Quality Improvement The Model for Improvement PDSA Cycles

- Slides: 39
Quality Improvement The Model for Improvement, PDSA Cycles, and Accelerating Improvement Heather Maciejewski BEACON Quality Improvement Coordinator Ohio Chapter, AAP
Session Objectives • To describe the components of the Model for Improvement • To identify measures and goals for your participation in EASE • To develop a clear plan for your team to test a change idea • To identify future tests of change
QUALITY IMPROVEMENT STRUCTURE, APPROACH AND ROADMAP
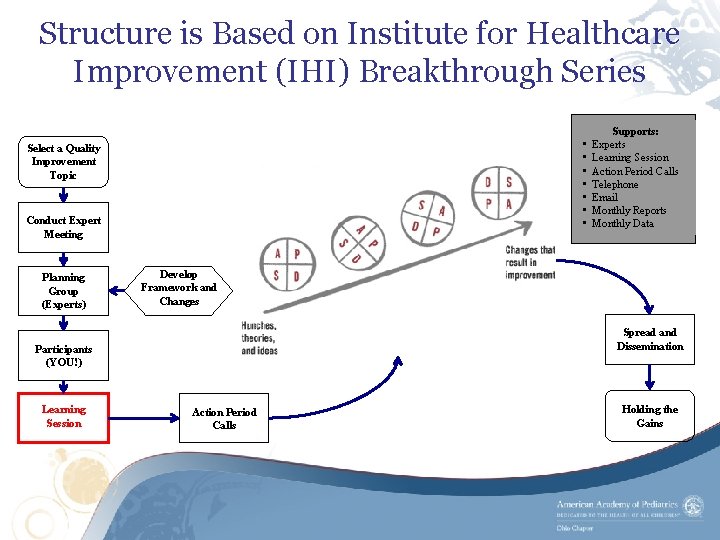
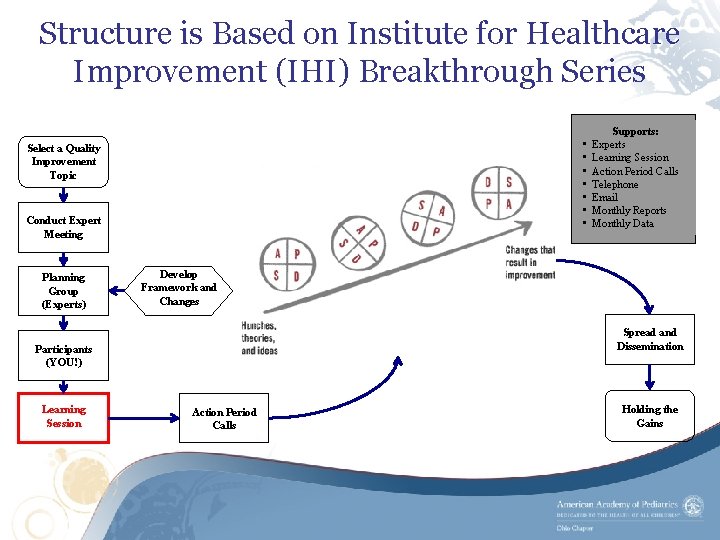
Structure is Based on Institute for Healthcare Improvement (IHI) Breakthrough Series • • Select a Quality Improvement Topic Conduct Expert Meeting Planning Group (Experts) Develop Framework and Changes Spread and Dissemination Participants (YOU!) Learning Session Supports: Experts Learning Session Action Period Calls Telephone Email Monthly Reports Monthly Data Action Period Calls Holding the Gains
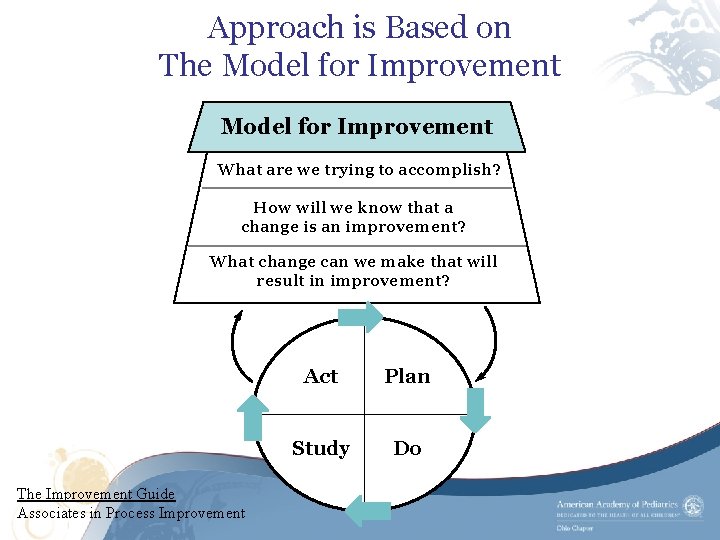
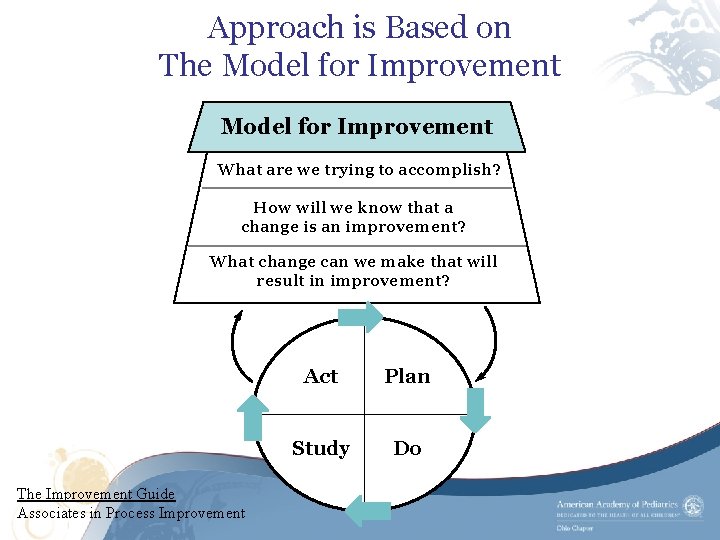
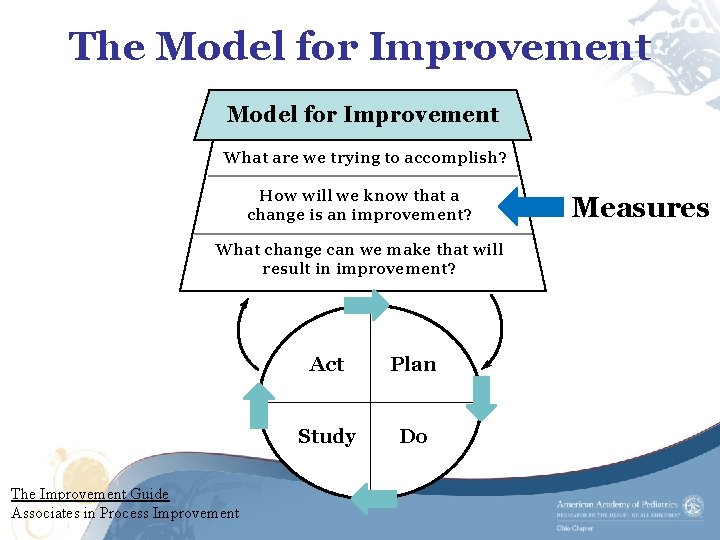
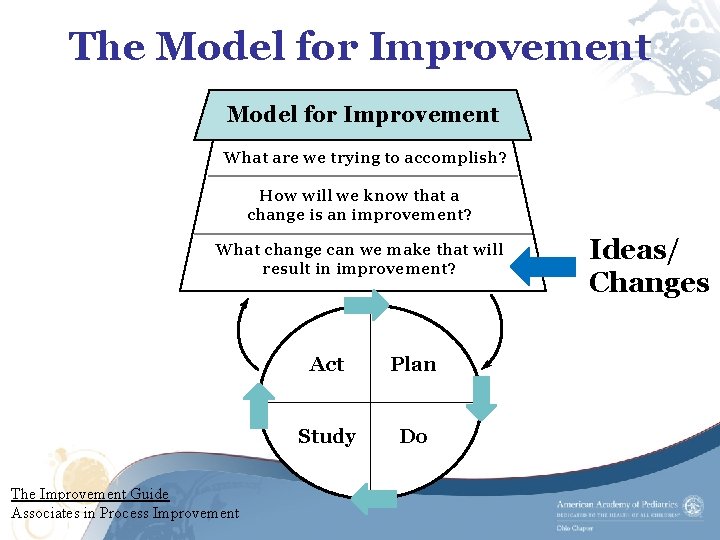
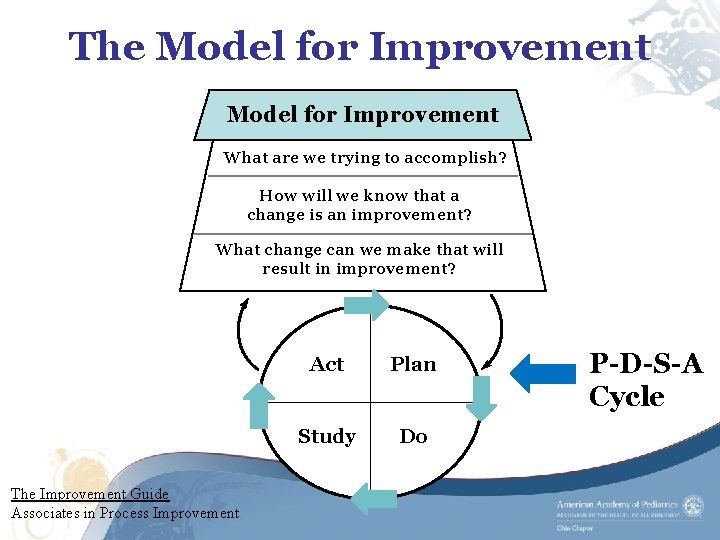
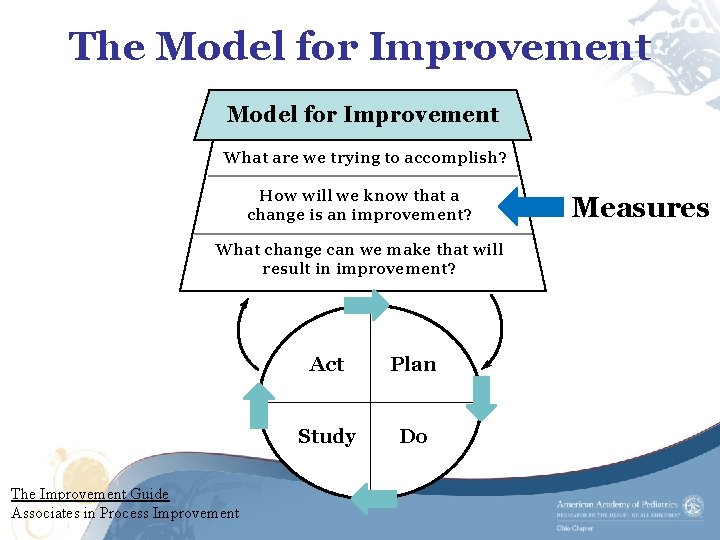
Approach is Based on The Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? The Improvement Guide Associates in Process Improvement Act Plan Study Do
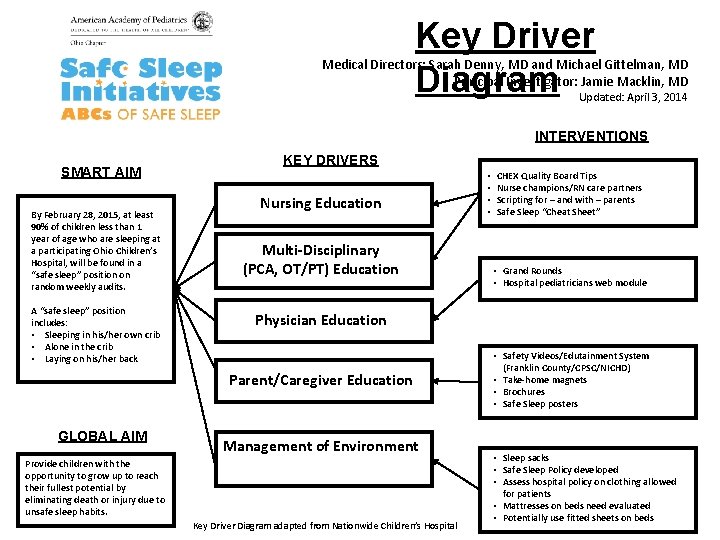
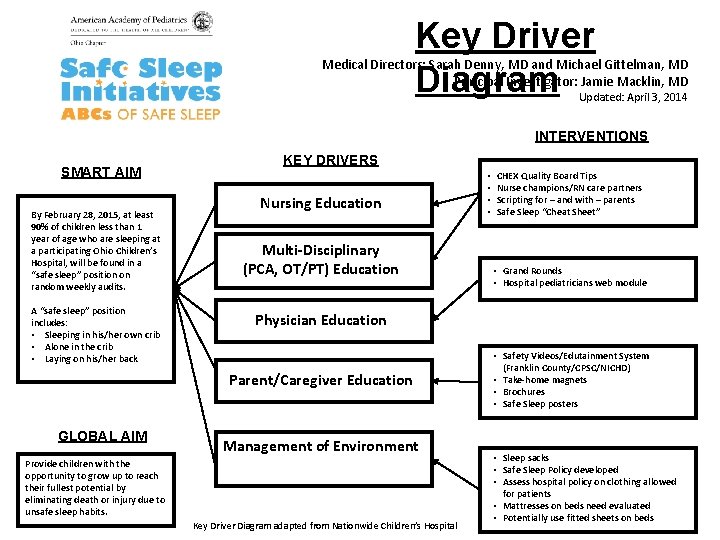
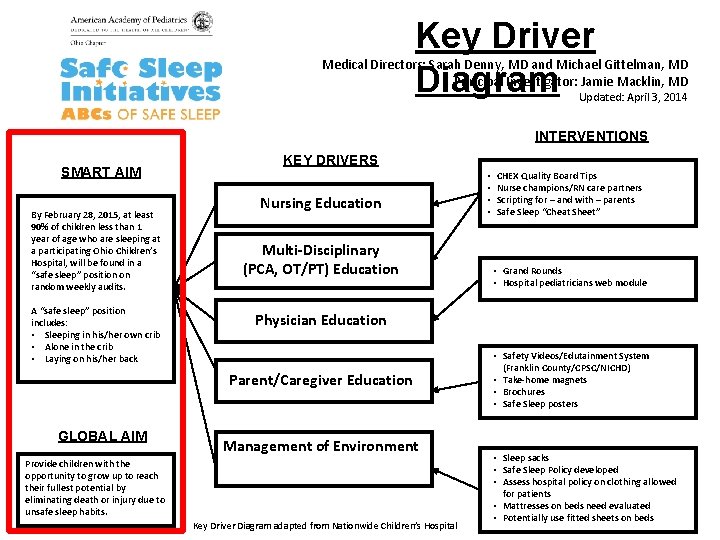
Key Driver Diagram Medical Directors: Sarah Denny, MD and Michael Gittelman, MD Principal Investigator: Jamie Macklin, MD Updated: April 3, 2014 INTERVENTIONS SMART AIM By February 28, 2015, at least 90% of children less than 1 year of age who are sleeping at a participating Ohio Children’s Hospital, will be found in a “safe sleep” position on random weekly