Public Health Perspective of Urogenital Infections 1 Urogenital
Public Health Perspective of Urogenital Infections 1
Urogenital Infections l 1 - Sexually transmitted infections l 2 - Urinary tract infections 2
Sexually Transmitted Infections l Sexually transmitted infections (STIs) or diseases (STDs) are infections that could be transmitted through sexual contact 3
Sexually Transmitted Infections More than 30 different bacteria, viruses and parasites are known to be transmitted through sexual contact. l Eight of these pathogens are linked to the greatest incidence of sexually transmitted disease. l Of these 8 infections, 4 are currently curable: syphilis, gonorrhoea, chlamydia and trichomoniasis. l The other 4 are viral infections which are incurable: hepatitis B, herpes simplex virus (HSV or herpes), HIV, and human papillomavirus (HPV). l l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 4
Sexually Transmitted Infections Symptoms or disease due to the incurable viral infections can be reduced or modified through treatment. l STIs are spread predominantly by sexual contact, including vaginal, anal and oral sex. l Some STIs can also be spread through non -sexual means such as via blood or blood products. l l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 5
Sexually Transmitted Infections Many STIs—including syphilis, hepatitis B, HIV, chlamydia, gonorrhoea, herpes, and HPV —can also be transmitted from mother to child during pregnancy and childbirth. l A person can have an STI without having obvious symptoms of disease. l Common symptoms of STIs include vaginal discharge, urethral discharge or burning in men, genital ulcers, and abdominal pain. l l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 6
Sexually Transmitted Infections l Magnitude: l STIs have a profound impact on sexual and reproductive health worldwide. l More than 1 million STIs are acquired every day. l In 2016, WHO estimated 376 million new infections with 1 of 4 STIs: chlamydia (127 million), l gonorrhoea (87 million), l syphilis (6. 3 million) and l trichomoniasis (156 million). l l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 7
Sexually Transmitted Infections l Magnitude: More than 500 million people are living with genital HSV (herpes) infection and l an estimated 300 million women have an HPV infection, the primary cause of cervical cancer. l An estimated 240 million people are living with chronic hepatitis B globally. Both HPV and hepatitis B infections are preventable with vaccination. l l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 8
Sexually Transmitted Infections l Impact: l STIs can have serious consequences beyond the immediate impact of the infection itself. l STIs like herpes and syphilis can increase the risk of HIV acquisition threefold or more. l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 9
Sexually Transmitted Infections l Impact: l Mother-to-child transmission of STIs can result in l l l stillbirth, neonatal death, low-birth-weight and prematurity, sepsis, pneumonia, neonatal conjunctivitis, and congenital deformities. l Approximately 1 million pregnant women were estimated to have active syphilis in 2016, resulting in over 350 000 adverse birth outcomes of which 200 000 occurred as stillbirth or neonatal death. l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 10
Sexually Transmitted Infections l Impact: l HPV infection causes 570 000 cases of cervical cancer and over 300 000 cervical cancer deaths each year. l STIs such as gonorrhoea and chlamydia are major causes of pelvic inflammatory disease (PID) and infertility in women. l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 11
Sexually Transmitted Infections l Prevention l of STIs Counselling and behavioural approaches l comprehensive sexuality education, STI and HIV pre- and post-test counselling; l safer sex/risk-reduction counselling, condom promotion; l STI interventions targeted to key populations, such as sex workers, men who have sex with men and people who inject drugs; and l STI prevention education and counselling tailored to the needs of adolescents. 12
