Pulmonary Function Tests Presenter Dr Sofia Patial Moderator

- Slides: 57
Pulmonary Function Tests Presenter: Dr. Sofia Patial Moderator: Dr. Gian Chauhan
GOALS To predict presence of pulmonary dysfunction Ø To know the functional nature of disease. Ø To assess the severity of disease Ø To assess the progression of disease Ø To assess the response to treatment Ø Medicolegal- to assess lung impairment as a result of occupational hazard. Ø To identify patients at perioperative risk of pulmonary complications Ø
INDICATIONS OF PFT IN PAC TISI GUIDELINES FOR PREOPERATIVE SPIROMETRY Ø Age > 70 yrs. Ø Morbid obesity Ø Thoracic surgery Ø Upper abdominal surgery Ø Smoking history and cough Ø Any pulmonary disease
�ACP GUIDELINES FOR PREOPERATIVE SPIROMETRY Ø Lung resection Ø H/o smoking, dyspnoea Ø Cardiac surgery Ø Upper abdominal surgery Ø Lower abdominal surgery Ø Uncharacterized pulmonary disease (defined as history of pulmonary Disease or symptoms and no PFT in last 60 days)
Contraindications: Ø Hemoptysis of unknown origin Ø Pneumothorax Ø Unstable cardiovascular status, recent MI, pulmonary embolism Ø Thoracic, abdominal or cerebral aneurysms Ø Recent eye surgery (cataract) Ø Nausea, vomiting Ø Recent surgery on thorax or abdomen
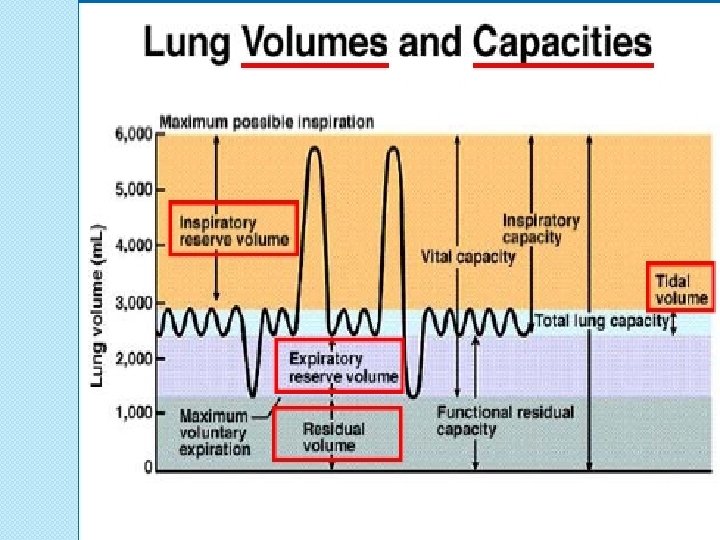
