Quadriceps Patellar Tendon Injuries Ian Rice MD Introduction
















- Slides: 54

Quadriceps & Patellar Tendon Injuries Ian Rice MD
Introduction • Tendinosis & Rupture • Extensor Mechanism Disruption • Quadriceps tendon rupture • Patellar tendon rupture

Anatomy • Extensor Mechanism • • Quadriceps tendon Patellar tendon (ligament)
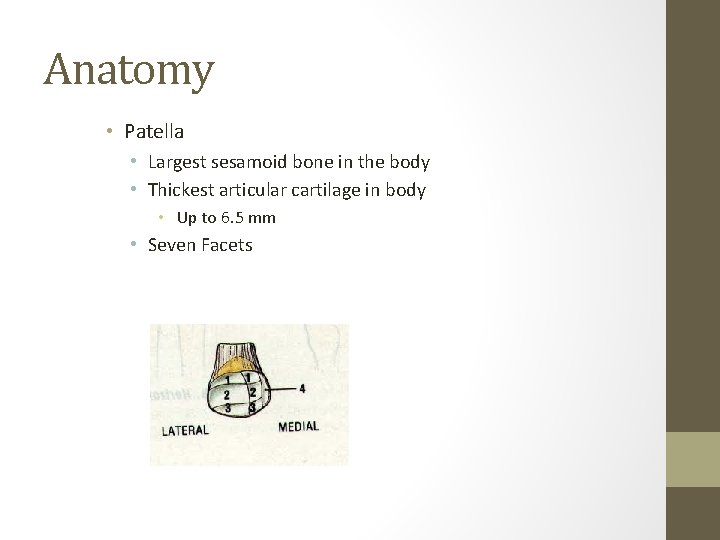
Anatomy • Patella • Largest sesamoid bone in the body • Thickest articular cartilage in body • Up to 6. 5 mm • Seven Facets
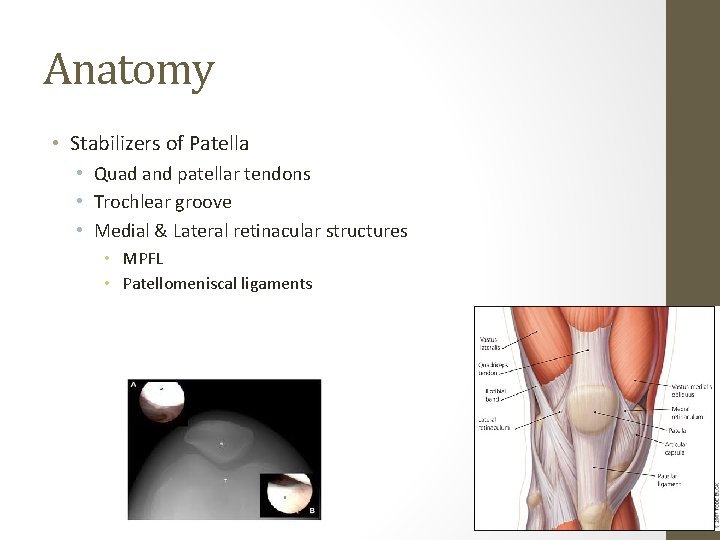
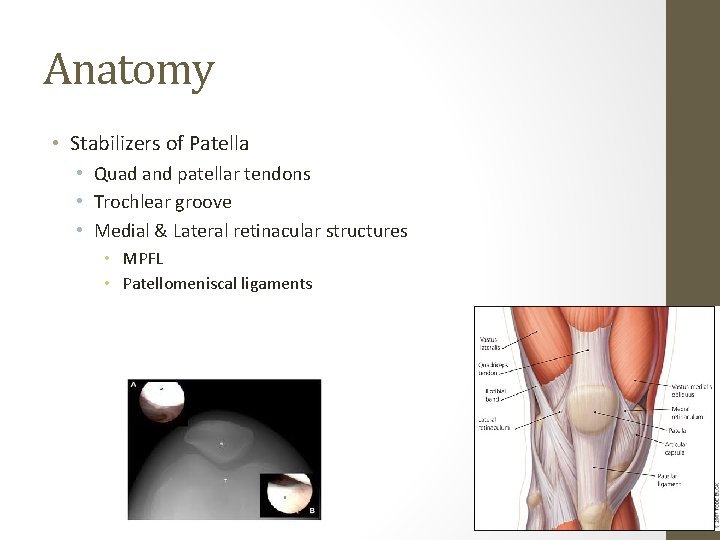
Anatomy • Stabilizers of Patella • Quad and patellar tendons • Trochlear groove • Medial & Lateral retinacular structures • MPFL • Patellomeniscal ligaments
Anatomy • Dynamic Stabilizers of Patella • Quad muscles • Innervated by femoral nerve • Posterior divisions of 2 nd, 3 rd, & 4 th lumbar spinal nerves
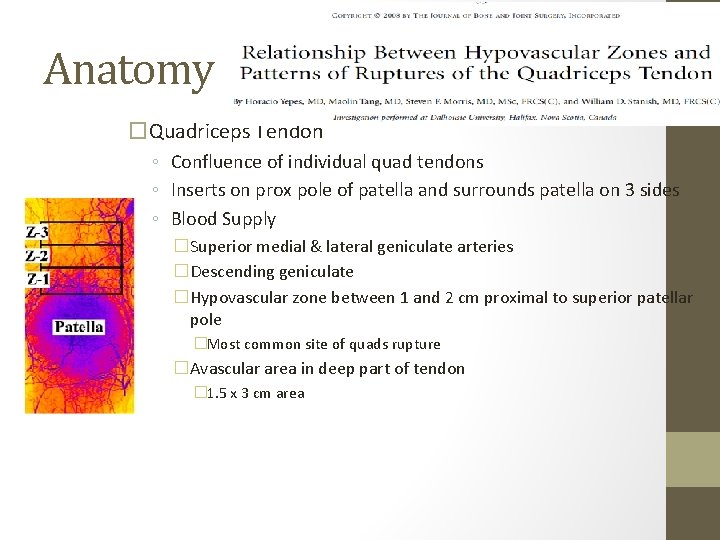
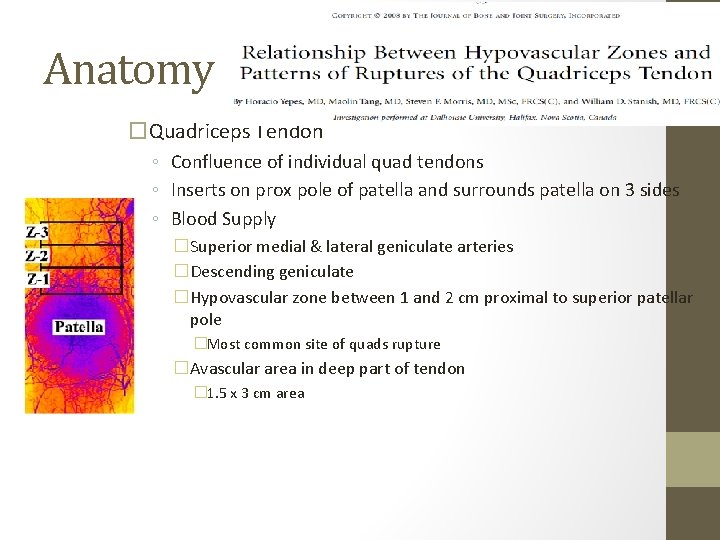
Anatomy �Quadriceps Tendon ◦ Confluence of individual quad tendons ◦ Inserts on prox pole of patella and surrounds patella on 3 sides ◦ Blood Supply �Superior medial & lateral geniculate arteries �Descending geniculate �Hypovascular zone between 1 and 2 cm proximal to superior patellar pole �Most common site of quads rupture �Avascular area in deep part of tendon � 1. 5 x 3 cm area
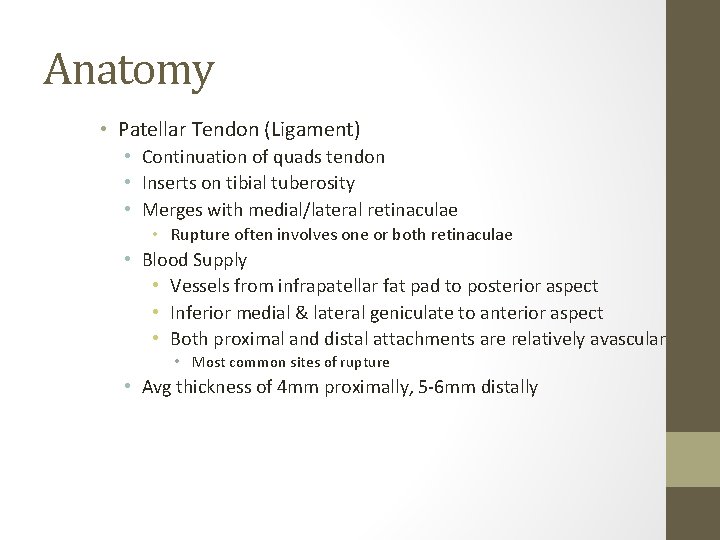
Anatomy • Patellar Tendon (Ligament) • Continuation of quads tendon • Inserts on tibial tuberosity • Merges with medial/lateral retinaculae • Rupture often involves one or both retinaculae • Blood Supply • Vessels from infrapatellar fat pad to posterior aspect • Inferior medial & lateral geniculate to anterior aspect • Both proximal and distal attachments are relatively avascular • Most common sites of rupture • Avg thickness of 4 mm proximally, 5 -6 mm distally
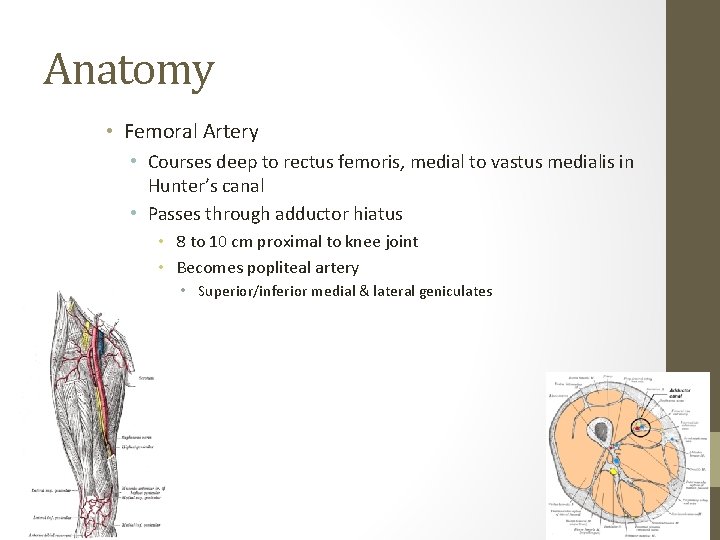
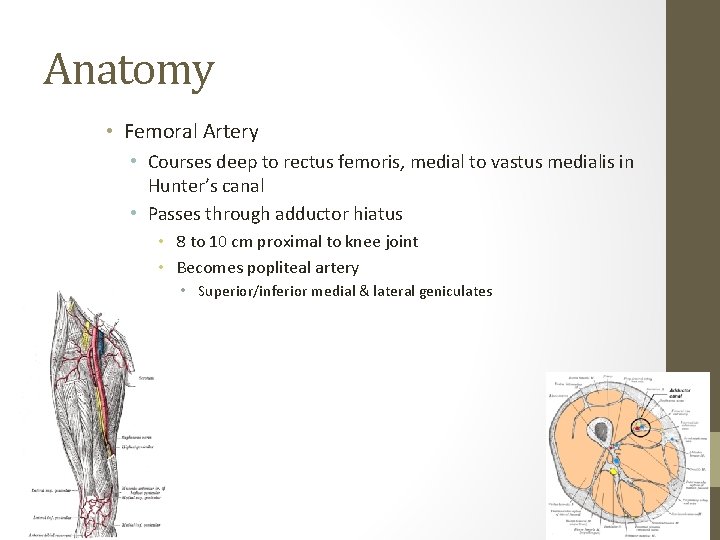
Anatomy • Femoral Artery • Courses deep to rectus femoris, medial to vastus medialis in Hunter’s canal • Passes through adductor hiatus • 8 to 10 cm proximal to knee joint • Becomes popliteal artery • Superior/inferior medial & lateral geniculates
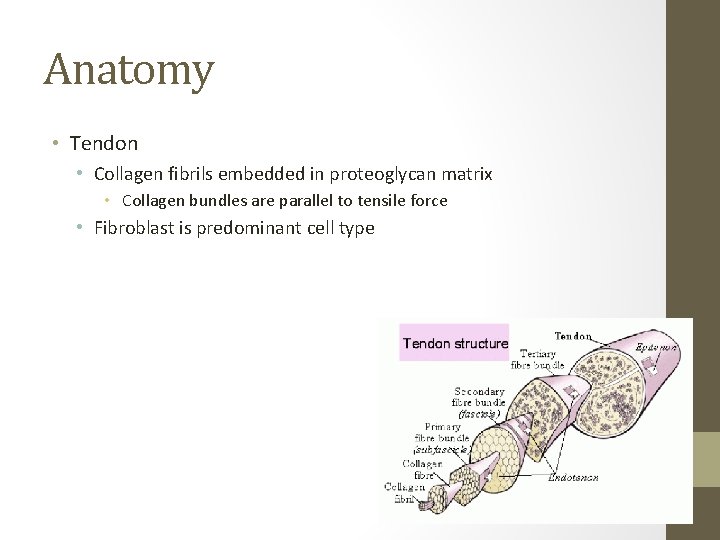
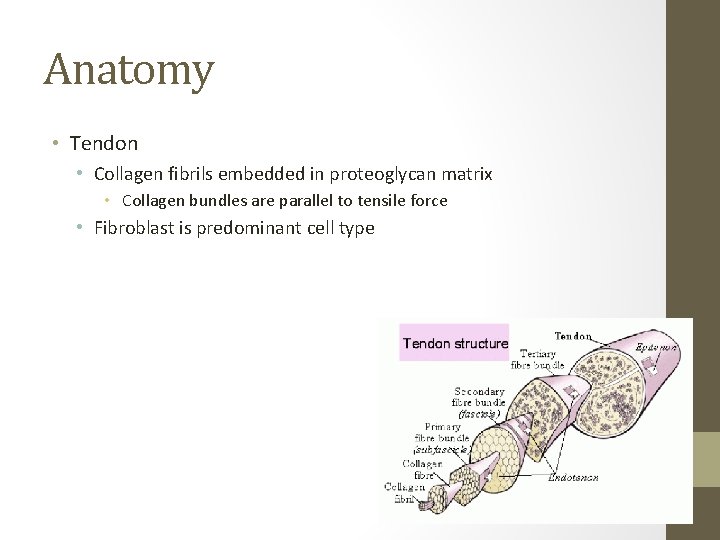
