PUBLIC WEBINAR CMS Measure Development Education Outreach Driving
PUBLIC WEBINAR CMS Measure Development Education & Outreach Driving Quality in the US: How CMS Evaluates its Measure Portfolio Presenters: Maria Durham (CMS) Sophia Chan (CMS) Melissa Castora-Binkley (HSAG) Kate Buchanan (Battelle) Meridith Eastman (Battelle) July 2021
Introduction • Welcome! This is an annual presentation to engage the public in the work CMS is doing around quality measurement • Aim to shed light on the processes and function of quality measurement in CMS programs and initiatives • If you are new to quality measurement, stay tuned for available resources that can help navigate development and use 1 2/6/2022
Learning Objectives • Articulate the role of the Measures Management System in advancing CMS goals and objectives • Identify how CMS ensures the quality of its measures – Standardized measure development processes as described in the MMS Blueprint – Evaluation throughout the measure lifecycle – Triennial Impact Assessment 2 2/6/2022
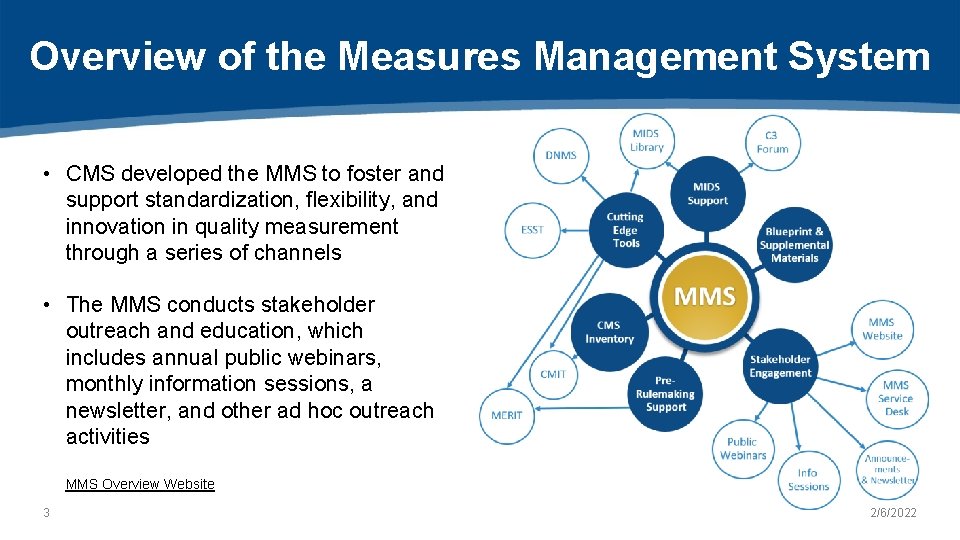
Overview of the Measures Management System • CMS developed the MMS to foster and support standardization, flexibility, and innovation in quality measurement through a series of channels • The MMS conducts stakeholder outreach and education, which includes annual public webinars, monthly information sessions, a newsletter, and other ad hoc outreach activities MMS Overview Website 3 2/6/2022

