Pumping up the Pressure Dr Steve Pincus July
- Slides: 24
Pumping up the Pressure Dr Steve Pincus July 2018
Terminology • Mode -3 variables – Control variable –volume &flow or pressure • What triggers the breath-time, flow, pressure • What limits it-time, pressure • What ends it-time, volume – Breath sequence • Continuous mandatory • Intermittent mandatory • Spontaneous – Type of control • Fixed, variable, adaptive, intuitive
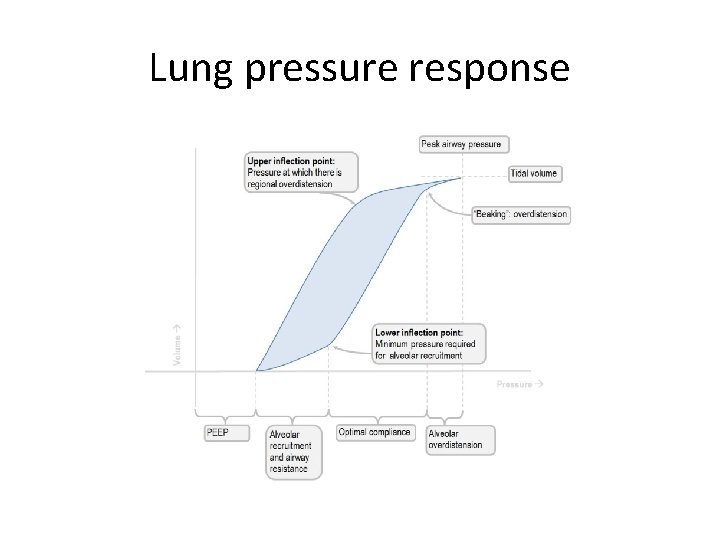
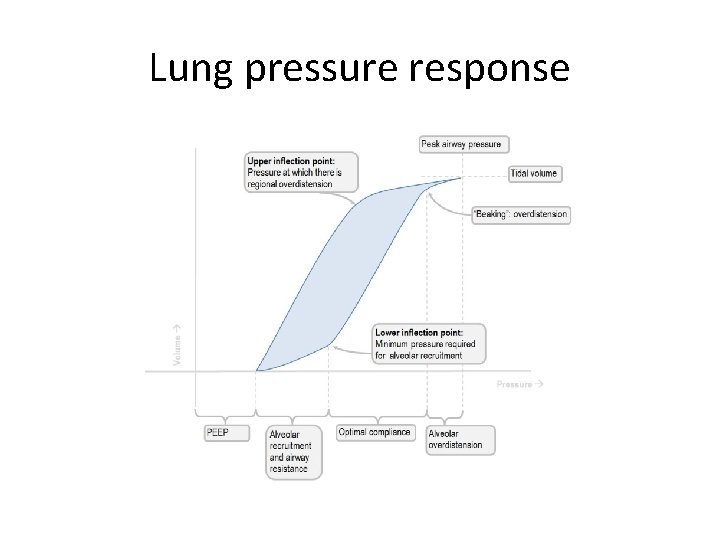
Lung pressure response
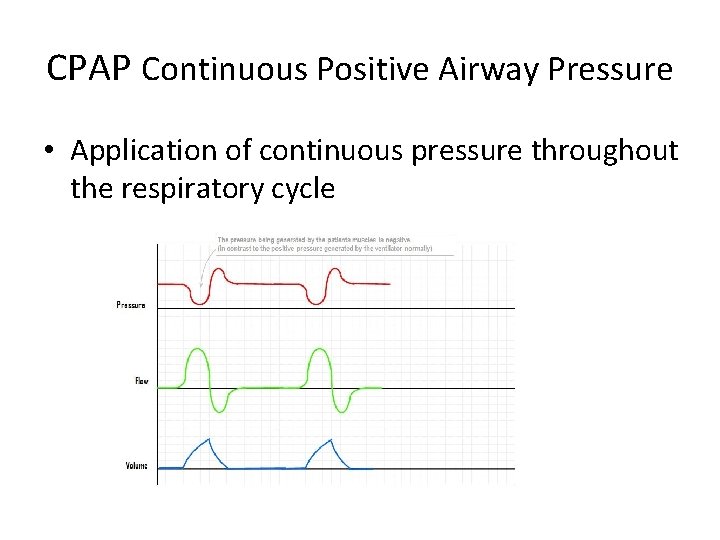
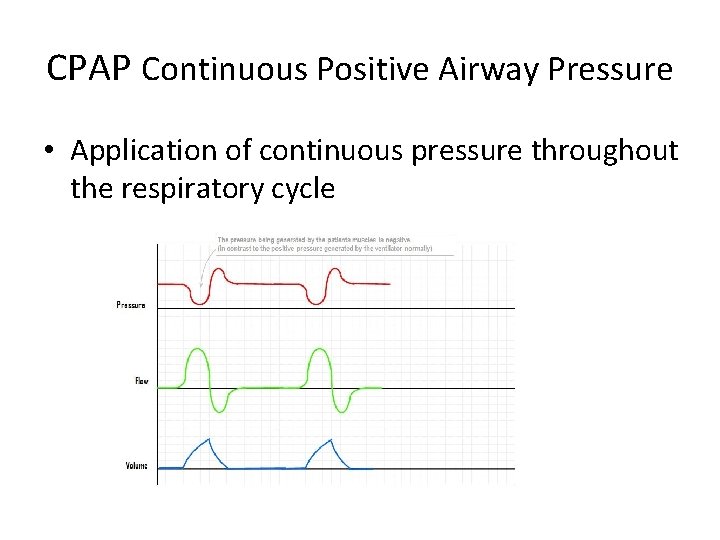
CPAP Continuous Positive Airway Pressure • Application of continuous pressure throughout the respiratory cycle
Physiology of CPAP • Lung volume – increases distension – Decreases airway closure & increases recruitment • Gas exchange – Increase lung volume increases gas exchange surface ( O 2 > C 02) – Increase alveolar volume reduces interstitial fluid which decreases diffusion distance= dewaters the lung • WOB – Positive assist for inspiration – Antagonises intrinsic PEEP
