Quality Improvement In the Carolinas Leonard Feld MD





- Slides: 37
Quality Improvement In the Carolinas Leonard Feld, MD, Ph. D. MMM, FAAP Department of Pediatrics Levine Children’s Hospital Carolinas Medical Center Charlotte, NC
Today’s Objectives • Discuss the Process of Quality • Discuss specifics related to Levine Children’s Hospital and the Department of Pediatrics
What is Quality? • The answer is quite simple: “It depends!” • It depends on who is answering the question and what is important to them. • It depends on who is defining quality and how they measure it. • It depends on theories you accept to guide your quality journey!
The Approach to Quality • Organizational commitment to quality • Focus on the customer • Fix systems, not people • Foster teamwork and group problem solving • Base improvement decisions on data versus intuition • Continuously improve • No quick fixes
Key Elements of System Change • Will to do what it takes to change to a new system • Ideas on which to base the design of the new system • Execution of the changes to system
Fundamental Questions for Improvement • What are we trying to accomplish? • How will we know that a change is an improvement? • What changes can we make that will result in an improvement?

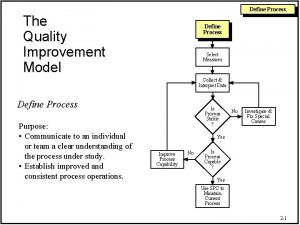
Methods of Improvement PDSA (Model of Improvement P Plan D Do S Study A Act Six Sigma (DMAIC) LEAN SCORE D Define S Select M Measure C Clarify A Analyze O Organize Description of Phase Kaizen Pre-work I Implement R Run Kaizen C Control Post-work E Evaluate • Identify improvement opportunity • Establish project boundaries • Establish Team • Validate current processes • Measure current performance • Financials • Assess gaps between performance & expectations • Identify Root Causes • Value added vs. non-value added • Develop improvement ideas • Prioritize change ideas • Test change ideas • Measure results (compare to baseline) • Validate improved process • Implement corrective actions as needed • Celebrate / publicize success
