Pulpotomy Apexogenesis and Apexification Pulpotomy Definition Pulpotomy is


- Slides: 38
Pulpotomy, Apexogenesis and Apexification
Pulpotomy Definition Ø Pulpotomy is defined as the amputation of damaged and inflammed vital pulp from the coronal chamber followed by placement of a medicament over the radicular pulp stumps to stimulate repair, fixation or mummification of the remaining vital radicular pulp. - Braham & Morris 1985 Ø Pulpotomy is defined as the surgical removal of infected coronal pulp and its objectives are preservation of the radicular pulp vitality and relief of pain.
Rationale of Pulpotomy Ø When the coronal pulp is exposed due to caries, trauma or operative procedures. It produces inflammatory changes in the pulp. Ø Through the surgical excision of the coronal pulp the infected and the inflamed area is removed leaving vital, unaffected pulpal tissue in the root canal well preserved. Ø This efforts in temporary and rapid relief of pulpalgia and the unaffected tissue undergoes repair.
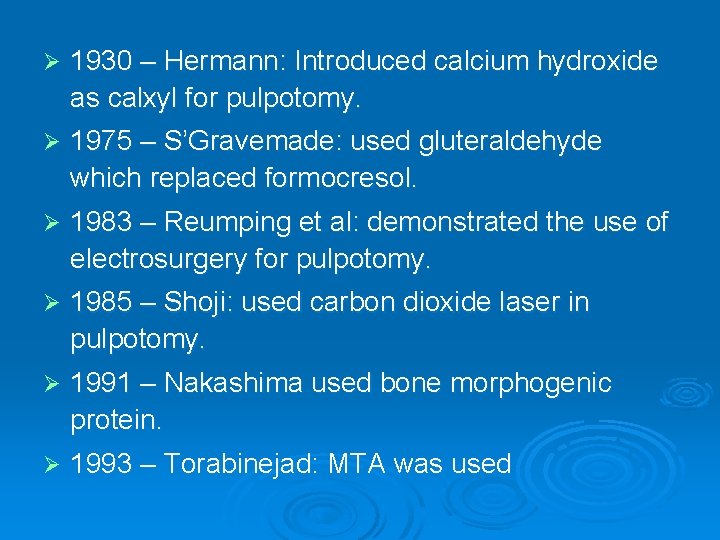
History Ø The Europeans were the first to introduce pulpotomy procedure. Ø 1885 – Leptowski: introduced formalin as fixative and mummifying agent. Ø 1886 – Gold foil was used to cover the exposed vital pulp. Ø 1898 – Gysi: Introduced paraformaldehyde as a pulpotomy medicament. Ø 1904 – Buckley: Introduced formocresol for pulpotomy.
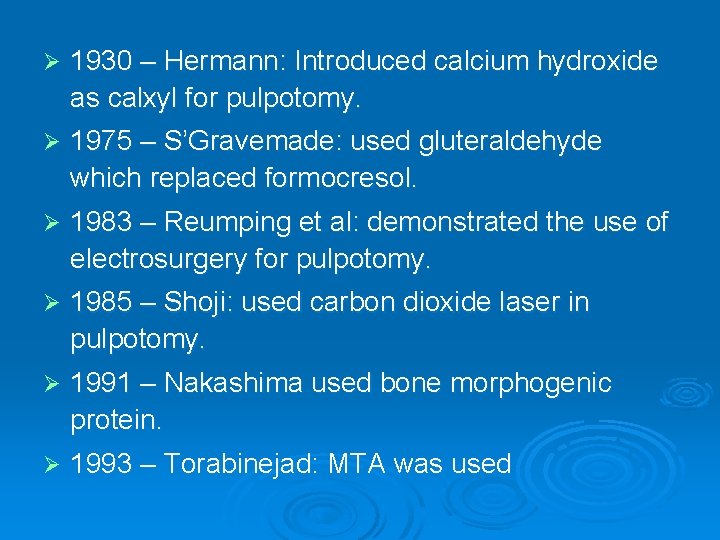
Ø 1930 – Hermann: Introduced calcium hydroxide as calxyl for pulpotomy. Ø 1975 – S’Gravemade: used gluteraldehyde which replaced formocresol. Ø 1983 – Reumping et al: demonstrated the use of electrosurgery for pulpotomy. Ø 1985 – Shoji: used carbon dioxide laser in pulpotomy. Ø 1991 – Nakashima used bone morphogenic protein. Ø 1993 – Torabinejad: MTA was used
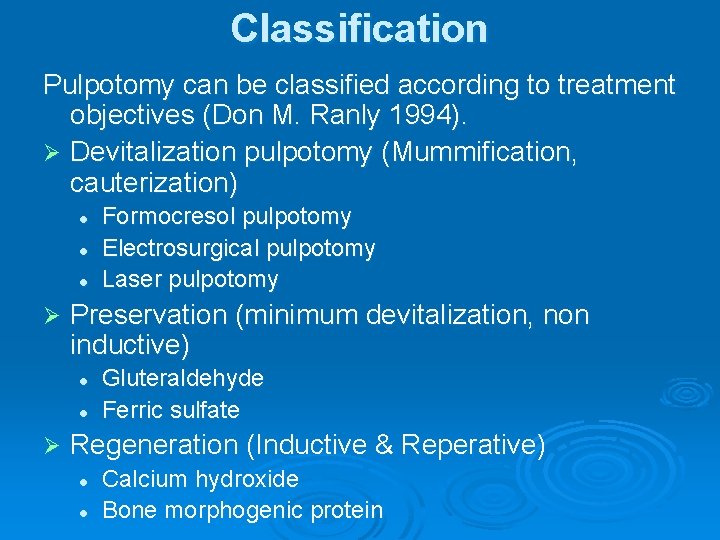
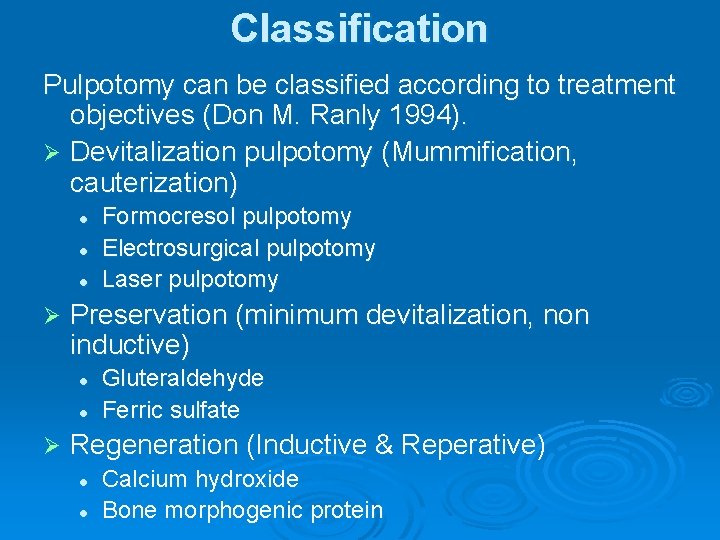
Classification Pulpotomy can be classified according to treatment objectives (Don M. Ranly 1994). Ø Devitalization pulpotomy (Mummification, cauterization) l l l Ø Preservation (minimum devitalization, non