Pulmonary Drug Delivery Dr Mohammad Issa 1 Pulmonary



- Slides: 39
Pulmonary Drug Delivery Dr Mohammad Issa 1
Pulmonary Drug Delivery ¡ ¡ ¡ Anatomy and Physiology of the Respiratory System Advantages of Pulmonary Delivery Lung epithelium at different sites within the lungs Pulmonary absorptive surfaces Systemic delivery of: l l l ¡ Small hydrophobic drugs Small hydrophilic drugs Macromolecules drugs Pulmonary Drug Delivery Devices 2
Anatomy and Physiology of the Respiratory System ¡ The human respiratory system is divided into upper and lower respiratory tracts ¡ The upper respiratory system consists of the nose, nasal cavities, nasopharynx, and oropharynx ¡ The lower respiratory tract consists of the larynx, trachea, bronchi, and alveoli, which are composed of respiratory tissues ¡ The left and right lungs are unequal in size. The right lung is composed of three lobes: the superior, middle, and inferior lobes. The smaller left lung has two lobes 3

Anatomy and Physiology of the Respiratory System 4
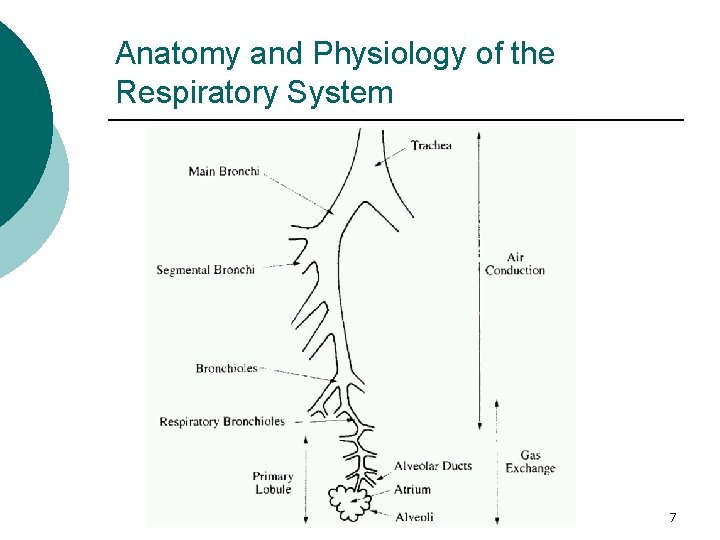
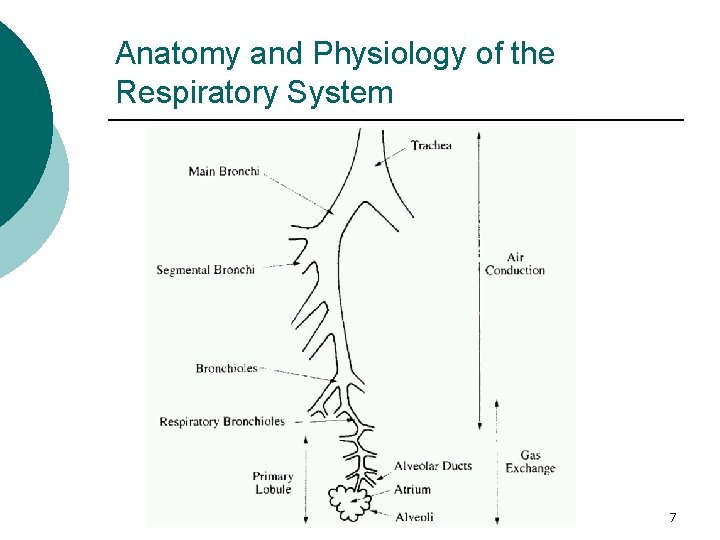
Anatomy and Physiology of the Respiratory System ¡ The nasopharynx is a passageway from the nose to the oral pharynx ¡ The larynx controls the airflow to the lungs and aids in phonation ¡ The larynx leads into the cartilaginous and fibromuscular tube, the trachea, which bifurcates into the right and left bronchi ¡ The bronchi, in turn, divide into bronchioles and finally into alveoli 5
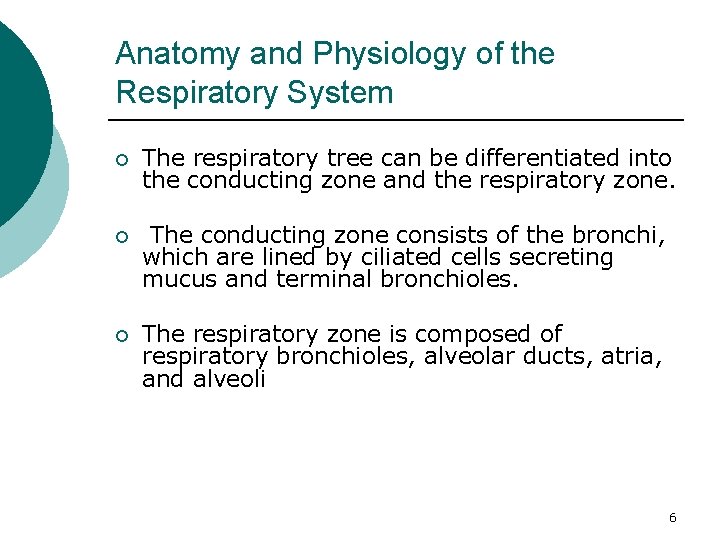
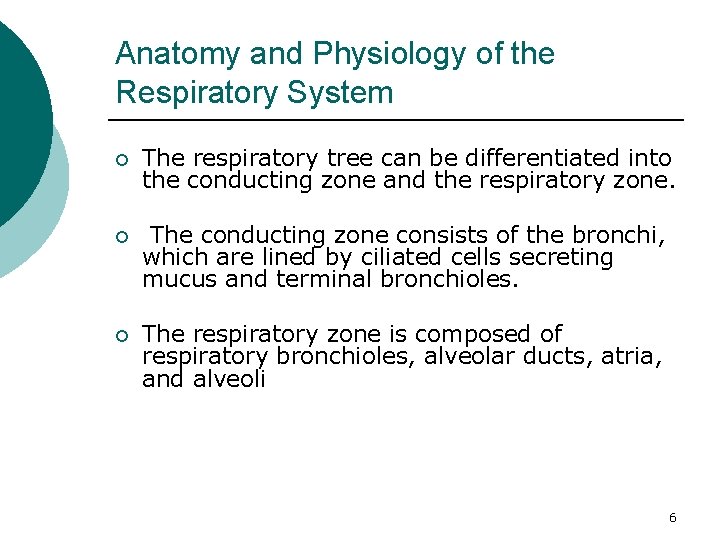
Anatomy and Physiology of the Respiratory System ¡ The respiratory tree can be differentiated into the conducting zone and the respiratory zone. ¡ The conducting zone consists of the bronchi, which are lined by ciliated cells secreting mucus and terminal bronchioles. ¡ The respiratory zone is composed of respiratory bronchioles, alveolar ducts, atria, and alveoli 6
Anatomy and Physiology of the Respiratory System 7
