Pulmonary infection Lecture 2 Pulmonary infections Pneumonia Any
- Slides: 32
Pulmonary infection Lecture 2
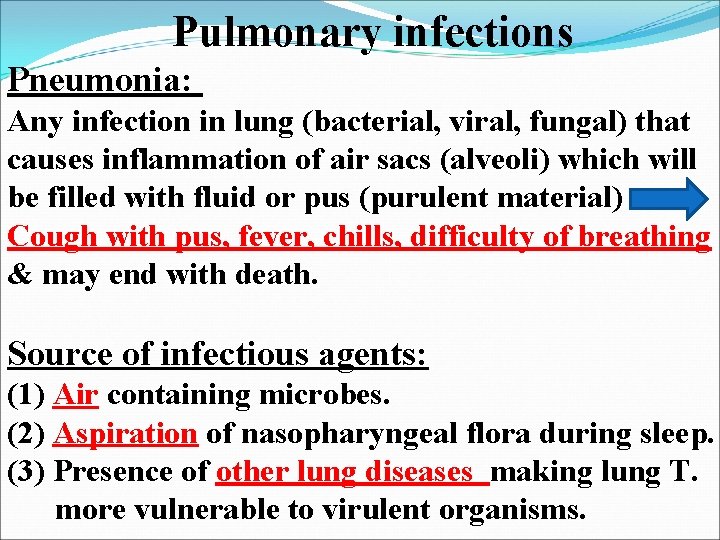
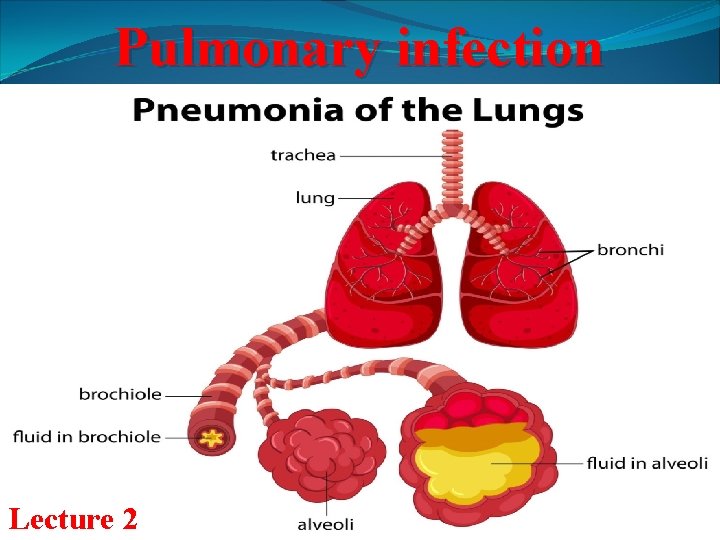
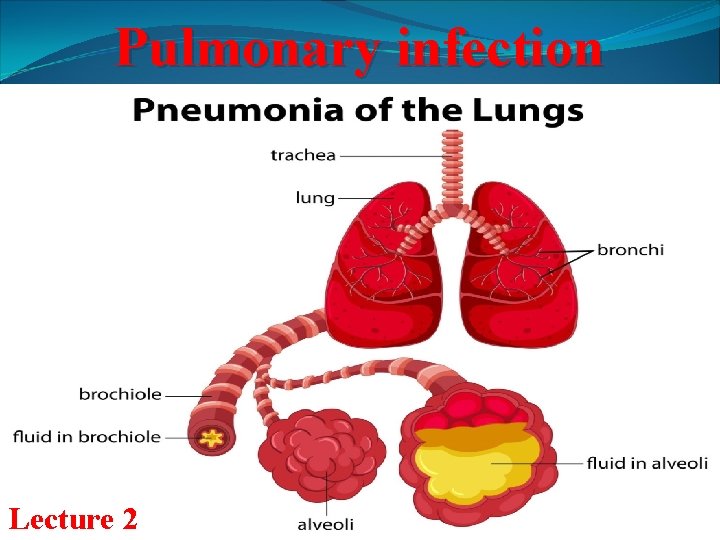
Pulmonary infections Pneumonia: Any infection in lung (bacterial, viral, fungal) that causes inflammation of air sacs (alveoli) which will be filled with fluid or pus (purulent material) Cough with pus, fever, chills, difficulty of breathing & may end with death. Source of infectious agents: (1) Air containing microbes. (2) Aspiration of nasopharyngeal flora during sleep. (3) Presence of other lung diseases making lung T. more vulnerable to virulent organisms.
v. Lung tissues remains sterile because of immune defense mechanisms in RS. v. Defects in immunity lead to increased incidence of infection with pyogenic bacteria. Factors interfere with immunity: A. Cigarette smoke: Compromises mucociliary clearance & macrophage activity. B. Alcohol: 1. Impairs cough & epiglottic reflexes, so increase risk of aspiration. 2. Interferes with mobilization & chemotaxis of neutrophil.