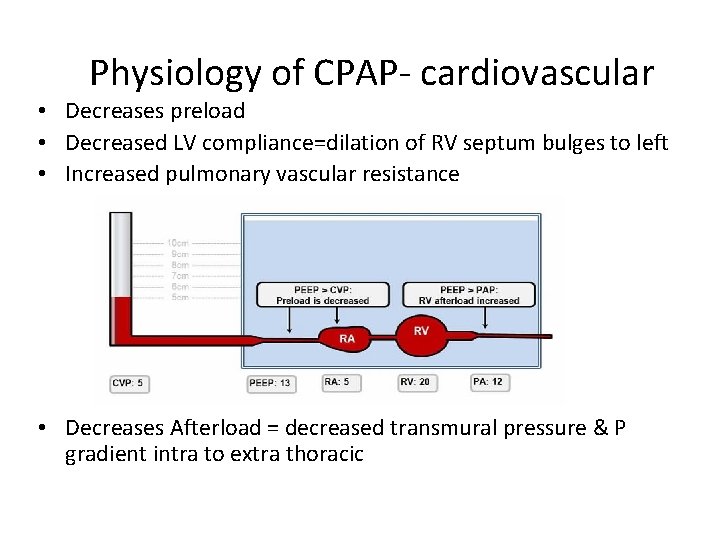
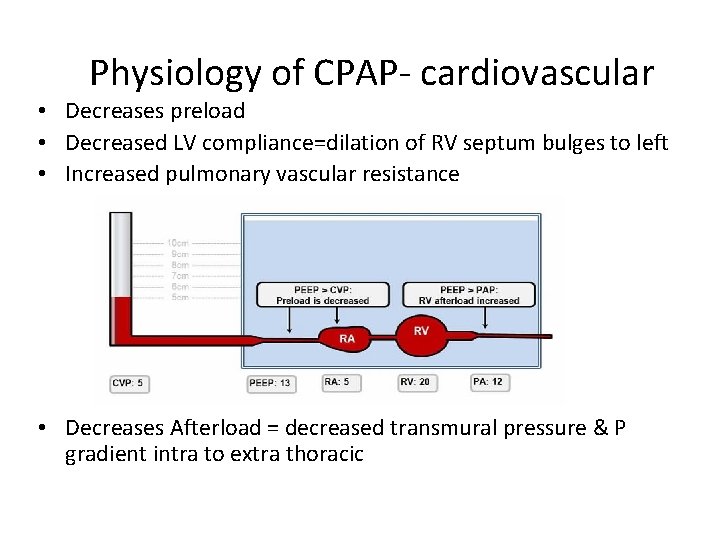
Physiology of CPAP- cardiovascular • Decreases preload • Decreased LV compliance=dilation of RV septum bulges to left • Increased pulmonary vascular resistance • Decreases Afterload = decreased transmural pressure & P gradient intra to extra thoracic
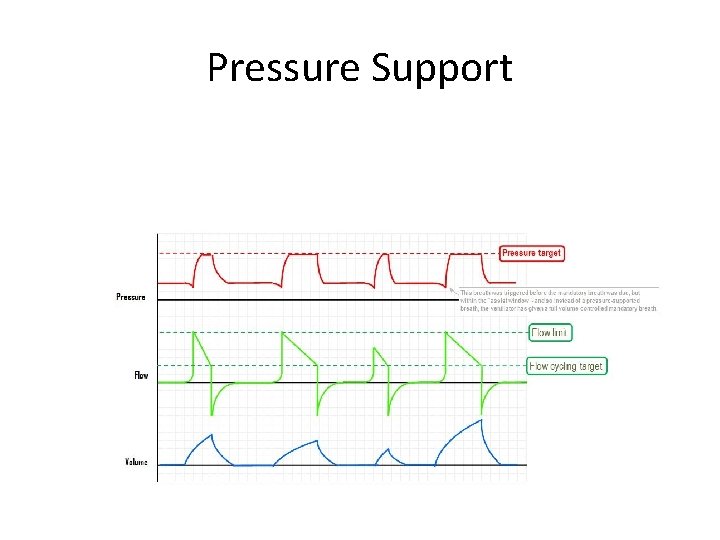
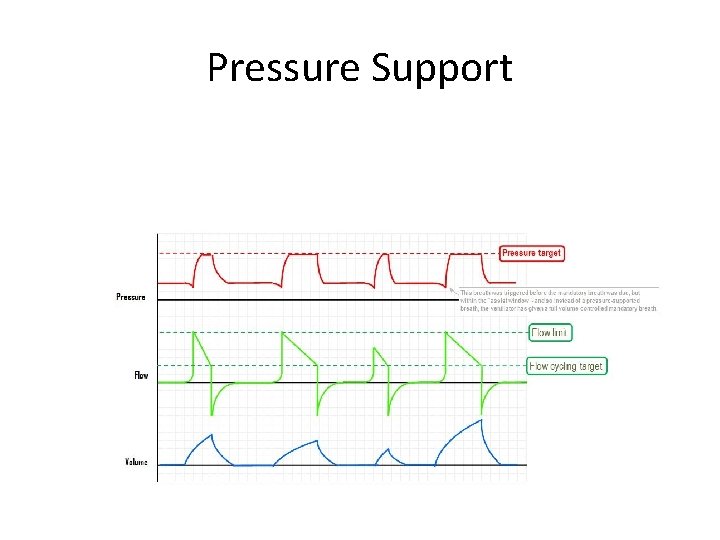
Pressure Support
IPS or IPAP • • Inspiratory pressure support Patient triggered assist for inspiration Increased tidal volume, decreased WOB Need to set – – pressure support Trigger (flow patient generated to trigger IPS Rate, volume , I: E ratio are all set by patient Can set an escape or backup rate • Flow must be faster than the patients own max inspiratory flow or P will drop ( also have to allow for leaks depending on interface)
