PYOGENIC INFECTIONS AND TYPHOID Dr Kiran H S























- Slides: 88

PYOGENIC INFECTIONS AND TYPHOID Dr. Kiran H S Assistant Proffessor Dept of Pathology
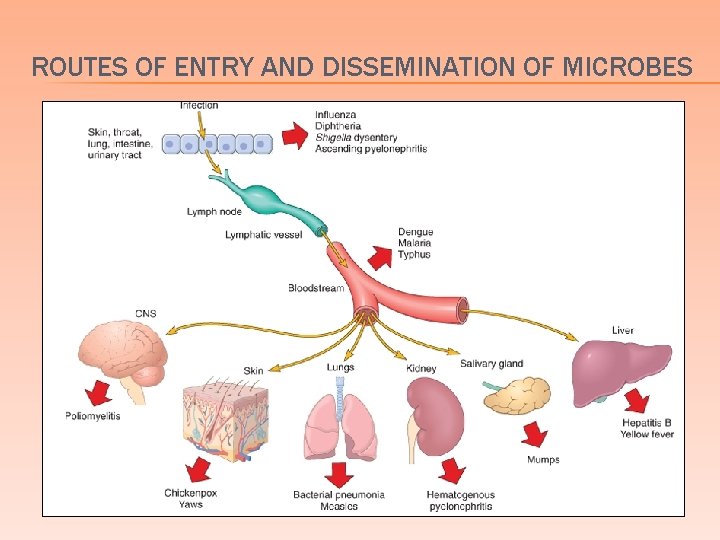
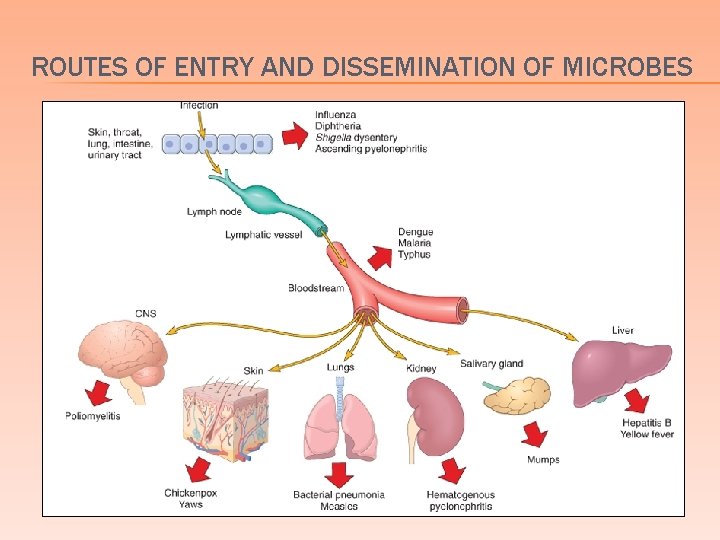
ROUTES OF ENTRY AND DISSEMINATION OF MICROBES
GRAM NEGATIVE AND POSITIVE BACTERIAL INFECTIONS 3
STAPHYLOCOCCUS AUREUS 4
TOXIN-RELATED DISEASES ASSOCIATED WITH STAPH. AUREUS � Toxic Shock syndrome � Scalded skin syndrome � Bullous impetigo � Food poisoning 5
1)TOXIC SHOCK SYNDROME (TSS) 6
TOXIC SHOCK SYNDROME � Caused by any of several related toxic exotoxins produced by S. aureus � TSST-1 � most frequently implicated exotoxin � staphylococcal enterotoxin B is 2 nd most frequently implicated � For illness to develop, an individual must be colonized or infected with a toxigenic strain of S. aureus and lack a protective level of antibody to the toxin 7
TOXIC SHOCK SYNDROME � Menstruation most common setting for TSS � May also be associated with barrier contraceptives, puerperium, septic abortion, non-obstetric gynecologic surgery and skin lesions � chemical or thermal burns, insect bites, varicella lesions and surgical wounds � Overt infection with S. aureus is not required for the development of TSS 8
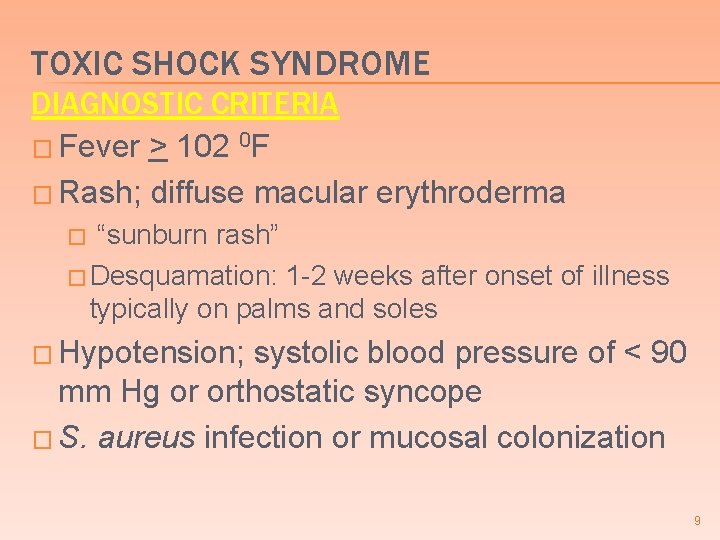
