care 2011; 27(1): 12 -19.

Additional therapy – Brachytherapy or – Photodynamic therapy Described for malignant pleural mesothelioma Could be applied for SFTP Reports of this are rare and Effectiveness is uncertain.
- Slides: 44