Anatomy • Tendon • Collagen fibrils embedded in proteoglycan matrix • Collagen bundles are parallel to tensile force • Fibroblast is predominant cell type
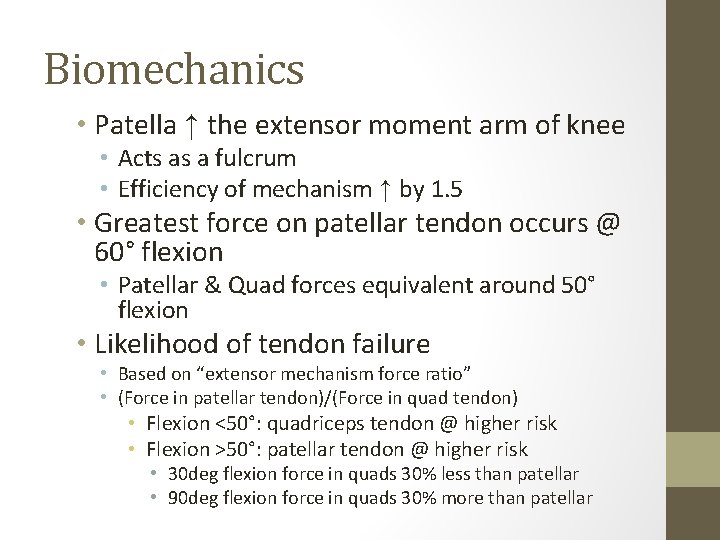
Biomechanics • Patella ↑ the extensor moment arm of knee • Acts as a fulcrum • Efficiency of mechanism ↑ by 1. 5 • Greatest force on patellar tendon occurs @ 60° flexion • Patellar & Quad forces equivalent around 50° flexion • Likelihood of tendon failure • Based on “extensor mechanism force ratio” • (Force in patellar tendon)/(Force in quad tendon) • Flexion <50°: quadriceps tendon @ higher risk • Flexion >50°: patellar tendon @ higher risk • 30 deg flexion force in quads 30% less than patellar • 90 deg flexion force in quads 30% more than patellar
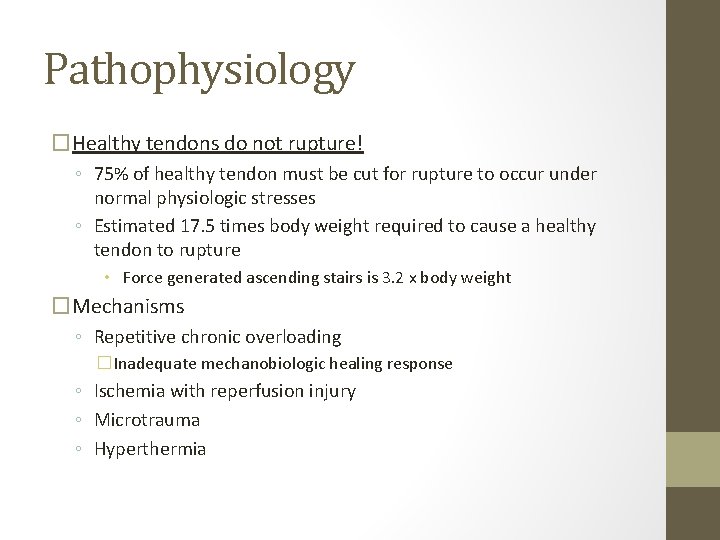
Pathophysiology �Healthy tendons do not rupture! ◦ 75% of healthy tendon must be cut for rupture to occur under normal physiologic stresses ◦ Estimated 17. 5 times body weight required to cause a healthy tendon to rupture • Force generated ascending stairs is 3. 2 x body weight �Mechanisms ◦ Repetitive chronic overloading �Inadequate mechanobiologic healing response ◦ Ischemia with reperfusion injury ◦ Microtrauma ◦ Hyperthermia
Pathophysiology �Most ruptures occur at osteotendinous or musculotendinous junction ◦ May also result in avulsion fractures �Midsubstance ruptures typically only occur in setting of pathology ◦ ◦ ◦ Hypoxic degenerative tendinopathy Mucoid degeneration Tendolipomatosis Calcifying tendinopathy Combination of above
Pathophysiology � Conditions Associated with Occult Tendinopathy ◦ Hyperparathyroidism ◦ Calcium pyrophosphate deposition ◦ Diabetes mellitus �Vasculopathy affects blood supply ◦ Steroid-induced tendinopathy �Both local and systemic use ◦ Fluoroquinolone-induced tendinopathy �Alters extra-cellular matrix in tendons �Induces IL-1 beta-mediated MMP-3 release (Cipro) ◦ Osteomalacia ◦ Chronic renal insufficiency �Causes muscle fiber atrophy ◦ Gout ◦ Uremia �Muscle fiber atrophy ◦ Systemic lupus erythematosus ◦ Rheumatoid arthritis �Leads to synovitis and diffuse fibrosis