audits. A “safe sleep” position includes: • Sleeping in his/her own crib • Alone in the crib • Laying on his/her back KEY DRIVERS Nursing Education Multi-Disciplinary (PCA, OT/PT) Education CHEX Quality Board Tips Nurse champions/RN care partners Scripting for – and with – parents Safe Sleep “Cheat Sheet” • Grand Rounds • Hospital pediatricians web module Physician Education Parent/Caregiver Education GLOBAL AIM • • Management of Environment Provide children with the opportunity to grow up to reach their fullest potential by eliminating death or injury due to unsafe sleep habits. Key Driver Diagram adapted from Nationwide Children’s Hospital • Safety Videos/Edutainment System (Franklin County/CPSC/NICHD) • Take-home magnets • Brochures • Safe Sleep posters • Sleep sacks • Safe Sleep Policy developed • Assess hospital policy on clothing allowed for patients • Mattresses on beds need evaluated • Potentially use fitted sheets on beds
THE MODEL FOR IMPROVEMENT
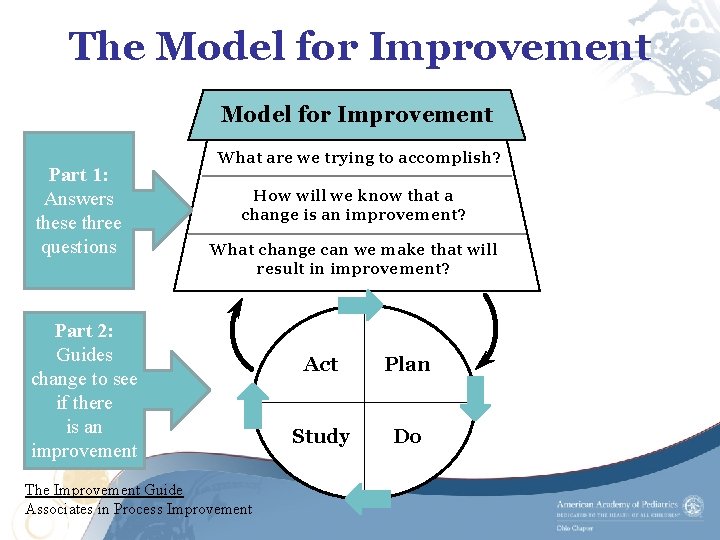
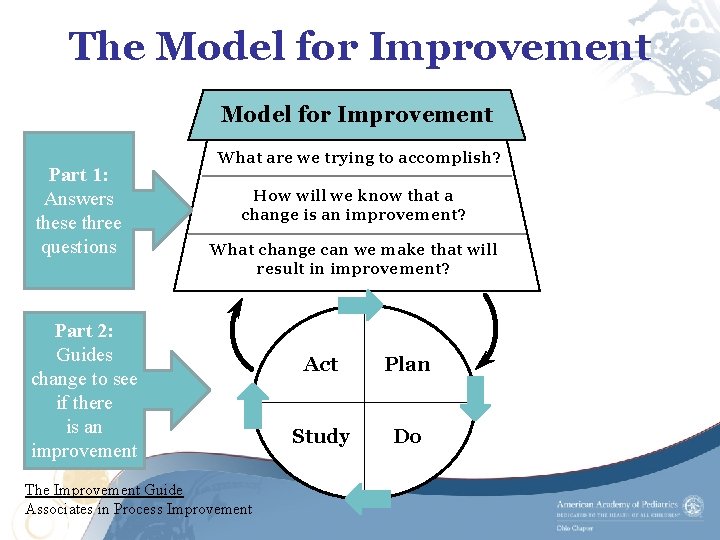
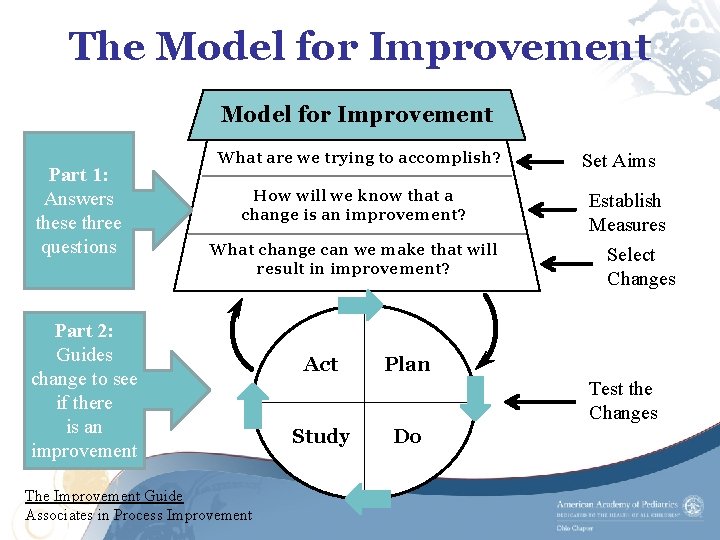
The Model for Improvement Part 1: Answers these three questions What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? Part 2: Guides change to see if there is an improvement The Improvement Guide Associates in Process Improvement Act Plan Study Do
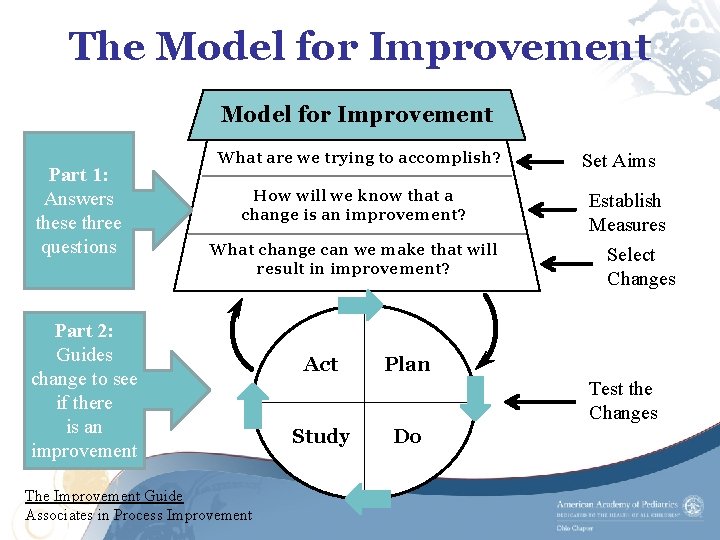
The Model for Improvement Part 1: Answers these three questions What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? Part 2: Guides change to see if there is an improvement The Improvement Guide Associates in Process Improvement Act Set Aims Establish Measures Select Changes Plan Test the Changes Study Do
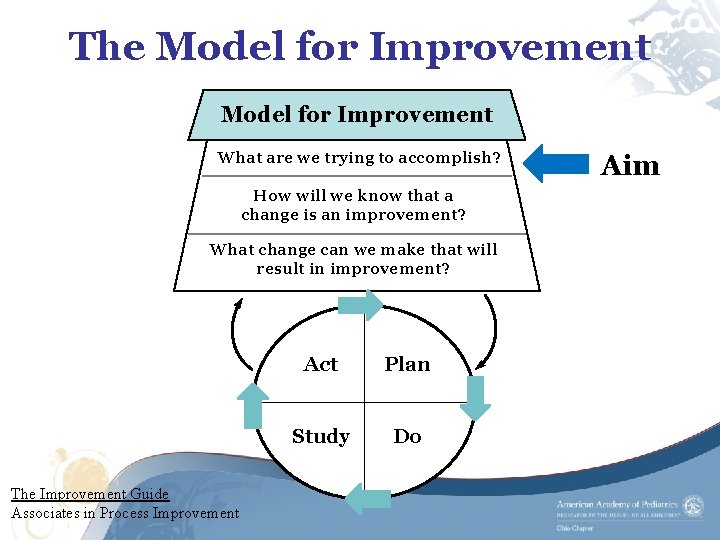
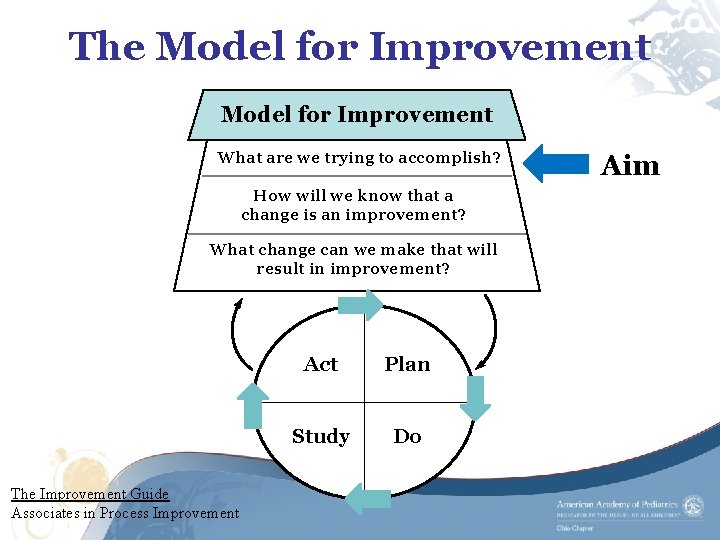
The Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? The Improvement Guide Associates in Process Improvement Act Plan Study Do Aim
