PULMONARY EMBOLISM Jan Tomis 2018 Pulmonary embolism Obstruction
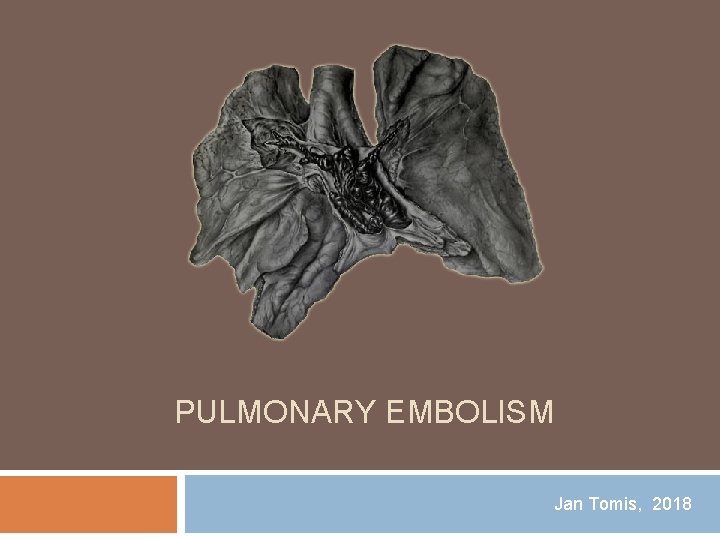
PULMONARY EMBOLISM Jan Tomis, 2018
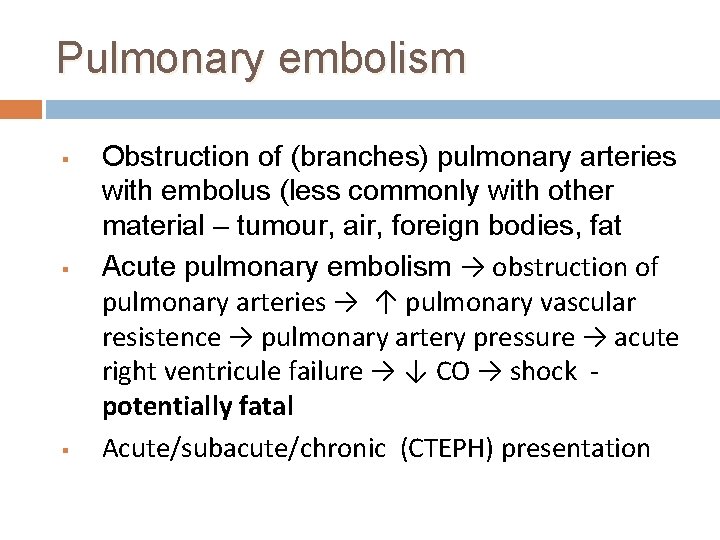
Pulmonary embolism § § § Obstruction of (branches) pulmonary arteries with embolus (less commonly with other material – tumour, air, foreign bodies, fat Acute pulmonary embolism → obstruction of pulmonary arteries → ↑ pulmonary vascular resistence → pulmonary artery pressure → acute right ventricule failure → ↓ CO → shock potentially fatal Acute/subacute/chronic (CTEPH) presentation
Pulmonary embolism In most cases (99%) venous tromboembolism – other forms (fat, foreign body, air embolism are very rare) Origin of emboli in proximal lower extremity veins – iliac, femoral, popliteal Other sources are