Pulmonary Conditions Pathology Amanda Sivic Objectives Pathology Chronic
Pulmonary Conditions Pathology Amanda Sivic
Objectives • Pathology • • • Chronic Obstructive Pulmonary Disease Pneumonia Pulmonary Edema Pulmonary Fibrosis Bronchiectasis • Research Summary • Effectiveness of Controlled Breathing Techniques on Anxiety and Depression in Hospitalized Patients With COPD: A Randomized Clinical Trial
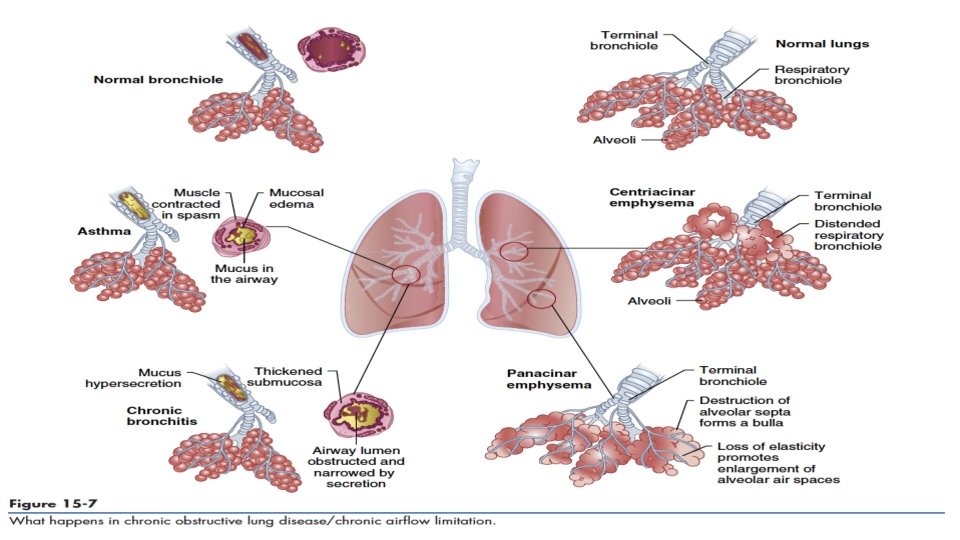
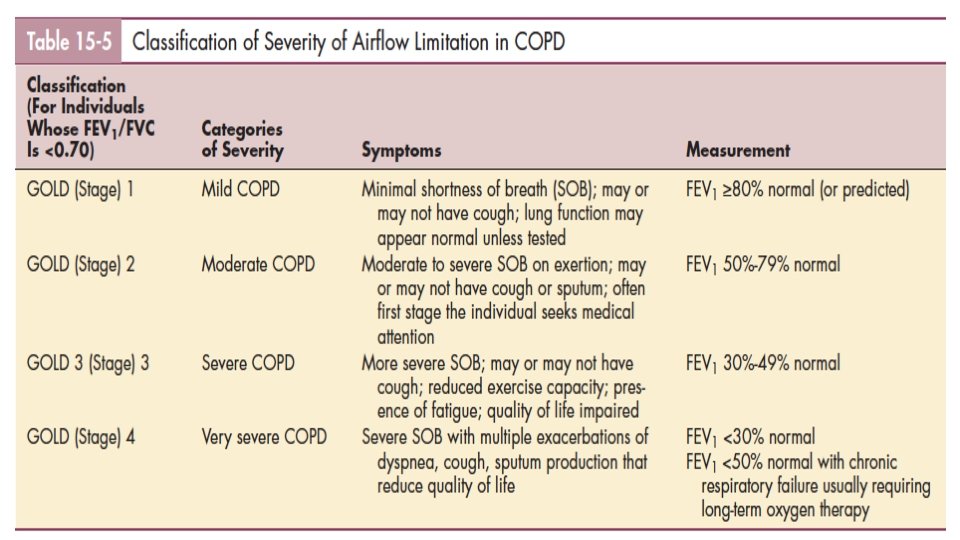
Chronic Obstructive Pulmonary Disease • Structural airway changes with inflammation cause airway narrowing and decreased expiratory flow • Air that can’t escape during expiration is trapped, resulting in hyperinflation and an increase in functional residual capacity • An increase in functional residual capacity reduces the volume of air available for inspiration during activities, resulting in shortness of breath
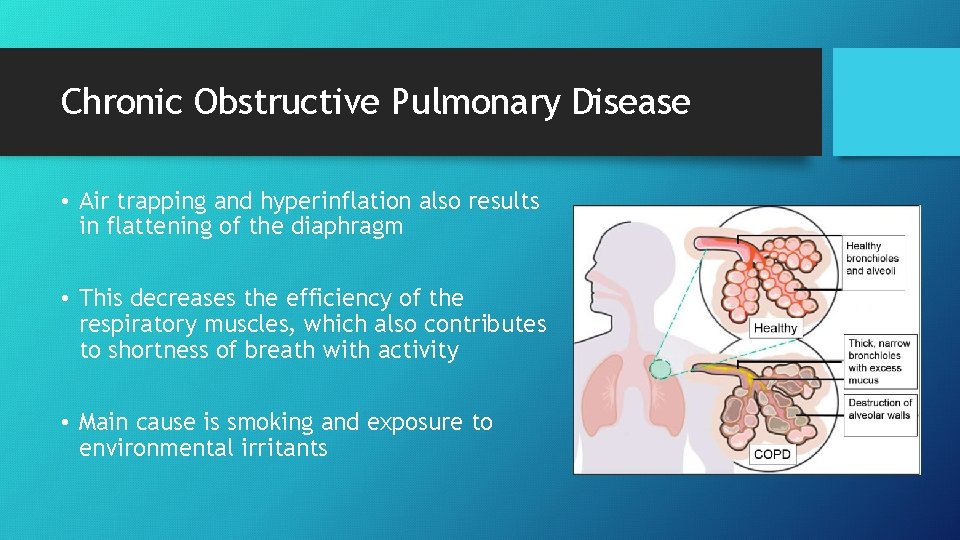