inductive) l l Ø Formocresol pulpotomy Electrosurgical pulpotomy Laser pulpotomy Gluteraldehyde Ferric sulfate Regeneration (Inductive & Reperative) l l Calcium hydroxide Bone morphogenic protein
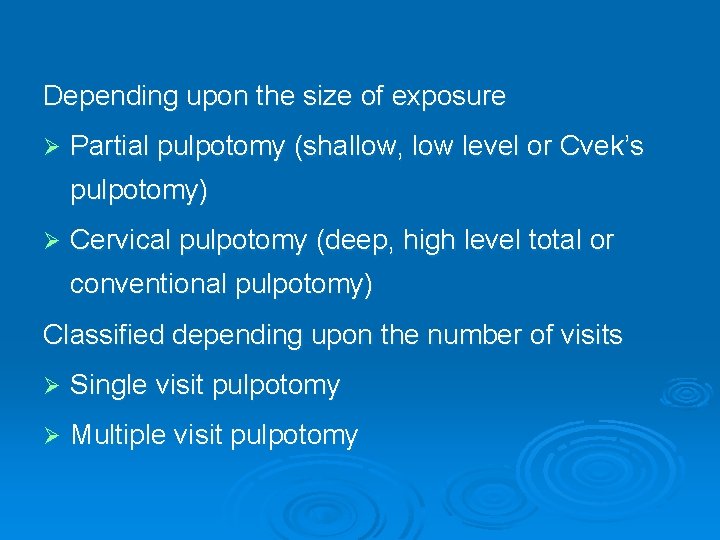
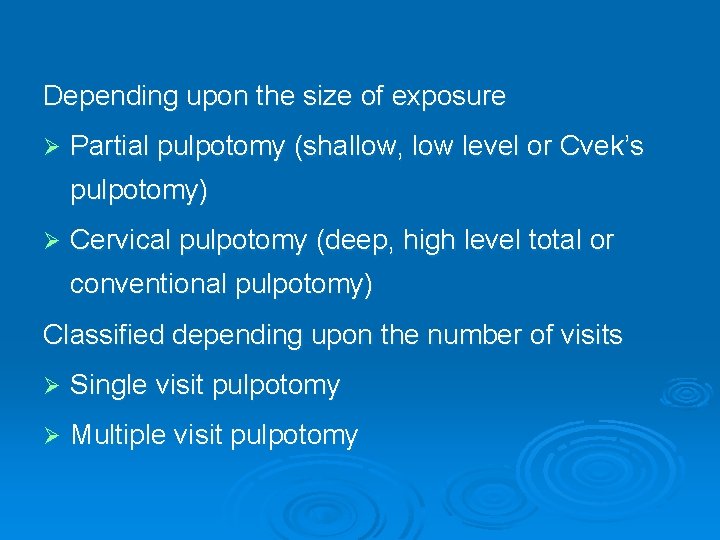
Depending upon the size of exposure Ø Partial pulpotomy (shallow, low level or Cvek’s pulpotomy) Ø Cervical pulpotomy (deep, high level total or conventional pulpotomy) Classified depending upon the number of visits Ø Single visit pulpotomy Ø Multiple visit pulpotomy
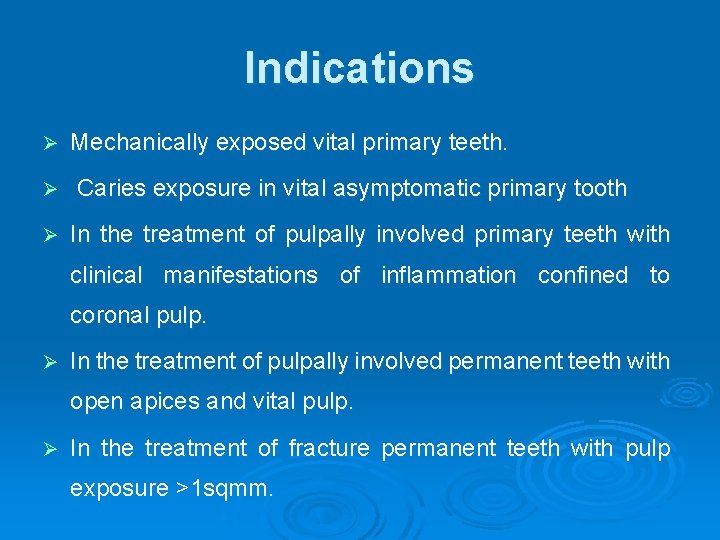
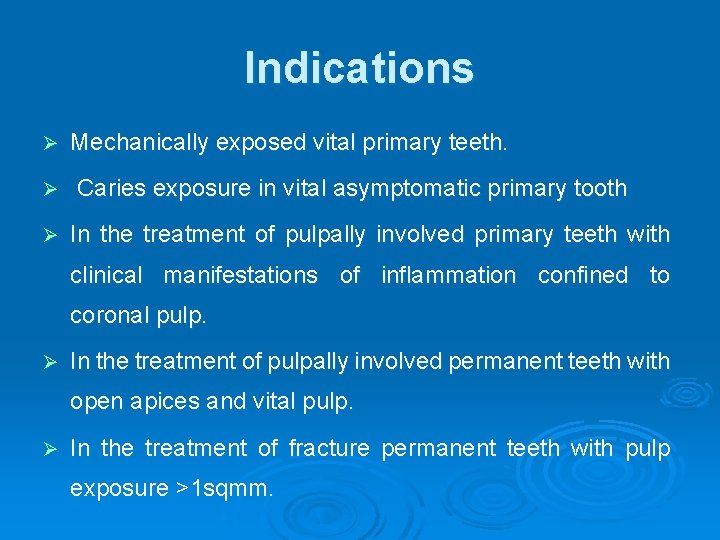
Indications Ø Ø Ø Mechanically exposed vital primary teeth. Caries exposure in vital asymptomatic primary tooth In the treatment of pulpally involved primary teeth with clinical manifestations of inflammation confined to coronal pulp. Ø In the treatment of pulpally involved permanent teeth with open apices and vital pulp. Ø In the treatment of fracture permanent teeth with pulp exposure >1 sqmm.