Components of PFT’s: Ø Spirometry for measuring airway mechanics (dynamic flow rates of gases) Ø Measuring lung volumes and capacities Ø Measuring diffusion capacity of lung
Spirometry
PREREQUISITIES Ø Prior explanation to the patient Ø Not to smoke /inhale short acting bronchodilators 4 hrs prior or oral aminophylline and long acting bronchodilator 12 hrs prior. Ø Remove any tight clothings/ waist belt/ dentures Ø Pt. Seated comfortably Ø If obese, child < 12 yrs- standing Ø Nose clip to close nostrils. Ø 3 acceptable tracings taken & largest value is used.
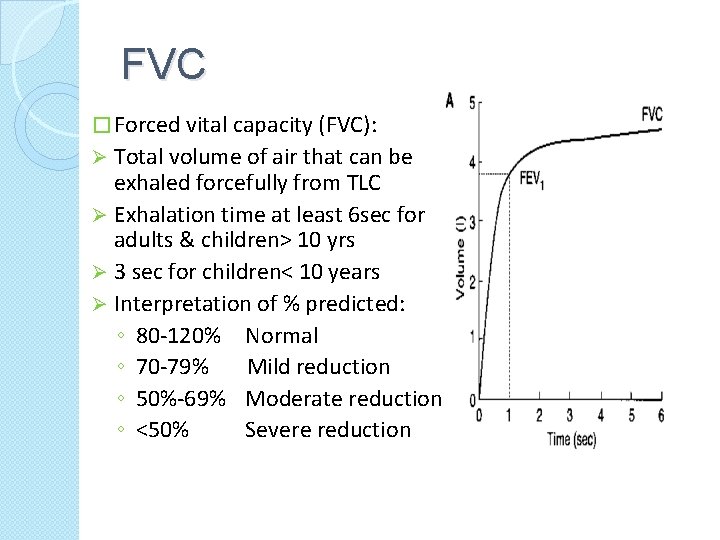
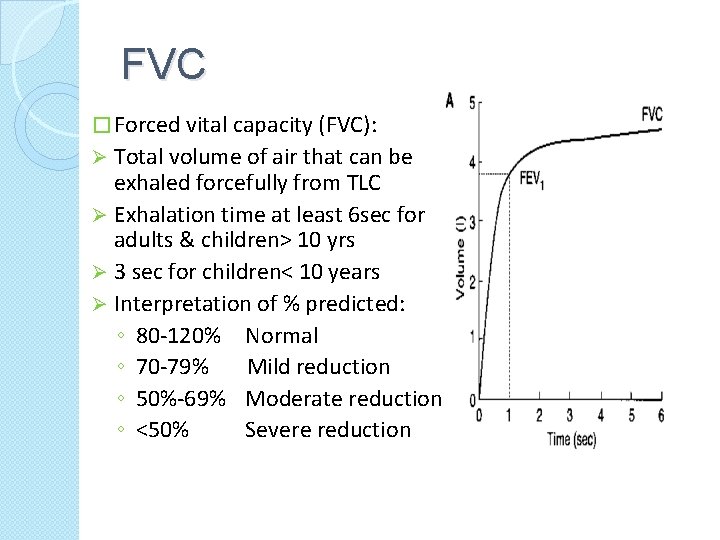
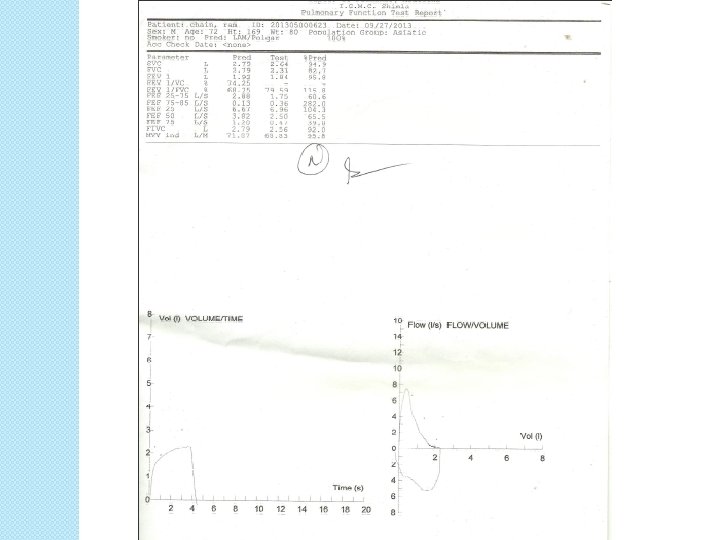
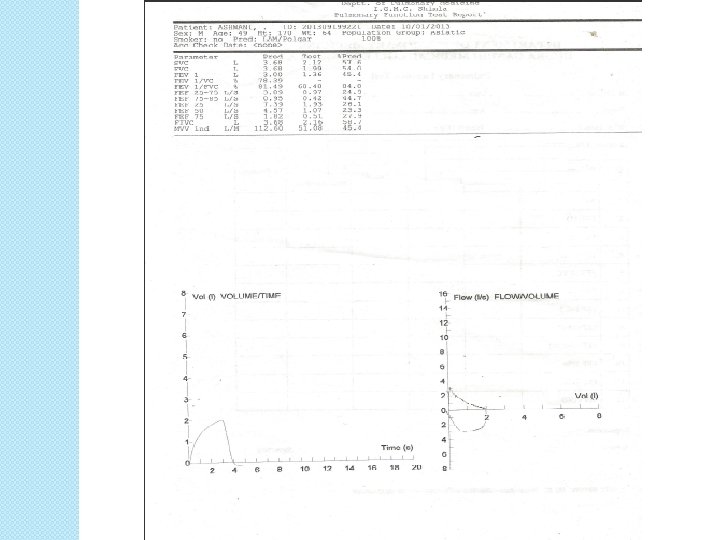
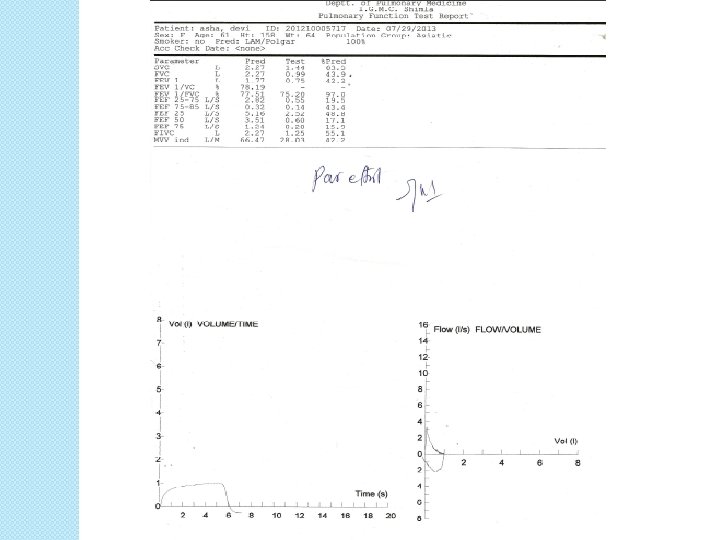
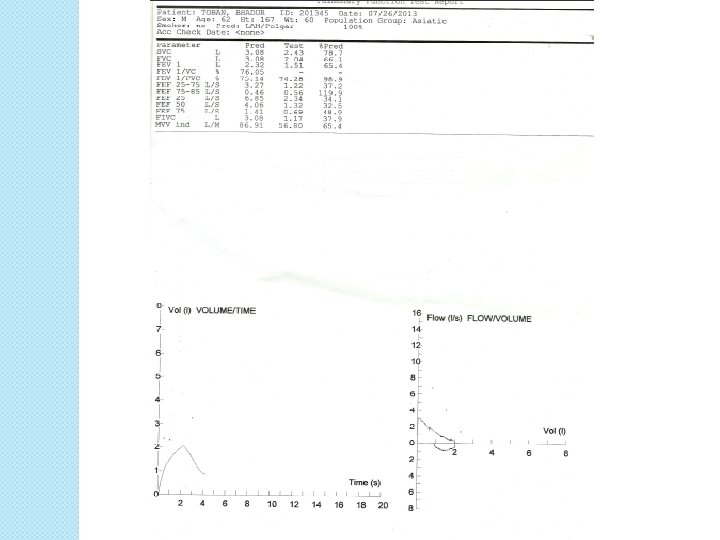
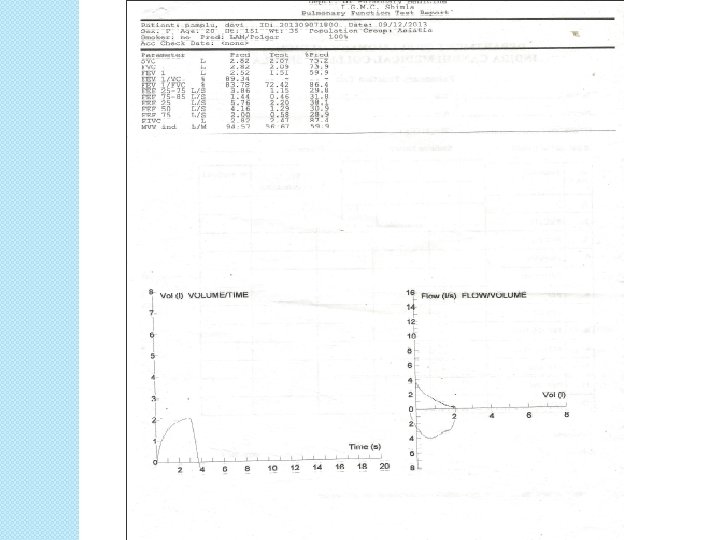
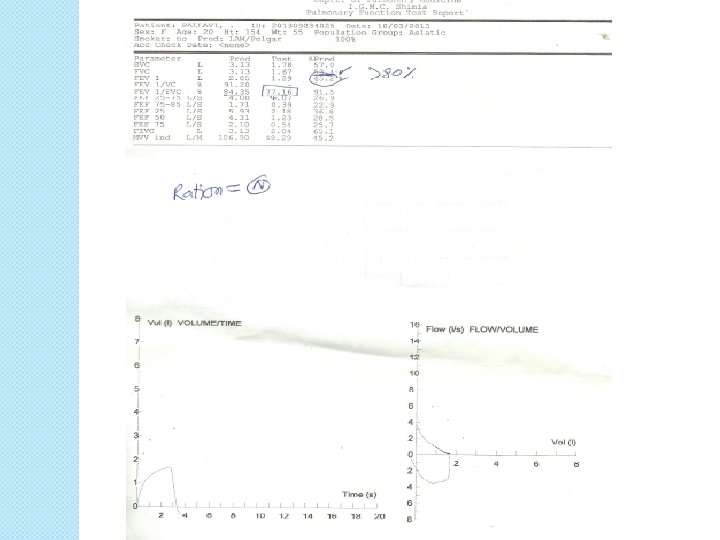
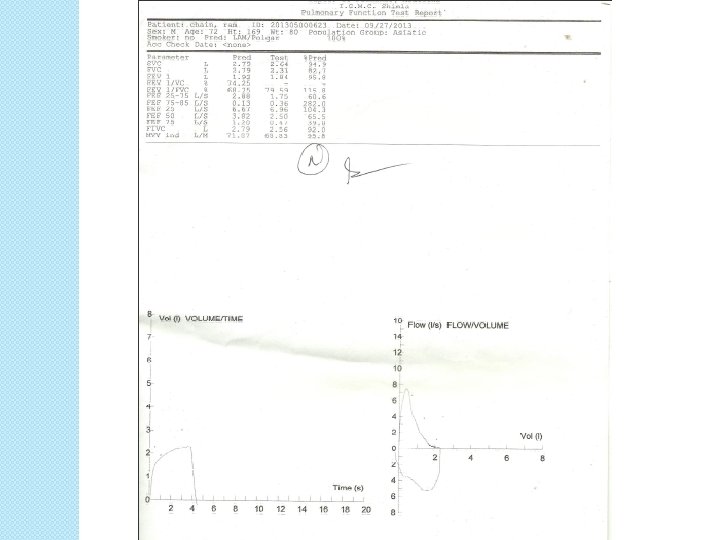
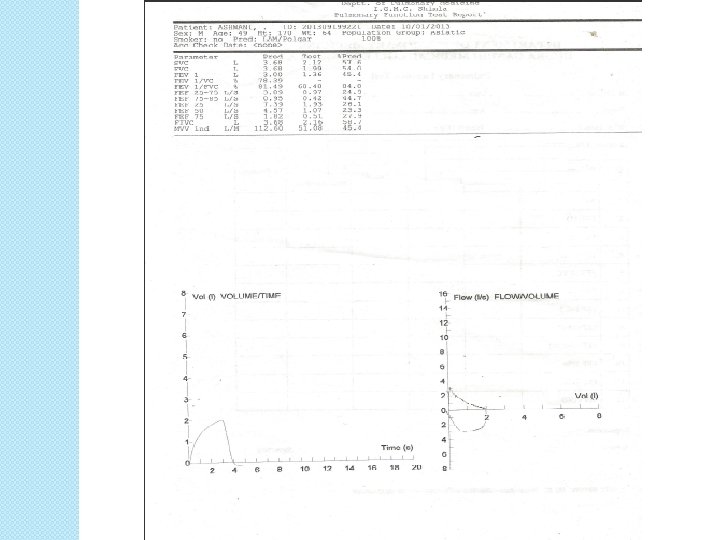
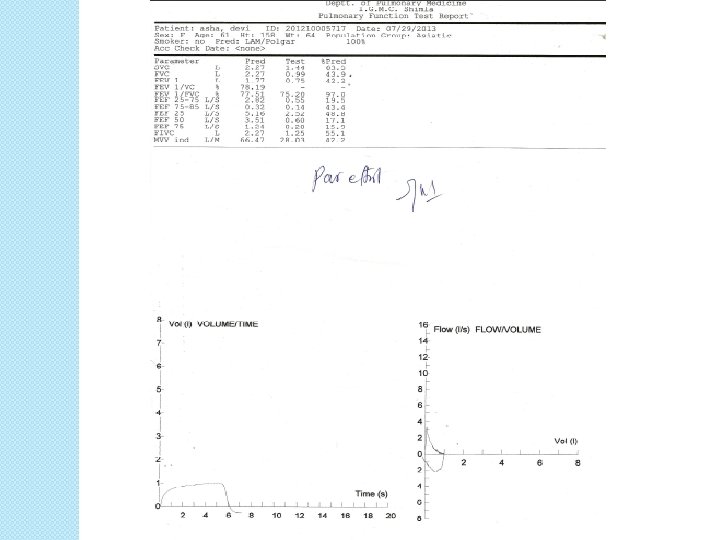
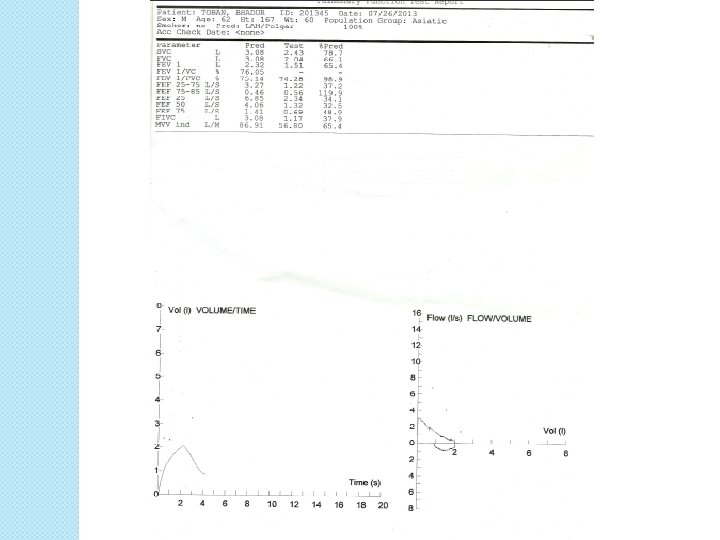
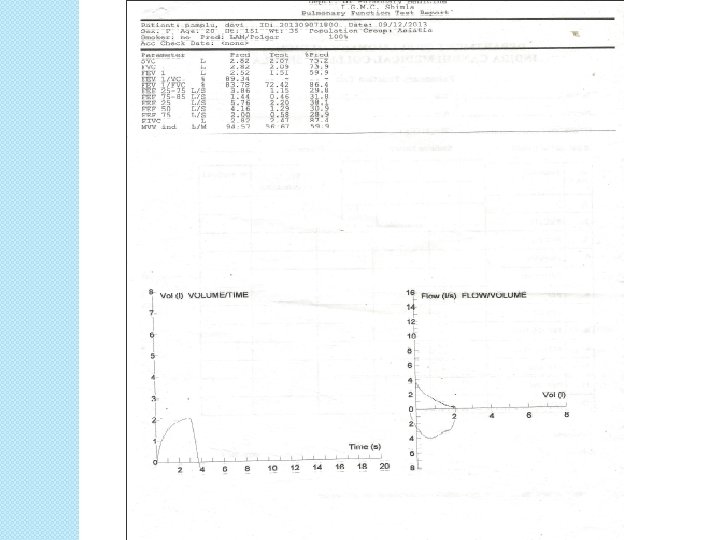
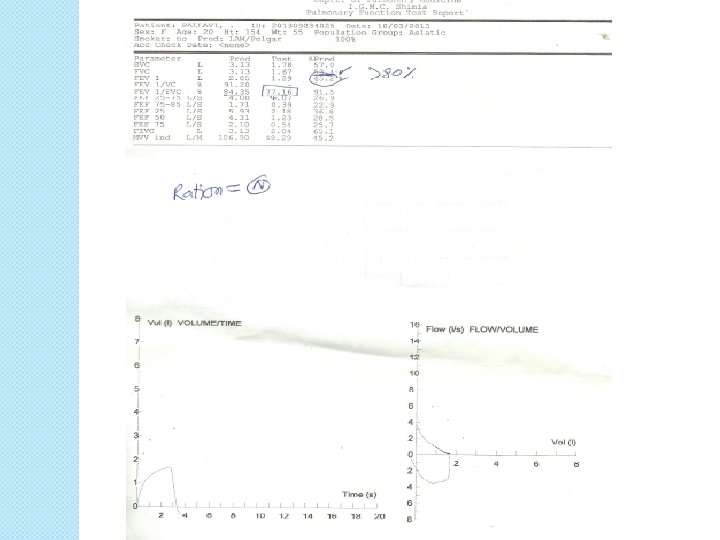
FVC � Forced vital capacity (FVC): Total volume of air that can be exhaled forcefully from TLC Ø Exhalation time at least 6 sec for adults & children> 10 yrs Ø 3 sec for children< 10 years Ø Interpretation of % predicted: ◦ 80 -120% Normal ◦ 70 -79% Mild reduction ◦ 50%-69% Moderate reduction ◦ <50% Severe reduction Ø
