Pulmonary Gas Exchange Acute Respiratory Insufficiency vs Respiratory




- Slides: 35
Pulmonary Gas Exchange Acute Respiratory Insufficiency vs. Respiratory Failure -M. Liebzeit MSN, RN, CPN
Defining: Respiratory insufficiency Chronic respiratory insufficiency acceptable levels of gas exchange are maintained normal p. H elevated Pa. CO 2 elevated HCO 3 to compensate normal to low Pa. O 2
Defining: Respiratory insufficiency Signs of impending failure tachypnea tachycardia increased use of accessory muscles nasal flaring abnormal chest wall movements labored breathing decreasing Sp. O 2
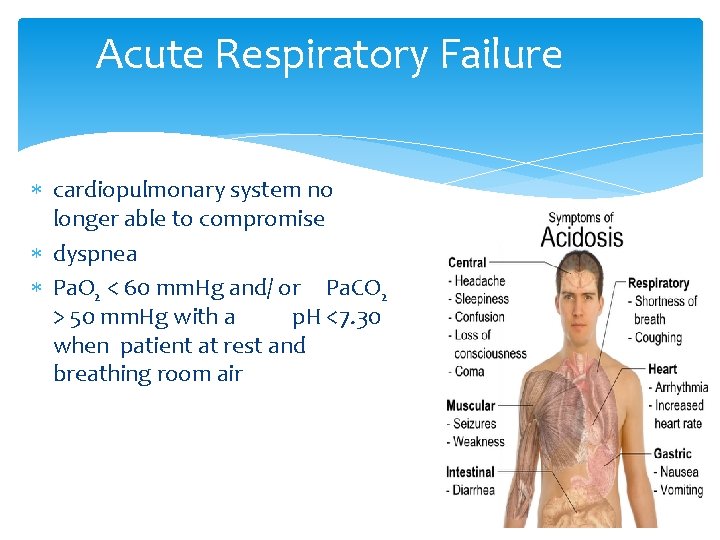
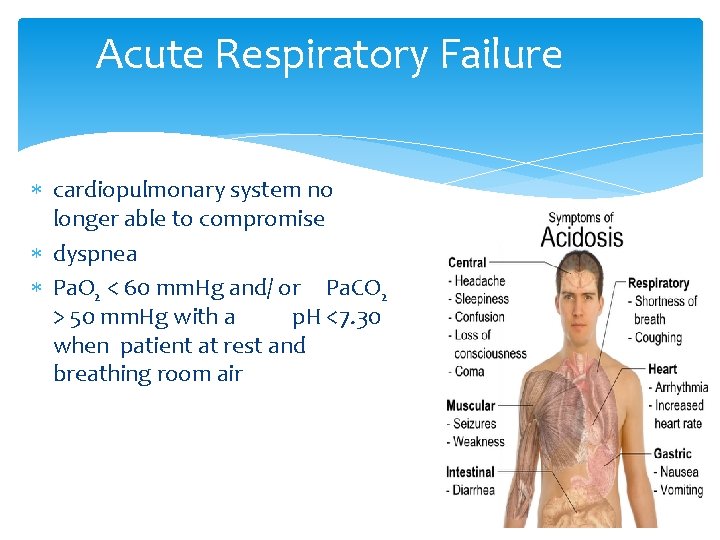
Acute Respiratory Failure cardiopulmonary system no longer able to compromise dyspnea Pa. O 2 < 60 mm. Hg and/ or Pa. CO 2 > 50 mm. Hg with a p. H <7. 30 when patient at rest and breathing room air
