Quality Improvement Organization QIO Update on the 11




- Slides: 65
Quality Improvement Organization (QIO): Update on the 11 Scope of Work (So. W) and Plans for the 12 So. W August 22, 2017
Presentation Objectives Overview of the Quality Innovation Network Quality Improvement Organization’s (QIN-QIO’s) current work Understand potential plans for the QIN-QIO’s 12 So. W Centers for Medicare & Medicaid Services (CMS) Strategic Goals 2

What is a Quality Improvement Organization? Funded by CMS – Dedicated to improving health quality at the community level – Ensures people with Medicare and Medicaid get the care they deserve – Improves care for everyone – Largest federal program dedicated to improving health quality at the community level 3 Department of Health & Human Services CMS
The QIO Program • 1982—Congress established the Medicare Professional Standards Review Organization (PSRO) • Initially, primary activity was utilization review • Late 1980 s—Focus shifted to quality of care, Peer Review Organization (PRO) • 1992—Focus shifted again to collaborative, communitybased quality improvement • 2002—Changed from PRO to QIO • 2014—Quality Innovation Network (QIN)-QIO and Beneficiary and Family-Centered Care (BFCC)-QIO 4
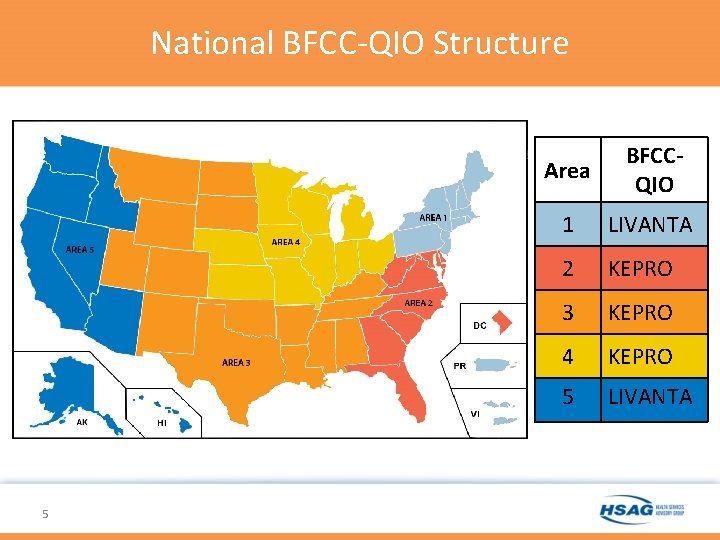
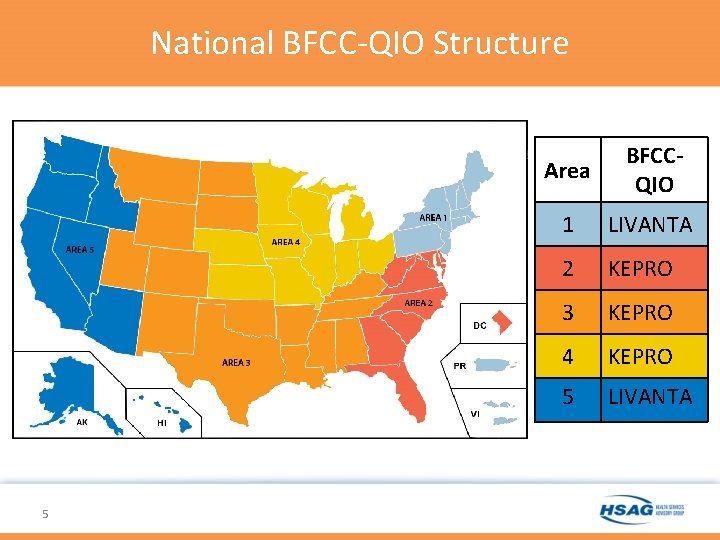
National BFCC-QIO Structure 5 Area BFCCQIO 1 LIVANTA 2 KEPRO 3 KEPRO 4 KEPRO 5 LIVANTA
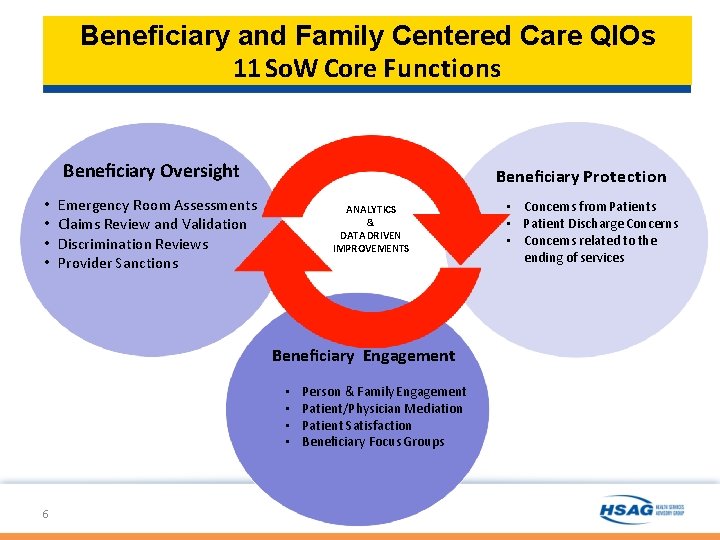
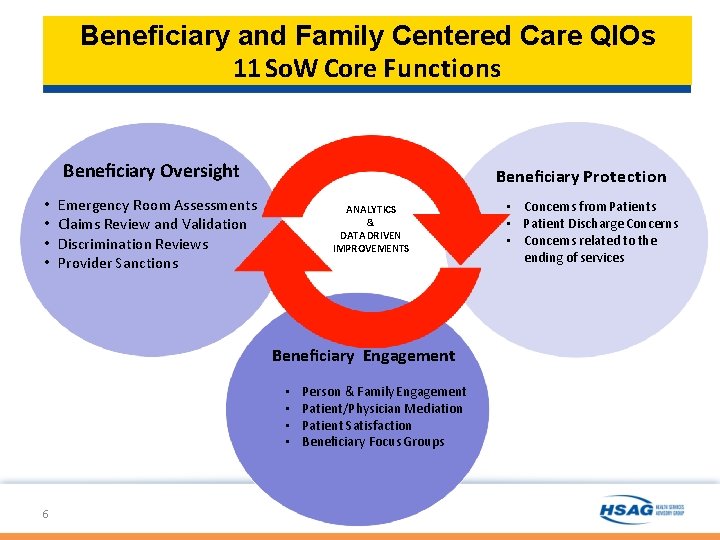
Beneficiary and Family Centered Care QIOs 11 So. W Core Functions Beneficiary Oversight • • Beneficiary Protection Emergency Room Assessments Claims Review and Validation Discrimination Reviews Provider Sanctions ANALYTICS & DATA DRIVEN IMPROVEMENTS Beneficiary Engagement • • 6 Person & Family Engagement Patient/Physician Mediation Patient Satisfaction Beneficiary Focus Groups • Concerns from Patients • Patient Discharge Concerns • Concerns related to the ending of services
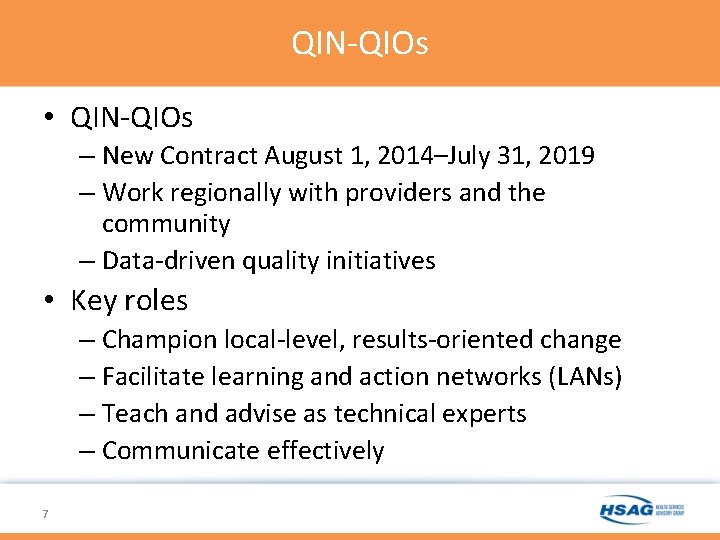