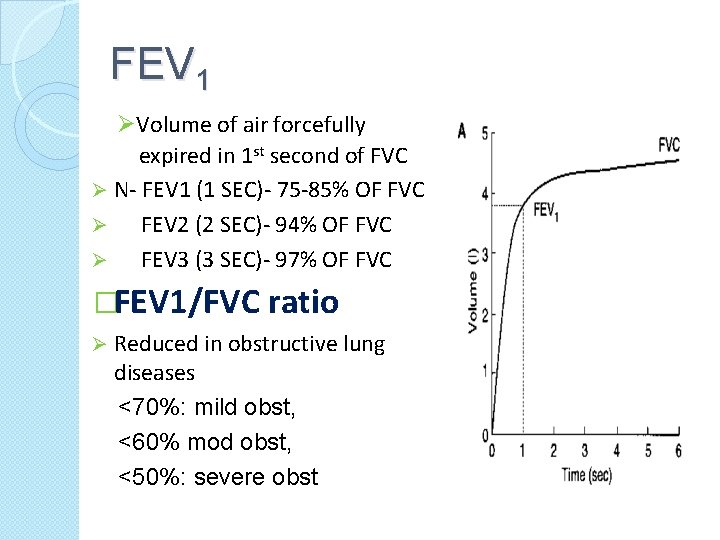
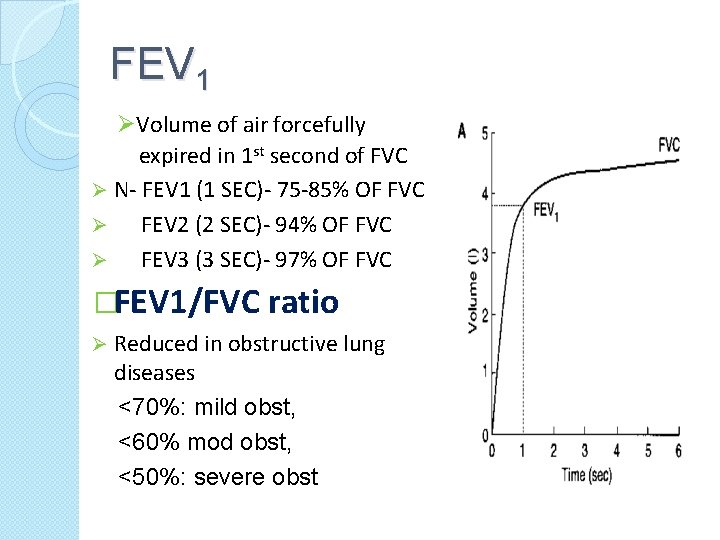
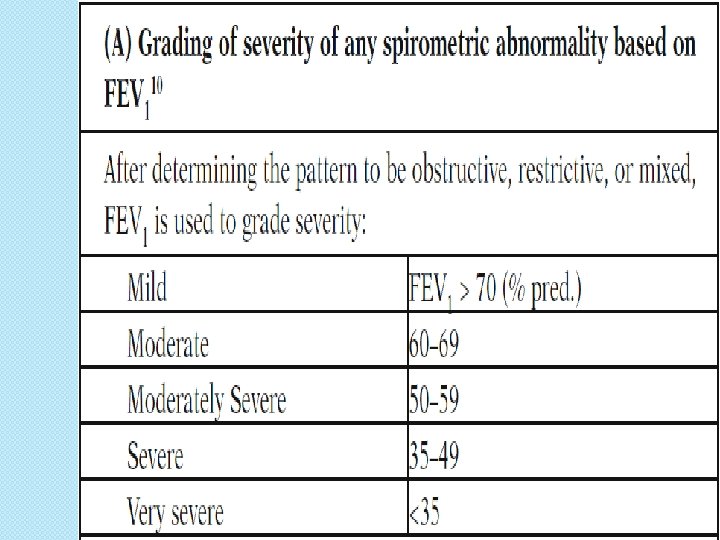
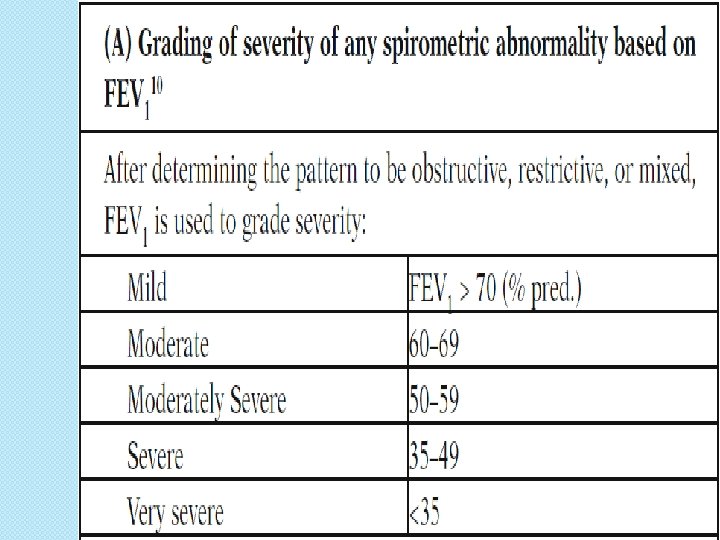
FEV 1 ØVolume of air forcefully expired in 1 st second of FVC Ø N- FEV 1 (1 SEC)- 75 -85% OF FVC Ø FEV 2 (2 SEC)- 94% OF FVC Ø FEV 3 (3 SEC)- 97% OF FVC �FEV 1/FVC ratio Ø Reduced in obstructive lung diseases <70%: mild obst, <60% mod obst, <50%: severe obst
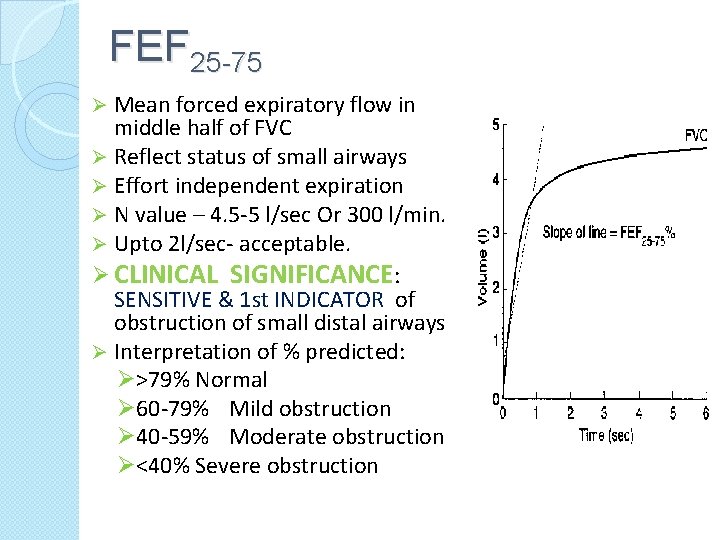
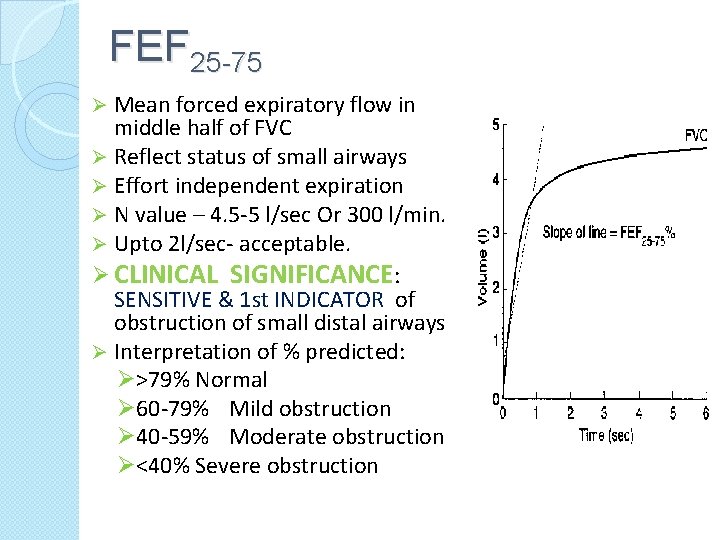
FEF 25 -75 Mean forced expiratory flow in middle half of FVC Ø Reflect status of small airways Ø Effort independent expiration Ø N value – 4. 5 -5 l/sec Or 300 l/min. Ø Upto 2 l/sec- acceptable. Ø CLINICAL SIGNIFICANCE: SENSITIVE & 1 st INDICATOR of obstruction of small distal airways Ø Interpretation of % predicted: Ø>79% Normal Ø 60 -79% Mild obstruction Ø 40 -59% Moderate obstruction Ø<40% Severe obstruction Ø
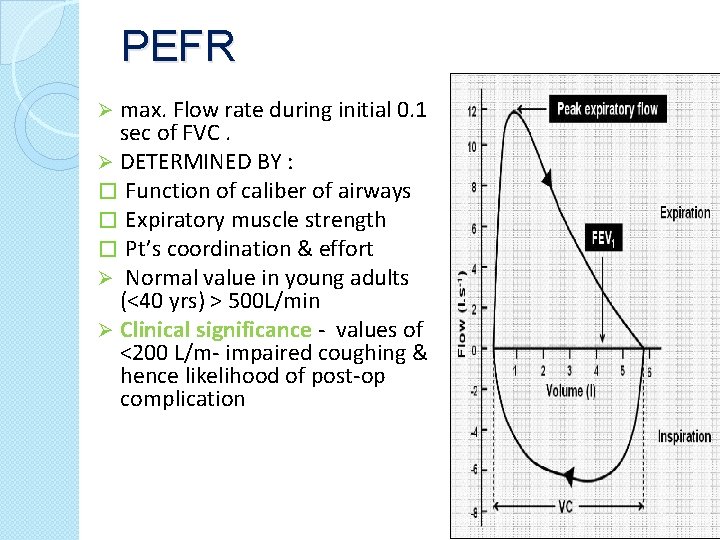
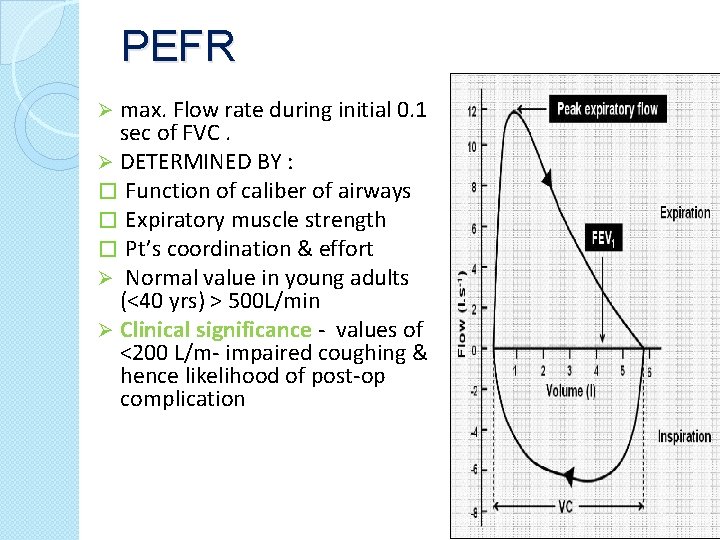
PEFR max. Flow rate during initial 0. 1 sec of FVC. Ø DETERMINED BY : � Function of caliber of airways � Expiratory muscle strength � Pt’s coordination & effort Ø Normal value in young adults (<40 yrs) > 500 L/min Ø Clinical significance - values of <200 L/m- impaired coughing & hence likelihood of post-op complication Ø