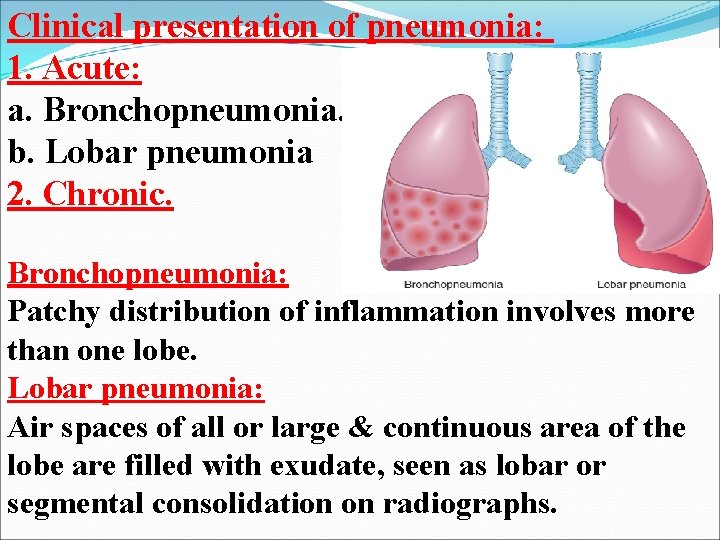
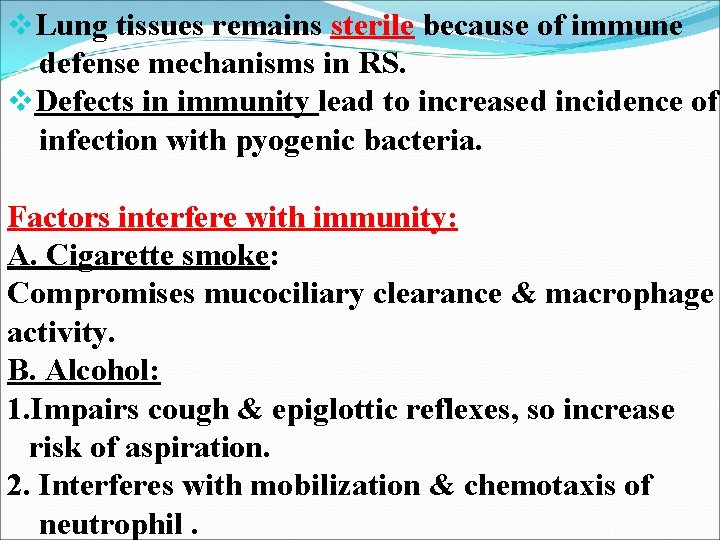
Clinical presentation of pneumonia: 1. Acute: a. Bronchopneumonia. b. Lobar pneumonia 2. Chronic. Bronchopneumonia: Patchy distribution of inflammation involves more than one lobe. Lobar pneumonia: Air spaces of all or large & continuous area of the lobe are filled with exudate, seen as lobar or segmental consolidation on radiographs.
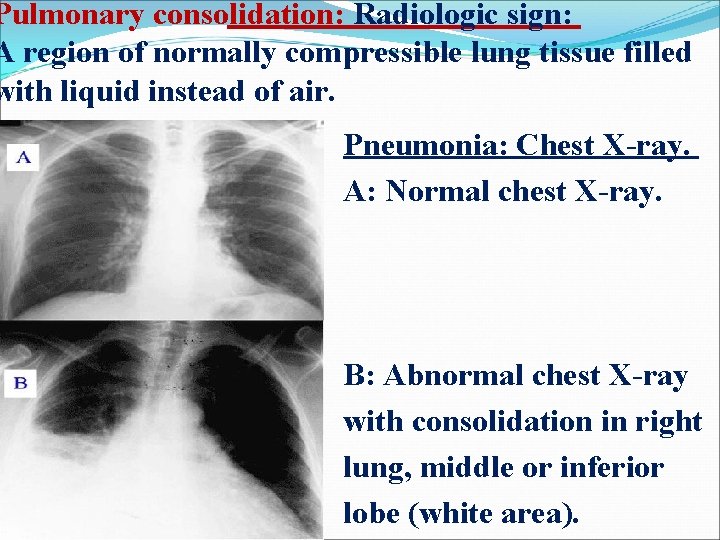
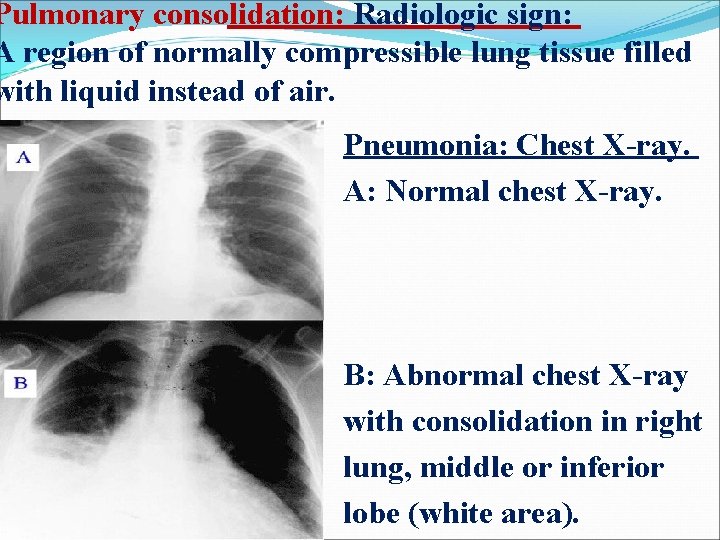
Pulmonary consolidation: Radiologic sign: A region of normally compressible lung tissue filled with liquid instead of air. Pneumonia: Chest X-ray. A: Normal chest X-ray. B: Abnormal chest X-ray with consolidation in right lung, middle or inferior lobe (white area).
Histologic picture of pneumonia: 1. Acute bacterial pneumonias: Fibrinopurulent intraalveolar exudate. 2. In viral & other atypical pneumonias: Mononuclear interstitial infiltrates. 3. In chronic pneumonias: Granulomas & cavitation.
Types of Pneumonia: 1. Community-Acquired Acute Pneumonia. 2. Community-Acquired Atypical Pneumonia. 3. Nosocomial pneumonia. (Hospital acquired) 4. Aspiration pneumonia. 5. Chronic pneumonia. 6. Necrotizing pneumonia & lung Abscess. 7. Pneumonia in immunocompromised host.
1. Community-Acquired Acute Pneumonia: v. Mostly bacterial in origin. v. Infection may follows viral upper RT infection. v. Abrupt onset. v. High fever. v. Shaking chills. v. Chest pain. v. Productive mucopurulent cough. v. Occasionally hemoptysis. (Coughing up of blood) v. Most common cause: v. Streptococcus pneumonia. (Pneumococcus)
Who have high risk of Streptococcus Pneumonia: (1) Patients with chronic diseases: CHF, COPD or diabetes. (2) Patients with acquired immune deficiency syndrome [AIDS]). (3) Those with decreased or absent splenic function: Ex. : Sickle cell disease or after splenectomy: Spleen: # Contains the largest collection of phagocytes. #Important organ for production of Abs against encapsulated bacteria.