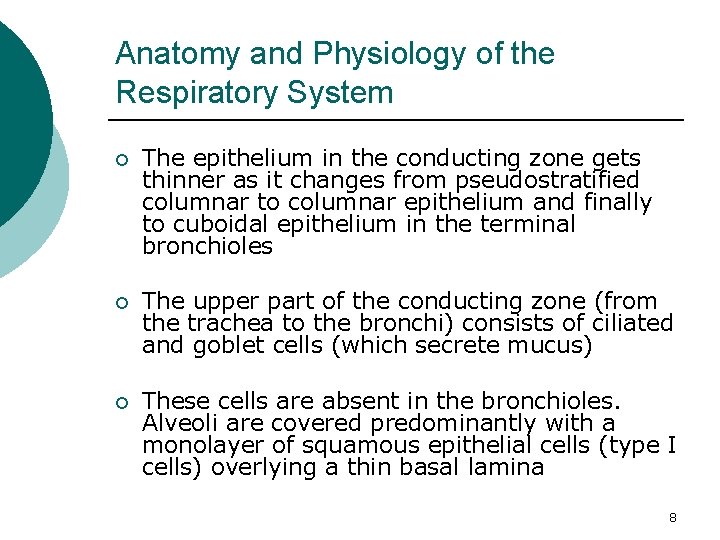
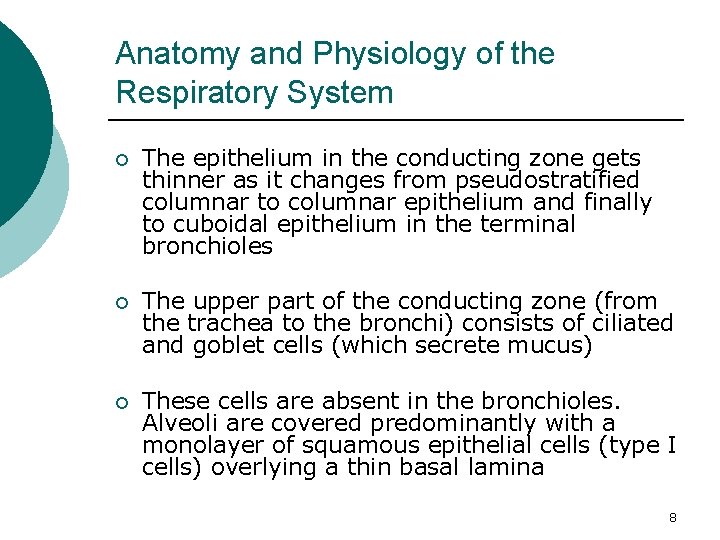
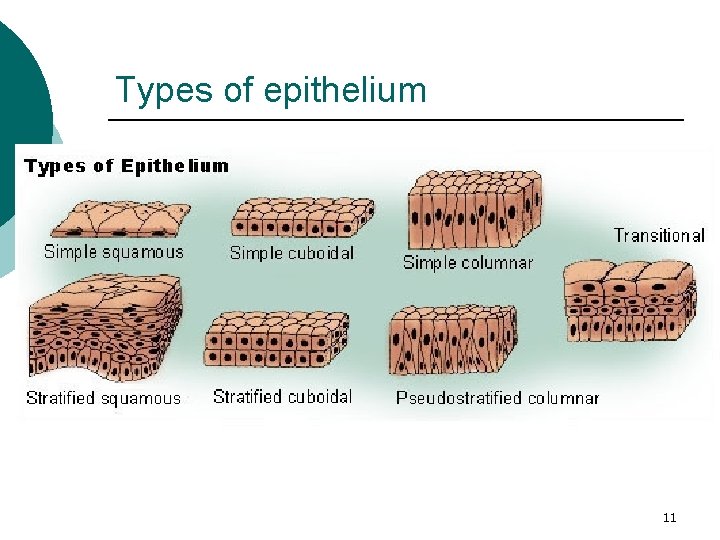
Anatomy and Physiology of the Respiratory System ¡ The epithelium in the conducting zone gets thinner as it changes from pseudostratified columnar to columnar epithelium and finally to cuboidal epithelium in the terminal bronchioles ¡ The upper part of the conducting zone (from the trachea to the bronchi) consists of ciliated and goblet cells (which secrete mucus) ¡ These cells are absent in the bronchioles. Alveoli are covered predominantly with a monolayer of squamous epithelial cells (type I cells) overlying a thin basal lamina 8
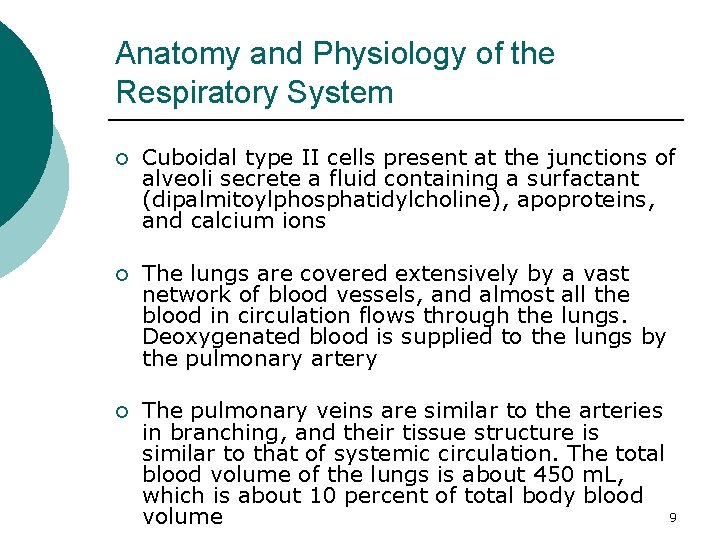
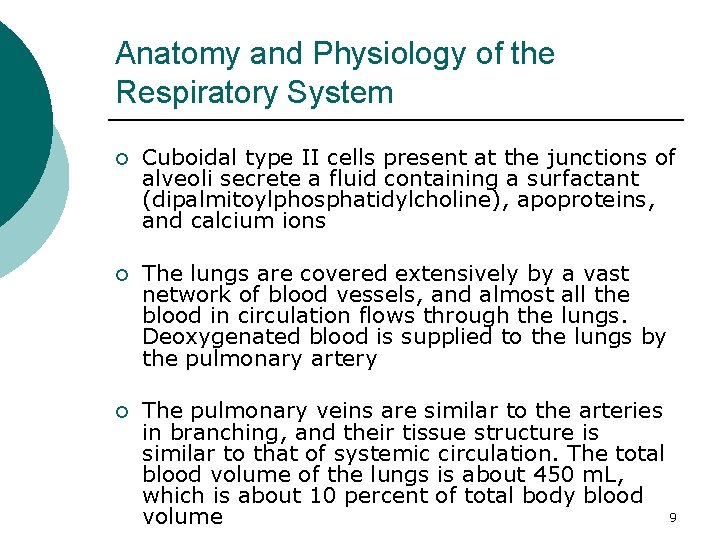
Anatomy and Physiology of the Respiratory System ¡ Cuboidal type II cells present at the junctions of alveoli secrete a fluid containing a surfactant (dipalmitoylphosphatidylcholine), apoproteins, and calcium ions ¡ The lungs are covered extensively by a vast network of blood vessels, and almost all the blood in circulation flows through the lungs. Deoxygenated blood is supplied to the lungs by the pulmonary artery ¡ The pulmonary veins are similar to the arteries in branching, and their tissue structure is similar to that of systemic circulation. The total blood volume of the lungs is about 450 m. L, which is about 10 percent of total body blood 9 volume

Comparison of the lung epithelium at different sites within the lungs 10
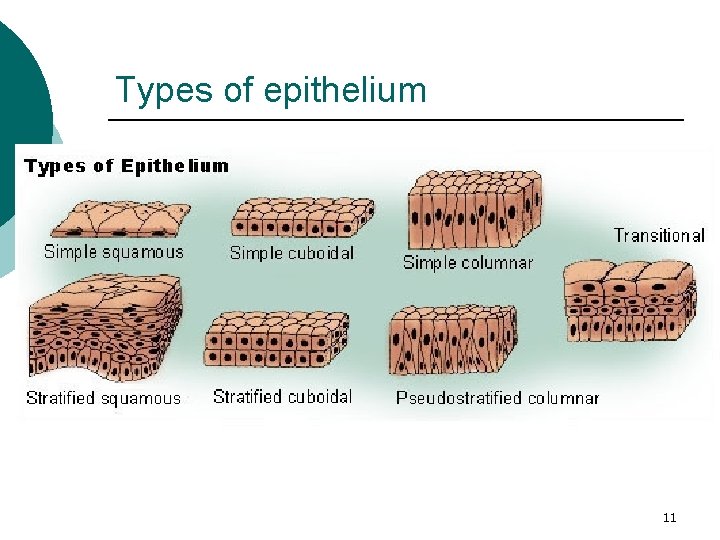
Types of epithelium 11
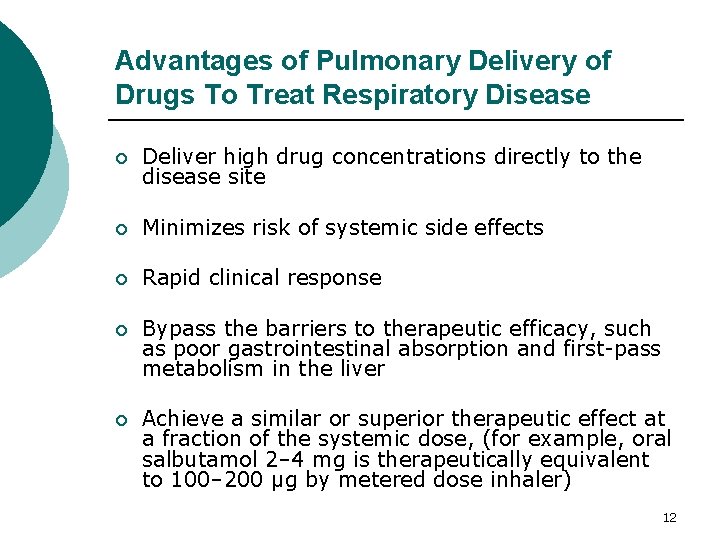
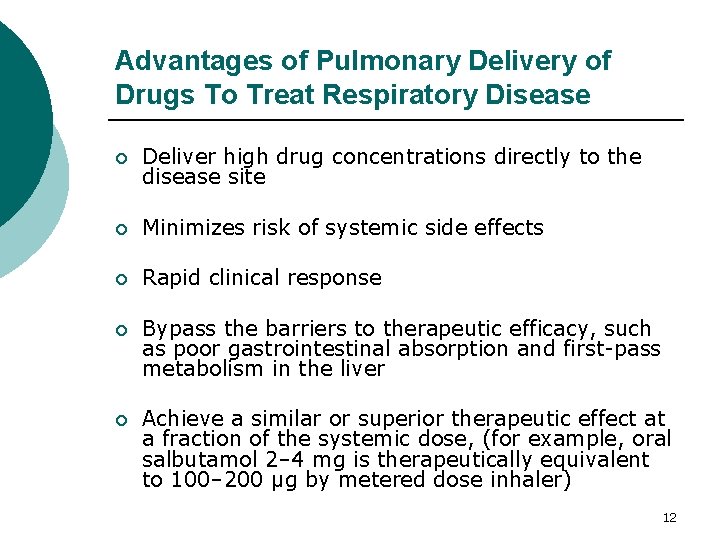
Advantages of Pulmonary Delivery of Drugs To Treat Respiratory Disease ¡ Deliver high drug concentrations directly to the disease site ¡ Minimizes risk of systemic side effects ¡ Rapid clinical response ¡ Bypass the barriers to therapeutic efficacy, such as poor gastrointestinal absorption and first-pass metabolism in the liver ¡ Achieve a similar or superior therapeutic effect at a fraction of the systemic dose, (for example, oral salbutamol 2– 4 mg is therapeutically equivalent to 100– 200 μg by metered dose inhaler) 12
