QAPI Quality Assurance Performance Improvement 11 th Scope



- Slides: 37

QAPI Quality Assurance Performance Improvement
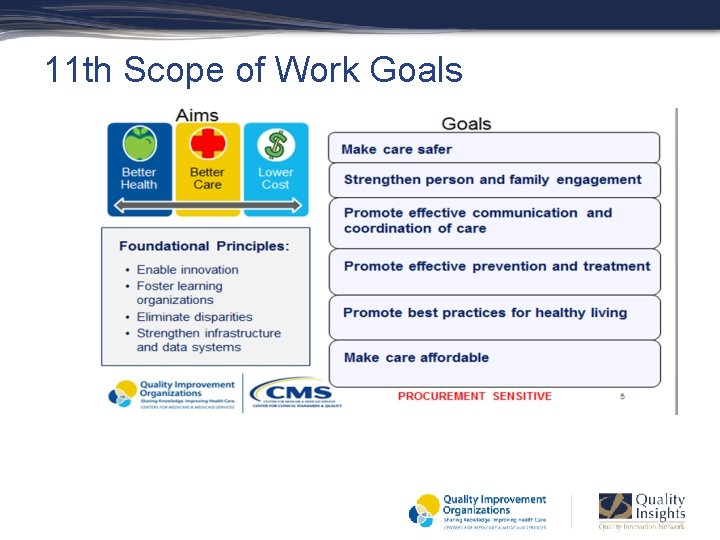
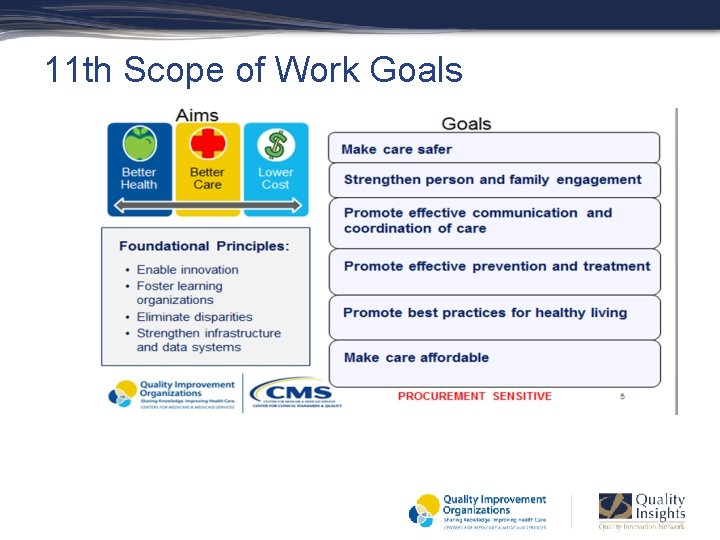
11 th Scope of Work Goals
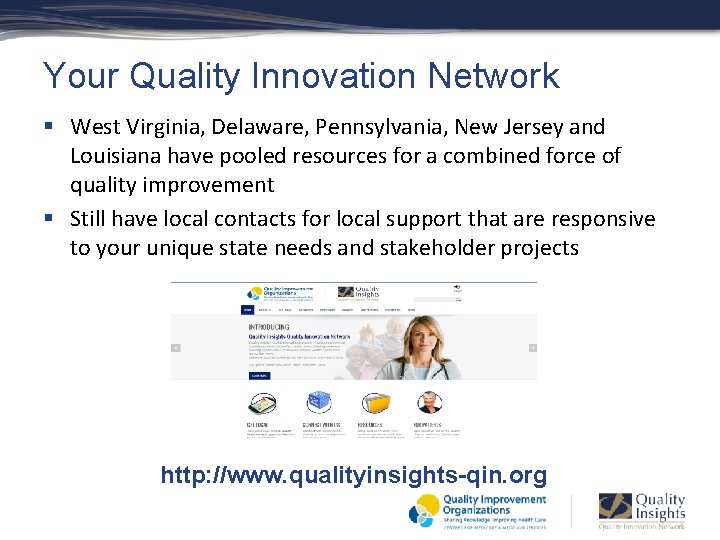
Your Quality Innovation Network § West Virginia, Delaware, Pennsylvania, New Jersey and Louisiana have pooled resources for a combined force of quality improvement § Still have local contacts for local support that are responsive to your unique state needs and stakeholder projects http: //www. qualityinsights-qin. org
Quality Assurance Performance Improvement (QAPI) § Mandated as part of the Affordable Care Act § Expands current regulations for QAA § Sets expectation for a sound, basic plan for QAPI that will support systems of care and quality of life in every nursing home § Final Rule expected….