TOXIC SHOCK SYNDROME DIAGNOSTIC CRITERIA � Fever > 102 0 F � Rash; diffuse macular erythroderma “sunburn rash” � Desquamation: 1 -2 weeks after onset of illness typically on palms and soles � � Hypotension; systolic blood pressure of < 90 mm Hg or orthostatic syncope � S. aureus infection or mucosal colonization 9
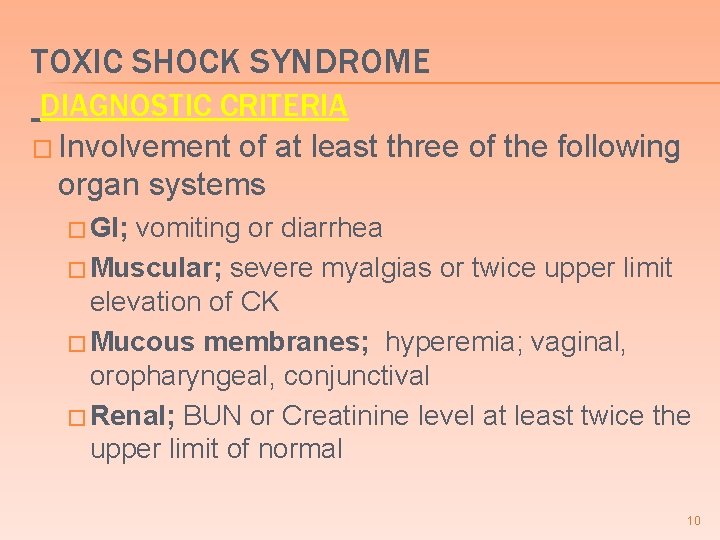
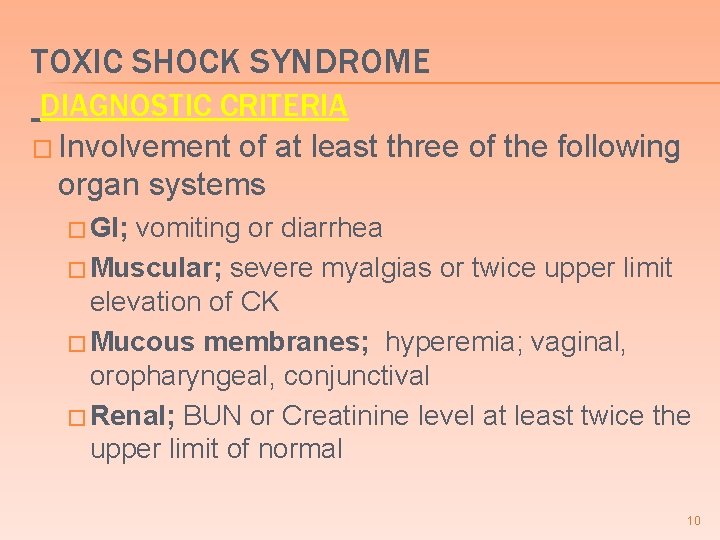
TOXIC SHOCK SYNDROME DIAGNOSTIC CRITERIA � Involvement of at least three of the following organ systems � GI; vomiting or diarrhea � Muscular; severe myalgias or twice upper limit elevation of CK � Mucous membranes; hyperemia; vaginal, oropharyngeal, conjunctival � Renal; BUN or Creatinine level at least twice the upper limit of normal 10
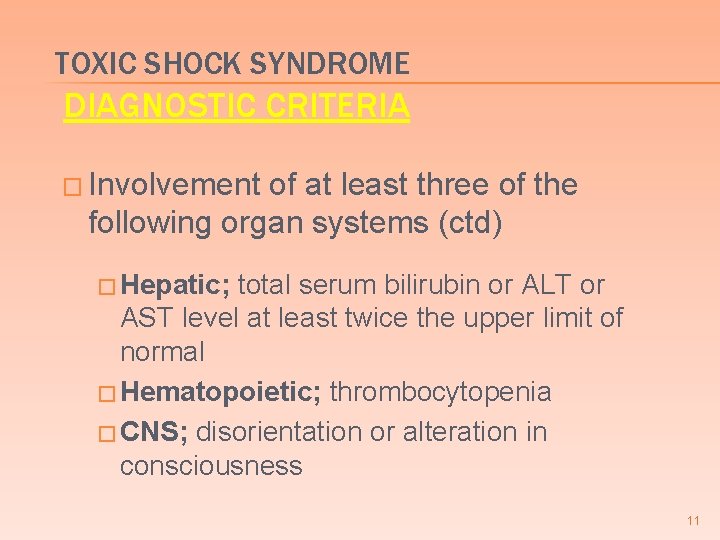
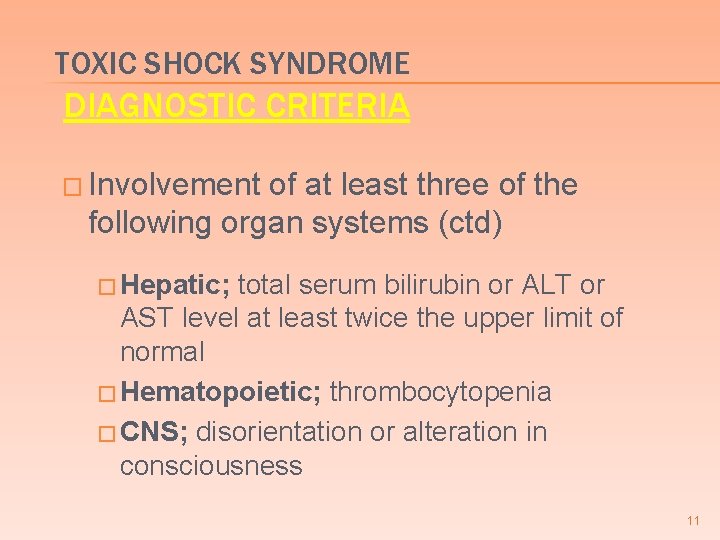
TOXIC SHOCK SYNDROME DIAGNOSTIC CRITERIA � Involvement of at least three of the following organ systems (ctd) � Hepatic; total serum bilirubin or ALT or AST level at least twice the upper limit of normal � Hematopoietic; thrombocytopenia � CNS; disorientation or alteration in consciousness 11
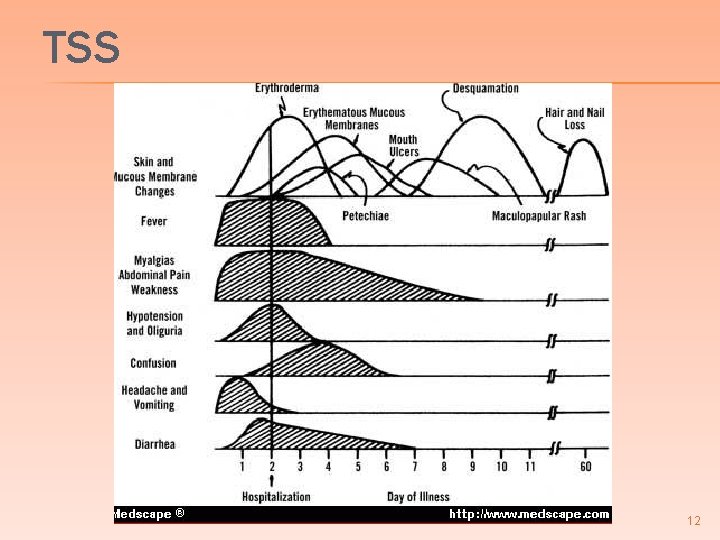
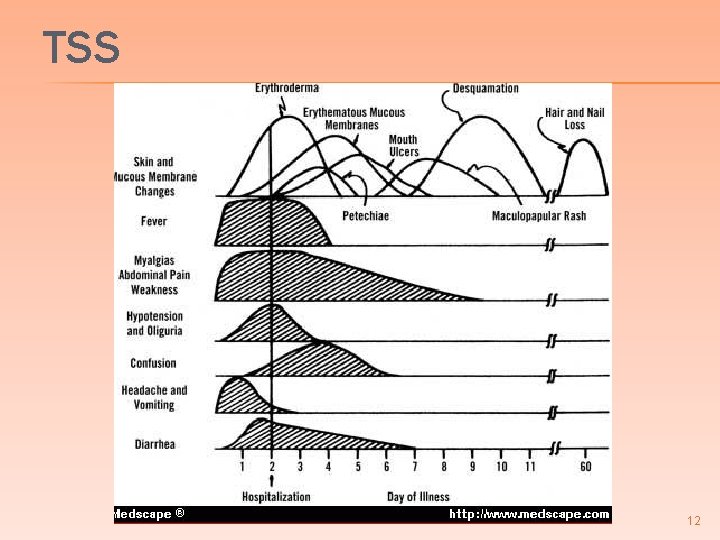
TSS 12
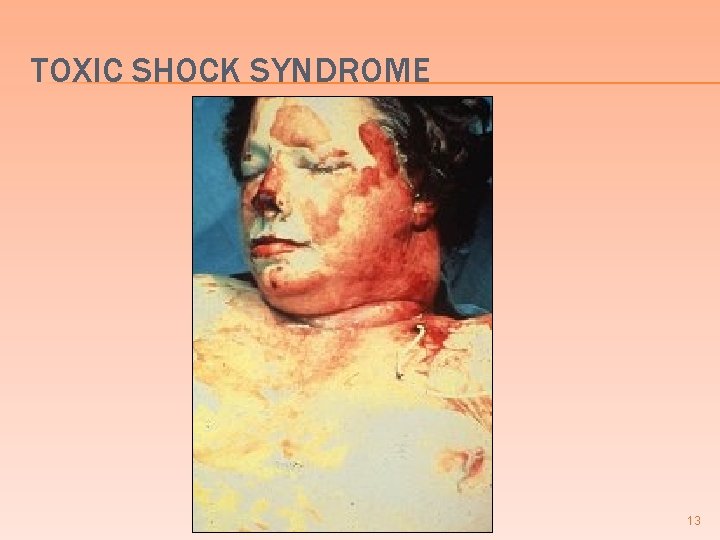
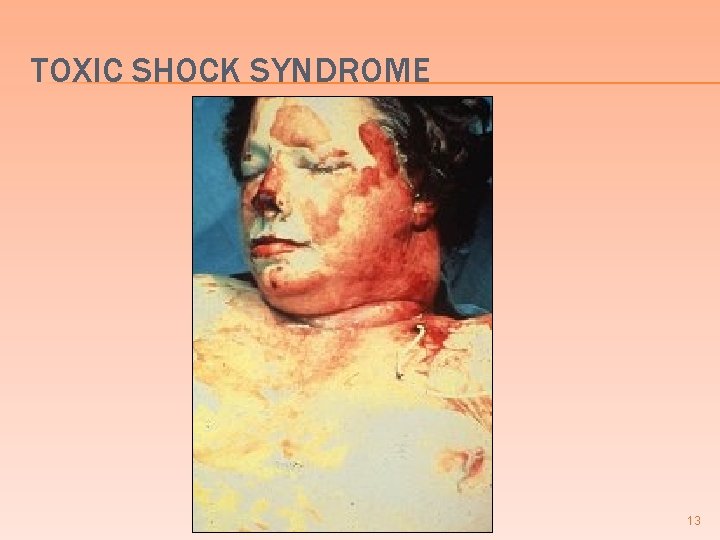
TOXIC SHOCK SYNDROME 13