Chronic Obstructive Pulmonary Disease • Air trapping and hyperinflation also results in flattening of the diaphragm • This decreases the efficiency of the respiratory muscles, which also contributes to shortness of breath with activity • Main cause is smoking and exposure to environmental irritants
Pneumonia • Inflammation and edema cause the alveoli and bronchioles to fill with fluid and mucus so that air cannot enter the alveoli • Gas exchange is impaired, leading to shortness of breath • Production of interleukin and tumor necrosis factor by alveolar macrophages can contribute to the effects of pneumonia such as fever, chills, and malaise
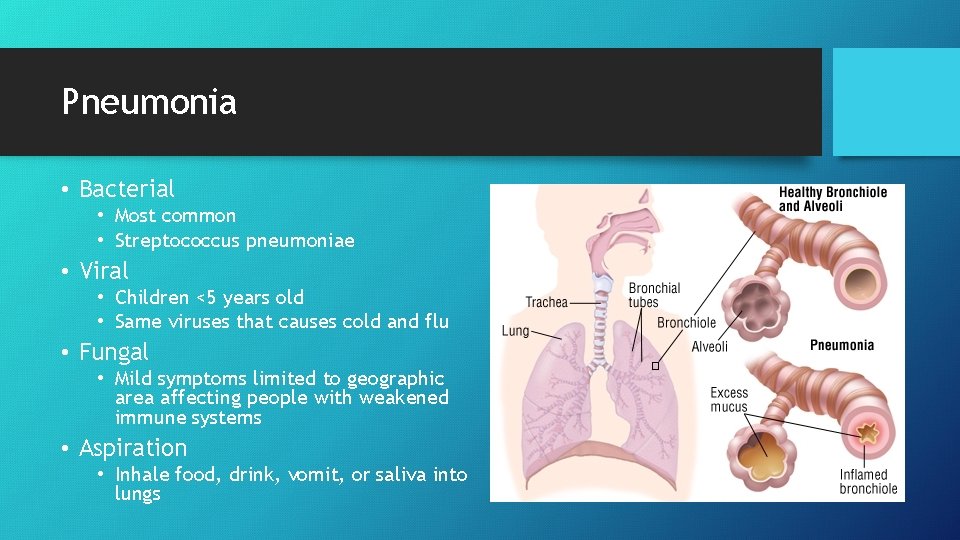
Pneumonia • Bacterial • Most common • Streptococcus pneumoniae • Viral • Children <5 years old • Same viruses that causes cold and flu • Fungal • Mild symptoms limited to geographic area affecting people with weakened immune systems • Aspiration • Inhale food, drink, vomit, or saliva into lungs
