Purpose Fishbone Measures MethodsProcedure Catheter associated urinary tract
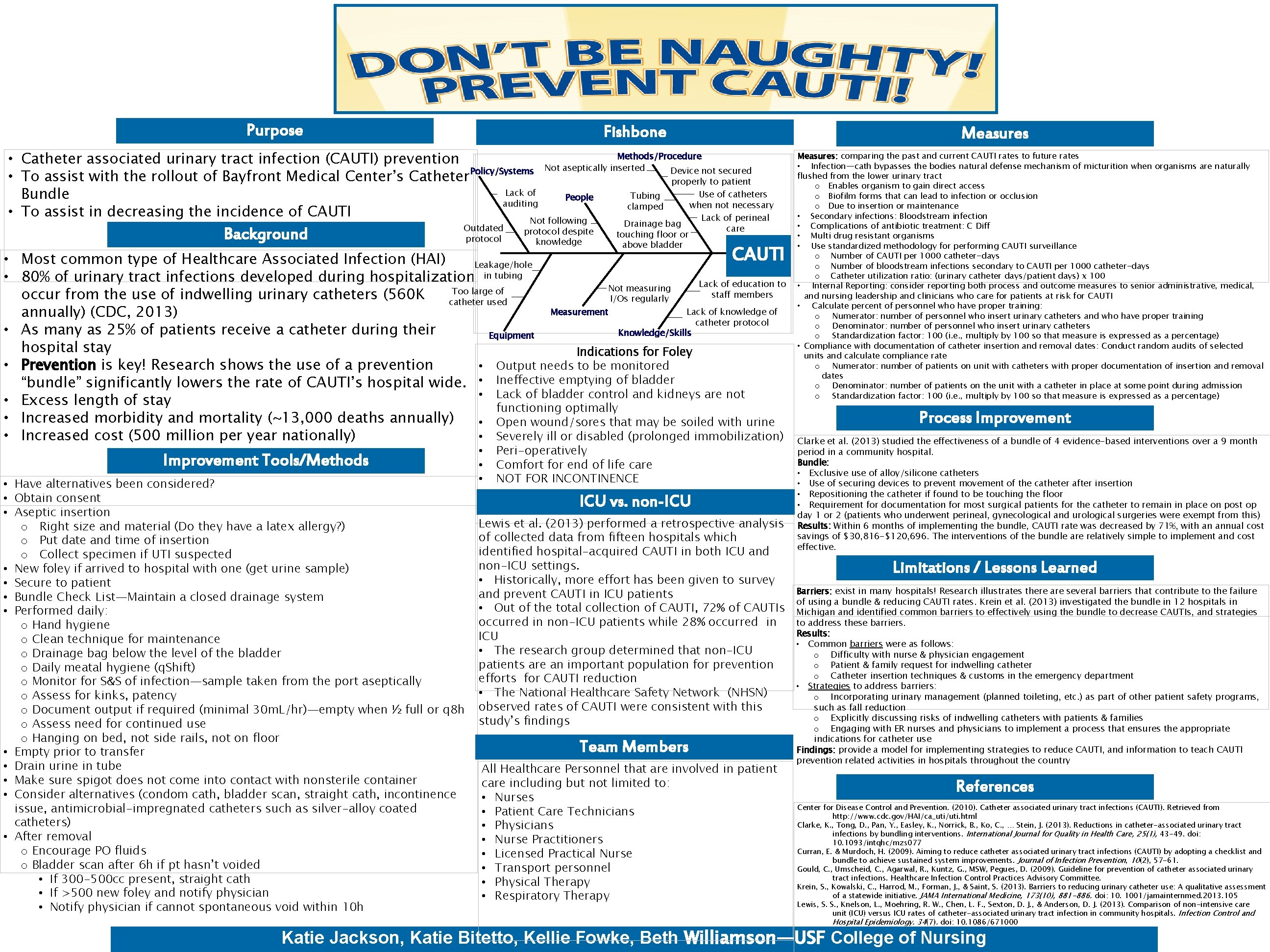
Purpose Fishbone Measures Methods/Procedure • Catheter associated urinary tract infection (CAUTI) prevention Device not secured Policy/Systems Not aseptically inserted • To assist with the rollout of Bayfront Medical Center’s Catheter properly to patient Lack of Use of catheters Tubing Bundle People auditing when not necessary clamped • To assist in decreasing the incidence of CAUTI Lack of perineal Not following Background Outdated protocol despite knowledge Drainage bag touching floor or above bladder care CAUTI • Most common type of Healthcare Associated Infection (HAI) Leakage/hole • 80% of urinary tract infections developed during hospitalization in tubing Lack of education to Not measuring Too large of staff members occur from the use of indwelling urinary catheters (560 K I/Os regularly catheter used Measurement Lack of knowledge of annually) (CDC, 2013) catheter protocol • As many as 25% of patients receive a catheter during their Knowledge/Skills Equipment hospital stay Indications for Foley • Output needs to be monitored • Prevention is key! Research shows the use of a prevention “bundle” significantly lowers the rate of CAUTI’s hospital wide. • Ineffective emptying of bladder • Lack of bladder control and kidneys are not • Excess length of stay functioning optimally • Increased morbidity and mortality (~13, 000 deaths annually) • Open wound/sores that may be soiled with urine • Severely ill or disabled (prolonged immobilization) • Increased cost (500 million per year nationally) Improvement Tools/Methods • Have alternatives been considered? • Obtain consent • Aseptic insertion o Right size and material (Do they have a latex allergy? ) o Put date and time of insertion o Collect specimen if UTI suspected • New foley if arrived to hospital with one (get urine sample) • Secure to patient • Bundle Check List—Maintain a closed drainage system • Performed daily: o Hand hygiene o Clean technique for maintenance o Drainage bag below the level of the bladder o Daily meatal hygiene (q. Shift) o Monitor for S&S of infection—sample taken from the port aseptically o Assess for kinks, patency o Document output if required (minimal 30 m. L/hr)—empty when ½ full or q 8 h o Assess need for continued use o Hanging on bed, not side rails, not on floor • Empty prior to transfer • Drain urine in tube • Make sure spigot does not come into contact with nonsterile container • Consider alternatives (condom cath, bladder scan, straight cath, incontinence issue, antimicrobial-impregnated catheters such as silver-alloy coated catheters) • After removal o Encourage PO fluids o Bladder scan after 6 h if pt hasn’t voided • If 300 -500 cc present, straight cath • If >500 new foley and notify physician • Notify physician if cannot spontaneous void within 10 h • • • Peri-operatively Comfort for end of life care NOT FOR INCONTINENCE ICU vs. non-ICU Lewis et