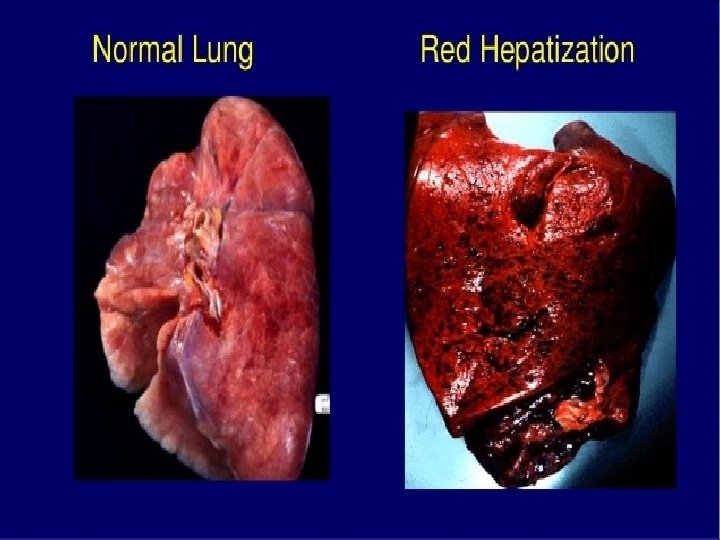
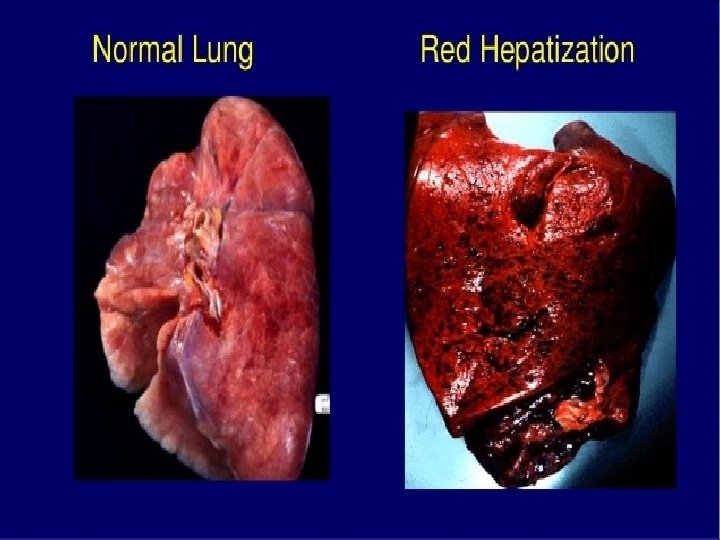
Morphology 1. Lobar pneumonia. 2. Bronchopneumonia: # More prevalent at extremes of age. Before antibiotics, typical progression of pneumonia include four stages: 1. Congestion. 2. Red hepatization. 3. Gray hepatization. 4. Resolution. Antibiotic therapy alter this typical progression.
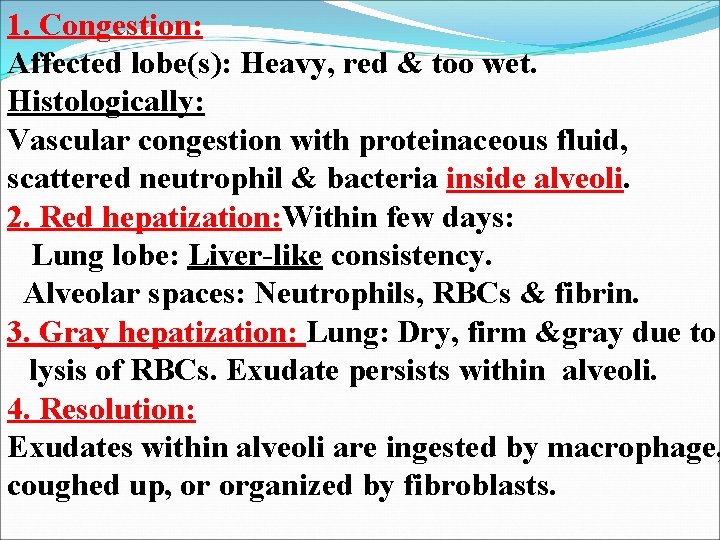
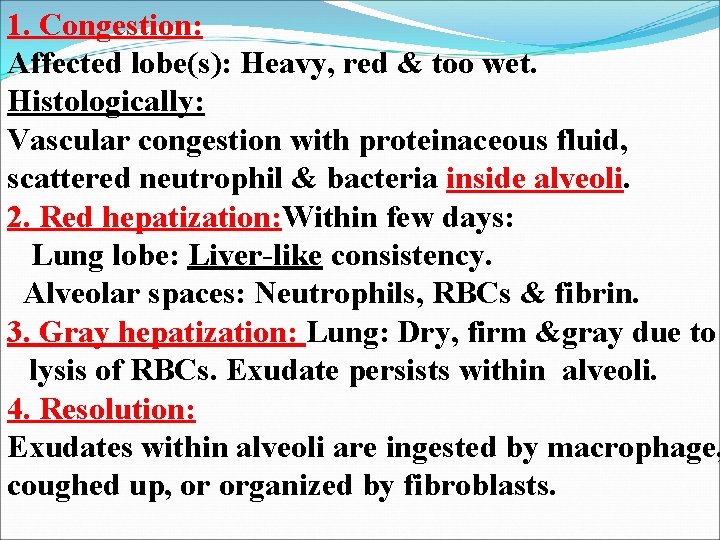
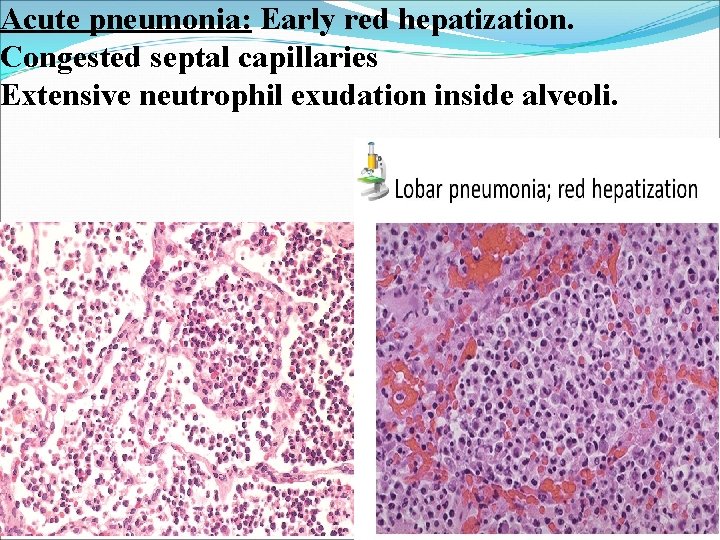
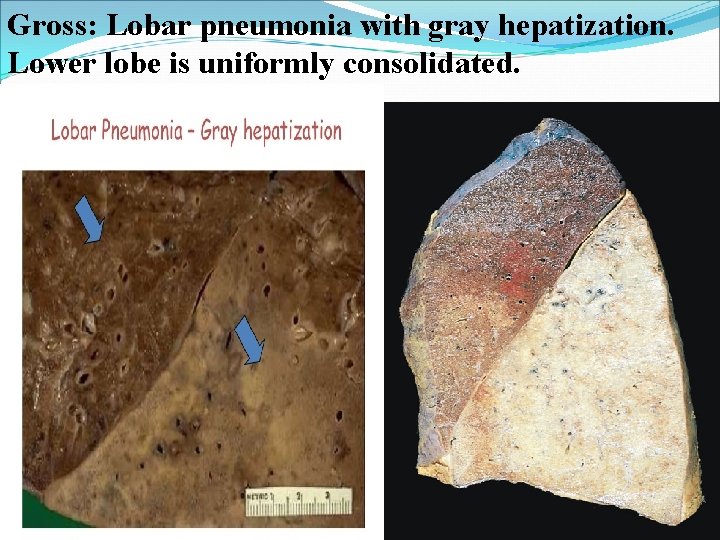
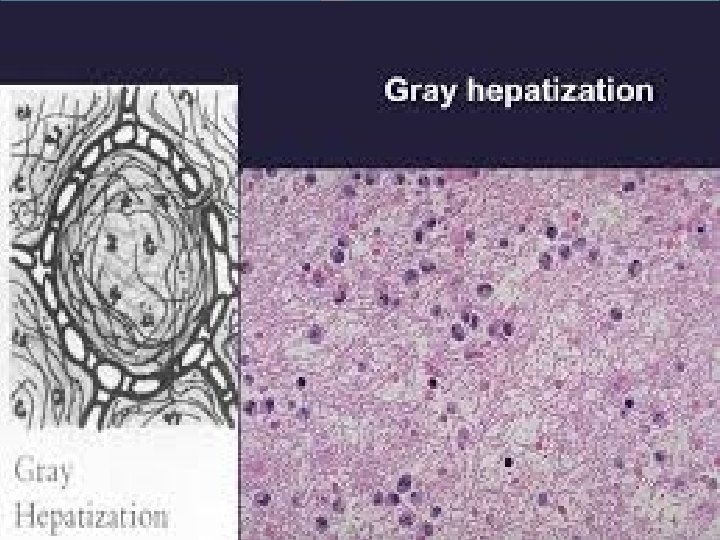