MAXIMUM BREATHING CAPACITY: (MBC/MVV) Ø Largest volume that can be breathed per minute by voluntary effort , as hard & as fast as possible. Ø N – 150 -175 l/min. Ø Estimate of max. ventilation available to meet increased physiological demand. Ø Measured for 12 secs – extrapolated for 1 min. Ø MVV = FEV 1 X 35 Ø MVV altered by- airway resistance - Elastic property -Muscle strength - Learning, Coordination, Motivation
RESPIRATORY MUSCLE STRENGTH � MAX STATIC INSP. PRESSURE: (PIMAX)- Measured when inspiratory muscles are at their optimal length i. e. at RV Ø PI MAX = -125 CM H 2 O Ø CLINICAL SIGNIFICANCE: Ø IF PI MAX< 25 CM H 2 O – Inability to take deep breath. � MAX. STATIC EXPIRATORY PRESSURE (PEMAX): Ø Measured after full inspiration to TLC Ø N VALUE OF PEMAX IS =200 CM H 20 Ø PEMAX < +40 CM H 20 – Impaired cough ability Ø Particularly useful in pts with NM Disorders during weaning Ø
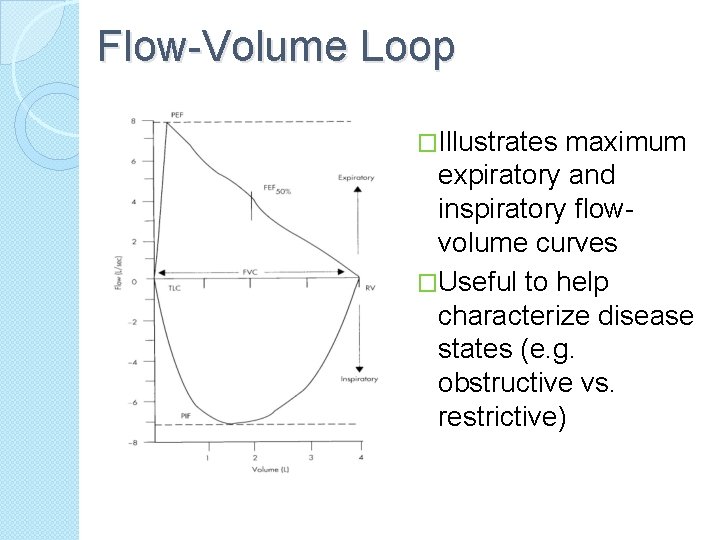
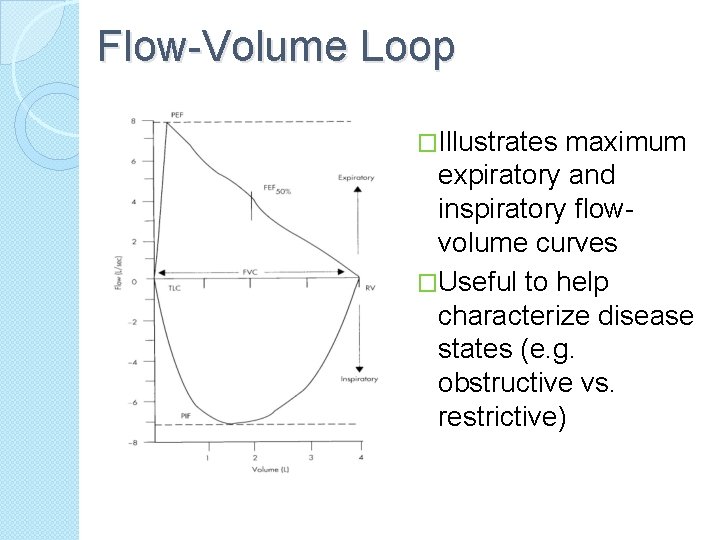
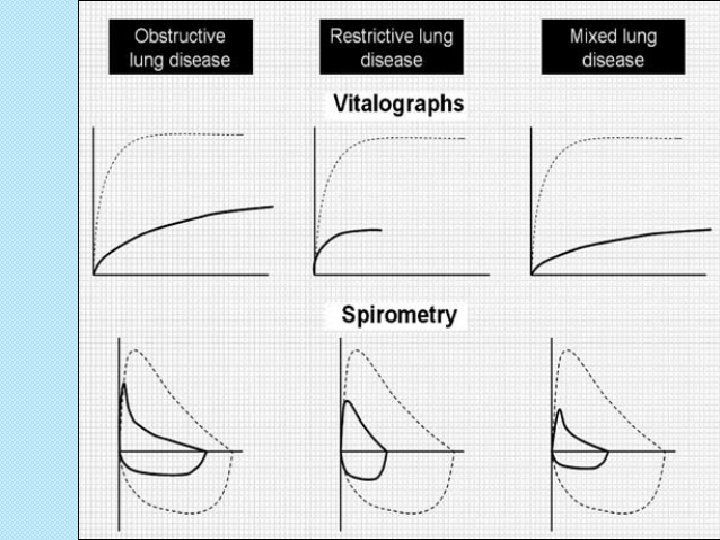
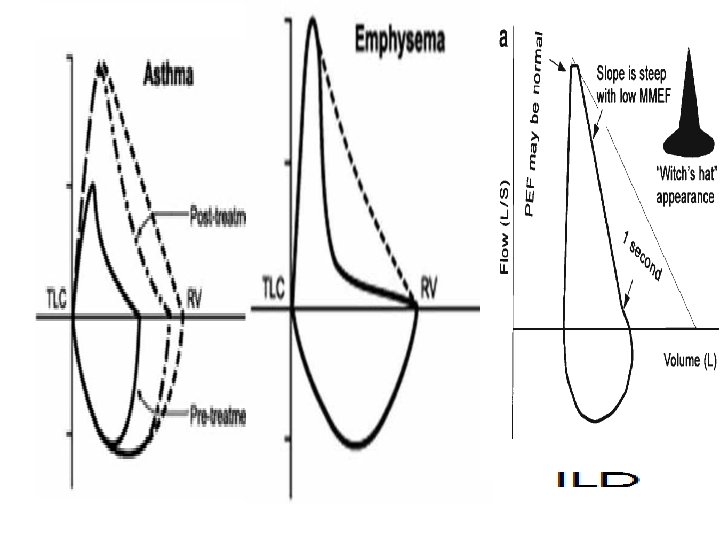
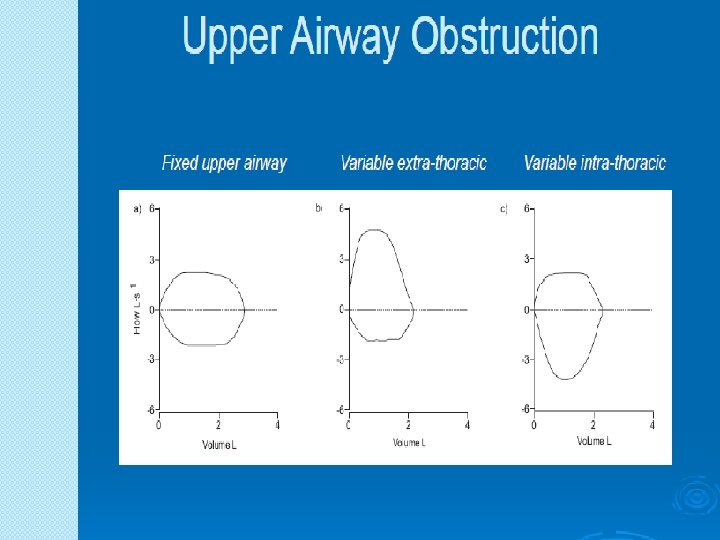
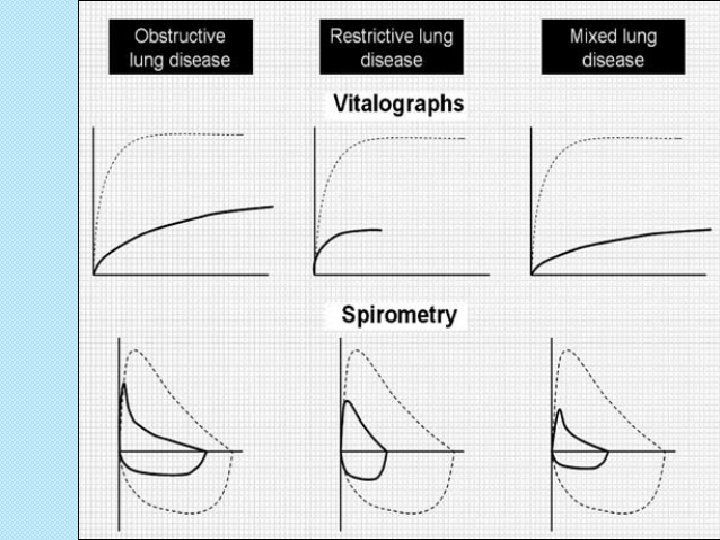
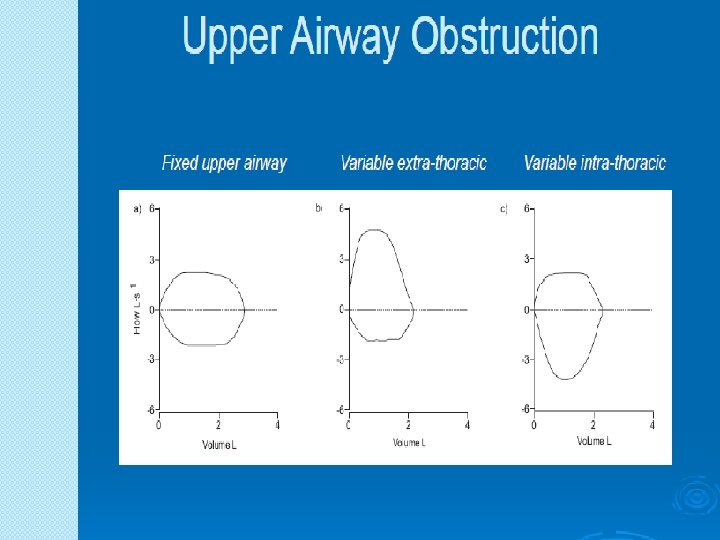