Ensuring Quality in Quality Measures 4 2/6/2022
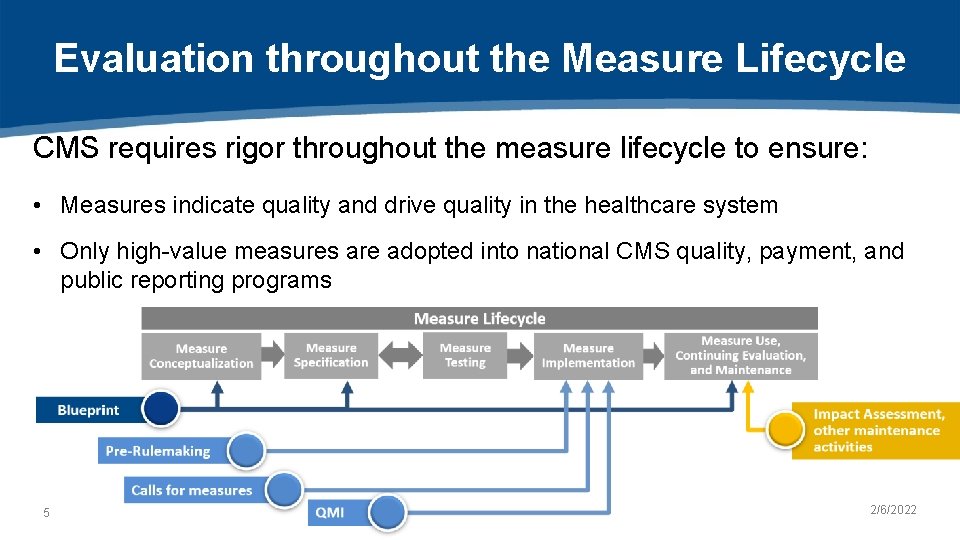
Evaluation throughout the Measure Lifecycle CMS requires rigor throughout the measure lifecycle to ensure: • Measures indicate quality and drive quality in the healthcare system • Only high-value measures are adopted into national CMS quality, payment, and public reporting programs 5 2/6/2022

Ensuring Quality during Development 6 2/6/2022
Standardized Processes • • • 7 Business Case Environmental Scan Technical Expert Panel Public Comment Specifications Testing requirements 2/6/2022
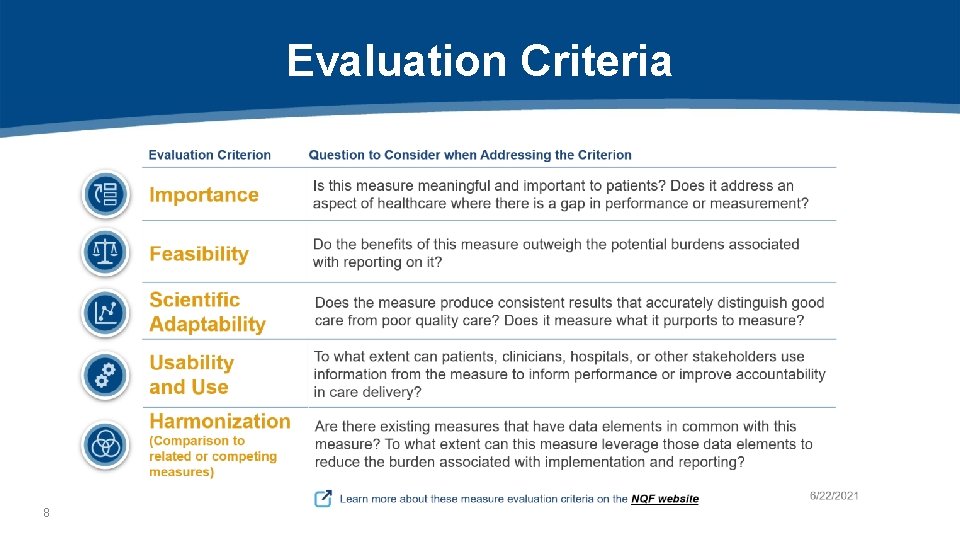
Evaluation Criteria 8
Risk Adjustment • Risk adjustment is a method to adjust for factors outside a clinician’s control that may impact an outcome or a measure score – Promotes better measure validity by helping to tie measure performance to the quality of care provided • Risk adjustment models for measures must be supported by evidence and the risk adjustment methodology must be tested during development as part of scientific acceptability testing 9 2/6/2022