Components of ARF: Oxygenation - failure of arterial blood oxygenation hypoxemia low inspired oxygen pressure V/Q mismatch shunting diffusion impairment
Components of ARF: Ventilation Alveolar hypoventilation - CO 2 accumulates in blood “CO 2 narcosis” Pa. CO 2 increases and eventually Pa. O 2 will decrease Increased dead space ventilation – dead space – volume of inspired air that does not participate in gas exchange

p. 290
Acute Respiratory Distress Syndrome (ARDS)
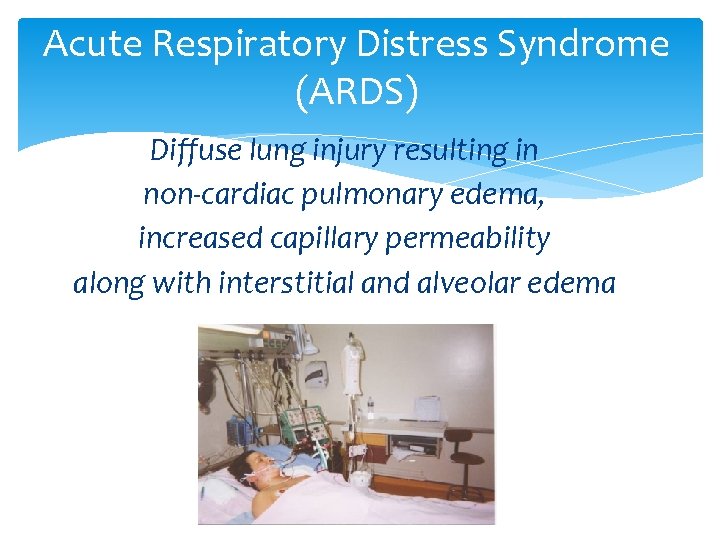
Acute Respiratory Distress Syndrome (ARDS) Diffuse lung injury resulting in non-cardiac pulmonary edema, increased capillary permeability along with interstitial and alveolar edema
Identifying ARDS clinical history physical findings refractory hypoxemia diminished pulmonary compliance CXR normal PAWP
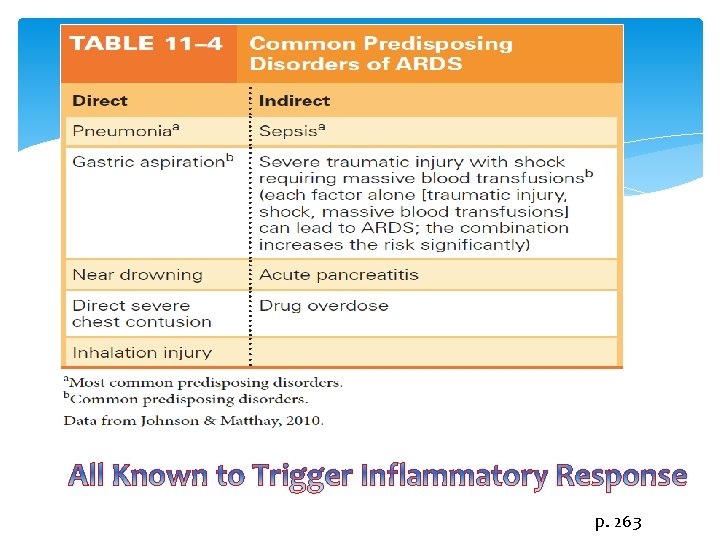
Etiology of ARDS Systemic inflammatory response Diffuse lung injury
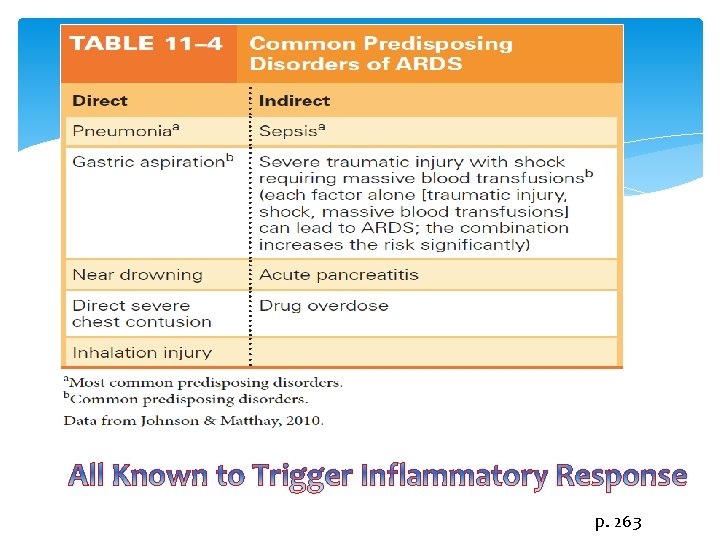
p. 263
