Putting education into practice optimising the referral process




- Slides: 57
Putting education into practice: optimising the referral process for paediatric critical care

Kathryn Claydon-Smith and Nicola Longden Clinical Nurse Specialists in Paediatric Intensive Care Transport
NWTS have been submitting referral and transport data since 2013
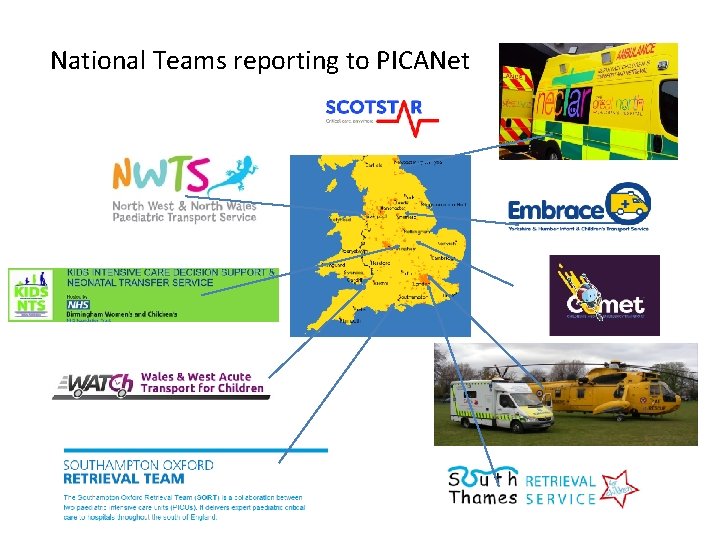
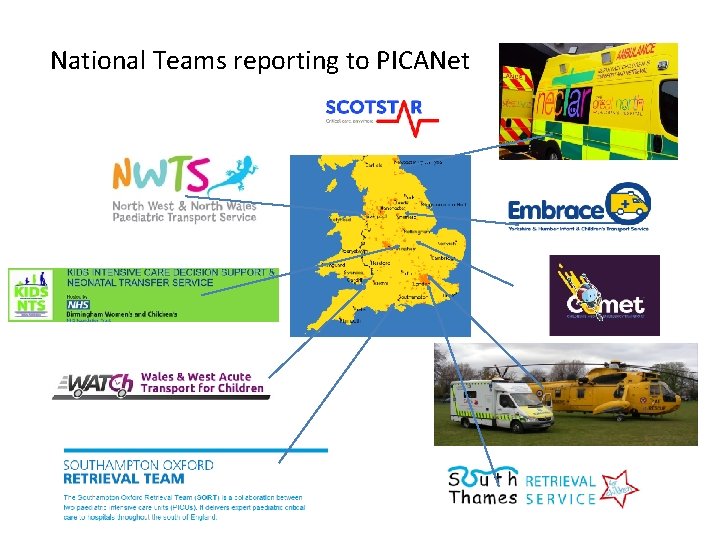
National Teams reporting to PICANet
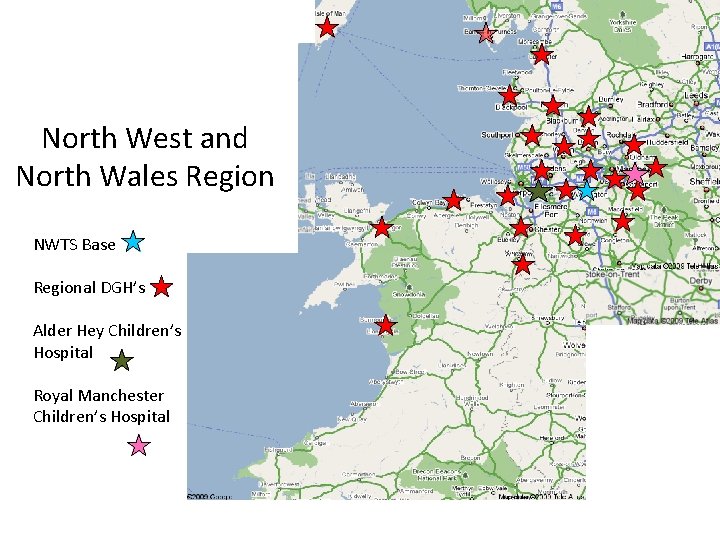
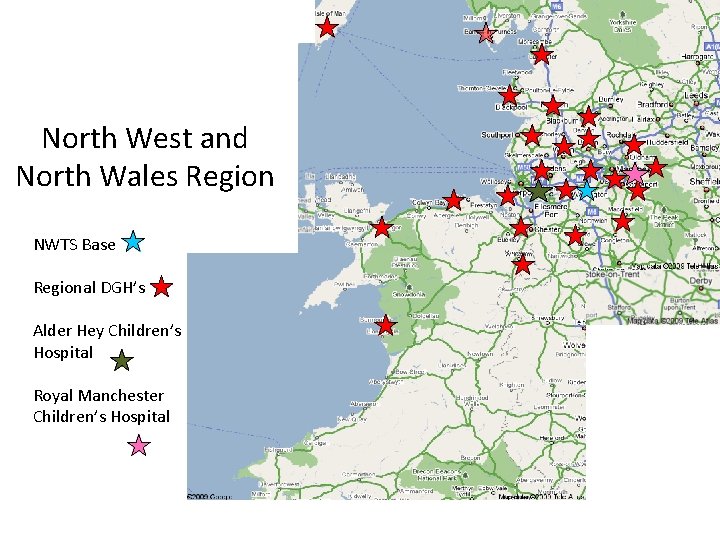
North West and North Wales Region NWTS Base Regional DGH’s Alder Hey Children’s Hospital Royal Manchester Children’s Hospital
NWTS provide advice and support to our regional district general hospitals when faced with a child requiring critical care.
or child remains in HDU with continued support from NWTS Team mobilised for PICU transfer
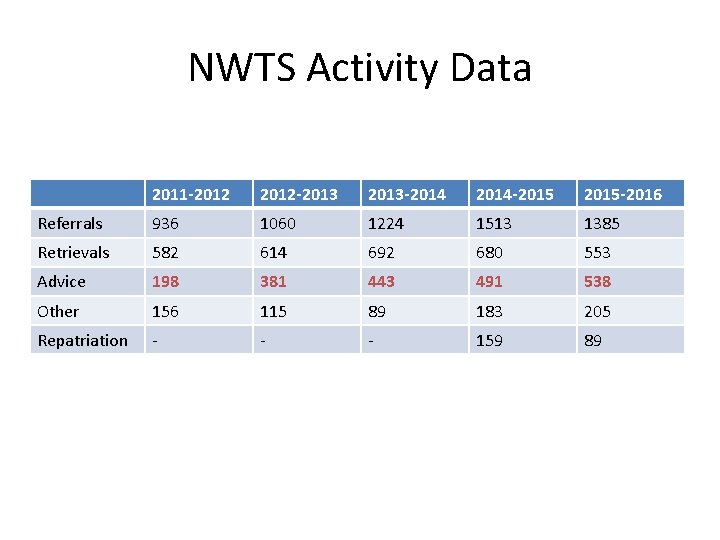
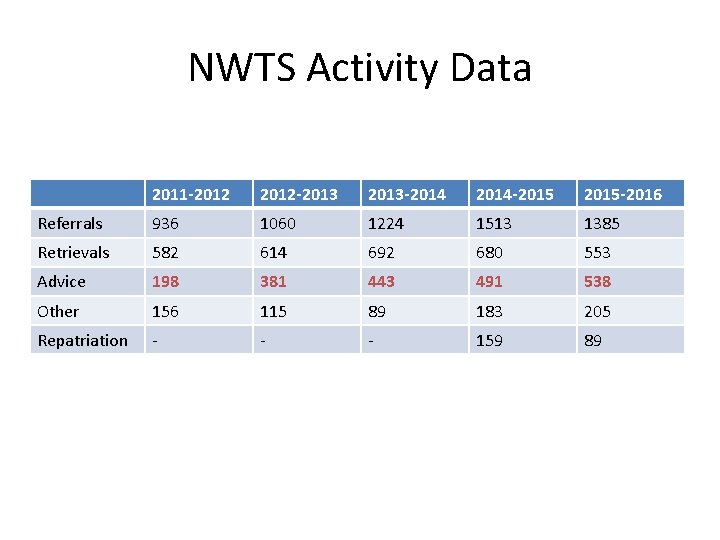
NWTS Activity Data 2011 -2012 -2013 -2014 -2015 -2016 Referrals 936 1060 1224 1513 1385 Retrievals 582 614 692 680 553 Advice 198 381 443 491 538 Other 156 115 89 183 205 Repatriation - - - 159 89
Annual Outreach Education provided for each DGH

In 2013 NWTS established a DGH link nurse group
Paediatric Critical Care Operational Delivery Network Group • Dr. Rajesh Phatak and Sarah Santo key drivers in establishing the nursing sub-group
Nursing Sub-Group Chair – Kathryn Claydon-Smith Deputy – John Horley

We have 90 members from our regional hospitals • • • Furness General Royal Lancaster Royal Blackburn Blackpool Victoria Royal Bolton Wigan Ormskirk Preston Warrington Bangor • • • Whiston Chester Tameside Royal Oldham NMGH Macclesfield Stepping Hill Wythenshawe Wrexham Glan Clwyd
• They work on; –Paediatric Wards –Paed Emergency Departments –ED Departments –Theatres –Adult Intensive Care Units
Meetings • Meet at NWTS base 4 times a year • Feedback always welcomed during the meeting • Educational component facilitated • Networking and exchange of ideas • Work stream plans fed back to the main PCCODN meeting the following month
Shadowing Shifts 2016 -2017 • Kate Walker - Whiston • Katie Davison – Stepping Hill • Katie Hinks – Stepping Hill • Cerys Cookson – Glan Clwyd • Kelly Bladen – North Manchester • Catherine Pollitt – Countess of Chester • Catrin Parry – Glan Clwyd • John Horley - Wigan • Rachel Crowther – Royal Oldham
2017 Work Stream Plans • Benchmarking each DGH against PICS - Level 1 (RAG rating) – HDU educational training – Development of a network wide patient HDU information leaflet • The transfer of level 1 and 2 patients between hospitals • Use of equipment and consumables used infrequently
Nurses Conference 2017 • Tuesday 27 th June 2017 • At The Centre, Birchwood Park. Warrington • ‘The care of the child in HDU’.