Quads & Patellar Tendinosis “Jumper’s Knee” �May affect either quads or patellar tendons �May be result of microtears of patellar ligament ◦ Chronic inflammatory response ensues �Related activities ◦ Jumping ◦ Kicking ◦ Leaping �Prevalence among sports ◦ Cycling: 0% ◦ Basketball (male): 32% ◦ Volleyball (male): 44% �Even higher prevalence with harder floor type �May affect younger pts entering rapid growth phase ◦ Bone growth exceeds tendon growth ◦ Different than Osgood-Schlatters
Quads & Patellar Tendinosis “Jumper’s Knee” • Pts c/o pain in area of patellar tendon • PE Findings • Tenderness over patellar/quad tendon • • Typically at distal patellar pole/prox tendon Inferior Pole 65% Superior pole 25% Tibial tubercle 10% “Bogginess” Pain with resisted extension Pain with full passive flexion Basset's sign • tenderness to palpation at distal pole of patella in full extension • no tenderness to palpation at distal pole of patella in full flexion • Movie Theater sign • Pain with prolonged knee flexion
Quads & Patellar Tendinosis “Jumper’s Knee” • Blazina Phases (based on history) • 1: Pain after activity only • 2: Pain at beginning of activity, disappears after warm-up • 3: Constant pain at rest and with activity • Phase 1 -2 respond well to rest and PT • Phase 3 require longer rest period • Chronic may require surgical debridement
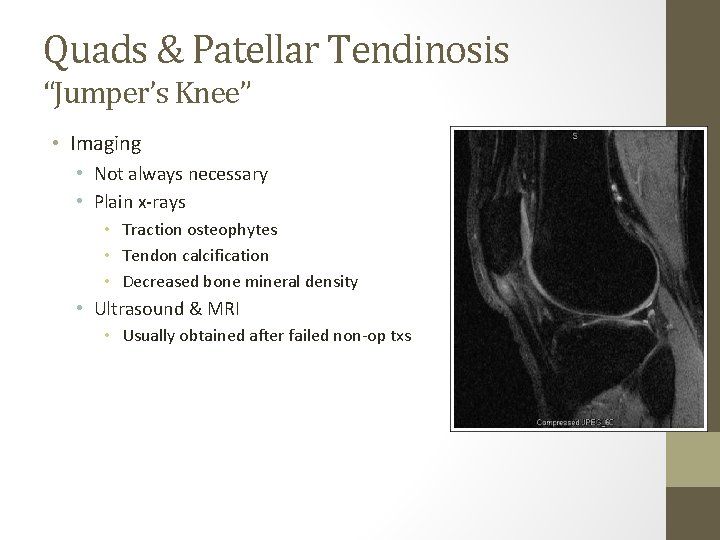
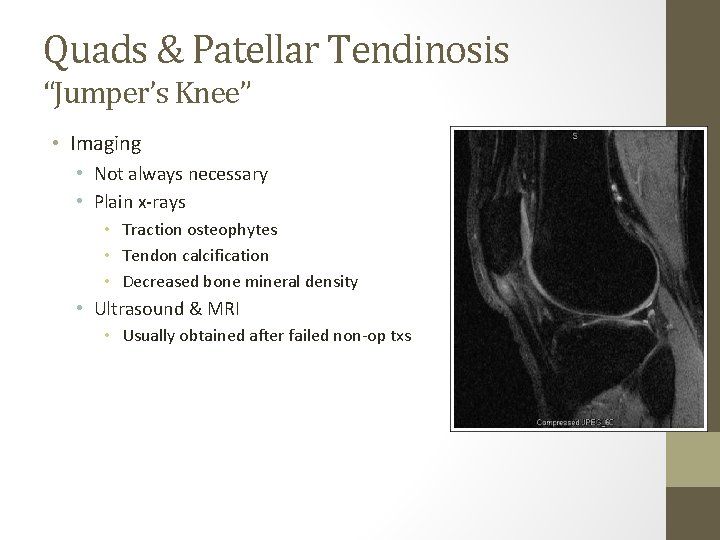
Quads & Patellar Tendinosis “Jumper’s Knee” • Imaging • Not always necessary • Plain x-rays • Traction osteophytes • Tendon calcification • Decreased bone mineral density • Ultrasound & MRI • Usually obtained after failed non-op txs
Quads & Patellar Tendinosis “Jumper’s Knee” �Treatment ◦ Non-op �Corticosteroid injection should not be used �Decreasing or stopping inciting activity (aka – rest) �Eccentric training proven as effective as surgery. �Isotonic or isokinetic exercises for quad strength should begin only after pain/sxs improve �NSAIDs �Cryotherapy �Stretching �Isometric strengthening of quads �Most pts improve after 6 months ◦ Operative (uncommon) �Failure of non-op tx, abnormal findings on MRI �Longitudinal tenotomies with debridement �Tenonectomy with longitudinal cuts
Quadriceps Tendon Rupture • Often related to deceleration injury • Semiflexed knee, strong contraction of quads, planted or obstructed foot/leg • More common > 40 yrs old • Multiple forms • Incomplete vs Complete • Unilateral • Bilateral (rare) • Pts report tearing sensation

