Pulmonary Alterations Pleural Effusion Pleurisy Pleural Effusion Excessive
- Slides: 31
Pulmonary Alterations Pleural Effusion & Pleurisy
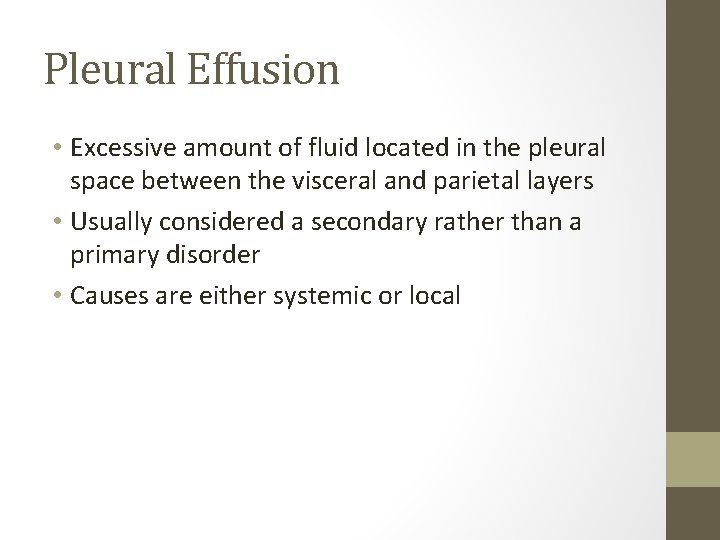
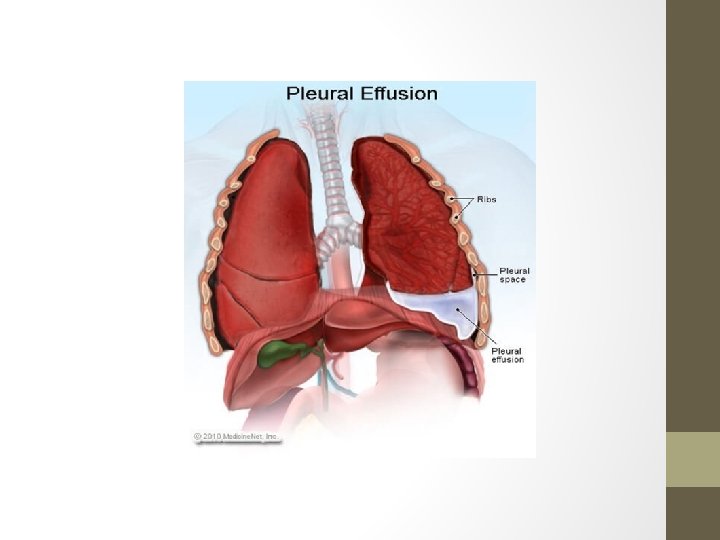
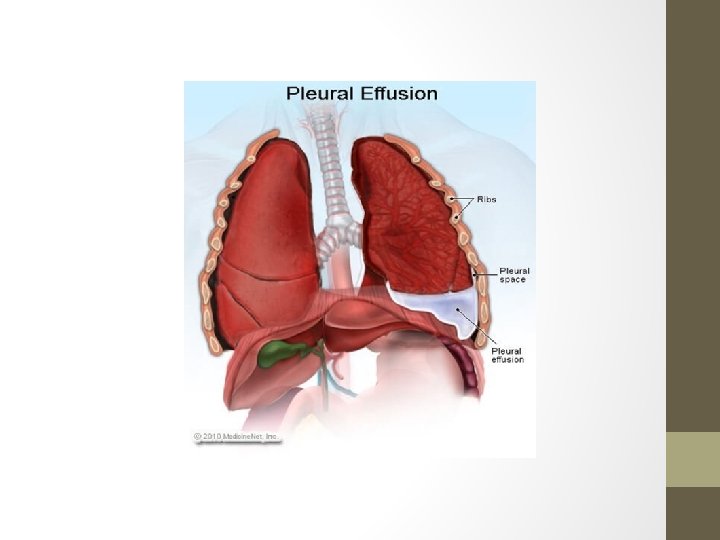
Pleural Effusion • Excessive amount of fluid located in the pleural space between the visceral and parietal layers • Usually considered a secondary rather than a primary disorder • Causes are either systemic or local
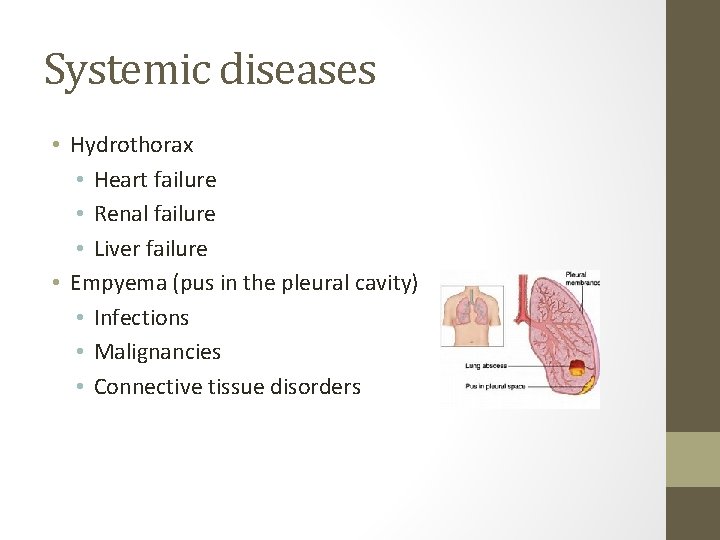
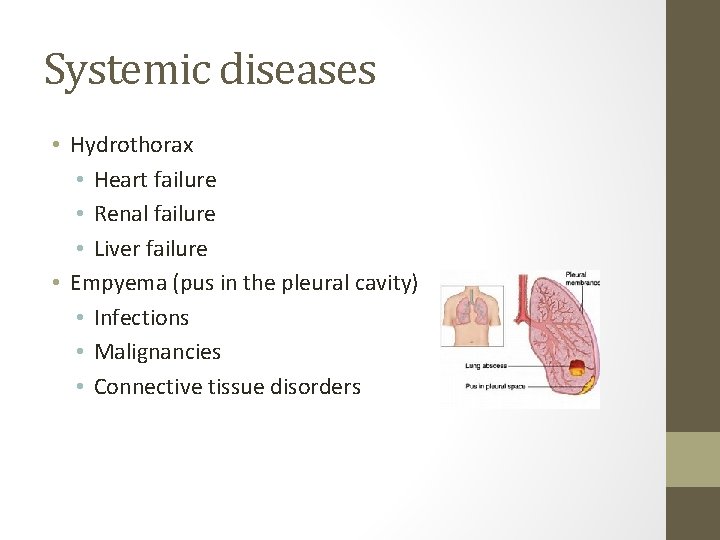
Systemic diseases • Hydrothorax • Heart failure • Renal failure • Liver failure • Empyema (pus in the pleural cavity) • Infections • Malignancies • Connective tissue disorders
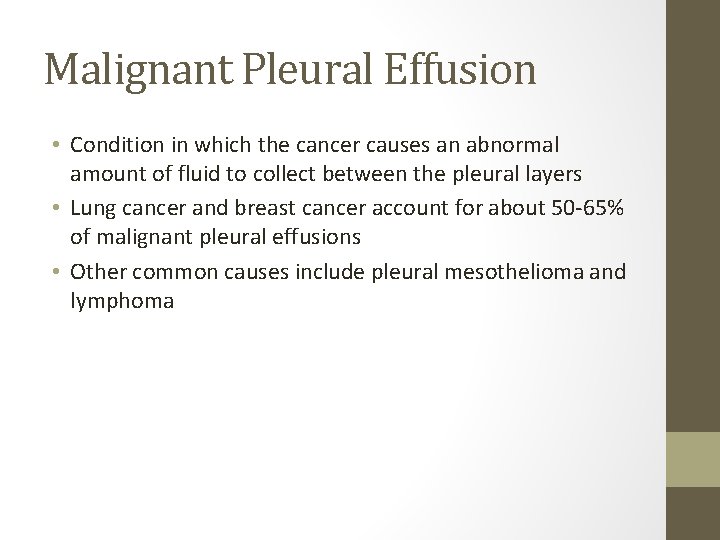