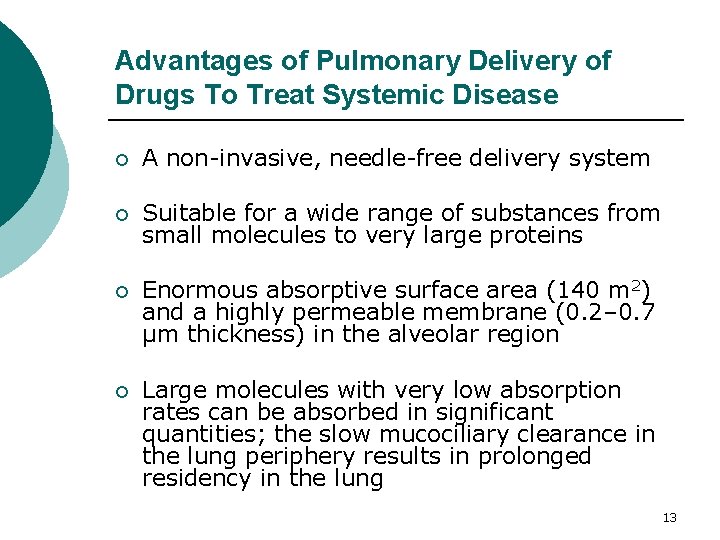
Advantages of Pulmonary Delivery of Drugs To Treat Systemic Disease ¡ A non-invasive, needle-free delivery system ¡ Suitable for a wide range of substances from small molecules to very large proteins ¡ Enormous absorptive surface area (140 m 2) and a highly permeable membrane (0. 2– 0. 7 μm thickness) in the alveolar region ¡ Large molecules with very low absorption rates can be absorbed in significant quantities; the slow mucociliary clearance in the lung periphery results in prolonged residency in the lung 13
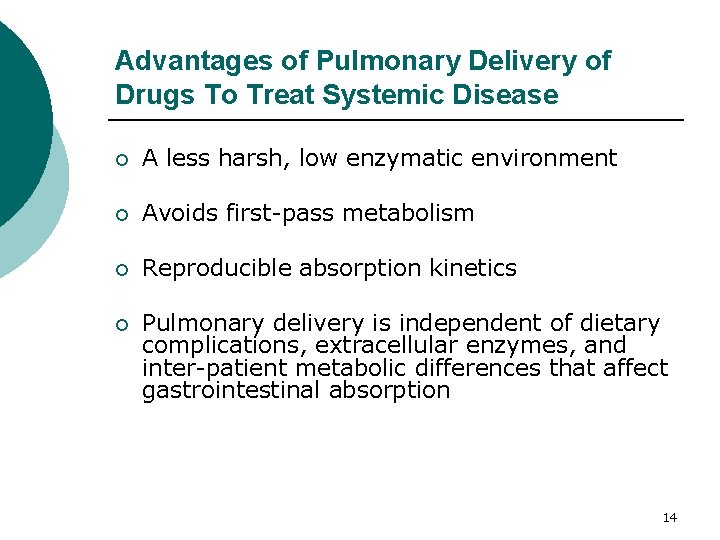
Advantages of Pulmonary Delivery of Drugs To Treat Systemic Disease ¡ A less harsh, low enzymatic environment ¡ Avoids first-pass metabolism ¡ Reproducible absorption kinetics ¡ Pulmonary delivery is independent of dietary complications, extracellular enzymes, and inter-patient metabolic differences that affect gastrointestinal absorption 14
Pulmonary absorptive surfaces ¡ The airways (the trachea, bronchi and bronchioles) are composed of a gradually thinning columnar epithelium populated by many mucus and ciliated cells that collectively form the mucociliary escalator ¡ The airways bifurcate roughly 16– 17 times before the alveoli are reached ¡ Inhaled insoluble particles that deposit in the airways are efficiently swept up and out of the lungs in moving patches of mucus, and for those deposited in the deepest airways this can be over a time period of about 24 hour 15
Pulmonary absorptive surfaces ¡ The monolayer that makes up the alveolar epithelium is completely different. The tall columnar mucus and cilia cells are replaced primarily (>95% of surface) by the very broad and extremely thin (<0. 1 µm in places) type 1 cells ¡ Distributed in the corners of the alveolar sacs are also the progenitor cells for the type 1 cells and the producers of lung surfactant, the type 2 cells ¡ The air-side surface of each of the 500 million alveoli in human lungs is routinely 'patrolled' by 12– 14 alveolar macrophages, which engulf and try to digest any insoluble particles that deposit 16 in the alveoli