Quadriceps Tendon Rupture �PE Findings ◦ Triad �Pain �Inability to actively extend knee �Pts may be able to maintain extension through intact retinaculum �Suprapatellar gap on palpation �Hemarthrosis may make this difficult �Flex hip to shorten rectus femoris – may make gap more apparent ◦ Aspiration with injection of lidocaine �Helps with pain �May improve exam

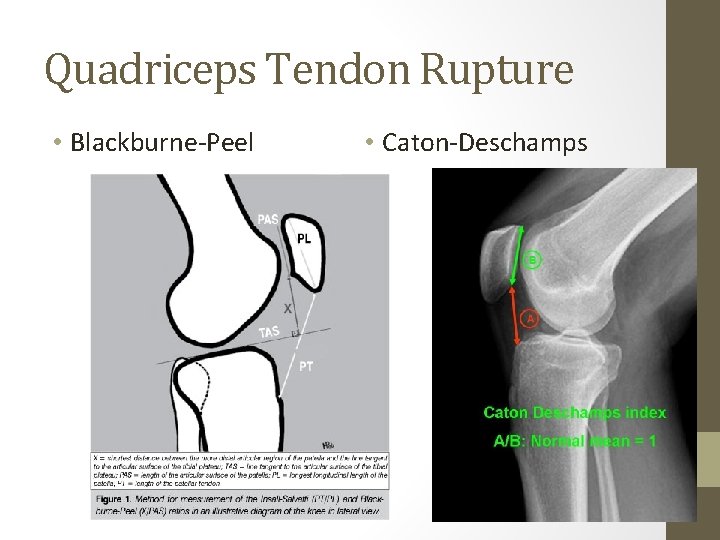
Quadriceps Tendon Rupture �Imaging ◦ X-rays �Insall-Salvati ratio < 1 �High intra/interobserver error rates �Blackburne-Peel < 0. 805 (men) or 0. 806 (women) �Lower intra/interobserver error rates compared to Insall-Salvati ratio �Caton-Deschamps �< 1 (normal ratio = 1) �Plateau-patella angle �Angle < 21° (normal angle 21 -29°) �May also be anterior tilt of patella �Only 10 of 18 pts had inferiorly displaced patellas �Kaneko et al. 1994 ◦ MRI
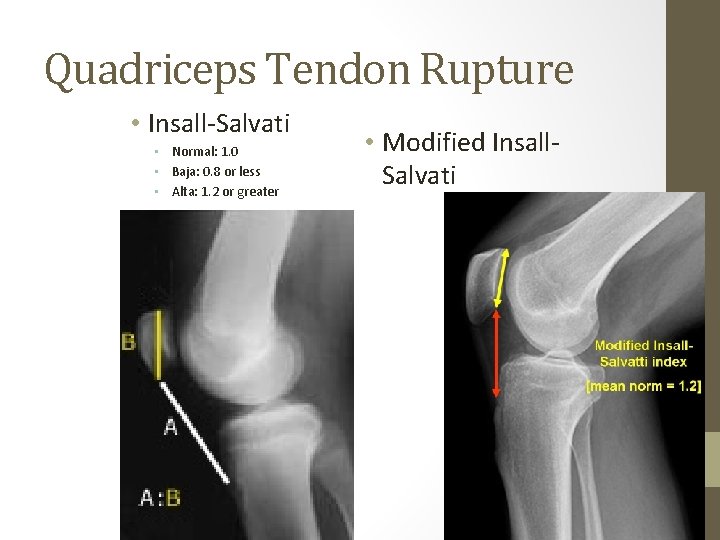
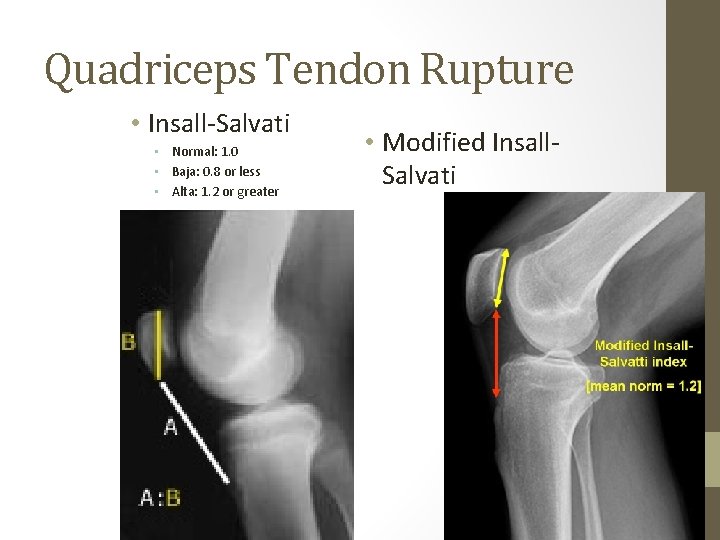
Quadriceps Tendon Rupture • Insall-Salvati • Normal: 1. 0 • Baja: 0. 8 or less • Alta: 1. 2 or greater • Modified Insall. Salvati
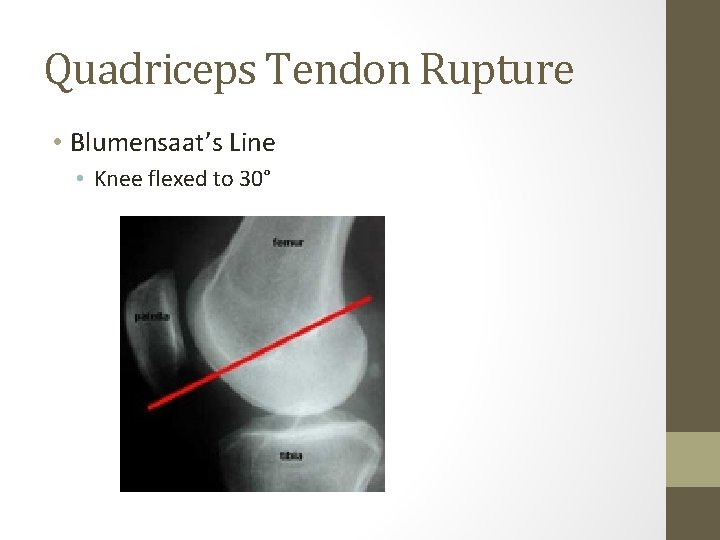
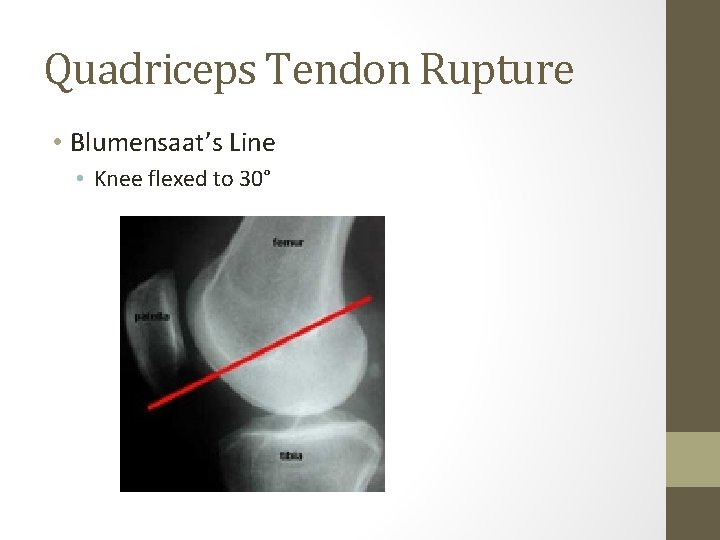
Quadriceps Tendon Rupture • Blumensaat’s Line • Knee flexed to 30°
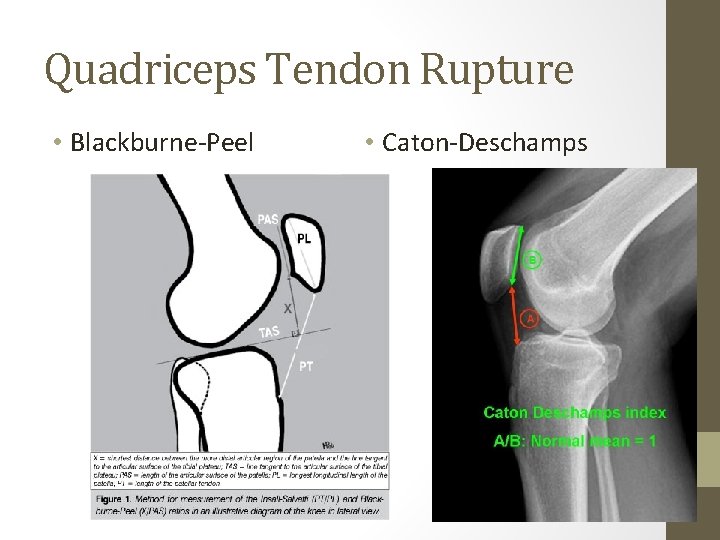
Quadriceps Tendon Rupture • Blackburne-Peel • Caton-Deschamps
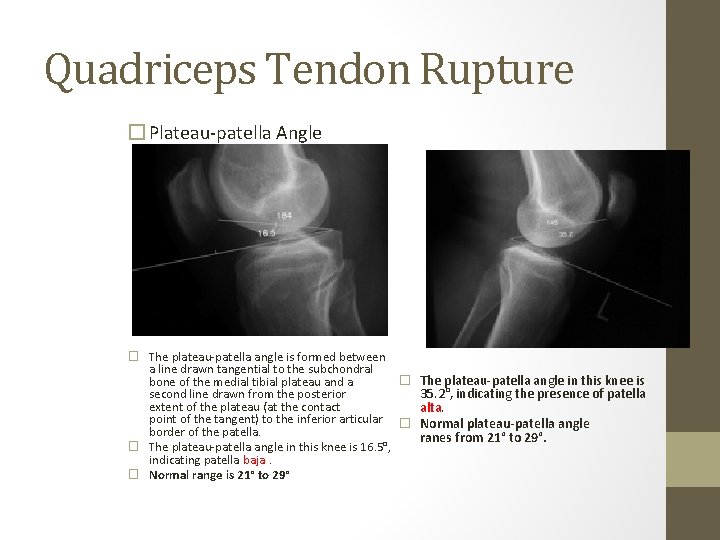
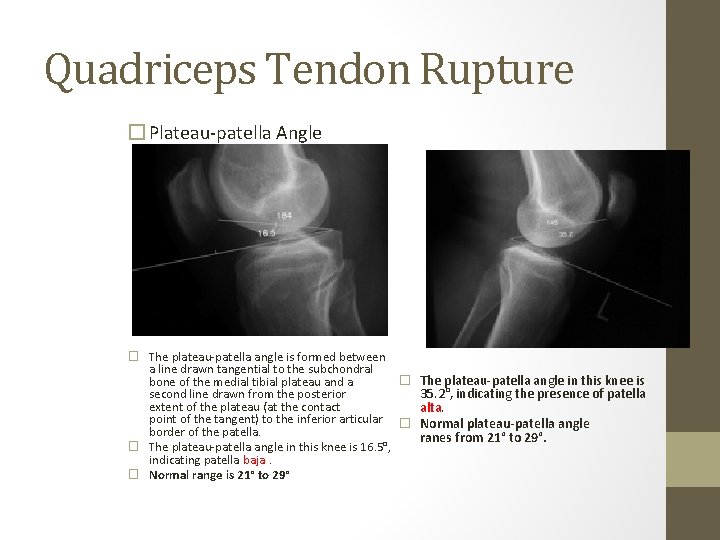
Quadriceps Tendon Rupture � Plateau-patella Angle � The plateau-patella angle is formed between a line drawn tangential to the subchondral � bone of the medial tibial plateau and a second line drawn from the posterior extent of the plateau (at the contact point of the tangent) to the inferior articular � border of the patella. � The plateau-patella angle in this knee is 16. 5°, indicating patella baja. � Normal range is 21° to 29° The plateau-patella angle in this knee is 35. 2°, indicating the presence of patella alta. Normal plateau-patella angle ranes from 21° to 29°.
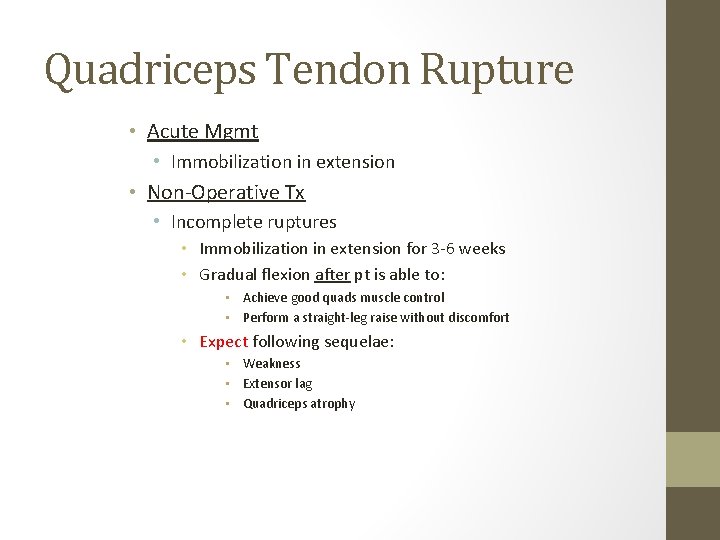
Quadriceps Tendon Rupture • Acute Mgmt • Immobilization in extension • Non-Operative Tx • Incomplete ruptures • Immobilization in extension for 3 -6 weeks • Gradual flexion after pt is able to: • Achieve good quads muscle control • Perform a straight-leg raise without discomfort • Expect following sequelae: • Weakness • Extensor lag • Quadriceps atrophy