QIN-QIOs • QIN-QIOs – New Contract August 1, 2014–July 31, 2019 – Work regionally with providers and the community – Data-driven quality initiatives • Key roles – Champion local-level, results-oriented change – Facilitate learning and action networks (LANs) – Teach and advise as technical experts – Communicate effectively 7
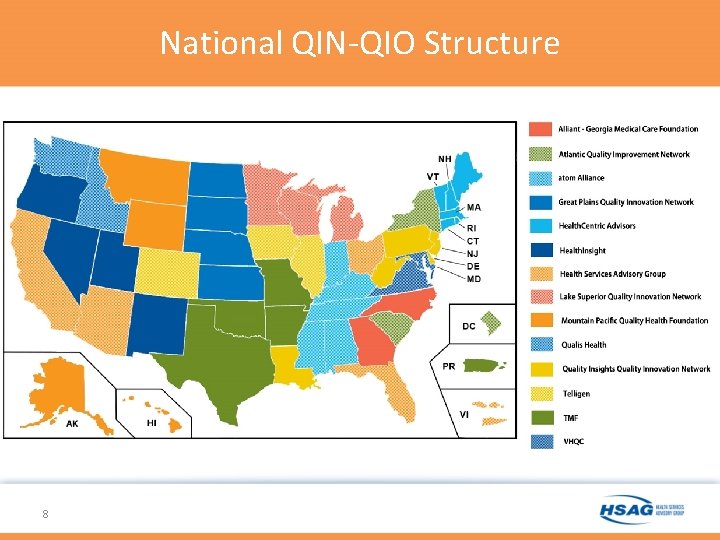
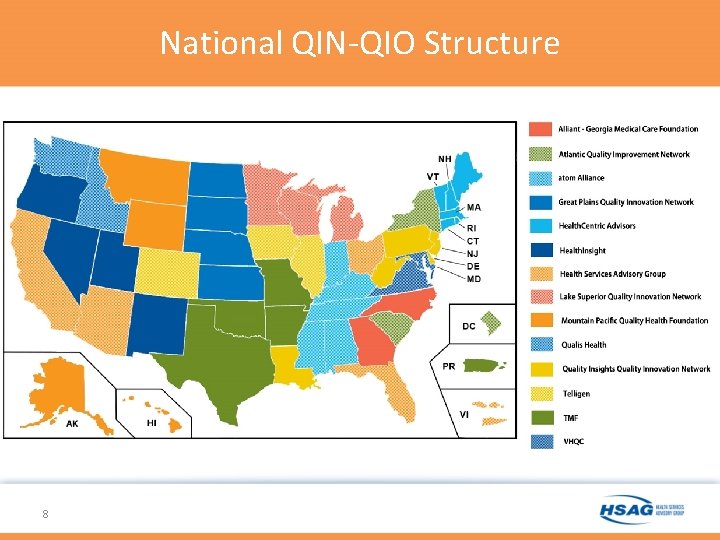
National QIN-QIO Structure 8
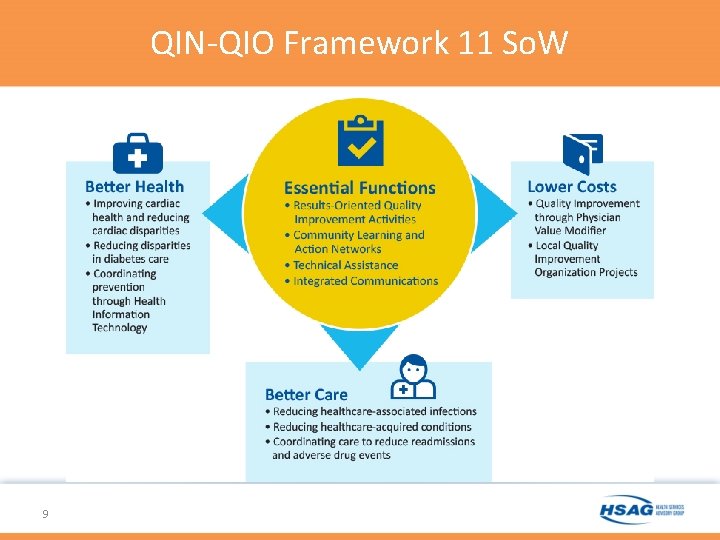
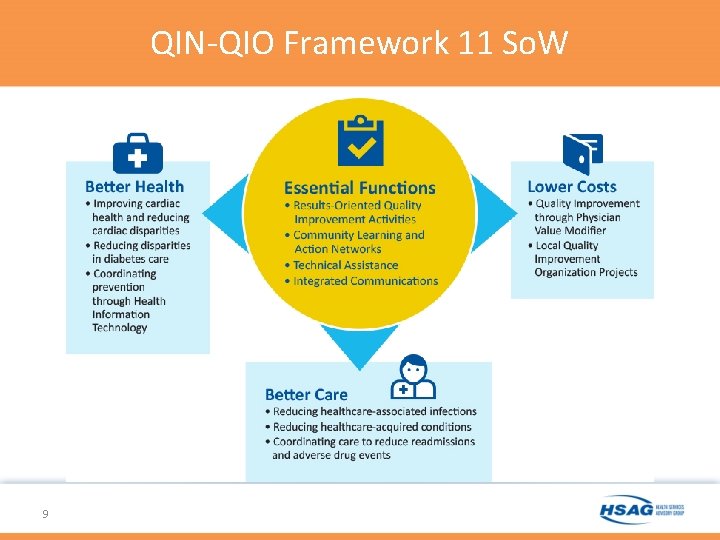
QIN-QIO Framework 11 So. W 9
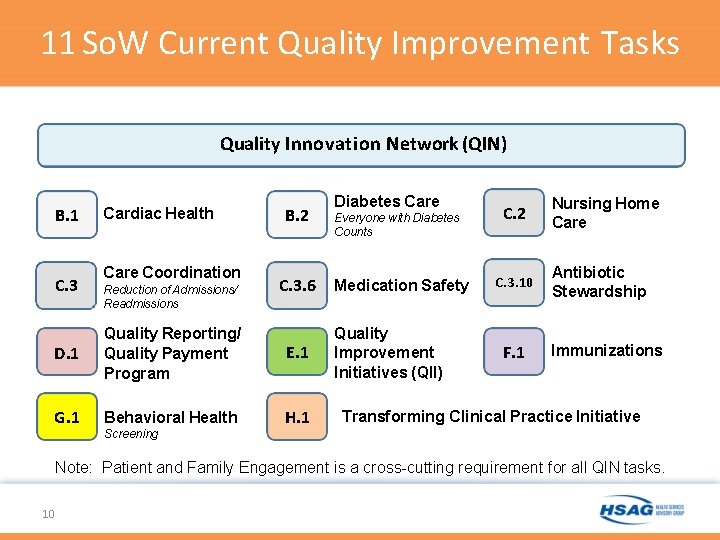
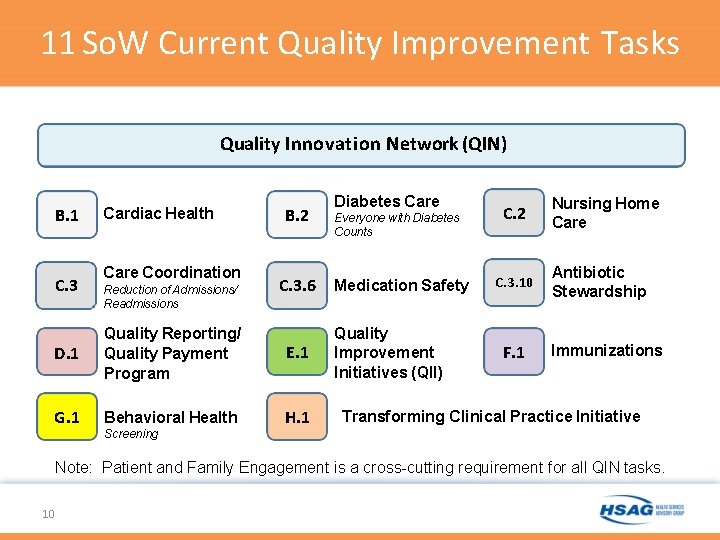
11 So. W Current Quality Improvement Tasks Quality Innovation Network (QIN) B. 1 C. 3 Cardiac Health Care Coordination Reduction of Admissions/ Readmissions B. 2 C. 3. 6 D. 1 Quality Reporting/ Quality Payment Program E. 1 G. 1 Behavioral Health H. 1 Screening Diabetes Care Everyone with Diabetes Counts Medication Safety Quality Improvement Initiatives (QII) C. 2 C. 3. 10 F. 1 Nursing Home Care Antibiotic Stewardship Immunizations Transforming Clinical Practice Initiative Note: Patient and Family Engagement is a cross-cutting requirement for all QIN tasks. 10
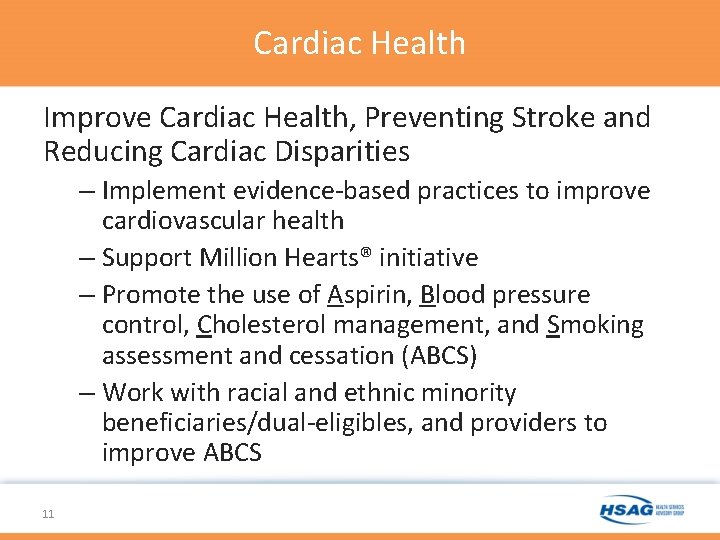
Cardiac Health Improve Cardiac Health, Preventing Stroke and Reducing Cardiac Disparities – Implement evidence-based practices to improve cardiovascular health – Support Million Hearts® initiative – Promote the use of Aspirin, Blood pressure control, Cholesterol management, and Smoking assessment and cessation (ABCS) – Work with racial and ethnic minority beneficiaries/dual-eligibles, and providers to improve ABCS 11

Cardiac Health: Physician Practice Focus Support achievement of the Million Hearts® initiative goals ─ Implement evidence-based practices ─ Target ethnic and racial minorities ─ Provide technical assistance for blood pressure control 12 The Million Hearts® word and logo marks, and the Be One in a Million Hearts® slogan and logo marks and associated trade dress are owned by the U. S. Department of Health and Human Services (HHS). Use of these marks does not imply endorsement by HHS. Use of the Marks also does not necessarily imply that the materials have been reviewed or approved by HHS.