Harmonization • Harmonization describes the process of aligning related measures so that their components are uniform or compatible, unless differences can be justified – The extent of harmonization depends on the relationship of the measures, the evidence for the measure focus, and differences in data sources • Contributes to burden reduction for measured entities and ensures that any novel data elements/measure logic are justifiable 10 2/6/2022
Stakeholder Engagement Stakeholder input helps ensure that measurement is • transparent • patient-centered • well-informed 11 2/6/2022

Measure Evaluation during Implementation 12 2/6/2022
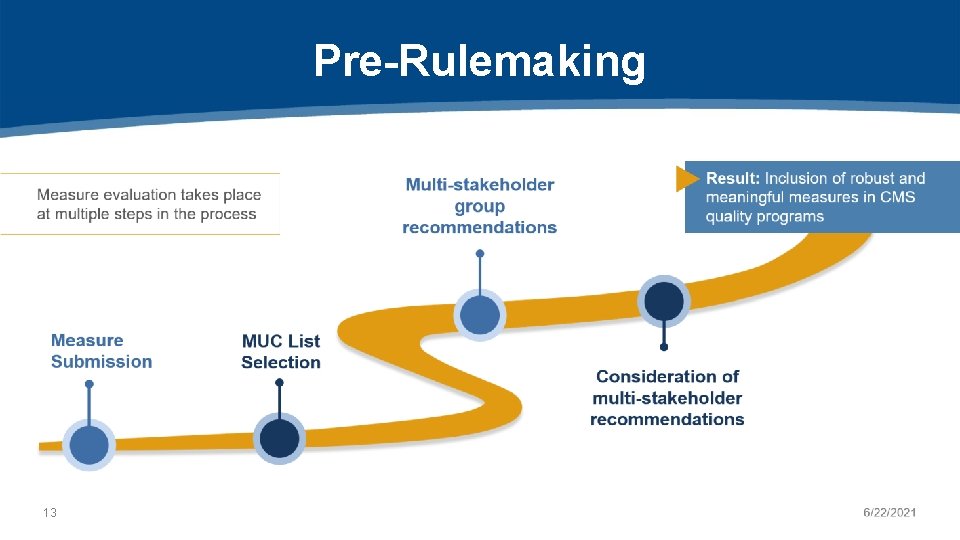
Pre-Rulemaking 13
CMS MERIT is the webbased tool used to submit measures for the MUC List • Ensures uniformity of information collected about each measure • Facilitates CMS review of submitted measures 14 2/6/2022
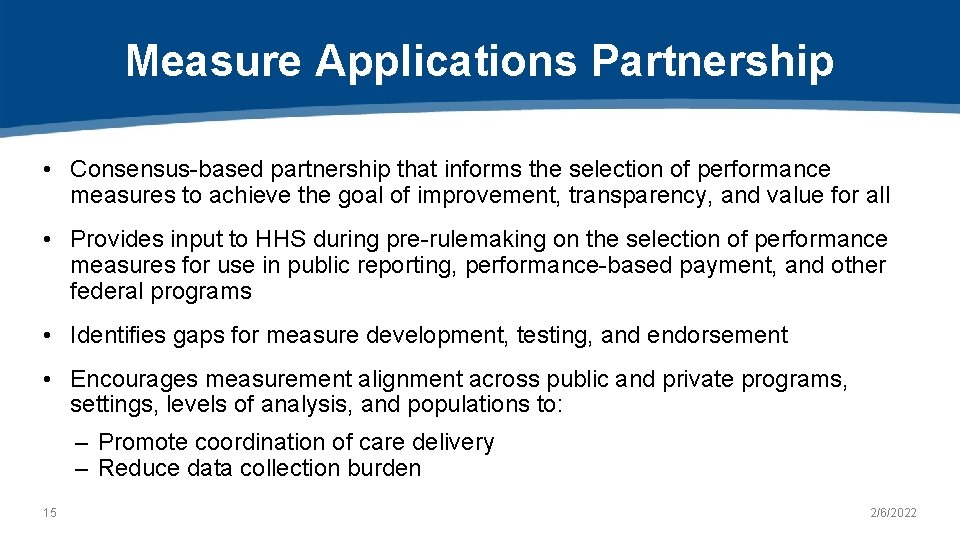
Measure Applications Partnership • Consensus-based partnership that informs the selection of performance measures to achieve the goal of improvement, transparency, and value for all • Provides input to HHS during pre-rulemaking on the selection of performance measures for use in public reporting, performance-based payment, and other federal programs • Identifies gaps for measure development, testing, and endorsement • Encourages measurement alignment across public and private programs, settings, levels of analysis, and populations to: – Promote coordination of care delivery – Reduce data collection burden 15 2/6/2022