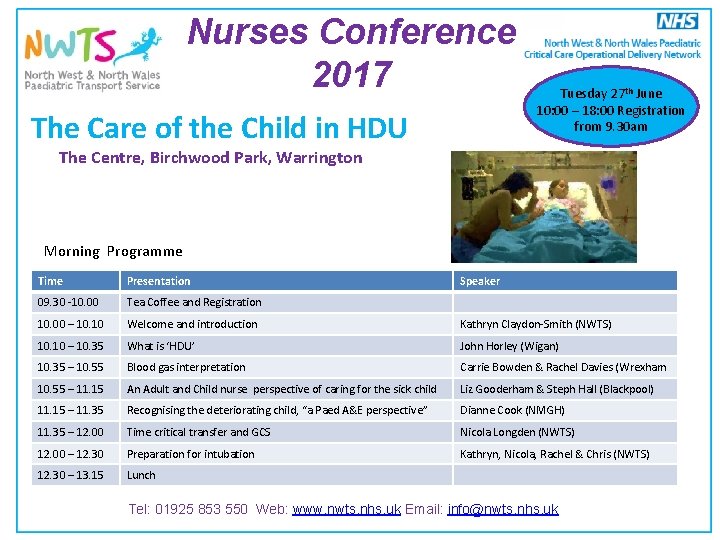
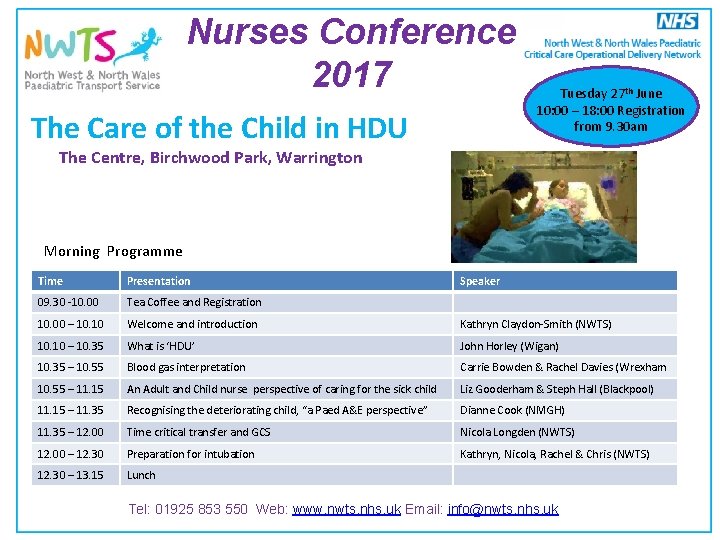
Nurses Conference 2017 The Care of the Child in HDU Tuesday 27 th June 10: 00 – 18: 00 Registration from 9. 30 am The Centre, Birchwood Park, Warrington Morning Programme Time Presentation Speaker 09. 30 -10. 00 Tea Coffee and Registration 10. 00 – 10. 10 Welcome and introduction Kathryn Claydon-Smith (NWTS) 10. 10 – 10. 35 What is ‘HDU’ John Horley (Wigan) 10. 35 – 10. 55 Blood gas interpretation Carrie Bowden & Rachel Davies (Wrexham 10. 55 – 11. 15 An Adult and Child nurse perspective of caring for the sick child Liz Gooderham & Steph Hall (Blackpool) 11. 15 – 11. 35 Recognising the deteriorating child, “a Paed A&E perspective” Dianne Cook (NMGH) 11. 35 – 12. 00 Time critical transfer and GCS Nicola Longden (NWTS) 12. 00 – 12. 30 Preparation for intubation Kathryn, Nicola, Rachel & Chris (NWTS) 12. 30 – 13. 15 Lunch Tel: 01925 853 550 Web: www. nwts. nhs. uk Email: info@nwts. nhs. uk
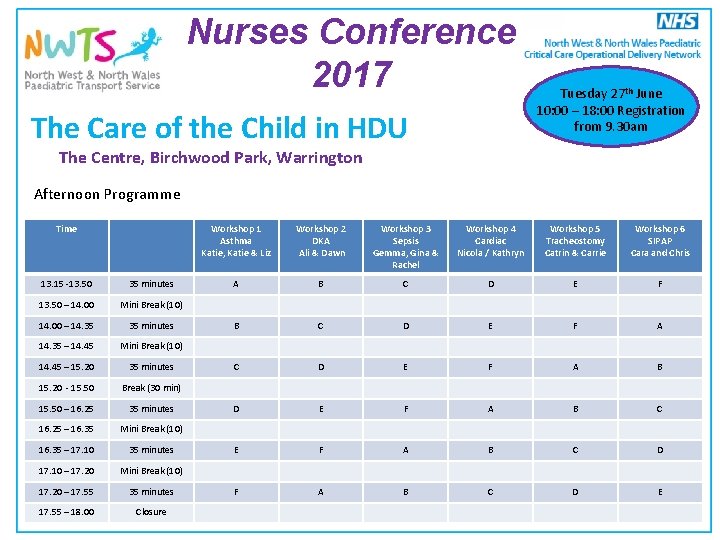
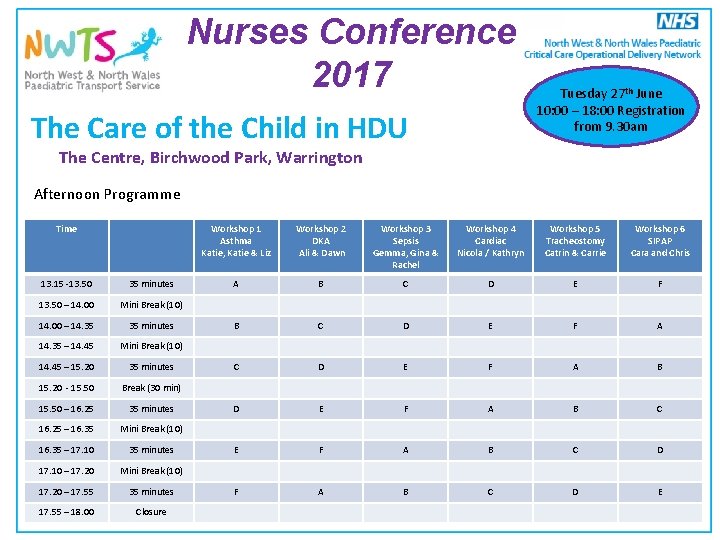
Nurses Conference 2017 The Care of the Child in HDU Tuesday 27 th June 10: 00 – 18: 00 Registration from 9. 30 am The Centre, Birchwood Park, Warrington Afternoon Programme Time Workshop 1 Asthma Katie, Katie & Liz Workshop 2 DKA Ali & Dawn Workshop 3 Sepsis Gemma, Gina & Rachel Workshop 4 Cardiac Nicola / Kathryn Workshop 5 Tracheostomy Catrin & Carrie Workshop 6 SIPAP Cara and Chris A B C D E F A B C E F A B C D E 13. 15 -13. 50 35 minutes 13. 50 – 14. 00 Mini Break (10) 14. 00 – 14. 35 35 minutes 14. 35 – 14. 45 Mini Break (10) 14. 45 – 15. 20 35 minutes 15. 20 - 15. 50 Break (30 min) 15. 50 – 16. 25 35 minutes 16. 25 – 16. 35 Mini Break (10) 16. 35 – 17. 10 35 minutes 17. 10 – 17. 20 Mini Break (10) 17. 20 – 17. 55 35 minutes 17. 55 – 18. 00 Tel: 01925 853 550 Web: www. nwts. nhs. uk Email: info@nwts. nhs. uk Closure