Cardiac Health: Home Health Agencies (HHA) Focus QIN-QIOs will be working with HHAs in each state on the following: – HHQI evidence-based practices – Cardiovascular health – Quality improvement www. Home. Health. Quality. org 13
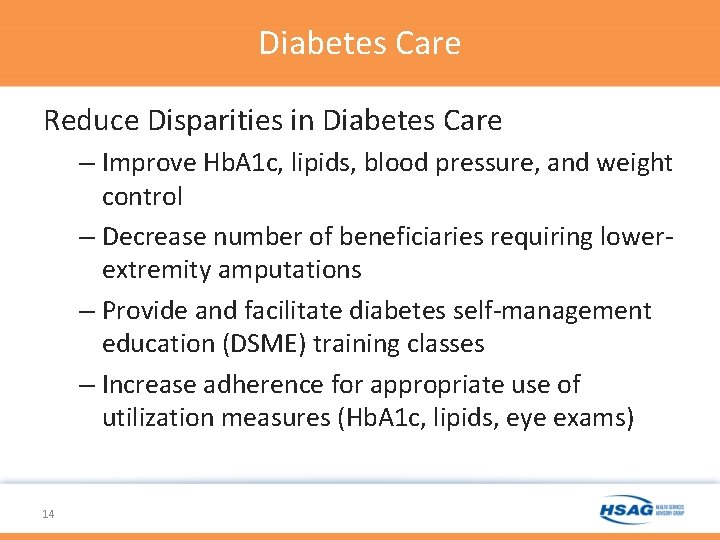
Diabetes Care Reduce Disparities in Diabetes Care – Improve Hb. A 1 c, lipids, blood pressure, and weight control – Decrease number of beneficiaries requiring lowerextremity amputations – Provide and facilitate diabetes self-management education (DSME) training classes – Increase adherence for appropriate use of utilization measures (Hb. A 1 c, lipids, eye exams) 14
Diabetes Care: Self-management Programs • Increase adoption and implementation of DSME – Diabetes Self-Management Program, Stanford University – Project Dulce, Scripps Health Whittier Diabetes Institute – Diabetes Empowerment Education Program (DEEP), University of Illinois at Chicago (UIC) • Train organizations statewide to offer DSME • Provide assistance to organizations offering DSME • Impact more than 64, 660 Medicare beneficiaries with diabetes or pre-diabetes 15

Diabetes Care: Interactive Demonstrations 16
Nursing Home: National Nursing Home Quality Care Collaborative (NNHQCC) • Eliminate healthcare-acquired conditions (HACs) – Achieve score of 6. 0 or lower on the nursing home quality measure composite score by January 2019 – Reduce use of unnecessary antipsychotic medications in residents with dementia – Improve rates of mobility among long-stay NH residents • Eliminate healthcare-associated infections (HAIs) • Instill Quality Assurance and Performance Improvement (QAPI) practices and assist with implementation of QAPI • Improve resident satisfaction • Convene stakeholders, providers, and improvement experts in an “all teach, all learn” model 17
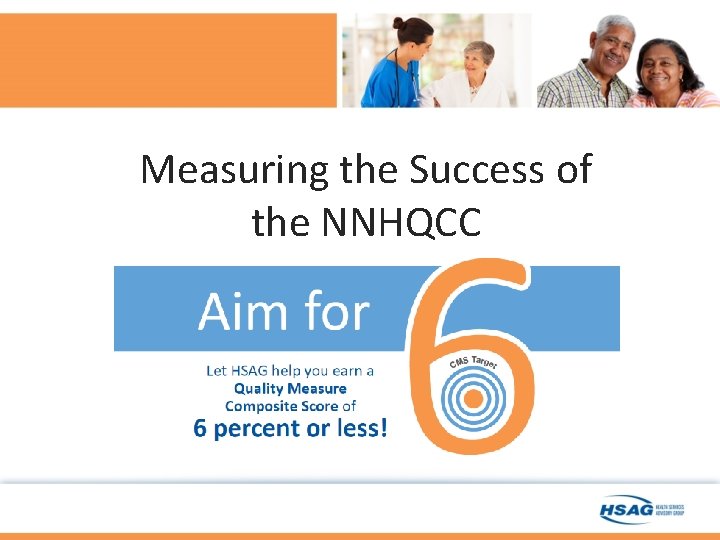
Measuring the Success of the NNHQCC
Nursing Home: Quality Measure (QM) Composite Score The quality measure composite score is comprised of 13 National Quality Forum (NQF) endorsed, long-stay quality measures that represent larger systems within the long-term care (LTC) setting: 1. Percent of residents with one or more falls with major injury 2. Percent of residents with a urinary tract infection (UTI) 3. Percent of residents who self-report moderate to severe pain 4. Percent of high-risk residents with pressure ulcer 5. Percent of low-risk residents with loss of bowels or bladder 6. Percent of residents with catheter inserted or left in bladder 19
Nursing Home: QM Composite Score (cont. ) 7. Percent of residents physically restrained 8. Percent of residents whose need for help with activities of daily living (ADL) has increased 9. Percent of residents who lose too much weight 10. Percent of residents who have depressive symptoms 11. Percent of residents who received antipsychotic medications 12. Percent of residents assessed and appropriately given flu vaccine* 13. Percent of residents assessed and appropriately given pneumococcal vaccine* *The direction of the two vaccination measures should be reversed because they are directionally opposite of the other measures. This is done by subtracting the numerator from the denominator to obtain a “new” numerator. 20
Nursing Home: Clostridium difficile (CDI) Reporting and Reduction Initiative Launched May 2016 – Target 15 percent of nursing homes in each state or 2, 330 nursing homes (NHs). – 16 percent of Florida NNHQCC members, 108 NHs, have joined HSAG and other local and national experts on a new CMS QAPI initiative to prevent and reduce CDI in their nursing homes. – As of October 2016, QIN-QIOs nationally have recruited 2, 999 NHs for the CDI initiative! 21