al. (2013) performed a retrospective analysis of collected data from fifteen hospitals which identified hospital-acquired CAUTI in both ICU and non-ICU settings. • Historically, more effort has been given to survey and prevent CAUTI in ICU patients • Out of the total collection of CAUTI, 72% of CAUTIs occurred in non-ICU patients while 28% occurred in ICU • The research group determined that non-ICU patients are an important population for prevention efforts for CAUTI reduction • The National Healthcare Safety Network (NHSN) observed rates of CAUTI were consistent with this study’s findings Team Members All Healthcare Personnel that are involved in patient care including but not limited to: • Nurses • Patient Care Technicians • Physicians • Nurse Practitioners • Licensed Practical Nurse • Transport personnel • Physical Therapy • Respiratory Therapy Measures: comparing the past and current CAUTI rates to future rates • Infection—cath bypasses the bodies natural defense mechanism of micturition when organisms are naturally flushed from the lower urinary tract o Enables organism to gain direct access o Biofilm forms that can lead to infection or occlusion o Due to insertion or maintenance • Secondary infections: Bloodstream infection • Complications of antibiotic treatment: C Diff • Multi drug resistant organisms • Use standardized methodology for performing CAUTI surveillance o Number of CAUTI per 1000 catheter-days o Number of bloodstream infections secondary to CAUTI per 1000 catheter-days o Catheter utilization ratio: (urinary catheter days/patient days) x 100 • Internal Reporting: consider reporting both process and outcome measures to senior administrative, medical, and nursing leadership and clinicians who care for patients at risk for CAUTI • Calculate percent of personnel who have proper training: o Numerator: number of personnel who insert urinary catheters and who have proper training o Denominator: number of personnel who insert urinary catheters o Standardization factor: 100 (i. e. , multiply by 100 so that measure is expressed as a percentage) • Compliance with documentation of catheter insertion and removal dates: Conduct random audits of selected units and calculate compliance rate o Numerator: number of patients on unit with catheters with proper documentation of insertion and removal dates o Denominator: number of patients on the unit with a catheter in place at some point during admission o Standardization factor: 100 (i. e. , multiply by 100 so that measure is expressed as a percentage) Process Improvement Clarke et al. (2013) studied the effectiveness of a bundle of 4 evidence-based interventions over a 9 month period in a community hospital. Bundle: • Exclusive use of alloy/silicone catheters • Use of securing devices to prevent movement of the catheter after insertion • Repositioning the catheter if found to be touching the floor • Requirement for documentation for most surgical patients for the catheter to remain in place on