rare (upper extremity veins, renal vein) Virchow triad - venous stasis, endothelial injury, and a hypercoagulable state
Epidemiology Incidence circa 50 -100 cases per 100000 a year 300000 deaths anually in Europe 1 year mortality after pulmonary embolism estimated at 10 -13%
Symptoms Wide range of symptoms – asymptomatic patiets (incident finding on CT) v. s. hemodynamic shock (SUDDEN ONSET) DYSPNOE!!!! Chest pain - pleuritic (with periferal emboli and infarction) v. s. stenocardia (central emboli with RV ischemia) Shock, syncope, hypotension Hemoptysis, palpitations, caught

Risk factors Inherited – hypercoagulation (FV Leiden, prothrombin mutation, factor C and S deficiency) Acquired – recent surgery, trauma, initiation of hormonet herapy, active cancer, obesity, heavy cigarette smoking, older age, generally any severe internal comorbidity (heart failure, COPD, pneumonia, infection, dehydration …. )
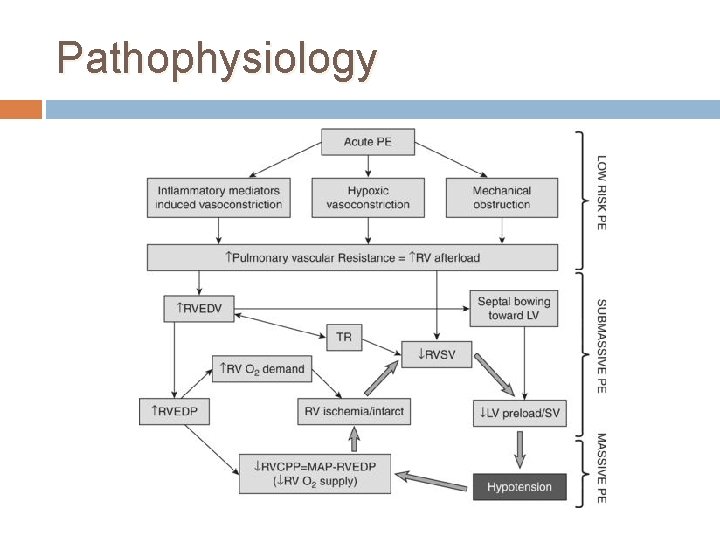
Pathophysiology
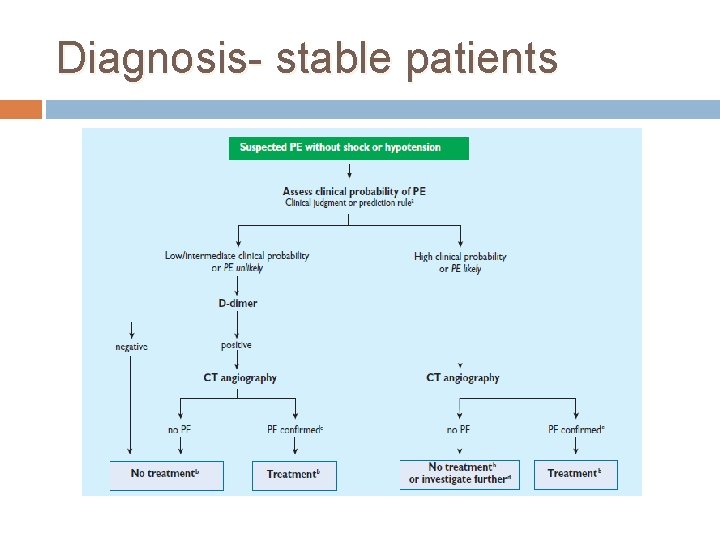
Diagnosis- stable patients
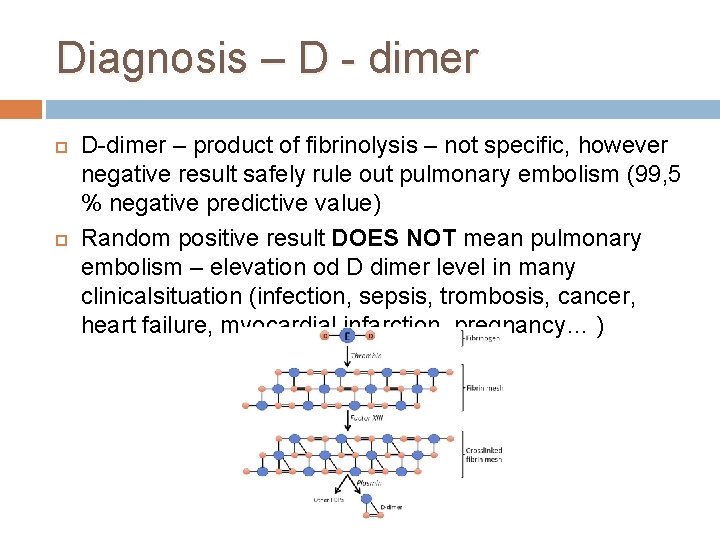
Diagnosis – D - dimer D-dimer – product of fibrinolysis – not specific, however negative result safely rule out pulmonary embolism (99, 5 % negative predictive value) Random positive result DOES NOT mean pulmonary embolism – elevation od D dimer level in many clinicalsituation (infection, sepsis, trombosis, cancer, heart failure, myocardial infarction, pregnancy… )
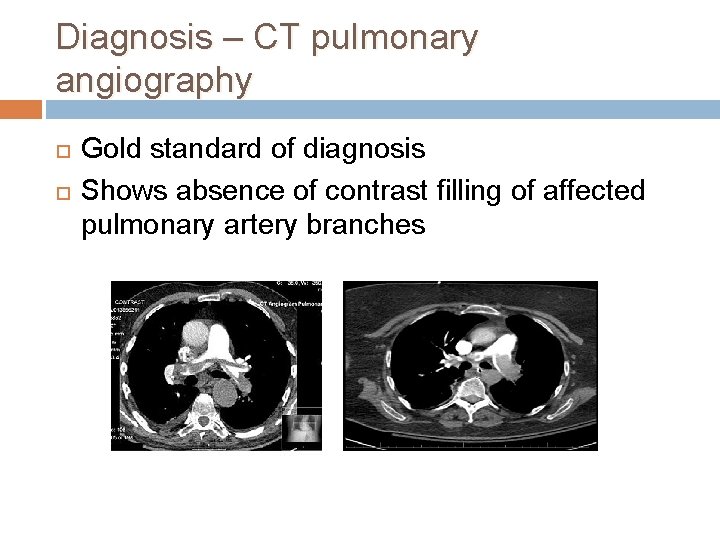
Diagnosis – CT pulmonary angiography Gold standard of diagnosis Shows absence of contrast filling of affected pulmonary artery branches