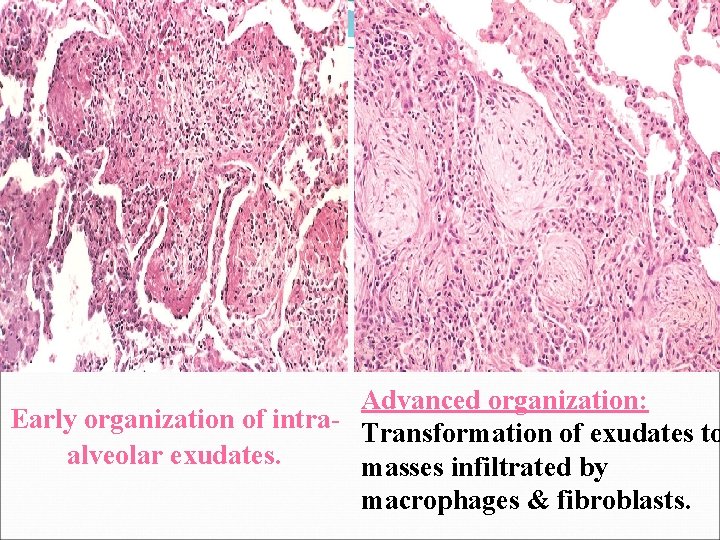
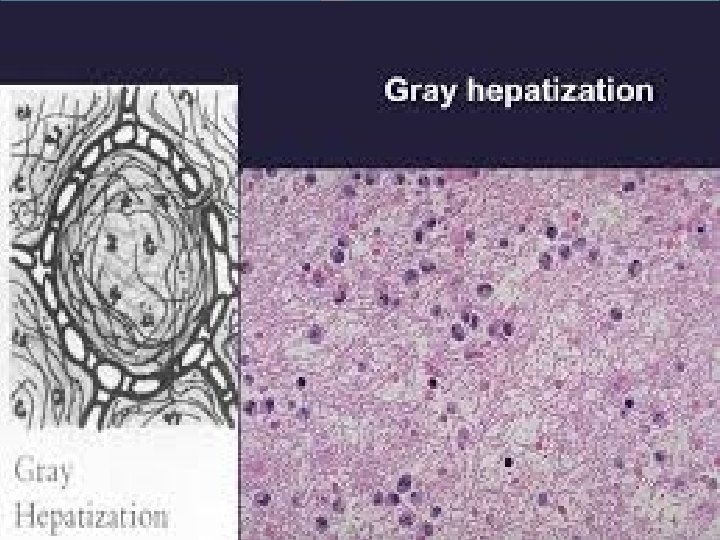
1. Congestion: Affected lobe(s): Heavy, red & too wet. Histologically: Vascular congestion with proteinaceous fluid, scattered neutrophil & bacteria inside alveoli. 2. Red hepatization: Within few days: Lung lobe: Liver-like consistency. Alveolar spaces: Neutrophils, RBCs & fibrin. 3. Gray hepatization: Lung: Dry, firm &gray due to lysis of RBCs. Exudate persists within alveoli. 4. Resolution: Exudates within alveoli are ingested by macrophage, coughed up, or organized by fibroblasts.