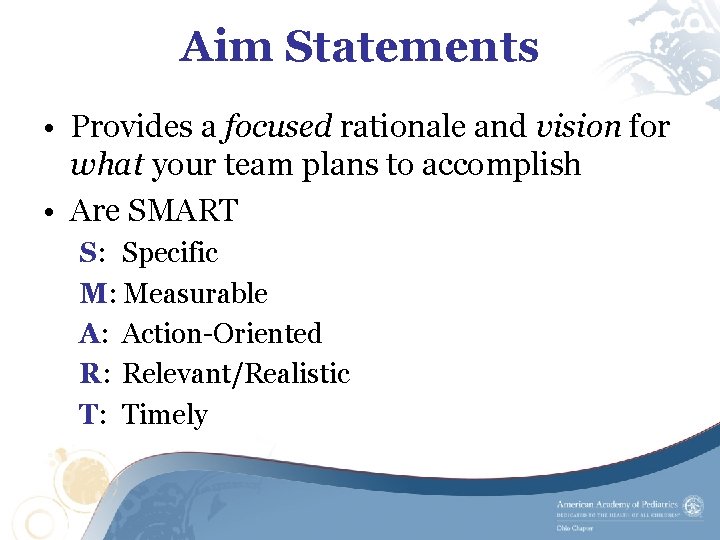
Aim Statements • Provides a focused rationale and vision for what your team plans to accomplish • Are SMART S: Specific M: Measurable A: Action-Oriented R: Relevant/Realistic T: Timely
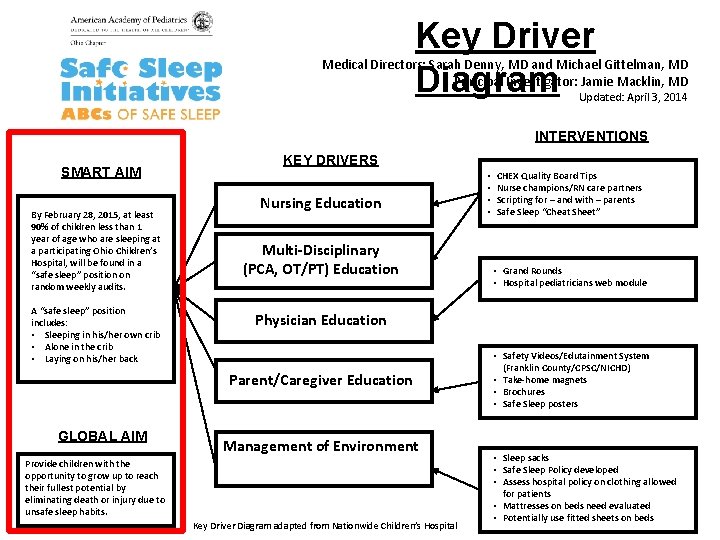
Key Driver Diagram Medical Directors: Sarah Denny, MD and Michael Gittelman, MD Principal Investigator: Jamie Macklin, MD Updated: April 3, 2014 INTERVENTIONS SMART AIM By February 28, 2015, at least 90% of children less than 1 year of age who are sleeping at a participating Ohio Children’s Hospital, will be found in a “safe sleep” position on random weekly audits. A “safe sleep” position includes: • Sleeping in his/her own crib • Alone in the crib • Laying on his/her back KEY DRIVERS Nursing Education Multi-Disciplinary (PCA, OT/PT) Education CHEX Quality Board Tips Nurse champions/RN care partners Scripting for – and with – parents Safe Sleep “Cheat Sheet” • Grand Rounds • Hospital pediatricians web module Physician Education Parent/Caregiver Education GLOBAL AIM • • Management of Environment Provide children with the opportunity to grow up to reach their fullest potential by eliminating death or injury due to unsafe sleep habits. Key Driver Diagram adapted from Nationwide Children’s Hospital • Safety Videos/Edutainment System (Franklin County/CPSC/NICHD) • Take-home magnets • Brochures • Safe Sleep posters • Sleep sacks • Safe Sleep Policy developed • Assess hospital policy on clothing allowed for patients • Mattresses on beds need evaluated • Potentially use fitted sheets on beds
Global vs. Specific Aim Statements Education and Sleep Environment (EASE): The Injury Prevention Learning Collaborative with Hospitalists • Global Aim: Provide children with the opportunity to grow up to reach their fullest potential by eliminating death or injury due to unsafe sleep habits.