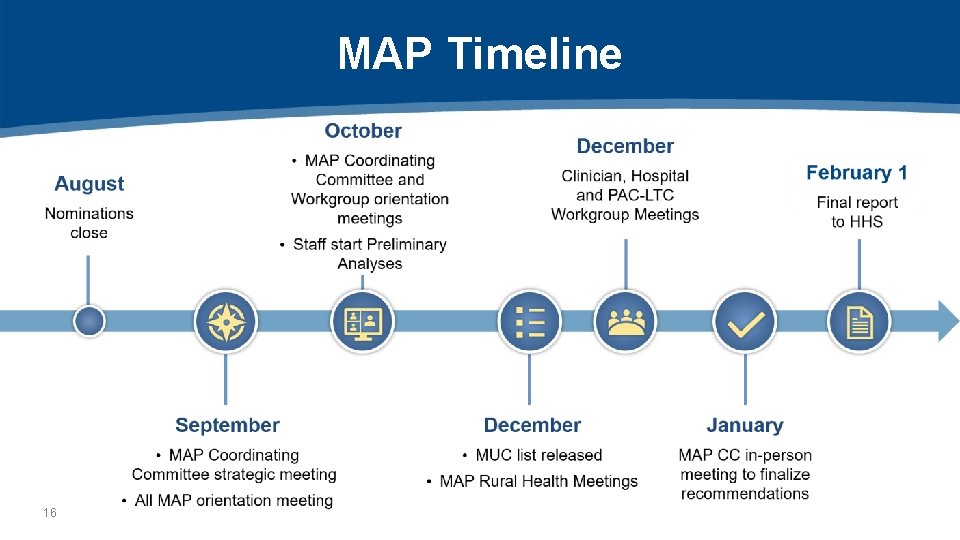
MAP Timeline 16
Calls for Measures • Some measure programs do not use the pre-rulemaking or rulemaking processes, but the same level of rigor is applied – Example: Quality Rating System (QRS) • These programs use Call Letters to communicate changes and request comments on proposed refinements 17 2/6/2022
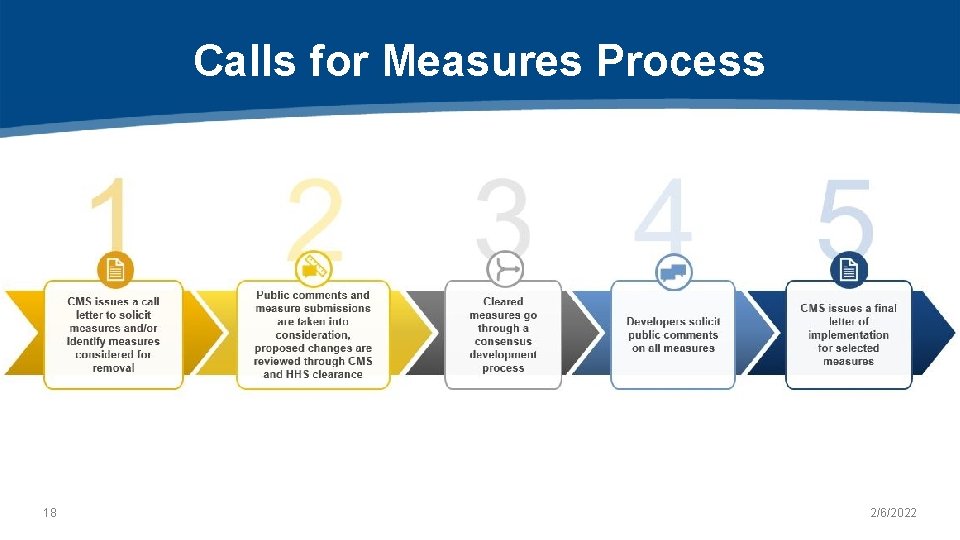
Calls for Measures Process 18 2/6/2022

Evaluating Measures Currently in Use 19 2/6/2022
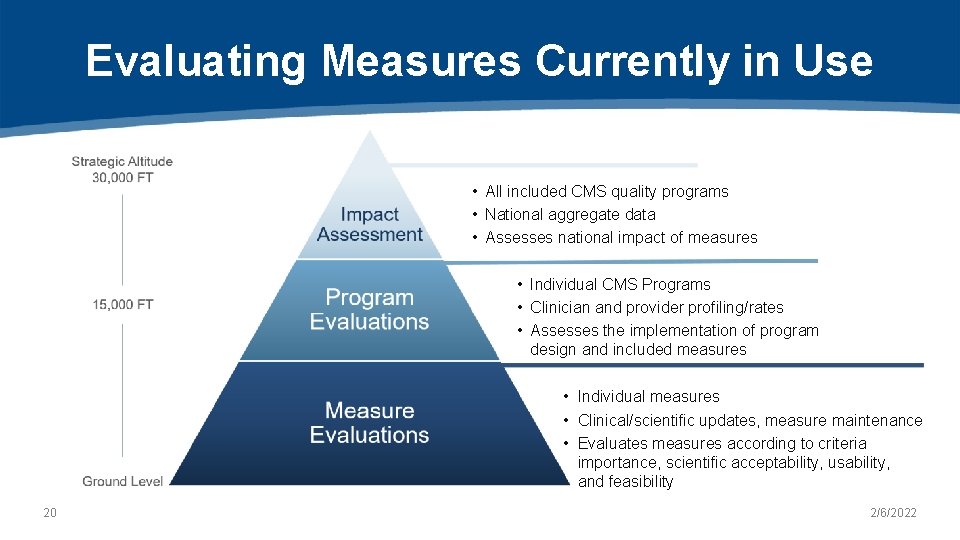
Evaluating Measures Currently in Use • All included CMS quality programs • National aggregate data • Assesses national impact of measures • Individual CMS Programs • Clinician and provider profiling/rates • Assesses the implementation of program design and included measures • Individual measures • Clinical/scientific updates, measure maintenance • Evaluates measures according to criteria importance, scientific acceptability, usability, and feasibility 20 2/6/2022
Impact Assessment • Required by section 1890 A(a)(6) of the Social Security Act • Triennial report • Structured by health care quality priorities (e. g. , Patient Safety) 21 2/6/2022
