Quality Payment Program Overview Kris Shay Health Care


- Slides: 29
Quality Payment Program Overview Kris Shay, Health. Care Data Systems Mona Mathews, MA, PMP, Meta. Star Chris Becker, CPHIMS, CPHIT, Meta. Star October 19, 2018

Lake Superior Quality Innovation Network The Lake Superior Quality Innovation Network (Lake Superior QIN) is comprised of three quality improvement organizations: • • • Stratis Health in Minnesota Meta. Star in Wisconsin MPRO in Michigan 1
Disclaimer Content provided in this presentation is based on the latest information made available by the Centers for Medicare & Medicaid Services (CMS) and is subject to change. CMS policies change, so we encourage you to review specific statutes and regulations that may apply to you for interpretation and updates. 2
Objectives 1. Knowledge on 2018 Merit-Based Incentive Payment System (MIPS) 2. Orthopaedic requirements for MIPS 3. Tips and Tricks for participating successfully in MIPS 3
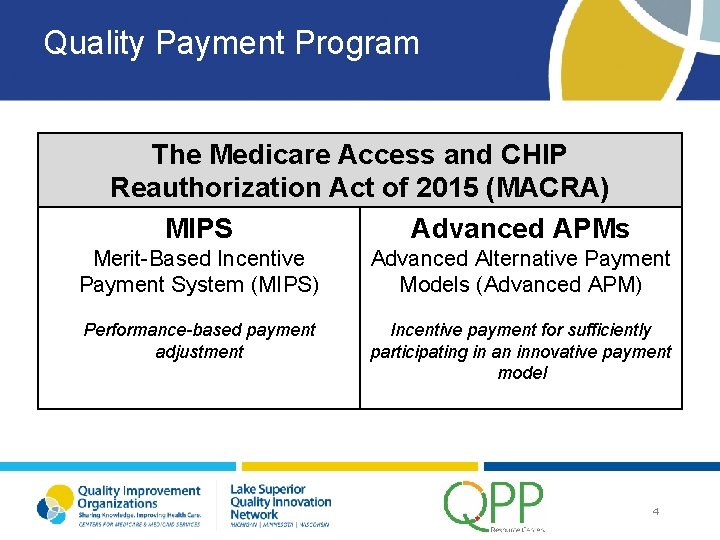
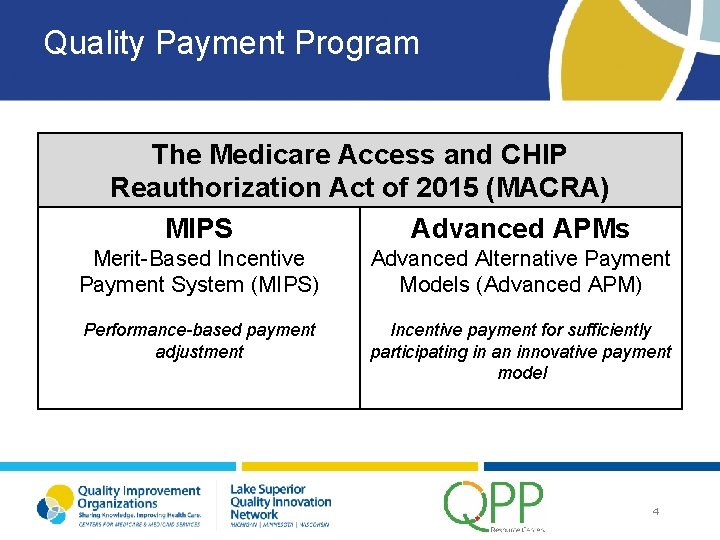
Quality Payment Program The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) MIPS Advanced APMs Merit-Based Incentive Payment System (MIPS) Advanced Alternative Payment Models (Advanced APM) Performance-based payment adjustment Incentive payment for sufficiently participating in an innovative payment model 4
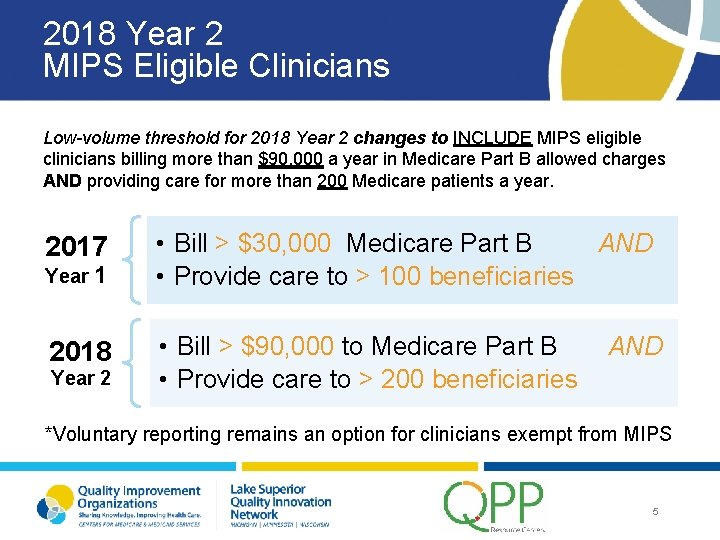