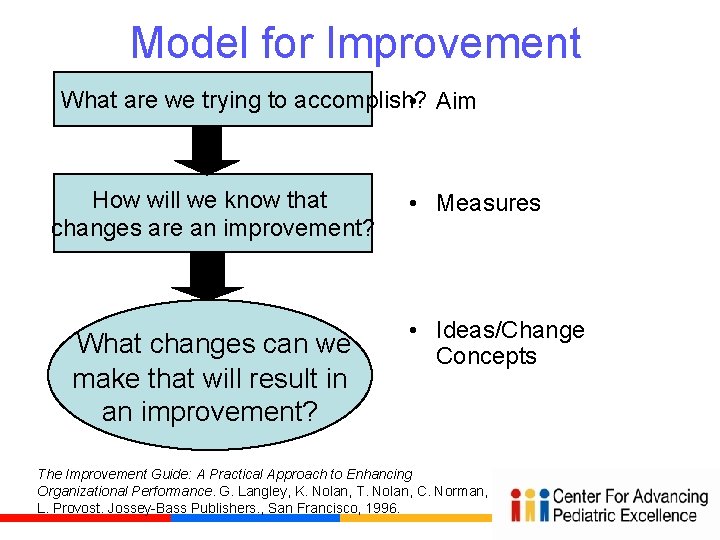
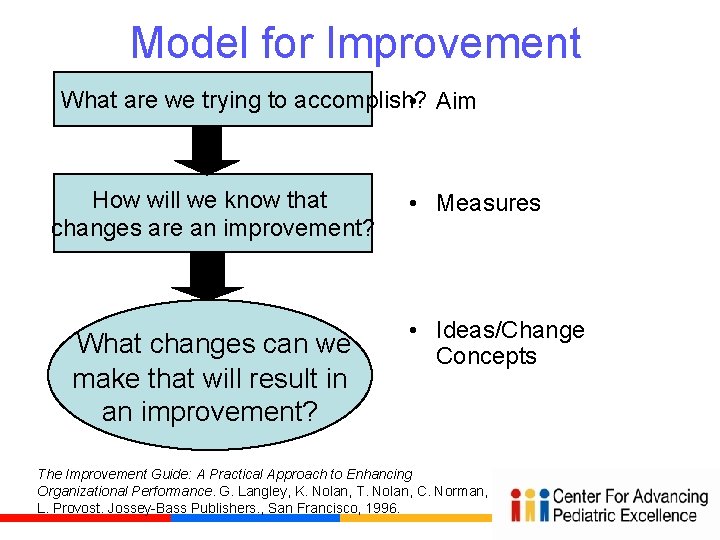
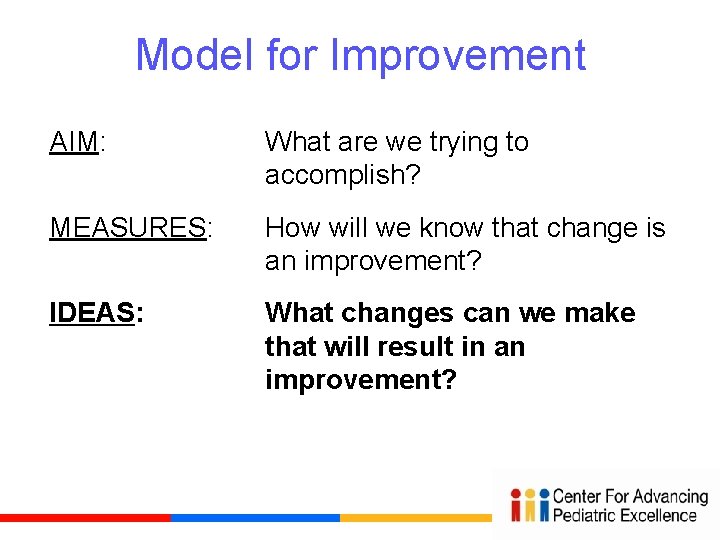
Model for Improvement What are we trying to accomplish? • Aim How will we know that changes are an improvement? What changes can we make that will result in an improvement? • Measures • Ideas/Change Concepts The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. G. Langley, K. Nolan, T. Nolan, C. Norman, L. Provost. Jossey-Bass Publishers. , San Francisco, 1996.
Model for Improvement AIM: What are we trying to accomplish? MEASURES: How will we know that changes are an improvement? IDEAS: What changes can we make that will result in an improvement?
Importance of Aim Statement • Captures early decisions • Alignment of team • Communication with others • Touchstone throughout project • Key to success
What is an Aim Statement? Aim: A written statement of the accomplishments expected from improvement effort Key components: – A general description of aim - should answer, “what are we trying to accomplish? ” – Rationale/importance – Some guidance for carrying out the work – Specify target population and time period – Measurable goals

Goals Should Be: • Measurable – Numeric – Preferably absolute rather than relative • A stretch, not business as usual – Achievable, not impossible
Model for Improvement AIM: What are we trying to accomplish? MEASURES: How will we know that changes are an improvement? IDEAS: What changes can we make that will result in an improvement?