Physiology of IPS • Increased Tidal volume, decrease WOB • Negative effects of CPAP are largely increased by addition of IPS • As the pressure is not sustained many of the benefits of CPAP are not greatly improved by adding IPS • CPAP for CCF & severe pneumonia • CPAP + IPS for everything else
SIMV- Synchronised Intermittent Mandatory Ventilation • • Volume or pressure controlled Triggered (time or flow) Time cycled Patient can influence the triggering of both mandatory breaths and spontaneous breaths – Mandatory breaths= assist control breath – True spontaneous breaths may have an IPS added
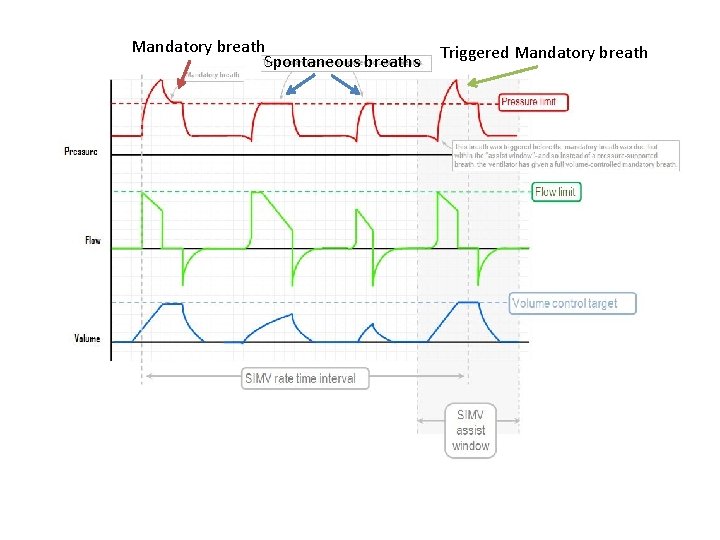
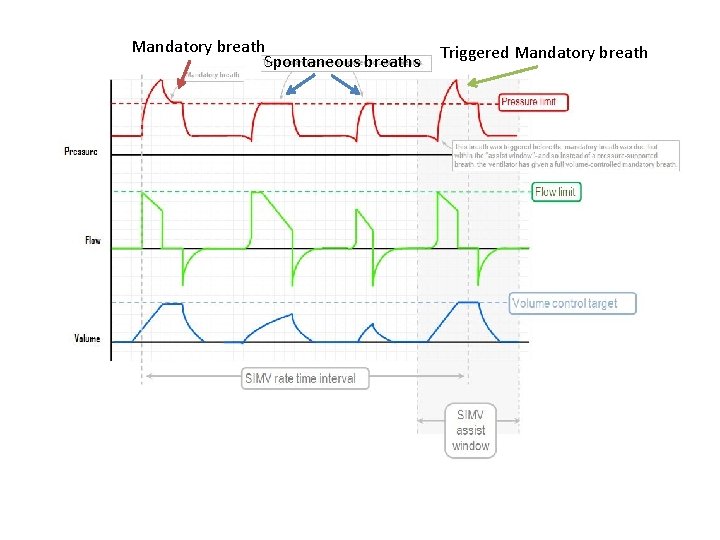
Mandatory breath Spontaneous breaths Triggered Mandatory breath
PCV Pressure controlled ventilation • • Pressure Controlled Time or flow triggered (SIMV) Time cycled Set – peak inspiratory pressure – Inspiratory time – Rate – Trigger – +/- IPS for true spontaneous breaths
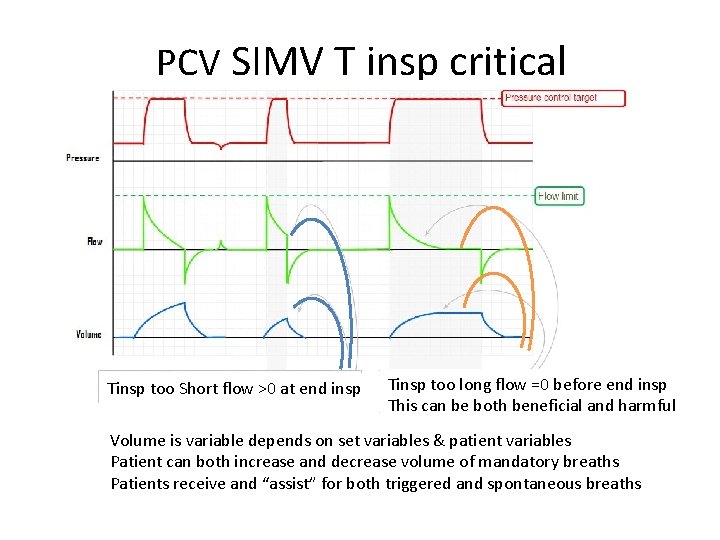
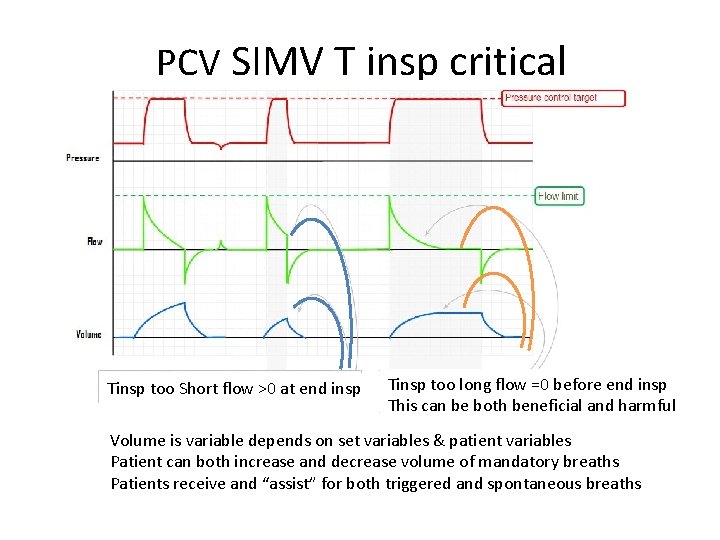