Contraindications Ø Spontaneous pain Ø Abnormal sensitivity to heat or cold / chronic pulpalgia Ø Tenderness to percussion Ø Swelling / sinus Ø Pus or serous exudates at the exposure site Ø Pathological mobility Ø Uncontrolled hemorrhage from the amputated pulp stumps Ø Pathological external root resorption Ø Periapical or inter radicular radiolucency Ø Internal root resorption Ø Pulp calcification / constriction of pulp chamber
Materials used Ø Ø Ø Formocresol Gluteraldehyde Devitalizing paraformaldehyde paste l l l l Ø Ø Gysi paste Easlicks paraformaldehyde paste Paraform devitalizing paste Camphorated paramonochlorophenol Cresol Metacresyl acetate Oxypara N 2 Compound Zinc oxide eugenol Ferric sulphate Calcium hydroxide Enriched collagen solution
Ø Ø Ø Ø Collagen calcium phosphate gel Dimethyl subirridemate Tetrandrine Freeze dried bone Tricalcium phosphate Chondritin sulfate Sodium hydluronate Dinatured albumin Pure calcium hydroxide apatite Antibiotic paste MTA Dentin bonding agent Bone morphogenic protein
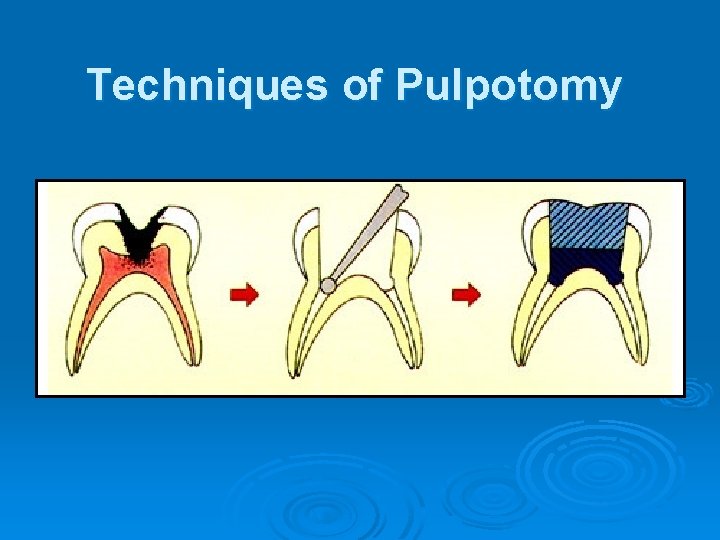
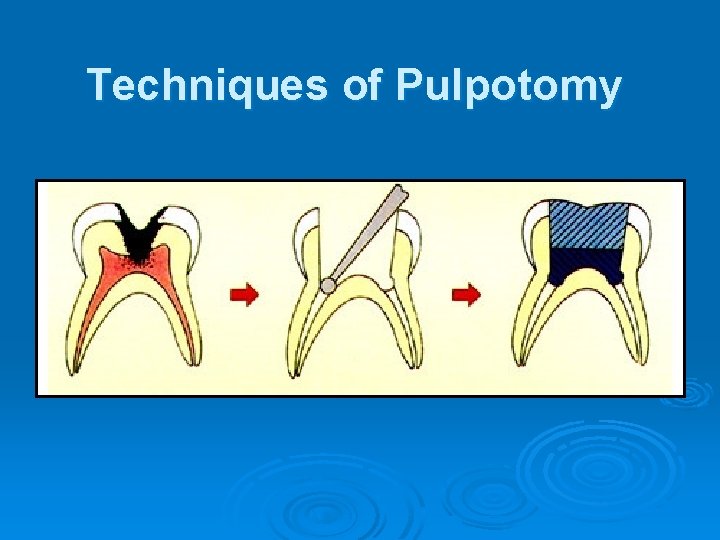
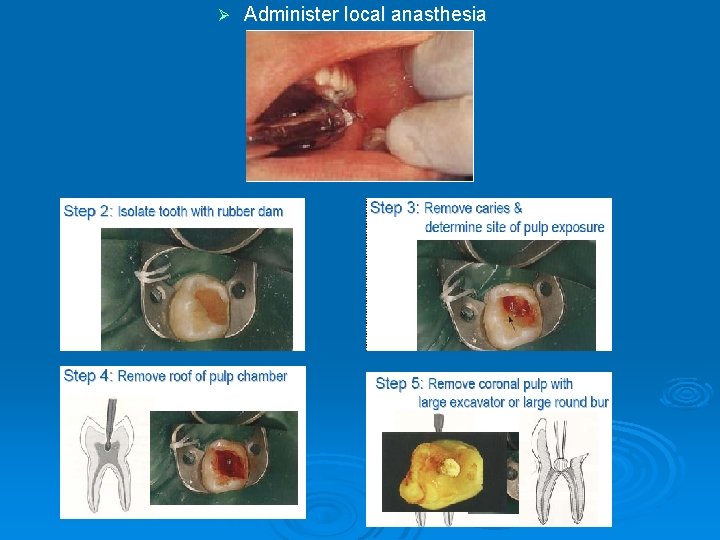
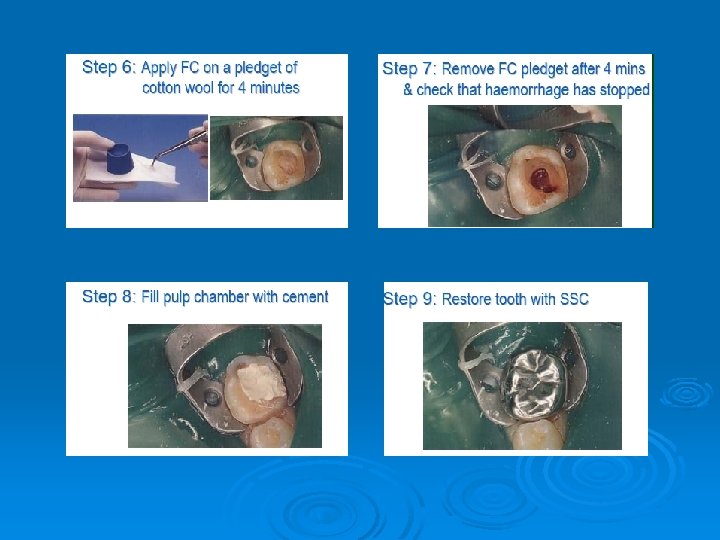
Techniques of Pulpotomy
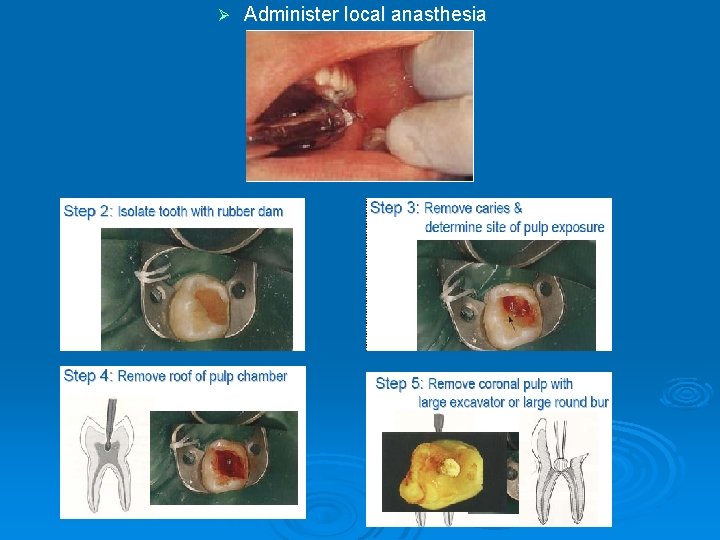
Ø Administer local anasthesia
Types of pulpotomies Ø Non-vital pulpotomy (mortal pulpotomy) Ø Electrosurgical pulpotomy Ø Laser pulpotomy Ø Preservation pulpotomy 1. Gluteraldehyde. 2. Ferric sulphate Ø Partial / Cvek’s pulpotomy Ø Cervical –Webbers pulpotomy Ø Regenerative pulpotomy
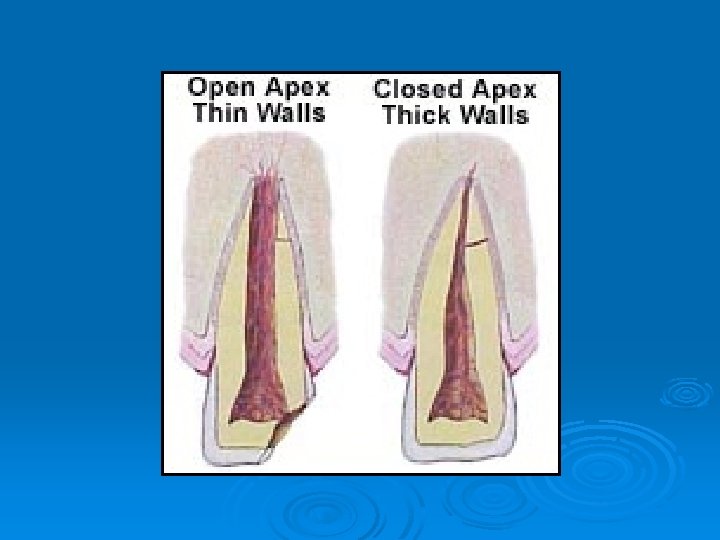
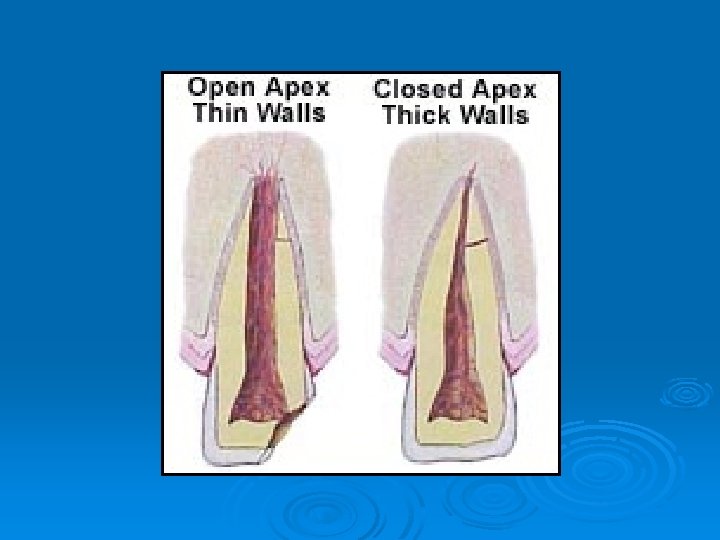
Apexogenesis & Apexification Open apex Ø At the time of tooth eruption root development is only 62 -80% i. e. , 2/3 rd of the root is formed. Ø If due to trauma or caries exposure the pulp undergoes necrosis, dentin formation ceases and root growth is arrested. Ø The resultant immature root will have an open apex which is also called as blunder buss canal.