What is HDU care? John Horley RN(Child) Dip. HE(Nursing) MSc(APNP) PGCE Advanced Paediatric Nurse Practitioner Wrightington Wigan and Leigh NHS Foundation Trust jhorley@nhs. net @johnnyhorley
Alienation: The Paediatric Patient in an Adult Critical Care Unit Liz Gooderham and Stephanie Holmes
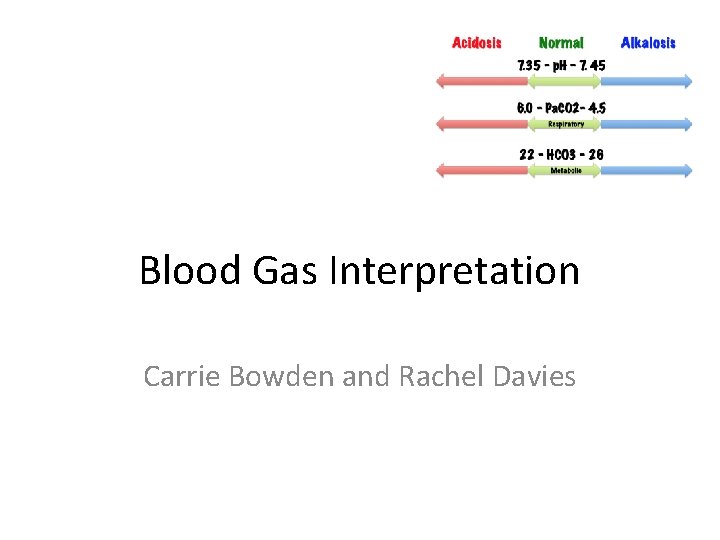
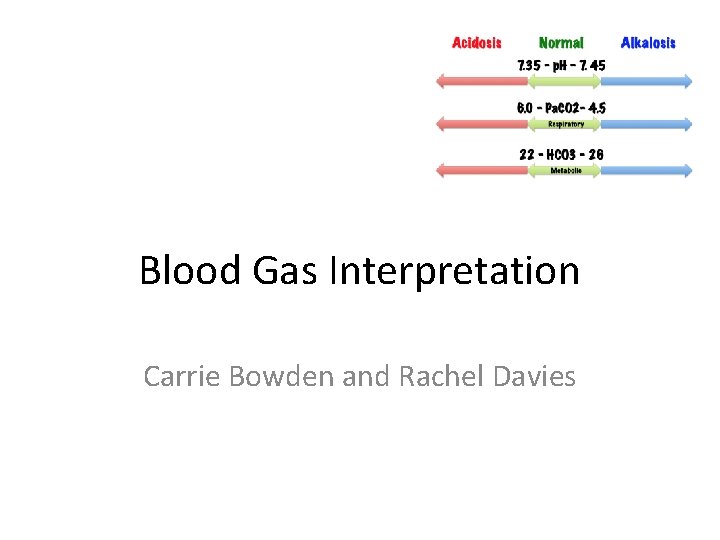
Blood Gas Interpretation Carrie Bowden and Rachel Davies
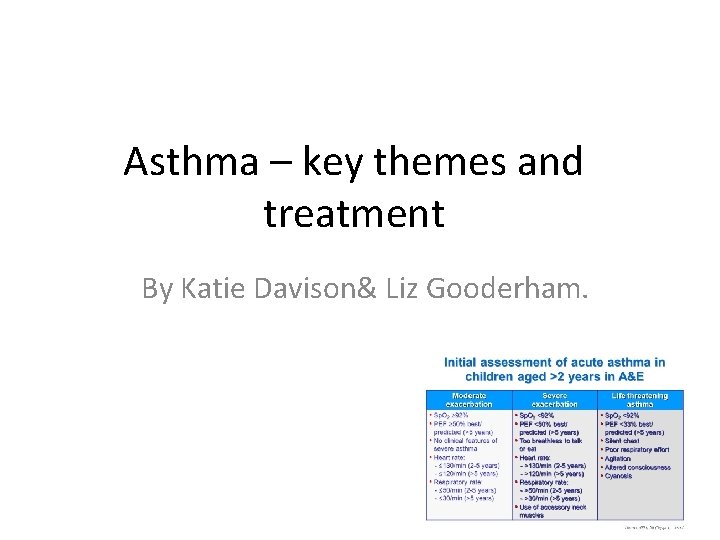
Asthma – key themes and treatment By Katie Davison& Liz Gooderham.
Catrin Parry and Rachel Davies
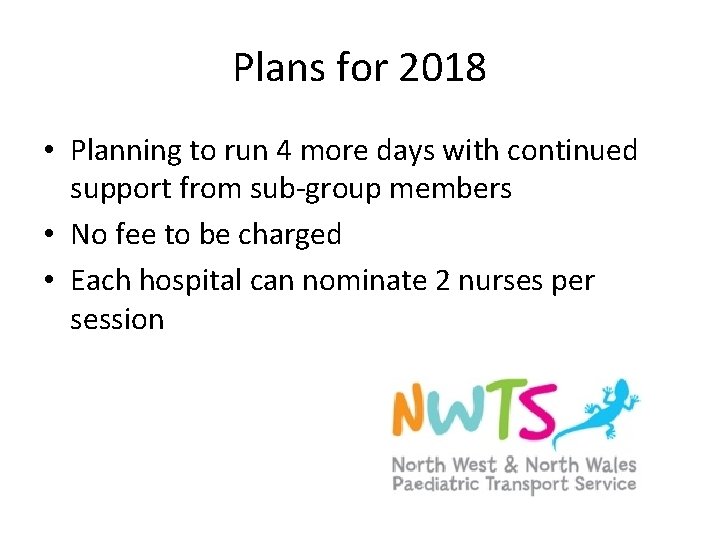
Plans for 2018 • Planning to run 4 more days with continued support from sub-group members • No fee to be charged • Each hospital can nominate 2 nurses per session
Case Presentation
Red Standby – 18: 02 pm
On arrival – 18: 06 pm • • • Arrived via Ambulance Followed by: Mum & Mum’s partner Biological father arrived 20 minutes later ‘Other relatives’ Police officer present • Fast Bleeped & Present on Arrival : ED Consultant, Consultant Paediatric Registrar, Paediatric SHO, Anaesthetic Registrar, ED Paediatric Nurse
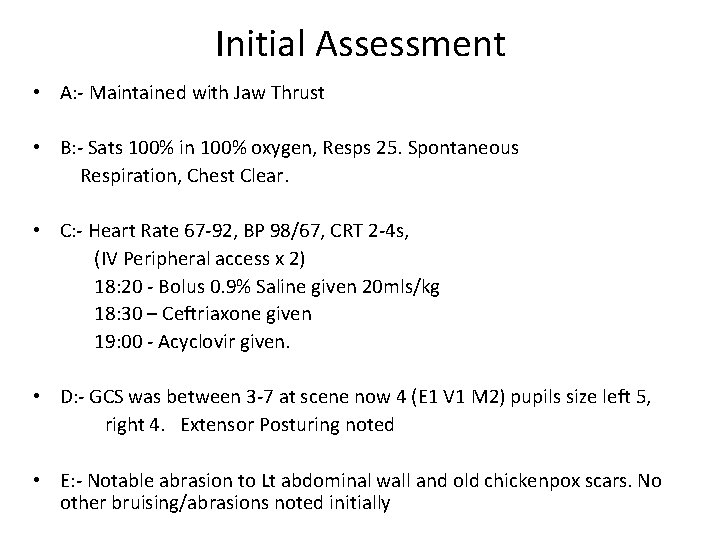
Initial Assessment • A: - Maintained with Jaw Thrust • B: - Sats 100% in 100% oxygen, Resps 25. Spontaneous Respiration, Chest Clear. • C: - Heart Rate 67 -92, BP 98/67, CRT 2 -4 s, (IV Peripheral access x 2) 18: 20 - Bolus 0. 9% Saline given 20 mls/kg 18: 30 – Ceftriaxone given 19: 00 - Acyclovir given. • D: - GCS was between 3 -7 at scene now 4 (E 1 V 1 M 2) pupils size left 5, right 4. Extensor Posturing noted • E: - Notable abrasion to Lt abdominal wall and old chickenpox scars. No other bruising/abrasions noted initially