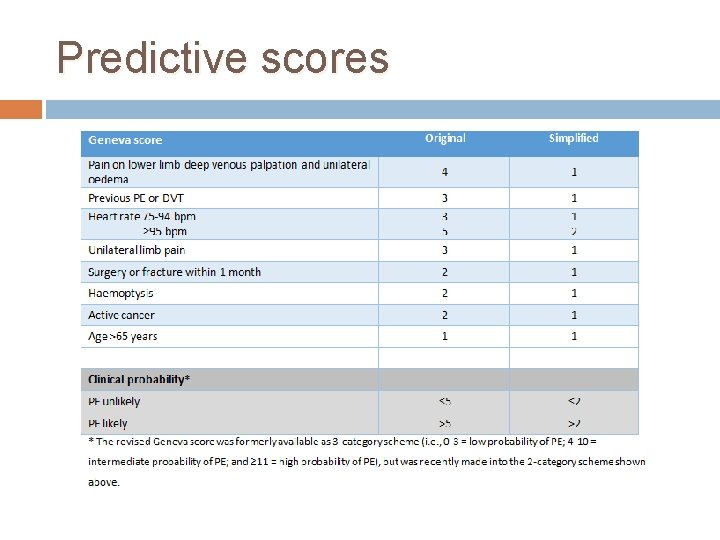
Predictive scores
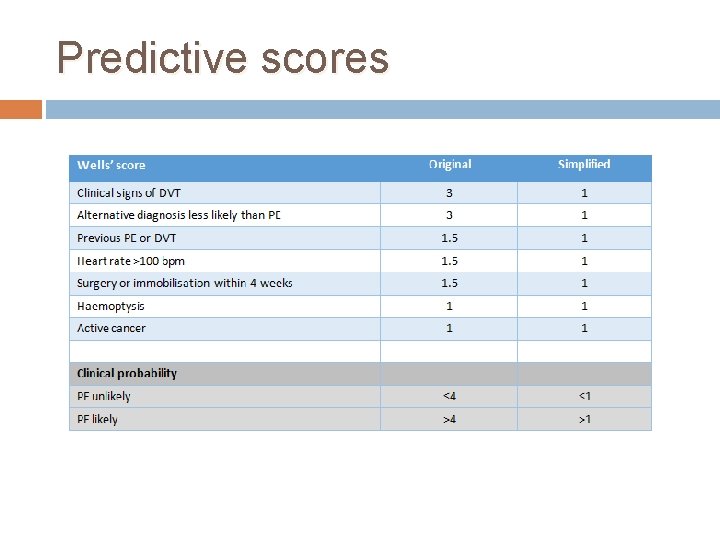
Predictive scores
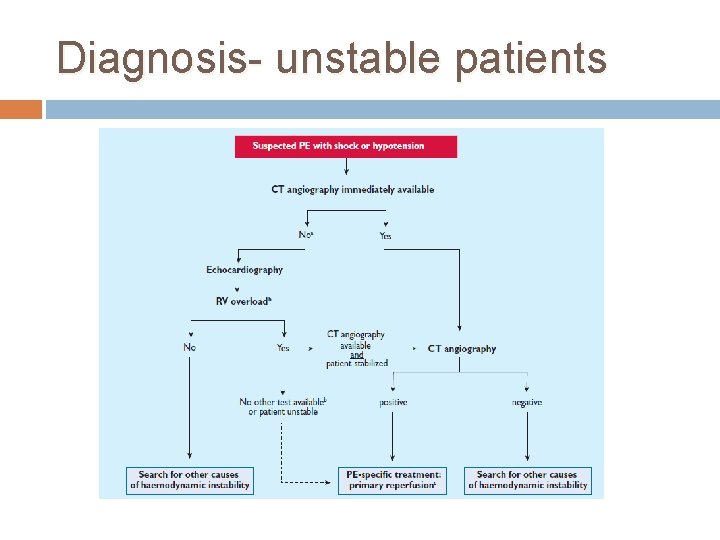
Diagnosis- unstable patients
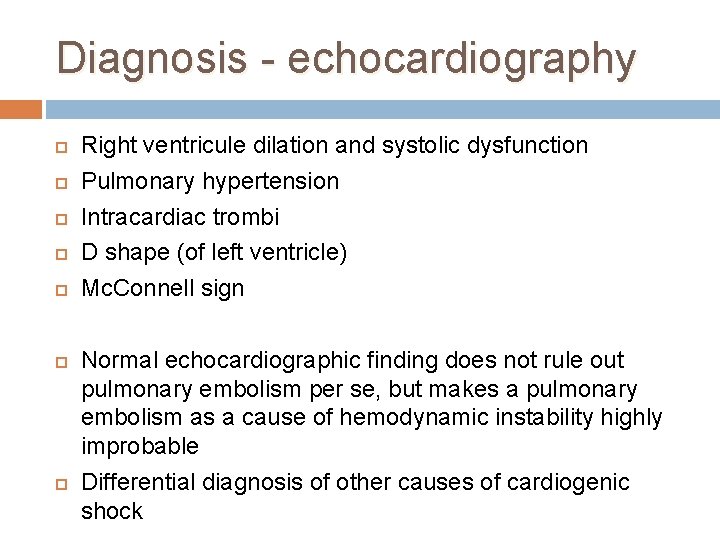
Diagnosis - echocardiography Right ventricule dilation and systolic dysfunction Pulmonary hypertension Intracardiac trombi D shape (of left ventricle) Mc. Connell sign Normal echocardiographic finding does not rule out pulmonary embolism per se, but makes a pulmonary embolism as a cause of hemodynamic instability highly improbable Differential diagnosis of other causes of cardiogenic shock

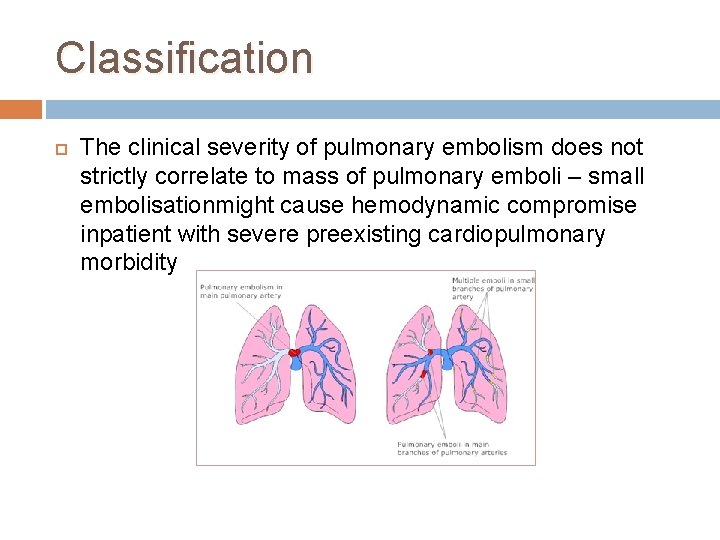