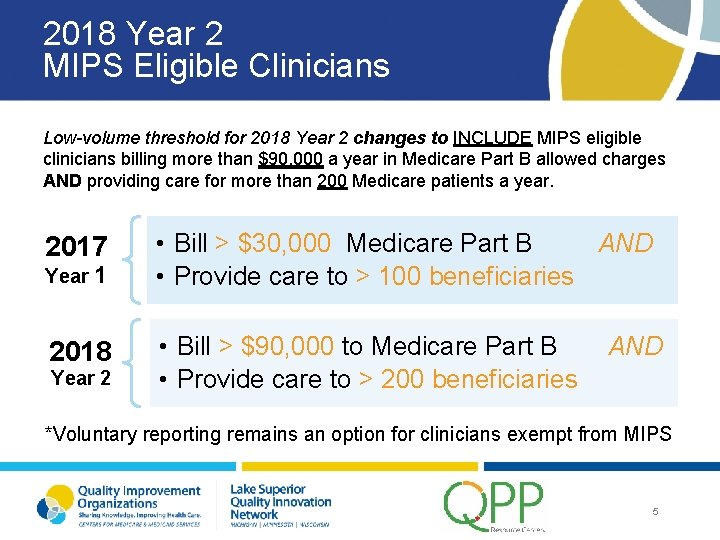
2018 Year 2 MIPS Eligible Clinicians Low-volume threshold for 2018 Year 2 changes to INCLUDE MIPS eligible clinicians billing more than $90, 000 a year in Medicare Part B allowed charges AND providing care for more than 200 Medicare patients a year. 2017 • Bill > $30, 000 Medicare Part B AND • Provide care to > 100 beneficiaries 2018 • Bill > $90, 000 to Medicare Part B • Provide care to > 200 beneficiaries Year 1 Year 2 AND *Voluntary reporting remains an option for clinicians exempt from MIPS 5
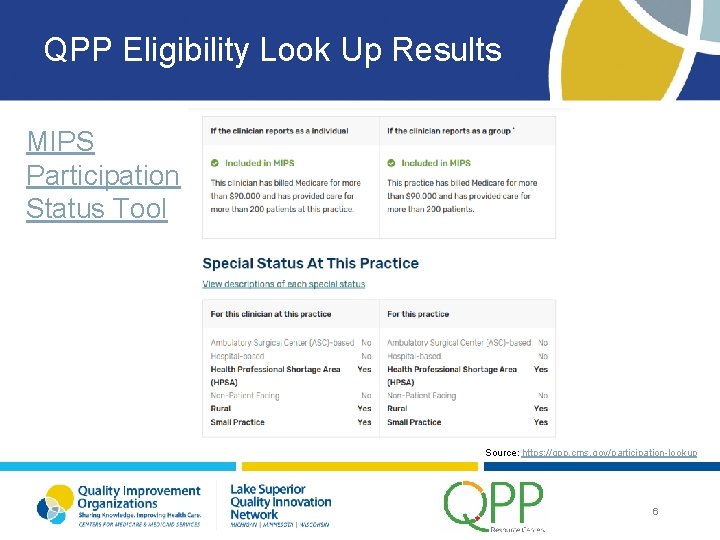
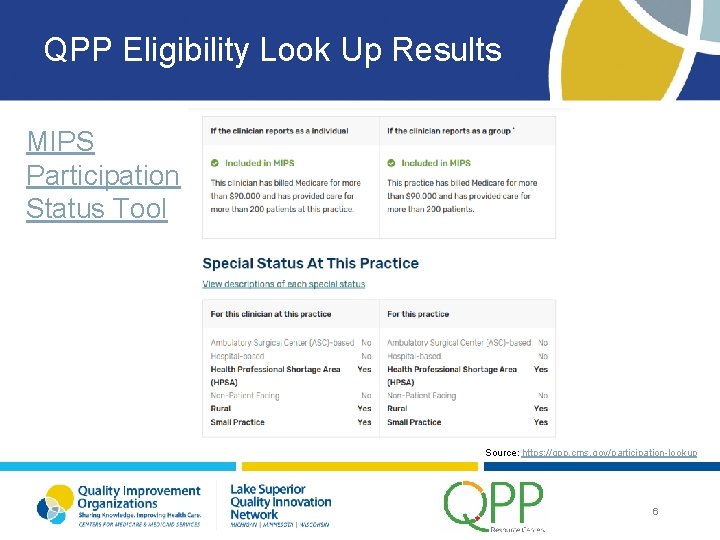
QPP Eligibility Look Up Results MIPS Participation Status Tool Source: https: //qpp. cms. gov/participation-lookup 6
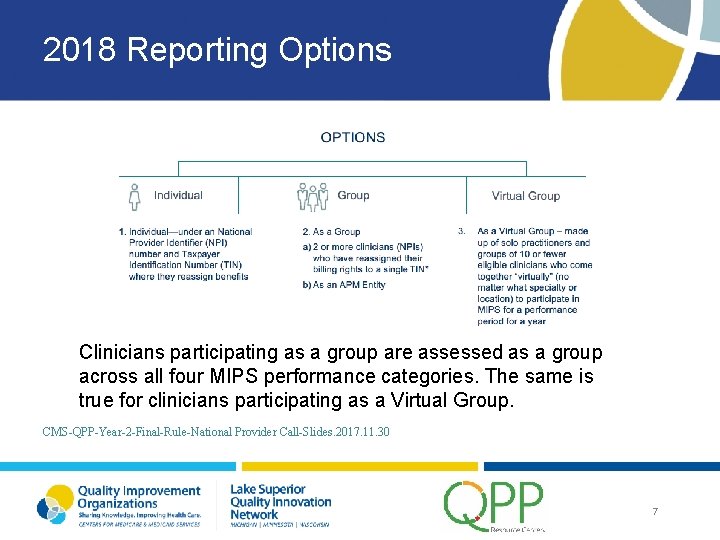
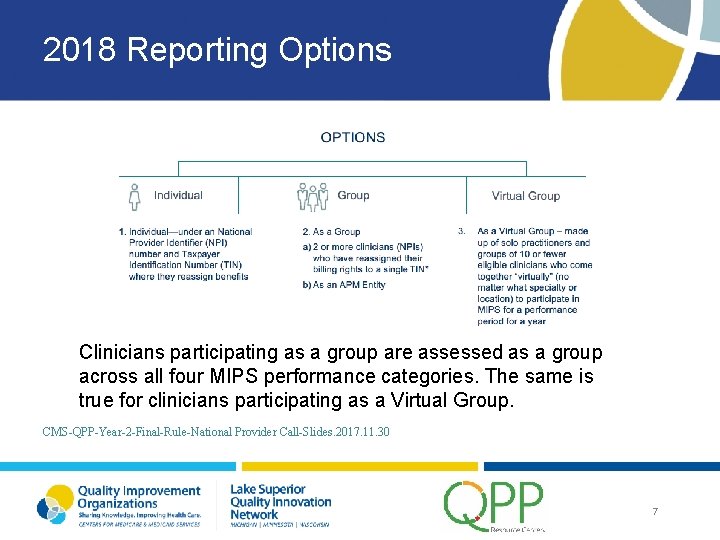
2018 Reporting Options Clinicians participating as a group are assessed as a group across all four MIPS performance categories. The same is true for clinicians participating as a Virtual Group. CMS-QPP-Year-2 -Final-Rule-National Provider Call-Slides. 2017. 11. 30 7
Focus on MIPS Reporting 8
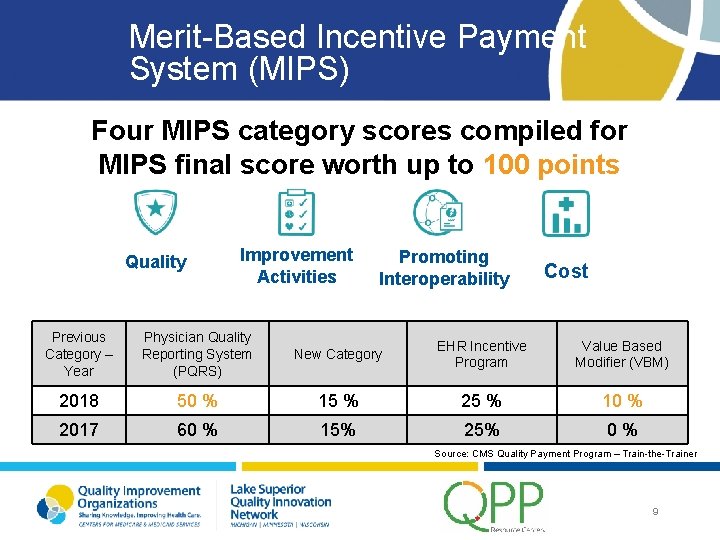
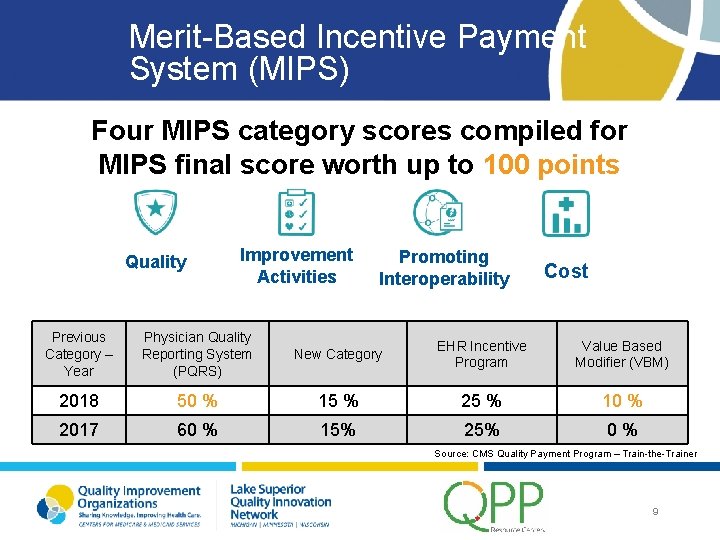