How will we know if a change is an improvement? “All improvement is change, but not all change is an improvement. ”
Balancing Measures • Are we improving parts of our system at the expense of others? • Usually not one of goals • Great source is to listen to skeptics… “Yes, but…”
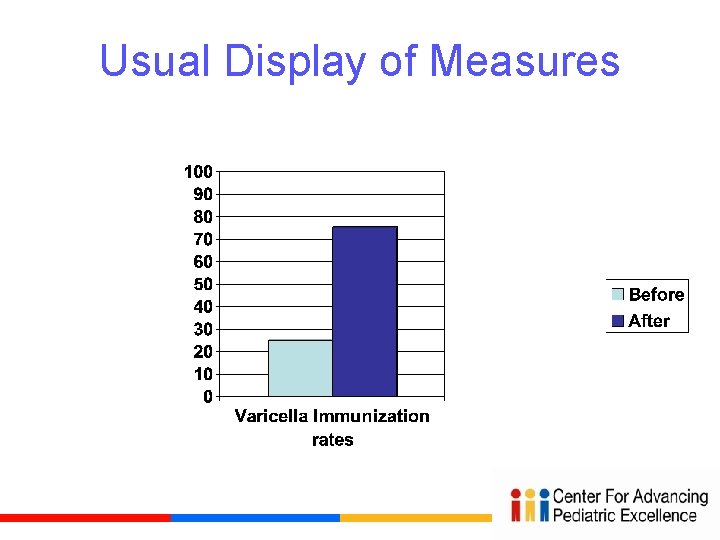
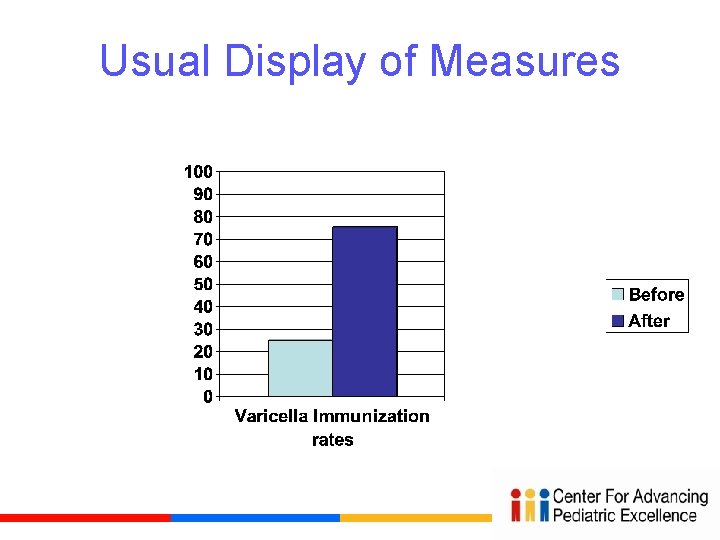
Usual Display of Measures
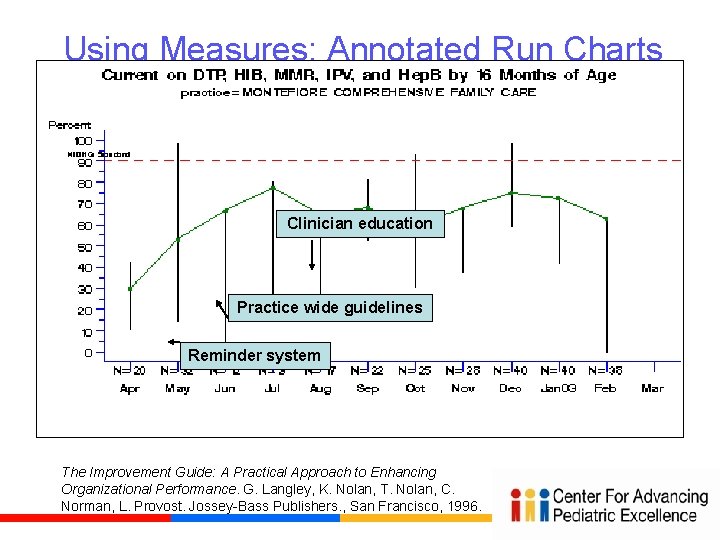
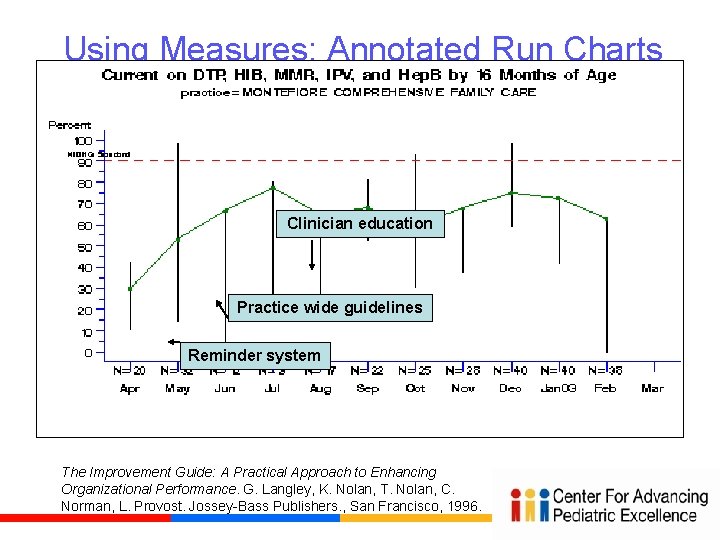