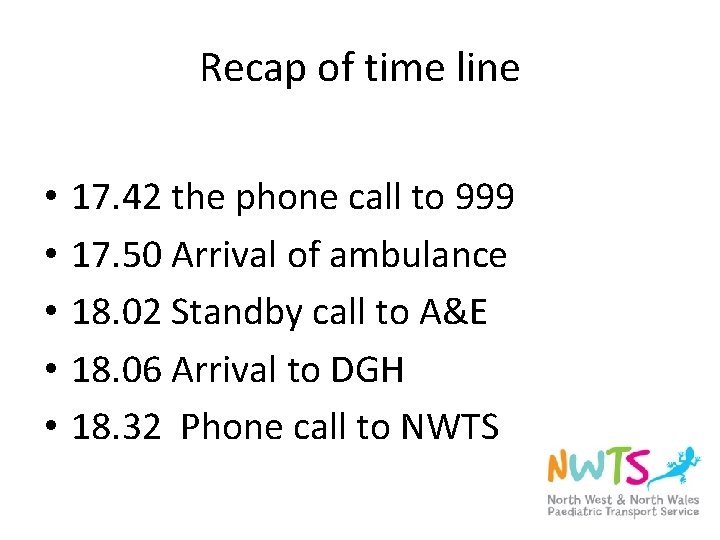
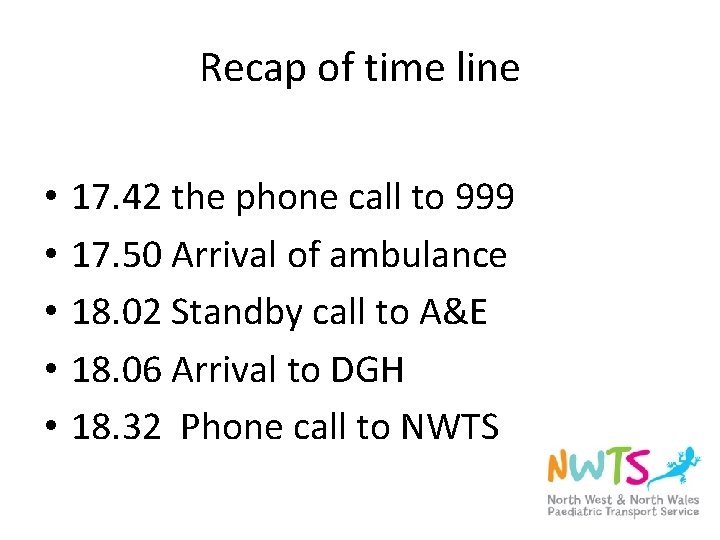
Recap of time line • • • 17. 42 the phone call to 999 17. 50 Arrival of ambulance 18. 02 Standby call to A&E 18. 06 Arrival to DGH 18. 32 Phone call to NWTS
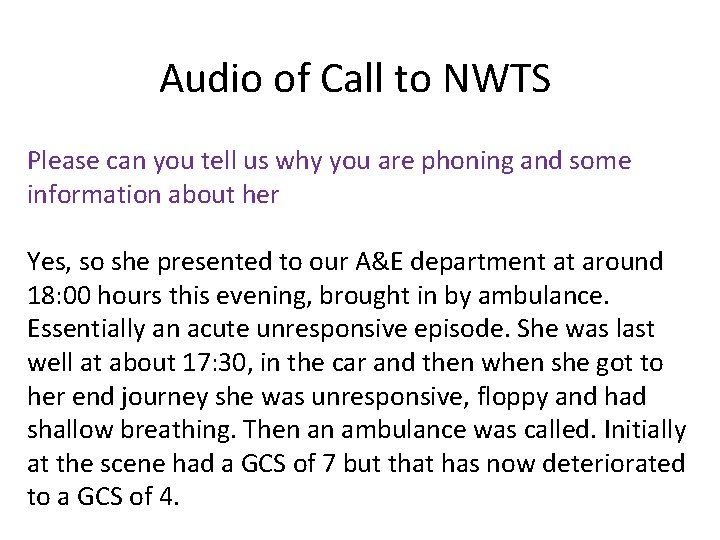
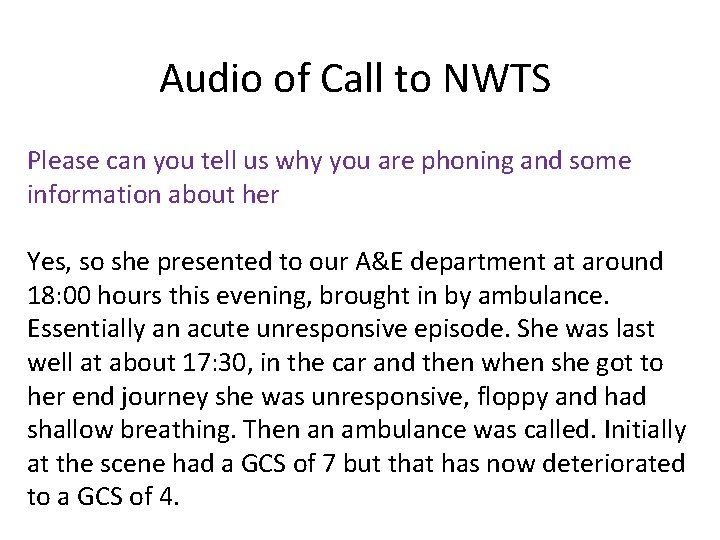
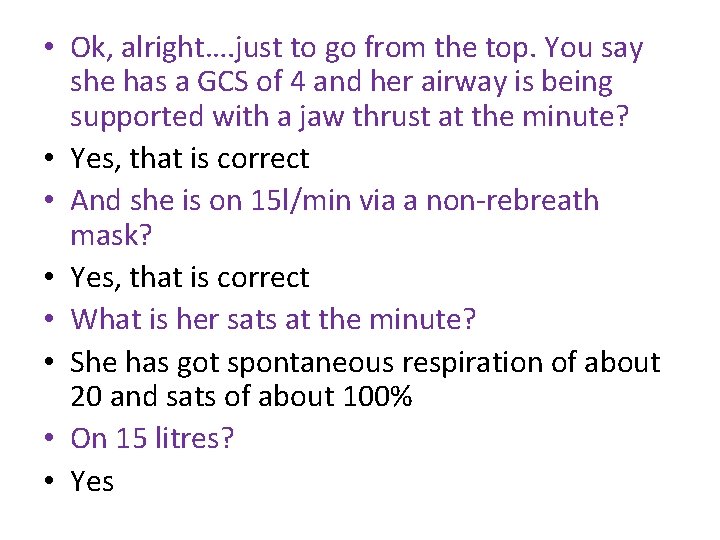
Audio of Call to NWTS Please can you tell us why you are phoning and some information about her Yes, so she presented to our A&E department at around 18: 00 hours this evening, brought in by ambulance. Essentially an acute unresponsive episode. She was last well at about 17: 30, in the car and then when she got to her end journey she was unresponsive, floppy and had shallow breathing. Then an ambulance was called. Initially at the scene had a GCS of 7 but that has now deteriorated to a GCS of 4.
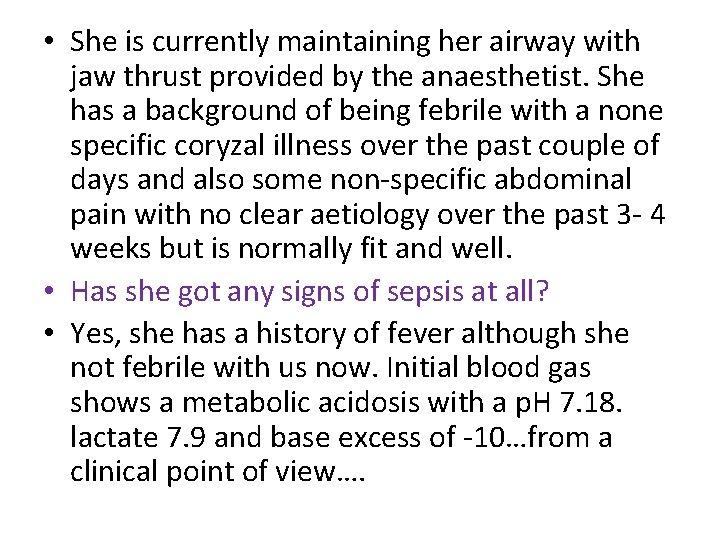
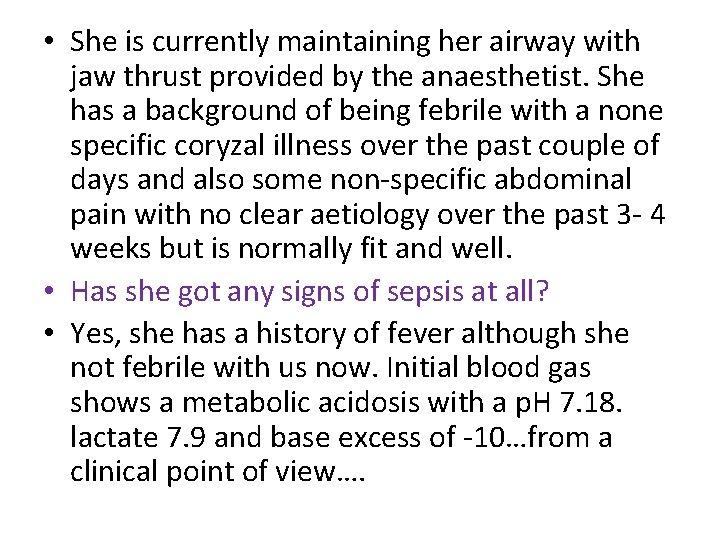
• She is currently maintaining her airway with jaw thrust provided by the anaesthetist. She has a background of being febrile with a none specific coryzal illness over the past couple of days and also some non-specific abdominal pain with no clear aetiology over the past 3 - 4 weeks but is normally fit and well. • Has she got any signs of sepsis at all? • Yes, she has a history of fever although she not febrile with us now. Initial blood gas shows a metabolic acidosis with a p. H 7. 18. lactate 7. 9 and base excess of -10…from a clinical point of view….