2)SCALDED SKIN SYNDROME 14

SCALDED SKIN SYNDROME Wide spread skin disease due to epidermolytic toxin � Separation of epidermis at stratum granulosum � Children and immunocompromised adults � � � rare in immunocompetent adults because of the presence of antibodies Begins with erythematous rash periorbital and perioral areas and spreads to the trunk and limbs generalized bulla formation 15
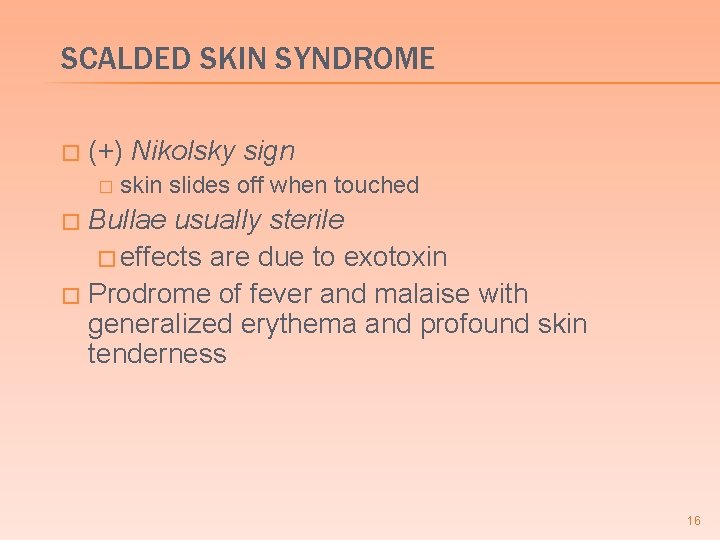
SCALDED SKIN SYNDROME � (+) Nikolsky sign � skin slides off when touched Bullae usually sterile � effects are due to exotoxin � Prodrome of fever and malaise with generalized erythema and profound skin tenderness � 16
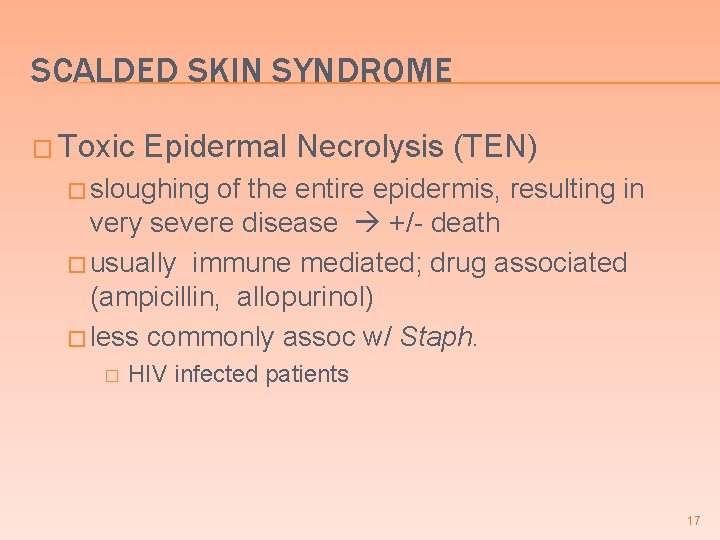
SCALDED SKIN SYNDROME � Toxic Epidermal Necrolysis (TEN) � sloughing of the entire epidermis, resulting in very severe disease +/- death � usually immune mediated; drug associated (ampicillin, allopurinol) � less commonly assoc w/ Staph. � HIV infected patients 17

SCALDED SKIN SYNDROME STAPHYLOCOCCUS AUREUS 18

NIKOLSKY’S SIGN 19

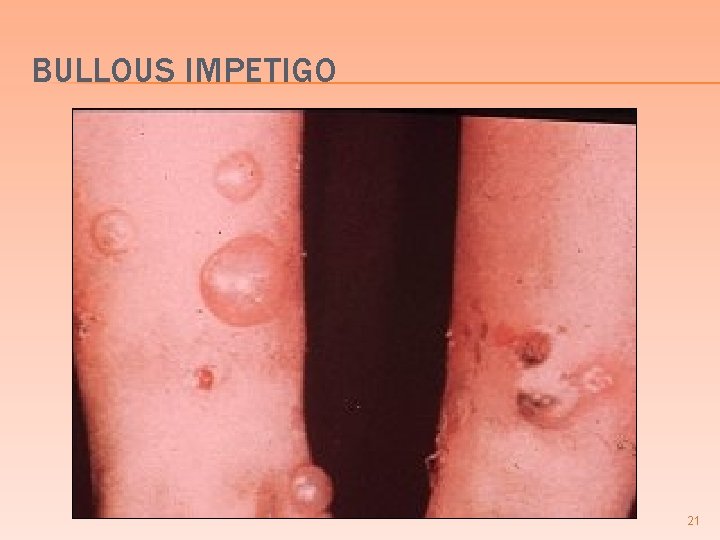
3) BULLOUS IMPETIGO � More localized & milder than scalded skin syndrome � Young children � Large friable clear to cloudy bulla honey yellow crusts � (+) Nikolsky sign � S. aureus can be recovered from lesions 20
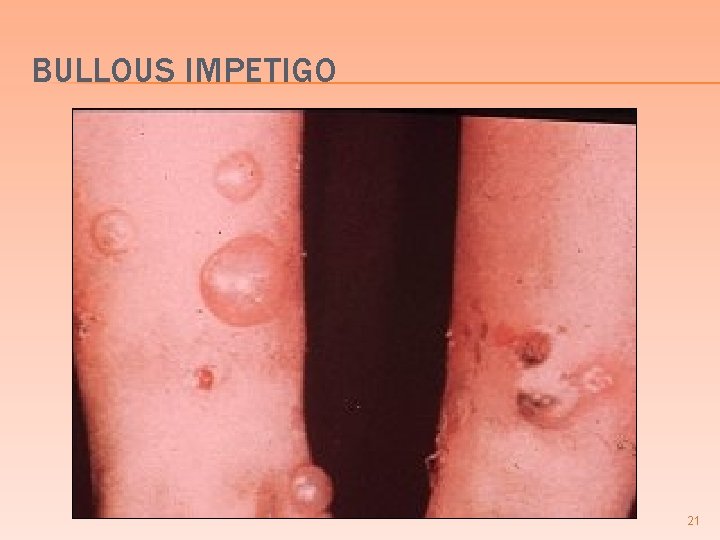
BULLOUS IMPETIGO 21
4) STAPHYLOCOCCAL FOOD POISONING 22

STAPHYLOCOCCAL FOOD POISONING � Due to preformed heat-stable enterotoxin produced in foods prior to ingestion � Custard filled baked goods & processed meats � More common in summer months � Symptoms occur between 2 -6 hours after ingestion of contaminated food 23
STAPHYLOCOCCAL FOOD POISONING � Symptoms � nausea, begin abruptly vomiting, crampy abdominal pain, and diarrhea � Self limited � Culture food, not patient 24
STAPHYLOCOCCAL OSTEOMYELITIS 25

STAPHYLOCOCCAL OSTEOMYELITIS S. aureus the most common cause of osteomyelitis � Usually secondary to hematogenous spread to bone � � less commonly due to trauma (open fx) or extension from adjacent infected tissue Acute osteomyelitis may be cured by antibiotics alone � Chronic osteomyelitis requires surgical debridement of infected bone + antibiotics � 26