Using Measures: Annotated Run Charts Clinician education Reduced appt delays Practice wide guidelines Reminder system The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. G. Langley, K. Nolan, T. Nolan, C. Norman, L. Provost. Jossey-Bass Publishers. , San Francisco, 1996.
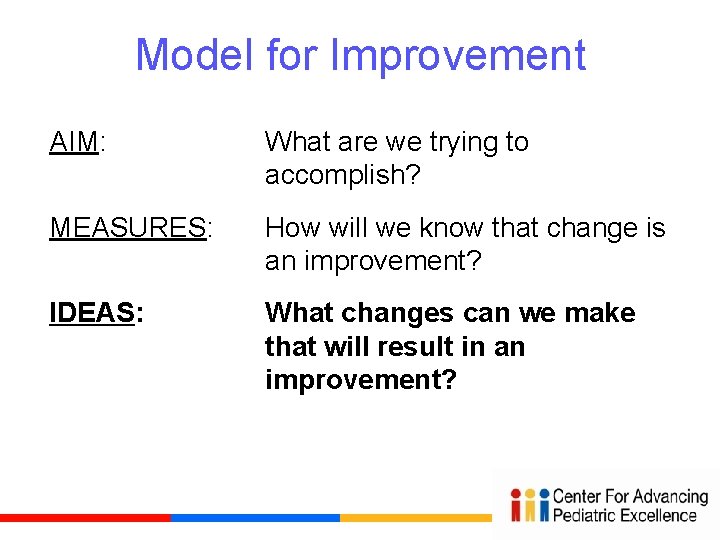
Model for Improvement AIM: What are we trying to accomplish? MEASURES: How will we know that change is an improvement? IDEAS: What changes can we make that will result in an improvement?