Merit-Based Incentive Payment System (MIPS) Four MIPS category scores compiled for MIPS final score worth up to 100 points Quality Improvement Activities Promoting Interoperability Cost Previous Category – Year Physician Quality Reporting System (PQRS) New Category EHR Incentive Program Value Based Modifier (VBM) 2018 50 % 15 % 25 % 10 % 2017 60 % 15% 25% 0% Source: CMS Quality Payment Program – Train-the-Trainer 9
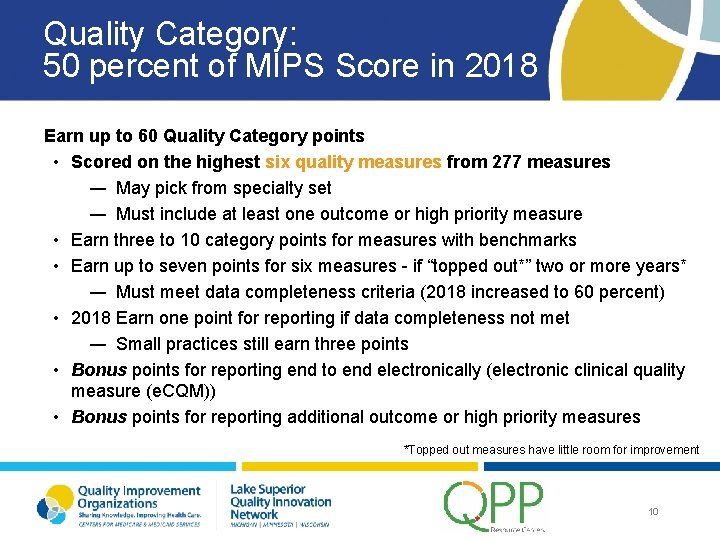
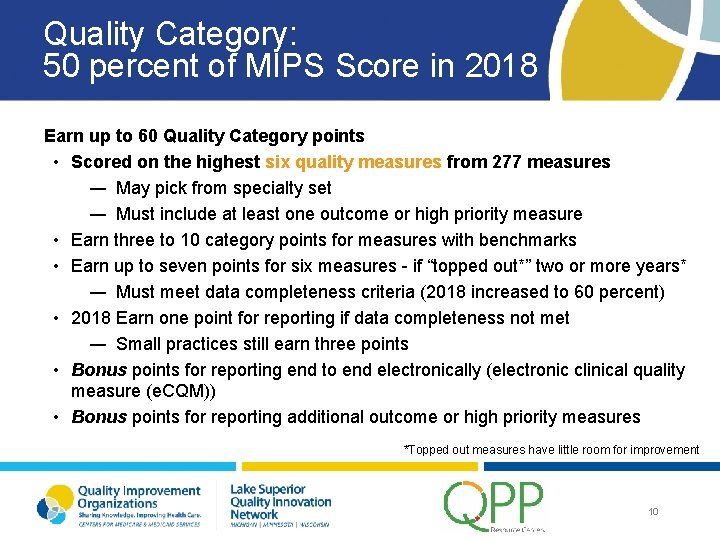
Quality Category: 50 percent of MIPS Score in 2018 Earn up to 60 Quality Category points • Scored on the highest six quality measures from 277 measures ― May pick from specialty set ― Must include at least one outcome or high priority measure • Earn three to 10 category points for measures with benchmarks • Earn up to seven points for six measures - if “topped out*” two or more years* ― Must meet data completeness criteria (2018 increased to 60 percent) • 2018 Earn one point for reporting if data completeness not met ― Small practices still earn three points • Bonus points for reporting end to end electronically (electronic clinical quality measure (e. CQM)) • Bonus points for reporting additional outcome or high priority measures *Topped out measures have little room for improvement 10
Examples of Orthopedic Quality Measures Closing the referral loop Documentation of current medications in the medical record Functional status assessment for total knee replacement Body Mass Index (BMI) screening and follow up plan Pain assessment and follow up 11