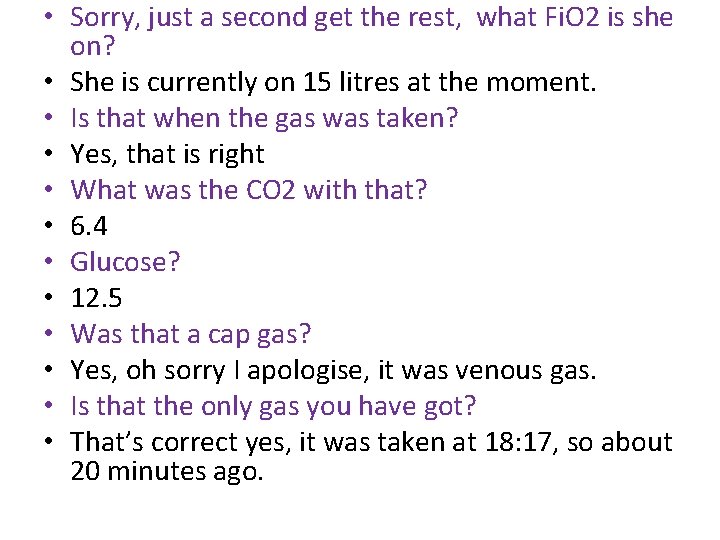
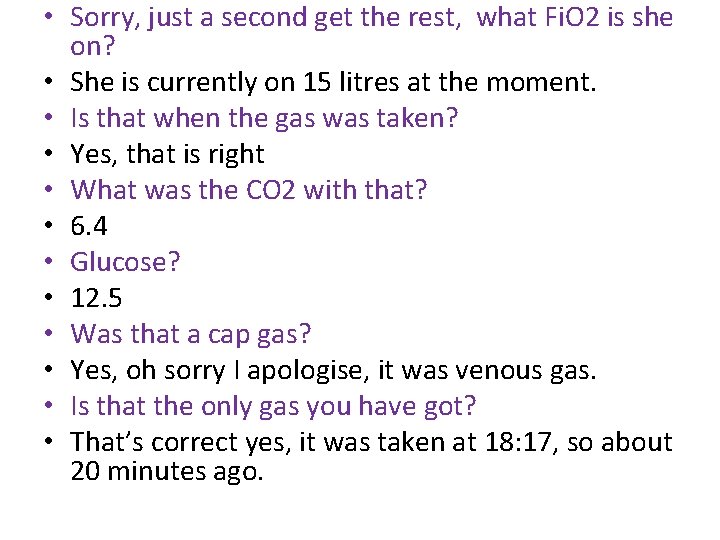
• Sorry, just a second get the rest, what Fi. O 2 is she on? • She is currently on 15 litres at the moment. • Is that when the gas was taken? • Yes, that is right • What was the CO 2 with that? • 6. 4 • Glucose? • 12. 5 • Was that a cap gas? • Yes, oh sorry I apologise, it was venous gas. • Is that the only gas you have got? • That’s correct yes, it was taken at 18: 17, so about 20 minutes ago.
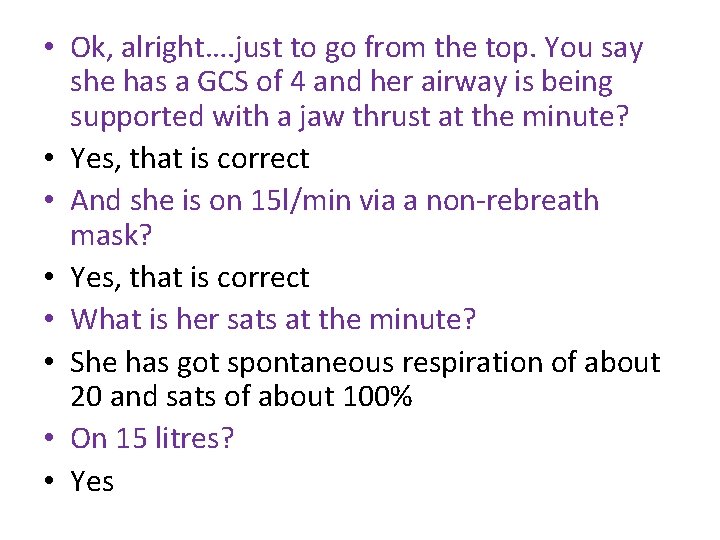
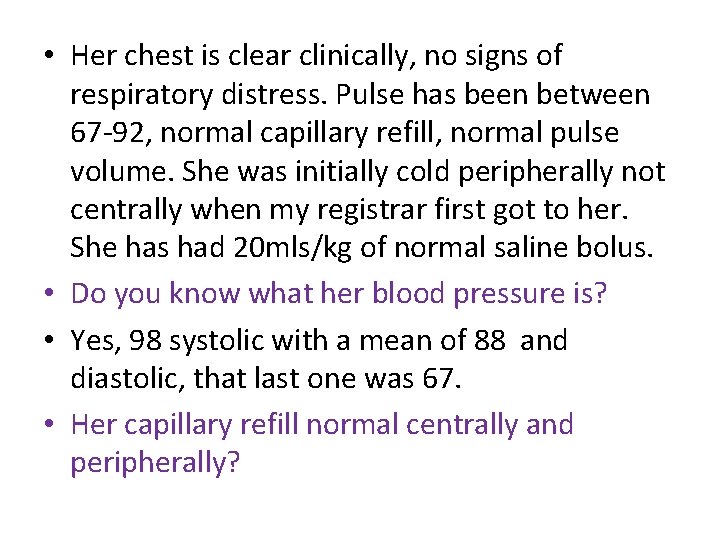
• Ok, alright…. just to go from the top. You say she has a GCS of 4 and her airway is being supported with a jaw thrust at the minute? • Yes, that is correct • And she is on 15 l/min via a non-rebreath mask? • Yes, that is correct • What is her sats at the minute? • She has got spontaneous respiration of about 20 and sats of about 100% • On 15 litres? • Yes
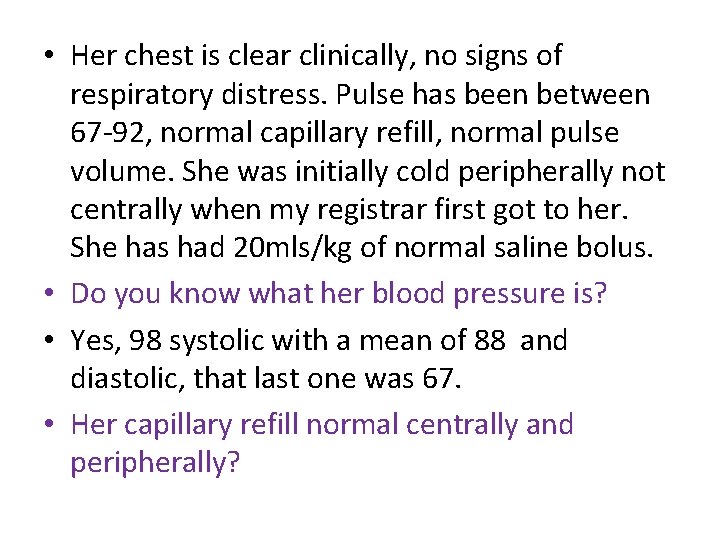
• Her chest is clear clinically, no signs of respiratory distress. Pulse has been between 67 -92, normal capillary refill, normal pulse volume. She was initially cold peripherally not centrally when my registrar first got to her. She has had 20 mls/kg of normal saline bolus. • Do you know what her blood pressure is? • Yes, 98 systolic with a mean of 88 and diastolic, that last one was 67. • Her capillary refill normal centrally and peripherally?