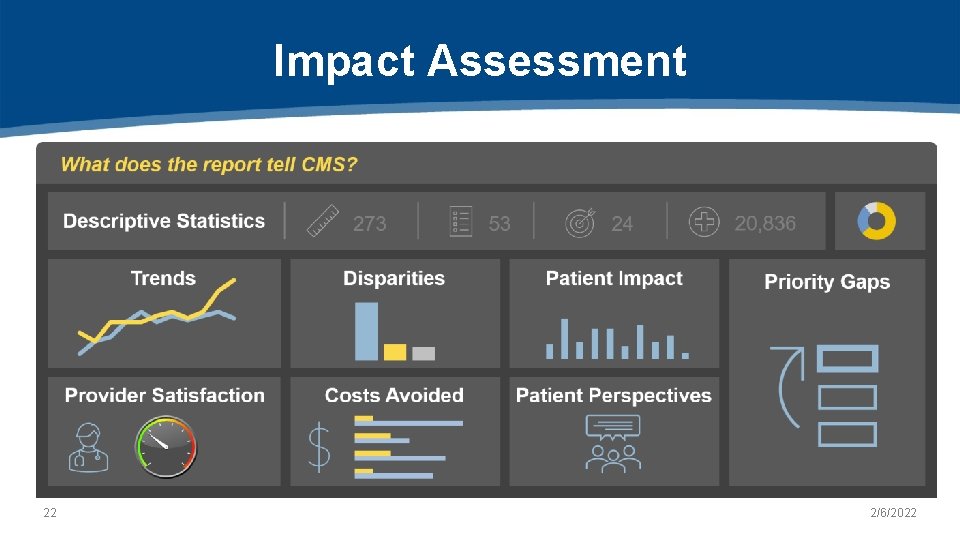
Impact Assessment 22 2/6/2022
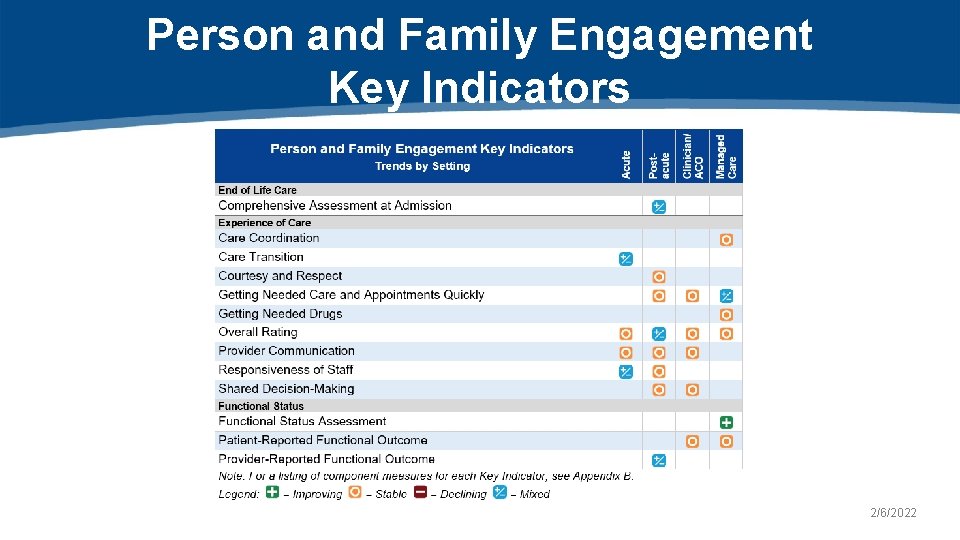
Person and Family Engagement Key Indicators 2/6/2022
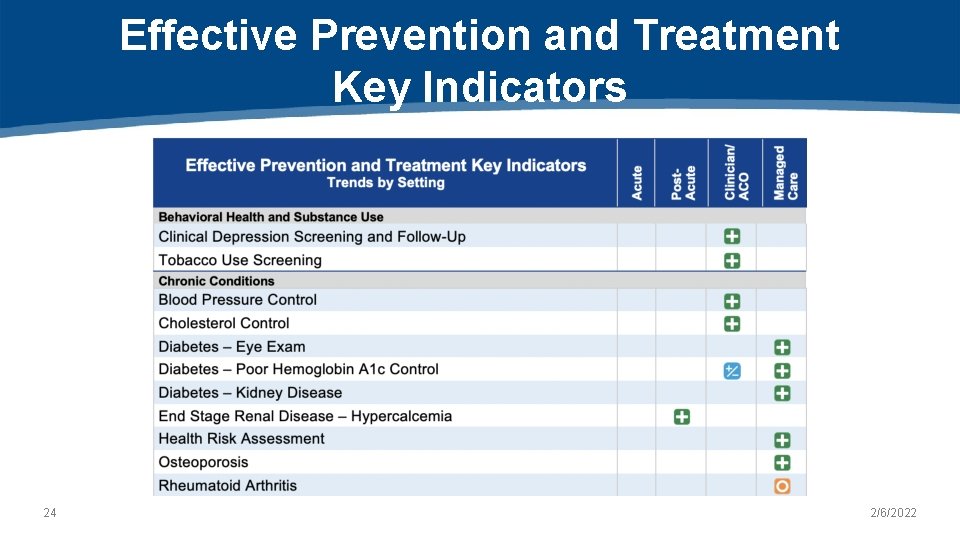
Effective Prevention and Treatment Key Indicators 24 2/6/2022
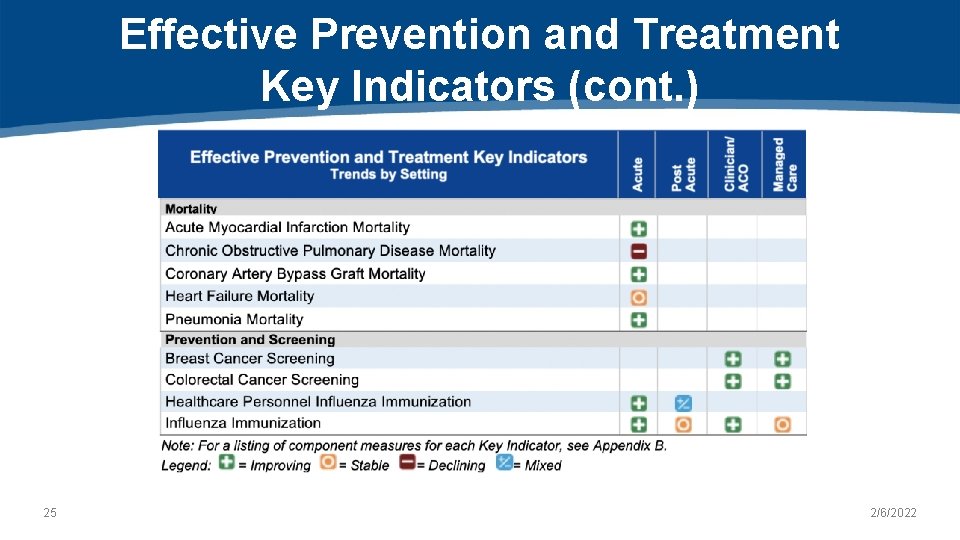
Effective Prevention and Treatment Key Indicators (cont. ) 25 2/6/2022
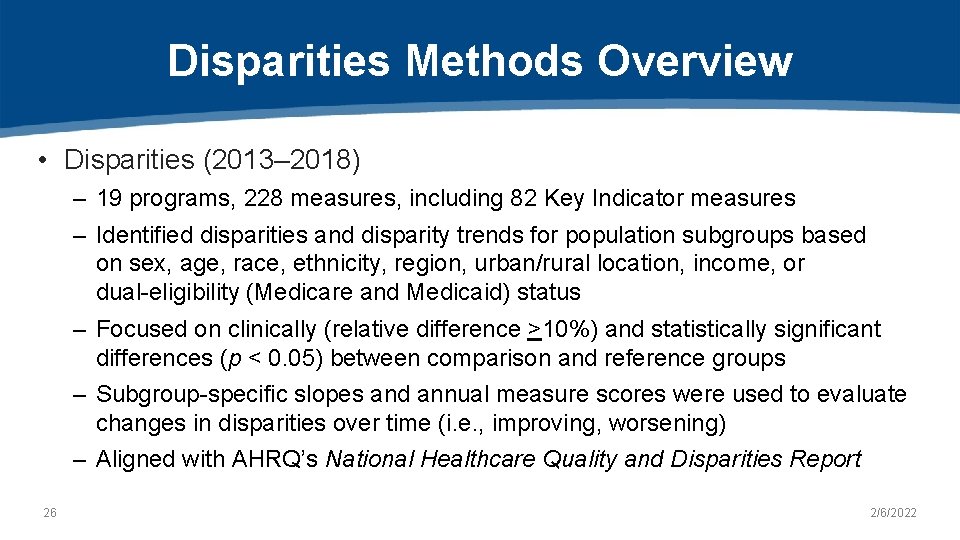
Disparities Methods Overview • Disparities (2013– 2018) – 19 programs, 228 measures, including 82 Key Indicator measures – Identified disparities and disparity trends for population subgroups based on sex, age, race, ethnicity, region, urban/rural location, income, or dual-eligibility (Medicare and Medicaid) status – Focused on clinically (relative difference >10%) and statistically significant differences (p < 0. 05) between comparison and reference groups – Subgroup-specific slopes and annual measure scores were used to evaluate changes in disparities over time (i. e. , improving, worsening) – Aligned with AHRQ’s National Healthcare Quality and Disparities Report 26 2/6/2022
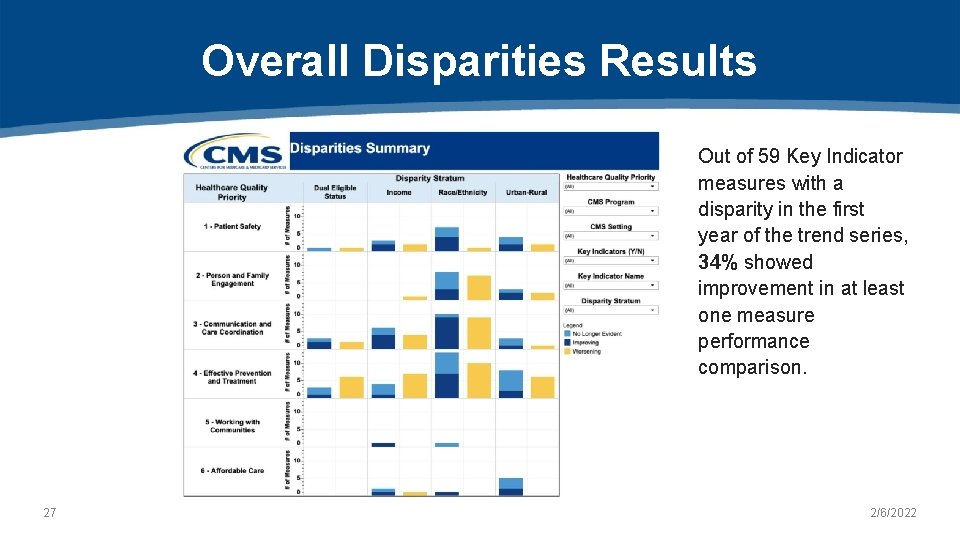
Overall Disparities Results Out of 59 Key Indicator measures with a disparity in the first year of the trend series, 34% showed improvement in at least one measure performance comparison. 27 2/6/2022