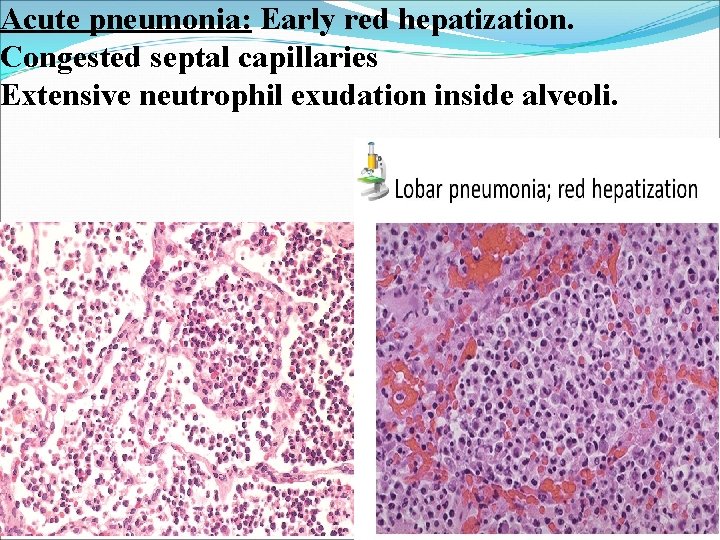
Acute pneumonia: Early red hepatization. Congested septal capillaries Extensive neutrophil exudation inside alveoli.
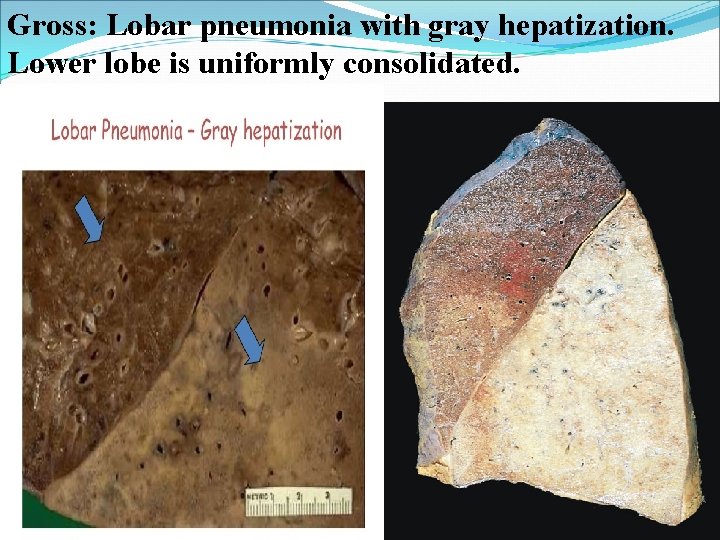
Gross: Lobar pneumonia with gray hepatization. Lower lobe is uniformly consolidated.
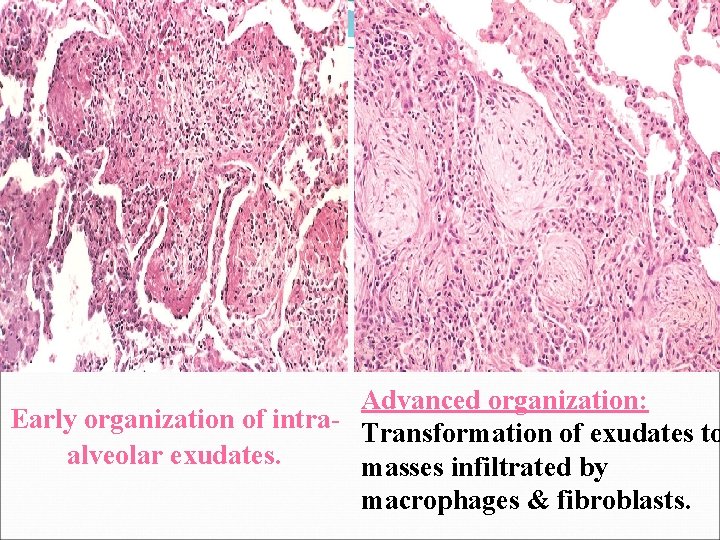
Advanced organization: Early organization of intra- Transformation of exudates to alveolar exudates. masses infiltrated by macrophages & fibroblasts.
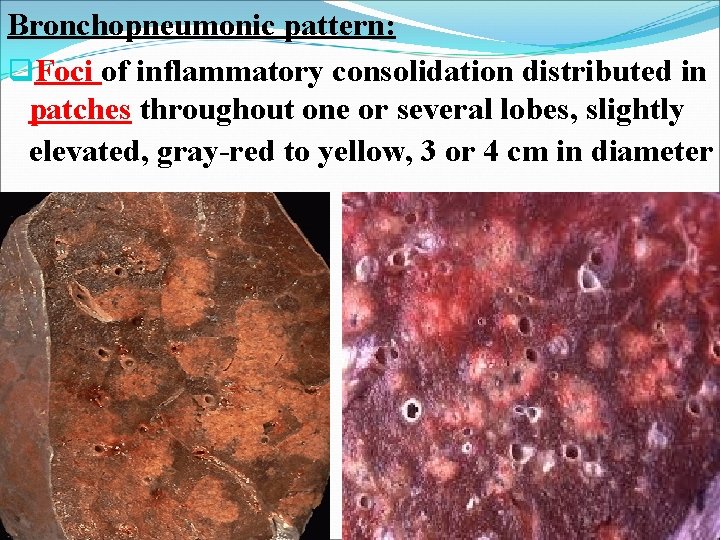
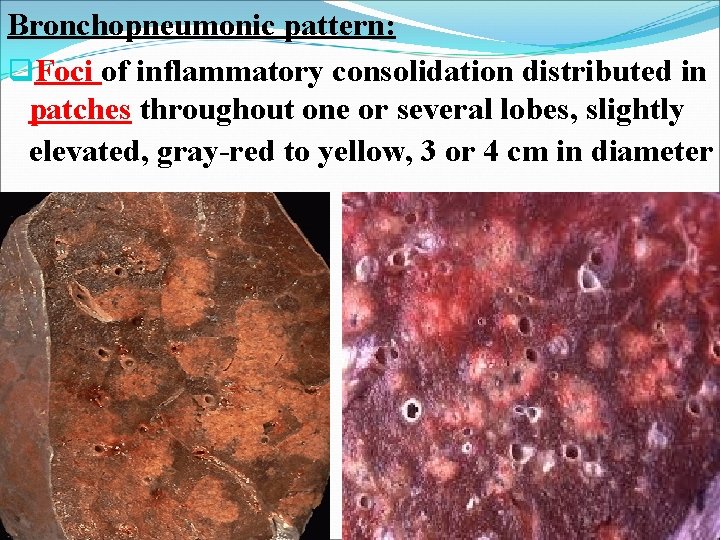
Bronchopneumonic pattern: q. Foci of inflammatory consolidation distributed in patches throughout one or several lobes, slightly elevated, gray-red to yellow, 3 or 4 cm in diameter
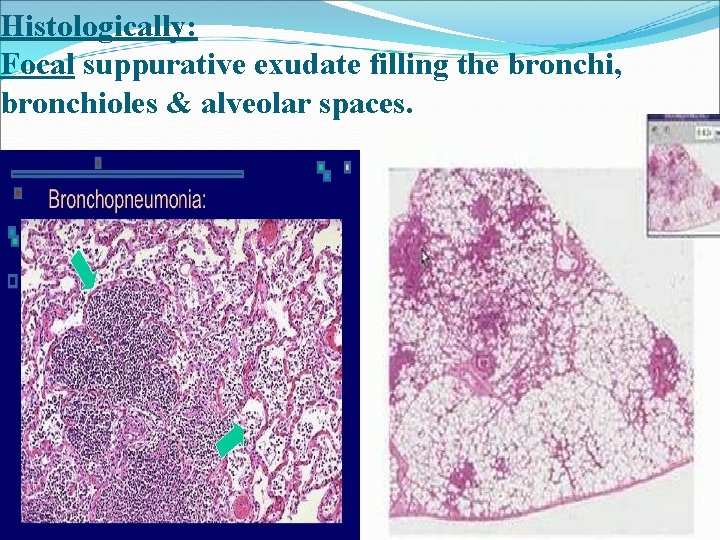
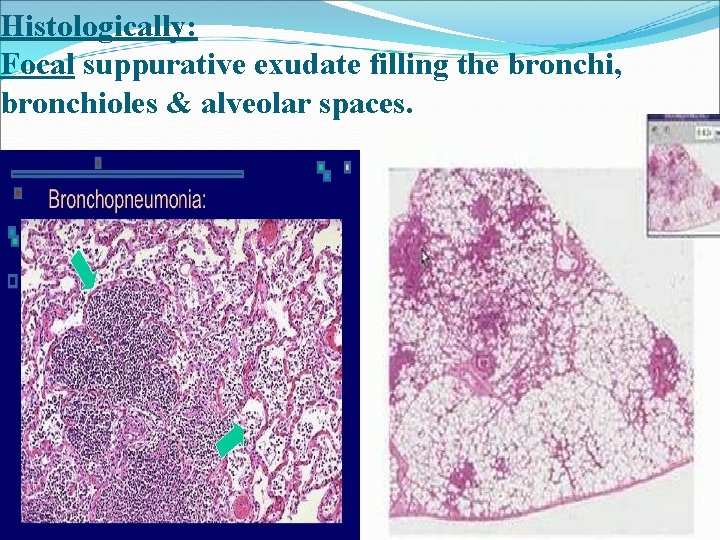
Histologically: Focal suppurative exudate filling the bronchi, bronchioles & alveolar spaces.