Pulmonary absorptive surfaces ¡ An excess of 90% of alveolar macrophages are located at or near alveolar septal junctional zones ¡ Insoluble, non-digestible particles that deposit in the alveoli can reside in the lungs for years, usually sequestered within macrophages ¡ Molecules such as insulin are formulated either as liquids or in highly water-soluble aerosol particles that dissolve rapidly in the lungs and thereby largely avoid macrophage degradation 17
Pulmonary absorptive surfaces ¡ Protein therapeutics that are taken up by macrophages can be rapidly destroyed in the lysosomal 'guts' of the phagocytic cells 18
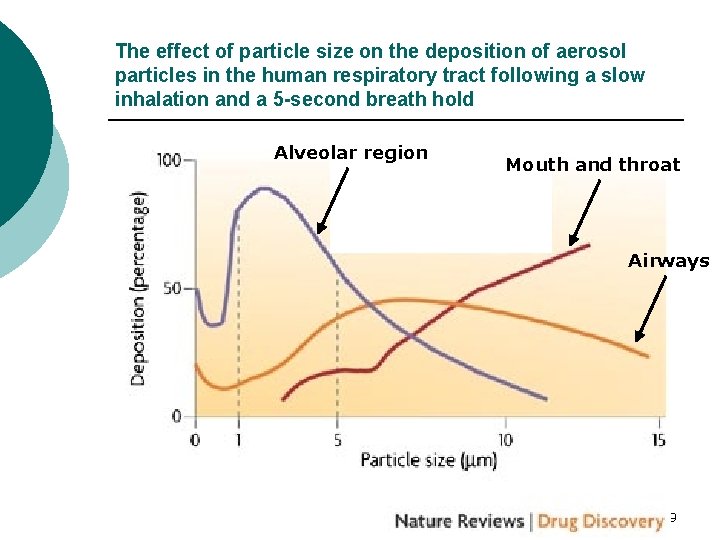
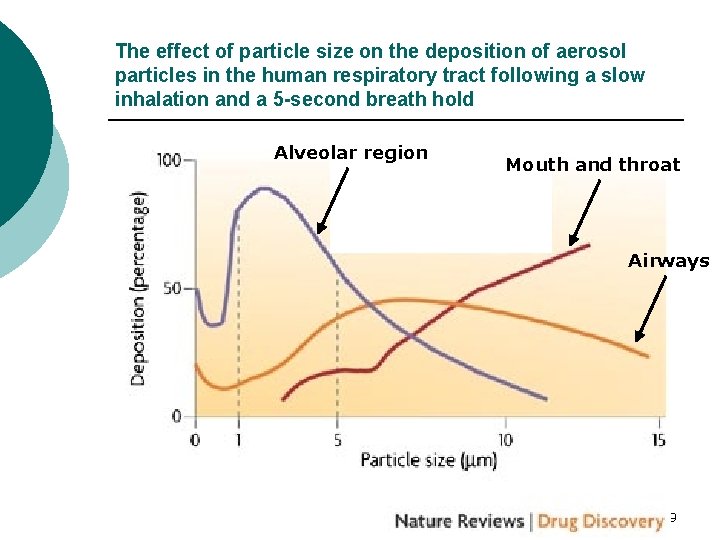
The effect of particle size on the deposition of aerosol particles in the human respiratory tract following a slow inhalation and a 5 -second breath hold Alveolar region Mouth and throat Airways 19
Systemic delivery of small hydrophobic molecules ¡ Small, mildly hydrophobic molecules can show extremely rapid absorption kinetics from the lungs ¡ However, as hydrophobicity increases, molecules can become too insoluble for rapid absorption and can persist in the lungs for hours, days or weeks ¡ Typical drug molecules with log octanol–water partition coefficients greater than 1 can be expected to be absorbed, with absorption halflives (the time it takes half of the molecules deposited into the lungs to disappear from the tissue) of approximately 1 minute or so; decreasing the log octanol–water partition coefficient to – 1 or lower can increase the half-life to around 60 minutes 20
Systemic delivery of small hydrophobic molecules ¡ Examples of rapidly absorbed inhaled hydrophobic drugs include nicotine, 9 -tetrahydrocannabinol (THC), morphine and fentanyl 21