Global vs. Specific Aim Statements • Specific Aim: By February 28, 2015, at least 90% of children less than 1 year of age who are sleeping at a participating Ohio Children’s Hospital, will be found in a “safe sleep” position during random weekly audits. – A “safe sleep” position includes a child who is: • Sleeping in his/her own crib • Sleeping alone in the crib • Laying on his/her back
The Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? The Improvement Guide Associates in Process Improvement Act Plan Study Do Measures
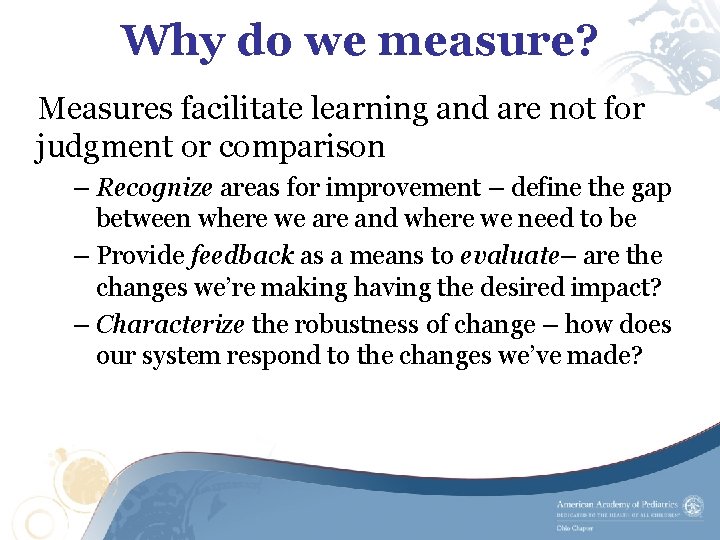
Why do we measure? Measures facilitate learning and are not for judgment or comparison – Recognize areas for improvement – define the gap between where we are and where we need to be – Provide feedback as a means to evaluate– are the changes we’re making having the desired impact? – Characterize the robustness of change – how does our system respond to the changes we’ve made?
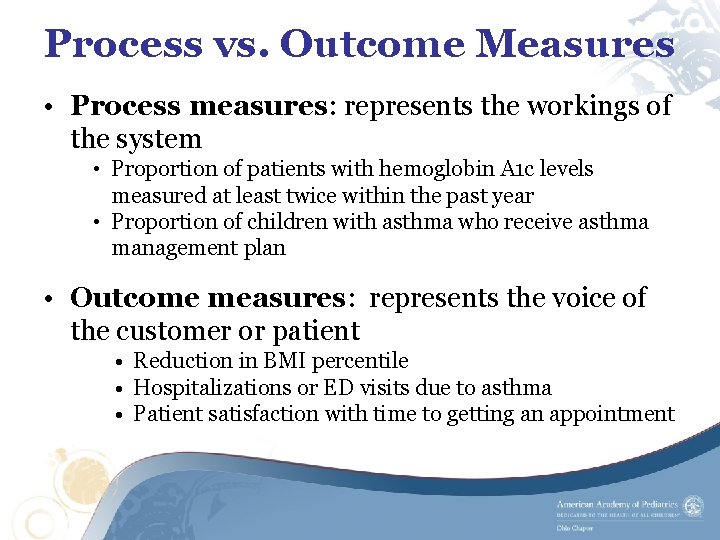
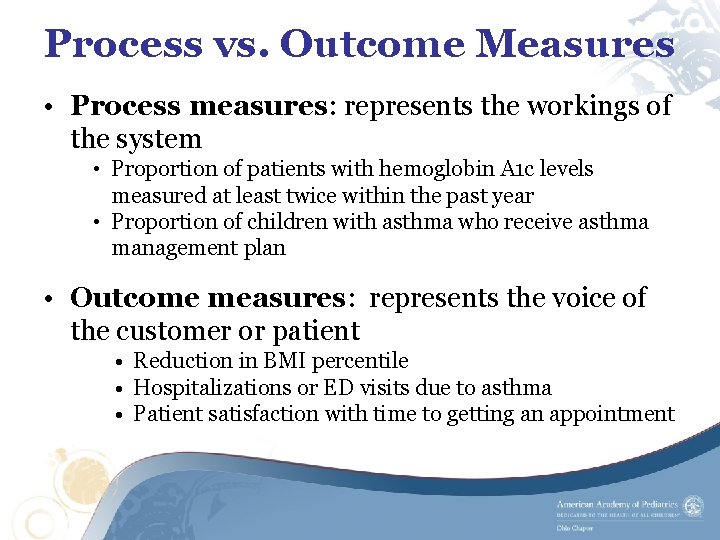
Process vs. Outcome Measures • Process measures: represents the workings of the system • Proportion of patients with hemoglobin A 1 c levels measured at least twice within the past year • Proportion of children with asthma who receive asthma management plan • Outcome measures: represents the voice of the customer or patient • Reduction in BMI percentile • Hospitalizations or ED visits due to asthma • Patient satisfaction with time to getting an appointment