Flow-Volume Loop �Illustrates maximum expiratory and inspiratory flowvolume curves �Useful to help characterize disease states (e. g. obstructive vs. restrictive)
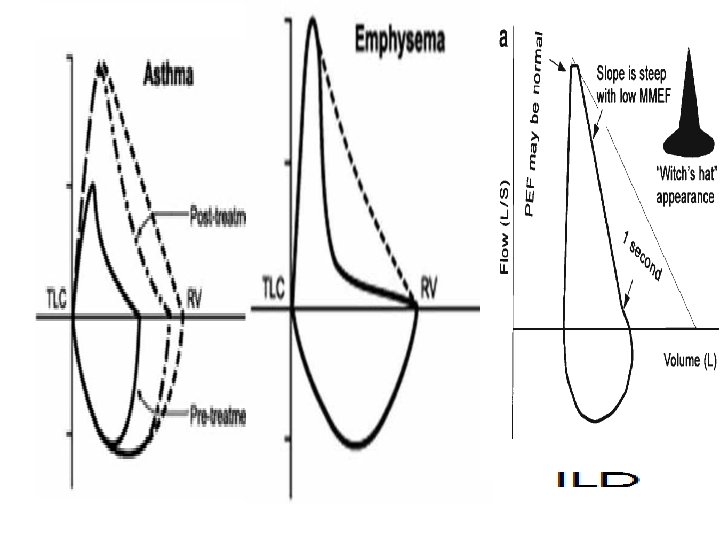
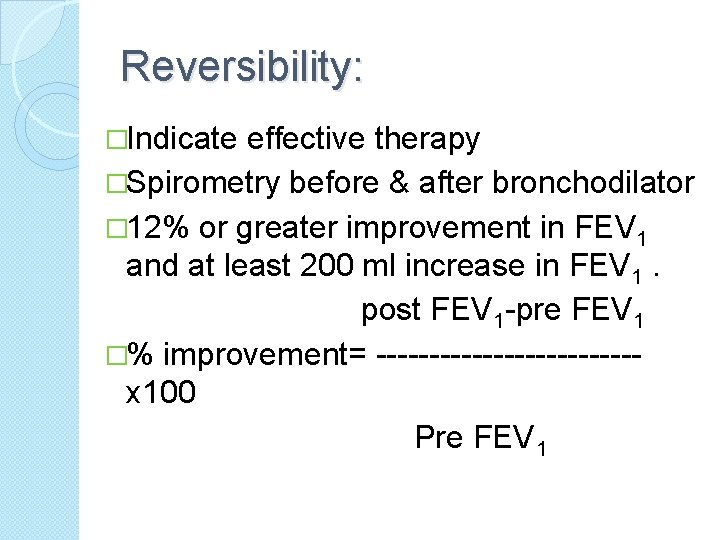
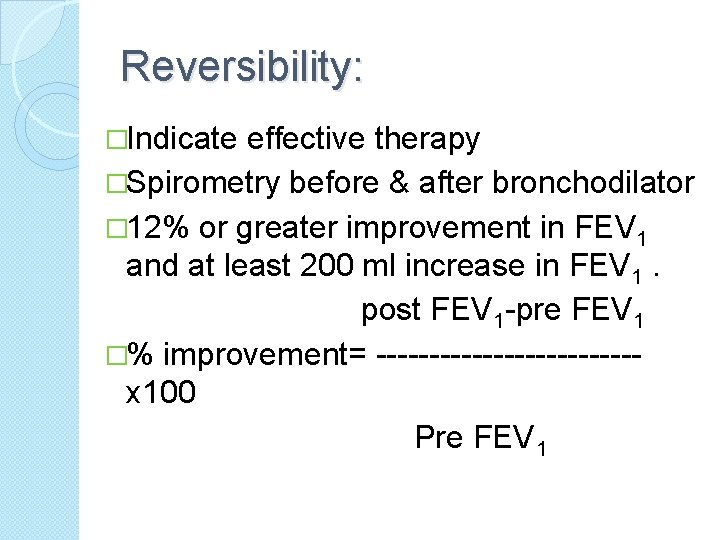
Reversibility: �Indicate effective therapy �Spirometry before & after bronchodilator � 12% or greater improvement in FEV 1 and at least 200 ml increase in FEV 1. post FEV 1 -pre FEV 1 �% improvement= ------------x 100 Pre FEV 1
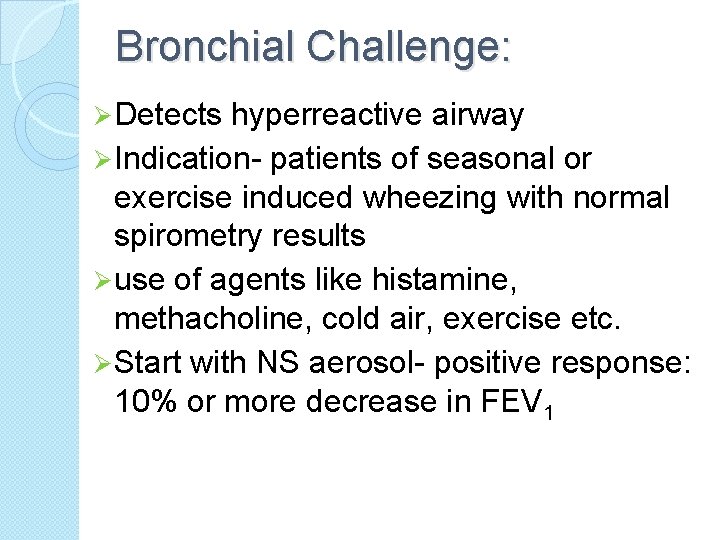
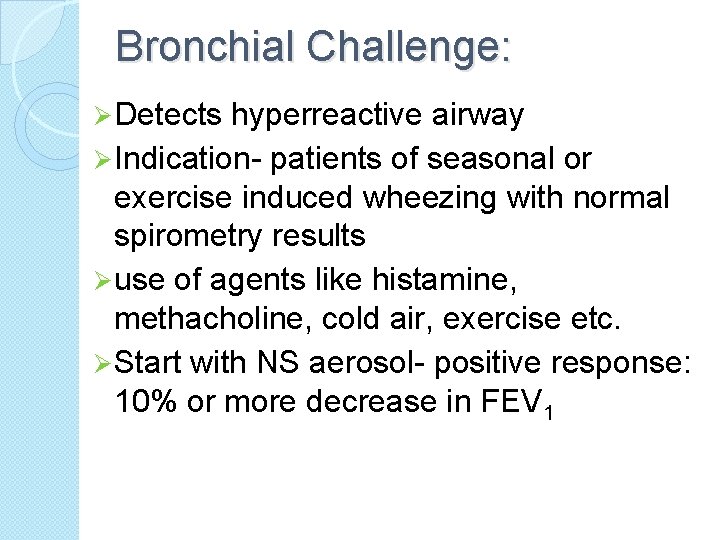
Bronchial Challenge: Ø Detects hyperreactive airway Ø Indication- patients of seasonal or exercise induced wheezing with normal spirometry results Ø use of agents like histamine, methacholine, cold air, exercise etc. Ø Start with NS aerosol- positive response: 10% or more decrease in FEV 1
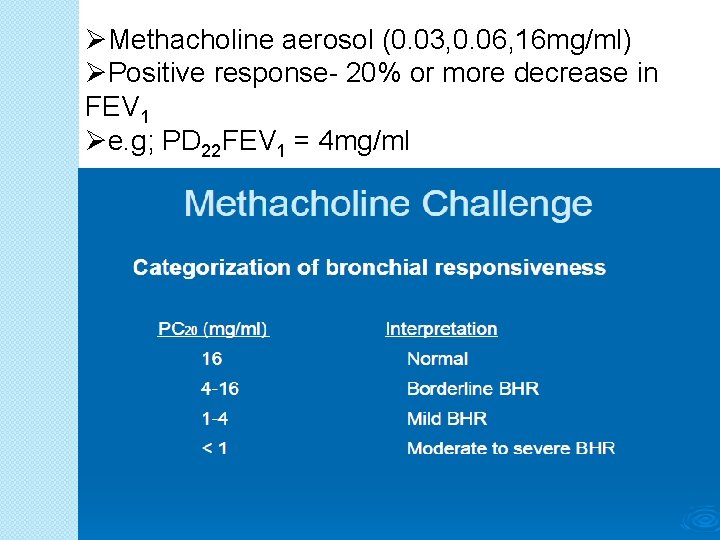
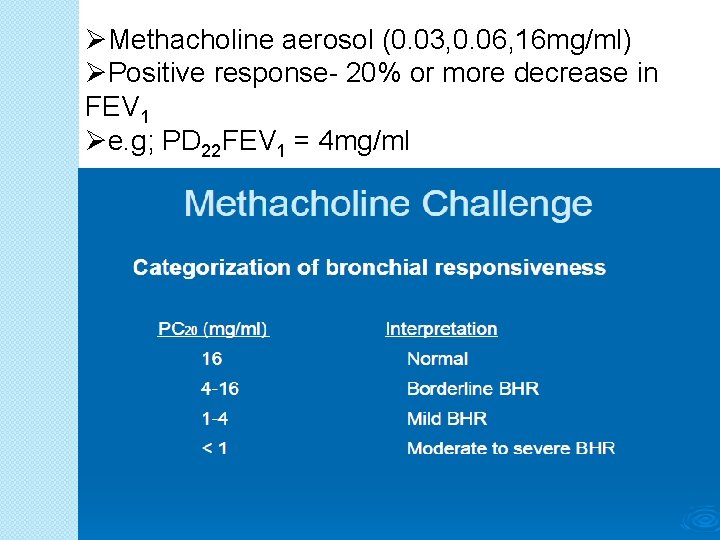
ØMethacholine aerosol (0. 03, 0. 06, 16 mg/ml) ØPositive response- 20% or more decrease in FEV 1 Øe. g; PD 22 FEV 1 = 4 mg/ml
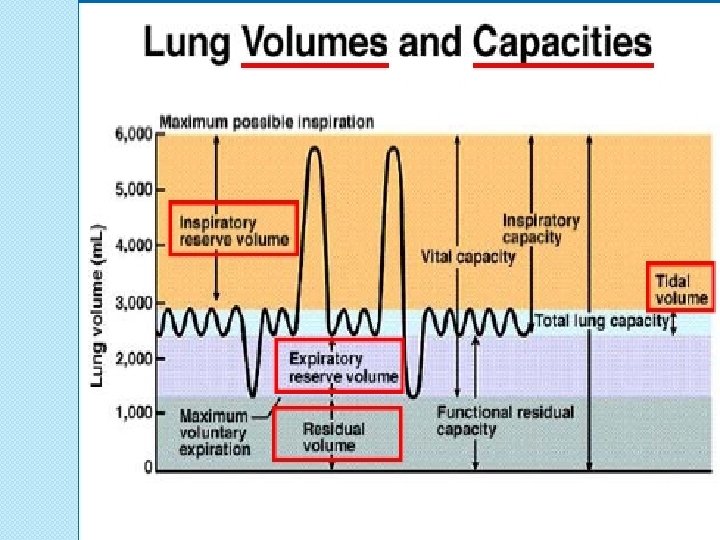
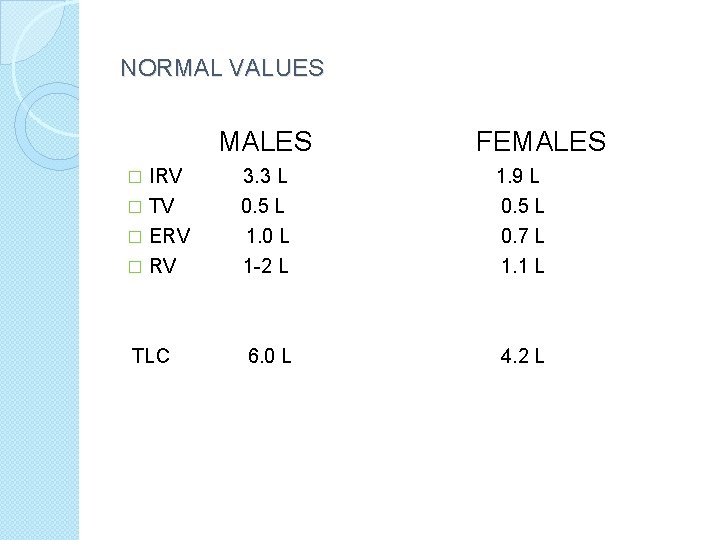
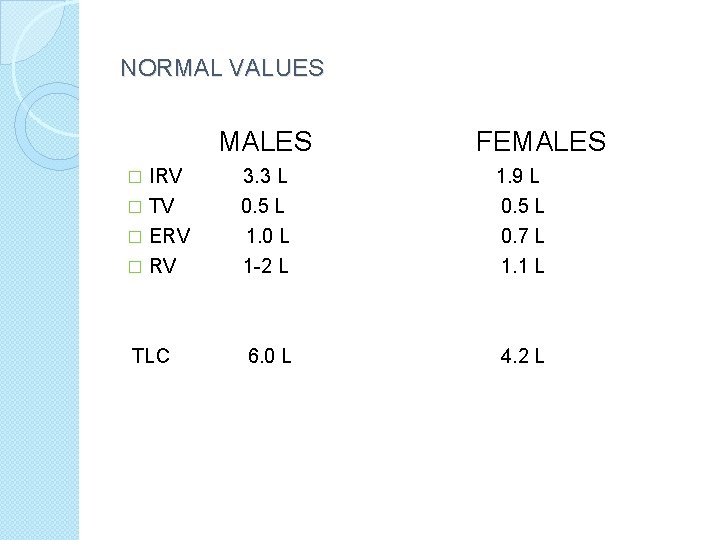
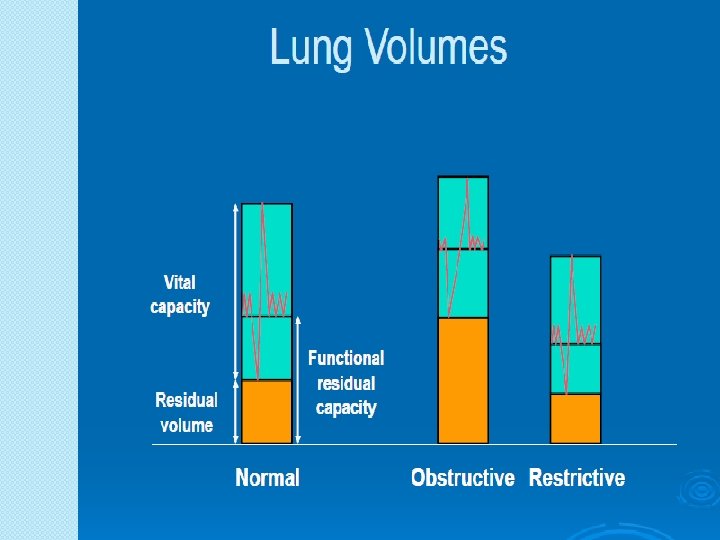
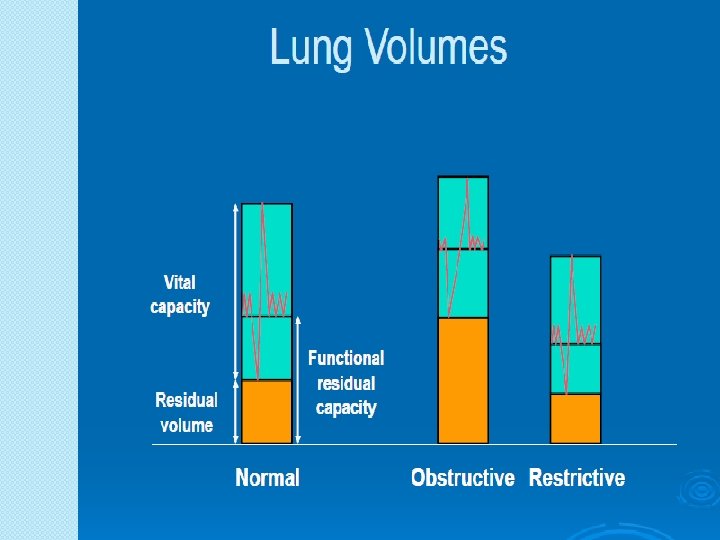
NORMAL VALUES MALES � IRV TV � ERV � TLC FEMALES 3. 3 L 1. 9 L 0. 5 L 1. 0 L 1 -2 L 0. 5 L 0. 7 L 1. 1 L 6. 0 L 4. 2 L