STAPHYLOCOCCAL OSTEOMYELITIS 27

CUTANEOUS STAPHYLOCOCCAL INFECTIONS 28
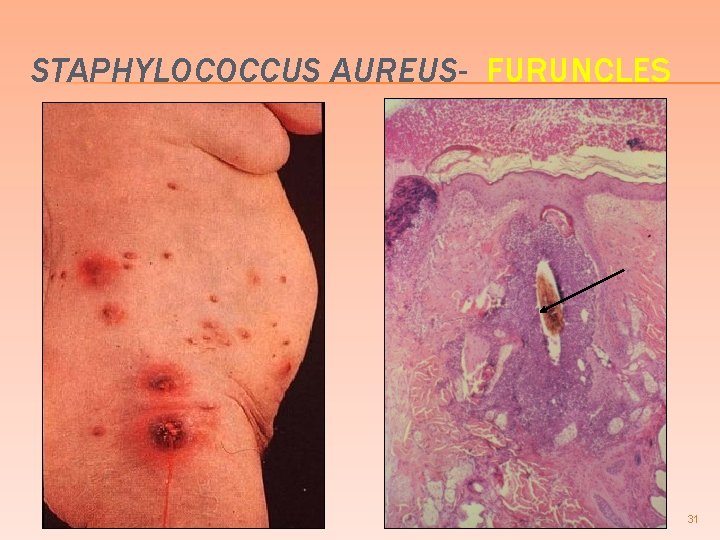
CUTANEOUS INFECTIONS DUE TO STAPHYLOCOCCUS AUREUS Bullous impetigo & scalded skin synd � Furuncles (boils) � � � deep infection of a single hair follicle Carbuncles � deep infection of a group of contiguous hair follicles Suppurative hidradenitis abscesses apocrine glands � Infection of the nail bed � Post-operative suture or wound abscess � Post-partum breast abscess � 29
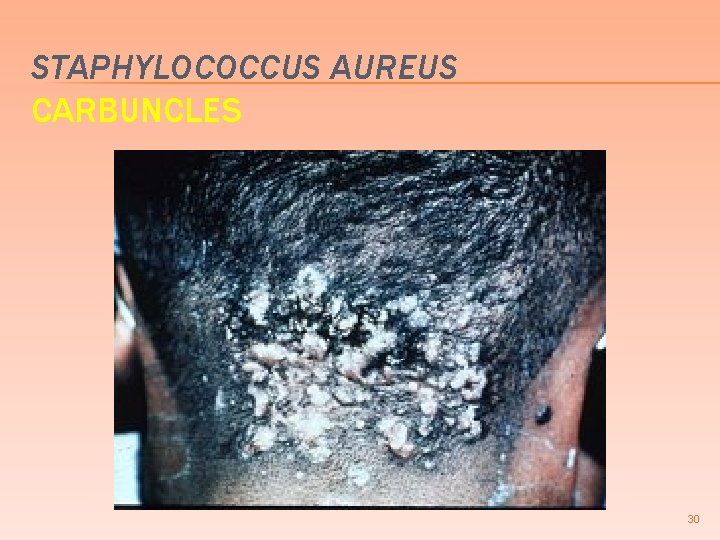
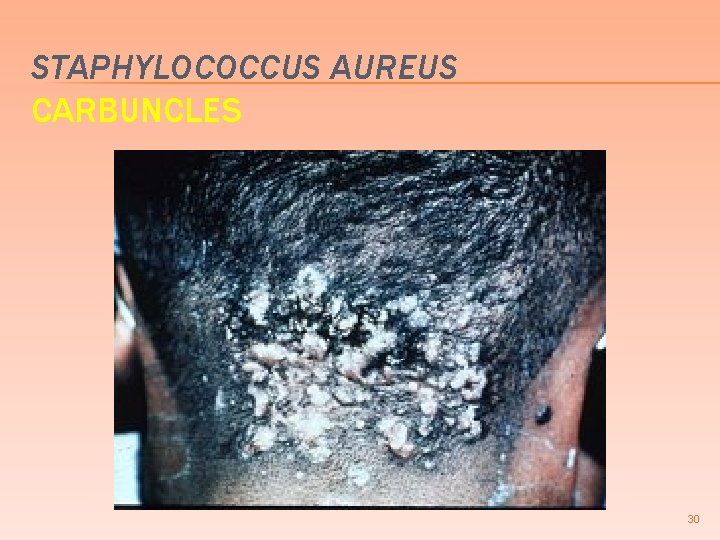
STAPHYLOCOCCUS AUREUS CARBUNCLES 30
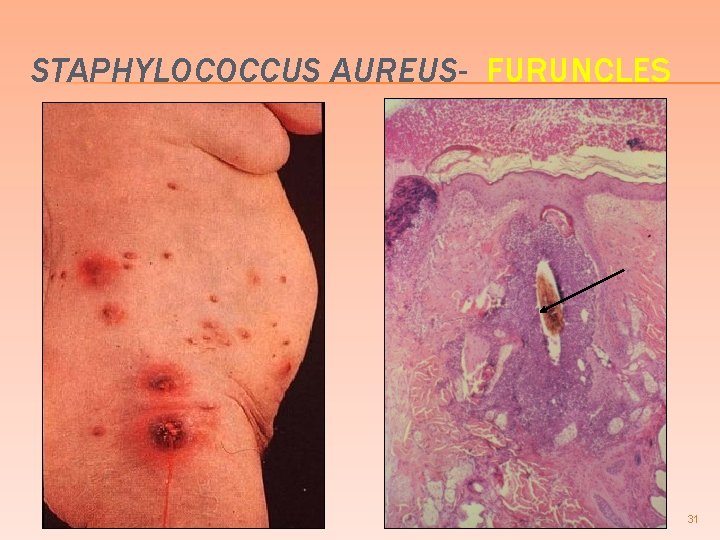
STAPHYLOCOCCUS AUREUS- FURUNCLES 31
STAPHYLOCOCCAL ENDOCARDITIS 32
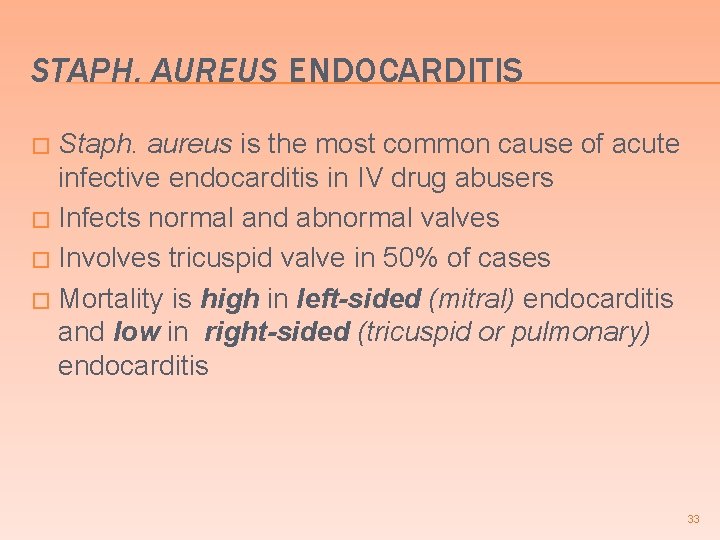
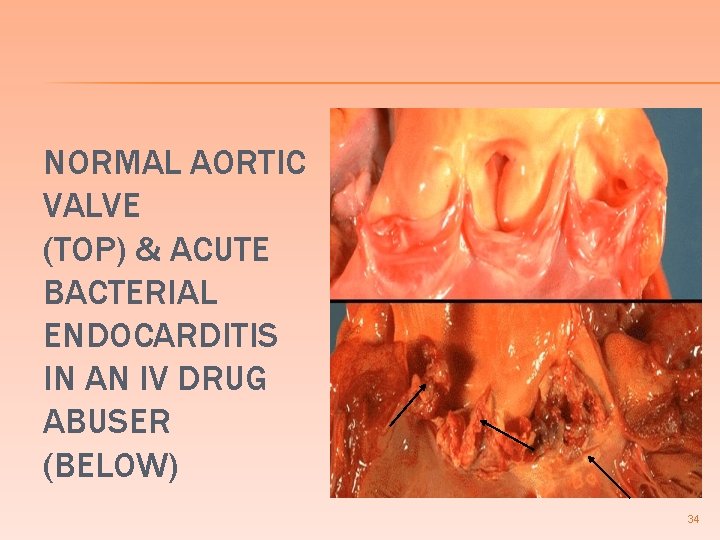
STAPH. AUREUS ENDOCARDITIS Staph. aureus is the most common cause of acute infective endocarditis in IV drug abusers � Infects normal and abnormal valves � Involves tricuspid valve in 50% of cases � Mortality is high in left-sided (mitral) endocarditis and low in right-sided (tricuspid or pulmonary) endocarditis � 33
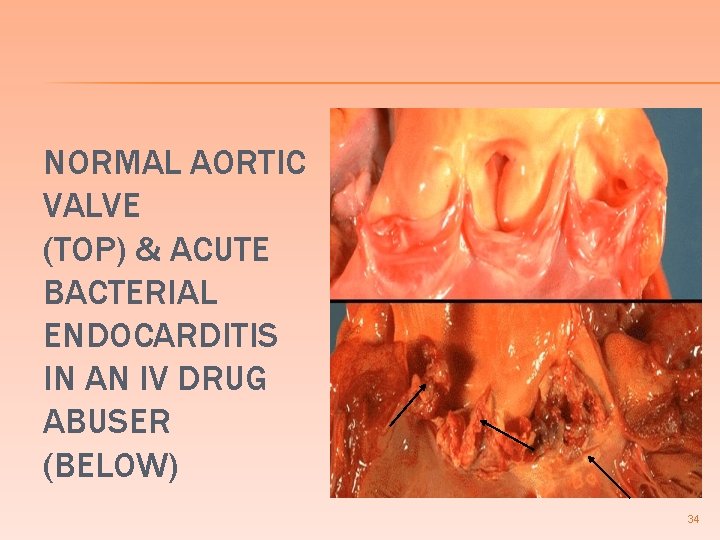
NORMAL AORTIC VALVE (TOP) & ACUTE BACTERIAL ENDOCARDITIS IN AN IV DRUG ABUSER (BELOW) 34
RX OF STAPHYLOCOCCUS AUREUS INFECTIONS � 90% of hospital and community strains of S. aureus are resistant to penicillin due to production of -lactamase � MRSA (methicillin resistant S. aureus) � resistant to all beta-lactam antibiotics and to cephalosporins � treat with vancomycin 35
RX OF STAPHYLOCOCCUS AUREUS INFECTIONS � Vancomycin-resistant Staphylococcus aureus � Associated with transfer of resistance from enterococci � Treat with Synercid I. V. 36
STREPTOCOCCAL INFECTIONS 37
STREPTOCOCCAL IMPETIGO 38
STREPTOCOCCAL IMPETIGO � Strep. � pyogenes most common cause of impetigo � Young children � Begins on face spreads to limbs � Erythematous macules vesicles & pustules honey colored crusts � Similar presentation as S. aureus � different from S. aureus � S. aureus; more likely to see bulla & + Nikolsky sign 39
STREPTOCOCCAL IMPETIGO � Highly contagious � avoid � Topical contact w/ other children antibiotics for localized infection � bacitracin, � Systemic mupirocin antibiotics for more generalized infection � penicillin, erythromycin, dicloxacillin 40