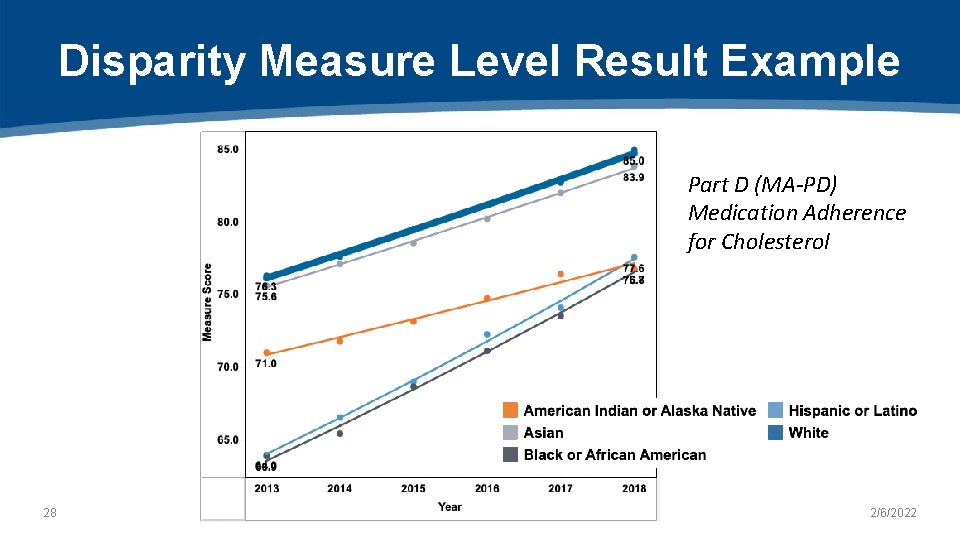
Disparity Measure Level Result Example Part D (MA-PD) Medication Adherence for Cholesterol 28 2/6/2022
Impact Assessment Strengths of 2021 Impact Assessment Report ü Accessible: Designed for a wide group of stakeholders, including patients ü Comprehensive: Includes 686 measures from 26 reporting programs ü Data-driven: Leverages data from multiple internal/external data sources ü Rigorous: Adopts methods recommended by experts, aligned with AHRQ ü Strategic: Assesses CMS health care quality priorities 29 2/6/2022
Impact Assessment Limitations • Attribution: Results cannot be attributed directly to measures – Plausible that measurement contributed to impacts • Missing data: Data for analyses may be incomplete – Number of measures analyzed by analysis indicated • Comparability: Results are not directly comparable to prior reports – Methods have been modified to enhance scientific rigor – Appendices contain period-of-record analysis 30 2/6/2022
Impact Assessment Results supplement other CMS efforts to understand impact • Fosters comparisons across settings/programs relative to key clinical topics and CMS health care quality priorities • Quantifies national impact of measures on improving care to inform measure