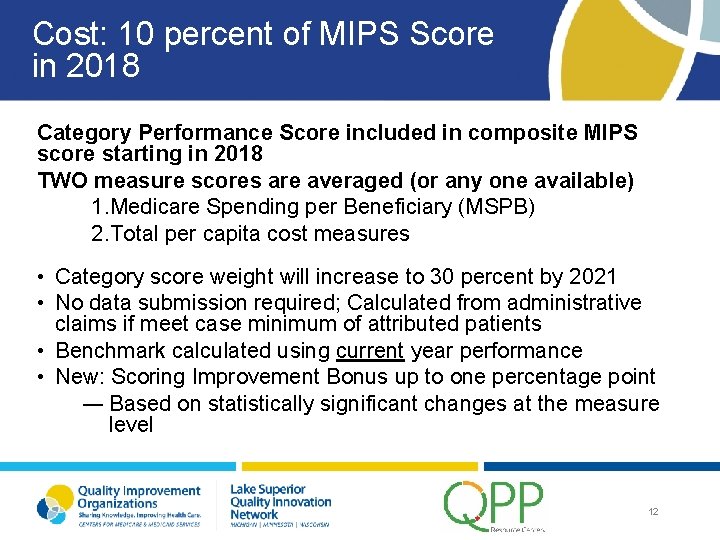
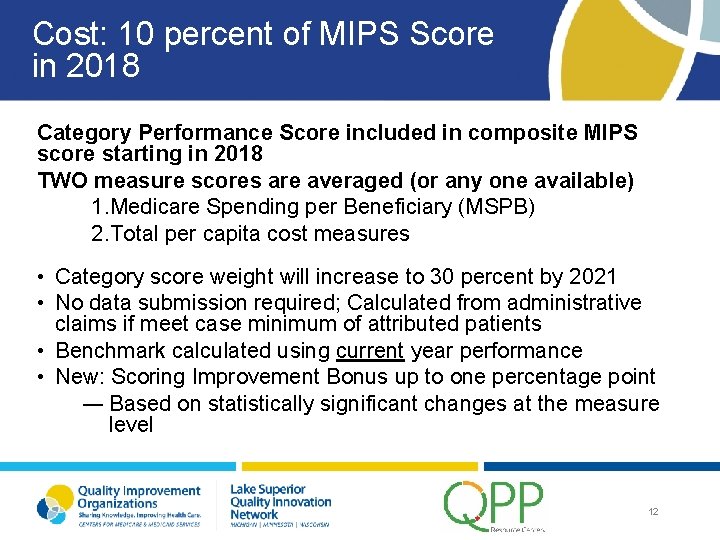
Cost: 10 percent of MIPS Score in 2018 Category Performance Score included in composite MIPS score starting in 2018 TWO measure scores are averaged (or any one available) 1. Medicare Spending per Beneficiary (MSPB) 2. Total per capita cost measures • Category score weight will increase to 30 percent by 2021 • No data submission required; Calculated from administrative claims if meet case minimum of attributed patients • Benchmark calculated using current year performance • New: Scoring Improvement Bonus up to one percentage point ― Based on statistically significant changes at the measure level 12
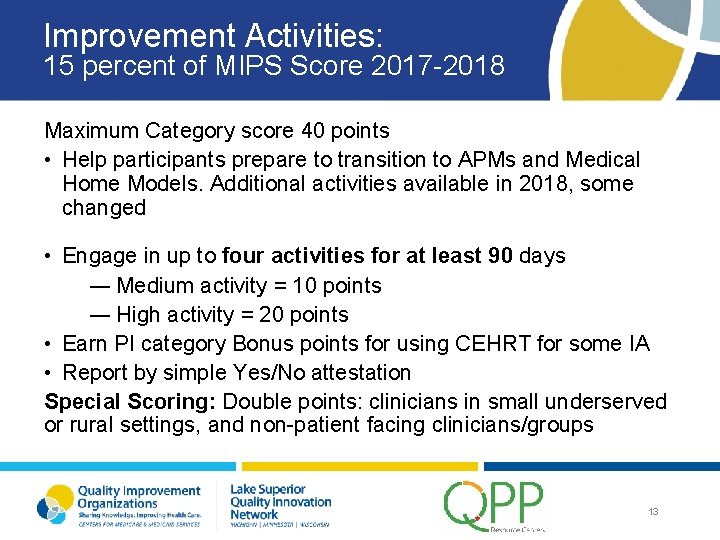
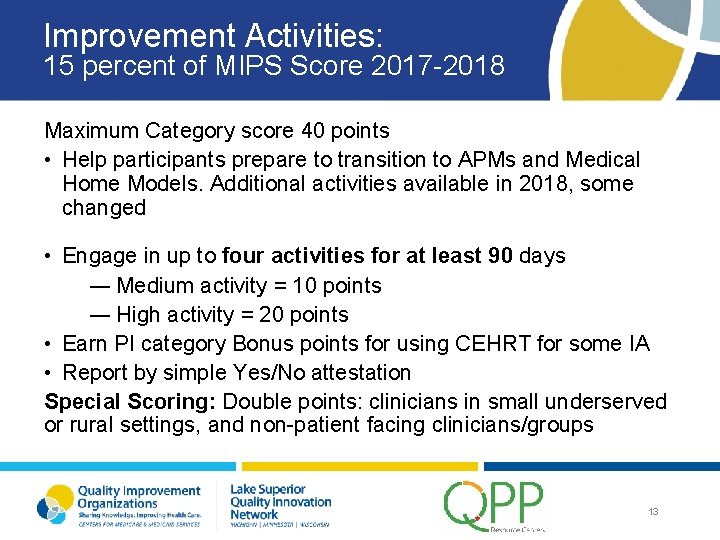
Improvement Activities: 15 percent of MIPS Score 2017 -2018 Maximum Category score 40 points • Help participants prepare to transition to APMs and Medical Home Models. Additional activities available in 2018, some changed • Engage in up to four activities for at least 90 days ― Medium activity = 10 points ― High activity = 20 points • Earn PI category Bonus points for using CEHRT for some IA • Report by simple Yes/No attestation Special Scoring: Double points: clinicians in small underserved or rural settings, and non-patient facing clinicians/groups 13
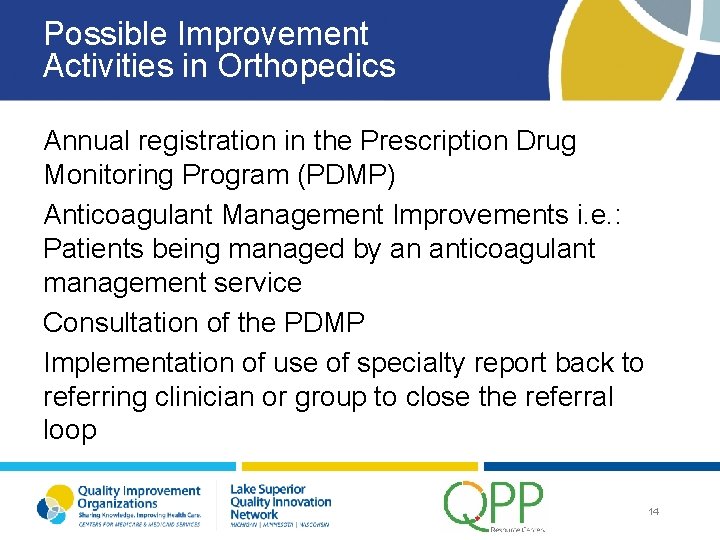