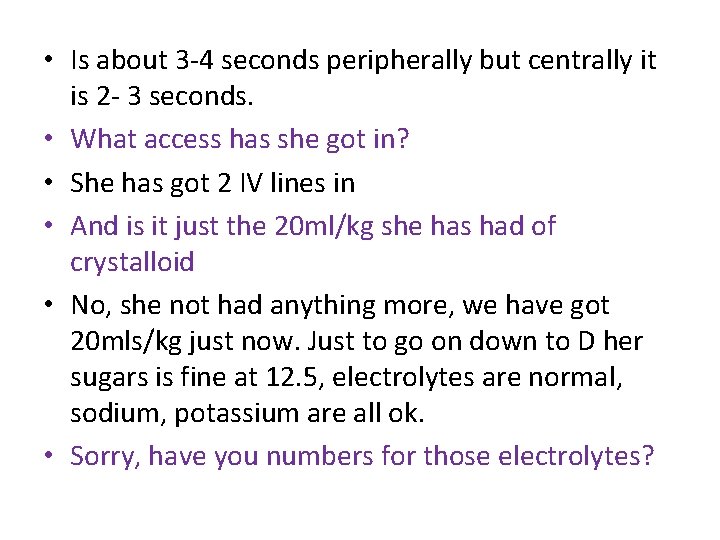
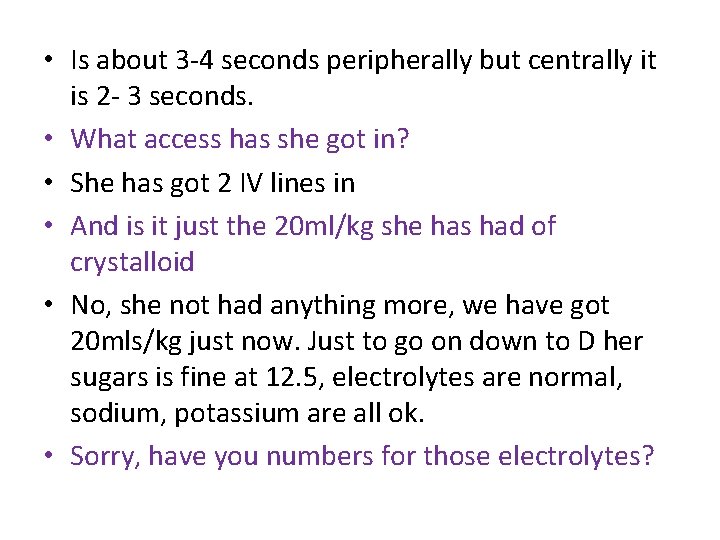
• Is about 3 -4 seconds peripherally but centrally it is 2 - 3 seconds. • What access has she got in? • She has got 2 IV lines in • And is it just the 20 ml/kg she has had of crystalloid • No, she not had anything more, we have got 20 mls/kg just now. Just to go on down to D her sugars is fine at 12. 5, electrolytes are normal, sodium, potassium are all ok. • Sorry, have you numbers for those electrolytes?
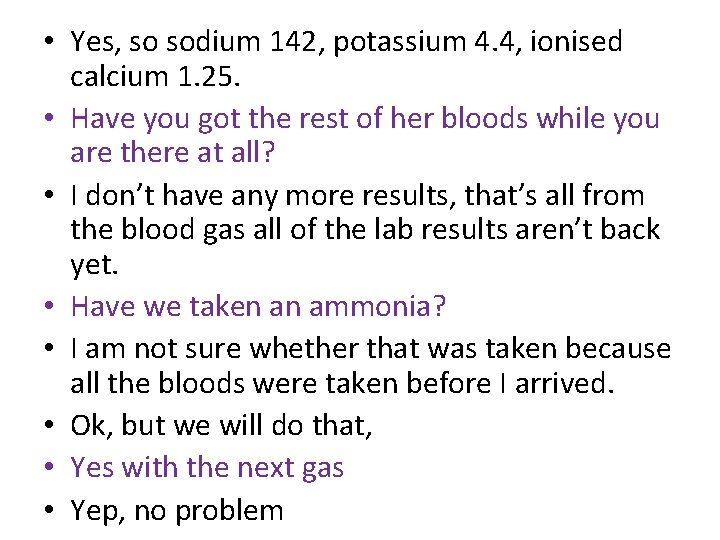
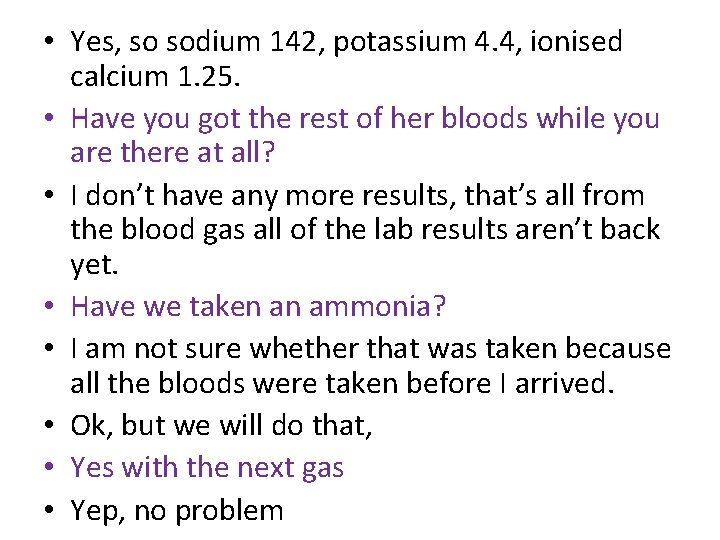
• Yes, so sodium 142, potassium 4. 4, ionised calcium 1. 25. • Have you got the rest of her bloods while you are there at all? • I don’t have any more results, that’s all from the blood gas all of the lab results aren’t back yet. • Have we taken an ammonia? • I am not sure whether that was taken because all the bloods were taken before I arrived. • Ok, but we will do that, • Yes with the next gas • Yep, no problem
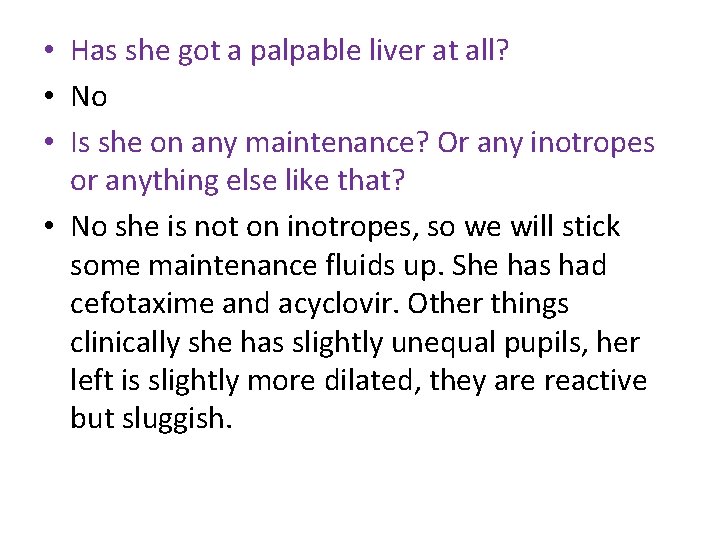
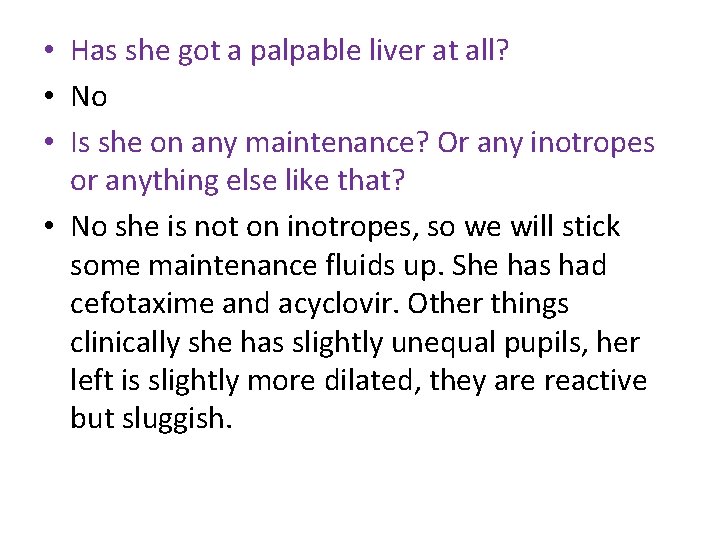
• Has she got a palpable liver at all? • No • Is she on any maintenance? Or any inotropes or anything else like that? • No she is not on inotropes, so we will stick some maintenance fluids up. She has had cefotaxime and acyclovir. Other things clinically she has slightly unequal pupils, her left is slightly more dilated, they are reactive but sluggish.