STREPTOCOCCAL IMPETIGO 41
STREPTOCOCCUS PYOGENES � Group A Beta-hemolytic � Most common cause of bacterial tonsillopharyngitis � Erythrogenic toxin � phage mediated � pyrogenic & cytotoxic � Also causes cellulitis, necrotizing fasciitis, streptococcal toxic shock syndrome, puerperal sepsis and endometritis 42
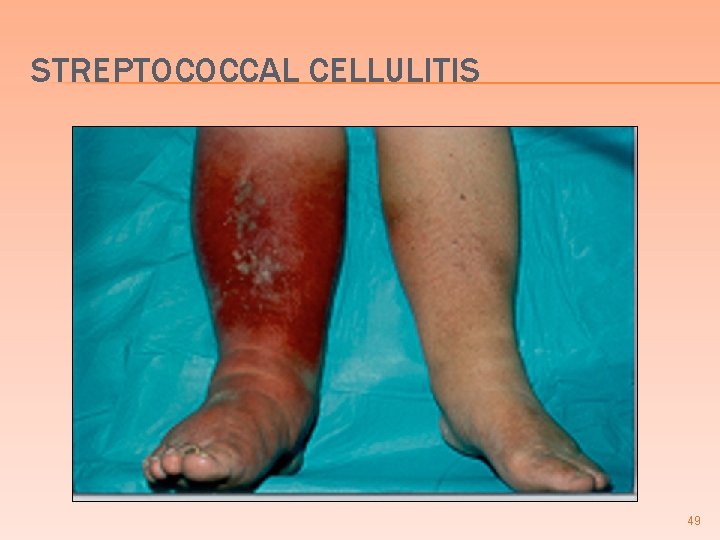
STREPTOCOCCAL CELLULITIS 43
PE; Labs: Temperature 39. 4; pulse 120; respirations 12; BP 130/80. Extremities: erythematous right leg, swollen and tender WBC 21, 000 (↑) with 80% neutrophils (↑) 44
CELLULITIS Infection of the subcutaneous tissue � Etiology � most commonly Strep. pyogenes & Staph. aureus � traumatic disruption of skin � +/- spontaneously (without obvious disruption) in very young elderly or immunocompromised patients � Strep. pyogens produces hyaluronidase, liquefies tissue, more likely to have diffuse spread rather than abscess formation � 45
STREPTOCOCCAL CELLULITIS � Clinical Area is acutely red, hot & tender/painful � leading edge is not raised but may be well defined � Rapid propagation centripetal from traumatic lesion � +/- lymphangitis lymphadenopathy � +/- desquamation of skin � � Tx; Erythromycin, cephalosporins, amoxicillin/clavulanate, azithromycin, clarithromycin, clindamycin 46
INFECTIOUS DISEASE PEARLS Recurrent streptococcal leg cellulitis may occur in patients after coronary bypass surgery if the saphenous vein was removed � Parenteral drug abusers have an increased risk of streptococcal cellulitis often associated with bacteremia, endocarditis, or septic thrombophlebitis � Patients with impaired lymphatic drainage may have recurrent cellulitis � Cellulitis of the foot or leg often co-exists with osteomyelitis in immunocompromised patients or diabetics � 47

STREPTOCOCCAL CELLULITIS surgical scar from vein stripping for coronary bypass 48
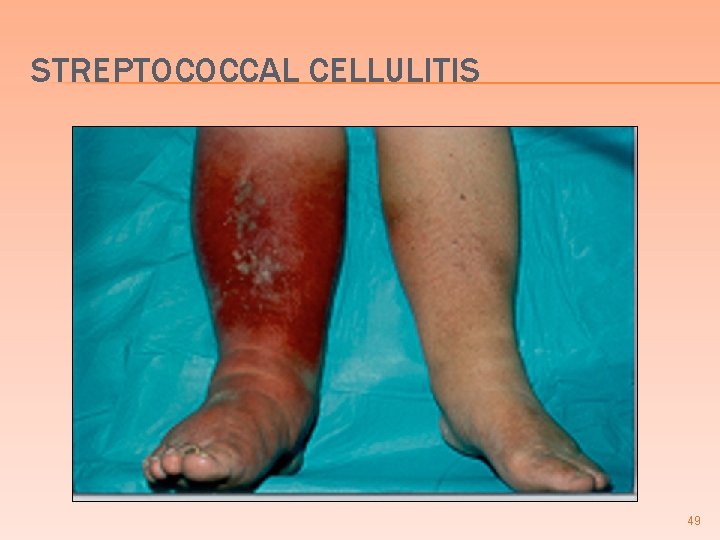
STREPTOCOCCAL CELLULITIS 49
NECROTIZING FASCIITIS 50

NECROTIZING FASCIITIS �A life threatening infection � Involves deep soft (SQ) tissue, muscle and fascia � Develops at sites of wounds � Perineal infection in post partum diabetic & immunocompromised women (Fournier’s gangrene) � rarely healthy women 51
NECROTIZING FASCIITIS � Clinical � Severely painful cellulitis that may become bullous and/or gangrenous � Initially, the pain may be out of proportion to the severity of the cellulitis � Pure Streptococcal infection, � exudate is odorless, without gas � Mixed infections, streptococci + anaerobes + enterobacteriaceae � foul smelling exudate with gas 52

NECROTIZING FASCIITIS 53
FOURNIER’S GANGRENE �A special case of necrotizing fasciitis involving the male or female genitalia � Usually associated with an underlying condition such as diabetes mellitus or immune compromised patients � Often involves mixed infections w/ Gram (+) and Gram (-), aerobic and anaerobic acting synergistically 54

FOURNIER’S GANGRENE 55

TREATMENT OF NECROTIZING FASCIITIS � Early surgical exploration and extensive debridement + antibiotics 56
STREPTOCOCCUS PYOGENES TONSILLOPHARYNGITIS � MOST COMMON CAUSE of bacterial tonsillopharyngitis � Erythrogenic (scarletinal) toxin is elaborated by some strains of group A strep. infected by a temperate bacteriophage � Most frequently seen in children from 515 years of age 57
STREPTOCOCCUS PYOGENES TONSILLOPHARYNGITIS � Clinical � (can also be seen w/ Staph. ) Red swollen tonsils, severely painful � Increased � +/- # follicles Peritonsillar abscess � peritonsillar abscess will deviate the uvula away from the involved tonsil � +/- Ludwig’s angina � diffuse suppurative inflammation of SQ tissue of pharynx, gingiva, & neck 58