Possible Improvement Activities in Orthopedics Annual registration in the Prescription Drug Monitoring Program (PDMP) Anticoagulant Management Improvements i. e. : Patients being managed by an anticoagulant management service Consultation of the PDMP Implementation of use of specialty report back to referring clinician or group to close the referral loop 14
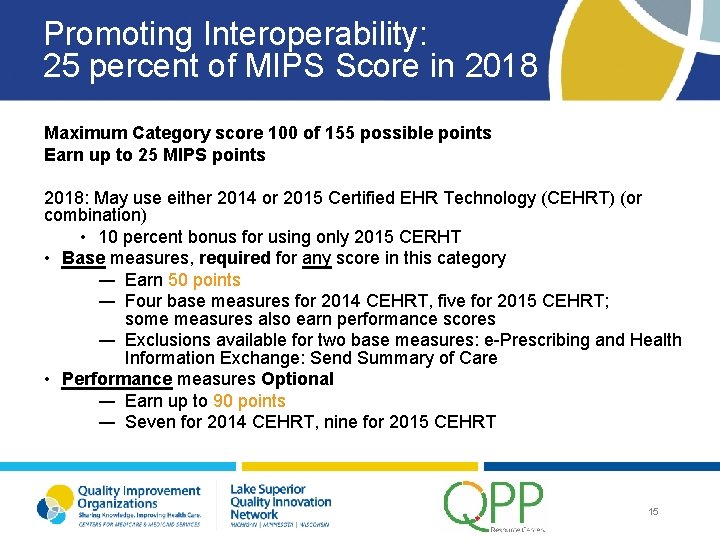
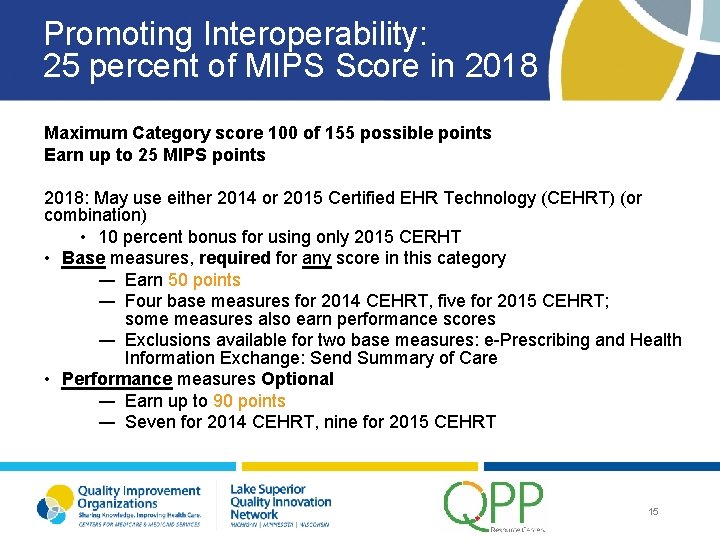
Promoting Interoperability: 25 percent of MIPS Score in 2018 Maximum Category score 100 of 155 possible points Earn up to 25 MIPS points 2018: May use either 2014 or 2015 Certified EHR Technology (CEHRT) (or combination) • 10 percent bonus for using only 2015 CERHT • Base measures, required for any score in this category ― Earn 50 points ― Four base measures for 2014 CEHRT, five for 2015 CEHRT; some measures also earn performance scores ― Exclusions available for two base measures: e-Prescribing and Health Information Exchange: Send Summary of Care • Performance measures Optional ― Earn up to 90 points ― Seven for 2014 CEHRT, nine for 2015 CEHRT 15
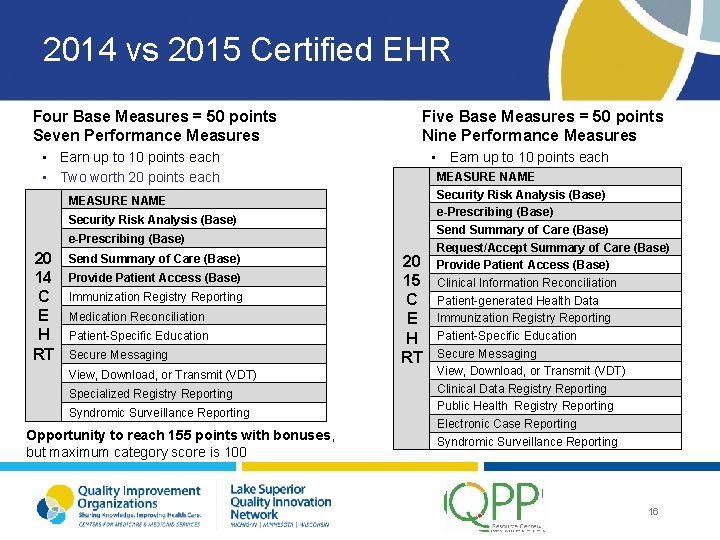
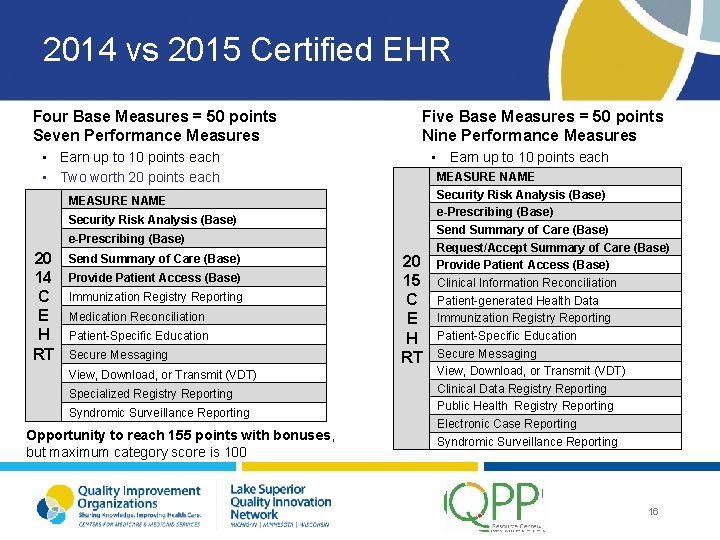