Definitions § Quality Assessment – an evaluation of a process to determine if a defined standard of quality is being achieved § Quality Assurance – the organizational structure, processes and procedures designed to ensure that care practices are consistently applied § Quality Improvement (Process or Performance Improvement) – an ongoing interdisciplinary process that is designed to improve the delivery of services and resident outcomes
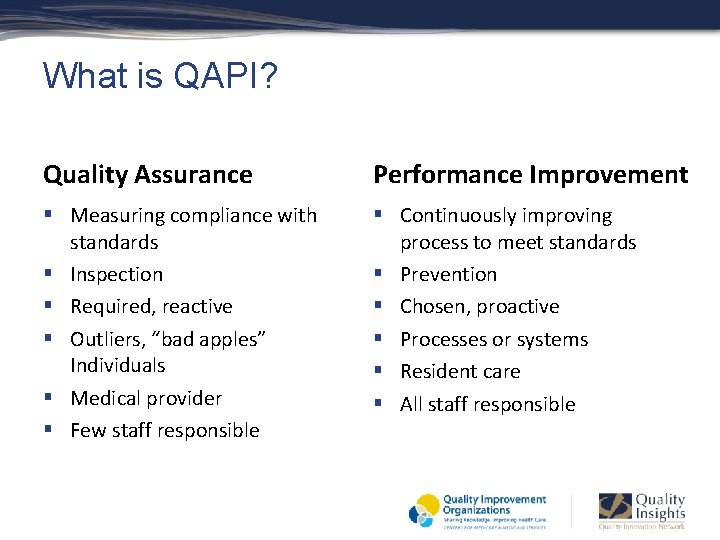
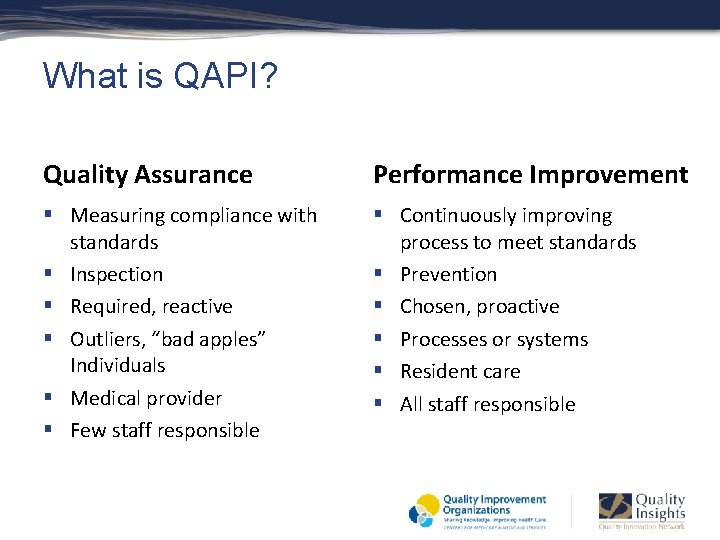
What is QAPI? Quality Assurance Performance Improvement § Measuring compliance with standards § Inspection § Required, reactive § Outliers, “bad apples” Individuals § Medical provider § Few staff responsible § Continuously improving process to meet standards § Prevention § Chosen, proactive § Processes or systems § Resident care § All staff responsible
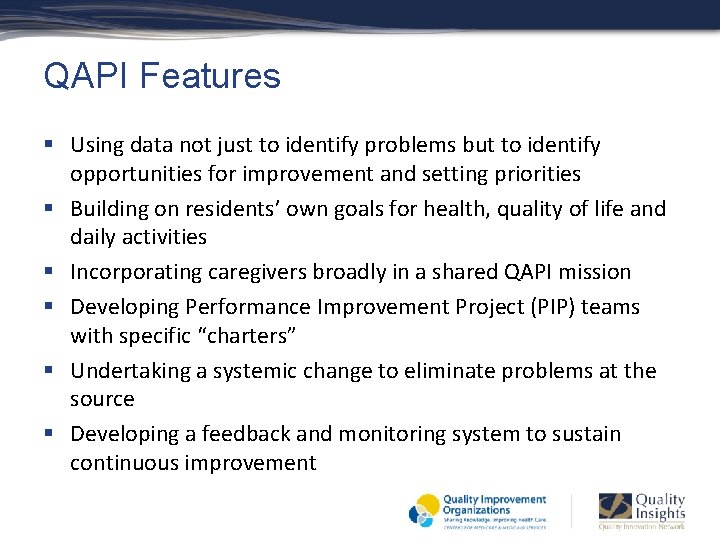
QAPI Features § Using data not just to identify problems but to identify opportunities for improvement and setting priorities § Building on residents’ own goals for health, quality of life and daily activities § Incorporating caregivers broadly in a shared QAPI mission § Developing Performance Improvement Project (PIP) teams with specific “charters” § Undertaking a systemic change to eliminate problems at the source § Developing a feedback and monitoring system to sustain continuous improvement
5 Elements of QAPI § § § Design and Scope – ongoing and comprehensive Governance and Leadership Feedback, Data Systems and Monitoring Performance and Improvement Projects Systemic Analysis and Systemic Action
5 Elements of QAPI § Design and Scope – – – Comprehensive and ongoing plan Includes all departments and functions Addresses safety, quality of care, quality of life, resident choice Based on best available evidence Written QAPI plan
5 Elements of QAPI § Governance and Leadership – Systemic approach to gather input from staff, residents and stakeholders – buy-in and support – Sufficient resources – money, time, staff, etc. – Ongoing and consistent staff training on QAPI – Non-punitive culture – Sustainability
5 Elements of QAPI § Feedback, Data monitoring Systems and Monitoring – – – Multiple sources, including resident and staff Benchmarking and targeting Adverse events Establish goals Ability to analyze, interpret and translate data into meaningful actionable information