STREPTOCOCCAL TONSILLOPHARYNGITIS 59
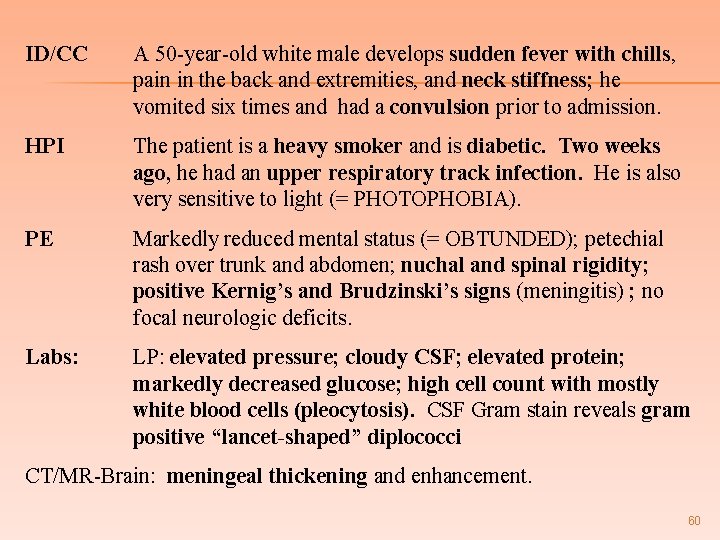
ID/CC A 50 -year-old white male develops sudden fever with chills, pain in the back and extremities, and neck stiffness; he vomited six times and had a convulsion prior to admission. HPI The patient is a heavy smoker and is diabetic. Two weeks ago, he had an upper respiratory track infection. He is also very sensitive to light (= PHOTOPHOBIA). PE Markedly reduced mental status (= OBTUNDED); petechial rash over trunk and abdomen; nuchal and spinal rigidity; positive Kernig’s and Brudzinski’s signs (meningitis) ; no focal neurologic deficits. Labs: LP: elevated pressure; cloudy CSF; elevated protein; markedly decreased glucose; high cell count with mostly white blood cells (pleocytosis). CSF Gram stain reveals gram positive “lancet-shaped” diplococci CT/MR-Brain: meningeal thickening and enhancement. 60
STREPTOCOCCAL MENINGITIS 61
STREPTOCOCCUS PNEUMONIAE Common cause of suppurative meningitis in children � r/o N. meningitidis � Most common cause of community-acquired bacterial pneumonia � > 20 years-old � empyema is the most common complication � Most common cause of otitis media, purulent sinusitis, and mastoiditis � Second most common cause of acute epiglottiditis 62
STREPTOCOCCUS PNEUMONIAE PEARLS � Pneumococcal meningitis is associated with sinusitis, otitis media, skull fractures, and CSF leaks � Pneumococcal endocarditis may result as a complication of pneumococcal meningitis � CSF in pneumococcal meningitis may have a greenish tint 63
� ID/CC � HPI few � PE A 35 year old woman complains of fever and pain in the face and upper teeth, especially upon leaning forward She has had a chronic cough for the past months as well as nasal congestion and discharge Fever. Halitosis; greenish-yellow postnasal discharge; bilateral boggy nasal mucosa; bilateral percussion tenderness and erythema over zygomatic arch; clouding of sinuses by transillumination; dental and cranial nerve exams normal 64
ACUTE SINUSITIS � DDX; � Streptococcus pneumoniae � Hemophilus influenzae � Moraxella catarrhalis 65
MENINGOCOCCEMIA NEISSERIA MENINGITIDIS 66
MENINGOCOCCEMIA NEISSERIA MENINGITIDIS Gram (-) diplococcus � Suppurative meningitis (+) Burdinski and Kernig signs � Small vessel vasculitis, capillary thrombosis & petechial hemorrhages purpura � Fulminating rapidly progressive septicemia with fever vascular collapse and DIC � induction of TNF & IL 1 & 6 cause the hypotension and vascular collapse � 67

MENINGOCOCCEMIA NEISSERIA MENINGITIDIS � +/- Waterhouse-Friderichsen syndrome � overwhelming bacterial infection � most commonly N. meningitidis rapidly progressive hypotension � DIC & purpura � bilateral adrenal cortical hemorrhage � � insufficiency � +/- Purpura Fulminans � a catastrophic febrile illness with initial hemorrhagic skin lesions that progress to gangrene 68
MENINGOCOCCEMIA NEISSERIA MENINGITIDIS � N. meningitidis is the most common cause of suppurative meningitis in patients 1 -18 yrsold � particularly common in crowded conditions (dormitories, boot camps) 69
MENINGOCOCCEMIA NEISSERIA MENINGITIDIS � Clinical severity is measured by how rapidly naturally occurring anticoagulants (protein C and S) are depleted, the degree of thrombocytopenia, and the presence of fibrin split products � High levels of TNF- and IFN- are associated with a poor prognosis 70

MENINGOCOCCEMIA NEISSERIA MENINGITIDIS � Patients with deficiency of properdin (serum protein kills bacteria) and ineffective alternative complement pathway (both sexlinked) have a very high risk of fulminant meningococcemia � Tx: Penicillin G � Treat family/contacts with Rifampin � vaccinate contacts > 2 yrs-old 71