Nursing Home: CDI Aims • Drive the Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) LTC enrollment and consistent data reporting • Identify a national baseline for CDIs in nursing homes • Prevention through learning, focused on CDI management, antibiotic stewardship principles and practices, and the Agency for Healthcare Research and Quality (AHRQ) Team. STEPPS® LTC Communications Module for uniform communication within and across nursing homes 22 https: //www. ahrq. gov/teamstepps/longtermcare/index. html
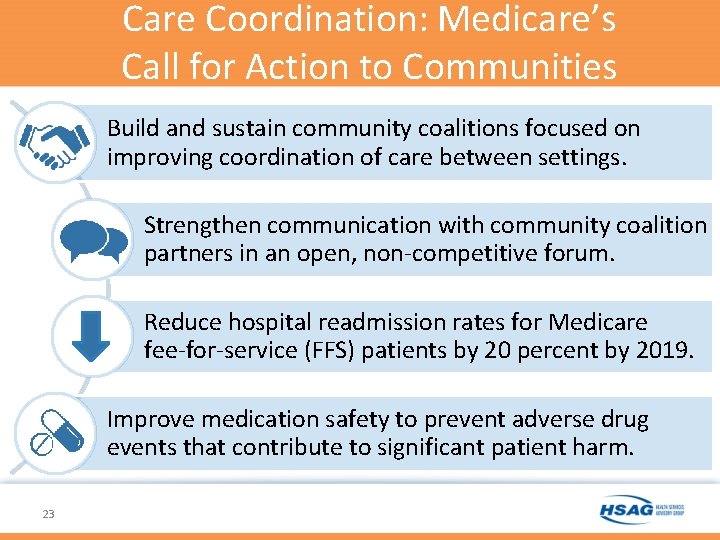
Care Coordination: Medicare’s Call for Action to Communities Build and sustain community coalitions focused on improving coordination of care between settings. Strengthen communication with community coalition partners in an open, non-competitive forum. Reduce hospital readmission rates for Medicare fee-for-service (FFS) patients by 20 percent by 2019. Improve medication safety to prevent adverse drug events that contribute to significant patient harm. 23
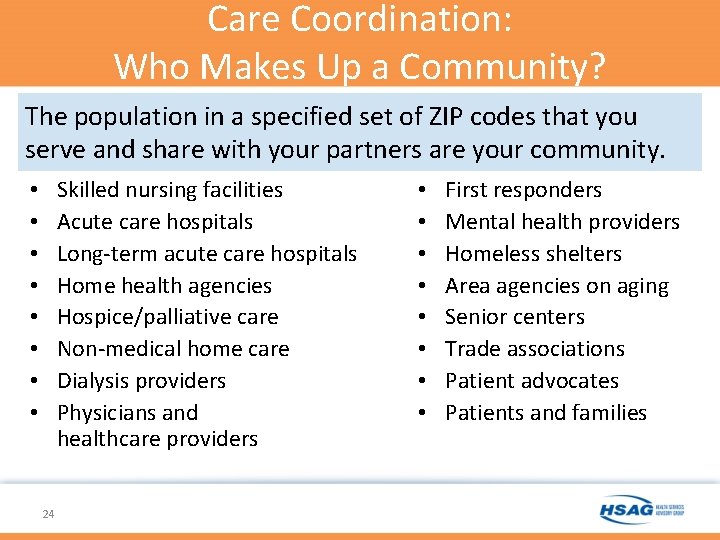
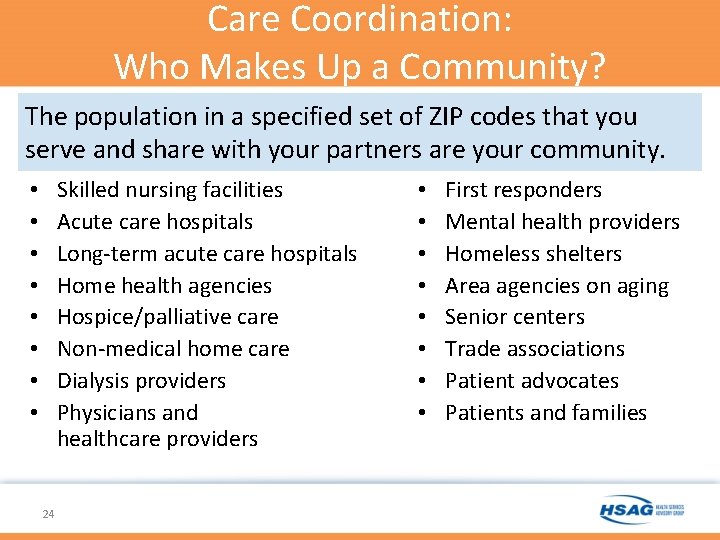
Care Coordination: Who Makes Up a Community? The population in a specified set of ZIP codes that you serve and share with your partners are your community. Skilled nursing facilities Acute care hospitals Long-term acute care hospitals Home health agencies Hospice/palliative care Non-medical home care Dialysis providers Physicians and healthcare providers • • 24 • • First responders Mental health providers Homeless shelters Area agencies on aging Senior centers Trade associations Patient advocates Patients and families
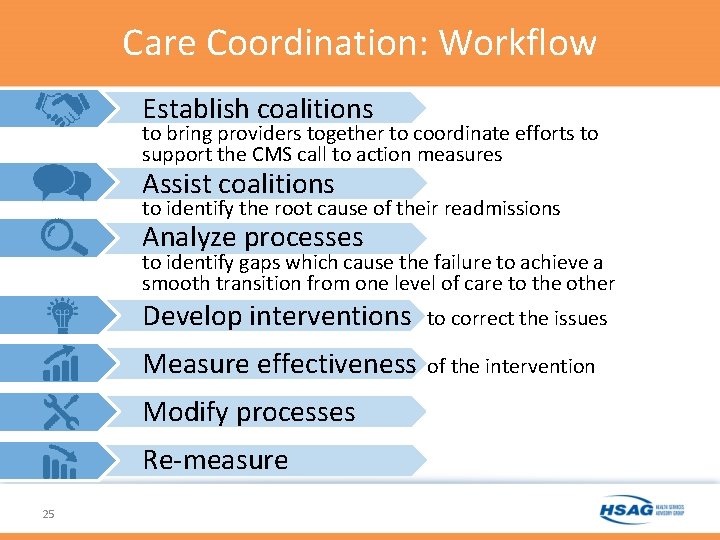
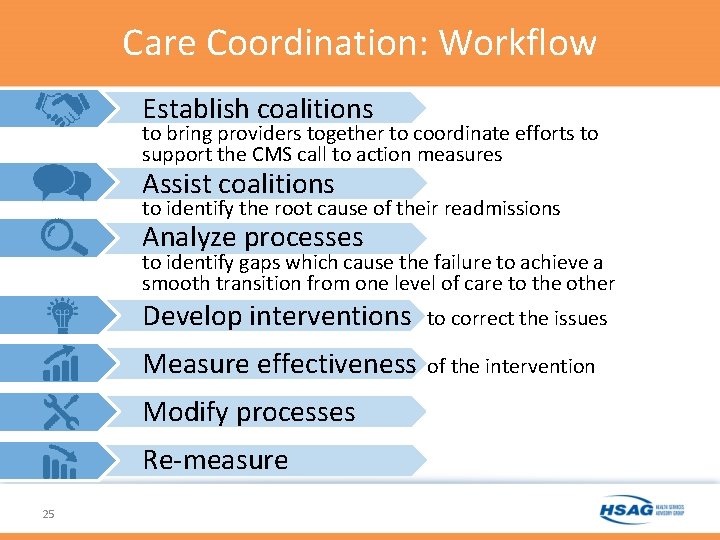
Care Coordination: Workflow Establish coalitions to bring providers together to coordinate efforts to support the CMS call to action measures Assist coalitions to identify the root cause of their readmissions Analyze processes to identify gaps which cause the failure to achieve a smooth transition from one level of care to the other Develop interventions to correct the issues Measure effectiveness of the intervention Modify processes Re-measure 25
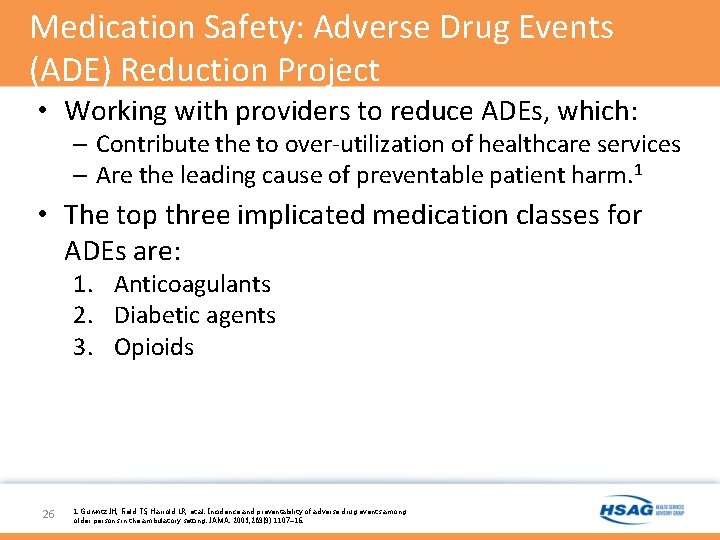
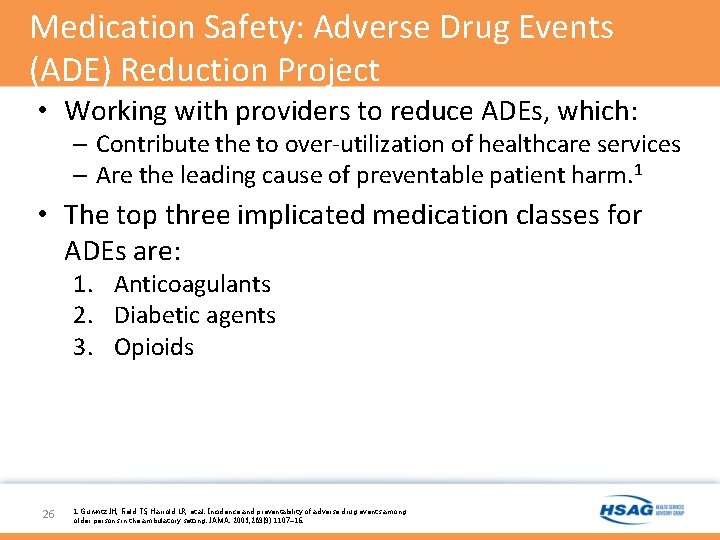
Medication Safety: Adverse Drug Events (ADE) Reduction Project • Working with providers to reduce ADEs, which: – Contribute the to over-utilization of healthcare services – Are the leading cause of preventable patient harm. 1 • The top three implicated medication classes for ADEs are: 1. Anticoagulants 2. Diabetic agents 3. Opioids 26 1. Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003; 289(9): 1107– 16.
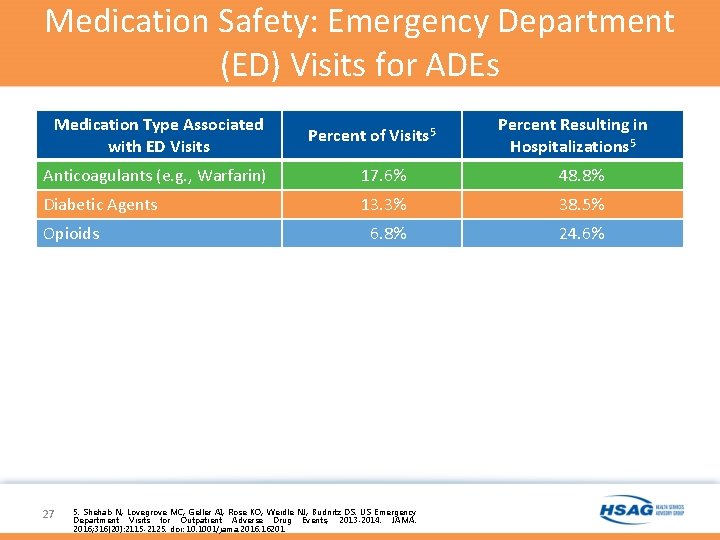
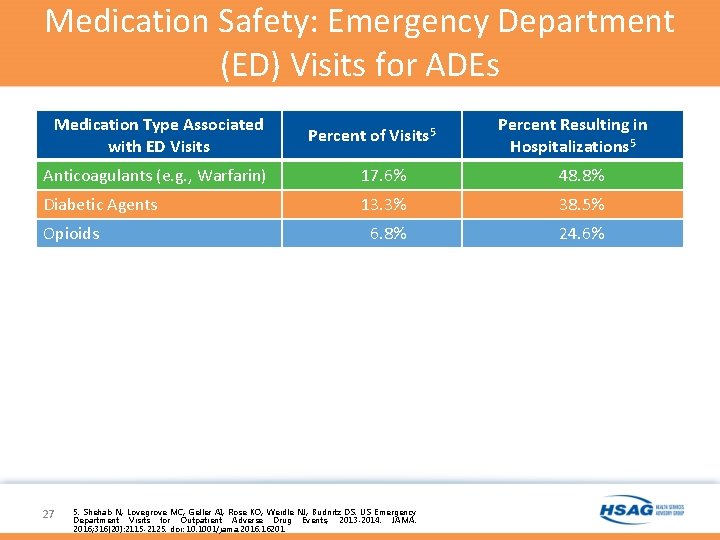
Medication Safety: Emergency Department (ED) Visits for ADEs • ciated with anticoagulants Percent Resulting in Medication Type Associated with ED Visits Hospitalizations • 17. 6% 5 Anticoagulants Warfarin) 48. 8% of(e. g. , cases resulting in 17. 6% hospitalization. 48. 8% Percent of Visits 5 • Associated with 13. 3% diabetic agents 38. 5% 24. 6% Opioids • 13. 3% of the visits, with 6. 8% 38. 5% resulting in hospitalization. 5 • Associated with opioids • 6. 8% of the visits, with 24. 6% resulting in hospitalization. 5 w Diabetic Agents 27 5. Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US Emergency Department Visits for Outpatient Adverse Drug Events, 2013 -2014. JAMA. 2016; 316(20): 2115 -2125. doi: 10. 1001/jama. 2016. 16201. 5
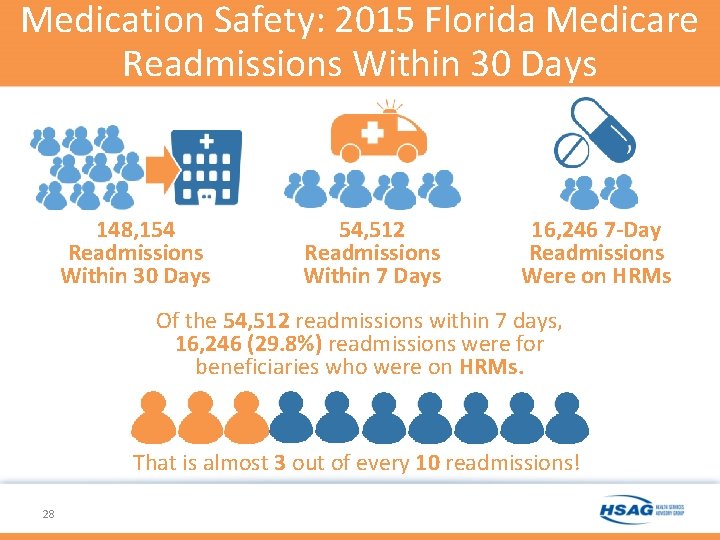
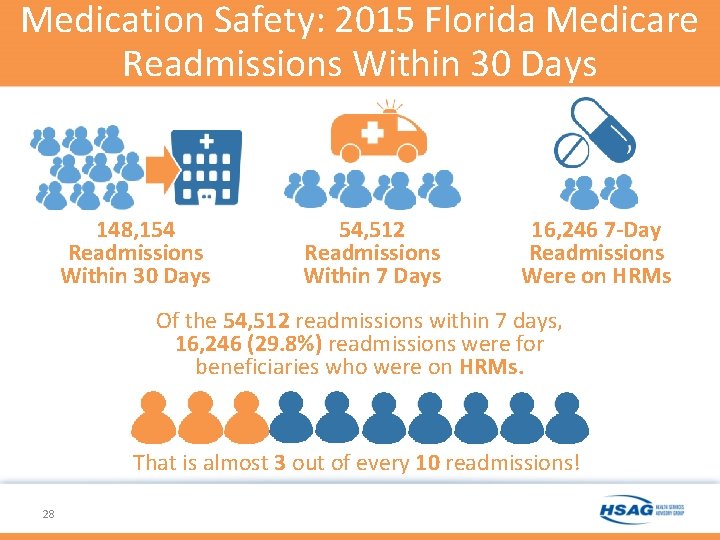