EASE Measures EASE process measures include: • > 90% of patients 1 year of age and younger will leave the hospital with information on safe sleep practices • Each hospital will show that > 90% of children ≤ 1 year of age will be in “safe sleep” position (own crib, nothing in crib and on back) on random weekly audits by the end of the 12 -month project – This is a bundled measure of all three items for a safe sleep position
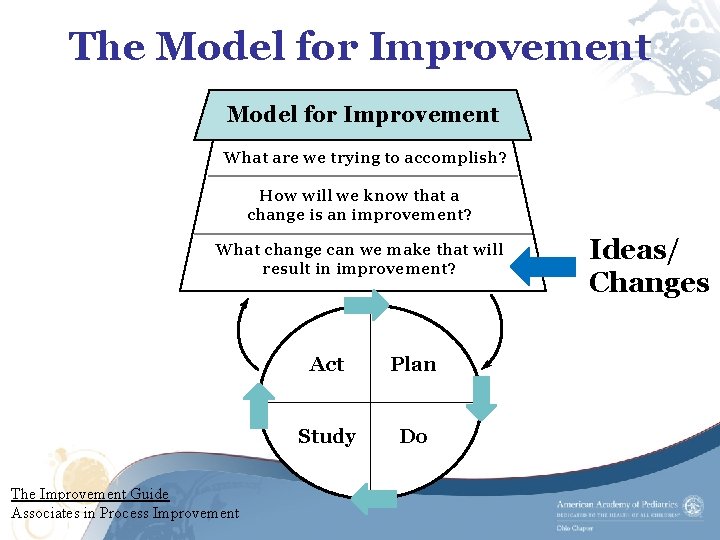
The Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? The Improvement Guide Associates in Process Improvement Act Plan Study Do Ideas/ Changes
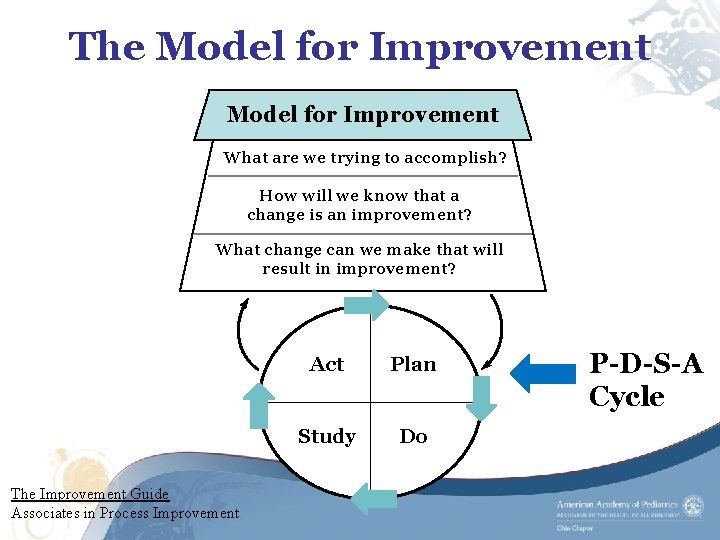
The Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? The Improvement Guide Associates in Process Improvement Act Plan Study Do P-D-S-A Cycle
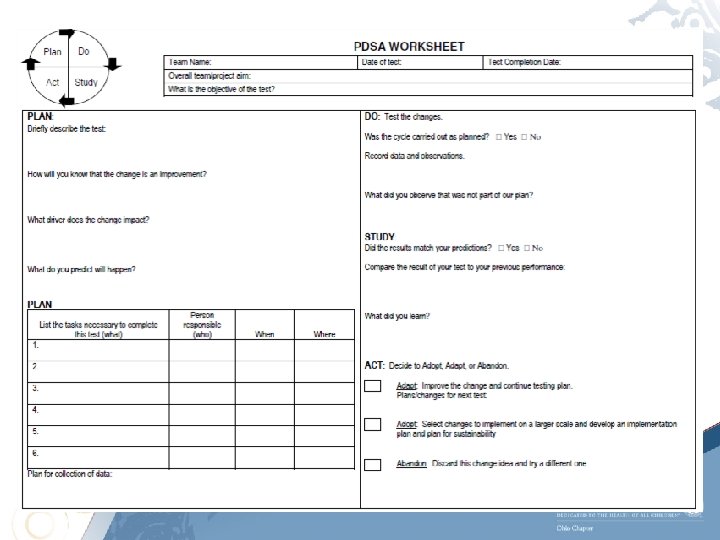
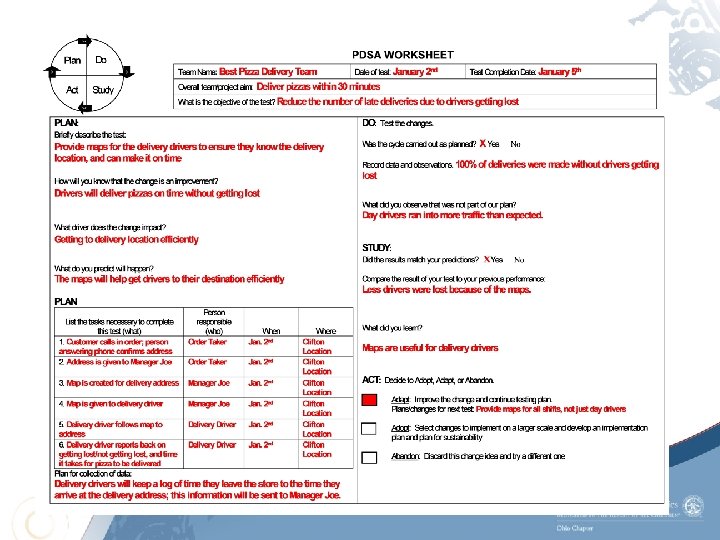
PLAN – DO – STUDY – ACT CYCLES
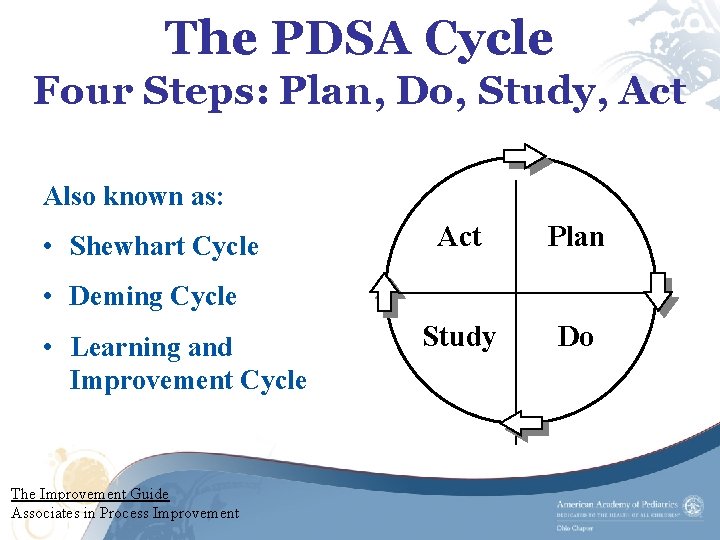
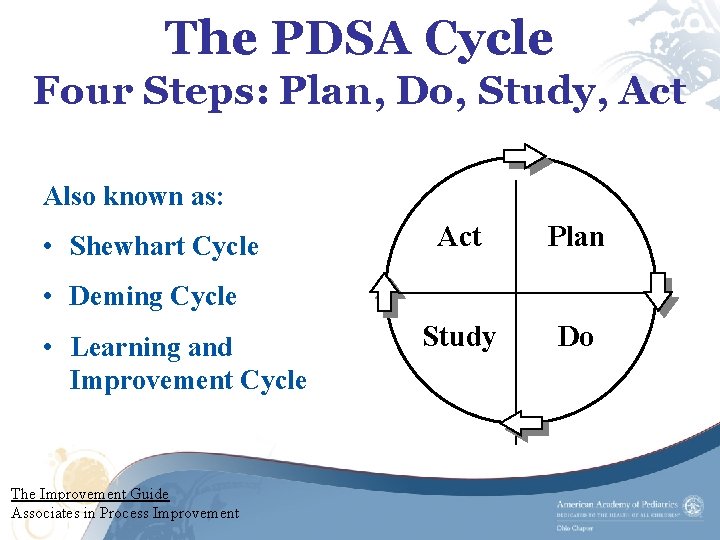
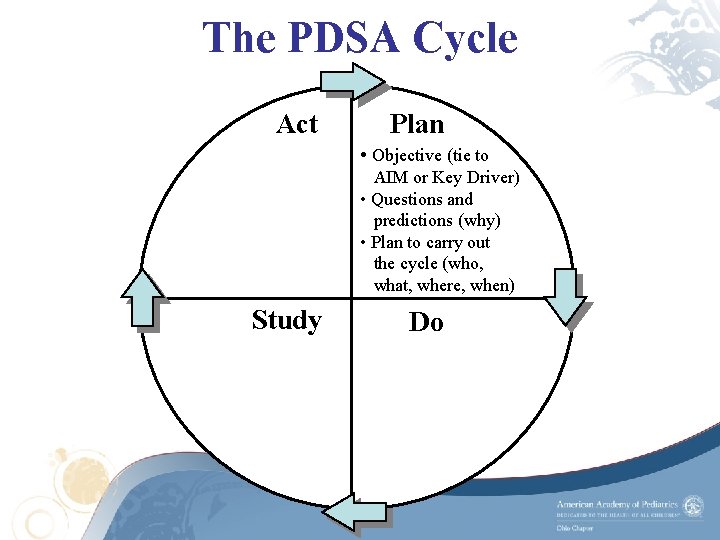
The PDSA Cycle Four Steps: Plan, Do, Study, Act Also known as: • Shewhart Cycle Act Plan Study Do • Deming Cycle • Learning and Improvement Cycle The Improvement Guide Associates in Process Improvement
Use PDSA Test Cycles for: • Testing or adapting a change idea – May answer a question related to the aim • Implementing a change • Spreading the changes to the rest of the system