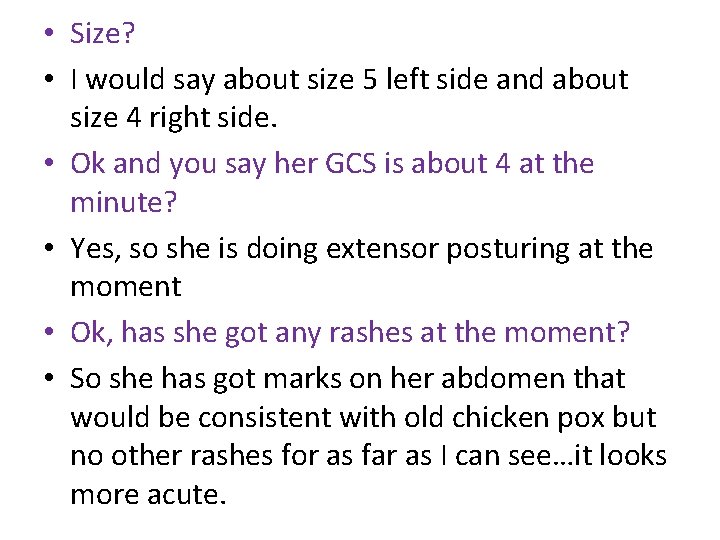
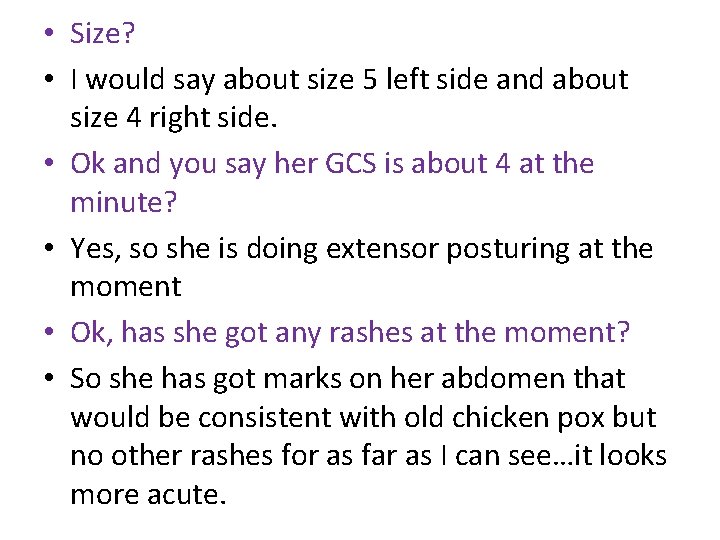
• Size? • I would say about size 5 left side and about size 4 right side. • Ok and you say her GCS is about 4 at the minute? • Yes, so she is doing extensor posturing at the moment • Ok, has she got any rashes at the moment? • So she has got marks on her abdomen that would be consistent with old chicken pox but no other rashes for as far as I can see…it looks more acute.
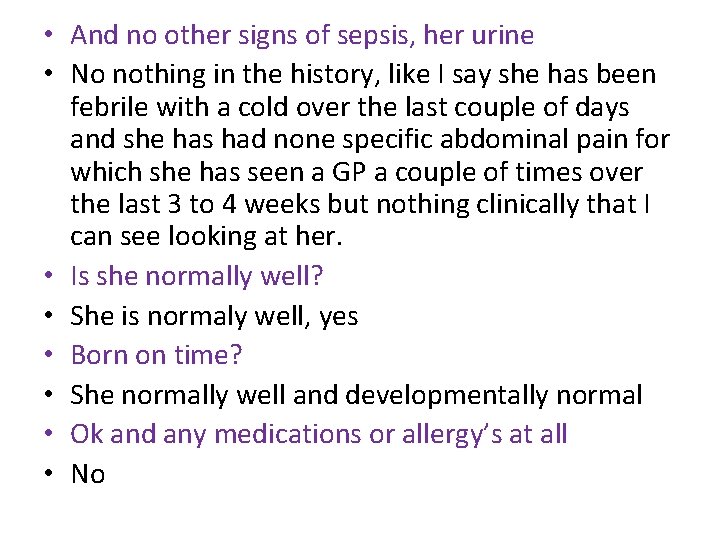
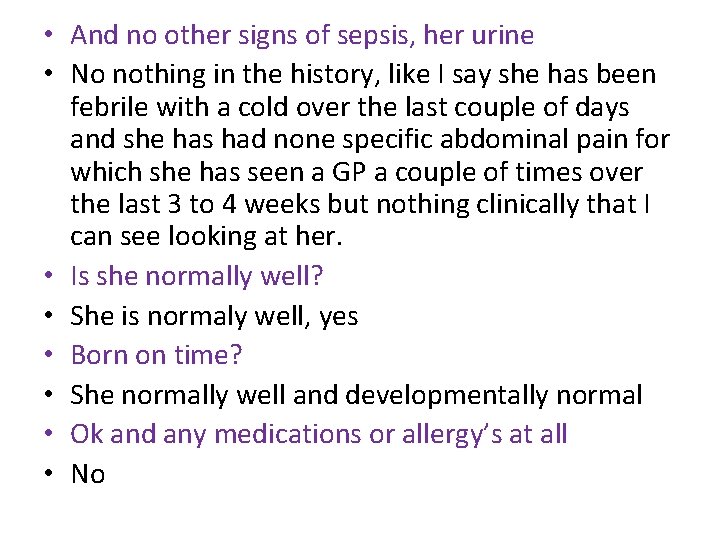
• And no other signs of sepsis, her urine • No nothing in the history, like I say she has been febrile with a cold over the last couple of days and she has had none specific abdominal pain for which she has seen a GP a couple of times over the last 3 to 4 weeks but nothing clinically that I can see looking at her. • Is she normally well? • She is normaly well, yes • Born on time? • She normally well and developmentally normal • Ok and any medications or allergy’s at all • No
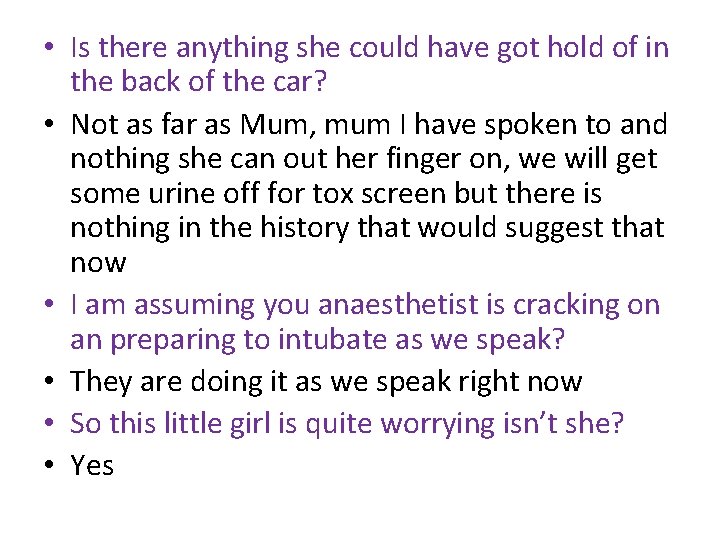
• Is there anything she could have got hold of in the back of the car? • Not as far as Mum, mum I have spoken to and nothing she can out her finger on, we will get some urine off for tox screen but there is nothing in the history that would suggest that now • I am assuming you anaesthetist is cracking on an preparing to intubate as we speak? • They are doing it as we speak right now • So this little girl is quite worrying isn’t she? • Yes
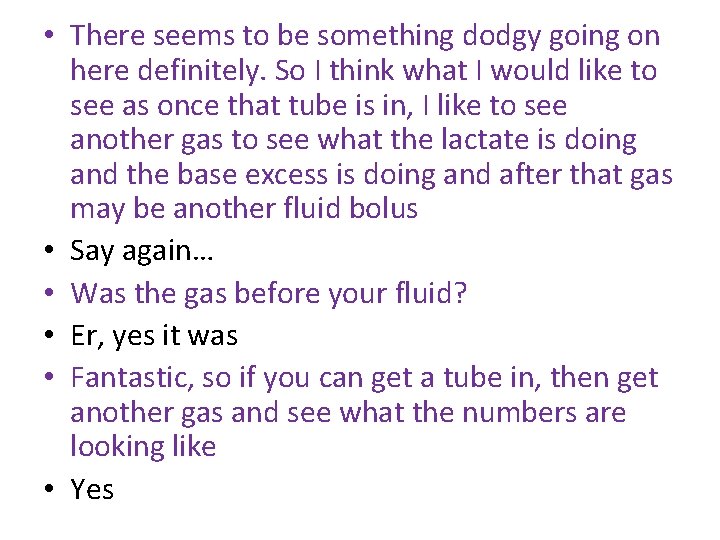
• There seems to be something dodgy going on here definitely. So I think what I would like to see as once that tube is in, I like to see another gas to see what the lactate is doing and the base excess is doing and after that gas may be another fluid bolus • Say again… • Was the gas before your fluid? • Er, yes it was • Fantastic, so if you can get a tube in, then get another gas and see what the numbers are looking like • Yes
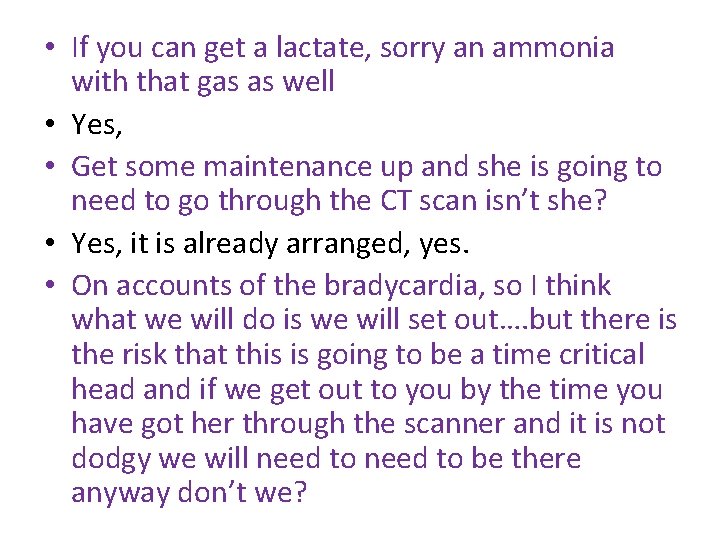
• If you can get a lactate, sorry an ammonia with that gas as well • Yes, • Get some maintenance up and she is going to need to go through the CT scan isn’t she? • Yes, it is already arranged, yes. • On accounts of the bradycardia, so I think what we will do is we will set out…. but there is the risk that this is going to be a time critical head and if we get out to you by the time you have got her through the scanner and it is not dodgy we will need to be there anyway don’t we?