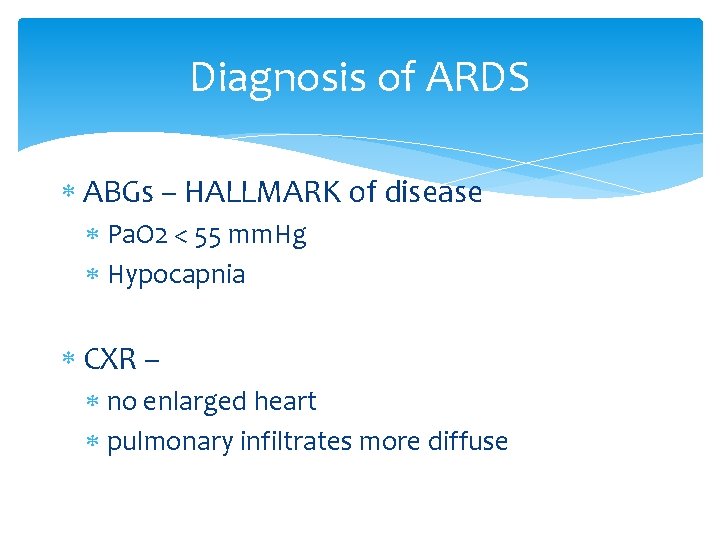
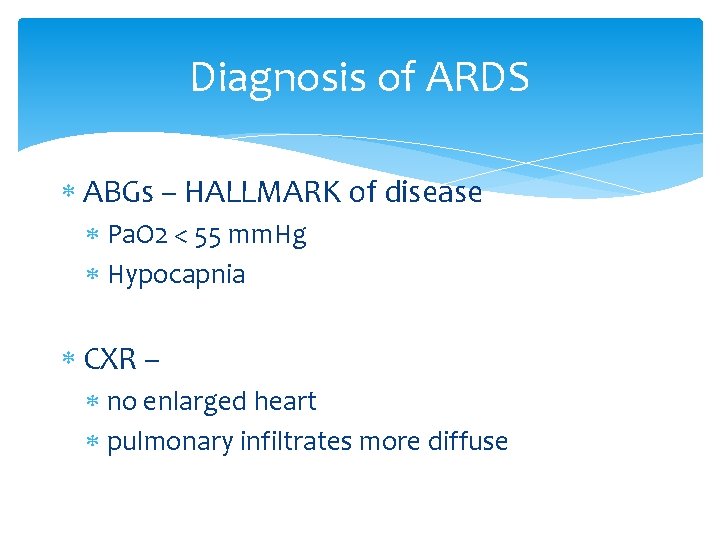
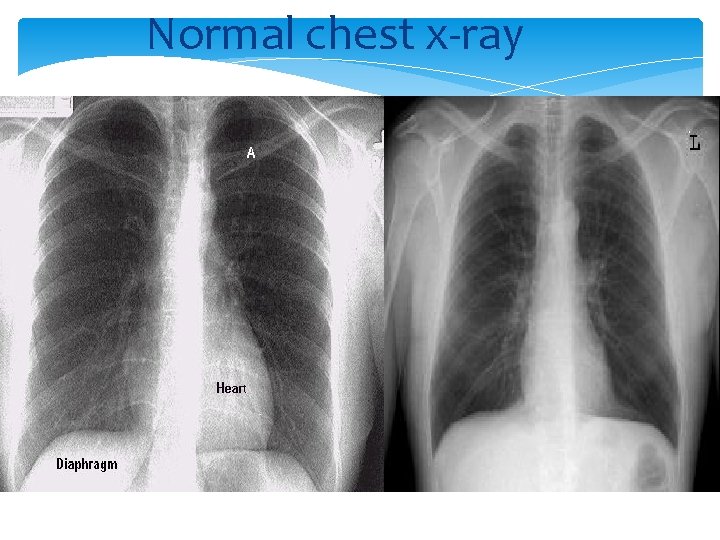
Diagnosis of ARDS ABGs – HALLMARK of disease Pa. O 2 < 55 mm. Hg Hypocapnia CXR – no enlarged heart pulmonary infiltrates more diffuse
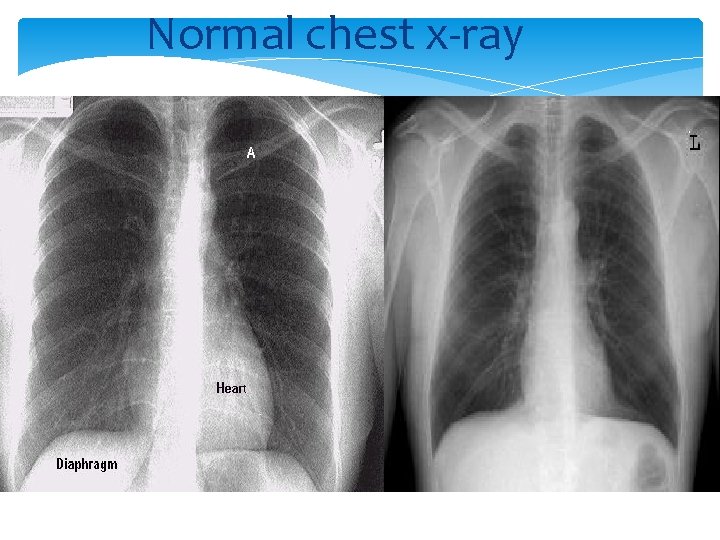
Normal chest x-ray

Diagnosis of ARDS (cont) Oxygenation status – P/F ratio 200 -300, 100 -200, <100 Pulmonary artery wedge pressure – normal or low 18 or less suggestive of ARDS; higher with CHF Broncho-alveolar lavage – protein rich / inflammatory cells Brain natriuretic peptide (BNP) Chest x-ray T 11 -5, p 292
Pathogenesis of ARDS Diffuse inflammatory injury to alveolar-capillary membrane Disruption in alveolar epithelium permits fluid and plasma proteins to shift into alveoli resulting non-hydrostatic pulmonary edema injury to type II cells increased surface wall tension atelectasis V/Q mismatching / shunting