Medication Safety: 2015 Florida Medicare Readmissions Within 30 Days 148, 154 Readmissions Within 30 Days 54, 512 Readmissions Within 7 Days 16, 246 7 -Day Readmissions Were on HRMs Of the 54, 512 readmissions within 7 days, 16, 246 (29. 8%) readmissions were for beneficiaries who were on HRMs. That is almost 3 out of every 10 readmissions! 28
Antibiotic Stewardship: Intended Audiences • • • Dialysis Facilities* Emergency Departments Federally Qualified Health Centers Ambulatory Surgical Centers* Urgent Care Clinics Physician Offices Outpatient Clinics Outpatient Pharmacies and Pharmacy-based Clinics Public Health Clinics * No longer eligible to participate 29
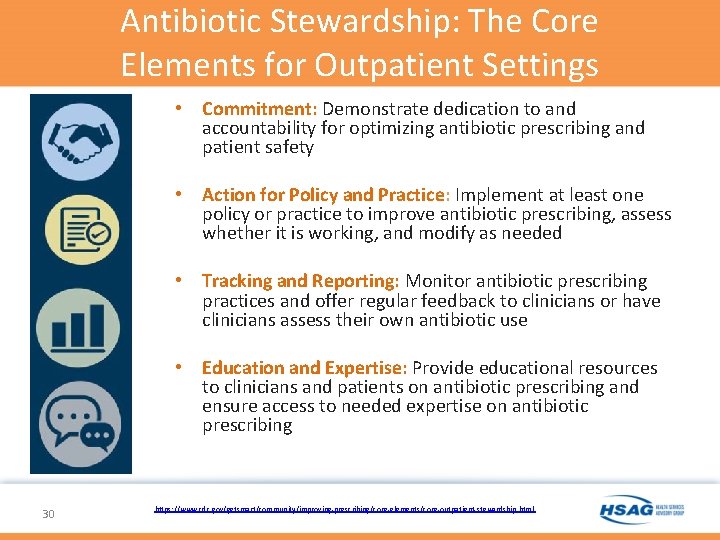
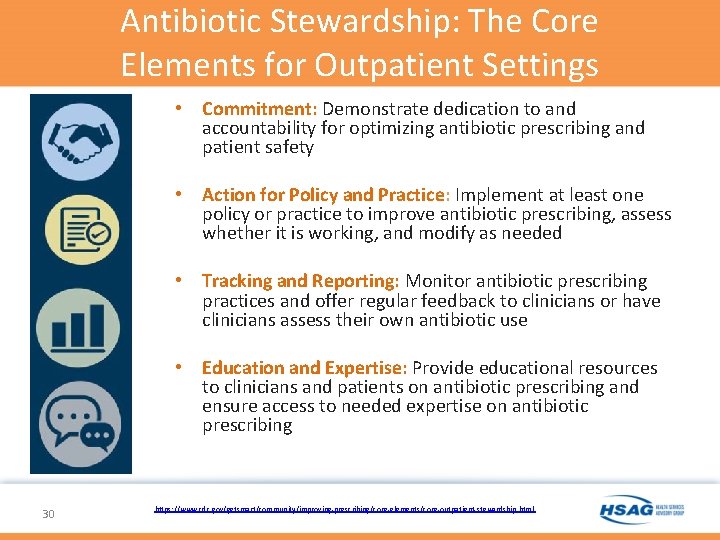
Antibiotic Stewardship: The Core Elements for Outpatient Settings • Commitment: Demonstrate dedication to and accountability for optimizing antibiotic prescribing and patient safety • Action for Policy and Practice: Implement at least one policy or practice to improve antibiotic prescribing, assess whether it is working, and modify as needed • Tracking and Reporting: Monitor antibiotic prescribing practices and offer regular feedback to clinicians or have clinicians assess their own antibiotic use • Education and Expertise: Provide educational resources to clinicians and patients on antibiotic prescribing and ensure access to needed expertise on antibiotic prescribing 30 https: //www. cdc. gov/getsmart/community/improving-prescribing/core-elements/core-outpatient-stewardship. html
Antibiotic Stewardship: Roadmap to Success 31
Quality Reporting Programs and Support of Clinicians in the Quality Payment Program (QPP) Assist the following: 1. Inpatient Hospitals; 2. Outpatient Hospitals; 3. PPS-Exempt Cancer Hospitals (PCHs); 4. Inpatient Psychiatric Facilities (IPFs); 5. Ambulatory Surgical Centers (ASCs); and 6. Eligible Clinicians Improve quality of care and efficiency of care through directed technical assistance, LANs, and outreach and education about CMS value-based payment and quality reporting programs. 32
QPP: Assist Hospitals and Facilities Quality Reporting QIN-QIOs: – Provide technical assistance in improving performance on quality measures – Help interpret and use performance data to drive quality improvement – Analyze performance improvement needs and offer appropriate interventions, tools, and resources – Facilitate networking opportunities with peer facilities for support and best practices – Provide information and resources that show linkages and inter-relationships among multiple quality incentive payment programs – Share successful interventions and improvement efforts related to quality of care and efficiency 33

Quality Payment Program (QPP) Clinician Focus 34
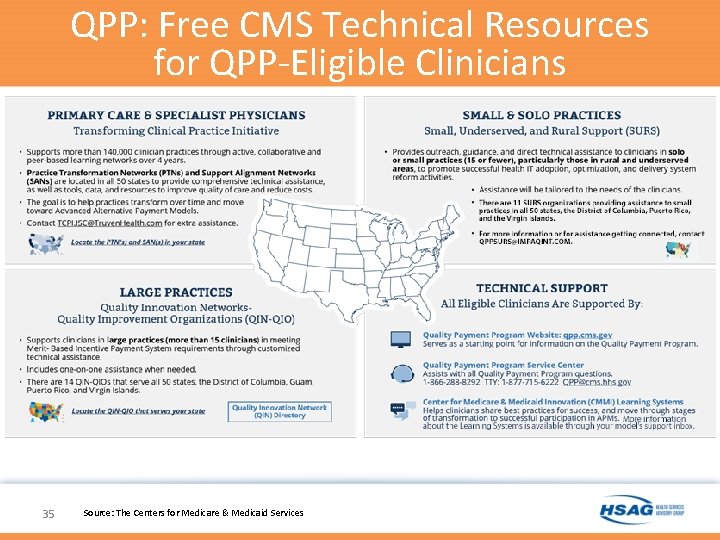
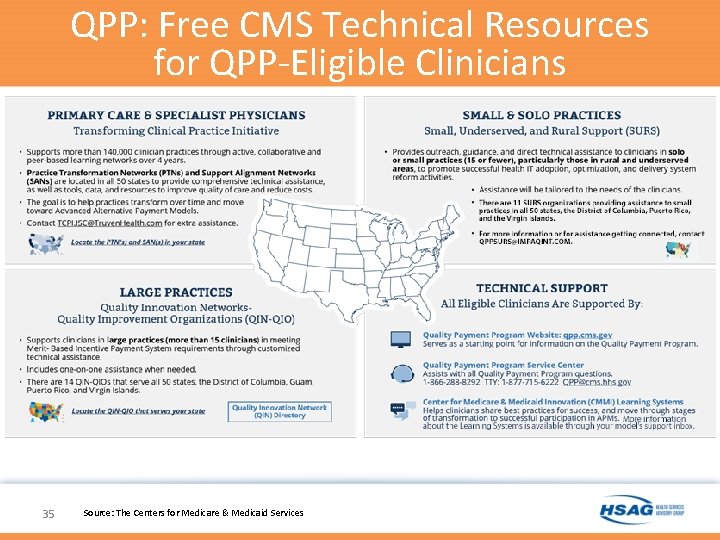
QPP: Free CMS Technical Resources for QPP-Eligible Clinicians 35 Source: The Centers for Medicare & Medicaid Services
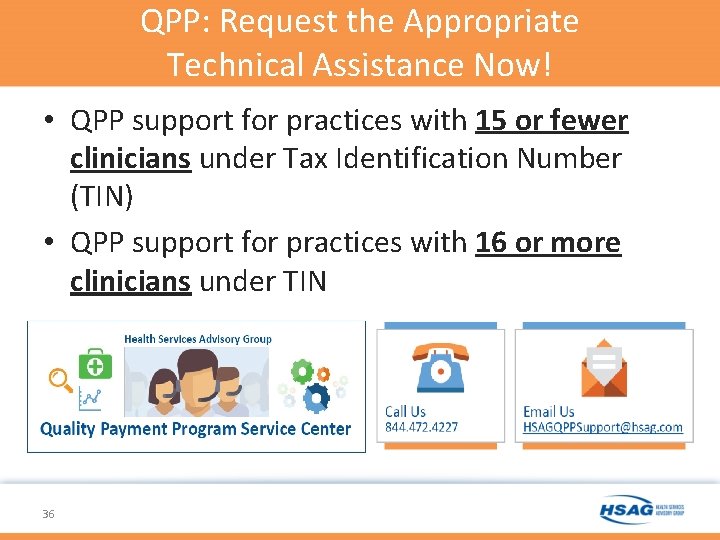
QPP: Request the Appropriate Technical Assistance Now! • QPP support for practices with 15 or fewer clinicians under Tax Identification Number (TIN) • QPP support for practices with 16 or more clinicians under TIN 36
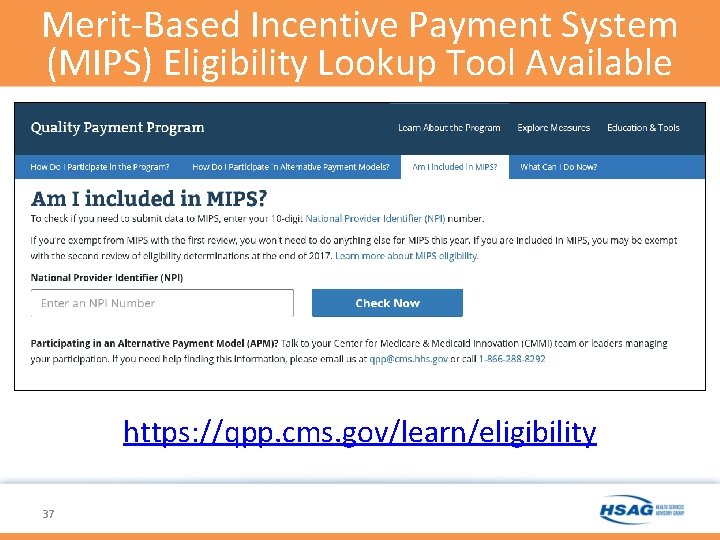
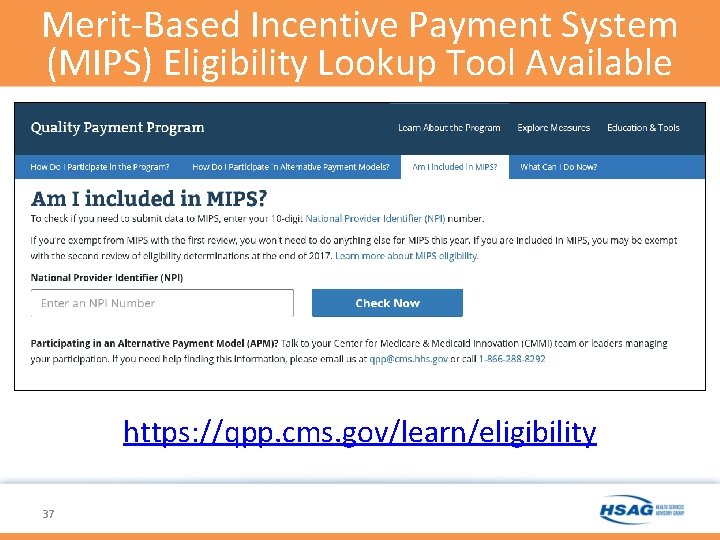
Merit-Based Incentive Payment System (MIPS) Eligibility Lookup Tool Available https: //qpp. cms. gov/learn/eligibility 37
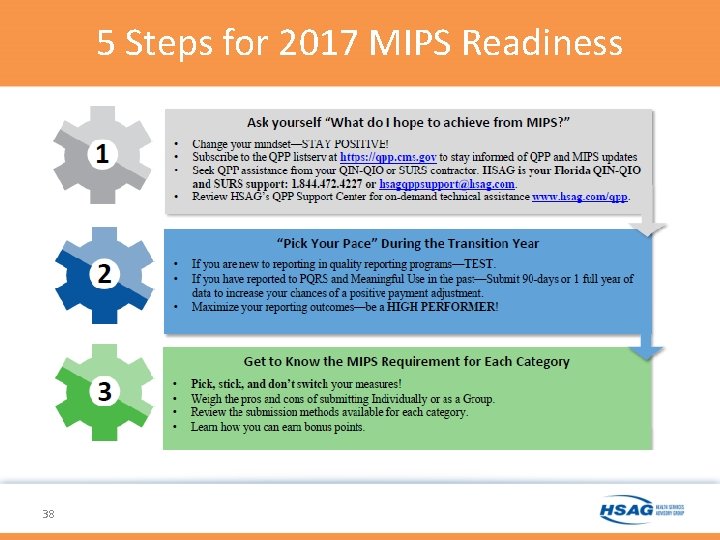
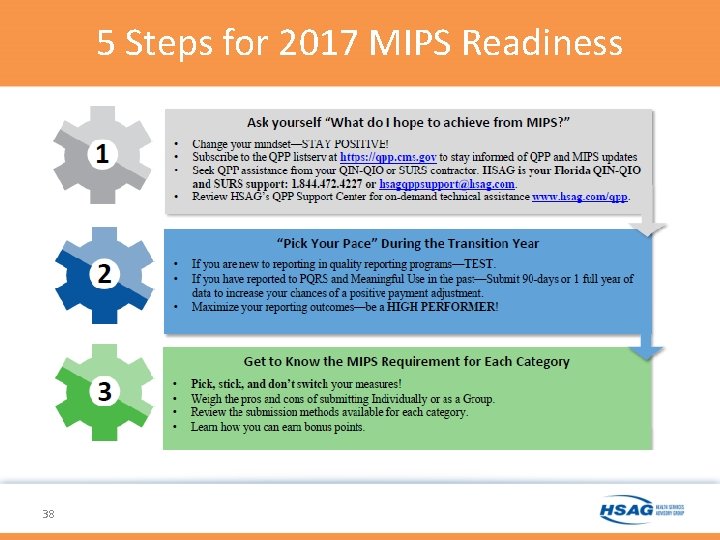
5 Steps for 2017 MIPS Readiness 38
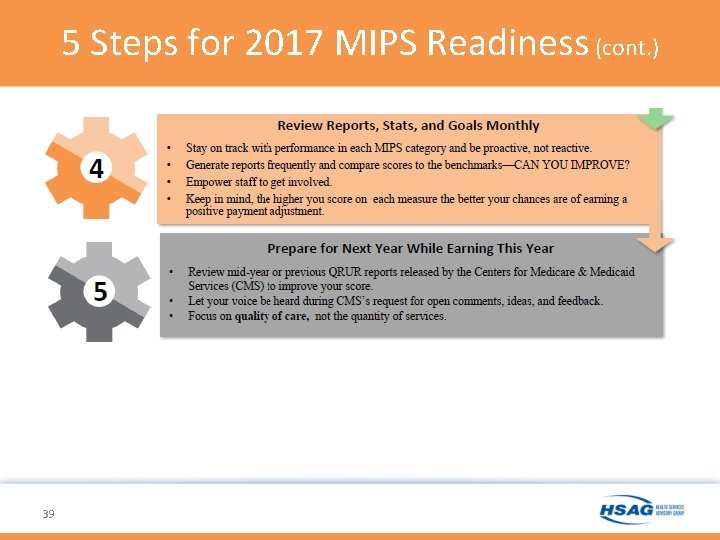
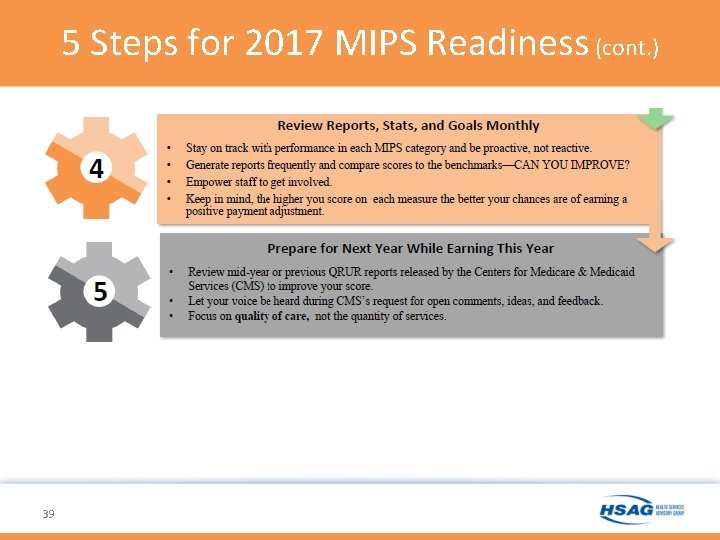