Malignant Pleural Effusion • Condition in which the cancer causes an abnormal amount of fluid to collect between the pleural layers • Lung cancer and breast cancer account for about 50 -65% of malignant pleural effusions • Other common causes include pleural mesothelioma and lymphoma
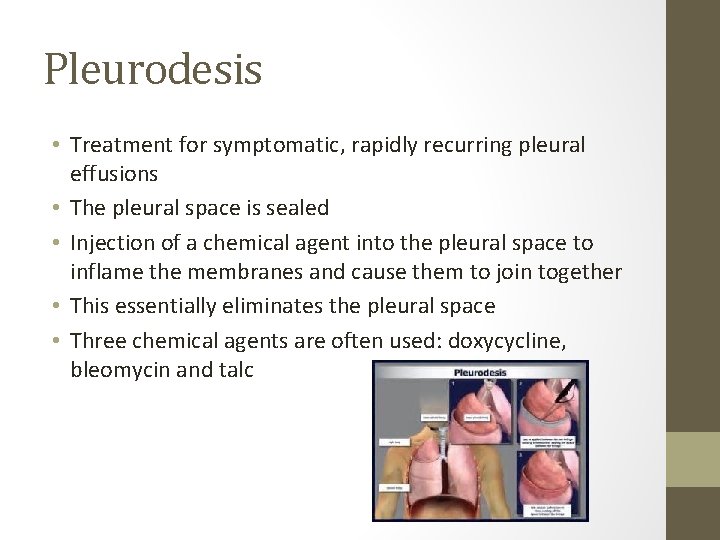
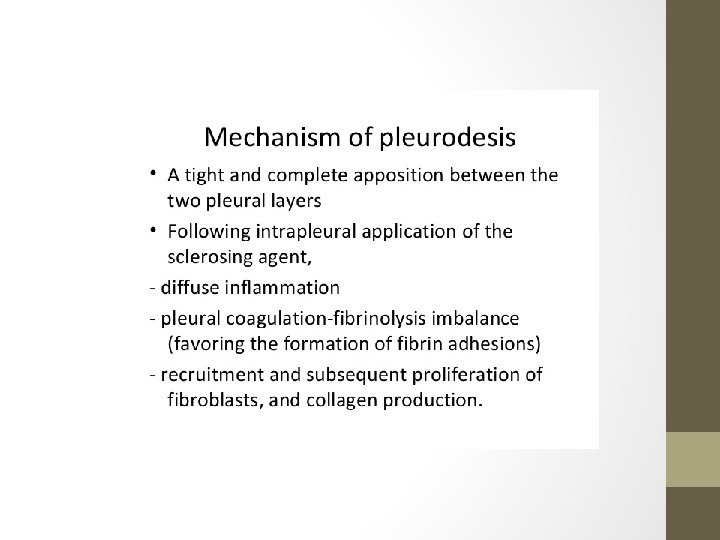
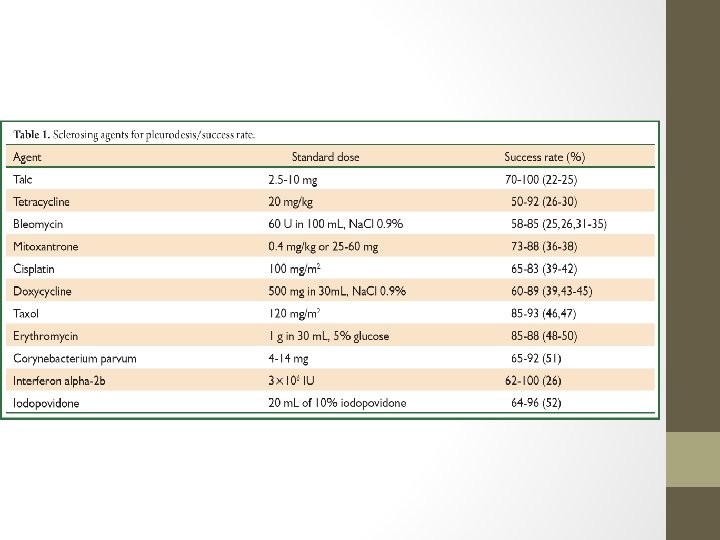
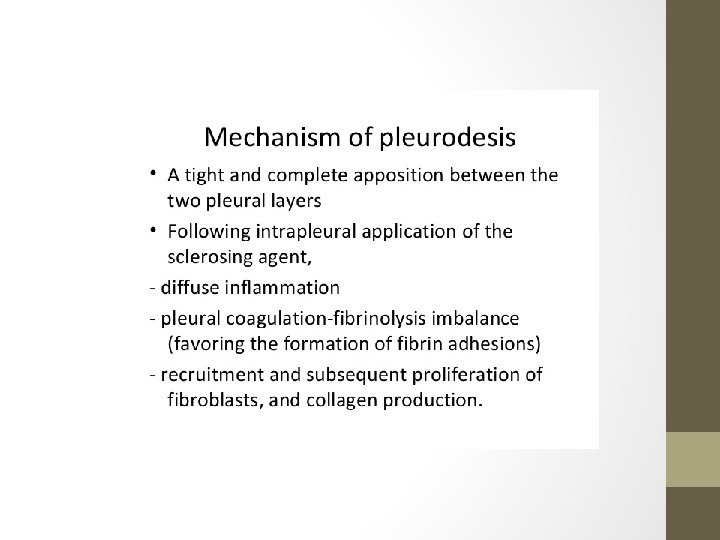
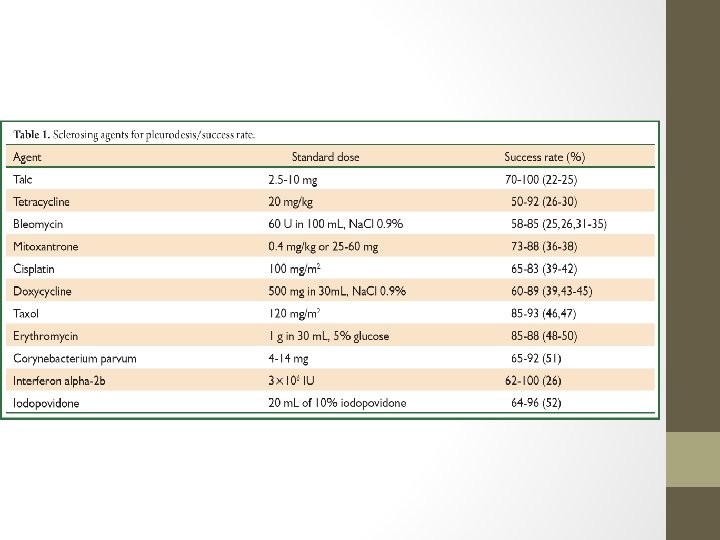
Pleurodesis • Treatment for symptomatic, rapidly recurring pleural effusions • The pleural space is sealed • Injection of a chemical agent into the pleural space to inflame the membranes and cause them to join together • This essentially eliminates the pleural space • Three chemical agents are often used: doxycycline, bleomycin and talc
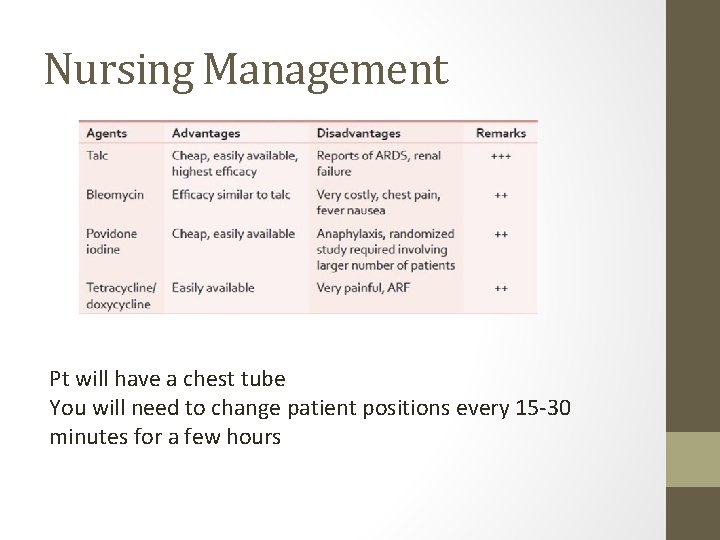
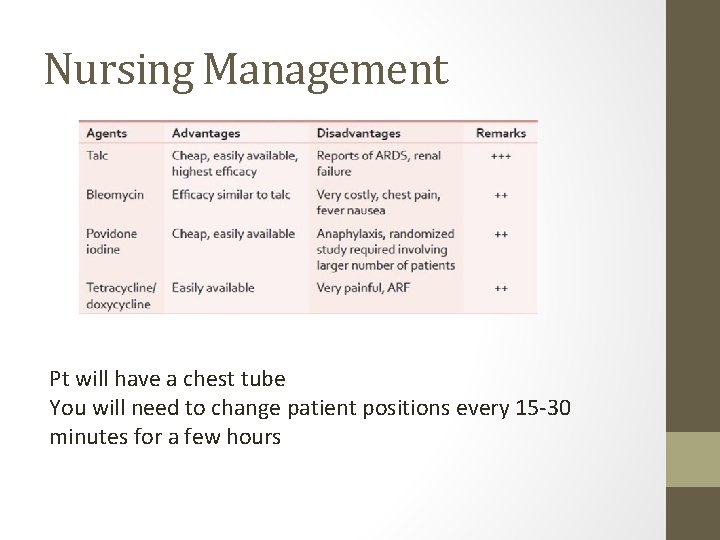
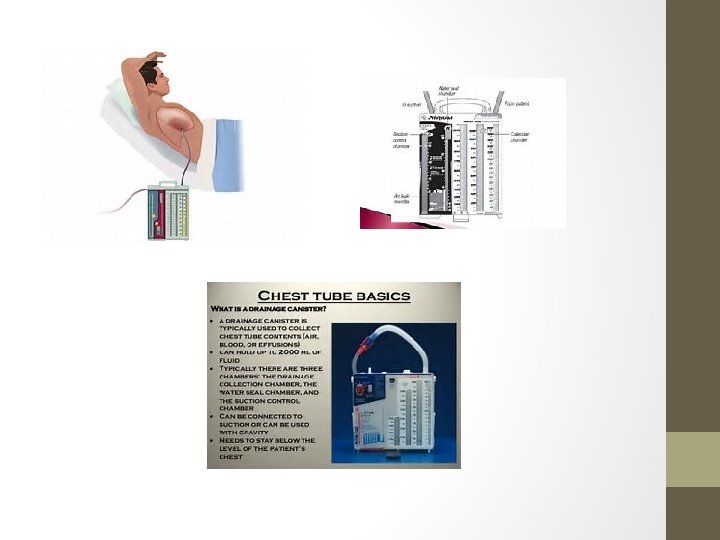