Pathogenesis of ARDS (cont) Invasion of lung tissue by neutrophils Activate inflammatory by-products Disruption in pulmonary capillary endothelium plasma proteins and fluid shift to pulmonary interstitial spaces pulmonary edema flooded alveoli
Clinical Presentation of ARDS Patient Typically onset 24 -48 hours Starts off as a respiratory alkalosis. Then becomes refractory to oxygen administration.
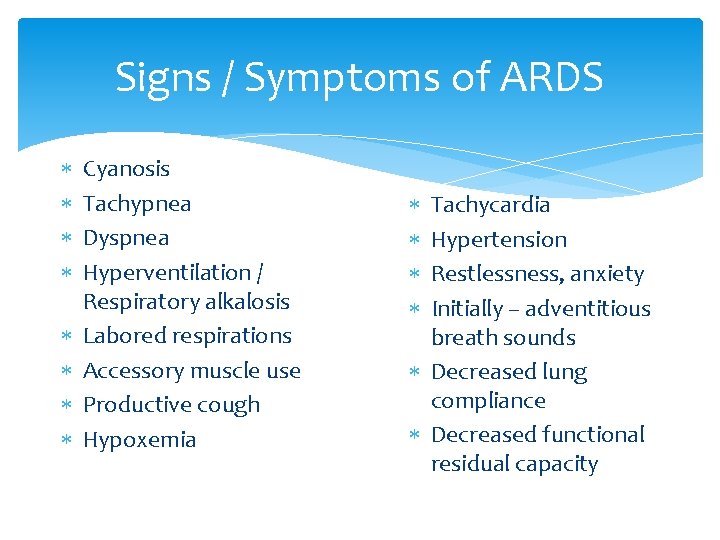
Signs / Symptoms of ARDS Cyanosis Tachypnea Dyspnea Hyperventilation / Respiratory alkalosis Labored respirations Accessory muscle use Productive cough Hypoxemia Tachycardia Hypertension Restlessness, anxiety Initially – adventitious breath sounds Decreased lung compliance Decreased functional residual capacity
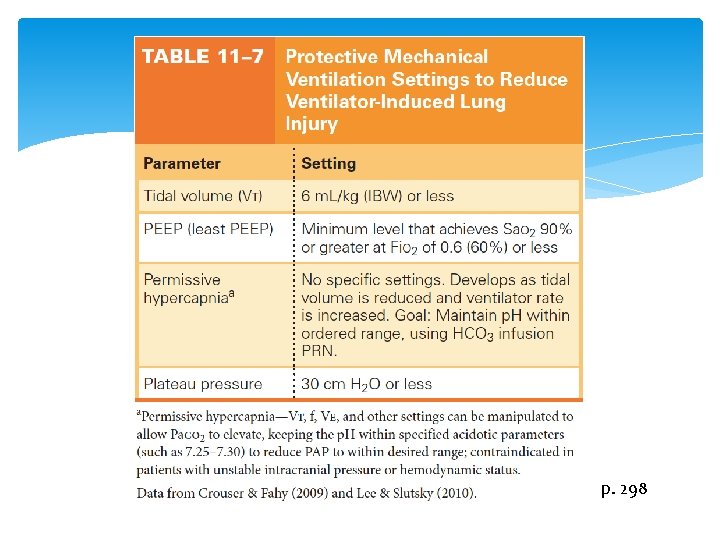
Management Overall Oxygenation Supportive therapy / prevent complications Mechanical ventilation Tidal volume PEEP Reduce Fi. O 2
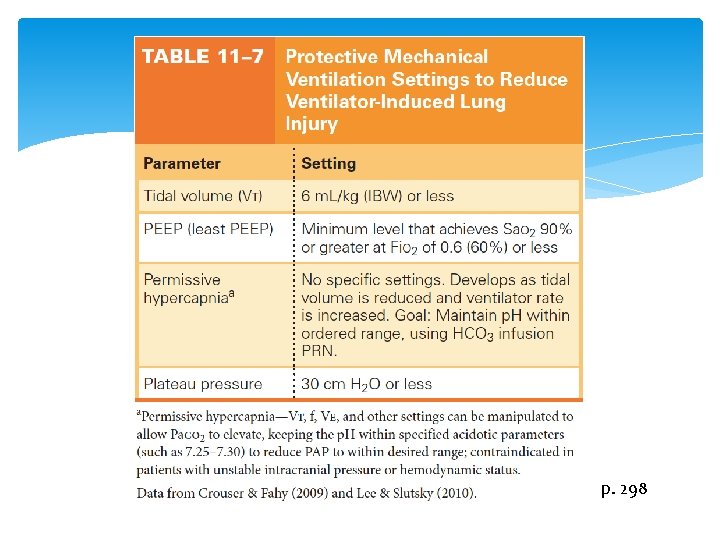