5 Steps for 2017 MIPS Readiness (cont. ) 39
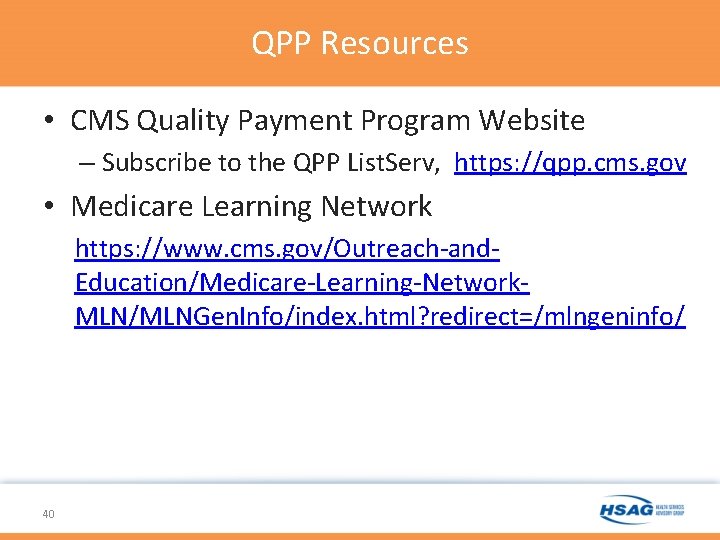
QPP Resources • CMS Quality Payment Program Website – Subscribe to the QPP List. Serv, https: //qpp. cms. gov • Medicare Learning Network https: //www. cms. gov/Outreach-and. Education/Medicare-Learning-Network. MLN/MLNGen. Info/index. html? redirect=/mlngeninfo/ 40
Quality Improvement Initiatives (QII) QIN-QIOs initiate a QII providing technical assistance to providers, physicians, and other practitioners based on receiving a confirmed quality of care concerns from the following: • BFCC-QIOs; • QIN National Coordinating Center (NCC); • Value Incentive and Quality Reporting Center contractors (VIQRs); or • CMS approved sources such as the state survey agencies. 41
QII: Assistance • Develop measureable inventions in collaboration with the provider(s), practitioner(s), or physician practice that address systemic confirmed concerns • Request that the provider and/or practitioner initiate and complete an improvement plan to correct the problem • Post tools and resources used in successful interventions 42
Immunization • In 2013, there were 3, 700 deaths in the U. S. , mostly adults, due to pneumococcal infections. Annually, up to 49, 000 deaths occur due to influenza-related complications around the world, according to the CDC. The Journal of Family Practice • In one study: – “During influenza seasons, influenza vaccination by itself was associated with a 52 percent reduction in hospitalizations for pneumonia and a 70 percent reduction in death. Pneumococcal vaccination by itself was associated with a 27 percent reduction in hospitalizations for pneumonia and a 34 percent reduction in death. Both vaccinations combined resulted in 63 percent reduction in hospitalizations for pneumonia and an 81 percent reduction in death. ” Vaccine 43 Sources: Rockwell, P. , What can you do to improve adult immunization rates, J Fam Pract. , 2015 October; 64(10): 625 -626, 628 -630, 633, available at http: //www. mdedge. com/jfponline/article/103052/infectious-diseases/what-you-can-do-improve-adult-immunization-rates; Nichol, KL, The additive benefits of influenza and pneumococcal vaccinations during influenza seasons among elderly persons with chronic lung disease, Vaccine, 1999 Jul 30; 17 Suppl 1: S 91 -3, available athttps: //www. ncbi. nlm. nih. gov/pubmed/10471189
Immunization: Assistance Workflow assessments and workflow re-designs Building forms and templates Running dashboard reports Data analysis Integration with Immunization Information System (IIS) Immunization Registry • Align across multiple quality improvement (QI) programs • • • 44
Behavioral Health • Primary care physician (PCP) offices – Improving identification of depression – Improving alcohol use disorder • Inpatient psychiatric facilities (IPFs) – Care transitions for behavioral health conditions 45
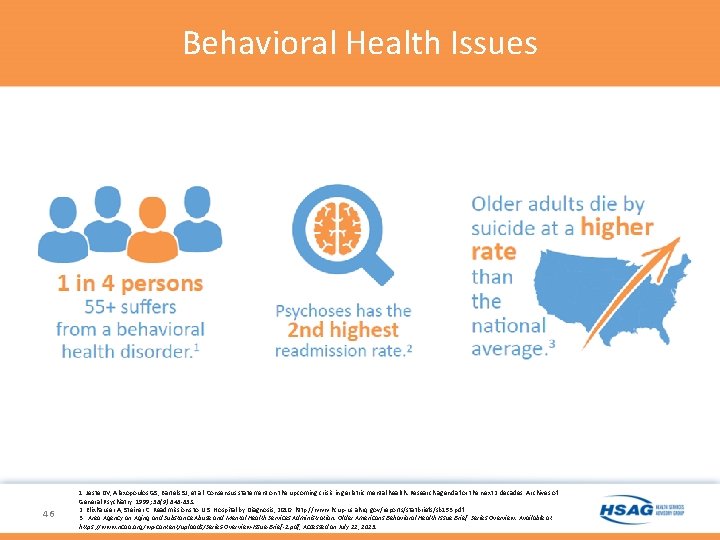
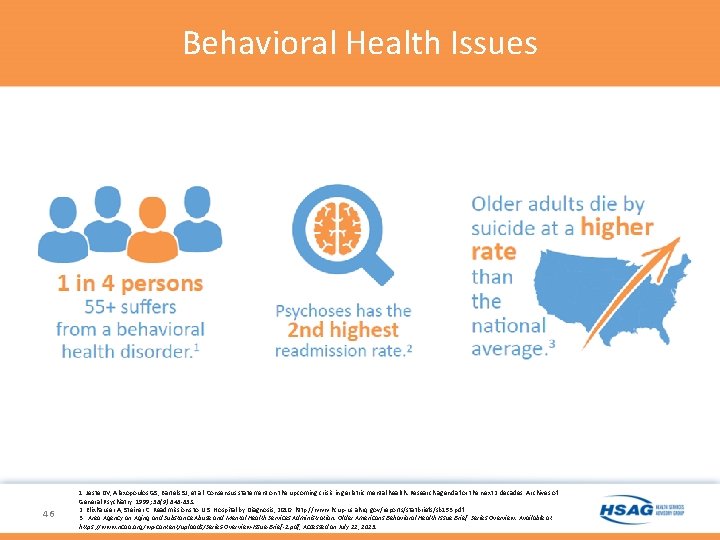
Behavioral Health Issues 46 1. Jeste DV, Alexopoulos GS, Bartels SJ, et al. Consensus statement on the upcoming crisis in geriatric mental health: Research agenda for the next 2 decades. Archives of General Psychiatry. 1999; 56(9): 848 -853. 2. Elixhauser A, Steiner C. Readmissions to U. S. Hospital by Diagnosis, 2010. http: //www. hcup-us. ahrq. gov/reports/statbriefs/sb 153. pdf 3. Area Agency on Aging and Substance Abuse and Mental Health Services Administration. Older Americans Behavioral Health Issue Brief: Series Overview. Available at https: //www. ncoa. org/wp-content/uploads/Series-Overview-Issue-Brief-1. pdf, Accessed on July 22, 2015.