Nursing Management Pt will have a chest tube You will need to change patient positions every 15 -30 minutes for a few hours
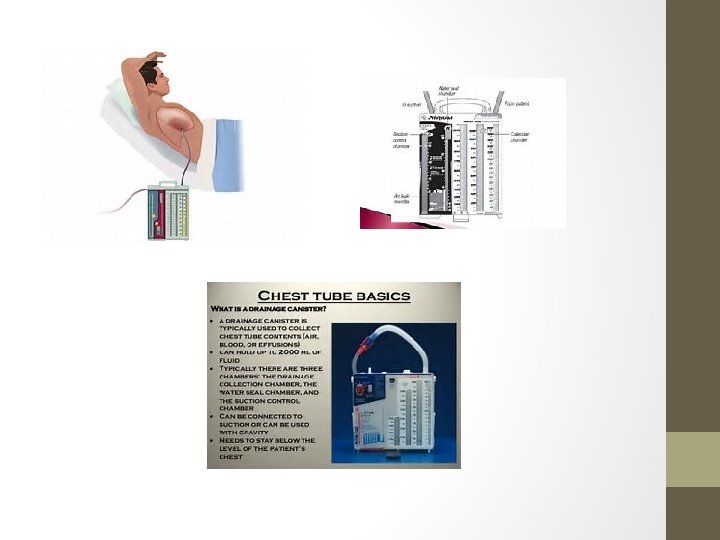
Nursing Management of Chest Tube • Make sure there are clamps at the bedside • Monitor water levels in the water-seal and suction-control chambers • Water in both chambers evaporates, so be sure to add water periodically to maintain the water-seal and suction levels
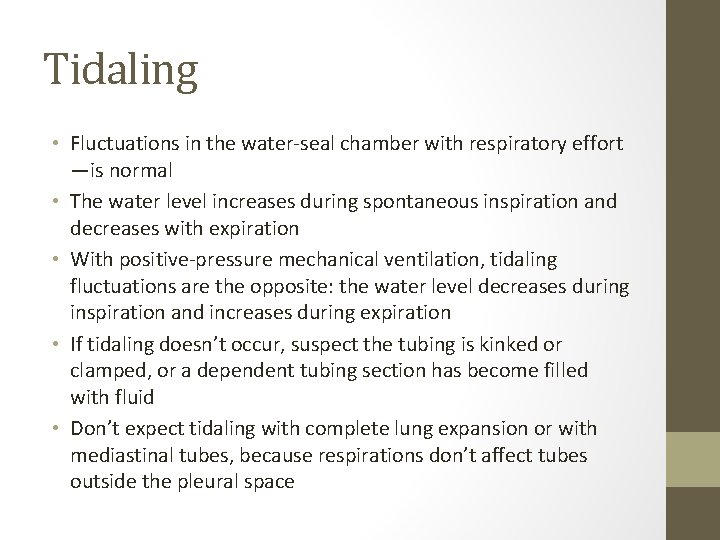
Tidaling • Fluctuations in the water-seal chamber with respiratory effort —is normal • The water level increases during spontaneous inspiration and decreases with expiration • With positive-pressure mechanical ventilation, tidaling fluctuations are the opposite: the water level decreases during inspiration and increases during expiration • If tidaling doesn’t occur, suspect the tubing is kinked or clamped, or a dependent tubing section has become