Pulmonary Edema • Pulmonary vasculature fills with fluid that leaks into the alveolar spaces and decreases the space available for gas exchange, leading to shortness of breath • Commonly caused by CHF when the heart is not able to pump efficiently, blood can back up into the veins that take blood through the lungs • As the pressure in these blood vessels increases fluid is pushed into the alveolar spaces in the lungs, impairing normal oxygen movement
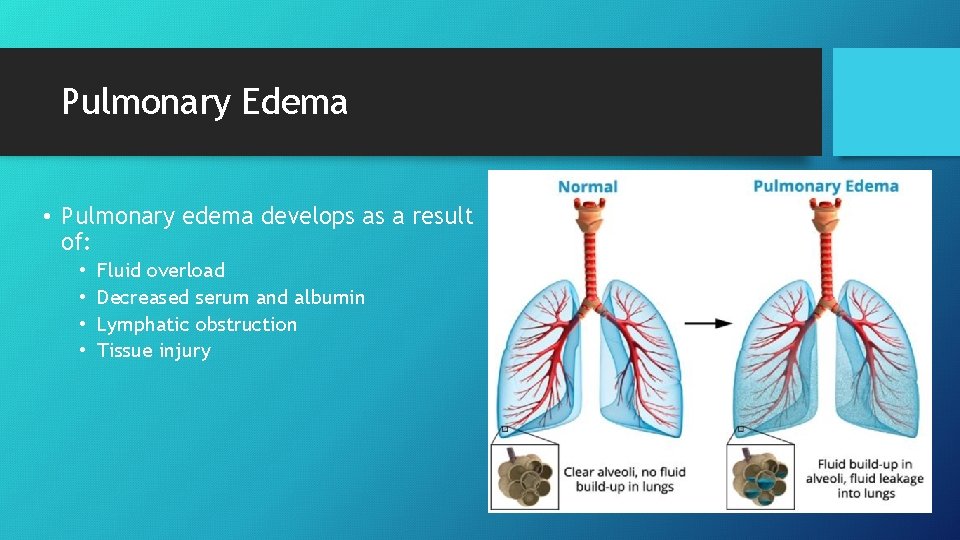
Pulmonary Edema • Pulmonary edema develops as a result of: • • Fluid overload Decreased serum and albumin Lymphatic obstruction Tissue injury
Pulmonary Fibrosis • Fibrosis irreversibly distorts and shrinks the lung lobe at the alveolar level • Abnormal wound healing occurs when dense fibrous connective tissue replaces lung tissue • The fibrous tissue stiffens the lungs, reduces space for inhaled air, and interferes with gas exchange
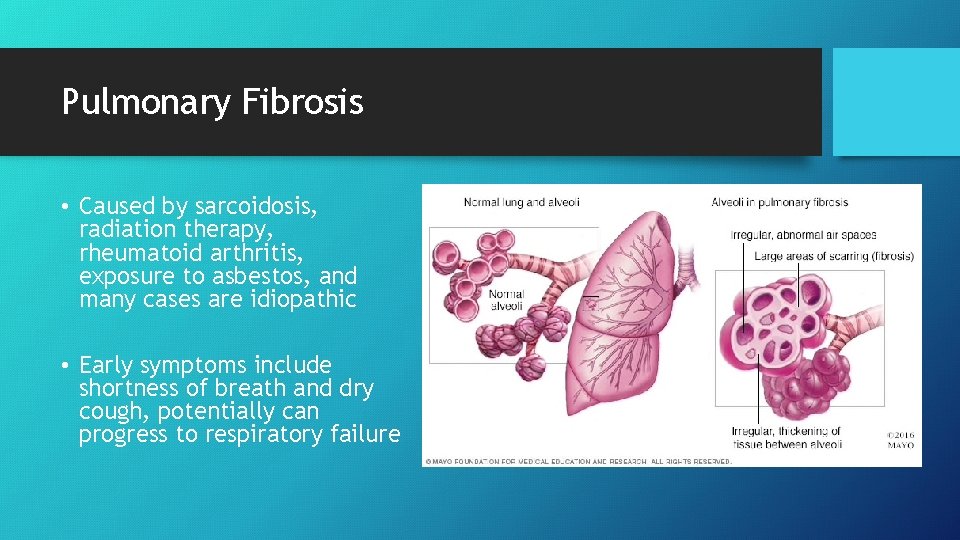
Pulmonary Fibrosis • Caused by sarcoidosis, radiation therapy, rheumatoid arthritis, exposure to asbestos, and many cases are idiopathic • Early symptoms include shortness of breath and dry cough, potentially can progress to respiratory failure