post op day 1 or 2 (patients who underwent perineal, gynecological and urological surgeries were exempt from this) Results: Within 6 months of implementing the bundle, CAUTI rate was decreased by 71%, with an annual cost savings of $30, 816 -$120, 696. The interventions of the bundle are relatively simple to implement and cost effective. Limitations / Lessons Learned Barriers: exist in many hospitals! Research illustrates there are several barriers that contribute to the failure of using a bundle & reducing CAUTI rates. Krein et al. (2013) investigated the bundle in 12 hospitals in Michigan and identified common barriers to effectively using the bundle to decrease CAUTIs, and strategies to address these barriers. Results: • Common barriers were as follows: o Difficulty with nurse & physician engagement o Patient & family request for indwelling catheter o Catheter insertion techniques & customs in the emergency department • Strategies to address barriers: o Incorporating urinary management (planned toileting, etc. ) as part of other patient safety programs, such as fall reduction o Explicitly discussing risks of indwelling catheters with patients & families o Engaging with ER nurses and physicians to implement a process that ensures the appropriate indications for catheter use Findings: provide a model for implementing strategies to reduce CAUTI, and information to teach CAUTI prevention related activities in hospitals throughout the country References Center for Disease Control and Prevention. (2010). Catheter associated urinary tract infections (CAUTI). Retrieved from http: //www. cdc. gov/HAI/ca_uti/uti. html Clarke, K. , Tong, D. , Pan, Y. , Easley, K. , Norrick, B. , Ko, C. , … Stein, J. (2013). Reductions in catheter-associated urinary tract infections by bundling interventions. International Journal for Quality in Health Care, 25(1), 43 -49. doi: 10. 1093/intqhc/mzs 077 Curran, E. & Murdoch, H. (2009). Aiming to reduce catheter associated urinary tract infections (CAUTI) by adopting a checklist and bundle to achieve sustained system improvements. Journal of Infection Prevention, 10(2), 57 -61. Gould, C. , Umscheid, C. , Agarwal, R. , Kuntz, G. , MSW, Pegues, D. (2009). Guideline for prevention of catheter associated urinary tract infections. Healthcare Infection Control Practices Advisory Committee. Krein, S. , Kowalski, C. , Harrod, M. , Forman, J. , & Saint, S. (2013). Barriers to reducing urinary catheter use: A qualitative assessment of a statewide initiative. JAMA International Medicine, 173(10), 881 -886. doi: 10. 1001/jamainternmed. 2013. 105 Lewis, S. S. , Knelson, L. , Moehring, R. W. , Chen, L. F. , Sexton, D. J. , & Anderson, D. J. (2013). Comparison of non-intensive care unit (ICU) versus ICU rates of catheter-associated urinary tract infection in community hospitals. Infection Control and Hospital Epidemiology. 34(7). doi: 10. 1086/671000 Katie Jackson, Katie Bitetto, Kellie Fowke, Beth Williamson—USF College of Nursing
- Slides: 1