Why Test? • Force us to think small • Increases your belief that the change will result in improvement • Opportunity for learning without impacting performance • Help teams adapt good ideas to their specific situation The Improvement Guide Associates in Process Improvement
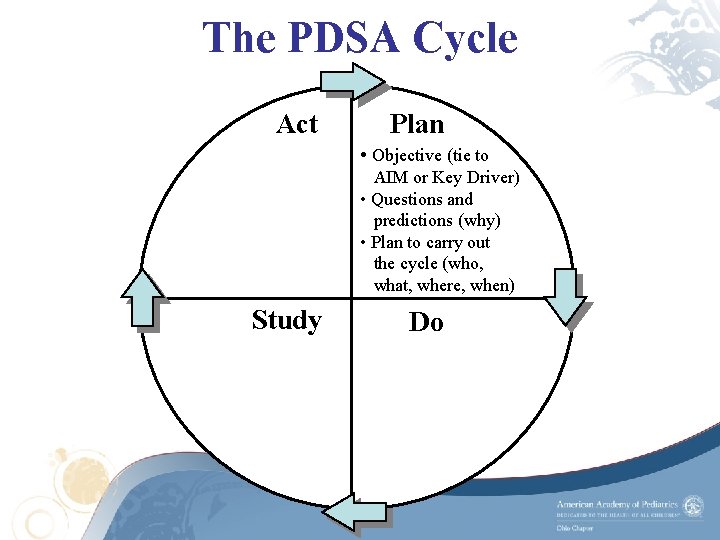
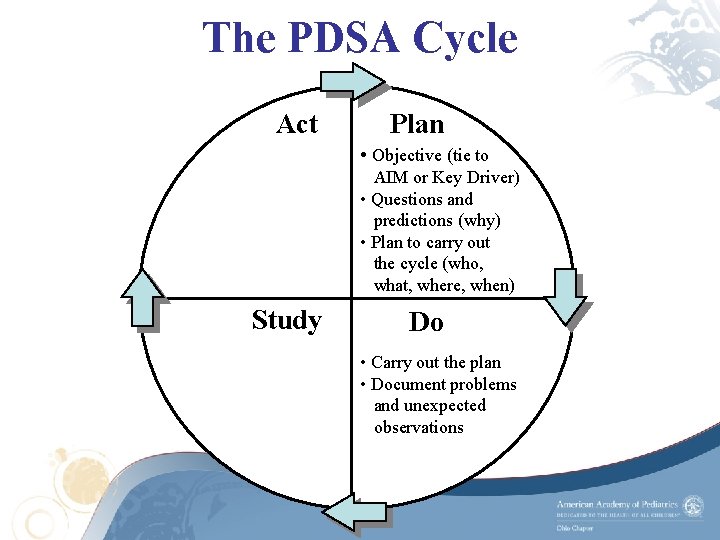
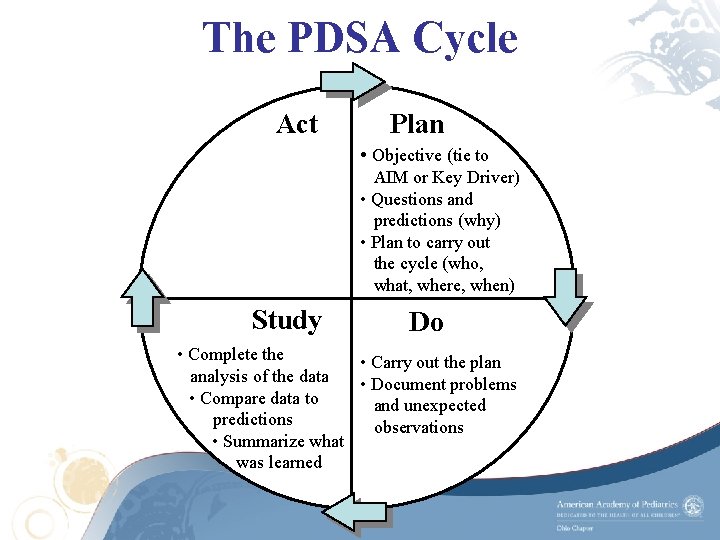
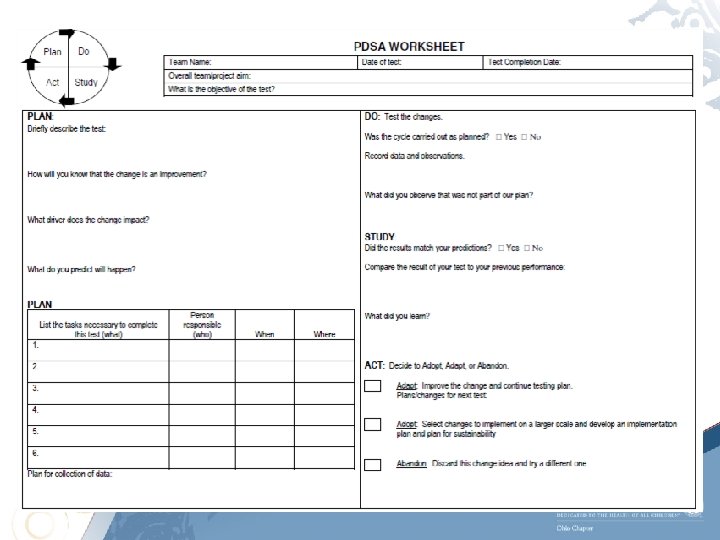
The PDSA Cycle Act Plan • Objective (tie to AIM or Key Driver) • Questions and predictions (why) • Plan to carry out the cycle (who, what, where, when) Study Do
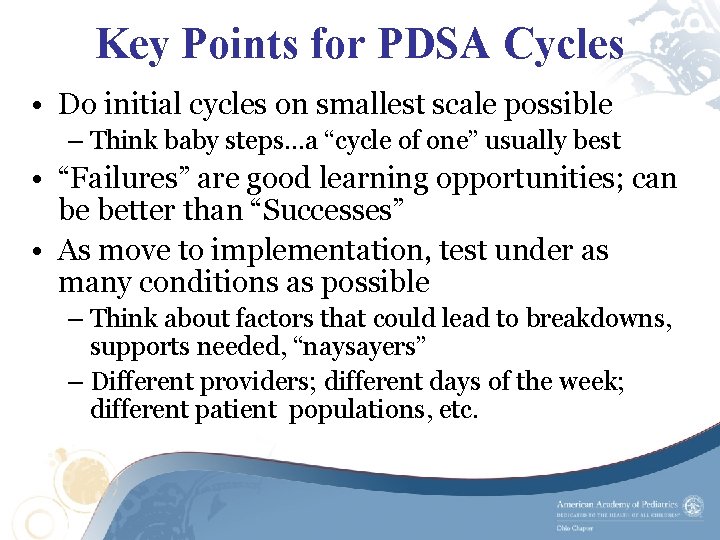
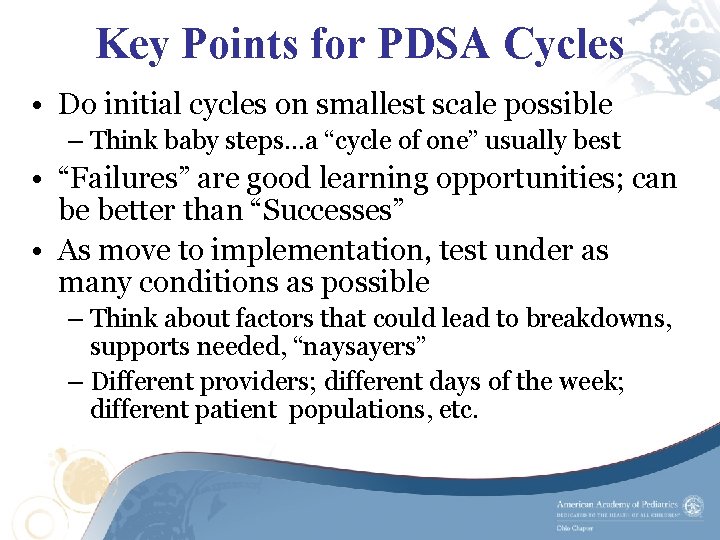
Key Points for PDSA Cycles • Do initial cycles on smallest scale possible – Think baby steps…a “cycle of one” usually best • “Failures” are good learning opportunities; can be better than “Successes” • As move to implementation, test under as many conditions as possible – Think about factors that could lead to breakdowns, supports needed, “naysayers” – Different providers; different days of the week; different patient populations, etc.
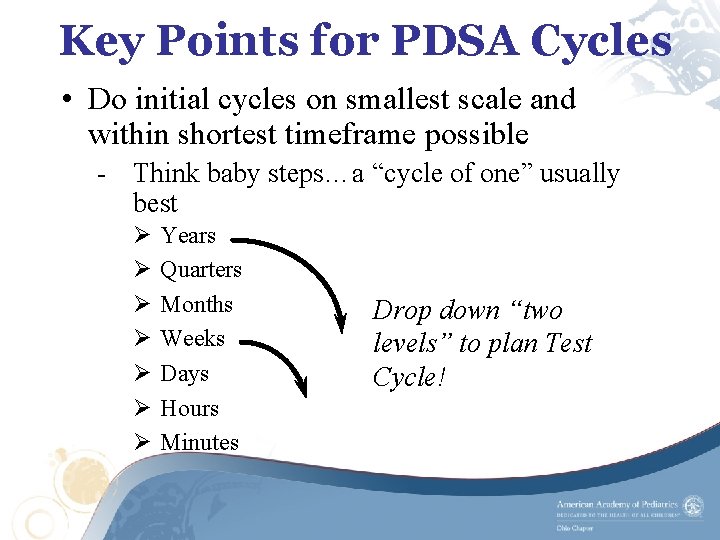
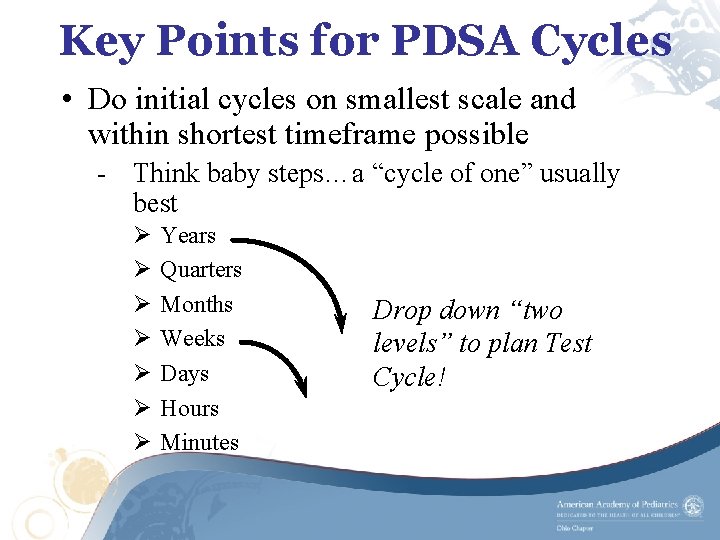
Key Points for PDSA Cycles • Do initial cycles on smallest scale and within shortest timeframe possible - Think baby steps…a “cycle of one” usually best Ø Ø Ø Ø Years Quarters Months Weeks Days Hours Minutes Drop down “two levels” to plan Test Cycle!