• Yes, that is great • She is really worrying…. Ok so if I let you get on with getting intubation done, a gas done and give us a ring back as soon as you have got that gas and we will gather our things together and head straight out to you • That’s great…thank you • Okay dokey • Cheers. Bye bye.
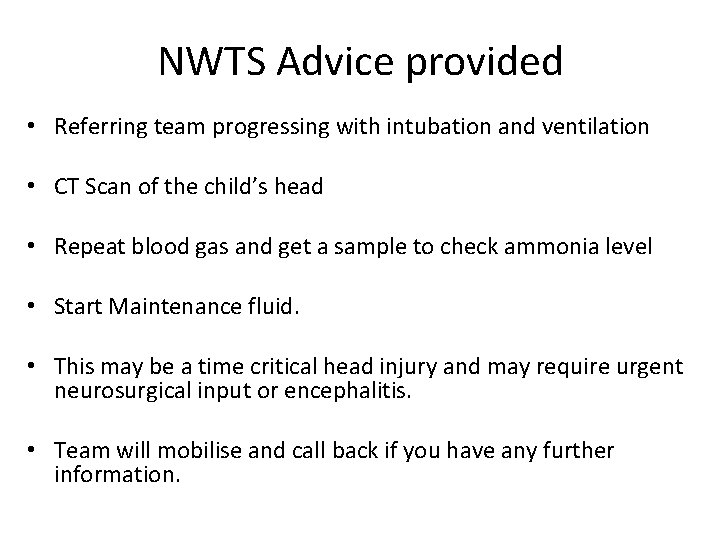
NWTS Advice provided • Referring team progressing with intubation and ventilation • CT Scan of the child’s head • Repeat blood gas and get a sample to check ammonia level • Start Maintenance fluid. • This may be a time critical head injury and may require urgent neurosurgical input or encephalitis. • Team will mobilise and call back if you have any further information.
NWTS Time line • 18. 32 Call received by administrator • 18. 42 NWTS agree to mobilise • 18. 54 NWTS left Base • 19. 18 Team Arrive at DGH
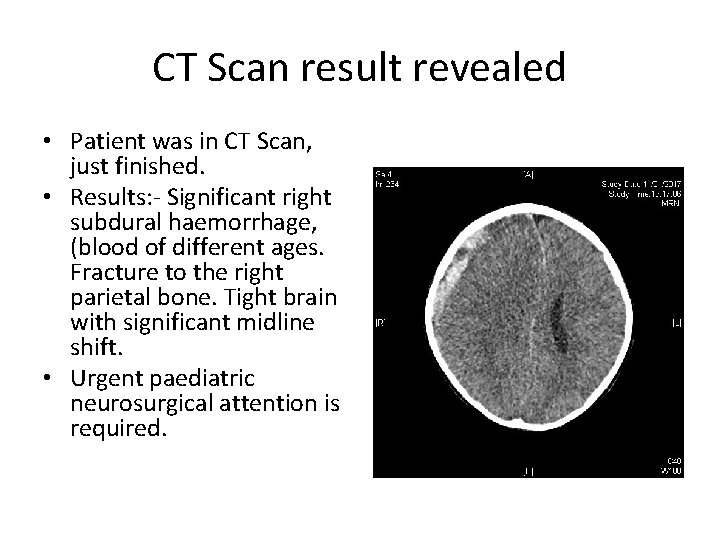
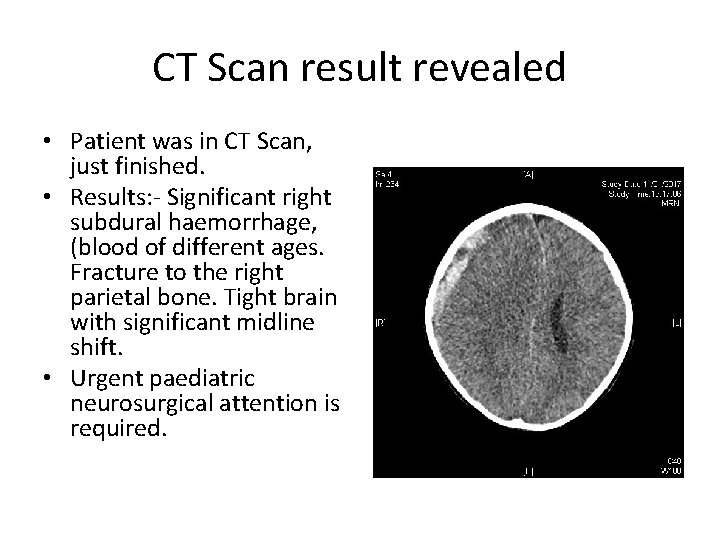
CT Scan result revealed • Patient was in CT Scan, just finished. • Results: - Significant right subdural haemorrhage, (blood of different ages. Fracture to the right parietal bone. Tight brain with significant midline shift. • Urgent paediatric neurosurgical attention is required.
Priorities at this point?
What priorities were established? • • Continued on propofol sedation Neuroprotective measures Emergency treatment – 3% saline Sited 3 rd IV line to commence dopamine 10 mcg/kg/minute Counselled family Senior communication with Royal Manchester Children’s Hospital Neurosurgeon and child straight to paediatric theatre Preparation for transfer – monitor, ventilator, harness, emergency drugs available (gelofusine, resus adrenaline and 3% saline), emergency airway kit (mask, bagging circuit and geudel, re-intubation kit) Pre-departure patient and team checks
Next Time line • 19. 18 Arrival at DGH • 20. 00 left DGH • 20. 18 Arrival at RMCH theatre
Learning points • • Mannitol / 3% Saline. Propofol / Morphine and Midazolam. NIBP / IVBP. Cannula / Central line. Start Inotropes / Not start. To Scan / Not to Scan. Take Parents / Police take Parents.
What went right for this child? • ED Leadership • Paediatric Consultant assessment and referral • Communication and action of the anaesthetic team • ED Nurses • Prompt CT scan • NWTS advice and mobilisation • Response of the paediatric neurosurgeon and theatre team at RMCH • Availability of a PICU bed post-op
Update • On arrival patient had a right sided craniotomy evacuation of the subdural Haemorrhage and a intracranial pressure monitor inserted • She went back to theatre for bone flap 72 hours later • The child was intubated for 18 days • Remained on PICU for 19 days • Transferred to ward for neuro rehabilitation • Biological father is the main carer • Mother has supervised access • Mothers partner remains in custody

Thank you to all the staff for allowing us to use the call and the information it provided
Any questions