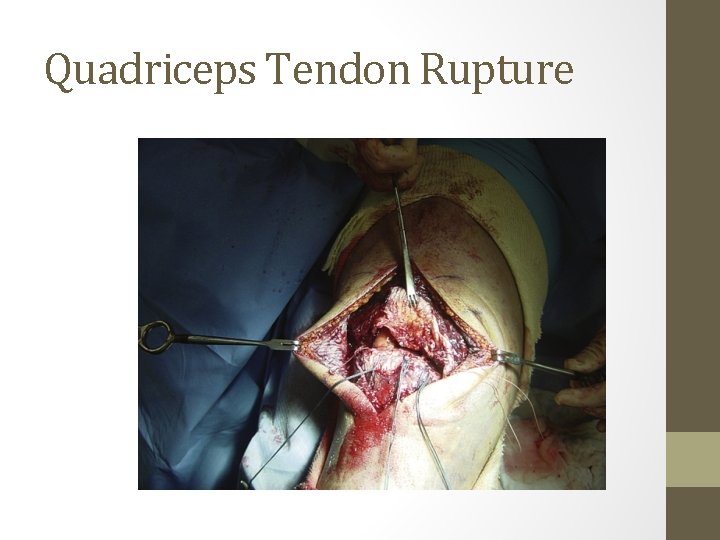
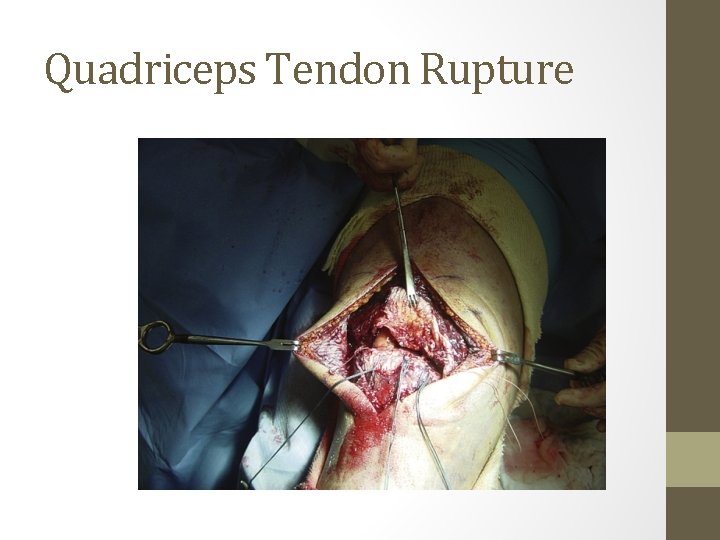
Quadriceps Tendon Rupture �Operative Tx ◦ Complete ruptures �Early repair leads to better results �Within 1 week �Beyond 72 hrs, retraction may make repair more difficult �Repair techniques vary �No single technique shown to be better than any other �Depends on location of rupture �Midsubstance tear • End-to-end repair �Tear at/near osteotendinous jxn (most common site) • Drill holes in patella • +/- reinforcing cerclage �Collagen remodels into organized longitudinal structure over 3 to 6 months

Quad Tendon Rupture Repair Midline incision Debride tendon edges Midsubstance with end to end At oseotendinous junction 3 drill holes in patella 2 heavy sutures in krakow or brunnell through tendon and passed through patella • Retinaculum repaired • Augmentation usually not necessary • Scuderi technique for tenuous repairs • • • Partial thickness triangular flap from anterior proximal tendon 2 inch base 3 inch sides, flap folded down and sutured

Chronic Repairs • Elevate quadriceps off femur and release adhesions to gain length • Codivilla lengthening • • • Full thickness V in proximal segment Lower margin should end 1. 3 to 2 cm proximal to rupture Tendon ends repaired Triangular flap turned down and sutured V sutured side to side
Quadriceps Tendon Rupture

Quadriceps Tendon Rupture �Results ◦ No differences based on repair technique �Delayed surgery leads to poorer functional outcomes and pt satisfaction � 92% pts satisfied – Konrath et al (1998) � 84% returned to previous activities � 51% unable to return to pre-surgery level of recreational activity � 12% quad strength loss � 14% hamstring strength loss � 8° ROM loss – flexion �Re-rupture uncommon
Patellar Tendon Rupture • • Same mechanism as quads rupture More common under age 40 yrs Popping or tearing sensation Multiple forms • Incomplete vs Complete • Unilateral • Bilateral (rare)

Patellar Tendon Rupture • PE Findings • Triad • Pain • Inability to actively extend knee • Infrapatellar gap on palpation • Hemarthrosis may make this difficult • Rule out other intra-articular pathology
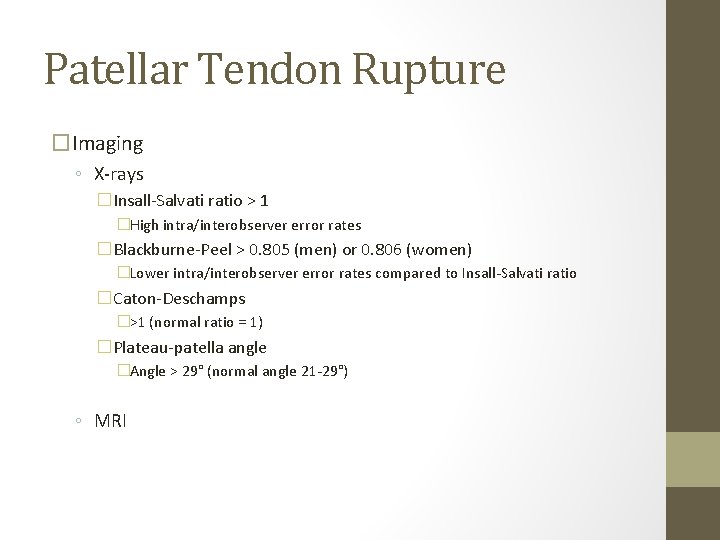
Patellar Tendon Rupture �Imaging ◦ X-rays �Insall-Salvati ratio > 1 �High intra/interobserver error rates �Blackburne-Peel > 0. 805 (men) or 0. 806 (women) �Lower intra/interobserver error rates compared to Insall-Salvati ratio �Caton-Deschamps �>1 (normal ratio = 1) �Plateau-patella angle �Angle > 29° (normal angle 21 -29°) ◦ MRI

Patellar Tendon Rupture • Acute Mgmt • Immobilization in extension • Non-Operative Tx • Incomplete ruptures • Immobilization in extension for 3 -6 weeks • Gradual flexion after pt is able to: • Achieve good quads muscle control • Perform a straight-leg raise without discomfort • Expect following sequelae: • Weakness • Extensor lag • Quadriceps atrophy

Patellar Tendon Rupture �Operative Tx ◦ Complete ruptures �Early repair leads to better results �Within 1 week �Beyond 72 hrs, retraction may make repair more difficult �Repair techniques vary �No single technique shown to be better than any other �Depends on location of rupture �Midsubstance tear • End-to-end repair �Tear at/near osteotendinous jxn (most common site) • Drill holes in patella • +/- reinforcing cerclage �Collagen remodels into organized longitudinal structure over 3 to 6 months �Post operatively- active knee flexion with passive knee extension using heel slides allowed immediately. Open chain exercises to be allowed later.