5 Elements of QAPI § Performance Improvement Projects – Prioritize topics – Improve care or services in areas identified as needing improvement – Gather information systematically to clarify issues or problems
5 Elements of QAPI § Systematic Analysis and Systemic Action – Organized approach to determine how an identified problem may be caused – How did the system cause the problem – Improvement of systems and processes – Use of PDSA, RCA to improve systems and prevent future adverse events

“Not all change is improvement, but all improvement is change. ” Donald Berwick, MD Former CMS Administrator
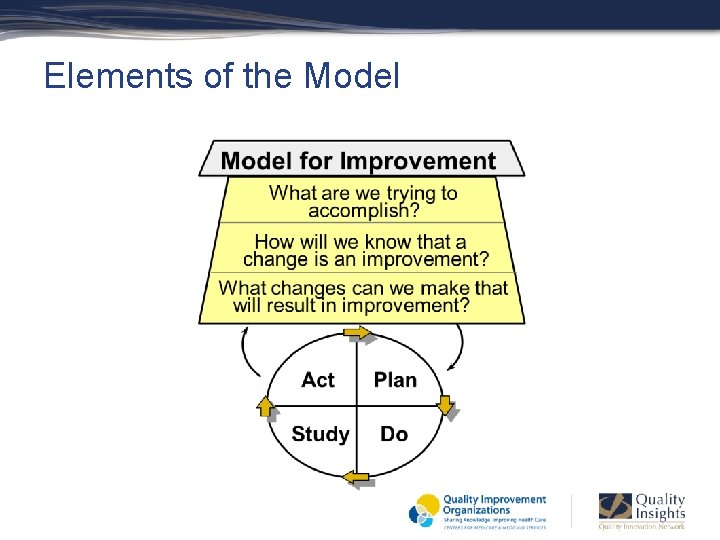
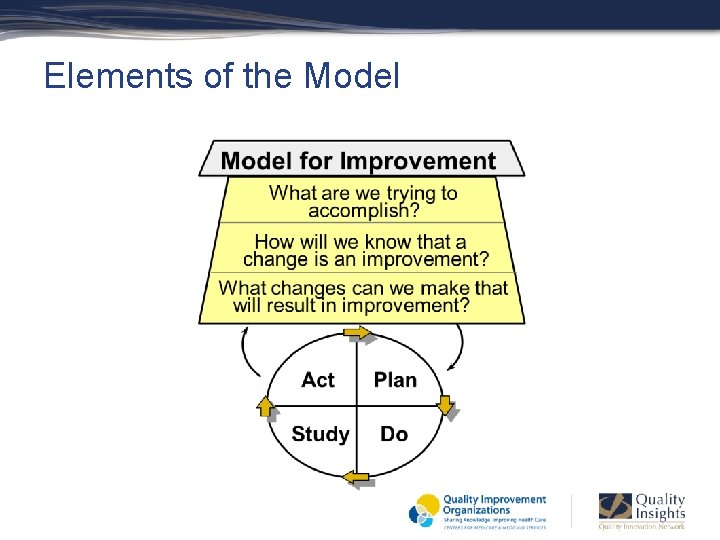
Elements of the Model
What Are We Trying to Accomplish? § § § Improvement requires setting goals or AIMs Agreeing on the aim is crucial Goals or AIMs keep everyone on track They define the desired result or purpose Are guides to action
Setting Stretch Goals (AIMS) § Examples: – Reduce the injury rate for residents in our household by 50 percent in 12 months – Reduce the use of antipsychotic medications by 50 percent in 12 months – Reduce complaints about meals by 75 percent in 12 months – Improve Pain LS QM by 25 percent in 3 months – Improve Pneumonia Vaccine rate by 50 percent in 6 months
How Will We Know a Change is an Improvement § § § Measurement for learning and process improvement Starting point for comparison of data Systematic gathering of information Gather objective data free from bias or opinion Personal observations may influence the results by seeing what we want to see or what we expect to happen
Data Collection § § § What type of data do we need How can we collect data with minimum effort Seek usefulness, not perfection Set a time period for data collection Collect baseline data
Examples § Where in the process can we get this data to determine why we have a high Antipsychotic LS QM rate? § Who is ordering antipsychotic medications § Has there been a change in staffing that is causing an increase in antipsychotic med usage § How do we know non-pharmacological interventions for pain/behaviors are effective § Are most transfers to a hospital made by a covering MD
Prioritize PIPS § Review QM report, NH Compare, pharmacy report § Staff, resident and family surveys § Begin with problems you feel are easy to solve then move to more complicated issues § Not all problems require a PIP