PURULENT MENINGITIS Purulent CSF 72

NEISSERIA MENINGITIDIS 73

MENINGOCOCCEMIA GANGRENE WATERHOUSEFRIDERICHSEN SYNDROME 74
NEISSERIA GONORRHEA 75
NEISSERIA. GONORRHEA � Women more likely to be asymptomatic carriers than men � Men more likely to transmit the disease than women after each sexual exposure � Purulent penile discharge (urethritis) 2 -5 d. after exposure � Cervicitis (cervical discharge) most common site in women +/- urethritis, Bartholins gland abscess, PID (10 -20 % of untreated women) � fever, pain subpubic region 76
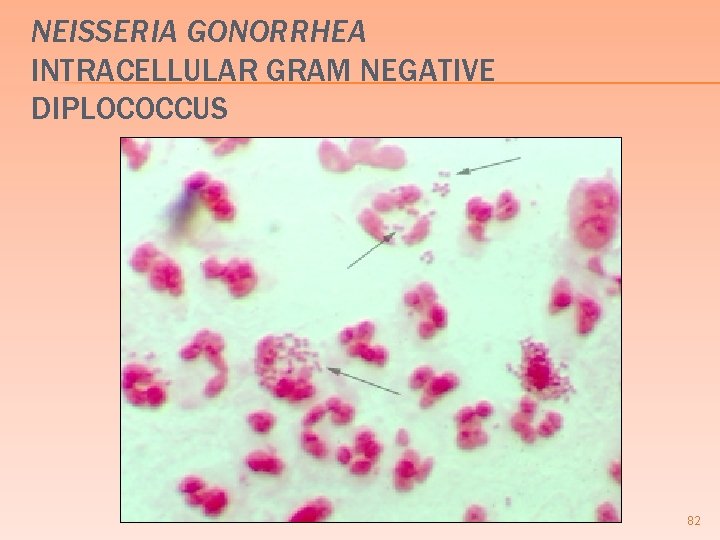
NEISSERIA. GONORRHEA � R/O Chlamydia trichomatis � Gram stain urethral exudate/cervical smear � intracellular organism are diagnostic 77
NEISSERIA. GONORRHEA � Conjunctivitis in neonates (ophthalmia neonatorum) � bilateral � develops 2 -5 days old � r/o �Chlamydia trichomatis � develops 5 -7 days old � most common cause �S. aureus usually unilateral 78
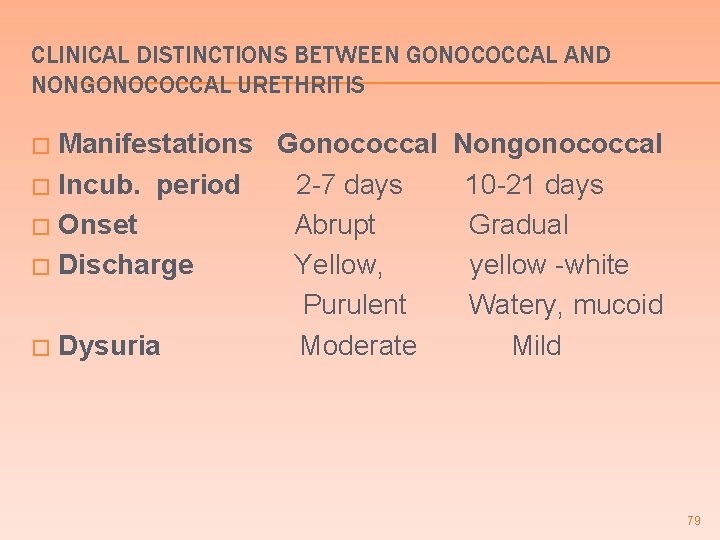
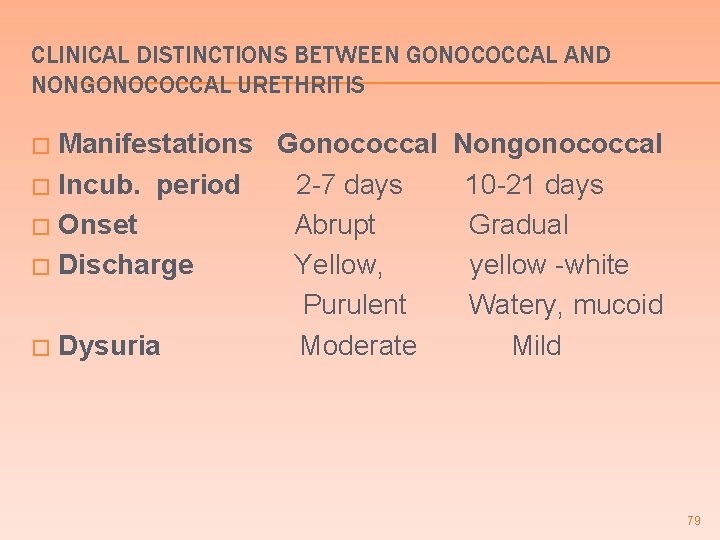
CLINICAL DISTINCTIONS BETWEEN GONOCOCCAL AND NONGONOCOCCAL URETHRITIS Manifestations Gonococcal Nongonococcal � Incub. period 2 -7 days 10 -21 days � Onset Abrupt Gradual � Discharge Yellow, yellow -white Purulent Watery, mucoid � Dysuria Moderate Mild � 79
NEISSERIA. GONORRHEA � Tx � All patients with gonorrhea should be treated simultaneously for chlamydia � ceftriaxone (gonorrhea) & doxycycline (Chlamydia) 80
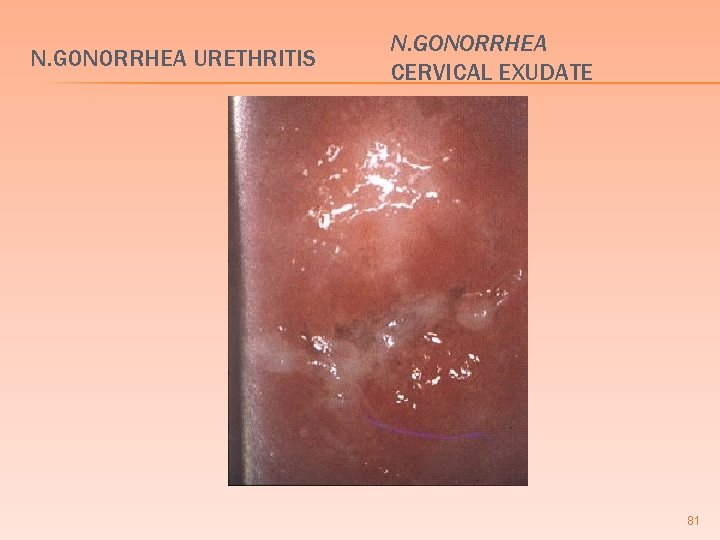
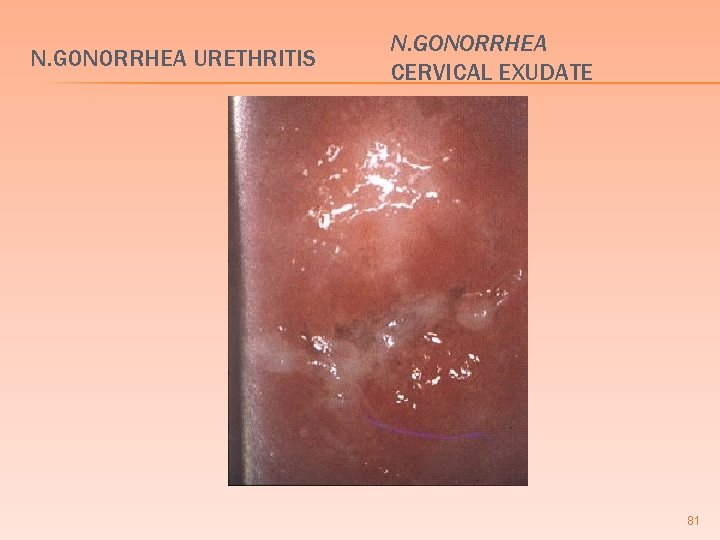
N. GONORRHEA URETHRITIS N. GONORRHEA CERVICAL EXUDATE 81
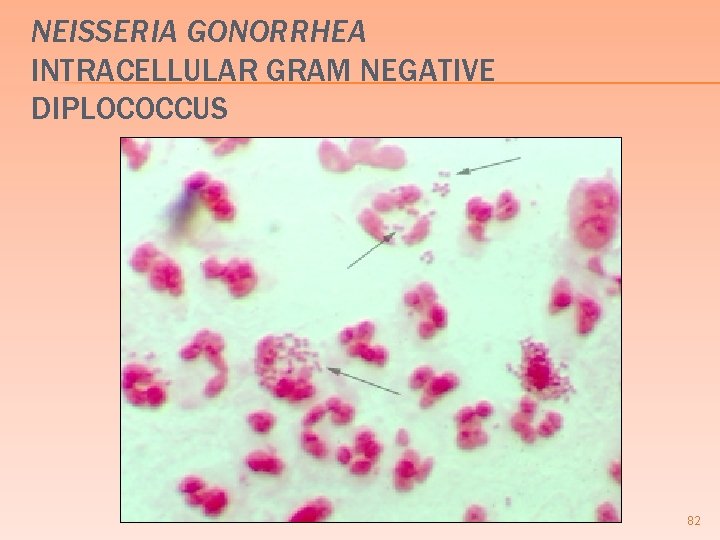
NEISSERIA GONORRHEA INTRACELLULAR GRAM NEGATIVE DIPLOCOCCUS 82
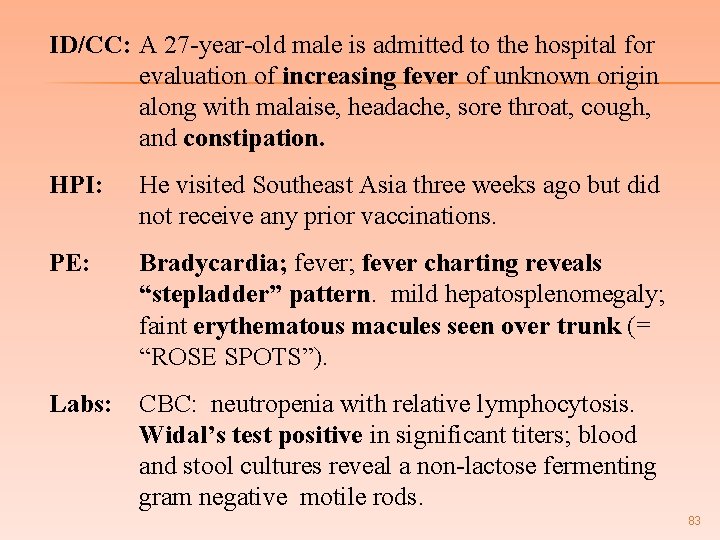
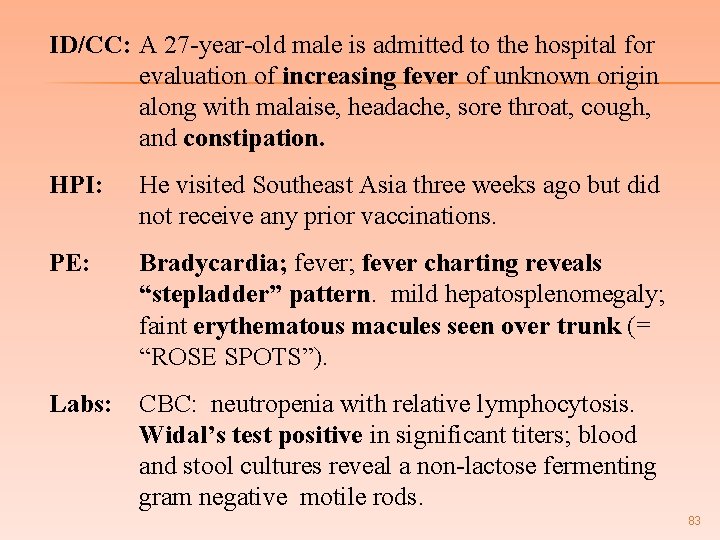
ID/CC: A 27 -year-old male is admitted to the hospital for evaluation of increasing fever of unknown origin along with malaise, headache, sore throat, cough, and constipation. HPI: He visited Southeast Asia three weeks ago but did not receive any prior vaccinations. PE: Bradycardia; fever charting reveals “stepladder” pattern. mild hepatosplenomegaly; faint erythematous macules seen over trunk (= “ROSE SPOTS”). Labs: CBC: neutropenia with relative lymphocytosis. Widal’s test positive in significant titers; blood and stool cultures reveal a non-lactose fermenting gram negative motile rods. 83
SALMONELLA TYPHI TYPHOID FEVER 84
SALMONELLA TYPHI TYPHOID FEVER Gram (-) rod, non-lactose fermenting, motile � Acquired by ingesting contaminated food or water � Carrier state: in gallbladder (up to 1 year) � DX: Blood culture (first week); stool and urine in third to fourth week � Widal’s test; agglutination test for S. typhi antibodies � � Vi antigens more sensitive & specific Only Salmonella w/ human reservoirs � RX: Fluoroquinolone; Ciprofloxacin � 85