Problems faced with open apex Ø due to large apical diameter and smaller coronal canal diameter debridement is difficult. Ø Lack of apical stop makes obturation difficult. Ø The thin root canal walls become prone to fracture.
Ø Earlier open apices have been treated by periapical surgery with a retrograde filling but surgery has its drawbacks. l l l Relative to the already shortened root, further root reduction (apicectomy) could result in an inadequate crown root ratio. The apical walls are thin and could shatter when touched with a rotating bur. The thin walls would make condensation of a retrograde filling difficult.
l l l The periapical tissue may not adapt to the wide and irregular surface of the amalgam. Surgery would remove the root sheath and prevent for further root development. Surgery would be both physically and psychologically traumatic to the patient.
Ø Thus It is best to treat immature teeth with a non surgical approach. Ø Based on the vitality of the pulp if the immature tooth has vital pulp exhibiting reversible pulpitis physiological root end development or apexogenesis is attempted. Ø If irreversible pulpitis is present there is when pulp is necrotic then root end closure is done by apexification.
Apexogenesis Ø It is defined as physiological development and formation – Association of Endodontists. ) root end (American Ø The current terminology is vital pulp therapy and is defined by (Walton and Torabinejad) as a treatment of vital pulp in an immature tooth to permit continued dentin formation and apical closure.
Ø This is achieved by: l Indirect pulp capping l Direct pulp capping l Apical closure pulpotomy
