Quality Improvement Programs and Critical Pathways STRIVE TM



- Slides: 8
Quality Improvement Programs and Critical Pathways STRIVE TM 1

Why Develop Critical Pathways? “A treatment gap between therapy that is dictated by evidence-based medicine and therapy that occurs in practice is not a deficit of knowledge; rather, it is a deficit of implementation. ” Sidney Smith, MD Director, Center for Cardiovascular Science and Medicine, UNC School of Medicine STRIVE TM 2

Critical Pathways l l l l l Standardized treatment protocols for the management of specific disorders Developed to optimize and streamline patient care Prevent underutilization of medications, time in ICU/hospital, costs Ensure quality-of-care measures (eg, door-to-drug times) Optimize patient triage Facilitate communication with specialists and PCP post-discharge Enhance patient compliance and outcomes Minimize potential for medical errors Improve compliance with national standards (JCAHO) Adapted from: Cannon CP, O’Gara PT. Critical Pathways in Cardiology. Lippincott Williams & Wilkins; 2001. STRIVE TM 3
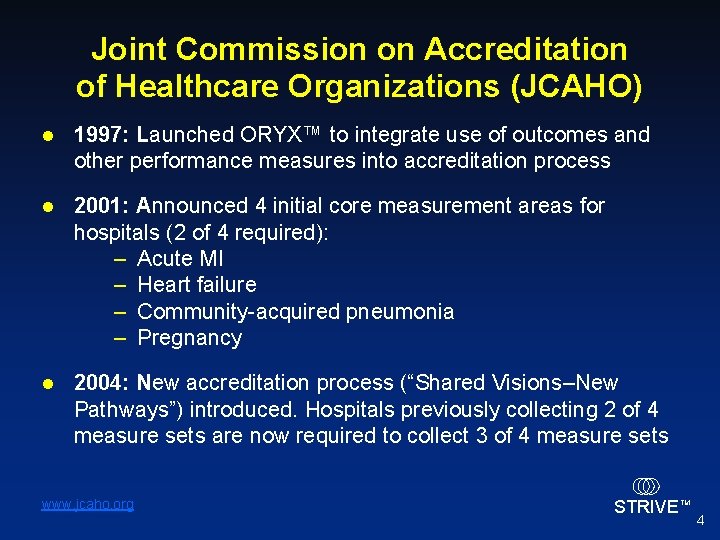
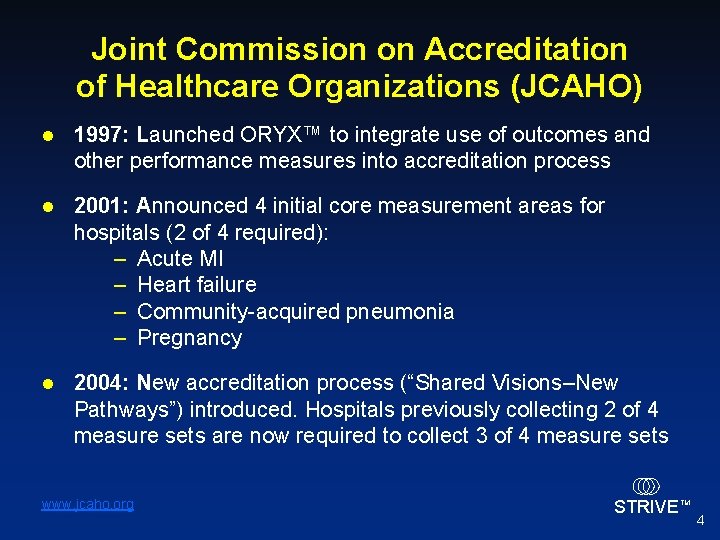
Joint Commission on Accreditation of Healthcare Organizations (JCAHO) l 1997: Launched ORYX™ to integrate use of outcomes and other performance measures into accreditation process l 2001: Announced 4 initial core measurement areas for hospitals (2 of 4 required): – Acute MI – Heart failure – Community-acquired pneumonia – Pregnancy l 2004: New accreditation process (“Shared Visions–New Pathways”) introduced. Hospitals previously collecting 2 of 4 measure sets are now required to collect 3 of 4 measure sets www. jcaho. org STRIVE TM 4