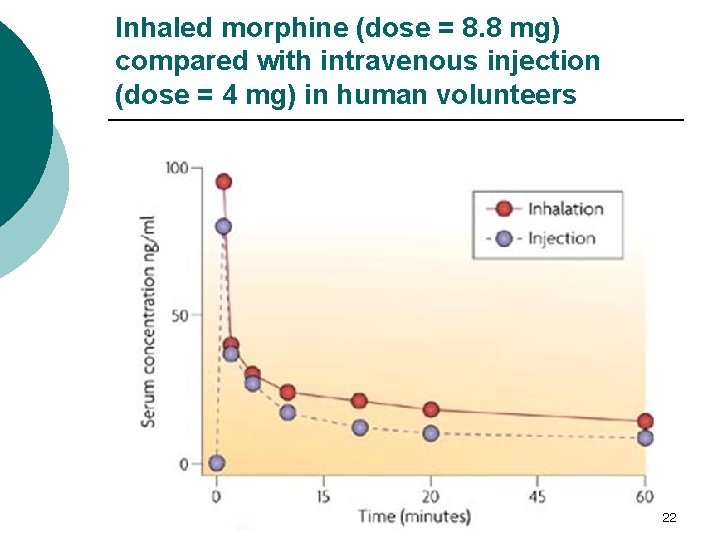
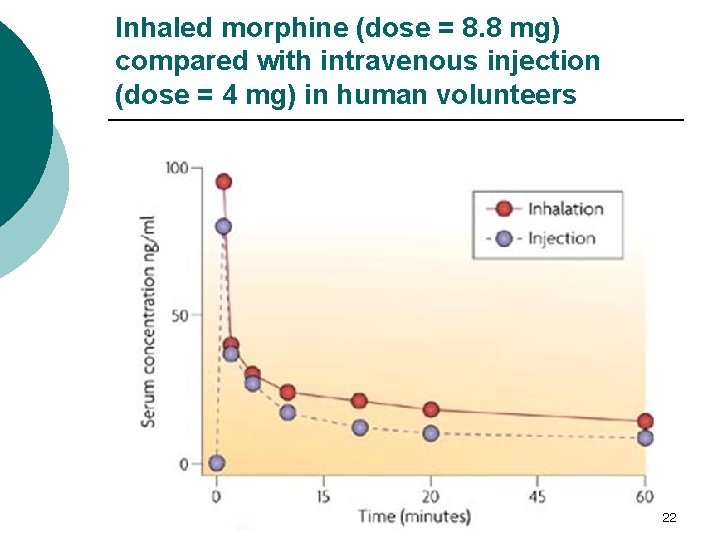
Inhaled morphine (dose = 8. 8 mg) compared with intravenous injection (dose = 4 mg) in human volunteers 22
Systemic delivery of small hydrophilic molecules ¡ In general, neutral or negatively charged hydrophilic small molecules are absorbed rapidly and with high bioavailabilities from the lungs ¡ This class of molecules has an average absorption half-life of about 60 minutes, in contrast to some of the lipophilic molecules that are absorbed in seconds to minutes 23
24
Systemic delivery of macromolecules ¡ The use of the lungs for the delivery of peptides and proteins, which otherwise must be injected, is one of the most exciting new areas in pulmonary delivery ¡ For reasons that are not completely understood, the lungs provide higher bioavailabilities for macromolecules than any other non-invasive route of delivery ¡ However, unlike the situation with small molecules, for which lung metabolism is minimal, enzymatic hydrolysis of small natural peptides can be very high unless they are chemically engineered (blocked) to inhibit peptidases 25
Systemic delivery of macromolecules ¡ Small natural peptides make poor drugs by any route of delivery because of peptidase sensitivity, whereas blocked peptides show high pulmonary bioavailabilities ¡ As molecular mass increases and peptides become proteins with greater tertiary and quaternary structure, peptidase hydrolysis is inhibited or even eliminated and bioavailabilities of natural proteins can be high ¡ Insulin can be considered to be a large peptide (or small protein), with enough size to avoid much of the metabolism seen with smaller peptides 26