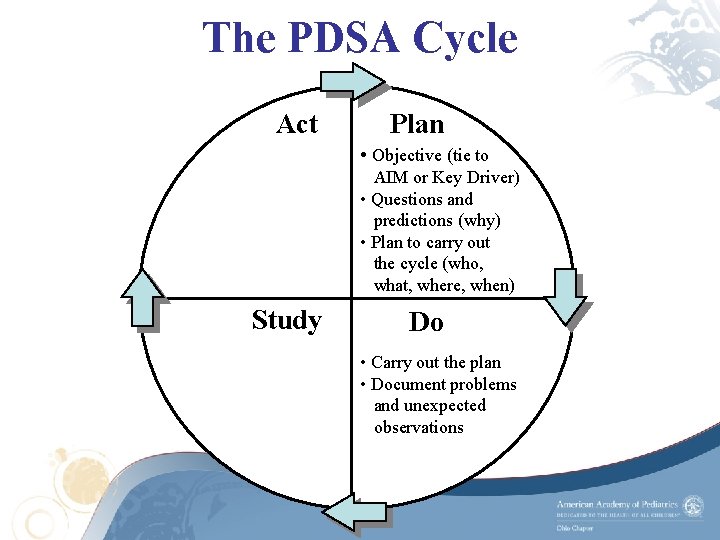
The PDSA Cycle Act Plan • Objective (tie to AIM or Key Driver) • Questions and predictions (why) • Plan to carry out the cycle (who, what, where, when) Study Do • Carry out the plan • Document problems and unexpected observations
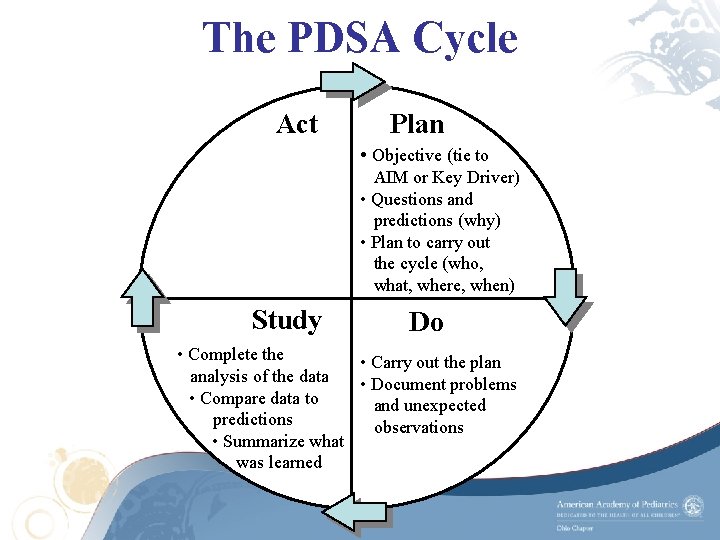
The PDSA Cycle Act Plan • Objective (tie to AIM or Key Driver) • Questions and predictions (why) • Plan to carry out the cycle (who, what, where, when) Study Do • Complete the • Carry out the plan analysis of the data • Document problems • Compare data to and unexpected predictions observations • Summarize what was learned
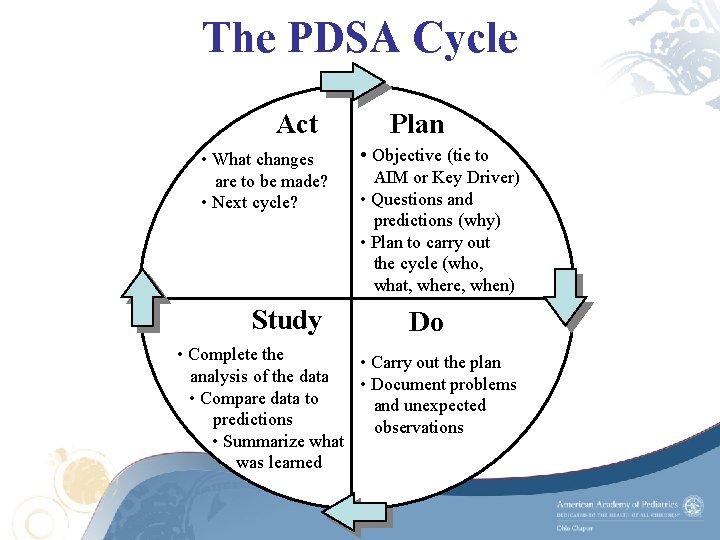
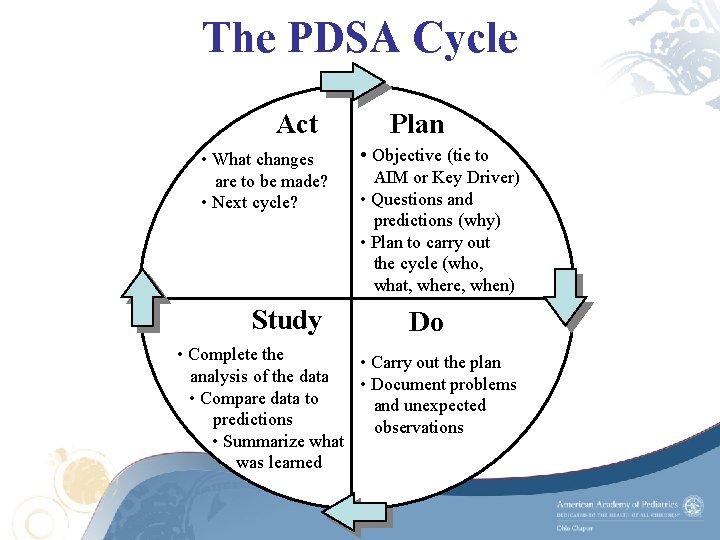
The PDSA Cycle Act • What changes are to be made? • Next cycle? Study Plan • Objective (tie to AIM or Key Driver) • Questions and predictions (why) • Plan to carry out the cycle (who, what, where, when) Do • Complete the • Carry out the plan analysis of the data • Document problems • Compare data to and unexpected predictions observations • Summarize what was learned
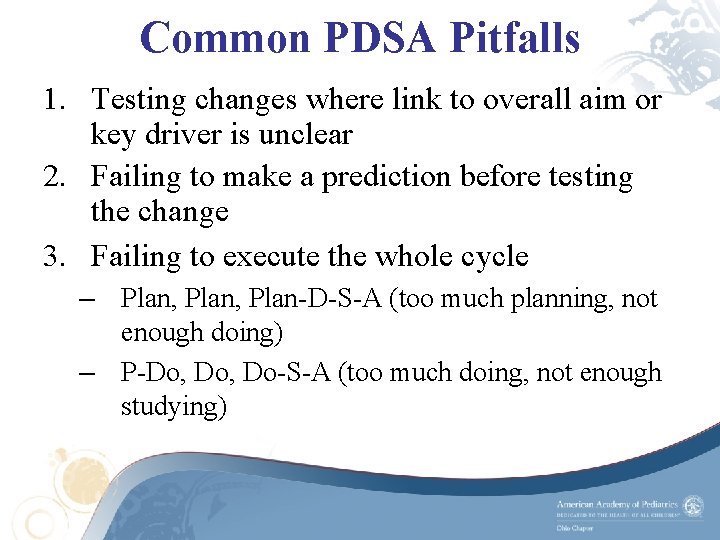
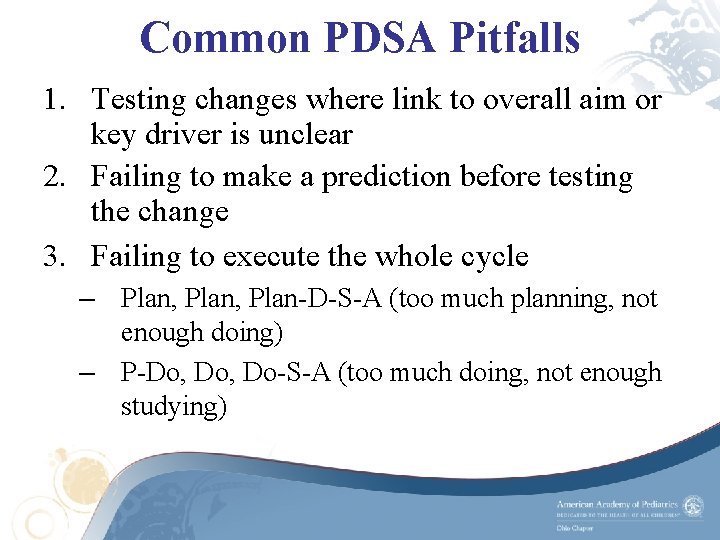
Common PDSA Pitfalls 1. Testing changes where link to overall aim or key driver is unclear 2. Failing to make a prediction before testing the change 3. Failing to execute the whole cycle – Plan, Plan-D-S-A (too much planning, not enough doing) – P-Do, Do-S-A (too much doing, not enough studying)
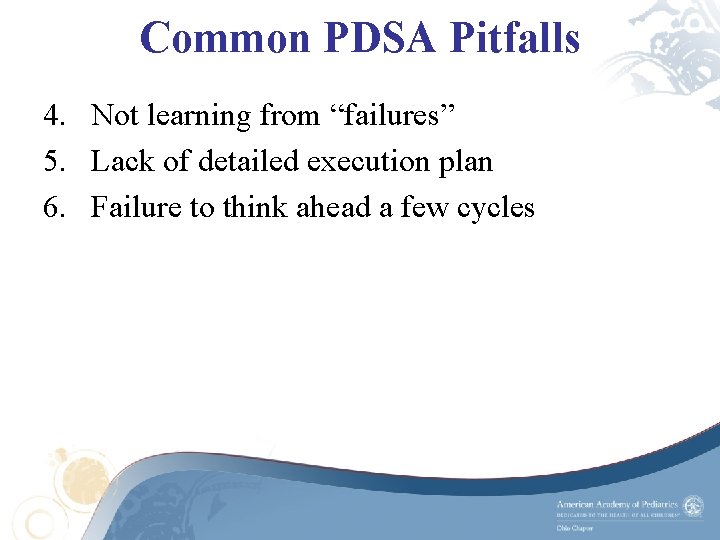
Common PDSA Pitfalls 4. Not learning from “failures” 5. Lack of detailed execution plan 6. Failure to think ahead a few cycles
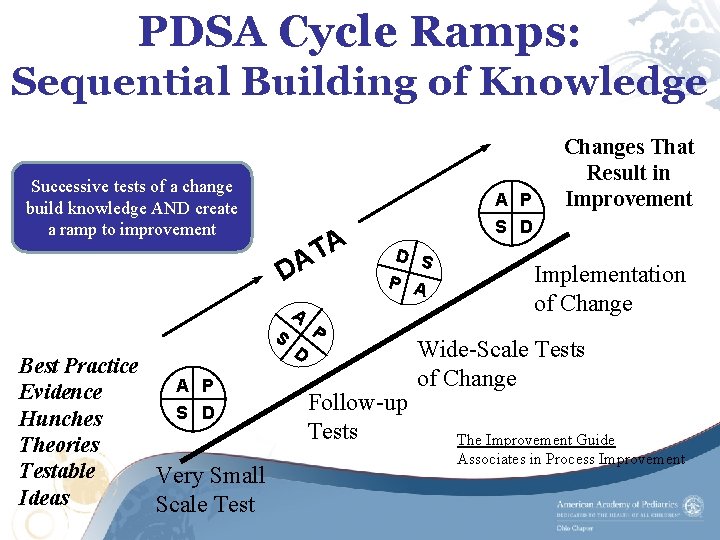
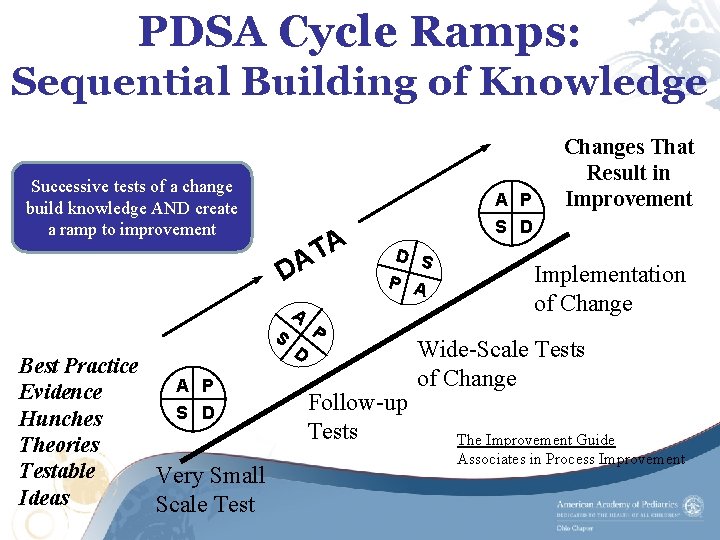
PDSA Cycle Ramps: Sequential Building of Knowledge Successive tests of a change build knowledge AND create a ramp to improvement A P A T A D A S Best Practice A P Evidence S D Hunches Theories Testable Very Small Ideas Scale Test Changes That Result in Improvement S D D S P A P D Follow-up Tests Implementation of Change Wide-Scale Tests of Change The Improvement Guide Associates in Process Improvement
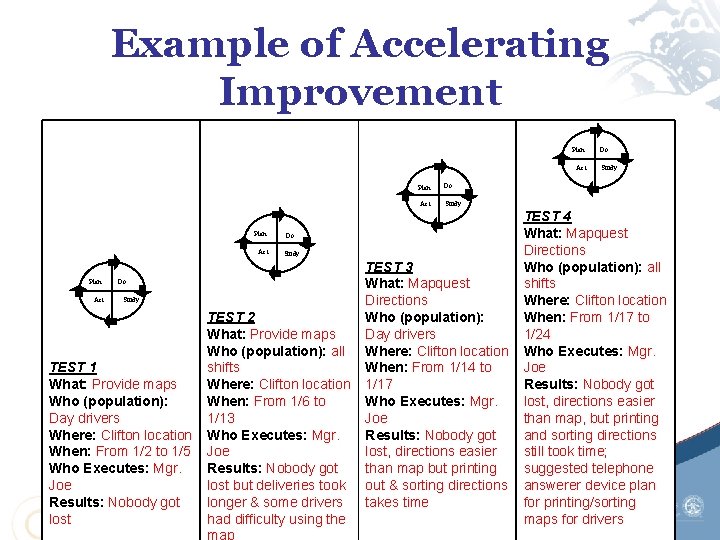
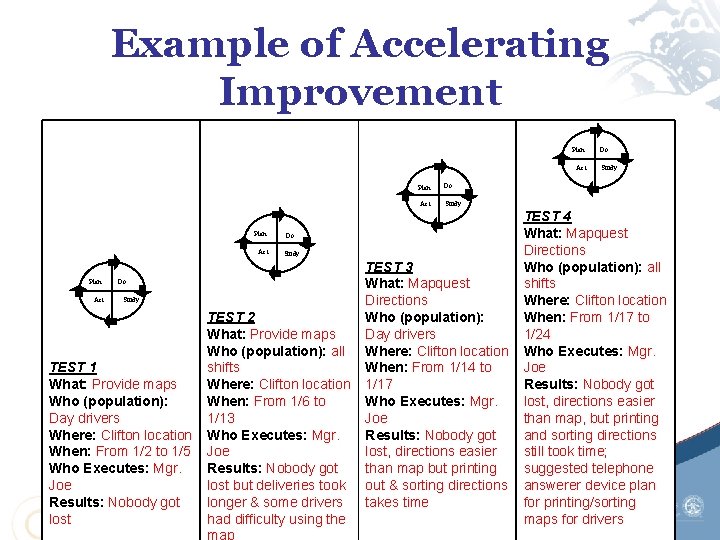
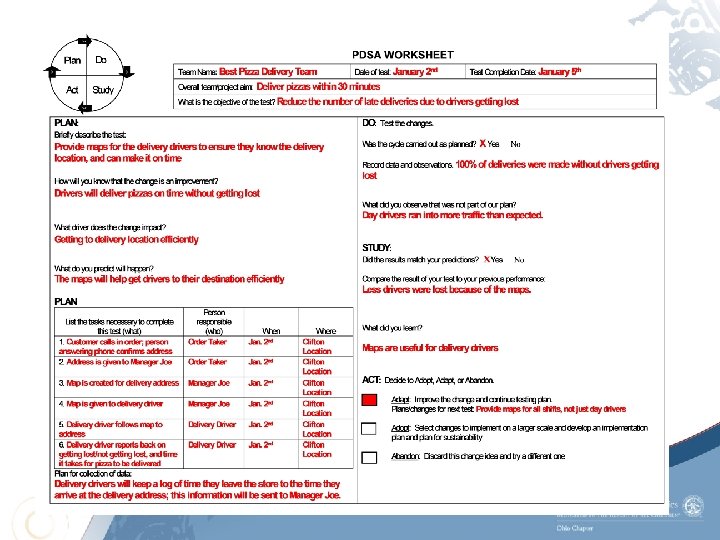