Classification The clinical severity of pulmonary embolism does not strictly correlate to mass of pulmonary emboli – small embolisationmight cause hemodynamic compromise inpatient with severe preexisting cardiopulmonary morbidity
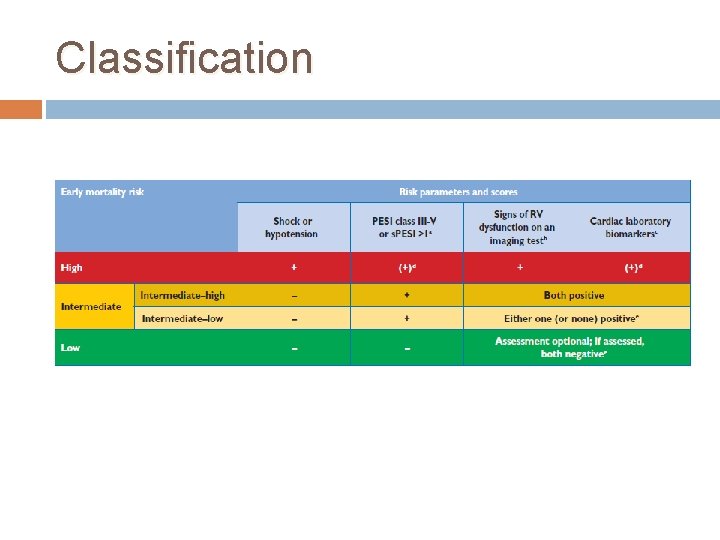
Classification
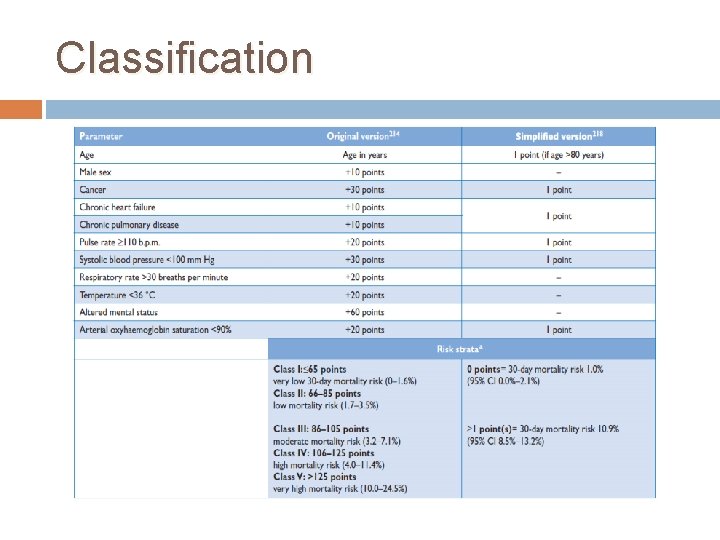
Classification
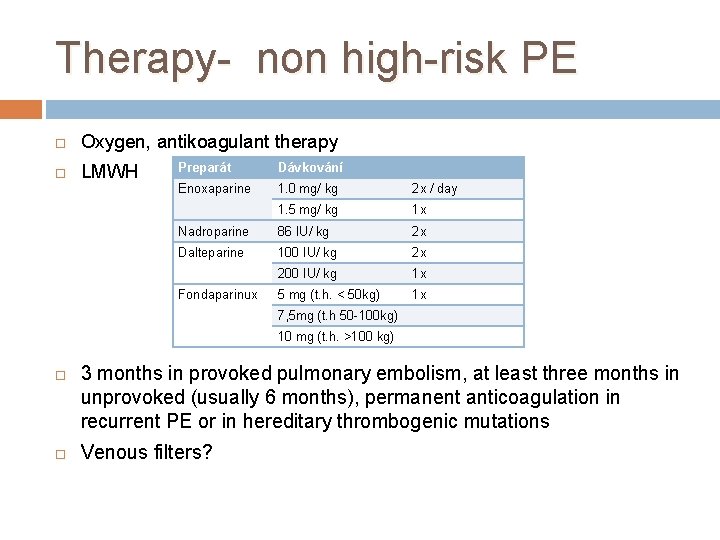
Therapy- non high-risk PE Oxygen, antikoagulant therapy LMWH Preparát Dávkování Enoxaparine 1. 0 mg/ kg 2 x / day 1. 5 mg/ kg 1 x Nadroparine 86 IU/ kg 2 x Dalteparine 100 IU/ kg 2 x 200 IU/ kg 1 x 5 mg (t. h. < 50 kg) 1 x Fondaparinux 7, 5 mg (t. h 50 -100 kg) 10 mg (t. h. >100 kg) 3 months in provoked pulmonary embolism, at least three months in unprovoked (usually 6 months), permanent anticoagulation in recurrent PE or in hereditary thrombogenic mutations Venous filters?