Patellar Tendon Repair • Midline incision from midpatella to tibial tubercle • Tendon edges debrided • 2 No. 5 nonabsorbable sutures woven Bunnell fashion passed through one of three transpatellar holes • Transverse 3. 2 mm drill hole 1 cm posterior to tibial tubercle • Heavy nonabsorbable suture placed through hole then transversely through quad tendon superior to patella • Tension applied to sutures, xray used to confirm patella height • Suture tied over patella • No. 2 sutures to oversew repair • If avulsed from tibia pass Bunnell sutures through second drill hole in tibia
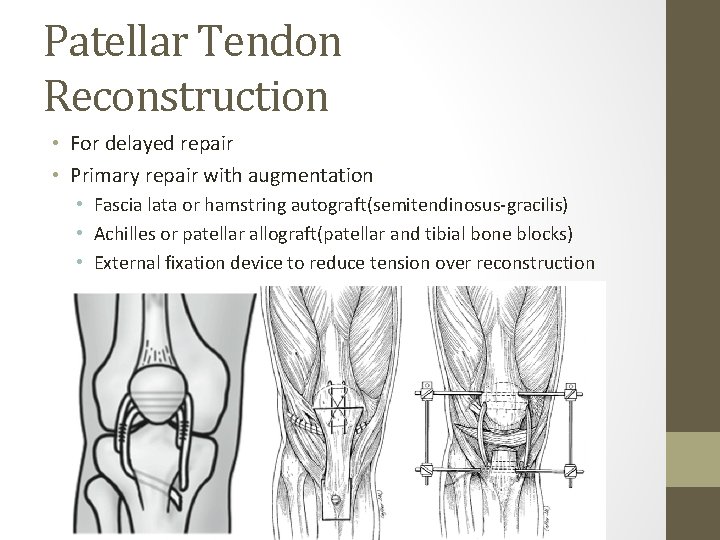
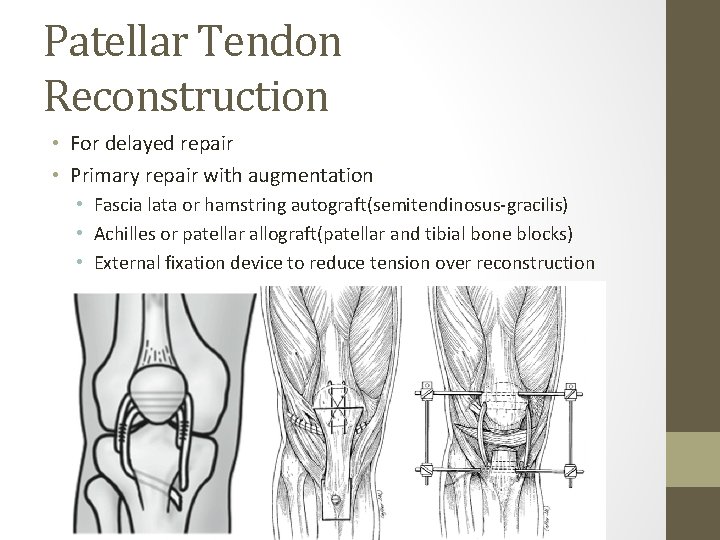
Patellar Tendon Reconstruction • For delayed repair • Primary repair with augmentation • Fascia lata or hamstring autograft(semitendinosus-gracilis) • Achilles or patellar allograft(patellar and tibial bone blocks) • External fixation device to reduce tension over reconstruction
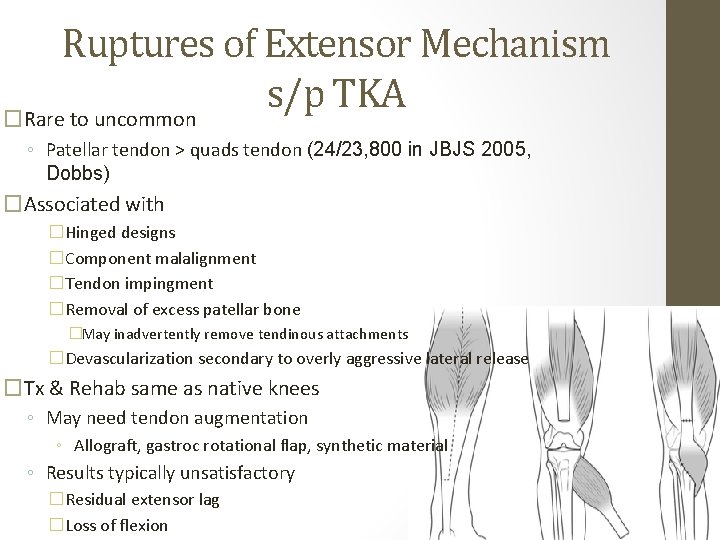
Ruptures of Extensor Mechanism s/p TKA �Rare to uncommon ◦ Patellar tendon > quads tendon (24/23, 800 in JBJS 2005, Dobbs) �Associated with �Hinged designs �Component malalignment �Tendon impingment �Removal of excess patellar bone �May inadvertently remove tendinous attachments �Devascularization secondary to overly aggressive lateral release �Tx & Rehab same as native knees ◦ May need tendon augmentation ◦ Allograft, gastroc rotational flap, synthetic material ◦ Results typically unsatisfactory �Residual extensor lag �Loss of flexion
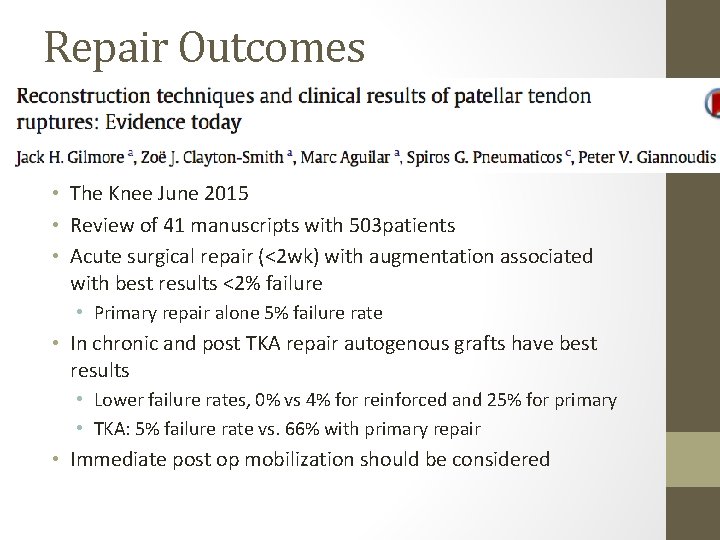
Repair Outcomes • The Knee June 2015 • Review of 41 manuscripts with 503 patients • Acute surgical repair (<2 wk) with augmentation associated with best results <2% failure • Primary repair alone 5% failure rate • In chronic and post TKA repair autogenous grafts have best results • Lower failure rates, 0% vs 4% for reinforced and 25% for primary • TKA: 5% failure rate vs. 66% with primary repair • Immediate post op mobilization should be considered
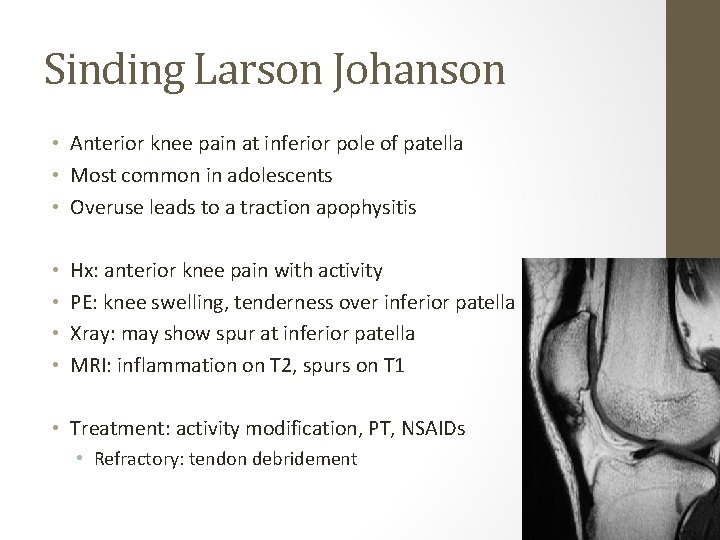
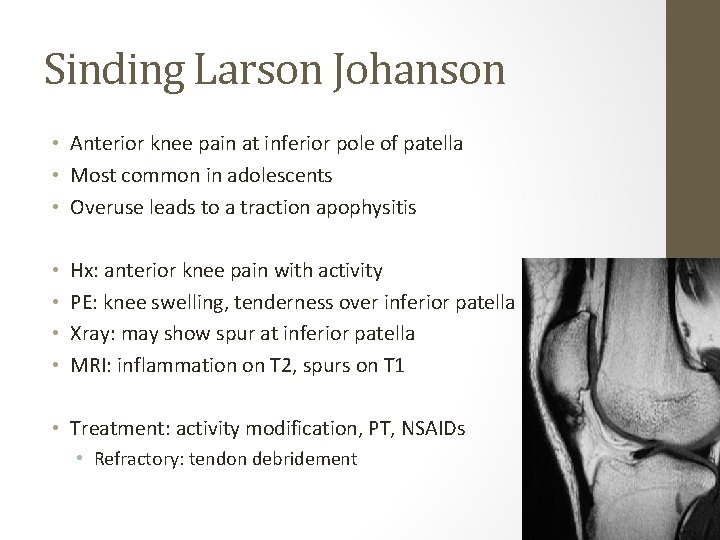
Sinding Larson Johanson • Anterior knee pain at inferior pole of patella • Most common in adolescents • Overuse leads to a traction apophysitis • • Hx: anterior knee pain with activity PE: knee swelling, tenderness over inferior patella Xray: may show spur at inferior patella MRI: inflammation on T 2, spurs on T 1 • Treatment: activity modification, PT, NSAIDs • Refractory: tendon debridement
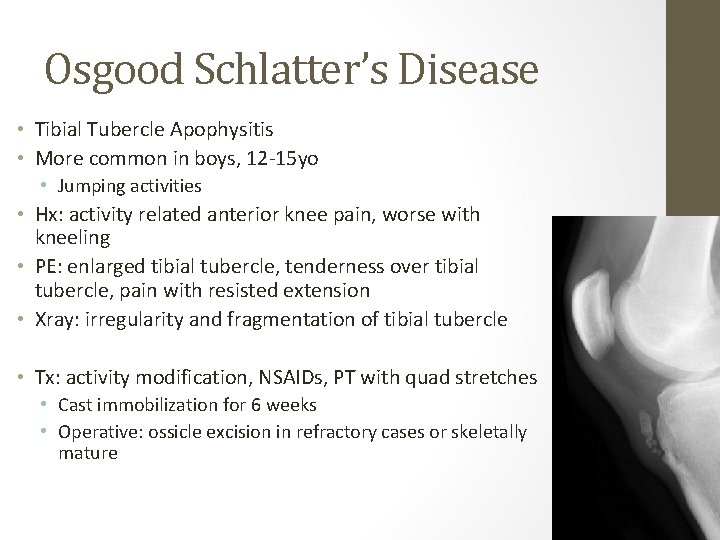
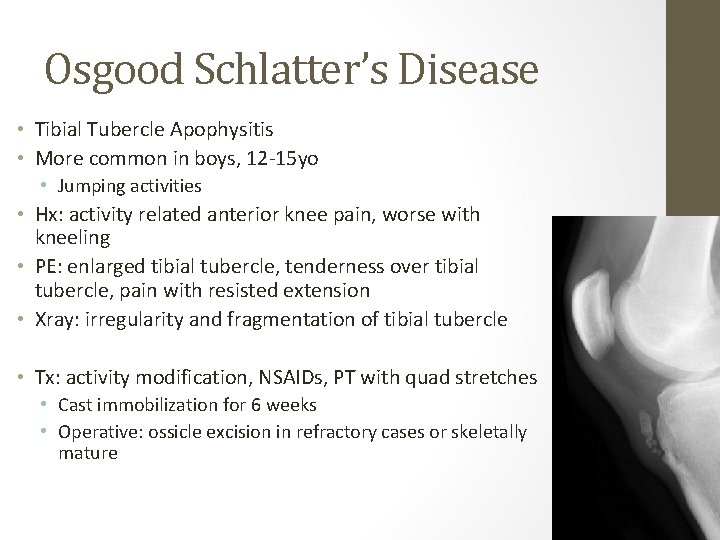
Osgood Schlatter’s Disease • Tibial Tubercle Apophysitis • More common in boys, 12 -15 yo • Jumping activities • Hx: activity related anterior knee pain, worse with kneeling • PE: enlarged tibial tubercle, tenderness over tibial tubercle, pain with resisted extension • Xray: irregularity and fragmentation of tibial tubercle • Tx: activity modification, NSAIDs, PT with quad stretches • Cast immobilization for 6 weeks • Operative: ossicle excision in refractory cases or skeletally mature
References • Ilan DI, Tejwani N, Keschner M, Leibman M. “Quadriceps Tendon Rupture. ” JAAOS 2003. 11(3): 192 -200. • Matava MJ. “Patellar Tendon Ruptures. ” JAAOS 1996. 4(6): 287 -296. • Rauh MA, Parker RD. “Patellar and Quadriceps Tendinopathies and Ruptures. ” Orthopaedic Sports Medicine 3 rd Ed. • Yepes H, Tang M, Morris SF, Stanish WD. “Relationship Between Hypovascular Zones and Patterns of Ruptures of the Quadriceps Tendon. ” J Bone Joint Surg Am. 2008. 90: 2135 -2141. • Portner O, Pakzad H. “The evaluation of patellar height: a simple method. ” J Bone Joint Surg Am. 2011 Jan 5; 93(1): 73 -80. • Thévenin-Lemoine C, Ferrand M, Courvoisier A, Damsin JP, Ducou le Pointe H, Vialle R. “Is the caton-deschamps index a valuable ratio to investigate patellar height in children? ” J Bone Joint Surg Am. 2011 Apr; 93(8): e 35. • Parker DA, Dunbar JM, Rorabeck CH. “Extensor Mechanism Failure Associated With Total Knee Arthroplasty: Prevention and Management. ” JAAOS 2003: 11(4): 238 -247.
Questions �Which of the following rehabilitation methods has proven as effective as surgical treatment for the treatment of patellar tendinopathy (jumper’s knee)? � 1. Electrotherapy � 2. Concentric training � 3. Eccentric training � 4. Massage � 5. Taping
Preferred Response � #3 � Common treatments for patellar tendinopathy include rest, ice, electrotherapy, massage, taping, and injection. None has been demonstrated to be effective. Eccentric training has proven to be as effective as surgical treatment. Achilles insertional tendinopathy has also proven to respond to eccentric training. � References ◦ Bahr R, Loken S, et al: Surgical treatment compared with eccentric training for patellar tendinopathy (jumper’s knee): A randomized, controlled trial. J Bone Joint Surg Am 2006; 88: 1689 -1698. ◦ Coleman BD, Khan KM, Maffulli N, et al: Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 2000; 10: 2 -11.