Systemic delivery of macromolecules ¡ The rate of macromolecule absorption is primarily dictated by size — the larger the size the slower the absorption ¡ Molecules such as insulin, growth hormone and many cytokines typically peak in blood following aerosol inhalation in 30– 90 minutes, whereas smaller blocked peptides can be absorbed faster ¡ After a 15 -year development effort, inhaled human insulin (IHI) applied regularly at meal time has been approved both in the US and the European Union for the treatment of adults with diabetes (Exubera) 27
Systemic delivery of macromolecules ¡ Conjugation of molecules such as interferons, follicle stimulating hormone (FSH) and erythropoietin (EPO) to the constant (Fc) region of antibodies has been shown to prolong the systemic duration ¡ Interestingly, the optimal pulmonary site of absorption of these conjugates seems to be the conducting airways, in contrast to the major site for insulin, which is in the deep lung ¡ The airways are enriched with antibody transcytosis receptor mechanisms. Fc conjugates of proteins have serum half-lives >1 day and are believed to be absorbed with high bioavailabilities (20– 50%) from the lungs 28
Pulmonary Drug Delivery Devices ¡ Dry Powder Inhalation (DPI) Devices ¡ The Pressurized Metered-Dose Inhalation (p. MDI) Device ¡ Nebulizers 29
Dry Powder Inhalation (DPI) Devices ¡ DPIs are used to treat respiratory diseases such as asthma and COPD, systemic disorders such as diabetes, cancer, neurological diseases (including pain), and other pulmonary diseases such as cystic fibrosis and pulmonary infectious diseases ¡ Devices requiring the patient's inspiration effort to aerosolize the powder aliquot are called passive devices because as they do not provide an internal energy source ¡ Active devices provide different kinds of energy for aerosolization: kinetic energy by a loaded spring and compressed air or electric energy by a battery 30
Dry Powder Inhalation (DPI) Devices ¡ Most DPIs contain micronized drug blended with larger carrier particles, which prevents aggregation and promotes flow 31

Principle of dry powder inhaler design 32
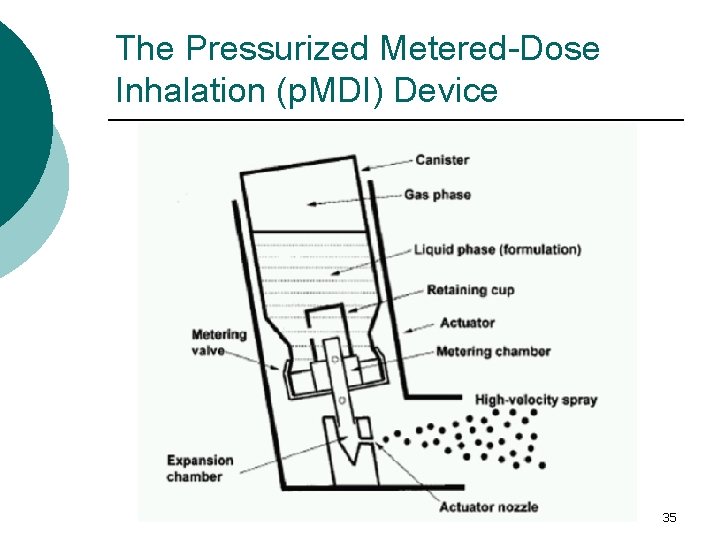