SALMONELLA TYPHI TYPHOID FEVER � First week of infection � � Fever, malaise, constipation, & abdominal pain; positive blood cultures Second week of infection Sustained bacteremia, abdominal pain, diarrhea w/ occult blood, (+) stool culture � Rose spots; few 2 -4 mm erythmatous papules most common upper abdomen lower thorax, fade 2 -3 days � Hepatosplenomegaly, Absolute neutropenia, Bradycardia � “classic triad” � � Third week of infection; melena, ileus 86
SALMONELLOSIS � Four species: S. typhi, S. enteritidis, S. choleraesuis, and S. typhimurium � Diabetes predisposes to salmonella enteritis due to loss of gastric acidity and poor bowel motility � Septicemia can produce osteomyelitis � Second most common cause of osteomyelitis in sickle cell patients 87
SALMONELLA FOOD POISONING One of the most common causes of food poisoning � S. enteritidis, S. choleraesuis, and S. typhimurium � Fever, vomiting, diarrhea, abdominal pain � 8 -48 hours incubation � Self-limited diarrhea lasting 7 -10 days � Carried in nature by animal reservoirs � � � chickens, turtles, cattle, pigs, sheep, lizards, iguanas, snakes Any condition with hypochlorhydria predisposes to infection 88
 Pyogenic meningitis adalah
Pyogenic meningitis adalah Pyogenic meningitis definition
Pyogenic meningitis definition Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Understanding the mirai botnet
Understanding the mirai botnet Bone and joint infections
Bone and joint infections Methotrexate yeast infection
Methotrexate yeast infection Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Longitudinal ulcers in typhoid
Longitudinal ulcers in typhoid Positive vs negative face
Positive vs negative face Opportunistic infections
Opportunistic infections Kiran kaja
Kiran kaja Dr kiran bidari
Dr kiran bidari Kiran embedded
Kiran embedded Opportunistic infections
Opportunistic infections Kiran ramchandani
Kiran ramchandani Define financial management
Define financial management Kiran atapattu vs pan asia bank
Kiran atapattu vs pan asia bank Storch infections
Storch infections Storch infections
Storch infections Infections opportunistes digestives
Infections opportunistes digestives Kiran abraham
Kiran abraham Bacterial vaginosis
Bacterial vaginosis Kiran fothergill
Kiran fothergill Postpartum infections
Postpartum infections Kiran kaja
Kiran kaja Genital infections
Genital infections Amber blumling
Amber blumling Kiran mundy
Kiran mundy Shashi kiran shetty net worth
Shashi kiran shetty net worth Cell lysis complement system
Cell lysis complement system Acute gingival infections
Acute gingival infections Drinking water
Drinking water Laboratory diagnosis of typhoid fever
Laboratory diagnosis of typhoid fever What are the stages of typhoid fever
What are the stages of typhoid fever Typhoid symptoms
Typhoid symptoms Defination of typhoid fever
Defination of typhoid fever Nursing care plan for typhoid fever slideshare
Nursing care plan for typhoid fever slideshare Introduction of typhoid fever
Introduction of typhoid fever Swimmer itch
Swimmer itch Typhoid mary
Typhoid mary Neil mooser reaction
Neil mooser reaction Typhoid fever treatment
Typhoid fever treatment Typhoid
Typhoid Cholera
Cholera Green orange purple
Green orange purple And because i am happy and dance and sing
And because i am happy and dance and sing Romeo and juliet vs west side story venn diagram
Romeo and juliet vs west side story venn diagram Taller and younger and shorter and older
Taller and younger and shorter and older Write each amount using the peso sign 75 centavos
Write each amount using the peso sign 75 centavos Indigo violet
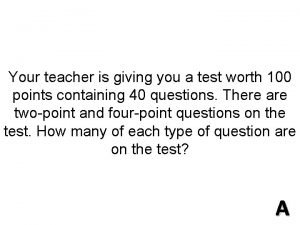
Indigo violet Gabby and sydney bought some pens
Gabby and sydney bought some pens Young and dyslexic summary
Young and dyslexic summary Compare and contrast maynard jackson and andrew young
Compare and contrast maynard jackson and andrew young West yorkshire and harrogate health and care partnership
West yorkshire and harrogate health and care partnership Draw and label a longitudinal wave
Draw and label a longitudinal wave Compare and contrast spring and neap tides.
Compare and contrast spring and neap tides. Independent and dependent variables
Independent and dependent variables Linking helping and action verbs
Linking helping and action verbs What are personal roles
What are personal roles Maintenance of records and reports
Maintenance of records and reports Transportation and assignment problems
Transportation and assignment problems Compare and contrast cold wave and wind chill factor
Compare and contrast cold wave and wind chill factor Trading account vertical format
Trading account vertical format Language spanish
Language spanish Tomorrow shakespeare
Tomorrow shakespeare Ritz-carlton motto
Ritz-carlton motto Conglomerates and franchises 1950s
Conglomerates and franchises 1950s Vastus lateralis origin insertion action
Vastus lateralis origin insertion action What does nick learn about jordan in chapter 3
What does nick learn about jordan in chapter 3 The giver chapter 3 and 4 questions and answers
The giver chapter 3 and 4 questions and answers Compare and contrast narrative expository and explanatory
Compare and contrast narrative expository and explanatory Definition of compare/contrast
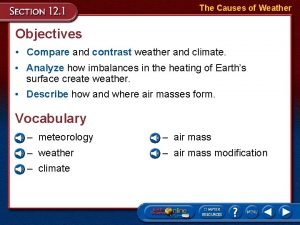
Definition of compare/contrast Compare and contrast weather
Compare and contrast weather Childhood is measured by sounds and smells and sights
Childhood is measured by sounds and smells and sights I see said the blind man poem
I see said the blind man poem Hub and spoke airline
Hub and spoke airline Comparison words
Comparison words Design input output
Design input output Zaroff and rainsford venn diagram
Zaroff and rainsford venn diagram Simple subjecy
Simple subjecy And compound inequalities
And compound inequalities Capillary action welding
Capillary action welding Similes about summer
Similes about summer Comparison of characteristics of parents and offspring
Comparison of characteristics of parents and offspring Separation of powers and checks and balances
Separation of powers and checks and balances Sdlc principles and practices
Sdlc principles and practices Local maximum and minimum vs. absolute maximum and minimum
Local maximum and minimum vs. absolute maximum and minimum Megan and ron ate too much and felt sick
Megan and ron ate too much and felt sick Rounding rules in math
Rounding rules in math