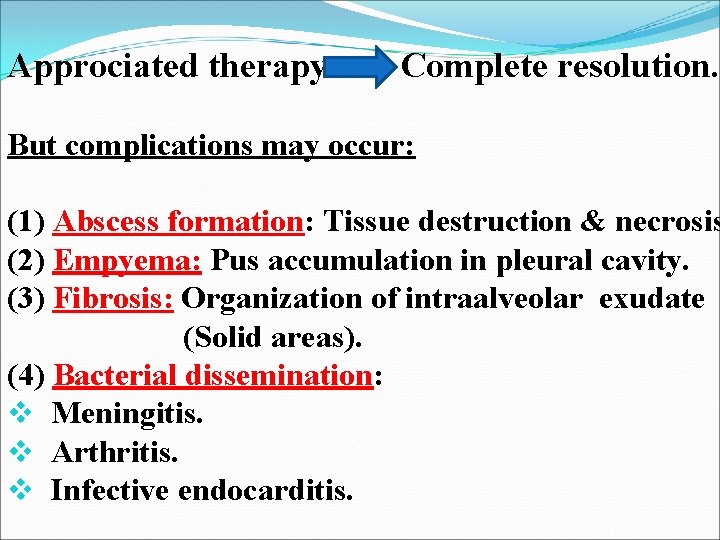
Approciated therapy Complete resolution. But complications may occur: (1) Abscess formation: Tissue destruction & necrosis (2) Empyema: Pus accumulation in pleural cavity. (3) Fibrosis: Organization of intraalveolar exudate (Solid areas). (4) Bacterial dissemination: v Meningitis. v Arthritis. v Infective endocarditis.
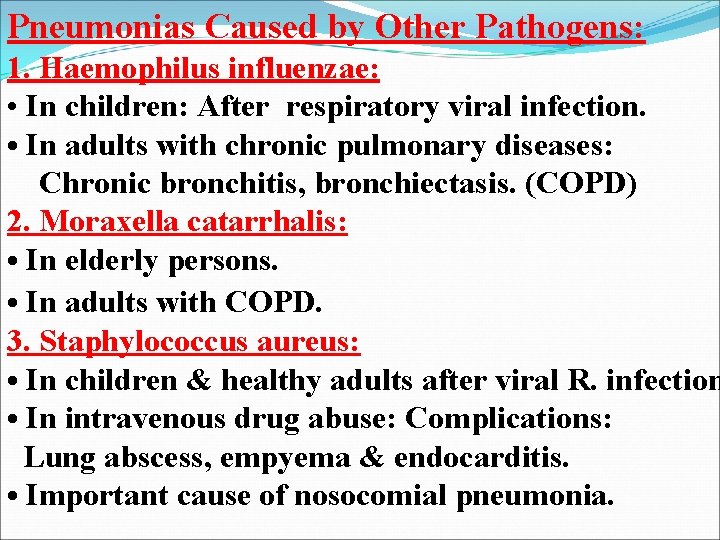
Pneumonias Caused by Other Pathogens: 1. Haemophilus influenzae: • In children: After respiratory viral infection. • In adults with chronic pulmonary diseases: Chronic bronchitis, bronchiectasis. (COPD) 2. Moraxella catarrhalis: • In elderly persons. • In adults with COPD. 3. Staphylococcus aureus: • In children & healthy adults after viral R. infection • In intravenous drug abuse: Complications: Lung abscess, empyema & endocarditis. • Important cause of nosocomial pneumonia.