Indirect pulp capping & Direct pulp capping Indirect pulp capping Ø It is defined as application of medicament over a thin layer of remaining caries dentin after deep excavation, with no exposure of the pulp. It was first described by Pierre Fauchard. Direct pulp capping Ø It is defined as a placement of a biocompatible agent on healthy pulp tissue that has been inadvertently exposed from caries excavation or traumatic injury.
Materials used Ø Calcium hydroxide Ø MTA Ø Bone morphogenic protein
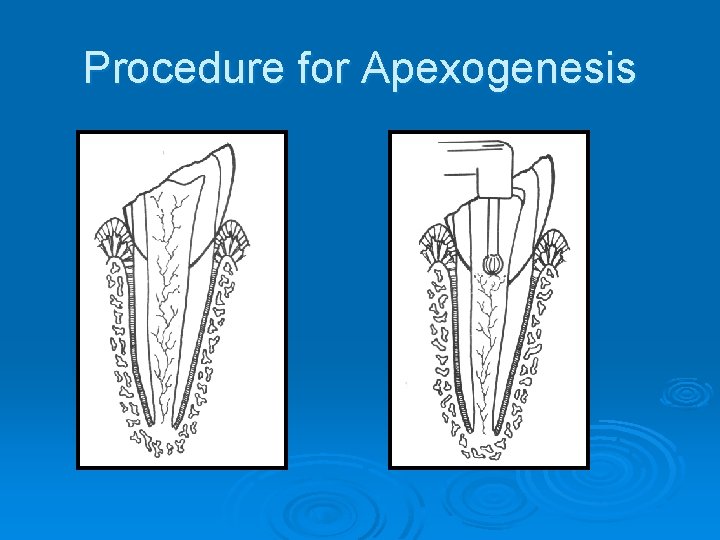
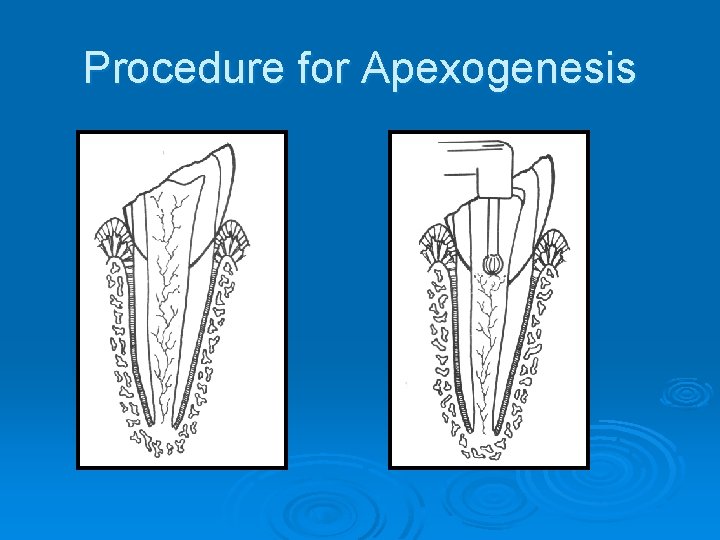
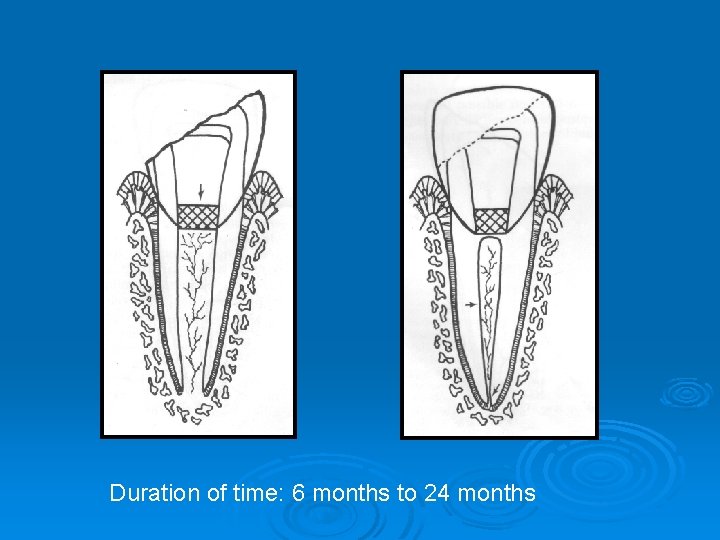
Procedure for Apexogenesis
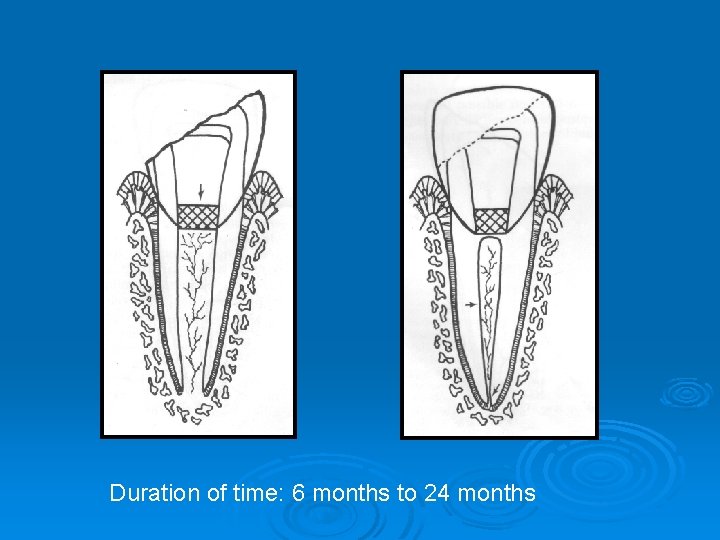
Duration of time: 6 months to 24 months
Clinical Evaluation of Apexogenesis Ø No clinical symptoms Ø No radiogarphic changes in pulp or periapex Ø Continued root development Ø Radiographically observed hard tissue barrier at the site of procedure Ø Sensitivity to vitality testing
Failures of Apexogenesis Ø Cessation of root growth Ø Development of signs and symptoms or periapical lesions Ø Calcific metamorphosis Goals of apexogenesis: Ø Sustain viable Hertwigs epithelial root sheet Ø Maintaining pulp vitality Ø Promoting root end closure Ø Generating a dental bridge at the site of pulpotomy
Apexification is a method of inducing apical closure through the formation mineralized tissue in apical pulp region of a non vital tooth with an incompletely formed root. Ø The mineralized tissue can be osteodentin, osteocementum, or bone or combination of all. Ø Indications Ø Restorable immature tooth with pulp necrosis Contraindications Ø All vertical and unfavourable horizontal root fractures, Ø Resorptions Ø Short roots Ø Periodontally broken down tooth Ø Vital pulp