filled with fluid • Don’t expect tidaling with complete lung expansion or with mediastinal tubes, because respirations don’t affect tubes outside the pleural space
Local diseases • Hemothorax • Chest wall injuries • Surgery to the chest • Chylothorax • the presence of lymphatic fluid in the pleural space secondary to leakage from the thoracic duct or one of its main tributaries • Trauma or surgery • Inflammation • Pneumonia • TB • Malignancy
Pathophysiology • Increase in hydrostatic pressure in the pleural capillaries or decreased colloid osmotic pressure in the circulatory system that can lead to excess pleural fluid (transudate) Or • An increased capillary permeability as a result of inflammation, infection, or malignancy (exudate)
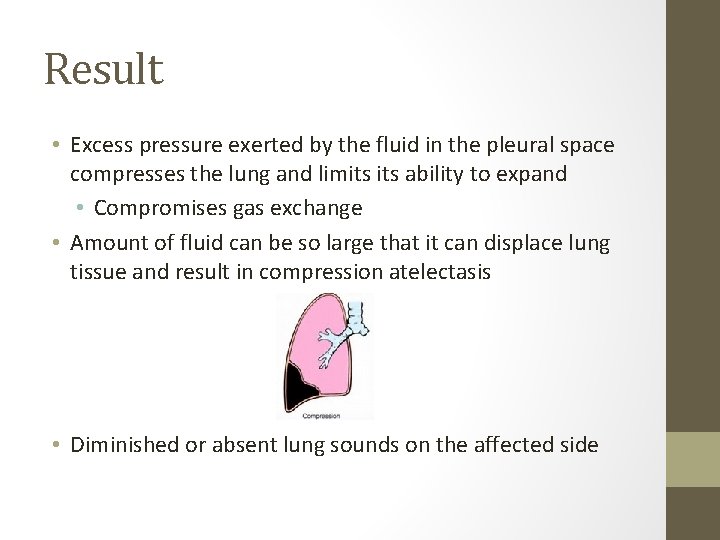
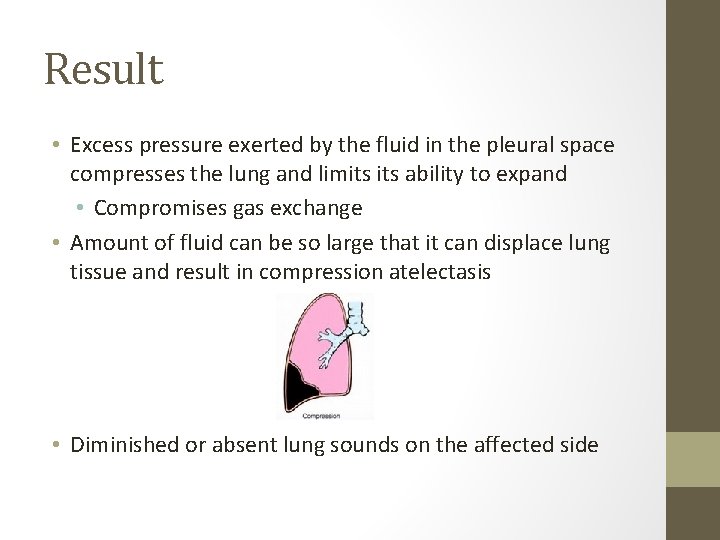