4. Klebsiella pneumoniae: • In debilitated, malnourished & chronic alcoholics. • Characteristic: Thick & gelatinous sputum difficult to be coughed out. 5. Pseudomonas aeruginosa: • Cause nosocomial pneumonia in neutropenic perso (low neutrophile No. ), on chemotherapy, extensive burns & with mechanical ventilation. • Invade blood vessels: Spread extrapulmonary & may cause death. • Histology: Coagulative necrosis with organisms invading walls of necrotic blood vessels Pseudomonas vasculitis.
2. Community-Acquired Atypical Pneumonias: Acute febrile respiratory disease characterized by: Patchy inflammatory changes confined to alveolar septa & pulmonary interstitium. Why Atypical: Because there are: 1. Moderate amounts of sputum. 2. Absence of physical findings of consolidation. 3. Moderate elevation of white cell count. 4. Lack of alveolar exudates. Cause: 1. Mycoplasma pneumoniae (In children & young adults). 2. Viruses (Influenza). q Occur sporadically. q Epidemics in closed communities: Schools, military camps, prisons.
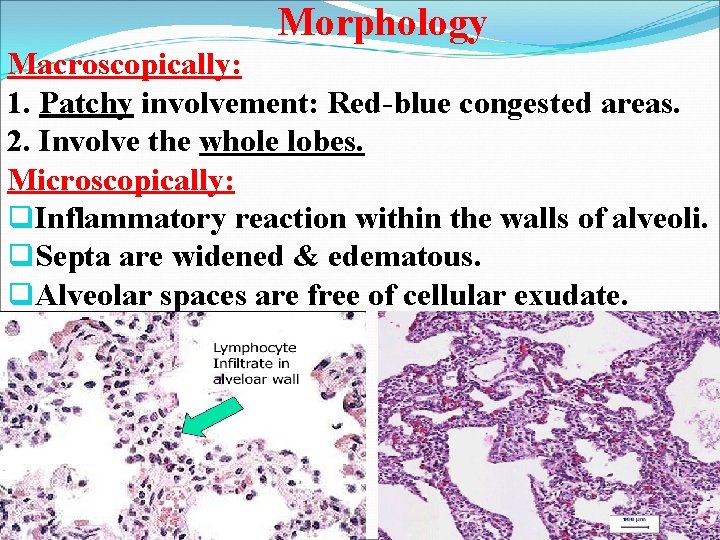
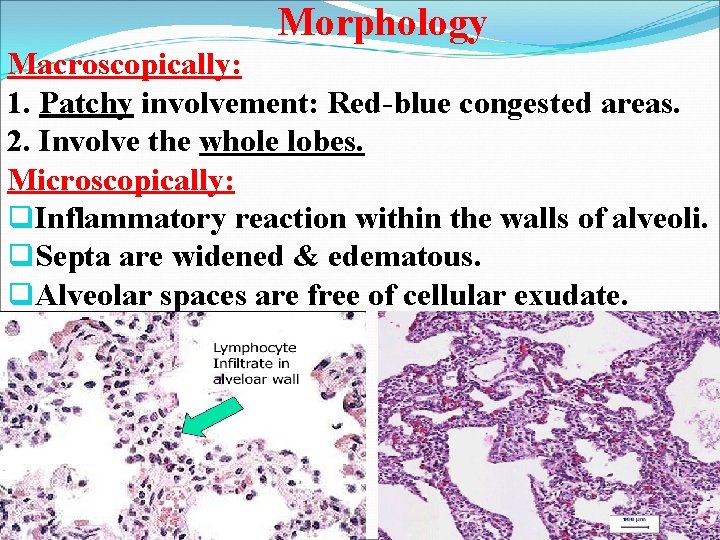
Morphology Macroscopically: 1. Patchy involvement: Red-blue congested areas. 2. Involve the whole lobes. Microscopically: q. Inflammatory reaction within the walls of alveoli. q. Septa are widened & edematous. q. Alveolar spaces are free of cellular exudate.
Clinical Features of primary atypical pneumonia: 1. Severe upper RT infection. 2. Undiagnosed chest cold. (Acute bronchitis). 3. Life-threatening infect. in immuno-compromised patients. Initial presentation: q. Acute nonspecific febrile illness characterized by fever, headache & malaise. Later: q. Cough with minimal sputum. q. Respiratory distress out of proportion to physical & radiographic findings, due to alveolocapillary block by edema & exudation.
3. Hospital-Acquired Pneumonias (Nosocomial): In: v. Hospitalized persons with severe underlying disease. v. Immunosuppressed patients. v. Patients on prolonged antibiotic regimens. v. Patients on mechanical ventilation. (Ventilator-associated pneumonia). Cause: 1. Gram-negative rods: Enterobacteriaceae & Pseudomonas spp. 2. S. aureus.
4. Aspiration Pneumonia: In: Debilitated patient with abnormal gag & swallowing reflexes that facilitate aspiration of gastric contents: q. Unconscious patient (after stroke). q. During repeated vomiting. Bacterial + Chemical irritation of gastric acid: Necrotizing &fulminant clinical course of pneumonia Death. Abscess formation is common complication in survived patients.