“Change Concepts” • A general approach to change (e. g. , Reduce backlog) • Purpose: to help teams generate specific changes to improve • “Change concepts” come from evidence and models that have been shown to work elsewhere – Feasible and effective in other settings (good ideas) – But need adaptation to specific setting (PDSAs)
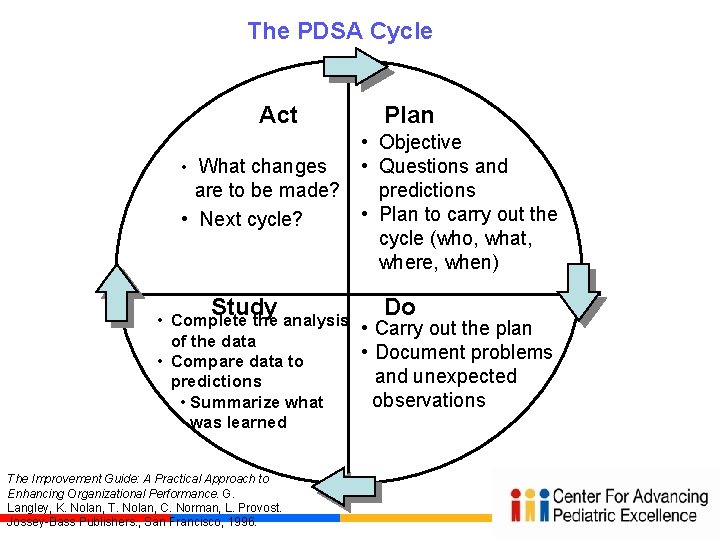
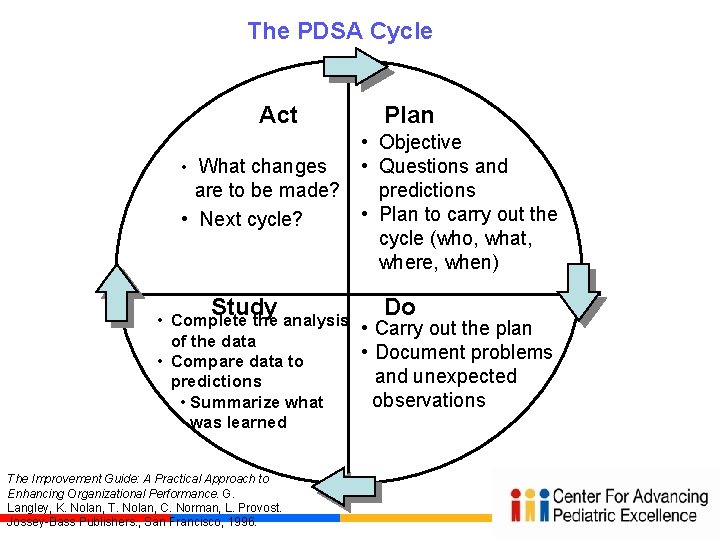
The PDSA Cycle Act • What changes are to be made? • Next cycle? Study Plan • Objective • Questions and predictions • Plan to carry out the cycle (who, what, where, when) Do • Complete the analysis • Carry out the plan of the data • Document problems • Compare data to and unexpected predictions observations • Summarize what was learned The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. G. Langley, K. Nolan, T. Nolan, C. Norman, L. Provost. Jossey-Bass Publishers. , San Francisco, 1996.
Key Points for PDSA Cycles • Do initial cycles on smallest scale possible – Think baby steps…a “cycle of one” usually best – “Failed” cycles are good learning opportunities when small • Learning from “failed” tests. Ask: – – Was test conducted well? Does the change tested need modification in our setting? Were measures sufficient to detect improvement? Was prediction/theory wrong?
Key References • The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. G. Langley, K. Nolan, T. Nolan, C. Norman, L. Provost. Jossey-Bass Publishers. , San Francisco, 1996. ( A MUST READ) • http: //www. apiweb. org/associates. htm (Provost) • “Eleven Worthy Aims for Clinical Leadership of Health System Reform, ” Don M. Berwick, JAMA, September 14, 1994, Vol. 272, #10, p. 797 -802.
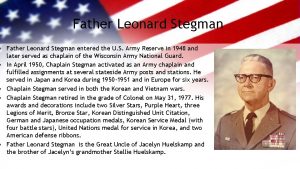
CAPE History The Center for Advancing Pediatric Excellence (CAPE) at Levine Children’s Hospital (LCH) developed as the Department of Pediatrics embraced an industry shift toward providing better patient care and QI education. Leadership in the LCH Department of Pediatrics determined that long-term success of QI initiatives depended on the development of an infrastructure to support ongoing improvement efforts. Residents needed dedicated resources to fully implement QI practice. CAPE resulted from this vision. • Began staffing and operations in the spring of 2009 • Curriculum launch in July 2009, followed by immediate application
Education Innovation: The CAPE Program Initially funded by a Duke Endowment grant, CAPE’s experiential program is unique. It provides intensive, one-on-one QI coaching to each resident within a 3 -year, progressive curriculum. CAPE features innovative, multi-faceted, individualized support: • QI Coach • Data Analyst • QI Faculty Mentor • CAPE director, co-director, and other staff Residents join and initiate real QI projects in LCH and associated clinics. Each project funnels into the overall system goals and priorities.