selection • Identifies disparities that may require further investigation to determine underlying causes and target quality improvement initiatives • Highlights actions taken by providers and barriers encountered in seeking to improve quality 31 2/6/2022
Conclusion • Results suggest that: – Use of CMS quality measures likely contributed to improving quality and reducing health care costs in key health care quality priorities – Opportunities for improvement remain • Reducing disparities and improving health equity • Increasing performance on declining measures • Improving EHR interoperability – CMS has taken steps to reduce burden, increase outcome measures, and better understand patient and provider perspectives 32 2/6/2022

Future Plans 33 2/6/2022
Evolving Priorities 1 Streamline quality measurement 1. 2. 2 Leverage measures to drive improvement in health outcomes more effectively 3 Transition to digital measures and use of advanced analytics 3. 4 Increase patient-centeredness through patient-reported quality 4. measures and increase transparency 5 Promote health equity and close gaps in care via quality measures 5. 34 2/6/2022
What Is the QMI? Tool that provides an objective and standard methodology to rapidly assess the relative value of quality measures in achieving CMS strategic objectives 35
Incentives to Develop the QMI • Measure information currently provided by stakeholders to CMS is heterogenous and imprecise • Key information on the scientific acceptability and impact of quality measures is often missing or not standardized • These factors limit fair comparisons of the relative value of quality measures in achieving CMS strategic objectives and selecting measures for programs * *A 2019 Government Accountability Office (GAO) study found CMS used multiple approaches to assess measures for inclusion, continued use, and removal, and lacked a systematic method to ensure measures met CMS strategic objectives. 1 36
Ongoing Evaluation: Alignment Efforts • Increased emphasis at CMS on evaluating the measure portfolio to identify opportunities for improved alignment across programs – High value measures identified for use across programs – Low value measures identified for potential removal pending stakeholder input • Alignment opportunities exist at multiple levels: – Agency-wide (Internal Alignment Workgroup) – Cross-agency (CMS/VA/Do. D Workgroup) – Public/private (Core Quality Measures Collaborative [CQMC]) 37 2/6/2022
Questions 38 2/6/2022

Battelle CMS Measures Manager Contact: MMSsupport@Battelle. org Kimberly Rawlings (CMS COR) Contact: Kimberly. Rawlings@cms. hhs. gov
- Slides: 40