The Pressurized Metered-Dose Inhalation (p. MDI) Device ¡ The pressurized metered-dose inhalation (p. MDI) device was introduced to deliver asthma medications in a convenient and reliable multidose presentation ¡ The key components of the p. MDI device are: container, propellants, formulation, metering valve, and actuator ¡ The p. MDI container must withstand high pressure generated by the propellant. Stainless steel has been used as a p. MDI container material. Aluminum is now preferred because, compared to glass, it is lighter, more compact, less fragile, and light-proof 33
The Pressurized Metered-Dose Inhalation (p. MDI) Device ¡ Coatings on the internal container surfaces may be useful to prevent adhesion of drug particles and chemical degradation of drug ¡ Propellants in p. MDIs are liquefied, compressed gases that are in the gaseous phase at atmospheric pressure but form liquids when compressed ¡ They are required to be nontoxic, nonflammable, compatible with drugs formulated either as suspensions or solutions, and to have appropriate boiling points and densities 34
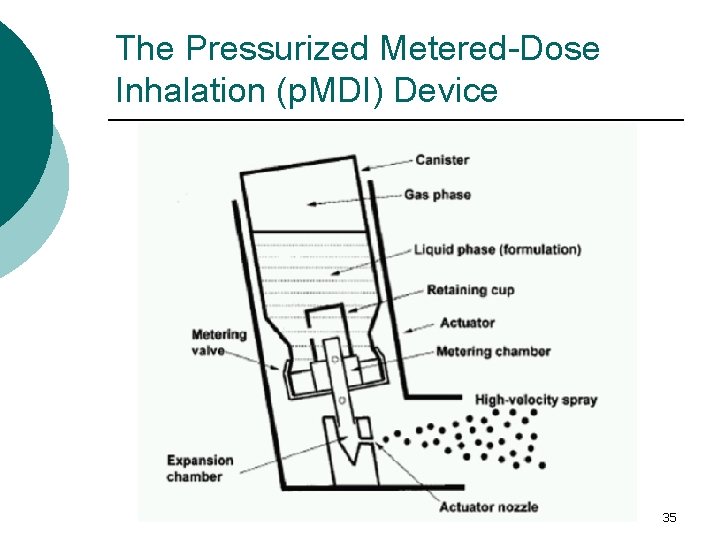
The Pressurized Metered-Dose Inhalation (p. MDI) Device 35
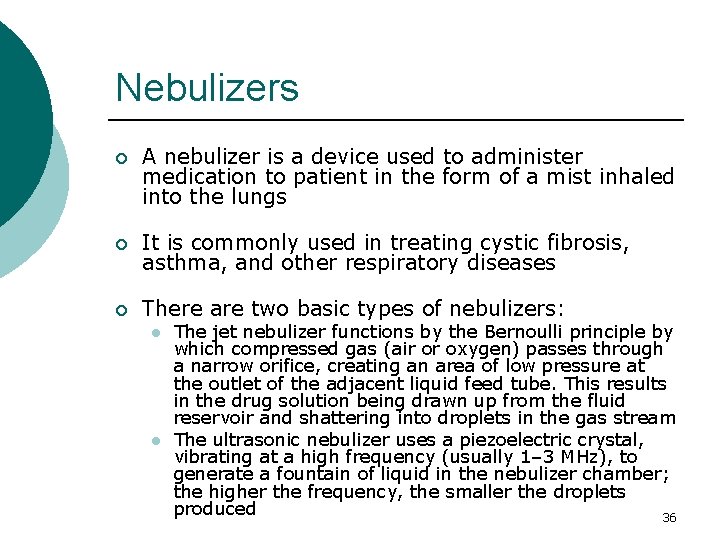
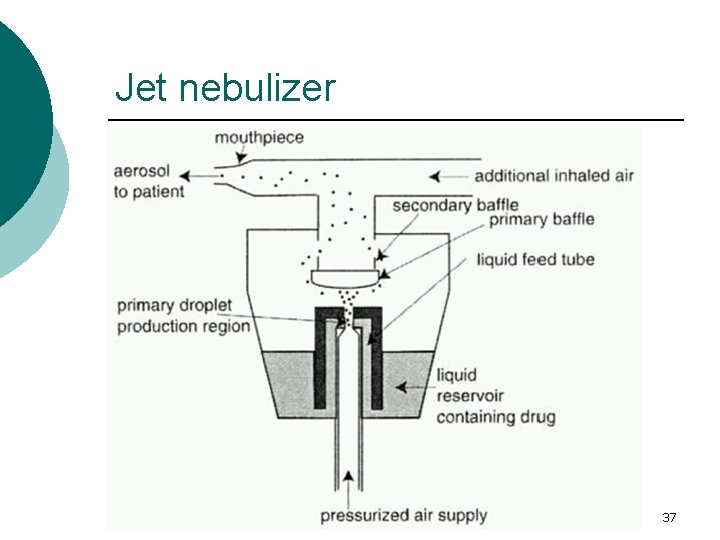
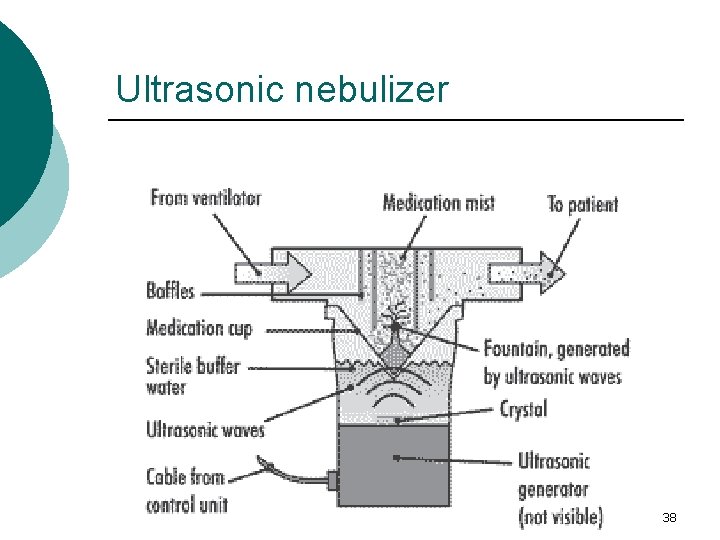
Nebulizers ¡ A nebulizer is a device used to administer medication to patient in the form of a mist inhaled into the lungs ¡ It is commonly used in treating cystic fibrosis, asthma, and other respiratory diseases ¡ There are two basic types of nebulizers: l l The jet nebulizer functions by the Bernoulli principle by which compressed gas (air or oxygen) passes through a narrow orifice, creating an area of low pressure at the outlet of the adjacent liquid feed tube. This results in the drug solution being drawn up from the fluid reservoir and shattering into droplets in the gas stream The ultrasonic nebulizer uses a piezoelectric crystal, vibrating at a high frequency (usually 1– 3 MHz), to generate a fountain of liquid in the nebulizer chamber; the higher the frequency, the smaller the droplets produced 36