Quality – LCH and CAPE LCH Quality Goals and Faculty/Resident Projects Update • • Noonan, Courtlandt, Doyle, Mabus, Walsh Koricke, and the entire faculty, nurses, residents and professional staff. LCH Quality Goals – Healthcare Acquired Conditions, Appropriate Care Measures, LOS, ED Efficiency Numerous QI projects throughout LCH are advancing with CAPE’s support ; 63 faculty; 29 resident projects – Health Literacy – Open Access and Office Efficiency – Primary care provider communication tool (RHICU) – Improve Care NOW (GI) – Discharge Prescription Project – Reduce CRBSI and VAPs – Improve surveillance of chronic GVHD – Time from Arrival to Antibiotics – Improve Immunizations rate in HIV infected children – Standardization processes in the Dialysis Unit CAPE continues to participate in QI education activities
Unique features • Utilizes a multi-faceted approach to teach QI • Didactic lectures • Self-instruction via reading and online modules • Experiential learning through actual projects • Reflective practice • One-on-one coaching • Faculty mentoring • Data management coaching • Employs a progressive 3 -year curriculum • Provides a dedicated staff to guide QI endeavors including a QI Coach and support from a Data Analyst
Curriculum PGY-1 Introduction to the Model for Improvement • Complete pre-assessment QI knowledge survey, Mandatory QI readings • Mandatory IHI online modules, Participation in QI didactic lectures • Personal Improvement Project (PIP), Short Ambulatory QI Project PGY-2 Experiential learning within a QI team • Mandatory QI readings, Mandatory IHI online modules • Participation in QI didactic lectures, Identify a Faculty QI Mentor • Joins an existing multi-disciplinary QI project, or starts own project
Curriculum PGY-3 Building leadership and sustainability • Mandatory QI readings and IHI online modules • Participation in QI didactic lectures • Work with Faculty QI Mentor • Functions as a Physician Champion of a multi-disciplinary QI project • Present QI project to broad LCH audience, including Department of Pediatrics faculty • Plans for sustainability of project • Complete post-assessment QI knowledge survey
Quality - Infection Free Days Catheter associated blood stream infections and ventilator associated infection. q. ICU q. Pediatric Hematology & Oncology q. NICU

Children’s Asthma Care Core Measure: Appropriate Care Score • This project focuses on the care of inpatients with asthma, the delivery of beta-agonists, corticosteroids, and discharge with a home maintenance plan of care. • The Appropriate Care Score reflects the percent of patients who received all required elements.
CHIPS Geography Project • Optimizing care teams, ensuring continuity, and effective transitions have been shown to produce improved health outcomes. • Co-location of healthcare providers in a specific geographic location is a strategy that can lead to improved continuity, transitions of care, and care teams. • LCH CHIPS teams will improve patient’s quality of stay at LCH by implementing geographically located teams. • CHIPS physicians will be able to work more closely with a smaller number of nurses, therapists, and consultants, and be in close proximity to our patients throughout the day and night.
Myers Park Pediatric Clinic Obesity QI Project • The goal of this project is to impact childhood obesity among MP pediatric patients through prevention, monitoring, and management. • Identification of patients who are overweight and obese using BMI measurement is essential in managing the pediatric population. • The initial phase of this project is development of tools for identification and management of overweight and obese children. • Subsequent phases will include evaluation of the presence of documentation of overweight and obesity in the medical record and evidence of provider counseling.