PIP Team § “Charter” a team § Specific written plan to explore the problem § PIP Team –staff closest to the issue – i. e. small group activities – include NAs and activity aides § What happened to allow the problem to occur § What change in the process can we make to prevent the problem in the future
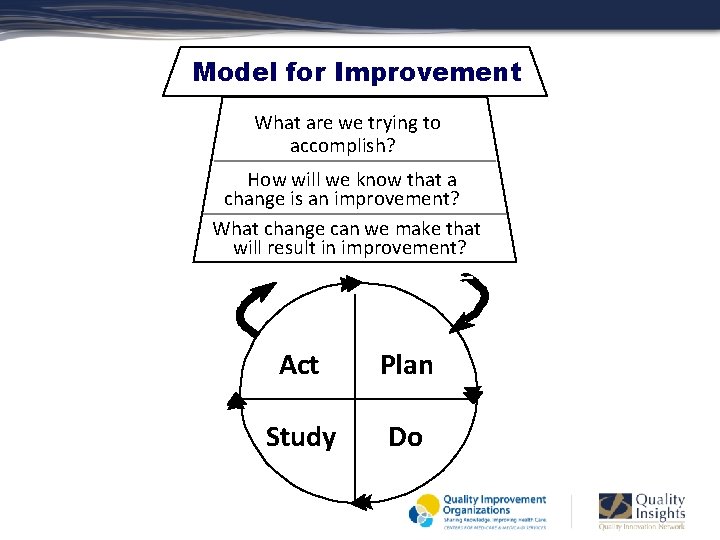
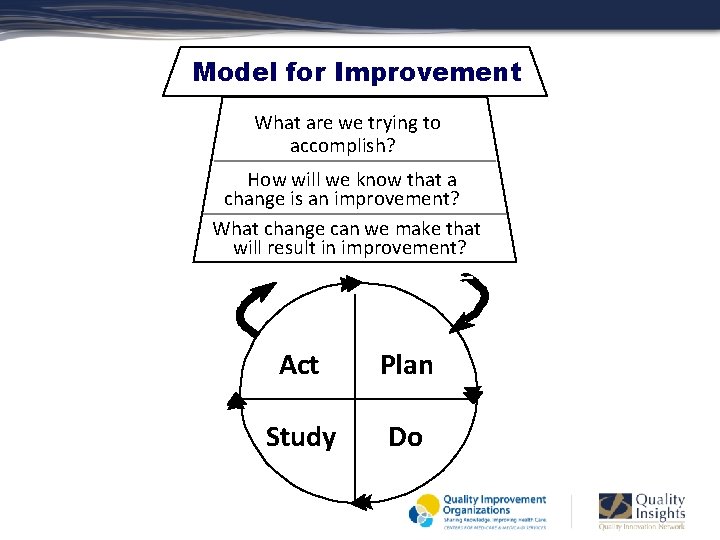
Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? Act Plan Study Do
PDSA Cycle § PLAN – Plan the test, make predictions about what will happen and why § DO – Carry out the plan on a small scale, document problems and unexpected observations § STUDY – Analyze the data, compare the data to your predictions § ACT – Decide next steps of adopting change or plan next test
Pilot Test § § § Test your action on a small scale Test over a short time period Observe the consequences Did staff like the new solution Evaluate
How Will We Know that a Change is an Improvement? § Three types of measures: – Outcome measures – voice of the customer – resident, family, staff – Process measures – the parts/systems performing as planned (residents with decrease antipsychotics, wt. loss, falls) – Balancing measures – looking at system from different direction, have improved changes caused new problems in another part of the system (reducing antipsychotics causing activity disruption, has change in meal times caused therapy and/or department issues)
What Change Can We Make That Will Result in Improvement § § All changes do not lead to improvement Improve work flow – weekly skin checks Optimize inventory – adequate adaptive utensils for meals Error Proofing – calibrate scale for accurate weights
Test the Change § Increase your belief that the change will result in improvement § Opportunity for learning from “failures” § Learn how to adapt the change to conditions in different environments § Minimize resistance to implementation
Attributes of Changes that are Readily Adopted* The change has a clear advantage over the current system The change is compatible with the current system and values The change is easy to try and reverse Understanding and adapting the change requires minimal complexity § The change and its impact can be observed § § *From Everett Rogers “Diffusion of Innovations”
Quality Improvement § § § Quality improvement is not an extra thing to do Monitor your QM report, staff and resident surveys, etc. Know and understand your numbers Share data with staff Quality improvement will improve your quality measure rates Quality improvement will improve resident, staff and family satisfaction