A 35 -year-old male slips on a patch of ice and falls on a hyperflexed knee. He reports hearing a "pop" during the fall and was unable to bear weight on the knee immediately after the injury. He has a large knee effusion on examination. A radiograph is shown in Figure A. He undergoes operative repair of the injury with standard technique. Which of the active range of motion exercises is MOST appropriate in the immediate postoperative period? Topic Review Topic FIGURES: A 1. Leg extensions 2. Heel slides 3. Standing squats 4. Rear lunges 5. Seated leg press
PREFERRED RESPONSE ▼ 2 CORRECT DISCUSSION: The clinical presentation and radiographs are consistent with a patellar tendon rupture. In the case of patellar or quad tendon repair, the initial focus is on regaining range of motion while protecting the repair. Non-weightbearing movement exercises like heel slides are encouraged. This can incorporate active knee flexion with passive extension. Alternatively, active knee flexion in the prone position with passive knee extension can be performed. Open chain strengthening exercises such as leg extensions are started later, as are weight bearing resistance exercises like squats, lunges and leg press. Matava presents a level 5 review on patellar tendon ruptures and states that active knee extension is permitted at 3 weeks postoperatively. West et al present level 4 evidence of 30 patellar tendon ruptures treated with direct repair supplemented with a cerclage technique. They report that 100% of the patients returned to a preinjury level of activity at 6 months. Illustration A shows a video demonstration of a heel slide in the supine position. Alternatively, they can be performed with the heel against the wall and the opposite leg assisting with leg extension as shown in the video demonstration in Illustration B. Illustrations: A B REFERENCES: 1. Matava MJ. Patellar tendon ruptures. J Am Acad Orthop Surg. 1996 Nov; 4(6): 287 -296. PMID: 10797196 (Link to Abstract) 2. West JL, Keene JS, Kaplan LD. Early motion after quadriceps and patellar tendon repairs: outcomes with singlesuture augmentation. Am J Sports Med. 2008 Feb; 36(2): 316 -23. Epub 2007 Oct 11. PMID: 17932403 (Link to Abstract)