Result • Excess pressure exerted by the fluid in the pleural space compresses the lung and limits ability to expand • Compromises gas exchange • Amount of fluid can be so large that it can displace lung tissue and result in compression atelectasis • Diminished or absent lung sounds on the affected side
Signs and Symptoms • • • Dyspnea Diminished or absent breath sounds on the affected side Pain Limited chest wall movement Low oxygen sats
Assessment Symptom analysis of pain c/o dyspnea Coughing Elevated temperature Respiratory rate and status • Shallow respirations • Asymmetry • Lung sounds • Diminished • Absent • • •
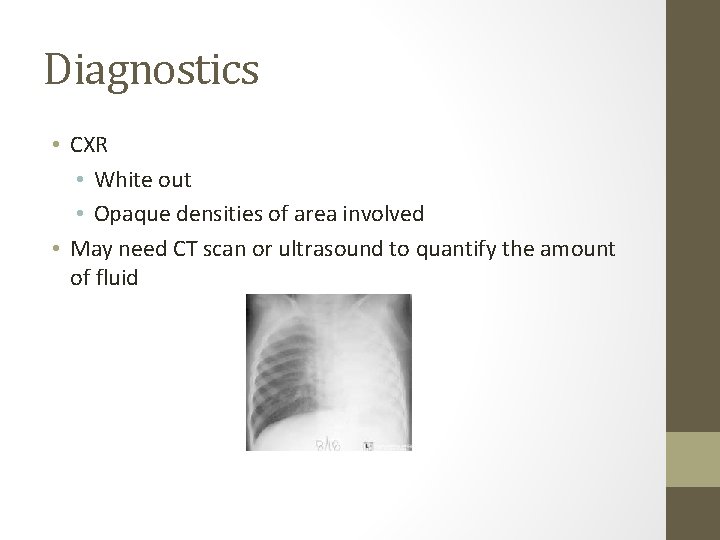
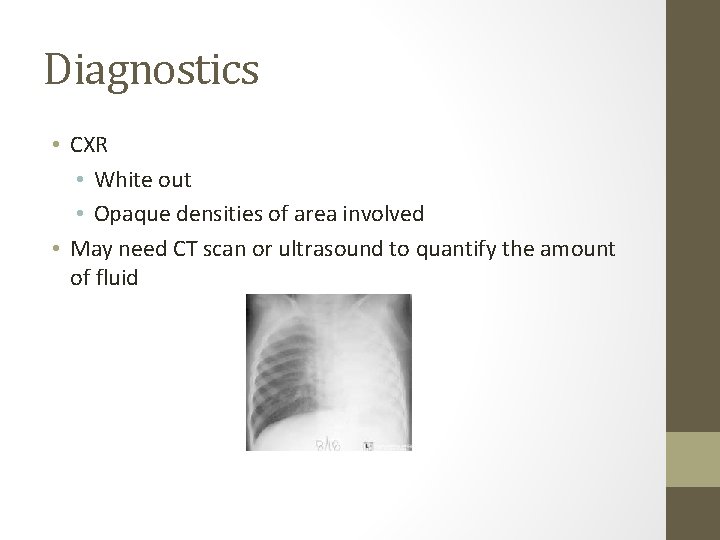
Diagnostics • CXR • White out • Opaque densities of area involved • May need CT scan or ultrasound to quantify the amount of fluid
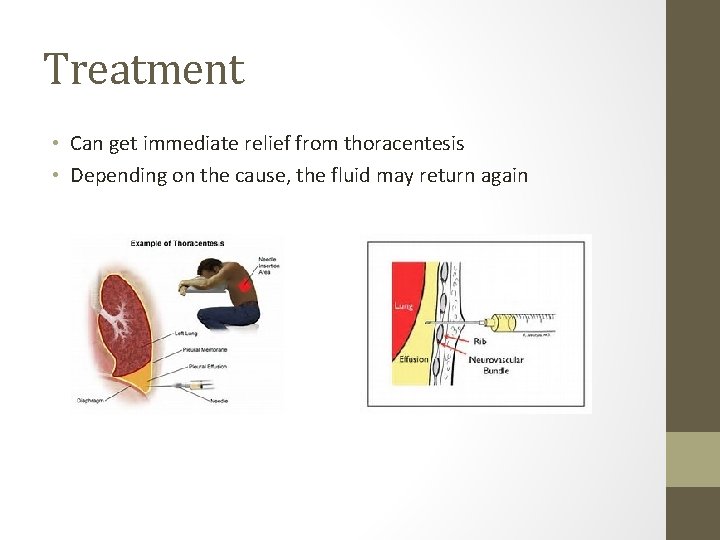
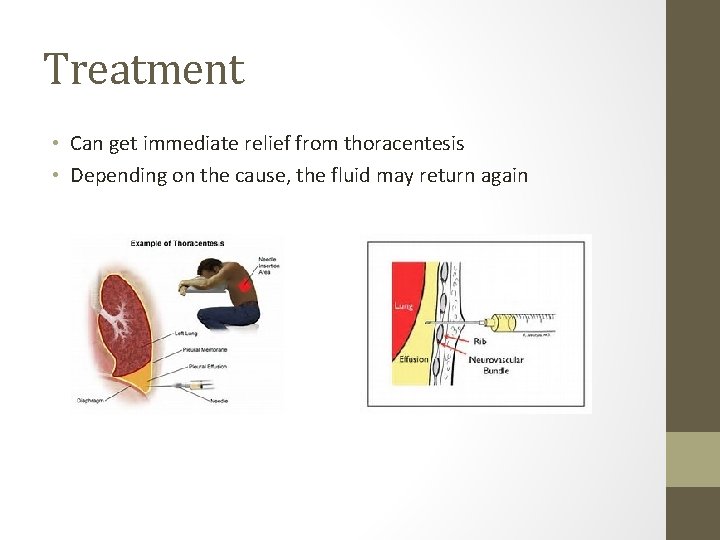