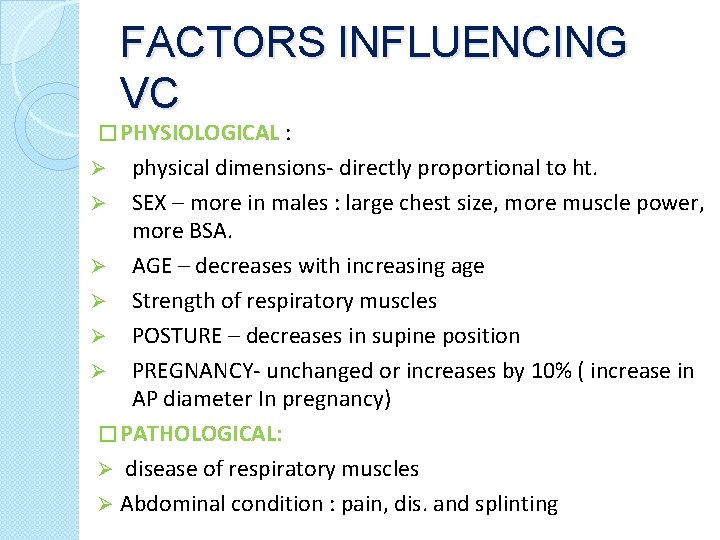
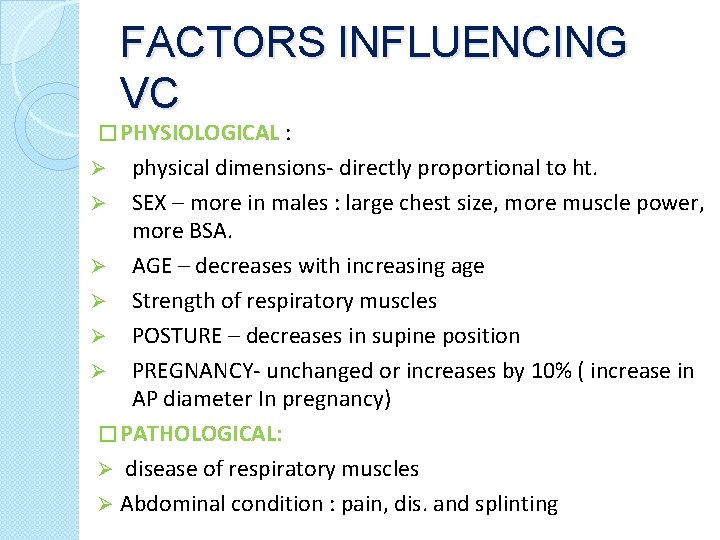
FACTORS INFLUENCING VC � PHYSIOLOGICAL : physical dimensions- directly proportional to ht. Ø SEX – more in males : large chest size, more muscle power, more BSA. Ø AGE – decreases with increasing age Ø Strength of respiratory muscles Ø POSTURE – decreases in supine position Ø PREGNANCY- unchanged or increases by 10% ( increase in AP diameter In pregnancy) � PATHOLOGICAL: Ø disease of respiratory muscles Ø Abdominal condition : pain, dis. and splinting Ø
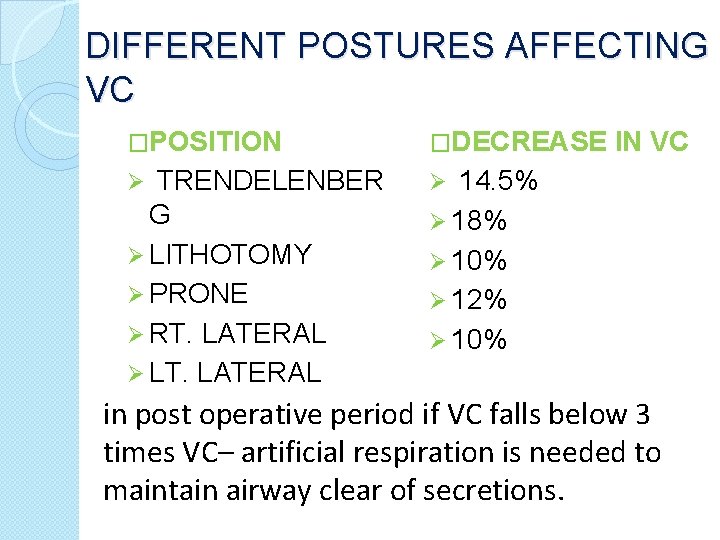
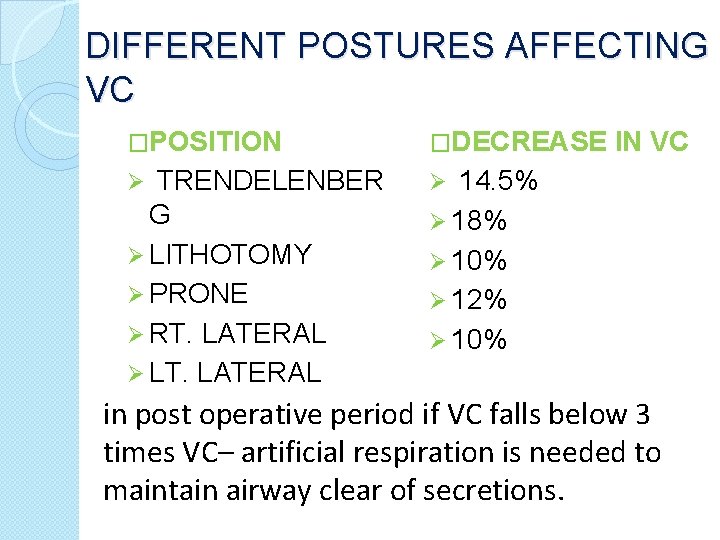
DIFFERENT POSTURES AFFECTING VC �POSITION �DECREASE TRENDELENBER G Ø LITHOTOMY Ø PRONE Ø RT. LATERAL Ø LT. LATERAL Ø Ø IN VC 14. 5% Ø 18% Ø 10% Ø 12% Ø 10% in post operative period if VC falls below 3 times VC– artificial respiration is needed to maintain airway clear of secretions.
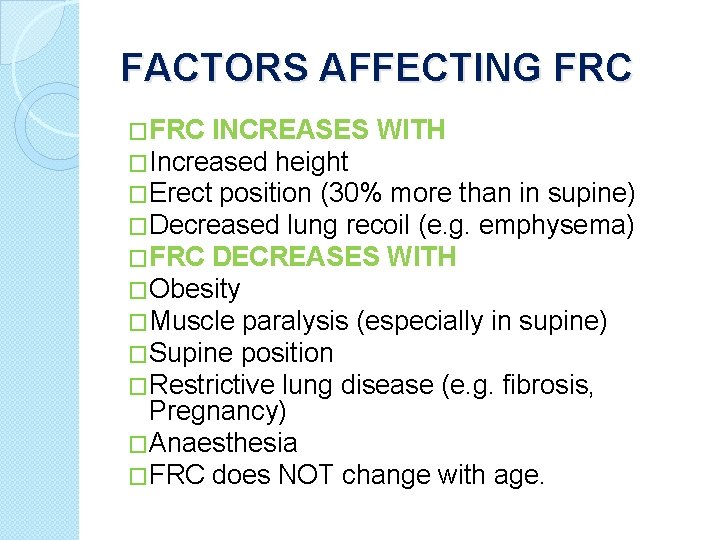
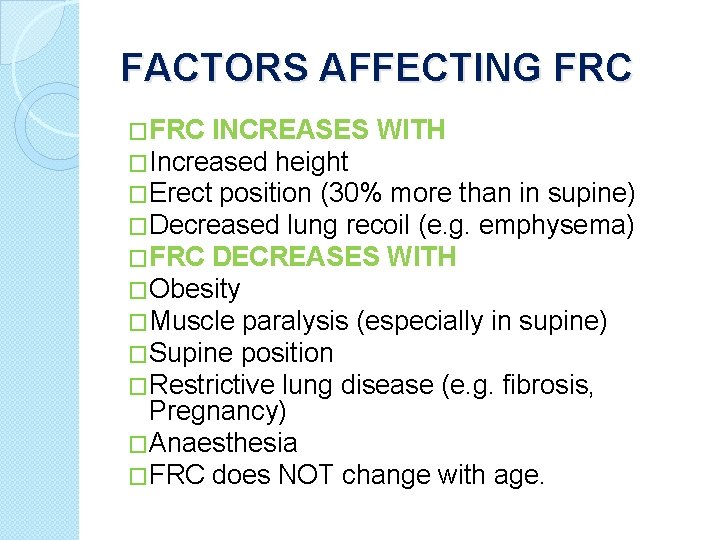
FACTORS AFFECTING FRC �FRC INCREASES WITH �Increased height �Erect position (30% more than in supine) �Decreased lung recoil (e. g. emphysema) �FRC DECREASES WITH �Obesity �Muscle paralysis (especially in supine) �Supine position �Restrictive lung disease (e. g. fibrosis, Pregnancy) �Anaesthesia �FRC does NOT change with age.