p. 298

Figure 10– 3: Roto. Rest bed. A form of CLRT therapy. Roto. Rest Delta TM Advanced Kinetic Therapy TM (System); Courtesy of KCI Licensing, Inc. 2008.

Reproduced with grateful recognition to: Barbara Mc. Lean, MN, RN, CCNP, CCNS, FCCM
Management Overall Fluid management Inotropic / vasoactive support “Normalize hemoglobin”
Management Overall Pharmacologic therapy – Corticosteroids – controversial Inhaled nitric oxide Surfactant replacement Partial liquid ventilation – perfluorocarbon Sedation / paralysis / pain management Antibiotics Anti-pyretics
Management Overall Nutritional support Psychological support
Prognosis of ARDS Mortality rate : 30 – 40% Quality of life with recovery Lung repair Physical, psychological, emotional impairment Muscle weakness Pain Depression Anxiety Cognitive changes
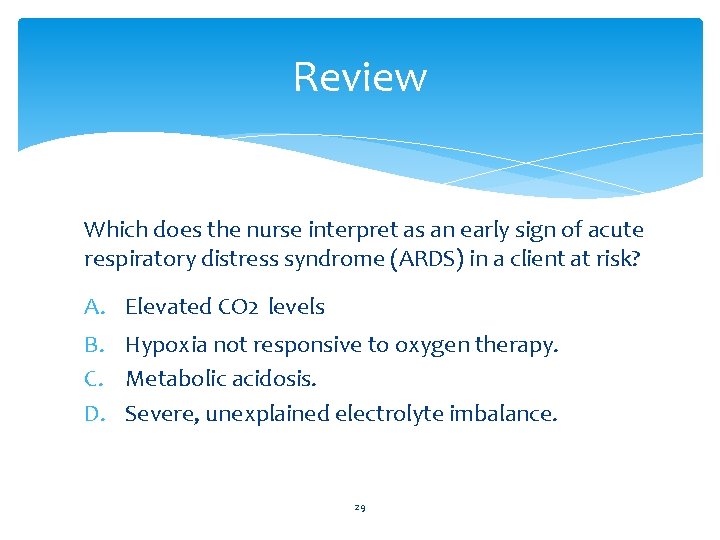