QAPI Summary § All of QAPI may not be new to your home § Think of your entire home as you assess your QAPI efforts § Involve staff directly working in a process in order to improve that process § Communication about QAPI should continue throughout your entire home § Solicit resident and family viewpoints about their quality experience
Composite Score Content § 13 long-stay quality measures from Casper data § Measures: Falls with injury, UTI, Pain, Pressure Ulcer, Incontinence, Foley catheter, Physical Restraints, ADL, Wt. loss, Depression, Antipsychotic Meds § Flu and Pneumococcal vaccines § All represent larger systems within long-term care settings § Sum of 13 numerators divided by sum of 13 denominators and multiplied by 100 = Composite Score
NNHQCC Composite Measure Score § Goal based on nearly 10% of nursing homes nationally having a composite score of 6 or less – Best Practice § Improving processes to impact QMs and achieve score of 6 or below may impact nursing home Star rating § QIN-QIO will assist you in improving processes
Centers for Medicare & Medicaid Services (CMS) Transforming nursing homes through continuous attention to quality of care and quality of life QAPI Resources: http: //go. cms. gov/nhqapi
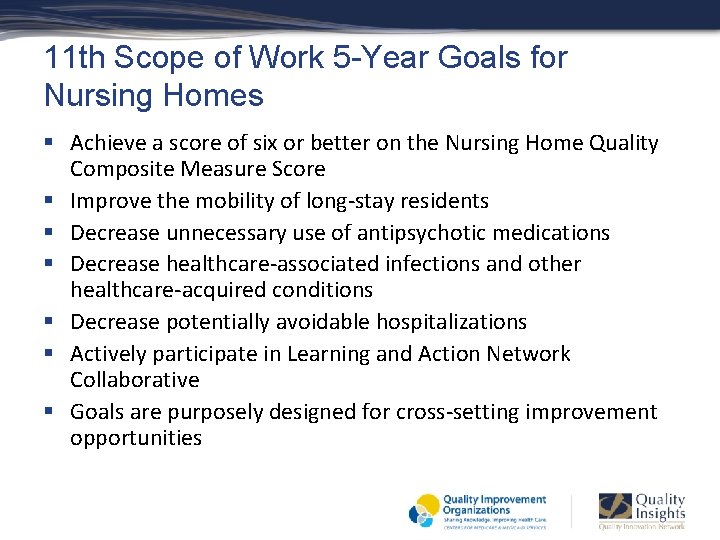
11 th Scope of Work 5 -Year Goals for Nursing Homes § Achieve a score of six or better on the Nursing Home Quality Composite Measure Score § Improve the mobility of long-stay residents § Decrease unnecessary use of antipsychotic medications § Decrease healthcare-associated infections and other healthcare-acquired conditions § Decrease potentially avoidable hospitalizations § Actively participate in Learning and Action Network Collaborative § Goals are purposely designed for cross-setting improvement opportunities
Thank You Toni Daly, RN, Project Coordinator Phone: 1. 877. 346. 6180, ext. 7843 E-mail: mdaly@wvmi. org Penny Imes, RN, Project Coordinator E-mail: pimes@wvmi. org Phone: 1. 877. 346. 6180, ext. 7644

This material was prepared by Quality Insights, the Medicare Quality Innovation Network-Quality Improvement Organization for West Virginia, Pennsylvania, Delaware, New Jersey and Louisiana under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U. S. Department of Health and Human Services. The contents presented do not necessarily reflect CMS policy. Publication number QI-C 2 -120814