PCV SIMV T insp critical Tinsp too Short flow >0 at end insp Tinsp too long flow =0 before end insp This can be both beneficial and harmful Volume is variable depends on set variables & patient variables Patient can both increase and decrease volume of mandatory breaths Patients receive and “assist” for both triggered and spontaneous breaths
PCV • Flow is dynamic & decelerates as approaches set Pinsp • Volume variable • Good for patients where you are happy to let them “take what they want” – May reduce sedation needs – Decreases WOB for spontaneous and triggered breaths • Dynamic flow good for variable compliance
Adaptive Pressure Control - APC • Aims to achieve a desired volume with the lowest possible pressure • Flow dynamic depends on set volume, Tinsp & lung compliance • Volume controlled • Time triggered &/or flow triggered • Time cycled • Pressure regulated=set max Pinsp
Where to next • APC • ASV • APRV
APC • Set – Tv – Pinsp max – IPS for true spontaneous breaths – Flow Trigger for triggered & spontaneous breaths – Rate & Tinsp • Ventilated “explores/learns” compliance & varies pressure to achieve targeted volume • Still has problems of all VCV –fixed volume • Autoflow is~=APC
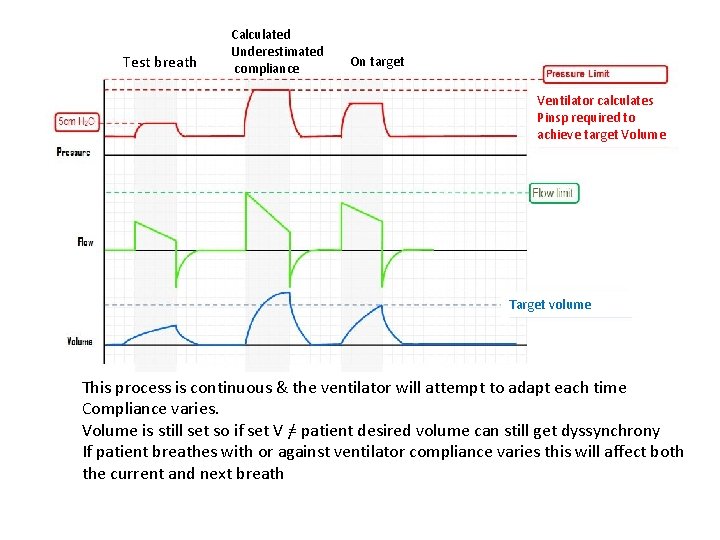
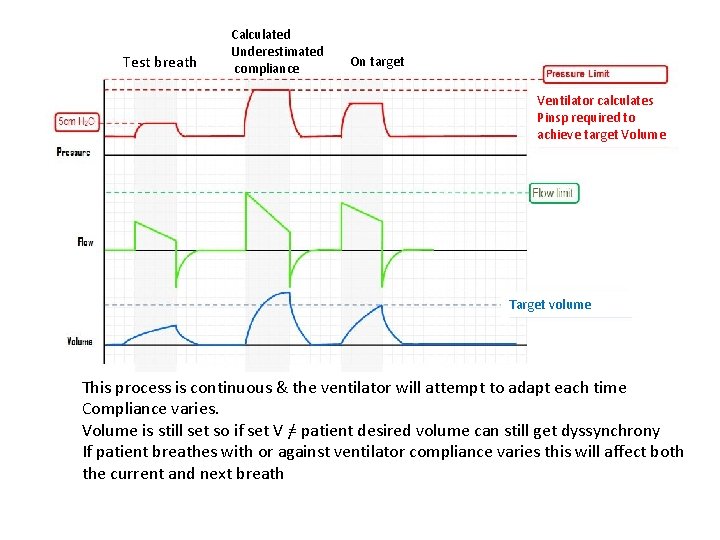
Test breath Calculated Underestimated compliance On target Ventilator calculates Pinsp required to achieve target Volume Target volume This process is continuous & the ventilator will attempt to adapt each time Compliance varies. Volume is still set so if set V =/ patient desired volume can still get dyssynchrony If patient breathes with or against ventilator compliance varies this will affect both the current and next breath
Adaptive Support Ventilation • Volume regulated pressure controlled ventilation • Aims to maintain minimum minute ventilation whilst avoiding – Rapid shallow breathing or excessive dead space ventilation – Excessive PEEP • Aims to recreate- tidal volume & rate – Least WOB – Least ventilator applied pressure