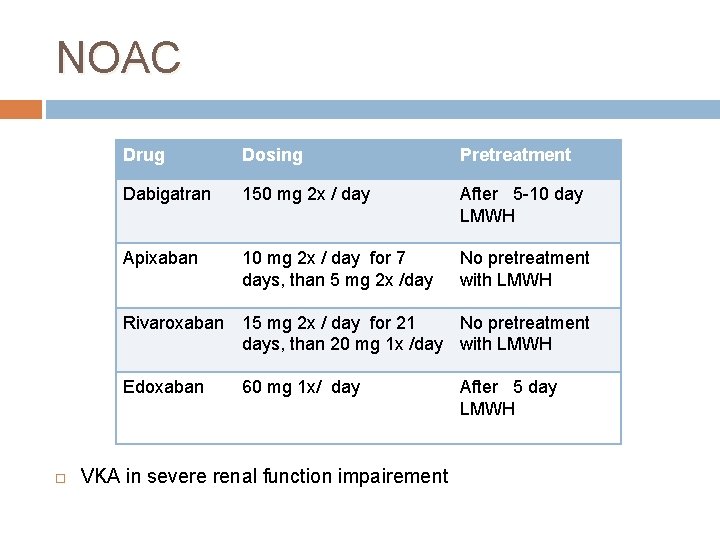
NOAC Drug Dosing Pretreatment Dabigatran 150 mg 2 x / day After 5 -10 day LMWH Apixaban 10 mg 2 x / day for 7 days, than 5 mg 2 x /day No pretreatment with LMWH Rivaroxaban 15 mg 2 x / day for 21 No pretreatment days, than 20 mg 1 x /day with LMWH Edoxaban 60 mg 1 x/ day VKA in severe renal function impairement After 5 day LMWH
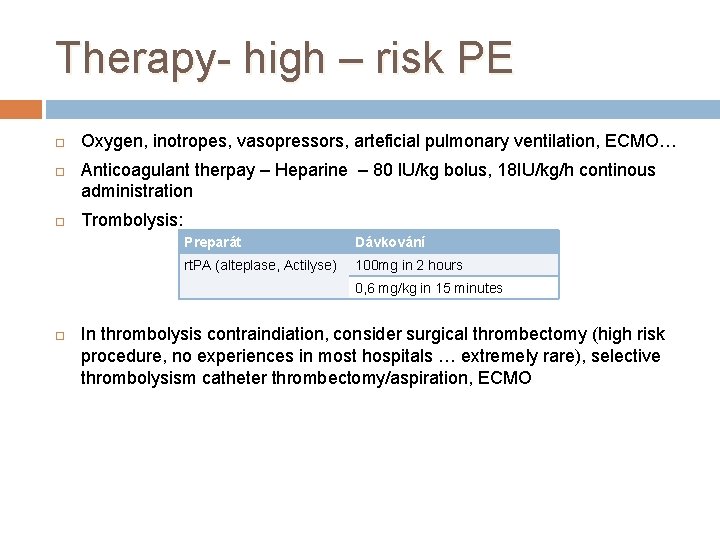
Therapy- high – risk PE Oxygen, inotropes, vasopressors, arteficial pulmonary ventilation, ECMO… Anticoagulant therpay – Heparine – 80 IU/kg bolus, 18 IU/kg/h continous administration Trombolysis: Preparát Dávkování rt. PA (alteplase, Actilyse) 100 mg in 2 hours 0, 6 mg/kg in 15 minutes In thrombolysis contraindiation, consider surgical thrombectomy (high risk