Behavioral Health: Alcohol Screenings • 29 Percent of U. S. Adults Drink Too Much – At risk drinkers include both the 4 percent of adults who are dependent on alcohol (alcoholic) and the 25 percent who are not dependent. Both groups drink in ways that put themselves and others at risk of harm. In addition, according to the CDC more than 38 million Americans binge drink and this occurs, on average, four times a month. • Health and Social Harm – Risky alcohol use contributes to a wide range of negative health and social consequences and, over time, can result in serious medical conditions, such as hypertension, gastritis, liver disease, and various cancers. • Costly and Fatal – Risky alcohol use cost the United States about $223. 5 billion in 2006. It accounts for 80, 000 deaths annually and is the third leading preventable cause of death. • Women and Alcohol – Non-pregnant women of reproductive age who drink at risky levels have an increased chance of experiencing alcohol-exposed pregnancy, and unintended pregnancy. If they become pregnant, their drinking may cause harm to their unborn child resulting in miscarriage, stillbirth, and a range of physical, behavioral, and learning problems. 47
Behavioral Health: Depression Screenings • First line of Defense – PCPs are the primary point of contact for more than 50 percent of patients with mental illnesses. Approximately 35 percent of patients seen in primary care meet criteria for some form of depression and 10 percent suffer from major depression. • Chronic Disease – Depression tends to lead to other destructive habits such as drinking, drug abuse, and smoking all of which have the potential to lead to chronic disease. • Older Adults – Depression, especially in midlife or older adults, can cooccur with other serious medical illnesses, such as diabetes, cancer, heart disease, and Parkinson’s disease. • Adverse Effects – Medications taken for these physical illnesses may cause side effects that contribute to depression. 48
Behavioral Health: Screening Tools • Depression Screening – The Patient Health Questionnaire(PHQ-9) • http: //www. cqaimh. org/pdf/tool_phq 9. pdf – Beck Depression Inventory • http: //www. hr. ucdavis. edu/asap/pdf_files/Beck_Depre ssion_Inventory. pdf • Alcohol Screening – Audit-C tool – Alcohol Use Disorders Identification Test (AUDIT) – www. Alcoholscreen. org 49
Behavioral Health: Work Specific to IPFs Gap analyses Facility-specific IPF readmission report Quarterly facility dashboard so all staff can view Development and monthly review of strategic action plans • Staff trainings: • • – Community Resource Guide – Teach-back – Medication History Toolkit • Readmission Risk Tool (at admission) • Readmission Audit Tool (any readmission < 30 days) 50
TCPI: Practice Assessment Tool (PAT) • Developed by CMS • Released in April 2016 51 • Meant to assess stages of practice transformation
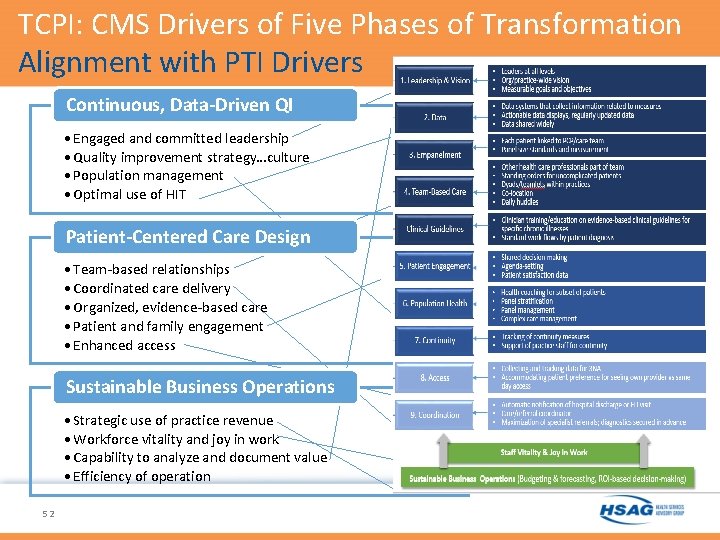
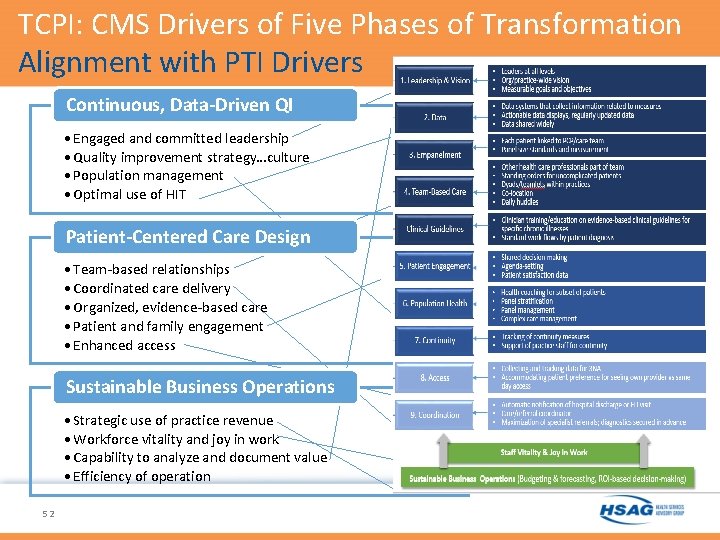
TCPI: CMS Drivers of Five Phases of Transformation Alignment with PTI Drivers Continuous, Data-Driven QI • Engaged and committed leadership • Quality improvement strategy…culture • Population management • Optimal use of HIT Patient-Centered Care Design • Team-based relationships • Coordinated care delivery • Organized, evidence-based care • Patient and family engagement • Enhanced access Sustainable Business Operations • Strategic use of practice revenue • Workforce vitality and joy in work • Capability to analyze and document value • Efficiency of operation 52
12 Scope of Work 53
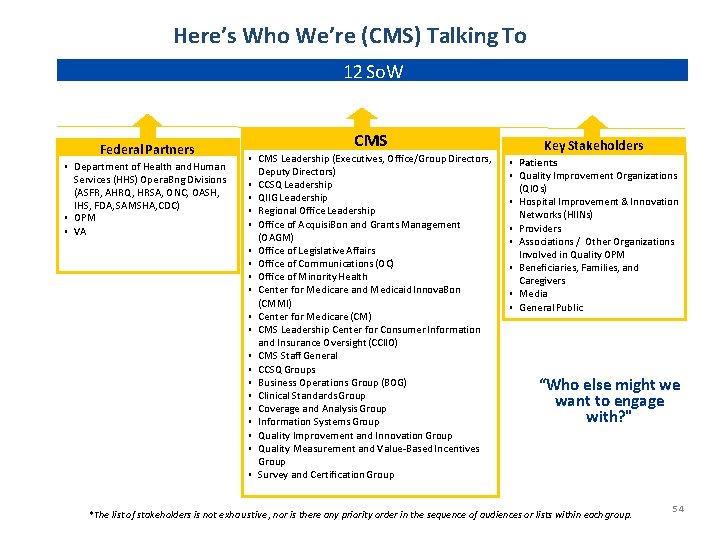
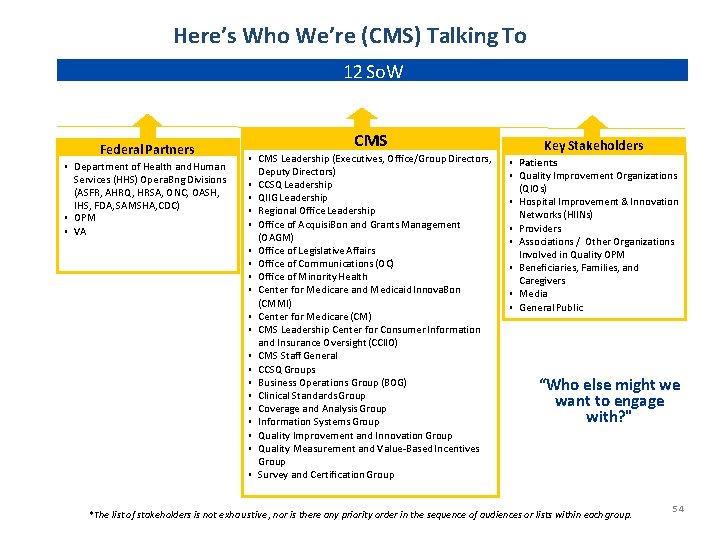
Here’s Who We’re (CMS) Talking To 12 So. W Federal Partners ▪ Department of Health and Human Services (HHS) Opera. Bng Divisions (ASFR, AHRQ, HRSA, ONC, OASH, IHS, FDA, SAMSHA, CDC) ▪ OPM ▪ VA CMS ▪ CMS Leadership (Executives, O ffice/Group Directors, Deputy Directors) ▪ CCSQ Leadership ▪ QIIG Leadership ▪ Regional Office Leadership ▪ Office of Acquisi. Bon and Grants Management (OAGM) ▪ Office of Legislative Affairs ▪ Office of Communications (OC) ▪ Office of Minority Health ▪ Center for Medicare and Medicaid Innova. Bon (CMMI) ▪ Center for Medicare (CM) ▪ CMS Leadership Center for Consumer Information and Insurance Oversight (CCIIO) ▪ CMS Staff General ▪ CCSQ Groups ▪ Business Operations Group (BOG) ▪ Clinical Standards Group ▪ Coverage and Analysis Group ▪ Information Systems Group ▪ Quality Improvement and Innovation Group ▪ Quality Measurement and Value-Based Incentives Group ▪ Survey and Certification Group Key Stakeholders ▪ Patients ▪ Quality Improvement Organizations (QIOs) ▪ Hospital Improvement & Innovation Networks (HIINs) ▪ Providers ▪ Associations / Other Organizations Involved in Quality OPM ▪ Beneficiaries, Families, and Caregivers ▪ Media ▪ General Public “Who else might we want to engage with? " *The list of stakeholders is not exhaustive, nor is there any priority order in the sequence of audiences or lists within each group. 54