2014 vs 2015 Certified EHR Four Base Measures = 50 points Seven Performance Measures Five Base Measures = 50 points Nine Performance Measures • Earn up to 10 points each • Two worth 20 points each • Earn up to 10 points each MEASURE NAME Security Risk Analysis (Base) e-Prescribing (Base) 20 14 C E H RT Send Summary of Care (Base) Provide Patient Access (Base) Immunization Registry Reporting Medication Reconciliation Patient-Specific Education Secure Messaging View, Download, or Transmit (VDT) Specialized Registry Reporting Syndromic Surveillance Reporting Opportunity to reach 155 points with bonuses, but maximum category score is 100 20 15 C E H RT MEASURE NAME Security Risk Analysis (Base) e-Prescribing (Base) Send Summary of Care (Base) Request/Accept Summary of Care (Base) Provide Patient Access (Base) Clinical Information Reconciliation Patient-generated Health Data Immunization Registry Reporting Patient-Specific Education Secure Messaging View, Download, or Transmit (VDT) Clinical Data Registry Reporting Public Health Registry Reporting Electronic Case Reporting Syndromic Surveillance Reporting 16
Reporting Scenarios of Orthopaedics 17
Scenario One Background • • Solo Practice Surgeon Eligible Clinician (exceeds low volume threshold) Must report to avoid a negative penalty Does not utilize an EHR Reporting Options • • Needs to obtain 15 MIPS Points to remain Neutral Could attest to Improvement Activities Report Quality Category via claims or registry Note: Practices with 15 or less clinicians get some special scoring 18