procedure, no experiences in most hospitals … extremely rare), selective thrombolysism catheter thrombectomy/aspiration, ECMO
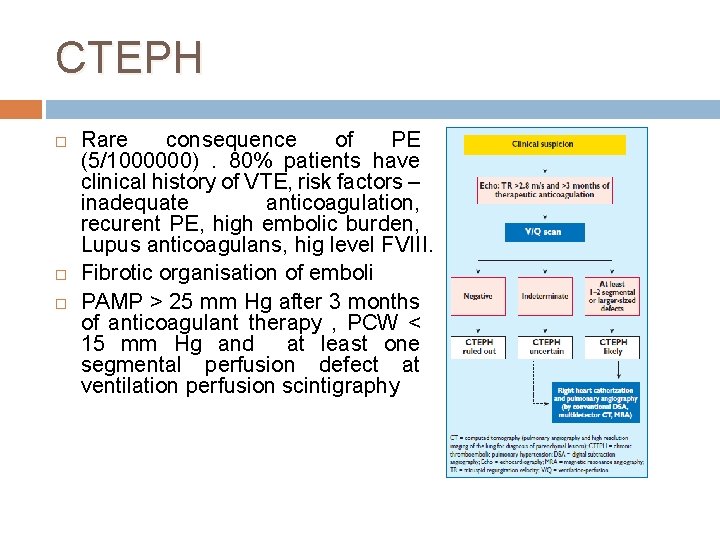
CTEPH Rare consequence of PE (5/1000000). 80% patients have clinical history of VTE, risk factors – inadequate anticoagulation, recurent PE, high embolic burden, Lupus anticoagulans, hig level FVIII. Fibrotic organisation of emboli PAMP > 25 mm Hg after 3 months of anticoagulant therapy , PCW < 15 mm Hg and at least one segmental perfusion defect at ventilation perfusion scintigraphy
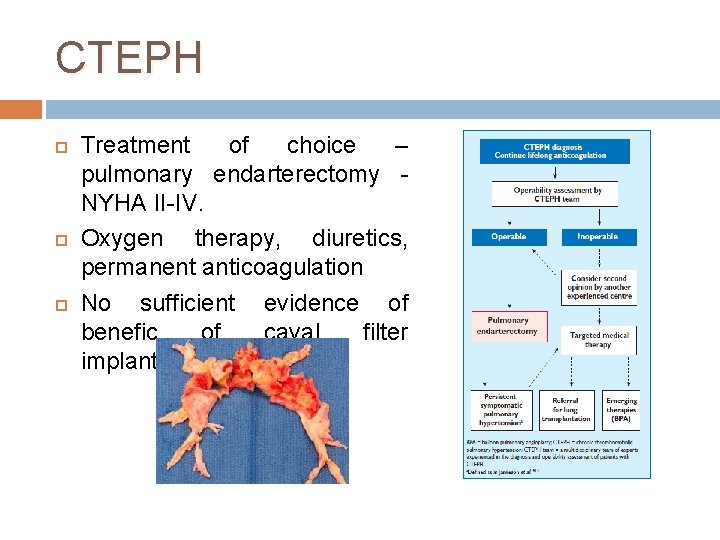
CTEPH Treatment of choice – pulmonary endarterectomy NYHA II-IV. Oxygen therapy, diuretics, permanent anticoagulation No sufficient evidence of benefic of caval filter implantation
- Slides: 24