Example of Accelerating Improvement Plan Act TEST 1 What: Provide maps Who (population): Day drivers Where: Clifton location When: From 1/2 to 1/5 Who Executes: Mgr. Joe Results: Nobody got lost Study TEST 2 What: Provide maps Who (population): all shifts Where: Clifton location When: From 1/6 to 1/13 Who Executes: Mgr. Joe Results: Nobody got lost but deliveries took longer & some drivers had difficulty using the Study Do Do TEST 3 What: Mapquest Directions Who (population): Day drivers Where: Clifton location When: From 1/14 to 1/17 Who Executes: Mgr. Joe Results: Nobody got lost, directions easier than map but printing out & sorting directions takes time TEST 4 What: Mapquest Directions Who (population): all shifts Where: Clifton location When: From 1/17 to 1/24 Who Executes: Mgr. Joe Results: Nobody got lost, directions easier than map, but printing and sorting directions still took time; suggested telephone answerer device plan for printing/sorting maps for drivers
“All improvements requires change, but not every change is improvement. ” The Improvement Guide, 2009

Quality Improvement Videos • The Model for Improvement: http: //www. youtube. com/watch? v=SCYgh xtio. IY • PDSA Cycles: http: //www. youtube. com/watch? v=_ce. S 9 Ta 820&feature=youtu. be
References Fuller, S. (2010). Model for Improvement. Power. Point slides Griffin, F. (2004). The PDSA Cycle Testing and Implementing Changes. Retrieved from: www. njha. com/qualityinstitute/pdf/628200432756 PM 63. ppt · PPT file Langley, G. , Moen, R. , Nolan, K. , Nolan T. , Norman, Provost, L. (2009). The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2 nd edition. Jossey-Bass Publishers. , San Francisco. Moen, R. and Norman, C. (2010). Circling back clearing up myths about the Deming cycle and seeing how it keeps evolving. Retrieved from www. qualityprogress. com NHS Institute for Innovation and Improvement. Quality and Service Improvement Tools: PDSA. Retrieved fromhttp: //www. institute. nhs. uk/quality_and_service_improvement_tools/quality_and_service_improvement _tools/plan_do_study_act. html Provost, L. , Murray, S. (2011). The Health Care Data Guide: Learning from data for Improvement. Jossey-Bass Publishers. , San Francisco. Society of Hospital Medicine. Plan-Do- Study- Act. Retrieved from: http: //www. hospitalmedicine. org/Resource. Room. Redesign/CSSSIS/html/06 Reliable/Plan_study. cfm The Model for Improvement National Primary Care Development Team (2004). Retrieved from: www. npdt. org