• ASV does not make clinical decisions • Operator specifies – Patient height & gender – % minute volume= for high ventilatory demand patients increase e. g. patient with temp > 38. 5 C % Min. Vol 120% – Trigger for assist and triggered breaths – Expiratory trigger sensitivity, PEEP, Fi. O 2, ramp as required
• Once started the ventilator calculates breathing pattern, tidal volume and rate, that are compatible with a lung protective strategy • ASV pressure limit is 10 mm. Hg below P high • Low Vt = 2 x dead space= 4. 4*IBW • High rate limit is calculated to prevent gas trapping and Auto. PEEP
• Initial Mode PCV SIMV – If patient breathes – triggers a breath which is Pressure supported and flow cycled – If patient does not breathe-PC and time cycled – Ventilator supports/delivers 3 breaths and compares the F and Vt to the target – If Vt < target Pinsp is – If F < target Rate is • This process is continuous based on the last 5 breaths • Really it is what we do without having to continuously fiddle with the ventilator
Airway Pressure Release Ventilation APRV Effectively Bilevel PEEP (inverse ratio PCV) Expiration occurs during low PEEP Inspiration occurs during transition from low to high Low PEEP short to avoid de-recruitment usually set to be when expiratory flow falls to ~75 -50% of maximum (I: E ratios 6 -12: 1 Tlow ~0. 25 -1 second) • Patient can breath during either phase • At high PEEP the patient can still breath but does from a full lung so compliance maybe very low • •
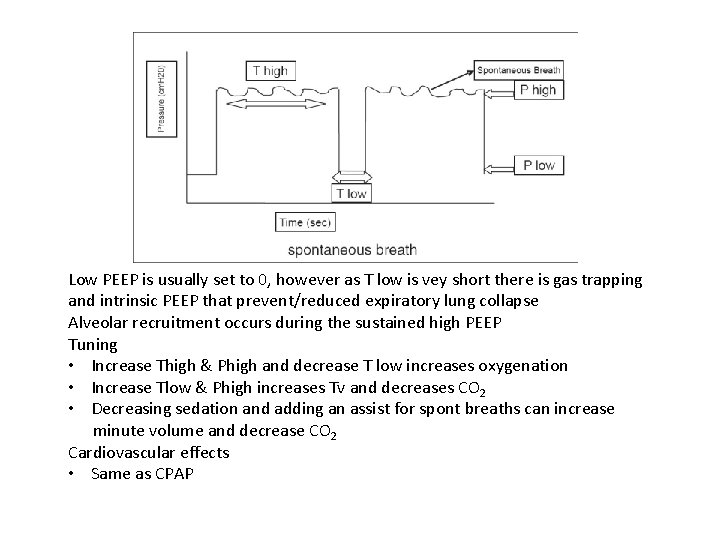
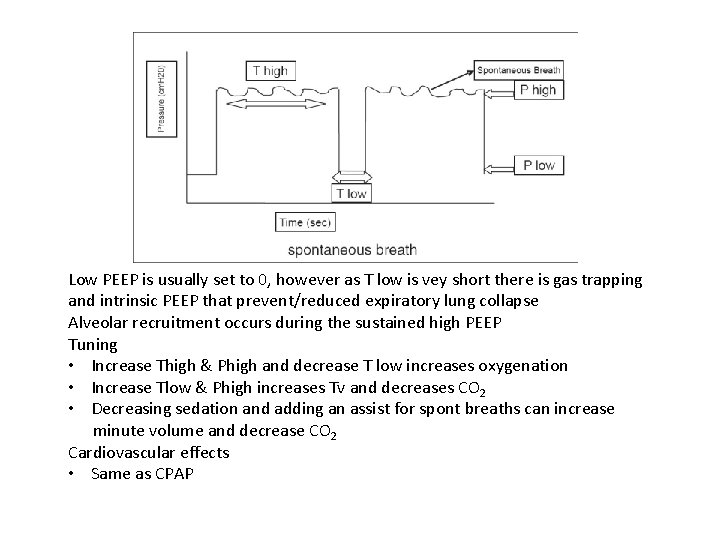
Low PEEP is usually set to 0, however as T low is vey short there is gas trapping and intrinsic PEEP that prevent/reduced expiratory lung collapse Alveolar recruitment occurs during the sustained high PEEP Tuning • Increase Thigh & Phigh and decrease T low increases oxygenation • Increase Tlow & Phigh increases Tv and decreases CO 2 • Decreasing sedation and adding an assist for spont breaths can increase minute volume and decrease CO 2 Cardiovascular effects • Same as CPAP