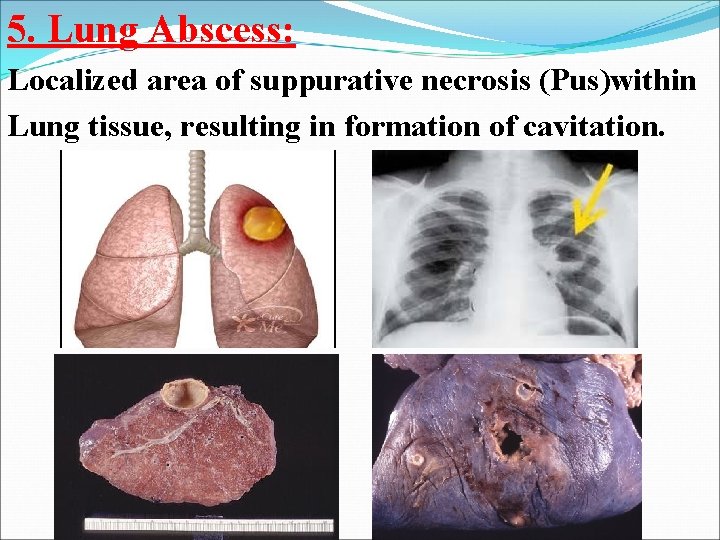
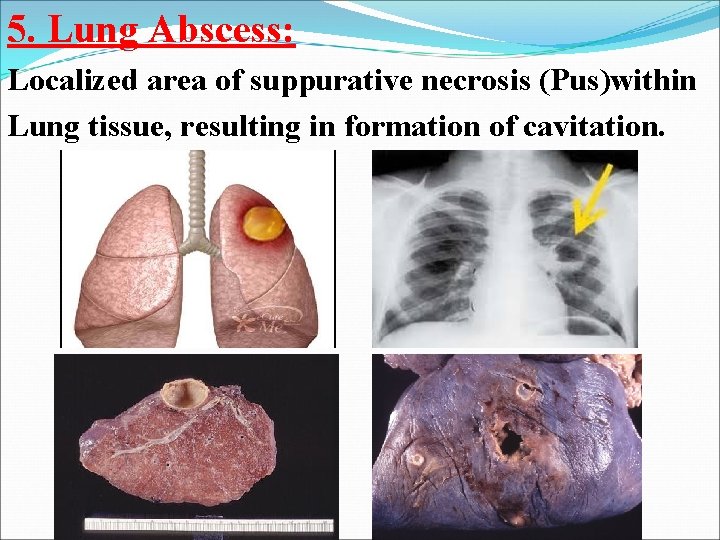
5. Lung Abscess: Localized area of suppurative necrosis (Pus)within Lung tissue, resulting in formation of cavitation.
Source of causative organism: • 1. Aspiration of infective material: # During oral surgery, anesthesia or coma. (Carious teeth, infected tonsils). # In debilitated p. with depressed cough reflexes. • 2. Aspiration of gastric contents, accompanied by infectious organisms from oropharynx. • 3. Complication of necrotizing pneumonias. • 4. Mycotic infections & bronchiectasis. • 5. Bronchial obstruction with carcinoma. • 6. Septic embolism: Hematogenous spread.
Morphology Few millimeters to large cavities, 5 -6 cm in diameter Localization & number of abscesses depend on their mode of development: 1. Abscesses resulting from aspiration of infective material: Common on right side & are single. 2. Abscesse develop after pneumonia or COPD: Multiple, basal & diffusely scattered. 3. Septic emboli & abscesses from hematogenous route are multiple & affect any region of lungs.
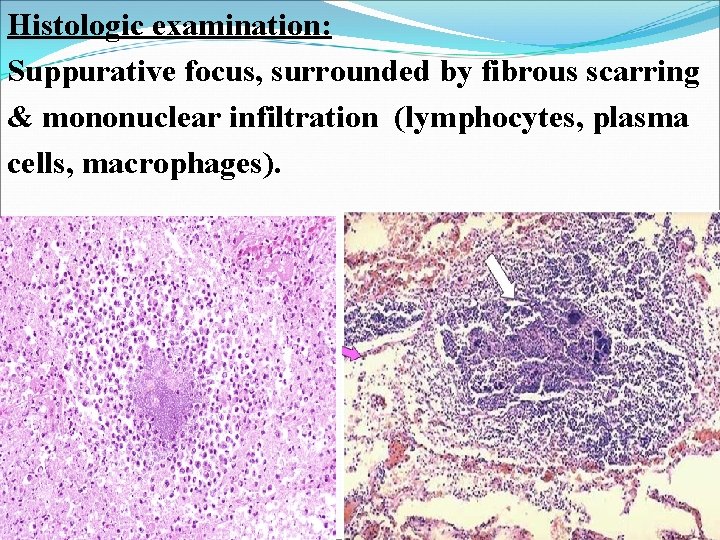
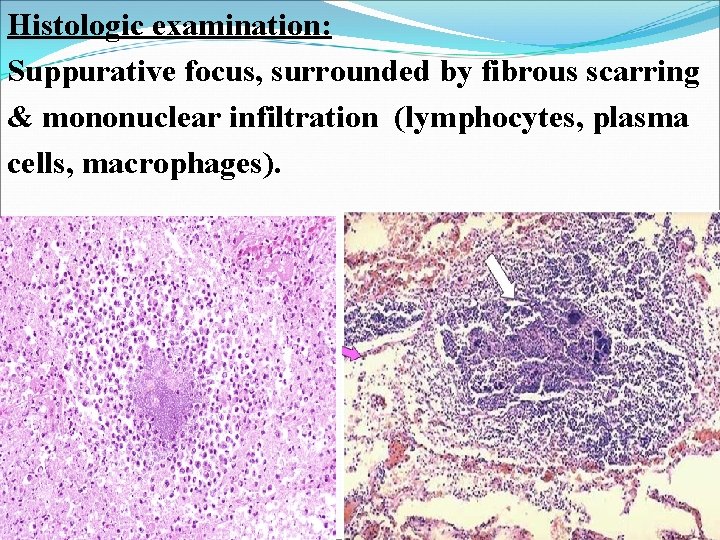
Histologic examination: Suppurative focus, surrounded by fibrous scarring & mononuclear infiltration (lymphocytes, plasma cells, macrophages).
Clinical Features of lung abscess: § Prominent cough with foul-smelling, purulent(pus) or sanguineous sputum (bloody). (Hemoptysis ) § Fever, malaise, clubbing of fingers (edema due to decrease O 2), weight loss & anemia. § Infective abscesses occur in 10 -15% of patients with bronchogenic carcinoma. § Thus lung abscess in old person should suspect carcinoma. § Treatment: Antibiotic therapy & surgical drainage if needed. § Mortality rate is 10%.
THANK YOU