Treatment • Can get immediate relief from thoracentesis • Depending on the cause, the fluid may return again
Pleural Fluid • Culture & sensitivity • Cytological exam • Check for cancer cells • Can check for LDH, protein, etc
Nursing Management • Medications • Antipyretic if fever is present • Antibiotics, parenterally or instilled into the pleural space • Monitor VS • RR • Respiratory rhythm • Use of accessory muscles • Monitor lung sounds and assess complaints of dyspnea • Manage pain • Monitor for change in status • Tachycardia • Hypotension • Worsening SOB
Based on the last slide, what nursing diagnoses would be most important to consider?
Pulmonary Alterations Pleurisy
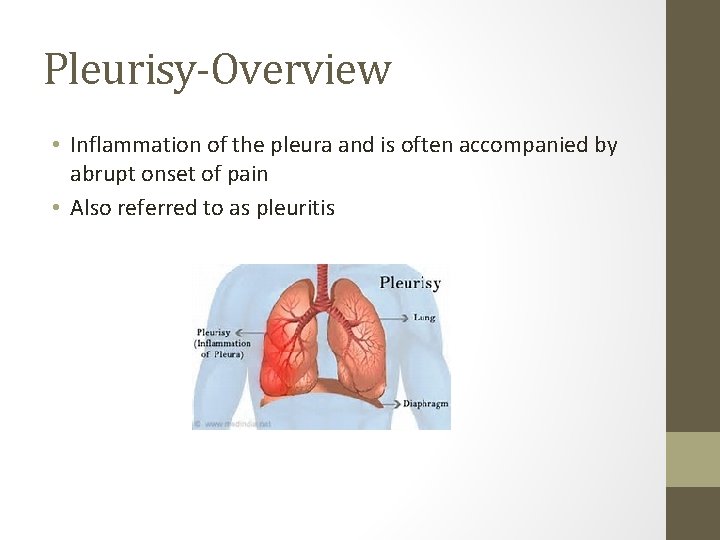
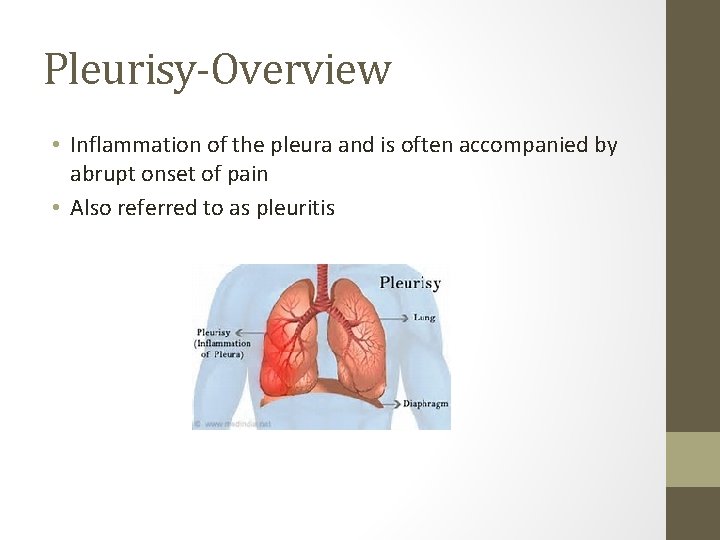
Pleurisy-Overview • Inflammation of the pleura and is often accompanied by abrupt onset of pain • Also referred to as pleuritis