Myers Park Pediatrics Health Literacy QI Project • A key strategy to ensuring patient understanding is the use of Teach Back. • A pediatric resident is currently spreading her clinic-based Teach Back project to other residents. • There is concern that use of Teach Back will increase the length of visits. • This project demonstrates a shorter visit length attributed to improved communication and improved patient understanding.

Expedited Partner Treatment for Sexually Transmitted Infections • Educate 100% of providers at THC and CMC ED on topic of EPT, including treatment algorithms and prescription instructions • Educate 100% of index patients about partner treatment options • Increase the percent of patients who are offered EPT by 75% • Increase the percent of patients who accept EPT by 75% • Notify 100% of positive GC/C cases at THC and CMC ED
The Future of QI at LCH and Dept of Peds is committed to broadening the QI program QI expansion will allow LCH and the Dept of Peds to significantly alter care for children in our own community, and at hospitals across the country. • Additional QI capacity will help our providers gain control over some of the most pervasive diseases plaguing our patients, e. g. asthma and obesity. • QI work will help our hospital reach unprecedented success in care measures like infection prevention and mortality rates. • As the nation addresses healthcare issues, CMC and LCH will need to rely heavily on QI to remain at the forefront of healthcare excellence.
Bottom line on Quality Accelerate cross learning and spread adoption Design systems to foster collaborative networks to learn Frontline leadership drives design and sets measureable QI participation and expectations Avoid stagnation Take population based improvements to the next level Let’s get interested in doing better all the time and achieve sustainability
We Learn – We teach Thank you to our team Laura Noonan, MD Cheryl Courtlandt, MD Sarah Mabus Maureen Walsh Koricke, RN Leslie Doyle, RN Entire LCH and Peds Team
 Quality assurance model in nursing management
Quality assurance model in nursing management Compliance vs quality
Compliance vs quality Course handicap formula
Course handicap formula South carolina state bird and flower
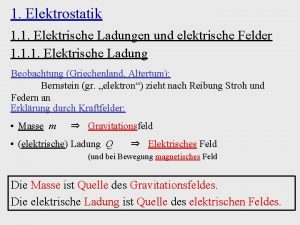
South carolina state bird and flower Spitzeneffekt elektrisches feld
Spitzeneffekt elektrisches feld Biomechanische prinzipien badminton
Biomechanische prinzipien badminton David feld today's man
David feld today's man Lutz feld
Lutz feld Lexikalisches feld
Lexikalisches feld Feld hell club
Feld hell club Phänomenales feld rogers
Phänomenales feld rogers Point of care quality improvement
Point of care quality improvement Continuous quality improvement plan example
Continuous quality improvement plan example Swot analysis for quality
Swot analysis for quality Cqi action plan template
Cqi action plan template Quality improvement vs research
Quality improvement vs research Cotinuous
Cotinuous Define continuous quality improvement
Define continuous quality improvement Rapid cycle quality improvement
Rapid cycle quality improvement Mqii toolkit
Mqii toolkit Tea quality improvement
Tea quality improvement Qsen safety examples
Qsen safety examples Quality improvement
Quality improvement Efmd quality improvement system
Efmd quality improvement system Quality is free: the art of making quality certain
Quality is free: the art of making quality certain Quality improvement
Quality improvement Xerox problem solving process
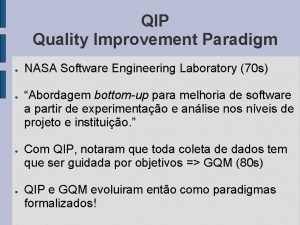
Xerox problem solving process Quality improvement paradigm
Quality improvement paradigm Juran 10 steps to quality improvement
Juran 10 steps to quality improvement Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Data driven quality
Data driven quality Sus qi
Sus qi Quality gurus and their contribution
Quality gurus and their contribution Pmp quality management
Pmp quality management Old quality vs new quality
Old quality vs new quality Pmp gold plating
Pmp gold plating Basic concept of quality management
Basic concept of quality management Perform quality assurance
Perform quality assurance