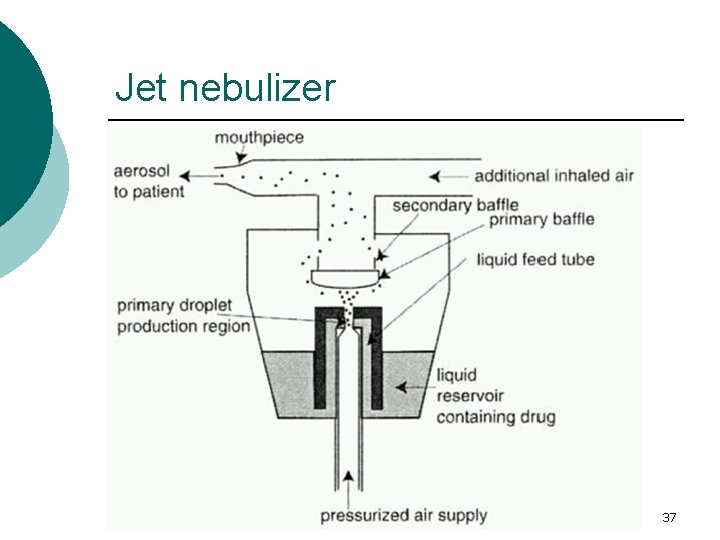
Jet nebulizer 37
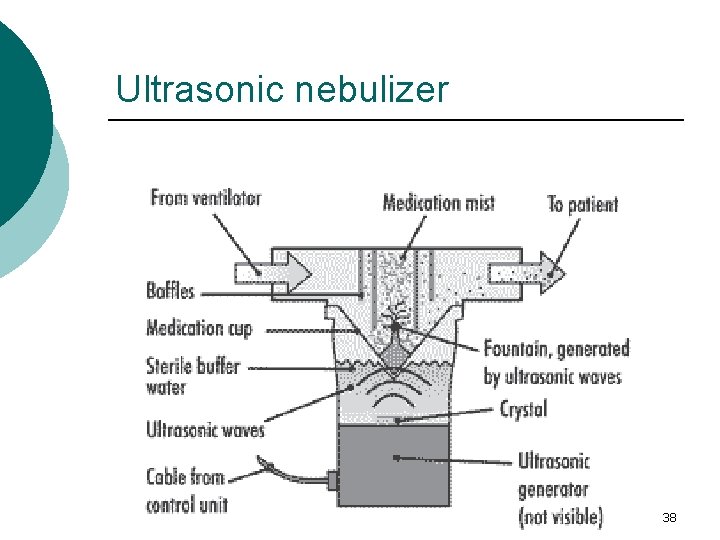
Ultrasonic nebulizer 38
39
 Types of adulteration of crude drugs
Types of adulteration of crude drugs Issa san francisco
Issa san francisco Estimating earthwork quantities
Estimating earthwork quantities Issa associates degree
Issa associates degree Opt notre dame
Opt notre dame Nabil baki
Nabil baki Issa saleh
Issa saleh White sheep white sheep on a blue hill meaning
White sheep white sheep on a blue hill meaning Richy carrasco
Richy carrasco Issa raleigh
Issa raleigh Issa tb 109
Issa tb 109 Carotenmia
Carotenmia Issa ottawa
Issa ottawa Ghassan issa
Ghassan issa Amanda issa
Amanda issa Pay palaccount
Pay palaccount Ocusert adalah
Ocusert adalah Diffusion controlled modified release system consists of
Diffusion controlled modified release system consists of New drug delivery system
New drug delivery system Rate limiting steps in drug absorption
Rate limiting steps in drug absorption Transdermal drug delivery system
Transdermal drug delivery system Dosage forms and drug delivery systems
Dosage forms and drug delivery systems Punch method capsules
Punch method capsules Parenteral dosage form example
Parenteral dosage form example Laila hammoud
Laila hammoud Mohammad sadegh rasooli
Mohammad sadegh rasooli Mohammad diab md
Mohammad diab md Mohammad ali javidian
Mohammad ali javidian Sumbangan mohammad eunos abdullah sejarah
Sumbangan mohammad eunos abdullah sejarah Mohammad arjomand
Mohammad arjomand Mohammad sharifkhani
Mohammad sharifkhani Dr elham altaf
Dr elham altaf Mohammad alipour
Mohammad alipour Mohammad sharifkhani
Mohammad sharifkhani Dr nur mohammad hadi zahalan
Dr nur mohammad hadi zahalan Dr mohammad aman
Dr mohammad aman Mohammad ridwan bkn
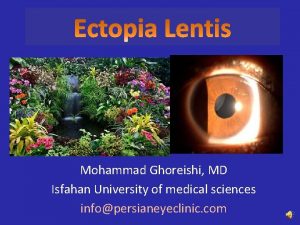
Mohammad ridwan bkn Mohammad ghoreishi
Mohammad ghoreishi Shaik mohammad tajuddin
Shaik mohammad tajuddin Mohammad ali abtahi
Mohammad ali abtahi