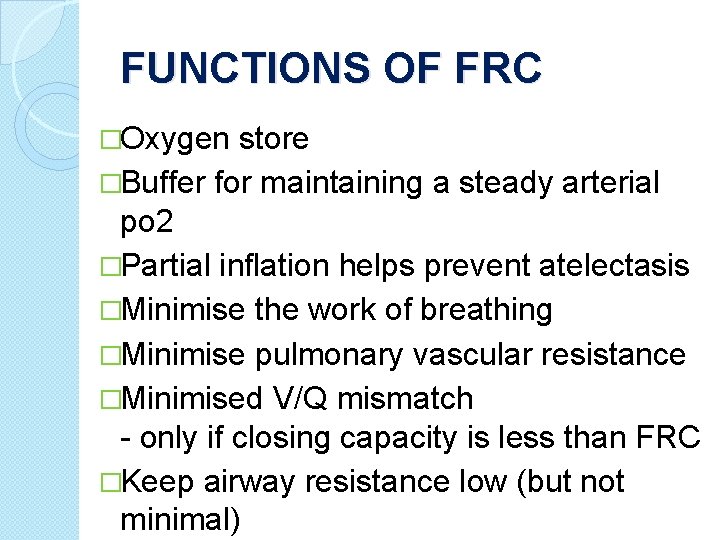
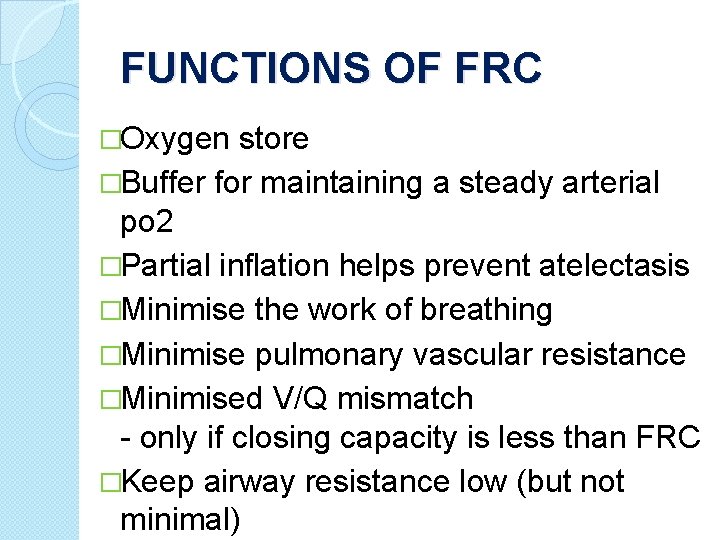
FUNCTIONS OF FRC �Oxygen store �Buffer for maintaining a steady arterial po 2 �Partial inflation helps prevent atelectasis �Minimise the work of breathing �Minimise pulmonary vascular resistance �Minimised V/Q mismatch - only if closing capacity is less than FRC �Keep airway resistance low (but not minimal)
MEASUREMENTS OF VOLUMES �TLC, RV, FRC – MEASURED USING Ø Nitrogen washout method Ø Inert gas (helium) dilution method Ø Total body plethysmography
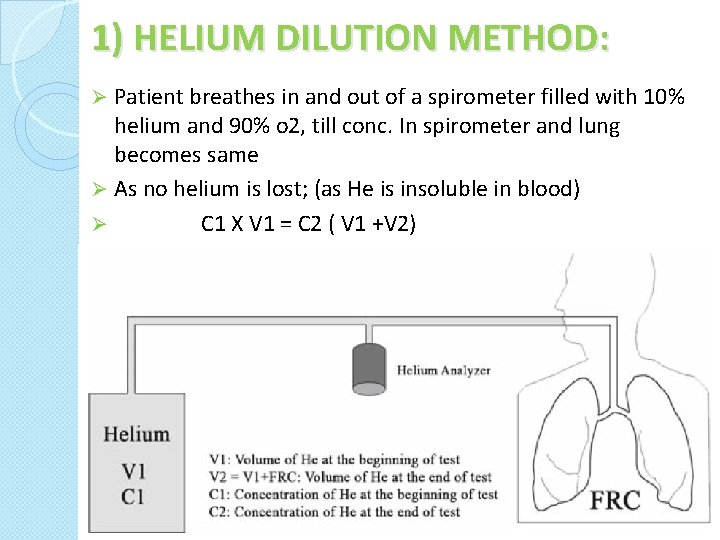
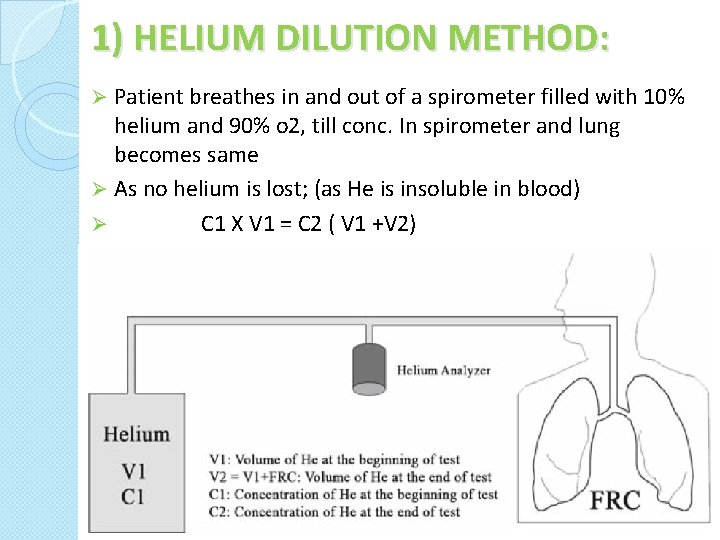
1) HELIUM DILUTION METHOD: Patient breathes in and out of a spirometer filled with 10% helium and 90% o 2, till conc. In spirometer and lung becomes same Ø As no helium is lost; (as He is insoluble in blood) Ø C 1 X V 1 = C 2 ( V 1 +V 2) Ø
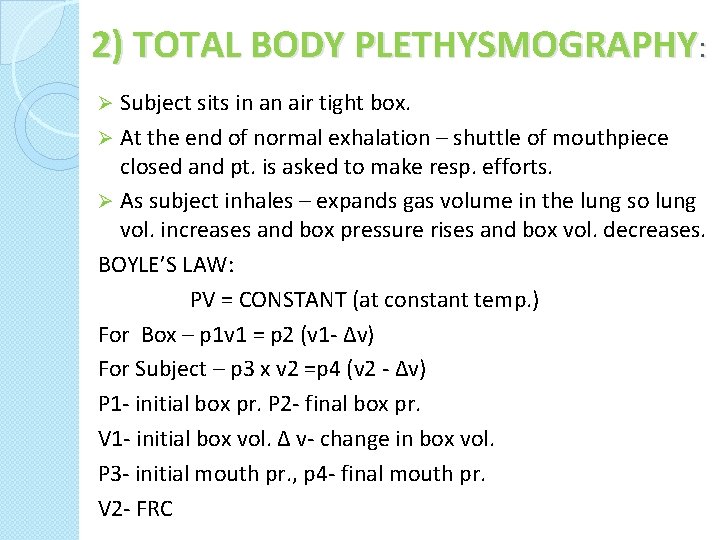
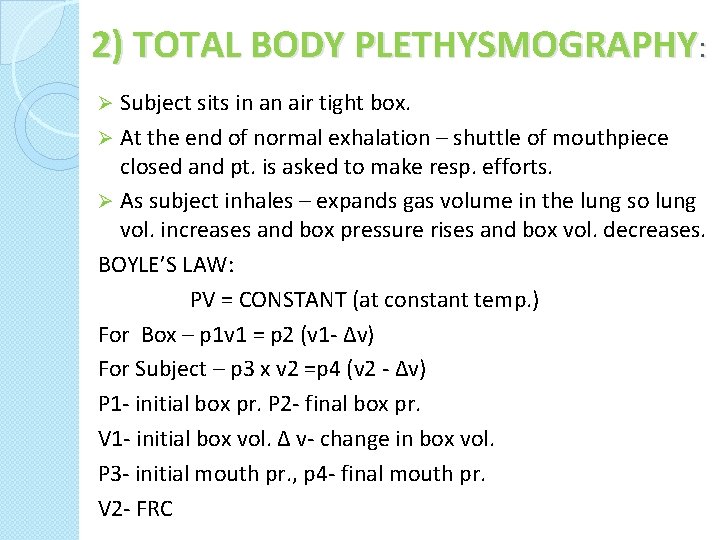
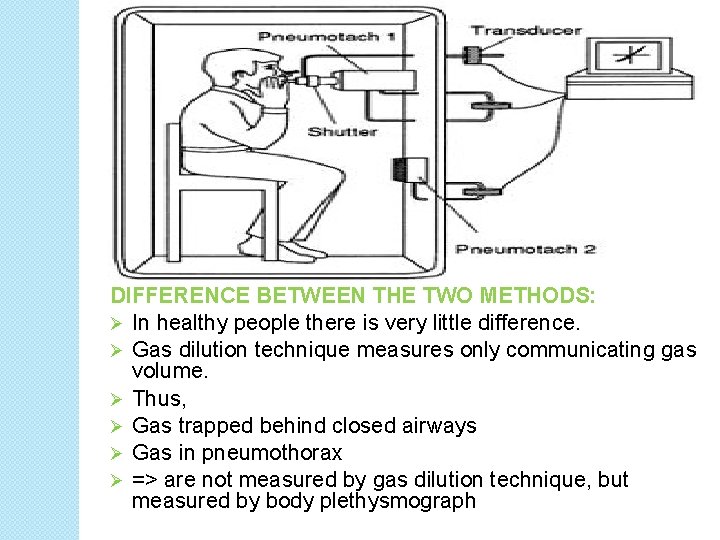
2) TOTAL BODY PLETHYSMOGRAPHY: Subject sits in an air tight box. Ø At the end of normal exhalation – shuttle of mouthpiece closed and pt. is asked to make resp. efforts. Ø As subject inhales – expands gas volume in the lung so lung vol. increases and box pressure rises and box vol. decreases. BOYLE’S LAW: PV = CONSTANT (at constant temp. ) For Box – p 1 v 1 = p 2 (v 1 - ∆v) For Subject – p 3 x v 2 =p 4 (v 2 - ∆v) P 1 - initial box pr. P 2 - final box pr. V 1 - initial box vol. ∆ v- change in box vol. P 3 - initial mouth pr. , p 4 - final mouth pr. V 2 - FRC Ø
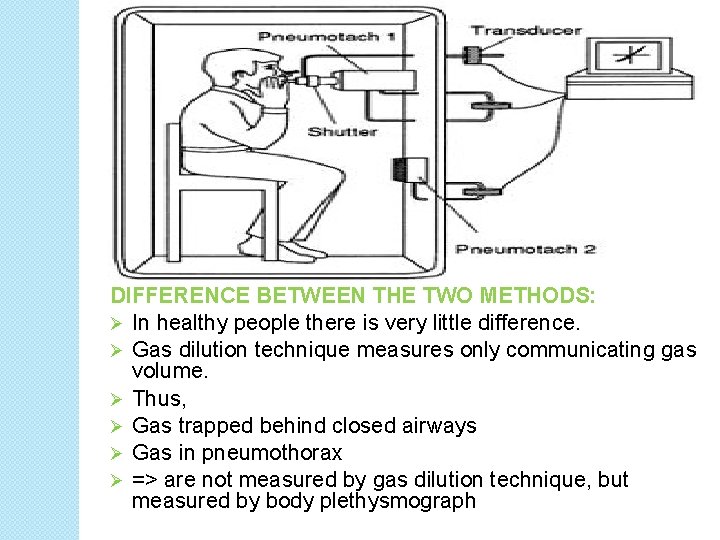
DIFFERENCE BETWEEN THE TWO METHODS: Ø In healthy people there is very little difference. Ø Gas dilution technique measures only communicating gas volume. Ø Thus, Ø Gas trapped behind closed airways Ø Gas in pneumothorax Ø => are not measured by gas dilution technique, but measured by body plethysmograph
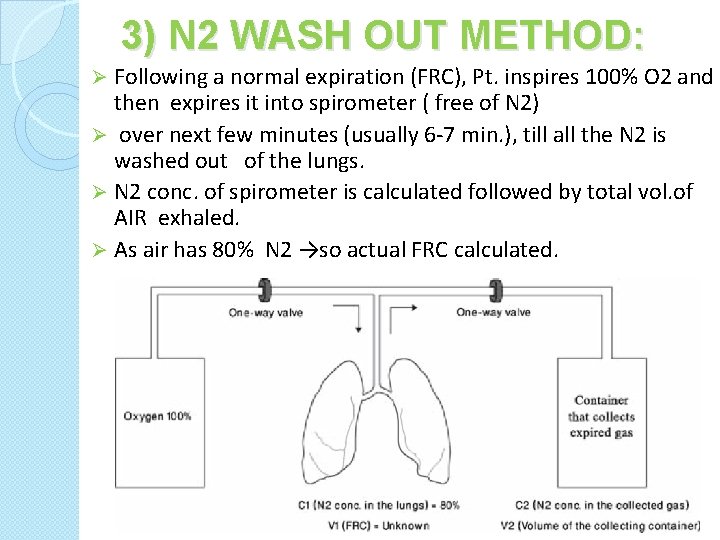
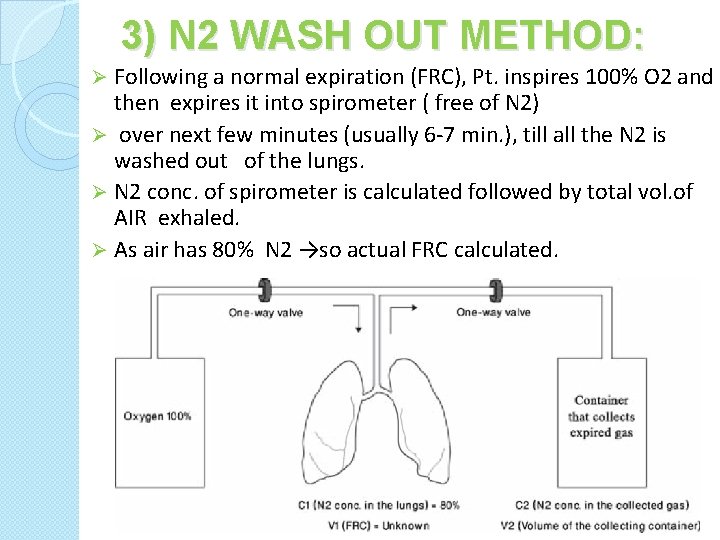
3) N 2 WASH OUT METHOD: Following a normal expiration (FRC), Pt. inspires 100% O 2 and then expires it into spirometer ( free of N 2) Ø over next few minutes (usually 6 -7 min. ), till all the N 2 is washed out of the lungs. Ø N 2 conc. of spirometer is calculated followed by total vol. of AIR exhaled. Ø As air has 80% N 2 →so actual FRC calculated. Ø
PROBLEMS WITH N 2 WASH OUT METHOD �Atelectasis may result from washout of nitrogen from poorly ventilated lung zones (obstructed areas) �Elimination of hypoxic drive in CO 2 retainers is possible �Underestimates FRC due to underventilation of areas with trapped gas
TESTS FOR GAS EXCHANGE FUNCTION 1) ALVEOLAR-ARTERIAL O 2 TENSION GRADIENT: Ø Sensitive indicator of detecting regional V/Q inequality Ø N value in young adult at room air = 8 mm. Hg to upto 25 mmhg in 8 th decade (d/t decrease in Pa. O 2) Ø Ab. N high values at room air is seen in asymptomatic smokers & chr. Bronchitis (min. symptoms) PAO 2 = PIO 2 – Pa. Co 2 R
2) DYSPNEA DIFFENRENTIATION INDEX (DDI): - To differentiate dyspnea due to resp/ cardiac disease DDI = PEFR x Pa. CO 2 1000 - DDI- Lower in resp. pathology
Ø 3) DIFFUSING CAPACITY OF LUNG: Ø depends upon gradient and thickness of alveolo-capillary membrane. Ø defined as the rate at which gas enters into blood divided by its driving pressure. Ø DRIVING PRESSURE: gradient b/w alveoli & end capillary tensions. Ø DL CO = Vco /(P A CO–P c CO)
SINGLE BREATH TEST USING CO �Pt inspires a dilute mixture of CO and hold the breath for 10 secs. �CO taken up is determined by infrared analysis �N range 20 - 30 ml/min. /mmhg. �NORMAL- 75 -120% of predicted �DL IS MEASURED BY USING CO, coz: A) High affinity for Hb which is approx. 210 times that of O 2 , so does not rapidly build up in plasma B) Therefore, pulm capillary partial pressure of CO ≈ 0