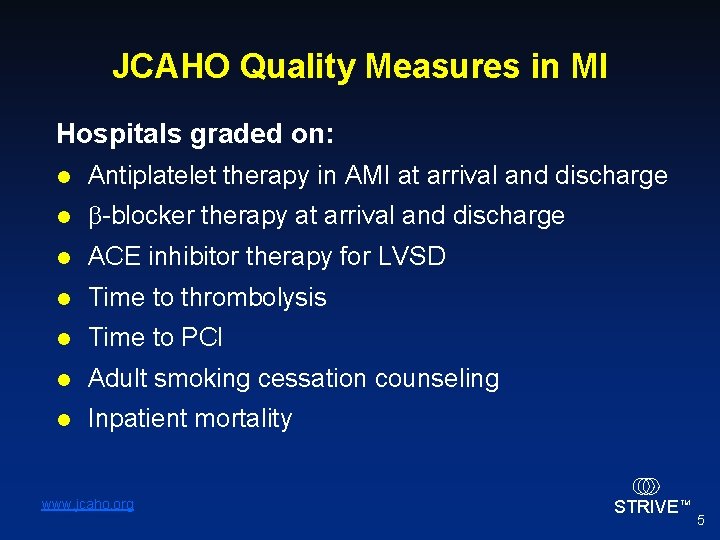
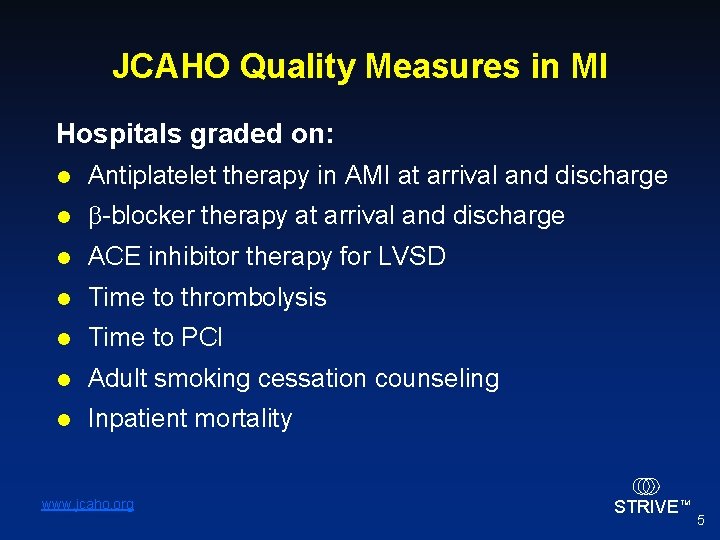
JCAHO Quality Measures in MI Hospitals graded on: l Antiplatelet therapy in AMI at arrival and discharge l b-blocker therapy at arrival and discharge l ACE inhibitor therapy for LVSD l Time to thrombolysis l Time to PCI l Adult smoking cessation counseling l Inpatient mortality www. jcaho. org STRIVE TM 5
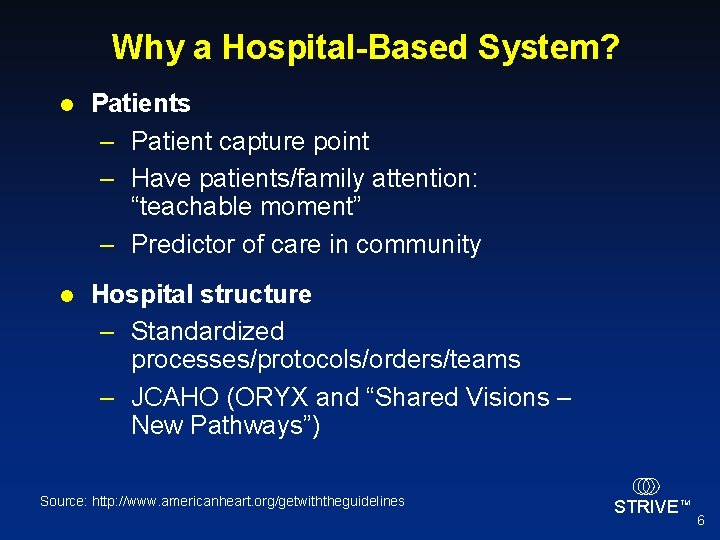
Why a Hospital-Based System? l Patients – Patient capture point – Have patients/family attention: “teachable moment” – Predictor of care in community l Hospital structure – Standardized processes/protocols/orders/teams – JCAHO (ORYX and “Shared Visions – New Pathways”) Source: http: //www. americanheart. org/getwiththeguidelines STRIVE TM 6
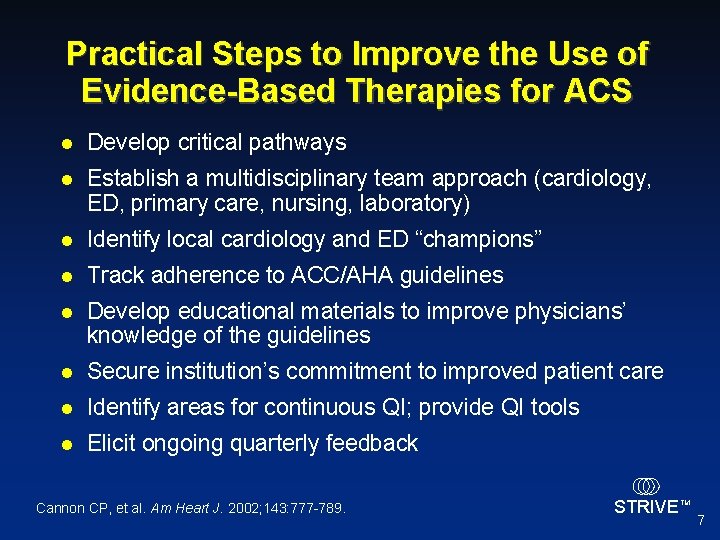
Practical Steps to Improve the Use of Evidence-Based Therapies for ACS l Develop critical pathways l Establish a multidisciplinary team approach (cardiology, ED, primary care, nursing, laboratory) l Identify local cardiology and ED “champions” l Track adherence to ACC/AHA guidelines l Develop educational materials to improve physicians’ knowledge of the guidelines l Secure institution’s commitment to improved patient care l Identify areas for continuous QI; provide QI tools l Elicit ongoing quarterly feedback Cannon CP, et al. Am Heart J. 2002; 143: 777 -789. STRIVE TM 7

Critical Pathways Begin in Ambulance and Extend to Long-term, Office-based Care EMS ED Community Inpatient Discharge Adapted from Cannon CP, O’Gara PT. Critical Pathways in Cardiology. Lippincott Williams & Wilkins; 2001. Corbelli J, et al. Critical Pathways in Cardiology. 2003; 2: 71 -87. STRIVE TM 8