Factors affecting apexification Ø Age of the patient Ø Root development Ø Location of apex Ø Apical diameter Ø Thorough cleaning & debridement Ø Temporary restorations
Materials used are : Ø Calcium hydroxide Ø Tricaclium phosphate Ø Bone growth factors Ø MTA
Techniques to deal with open apex Ø Custom made roll cone technique Ø Short fill technique by Moodnick Ø Obturation done with guttapercha and sealer with periapical surgery Ø Instrumentation only Ø Induction of periapical bleeding with instrumentations Ø Apical closure technique Ø One visit apexification
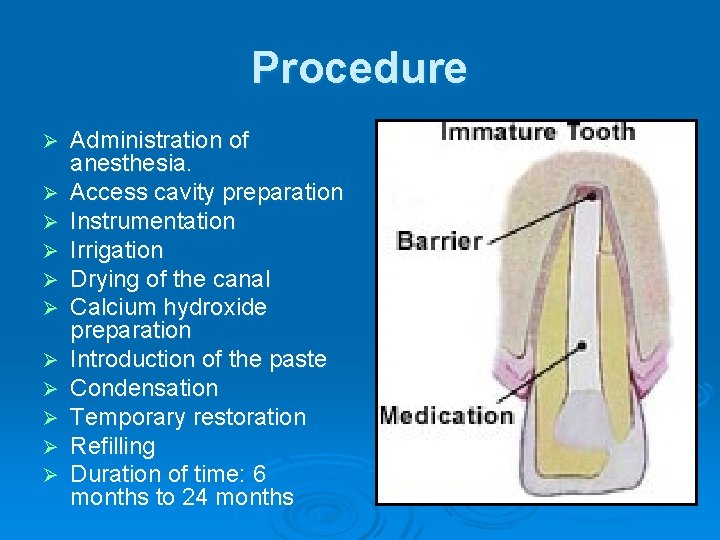
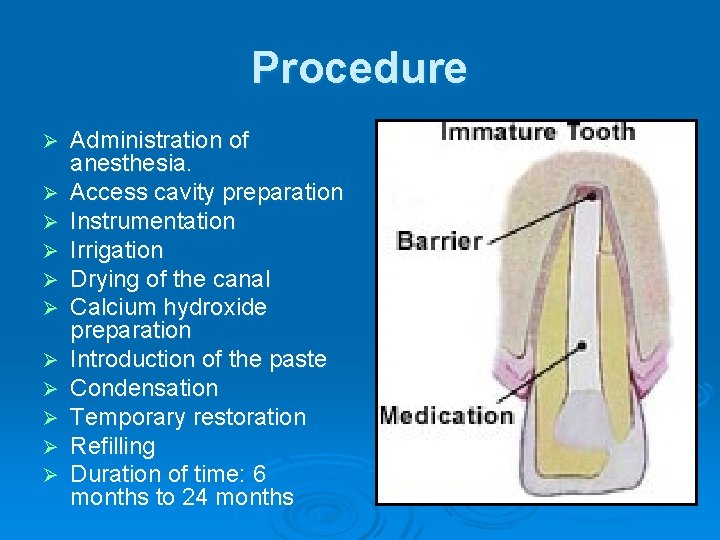
Procedure Ø Ø Ø Administration of anesthesia. Access cavity preparation Instrumentation Irrigation Drying of the canal Calcium hydroxide preparation Introduction of the paste Condensation Temporary restoration Refilling Duration of time: 6 months to 24 months
Evaluating the tooth for obturation Ø Tooth should be symptomless Ø Radiographic observation shows osseous deposition in the periapex Ø Calcium hydroxide is dry in the canal when tested by probing Ø Drying of the canal with paper points Ø Elicits no haemorrhage or tissue fluids Ø Confirming the calcific barrier with small file
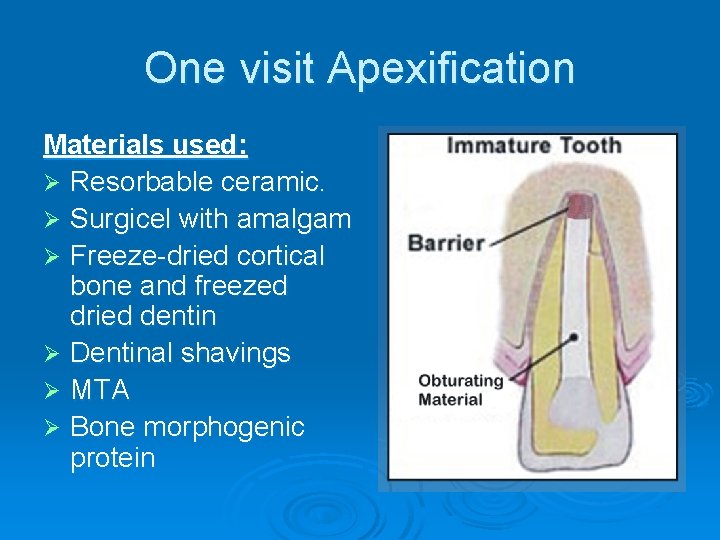
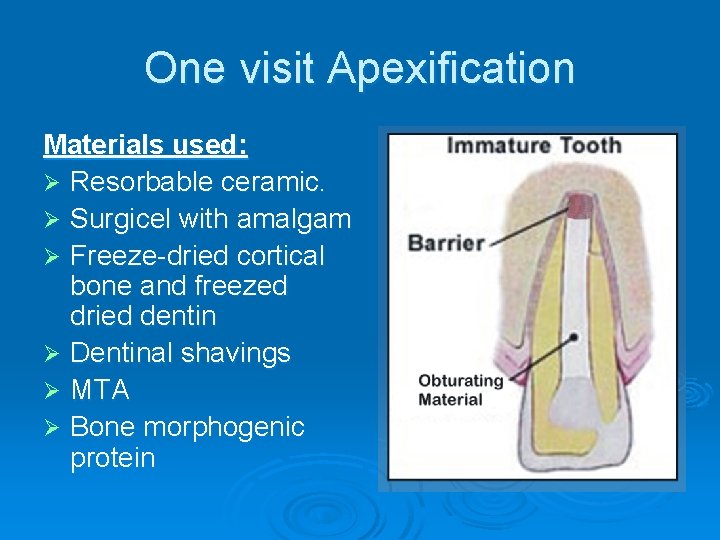
One visit Apexification Materials used: Ø Resorbable ceramic. Ø Surgicel with amalgam Ø Freeze-dried cortical bone and freezed dried dentin Ø Dentinal shavings Ø MTA Ø Bone morphogenic protein

Conclusion