DLCO decreases inØ Emphysema, lung resection, pul. Embolism, anaemia Ø Pulmonary fibrosis, sarcoidosis- increased thickness DLCO increases in: (Cond. Which increase pulm. bld flow) Ø Supine position Ø Exercise Ø Obesity Ø L-R shunt
TESTS FOR CARDIOPLULMONARY INTERACTIONS �Reflects gas exchange, ventilation, tissue O 2. �QUALITATIVE- history, exam, ABG, stair climbing test �QUANTITATIVE- 6 minute walk test
� 1) STAIR CLIMBING TEST: Ø If able to climb 3 flights of stairs without stopping/ dypnoea at his/her own pace-↓ed morbidity & mortality Ø If not able to climb 2 flights – high risk Ø Quantitative assessment by measuring the max O 2 uptake during exercise(VO 2 max). Ø A 2 -flight stair climb (20 steps/min) without dyspnea is approx VO 2 max of 16 ml/kg/min. ü VO 2 max≥ 20 ml/kg/min: minimal risk ü VO 2 max≤ 15 ml/kg/min: inc cardiopulmonary risk ü VO 2 max≤ 10 ml/kg/min: high risk with 30% mortality
� 2) 6 MINUTE WALK TEST: Ø Gold standard Ø C. P. reserve is measured by estimating max. O 2 uptake during exercise Ø Modified if pt. can’t walk – bicycle/ arm exercises Ø If pt. is able to walk for >2000 feet during 6 min, VO 2 max > 15 ml/kg/min Ø If 1080 feet in 6 min( 180 feet in 1 min): VO 2 of 12 ml/kg/min Ø Simultaneously oximetry is done & if Spo 2 falls >4%- high risk
BED SIDE PFT 1). Sabrasez breath holding test: >25 sec. -normal 15 -25 sec- limited CPR <15 sec- very poor CPR (Contraindication for elective surgery) 25 - 30 SEC - 3500 ml VC 20 – 25 SEC - 3000 ml VC 15 - 20 SEC - 2500 ml VC 10 - 15 SEC - 2000 ml VC 5 - 10 SEC - 1500 ml VC
2). SINGLE BREATH COUNT: It is a measure of the FRC. >15 : normal <15 : dec reserve 11 -15 : mild impairment 5 -10 : mod impaired <5 : severe impairment 3). FET (WATCH AND STETHOSCOPE TEST ): After deep breath, exhale maximally and forcefully & keep stethoscope over trachea & listen. N. – 3 -5 SECS. OBS. LUNG DIS. - > 6 SEC RES. LUNG DIS. - < 3 SEC
4) SCHNEIDER’S MATCH BLOWING TEST: Measures MBC Ø ü ü ü Ø Ø Ø Ask to blow a match stick from a distance of 6” (15 cms) with. Mouth wide open, Chin rested, No purse lipping No head movement, No air movement in the room Mouth and match at the same level Can not blow out a match MBC < 60 L/min FEV 1 < 1. 6 L Able to blow out a match MBC > 60 L/min FEV 1 > 1. 6 L MODIFIED MATCH TEST: DISTANCE MBC 9” >150 L/MIN. 6” >60 L/MIN. 3” > 40 L/MIN.
5) GREENE & BEROWITZ COUGH TEST: �deep breath f/by cough Ø ABILITY TO COUGH Ø STRENGTH Ø EFFECTIVENESS �INADEQUATE COUGH IF: FVC<20 ML/KG FEV 1 < 15 ML/KG PEFR < 200 L/MIN. Ø VC ~ 3 times TV for effective cough. Ø wet productive cough / self propagated paraoxysms of coughing – patient susceptible for pulmonary Complication.

6) WRIGHT PEAK FLOW METER: Measures PEFR N – MALES- 450 -700 L/MIN. FEMALES- 350 -500 L/MIN. <200 L/min. –inadequate cough efficiency.
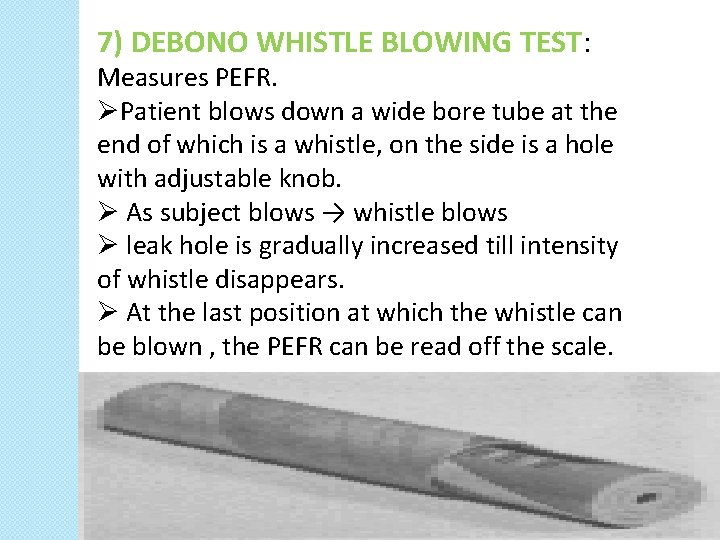
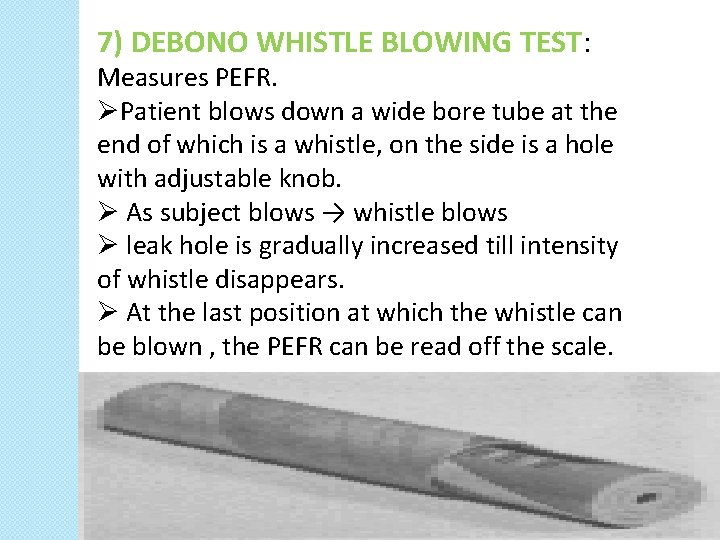
7) DEBONO WHISTLE BLOWING TEST: Measures PEFR. ØPatient blows down a wide bore tube at the end of which is a whistle, on the side is a hole with adjustable knob. Ø As subject blows → whistle blows Ø leak hole is gradually increased till intensity of whistle disappears. Ø At the last position at which the whistle can be blown , the PEFR can be read off the scale.
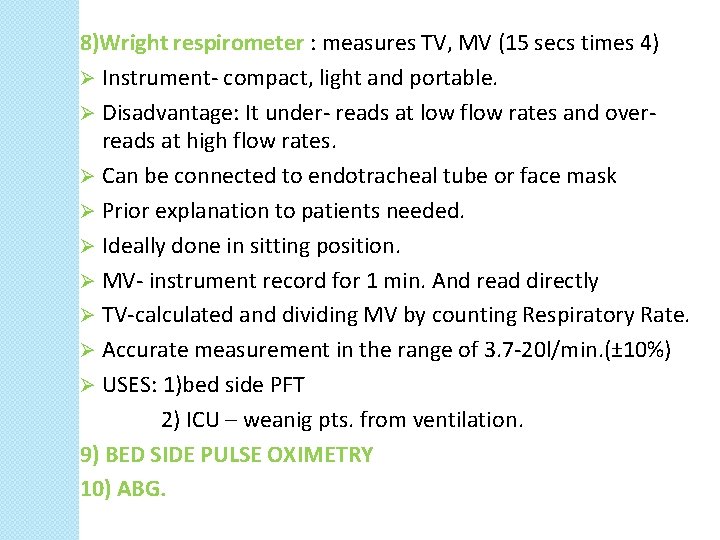
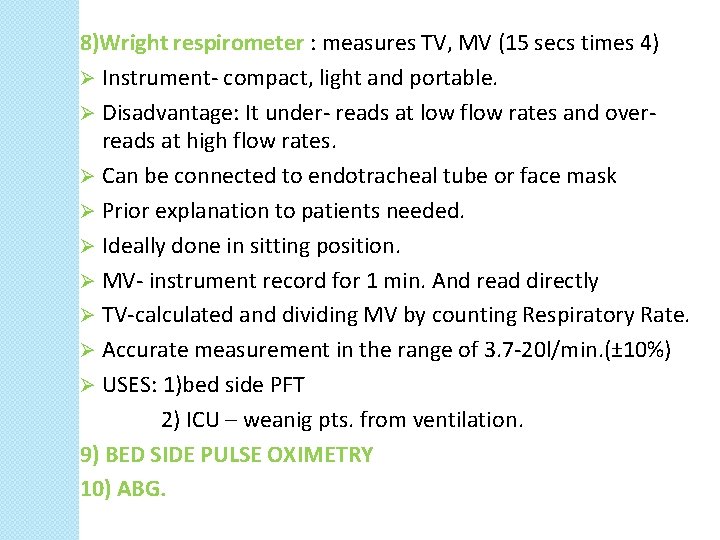
8)Wright respirometer : measures TV, MV (15 secs times 4) Ø Instrument- compact, light and portable. Ø Disadvantage: It under- reads at low flow rates and overreads at high flow rates. Ø Can be connected to endotracheal tube or face mask Ø Prior explanation to patients needed. Ø Ideally done in sitting position. Ø MV- instrument record for 1 min. And read directly Ø TV-calculated and dividing MV by counting Respiratory Rate. Ø Accurate measurement in the range of 3. 7 -20 l/min. (± 10%) Ø USES: 1)bed side PFT 2) ICU – weanig pts. from ventilation. 9) BED SIDE PULSE OXIMETRY 10) ABG.
THANK YOU