Classifications of Pleurisy • Primary • Secondary • Result of another respiratory illness • Pneumonia • Pleural effusion • Trauma to the lung • Unilateral • Most common • Bilateral • Acute • Most common • Chronic
Different characteristics • Fibrinous • Severe pain without any fluid return upon aspiration • Adhesive • Occurs when the parietal pleura adhere to the visceral pleura • Complete obliteration of the pleural space can occur • Dry • More painful • Usually accompanies pneumonia • Adhesions may form • With effusion • i. e. , pleural effusion
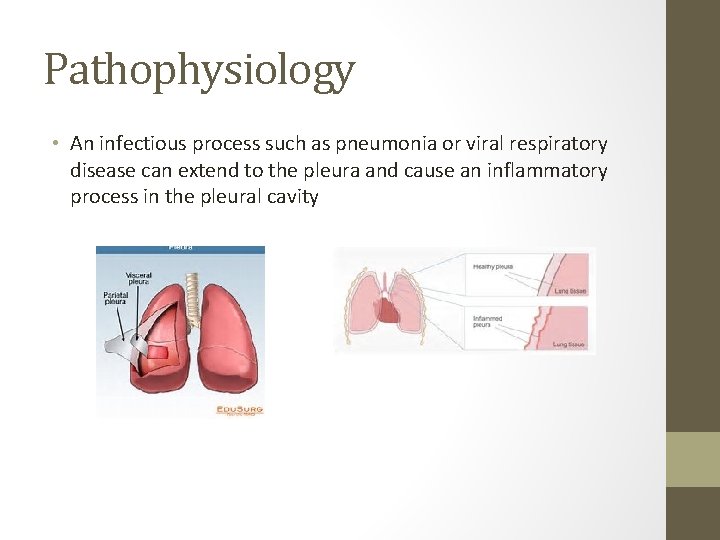
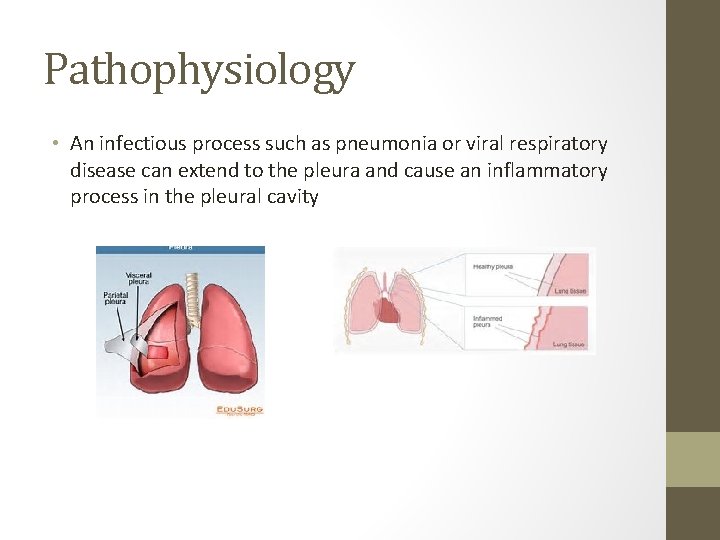
Pathophysiology • An infectious process such as pneumonia or viral respiratory disease can extend to the pleura and cause an inflammatory process in the pleural cavity
Signs and Symptoms • Abrupt pain that is usually unilateral and localized to a specific portion of the chest • Pain is sharp, stabbing and may radiate to the neck or shoulder • Pressure changes caused by breathing, movement or coughing will intensify the pain • Other symptoms: • • • Fever Dry, hacking cough Localized tenderness Diminished breath sounds Tachypnea Pleural friction rub
Nursing Assessment • • Symptom analysis of pain Vial signs Lung sounds Visual inspection for symmetry of chest wall during respirations
Nursing Management • Medications • Analgesics • NSAIDS for pain and/or fever • Antibiotics • Cough suppressant for non-productive cough • Avoid if productive cough is present • Encourage bedrest • Monitor VS, note fever and RR • Assess respiratory status • Encourage deep breathing and coughing • Show patient how to splint chest
If the pleurisy isn’t caused by pneumonia, what do you think bedrest and fear of taking a deep breath will put your patient at risk for?