Review Which does the nurse interpret as an early sign of acute respiratory distress syndrome (ARDS) in a client at risk? A. Elevated CO 2 levels B. Hypoxia not responsive to oxygen therapy. C. Metabolic acidosis. D. Severe, unexplained electrolyte imbalance. 29
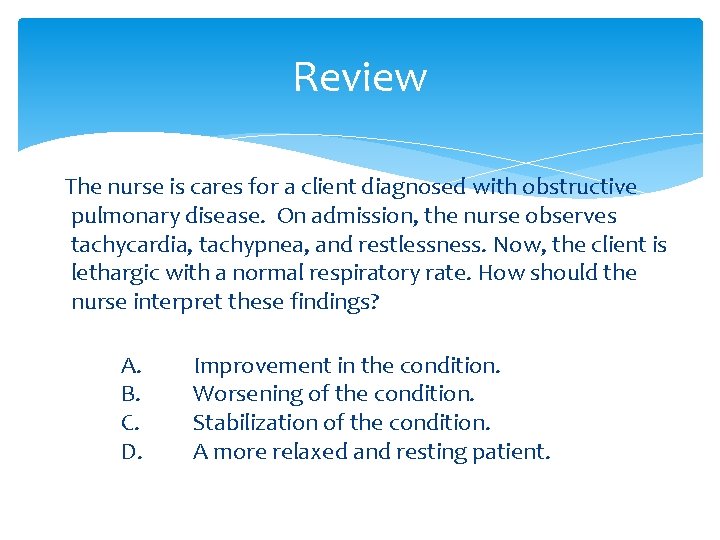
Review The nurse is cares for a client diagnosed with obstructive pulmonary disease. On admission, the nurse observes tachycardia, tachypnea, and restlessness. Now, the client is lethargic with a normal respiratory rate. How should the nurse interpret these findings? A. B. C. D. Improvement in the condition. Worsening of the condition. Stabilization of the condition. A more relaxed and resting patient.
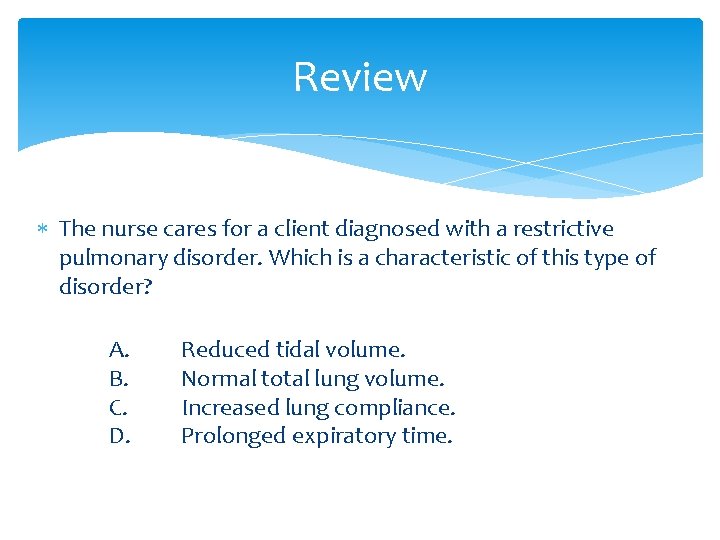
Review The nurse cares for a client diagnosed with a restrictive pulmonary disorder. Which is a characteristic of this type of disorder? A. B. C. D. Reduced tidal volume. Normal total lung volume. Increased lung compliance. Prolonged expiratory time.