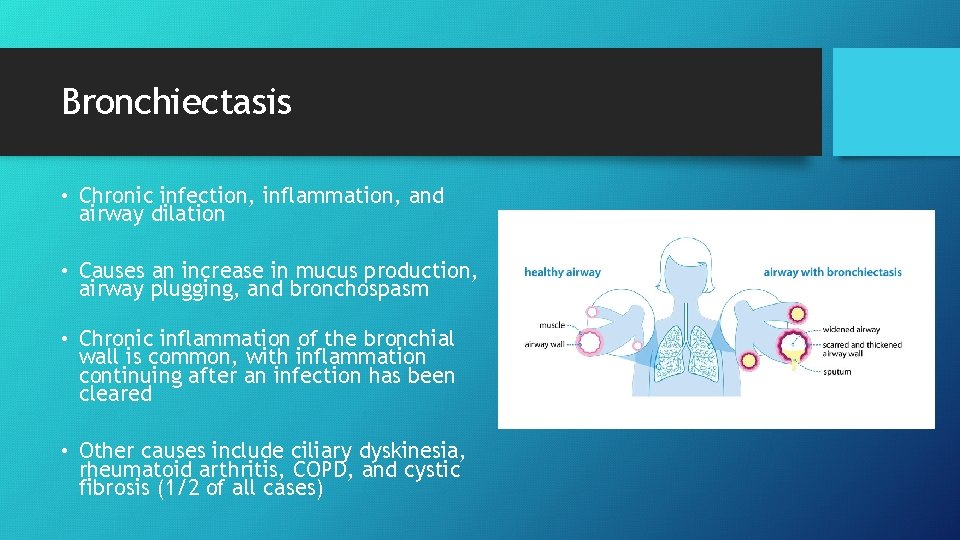
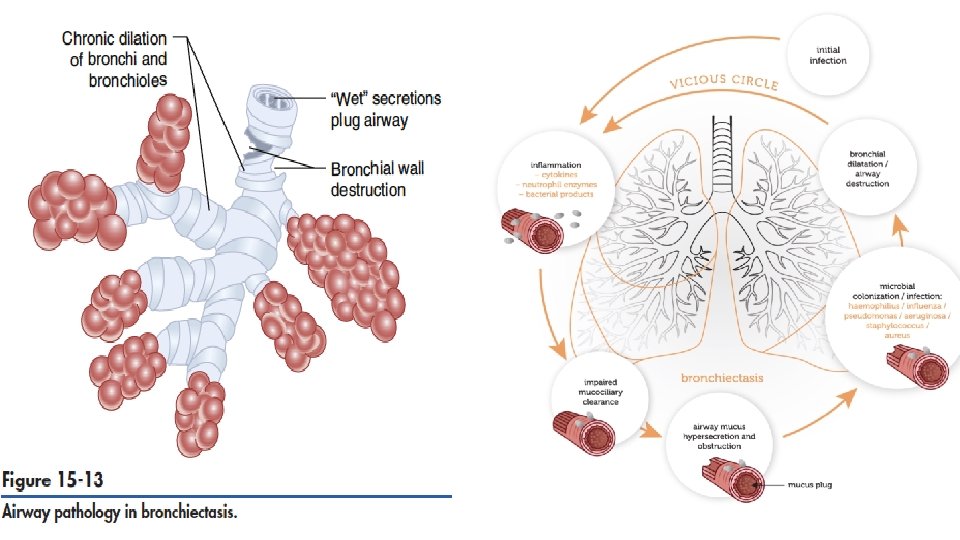
Bronchiectasis • Chronic infection, inflammation, and airway dilation • Causes an increase in mucus production, airway plugging, and bronchospasm • Chronic inflammation of the bronchial wall is common, with inflammation continuing after an infection has been cleared • Other causes include ciliary dyskinesia, rheumatoid arthritis, COPD, and cystic fibrosis (1/2 of all cases)
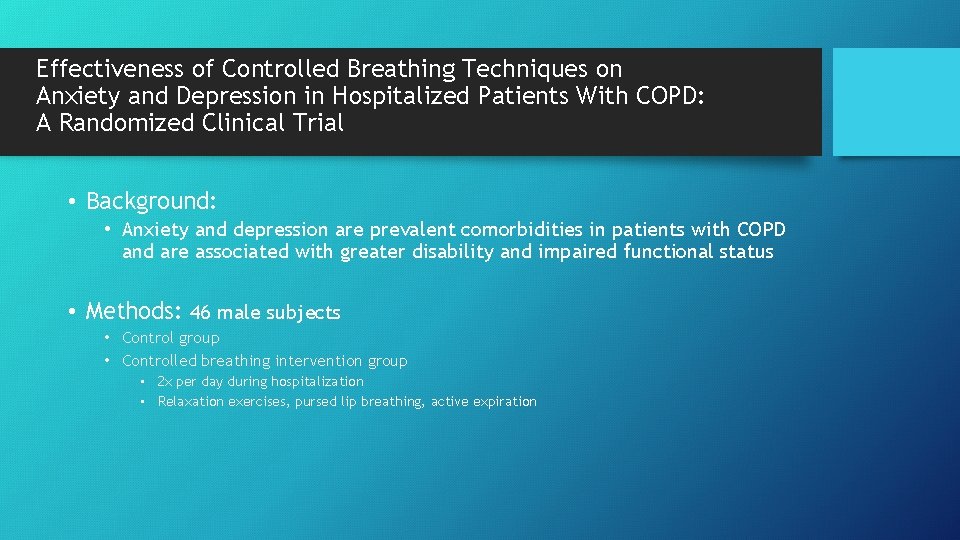
Effectiveness of Controlled Breathing Techniques on Anxiety and Depression in Hospitalized Patients With COPD: A Randomized Clinical Trial • Background: • Anxiety and depression are prevalent comorbidities in patients with COPD and are associated with greater disability and impaired functional status • Methods: 46 male subjects • Control group • Controlled breathing intervention group • 2 x per day during hospitalization • Relaxation exercises, pursed lip breathing, active expiration
Measures • Baseline and Post-Intervention • Dyspnea • Anxiety and depression • Quality of life (with the St George’s Respiratory Questionnaire and the European Quality of Life Questionnaire) • Maximum inspiratory and expiratory pressure • Hand-grip strength • Sleep quality

Results/Conclusions • Controlled breathing techniques significantly improved dyspnea, anxiety, and mobility • All the measured variables improved in the intervention group • The control group had poorer values in all the variables after the hospitalization period • Controlled breathing exercises improve anxiety and depression in patients hospitalized for COPD exacerbation
References 1. Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist, 4 th ed. St. Louis, Missouri: Elsevier; 2016. 2. Valenza MC, Valenza-Pena G, Torres-Sanchez I, Gonzalez. Jimenez E, Conde-Valero A, Valenza-Demet G. Effectiveness of Controlled Breathing Techniques on Anxiety and Depression in Hospitalized Patients With COPD: A Randomized Clinical Trial. Respiratory Care. 2014; 59(2): 209 -215.
- Slides: 18