Solo Surgeon Reporting with No EHR • • • Clinician decides that she does not want to pay for a registry and go through the trouble of doing chart reviews to populate the registry Finds out that billers have been submitting some “G” Codes for Medication Reconciliation and Body Mass Index Screening but they did not meet the 60 percent data completeness for quality Attests to using the Prescription Drug Monitoring Program (PDMP) 19
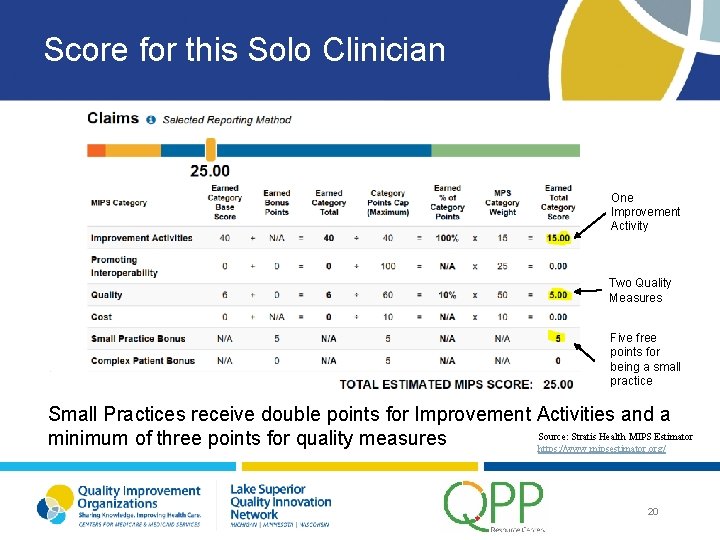
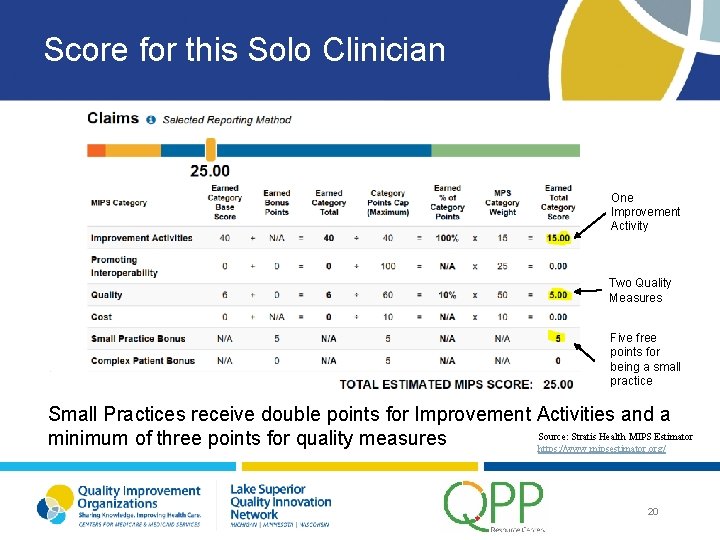
Score for this Solo Clinician One Improvement Activity Two Quality Measures Five free points for being a small practice Small Practices receive double points for Improvement Activities and a Source: Stratis Health MIPS Estimator minimum of three points for quality measures https: //www. mipsestimator. org/ 20
Scenario Two Background • • Orthopaedics Group Practice with 16 Eligible Clinician Types Has EHR through the local hospital Two of the clinicians exceed the low Volume Threshold The remaining 14 are eligible at the group level but not individually Reporting Options • Group Reporting • Individual Reports (2 mandatory and 14 voluntary) 21
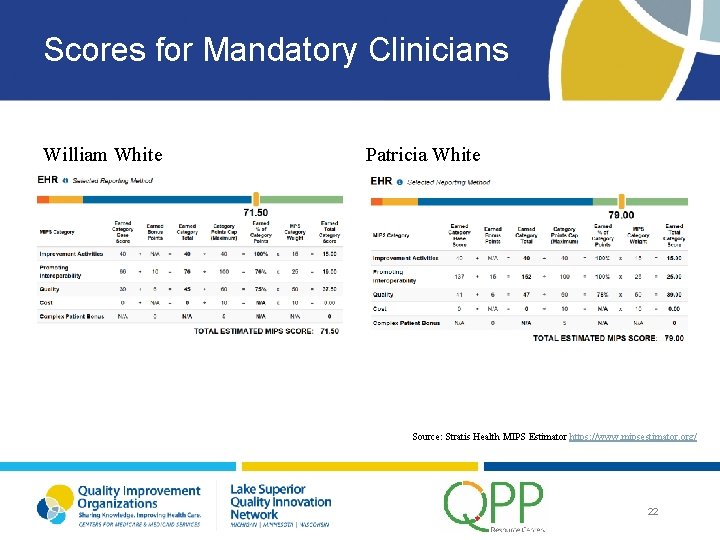
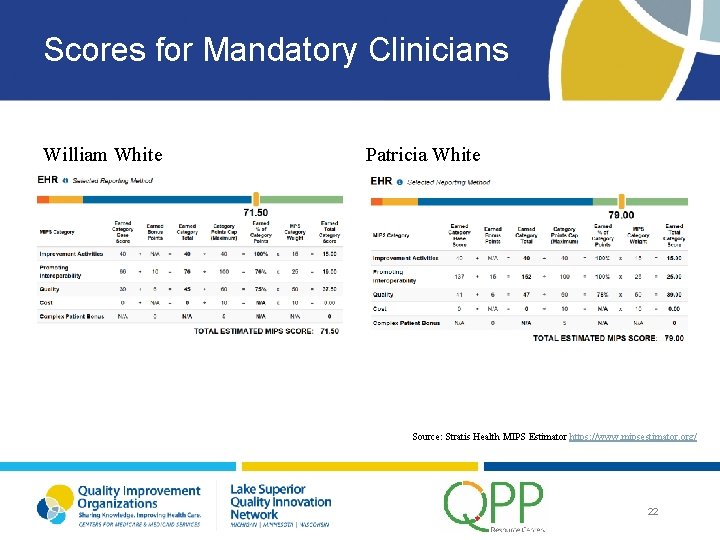
Scores for Mandatory Clinicians William White Patricia White Source: Stratis Health MIPS Estimator https: //www. mipsestimator. org/ 22
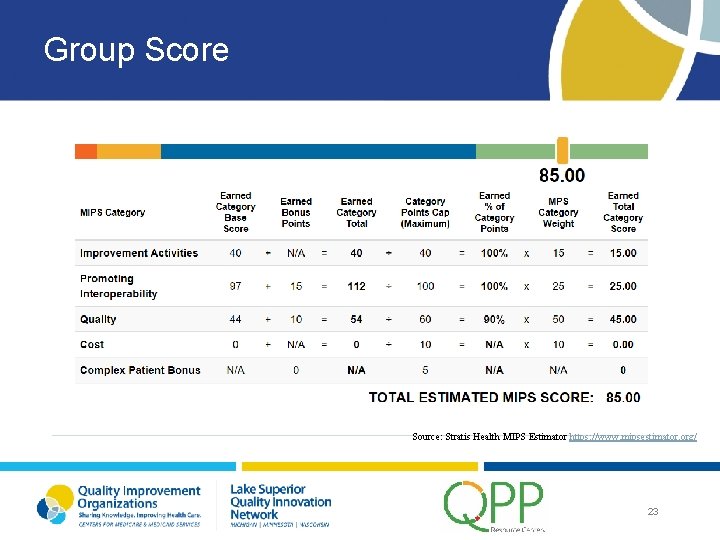