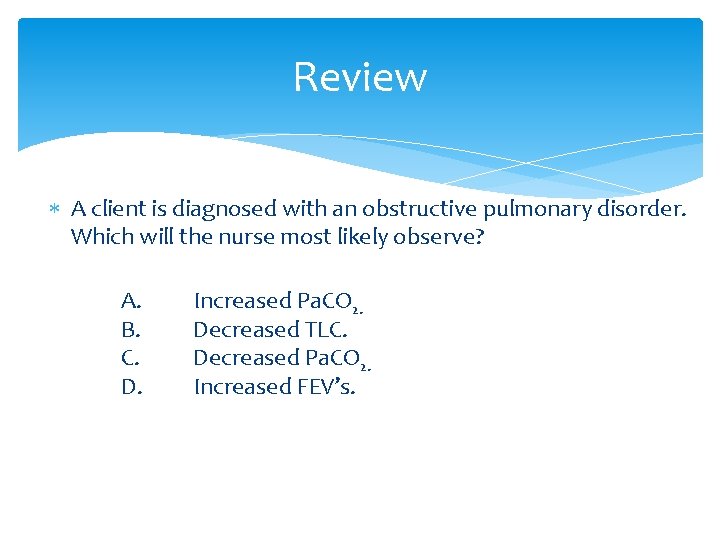
Review A client is diagnosed with an obstructive pulmonary disorder. Which will the nurse most likely observe? A. B. C. D. Increased Pa. CO 2. Decreased TLC. Decreased Pa. CO 2. Increased FEV’s.
Review How does the pulmonary edema of ALI / ARDS differ from pulmonary edema of CHF? A. In CHF, PAWP is less than 18. B. In CHF, bronchoalveolar lavage fluid is rich in proteins. C. In ARDS, heart enlargement is typically noted on CXR. D. In ARDS, bronchial fluid contains inflammatory cells.
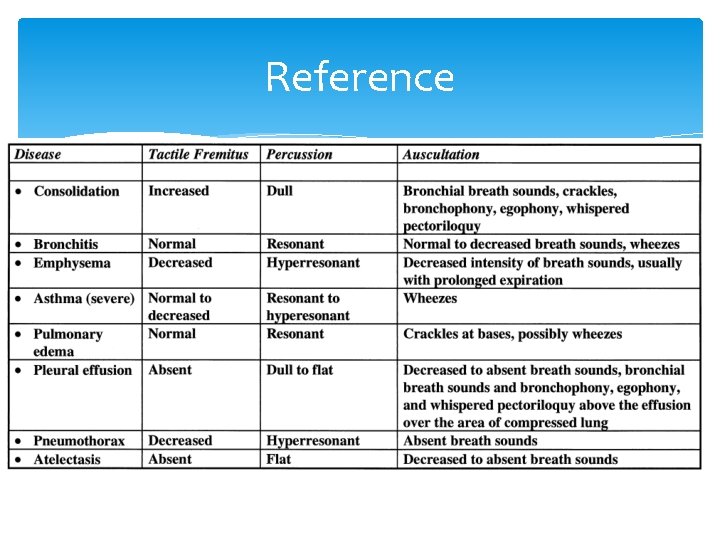
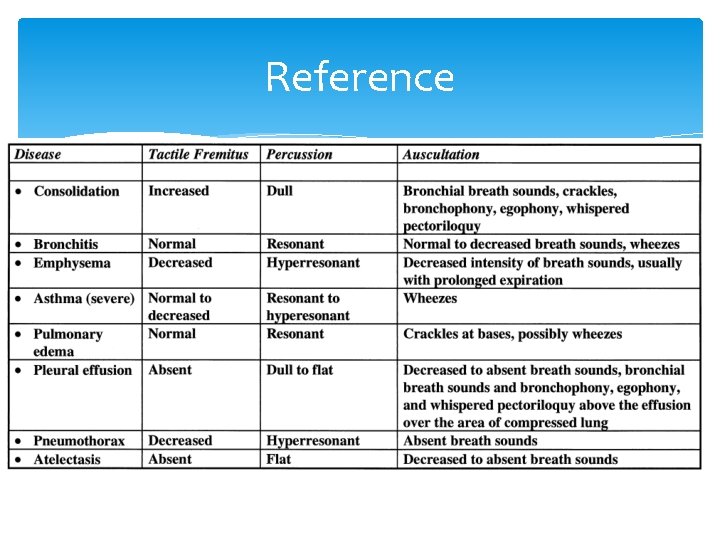
Reference