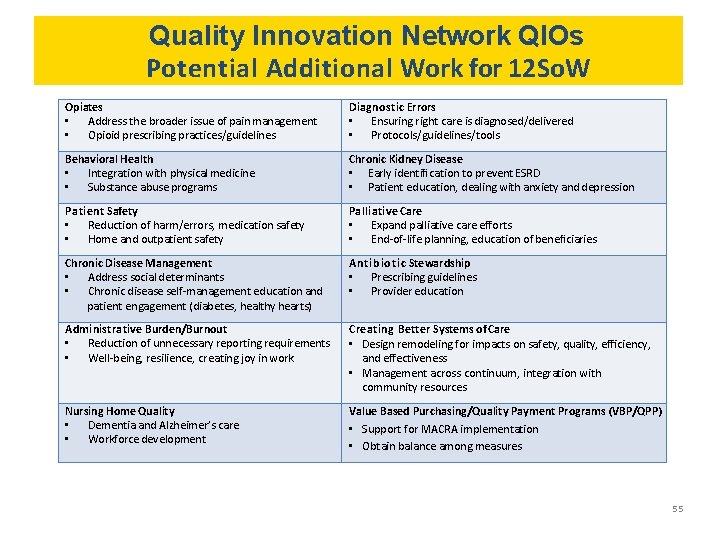
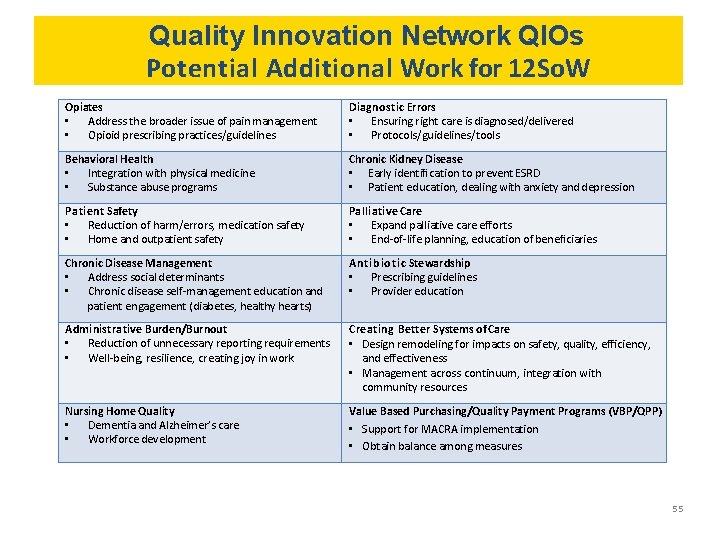
Quality Innovation Network QIOs Potential Additional Work for 12 So. W Opiates • Address the broader issue of pain management • Opioid prescribing practices/guidelines Diagnostic Errors • Ensuring right care is diagnosed/delivered • Protocols/guidelines/tools Behavioral Health • Integration with physical medicine • Substance abuse programs Chronic Kidney Disease • Early identification to prevent ESRD • Patient education, dealing with anxiety and depression Patient Safety • Reduction of harm/errors, medication safety • Home and outpatient safety Palliative Care • Expand palliative care efforts • End-of-life planning, education of beneficiaries Chronic Disease Management • Address social determinants • Chronic disease self-management education and patient engagement (diabetes, healthy hearts) Antibiotic Stewardship • Prescribing guidelines • Provider education Administrative Burden/Burnout • Reduction of unnecessary reporting requirements • Well-being, resilience, creating joy in work Creating Better Systems of Care • Design remodeling for impacts on safety, quality, efficiency, and effectiveness • Management across continuum, integration with community resources Nursing Home Quality • Dementia and Alzheimer’s care • Workforce development Value Based Purchasing/Quality Payment Programs (VBP/QPP) • Support for MACRA implementation • Obtain balance among measures 55
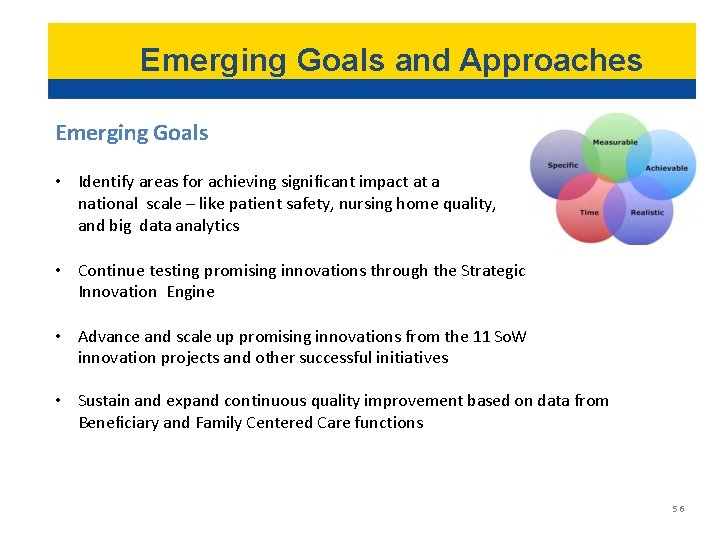
Emerging Goals and Approaches Emerging Goals • Identify areas for achieving significant impact at a national scale – like patient safety, nursing home quality, and big data analytics • Continue testing promising innovations through the Strategic Innovation Engine • Advance and scale up promising innovations from the 11 So. W innovation projects and other successful initiatives • Sustain and expand continuous quality improvement based on data from Beneficiary and Family Centered Care functions 56
Cross-Cutting Areas In addition to various priority focus areas, the following three crosscutting areas are being taken into consideration: Health Equity Person/Patient & Family Engagement Rural Health 57
Voice of the Beneficiary • Coordination of care, improving systems of care • Provider-patient communication, involvement in care • Avoidance of harm, patient safety • Understanding of all costs of care • Health literacy • Patient engagement mechanisms (councils, portals) • End-of-life planning • Involvement in quality improvement projects/redesign • Outreach to underserved, community resources • Attention to caregivers/care partners 58
CMS Strategic Goals THE CMS STRATEGY WILL BE BUILT ON ONE MAIN GOAL: PUT PATIENTS FIRST 59
“Secretary Tom Price calls on HHS to ‘reimagine’ how to carry out its mission. ” 60
Centers for Medicare and Medicaid Services: Strategic Goals 1. Empower patients and doctors to make decisions about their healthcare. 2. Usher in a new era of state flexibility and local leadership. 3. Support innovative approaches to improve quality, accessibility, and affordability. 4. Improve the CMS customer experience. 61
Key Priorities Identified by Health and Human Services Secretary Price • Opioids • Behavioral Health • Obesity • Reducing Burden 62
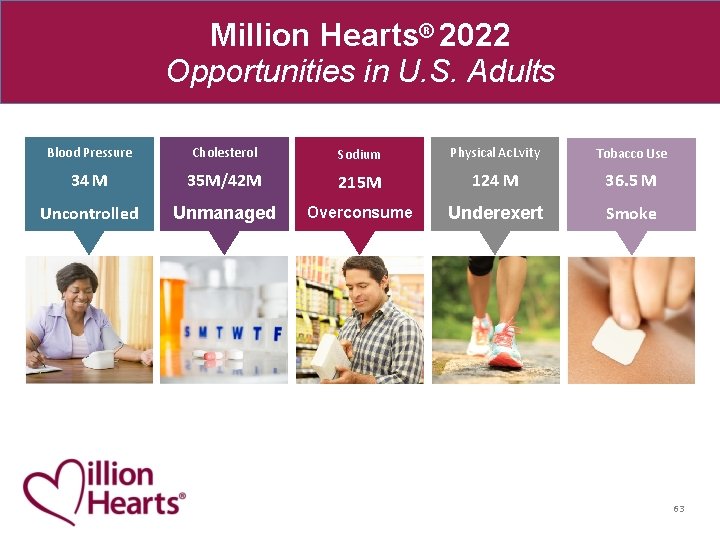
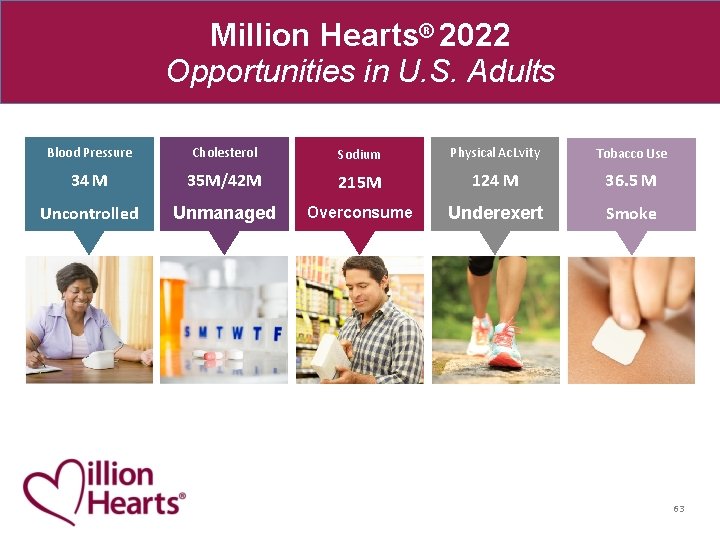
Million Hearts® 2022 Opportunities in U. S. Adults Blood Pressure Cholesterol Sodium Physical Ac. Lvity Tobacco Use 34 M 35 M/42 M 215 M 124 M 36. 5 M Uncontrolled Unmanaged Overconsume Underexert Smoke 63
HHSStrategic Goals q Healthcare System: Strengthen and Modernize the Nation’s Health Care System q Public Health System: Protect the Health of Americans where they Live, Learn, Work, and Play q Economic and Social Well-Being (Human Services): Strengthen the Economic and Social Well-Being of Americans across the Lifespan q Advance Science: Foster Sound, Sustained Advances in Science q Stewardship: Promote Effective and Efficient Management & Stewardship 64
65 This material was prepared by Health Services Advisory Group, Inc. , the Medicare Quality Improvement Organization for Florida, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U. S. Department of Health and Human Services. The contents presented do not necessarily reflect CMS policy. Publication No. FL-11 SOW-A. 1 -07072017 -01