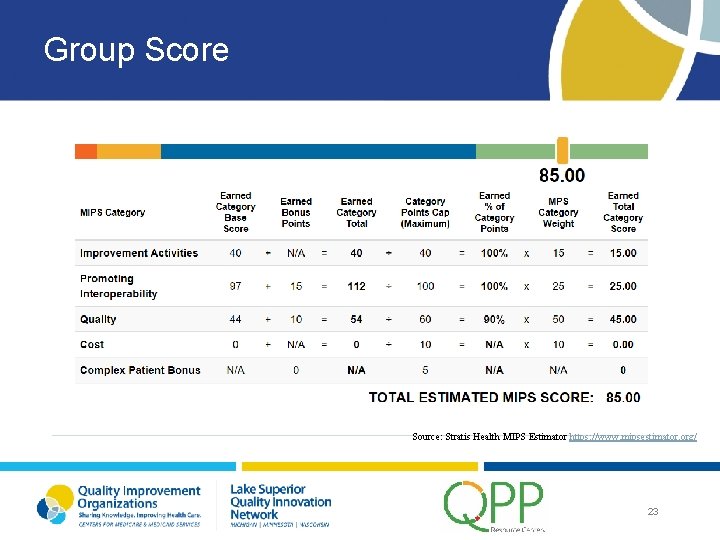
Group Score Source: Stratis Health MIPS Estimator https: //www. mipsestimator. org/ 23
Group versus Individual Report – The individual clinicians will receive a payment adjustment Group report – All eligible clinician types in the group will receive a payment adjustment In this example, the group score was greater than either of the mandatory reporters so if a group report was submitted, they would receive the higher of the two scores. 24
Important Information About the Scenarios Did not give any points for cost or complex patient bonus The scores were calculated based on the most current benchmarks (some benchmarks will be recalculated during the performance year) 25
Resources Stratis Health MIPS Estimator https: //www. mipsestimator. org/ Quality Payment Program Website: https: //qpp. cms. gov/ 26
Questions? Kris Shay – Health. Care Data Systems (kshay@hcds. us) 262 -369 -3460 Mona Mathews, MA, PMP – Meta. Star mmathews@metastar. com 608 -441 -8241 Chris Becker, CPHIMS, CPHIT – Meta. Star cbecker@metastar. com 608 -441 -8217 www. lsqin. org www. metastar. com 27

This material was prepared by the Lake Superior Quality Innovation Network, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U. S. Department of Health and Human Services. The materials do not necessarily reflect CMS policy. 11 SOW-WI-D 1 -18 -107 100518