A 24 -year-old basketball player feels a painful "pop" in his knee when landing from a rebound. He develops immediate swelling, pain, and inability to extend his knee. A lateral radiograph is shown in Figure A. Proper management should include: Topic Review Topic FIGURES: A 1. Long leg cast in full extension 2. Long leg cast at 30 -degrees of flexion 3. Tibial tubercle osteotomy 4. Primary surgical repair 5. Rest, ice, compressive dressing, elevation followed by slow return to play
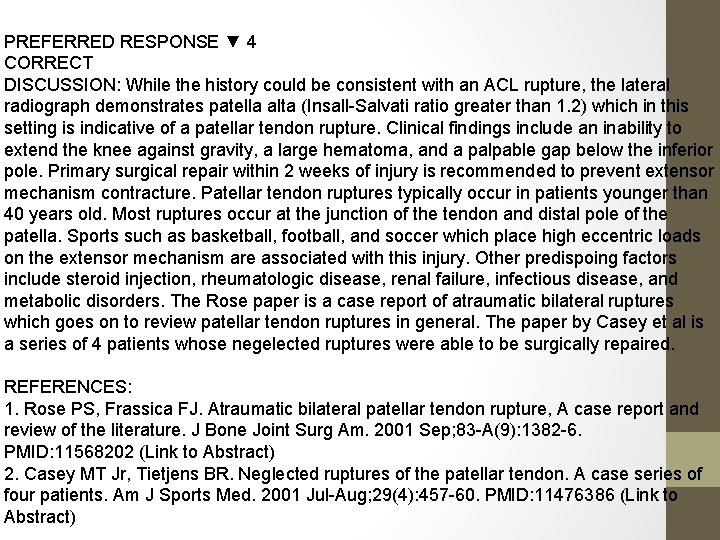
PREFERRED RESPONSE ▼ 4 CORRECT DISCUSSION: While the history could be consistent with an ACL rupture, the lateral radiograph demonstrates patella alta (Insall-Salvati ratio greater than 1. 2) which in this setting is indicative of a patellar tendon rupture. Clinical findings include an inability to extend the knee against gravity, a large hematoma, and a palpable gap below the inferior pole. Primary surgical repair within 2 weeks of injury is recommended to prevent extensor mechanism contracture. Patellar tendon ruptures typically occur in patients younger than 40 years old. Most ruptures occur at the junction of the tendon and distal pole of the patella. Sports such as basketball, football, and soccer which place high eccentric loads on the extensor mechanism are associated with this injury. Other predispoing factors include steroid injection, rheumatologic disease, renal failure, infectious disease, and metabolic disorders. The Rose paper is a case report of atraumatic bilateral ruptures which goes on to review patellar tendon ruptures in general. The paper by Casey et al is a series of 4 patients whose negelected ruptures were able to be surgically repaired. REFERENCES: 1. Rose PS, Frassica FJ. Atraumatic bilateral patellar tendon rupture, A case report and review of the literature. J Bone Joint Surg Am. 2001 Sep; 83 -A(9): 1382 -6. PMID: 11568202 (Link to Abstract) 2. Casey MT Jr, Tietjens BR. Neglected ruptures of the patellar tendon. A case series of four patients. Am J Sports Med. 2001 Jul-Aug; 29(4): 457 -60. PMID: 11476386 (Link to Abstract)
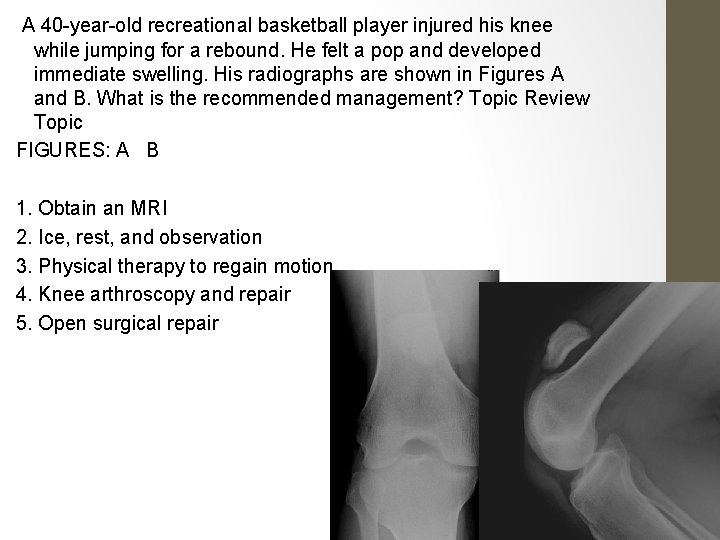
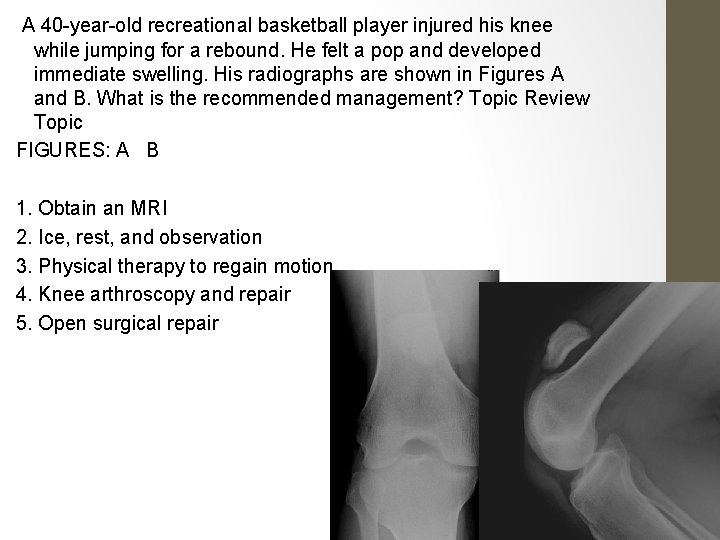
A 40 -year-old recreational basketball player injured his knee while jumping for a rebound. He felt a pop and developed immediate swelling. His radiographs are shown in Figures A and B. What is the recommended management? Topic Review Topic FIGURES: A B 1. Obtain an MRI 2. Ice, rest, and observation 3. Physical therapy to regain motion 4. Knee arthroscopy and repair 5. Open surgical repair

PREFERRED RESPONSE ▼ 5 CORRECT DISCUSSION: The mechanism of injury and radiographs are consistent with a complete patellar tendon rupture. The radiographs reveal a patella alta, which in this case is indicative of complete patellar tendon rupture. This can be quantified by using the Insall. Salvati ratio (patellar tendon length / patellar bone length): PTL/PBL normal =1, >1. 2 is patella alta, <0. 8 is patella baja) with the knee flexed to 30 degrees. The reference by Brooks et al reviews the diagnosis and treatment of extensor mechanism ruptures. A complete patellar tendon rupture requires open surgical repair. A partial tear with an intact extension mechanism may be treated conservatively. An MRI is not needed for diagnosis. REFERENCES: 1. Brooks P. Extensor mechanism ruptures. Orthopedics. 2009 Sep; 32(9). PMID: 19751001 (Link to Abstract) 2. Hyman J, Rodeo S, Wickiewicz T. Patellofemoral Tendinopathies. in De. Lee, Drez & Miller: De. Lee and Drez's Orthopaedic Sports Medicine, edition 2. 2003, pp 1850 -1854. 3. Orthopaedic Knowledge Update: Sports Medicine 3. 9, Orthopaedic Knowledge Update 9, Garrick JG (Editor). Published by American Academy of Orthopaedic Surgeons, Rosemont IL. Copyright 2004

Which of the following rehabilitation exercises provides for restoration of range of motion while limiting stress on the repair of a ruptured patellar tendon? Topic Review Topic 1. Active open chain flexion, active closed chain extension 2. Passive flexion, active closed chain extension 3. Active open chain flexion, passive extension 4. Active closed chain flexion, passive extension 5. Active open chain flexion, active open chain extension
PREFERRED RESPONSE ▼ 4 DISCUSSION: To avoid stress on the repair, no form of active extension should be used for at least 4 -6 weeks. Closed versus open chain refers to strengthening exercises, not just range of motion. Closed kinetic chain exercise occurs when the terminal or distal segment of an appendage is fixed (squat, leg press, pull-up). Open kinetic chain exercise occurs when the terminal or distal segment is free to move (leg extension / hamstring curl) – this type of exercise tends to produce greater shear stress and is therefore avoided in many standardized rehab protocols. In the case of patellar or quad tendon repair, active closed chain flexion may be allowed with passive extension. Many of the rehab studies have looked at the effects of various exercises with respect to ACL graft strain. Stuart et al. showed that for common closed chain exercises like squats and lunges the shear force is predominantly posterior and therefore may not stress an ACL graft. Wilk et al study showed the differences in contact forces and EMG activity for various closed and open chain exercises. Open chain terminal knee extension provided the greatest anterior shear. REFERENCES: Stuart MJ, Meglan DA, Lutz GE, Growney ES, An KN. Comparison of intersegmental tibiofemoral joint forces and muscle activity during various closed kinetic chain exercises. Am J Sports Med 1996; 24: 792 -799. PMID: 8947402 (Link to Abstract) 2. Wilk KE, Escamilla RF, Fleisig GS, Barrentine SW, Andrews JR, Boyd ML. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am J Sports Med