Sexually Transmitted Infections Prevention of STIs l Counselling and behavioural approaches l In addition, counselling can improve people’s ability to recognize the symptoms of STIs and increase the likelihood they will seek care or encourage a sexual partner to do so. l l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) l Commitment within marital bond 13
Sexually Transmitted Infections Prevention of STIs l Counselling and behavioural approaches l Barrier methods l l When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms. https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 14
Sexually Transmitted Infections l Prevention of STIs l Unfortunately, lack of public awareness, l lack of training of health workers, l and long-standing, widespread stigma around STIs remain barriers to greater and more effective use of these interventions. l l https: //www. who. int/en/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) 15
Sexually Transmitted Infections Management: l Case management: l l STI case management is the care of a person with an STI-related syndrome or with a positive test for one or more STI. Effective case management consists not only of antimicrobial therapy to obtain cure and reduce infectivity, but also comprehensive care of the patient’s needs for reproductive health. https: //www. who. int/hiv/topics/vct/sw_toolkit/guidelines_management_sti. pdf 16
Sexually Transmitted Infections Management: l Case management: l l The components of case management include: l history taking, examination, correct diagnosis, early and effective treatment, advice on sexual behaviour, promotion and/or provision of condoms, partner notification and treatment, case reporting and l clinical follow-up as appropriate l l https: //www. who. int/hiv/topics/vct/sw_toolkit/guidelines_management_sti. pdf 17
Sexually Transmitted Infections l Management: l STI case management l Low- and middle-income countries rely on identifying consistent, easily recognizable signs and symptoms to guide treatment, without the use of laboratory tests. l This is called syndromic management. 18
Sexually Transmitted Infections Management: l STI case management l l This approach, which often relies on clinical algorithms, allows health workers to diagnose a specific infection on the basis of observed syndromes as: vaginal discharge, l urethral discharge, l genital ulcers, l abdominal pain l 19
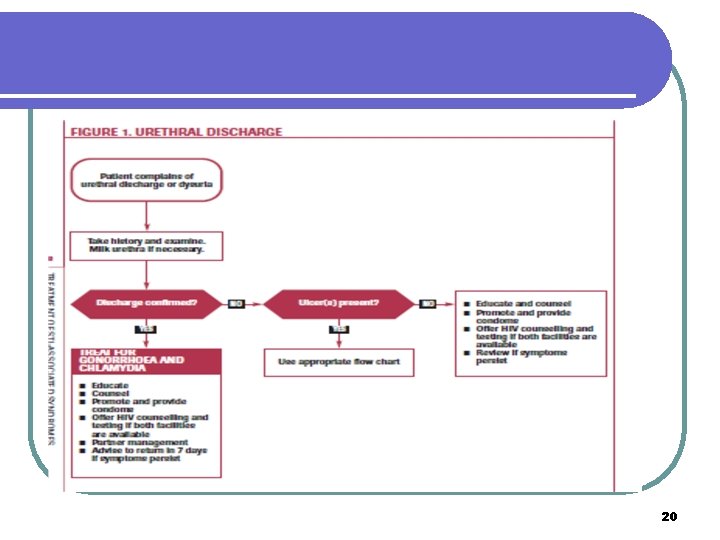
20
Sexually Transmitted Infections l Management: l STI l l case management Syndromic management is simple, assures rapid, same-day treatment, and avoids expensive or unavailable diagnostic tests for patients that present with symptoms. This approach results to overtreatment and missed treatment as majority of STIs are asymptomatic. Thus, in addition to syndromic management, screening strategies are essential. To interrupt transmission of infection and prevent re-infection, treating sexual partners is an important component of STI case management. 21
Urinary Tract Infections (UTI) UTIs are common infections that happen when bacteria, often from the skin or rectum, enter the urethra, and infect the urinary tract. The infections can affect several parts of the urinary tract but the most common type is a bladder infection (cystitis). l Kidney infection (pyelonephritis) is another type of UTI. They’re less common, but more serious than bladder infections. l l https: //www. cdc. gov/antibiotic-use/community/for-patients/common-illnesses/uti. html 22
UTI Inflammatory response of urothelium to bacterial invasion. ü Bacteriuria : bacteria in urine ü Asymptomatic or symptomatic ü Bacteriuria + pyuria= infection ü Bacteriuria NO pyuria = colonization 23
Urinary Tract Infection l Upper l urinary tract Infections: Pyelonephritis l Lower urinary tract infections Cystitis (“traditional” UTI) l Urethritis (often sexually-transmitted) l Prostatitis l 24
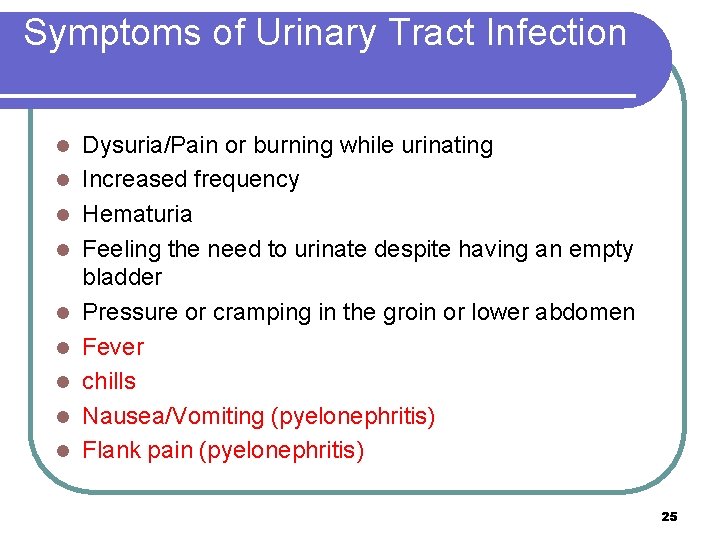
Symptoms of Urinary Tract Infection l l l l l Dysuria/Pain or burning while urinating Increased frequency Hematuria Feeling the need to urinate despite having an empty bladder Pressure or cramping in the groin or lower abdomen Fever chills Nausea/Vomiting (pyelonephritis) Flank pain (pyelonephritis) 25
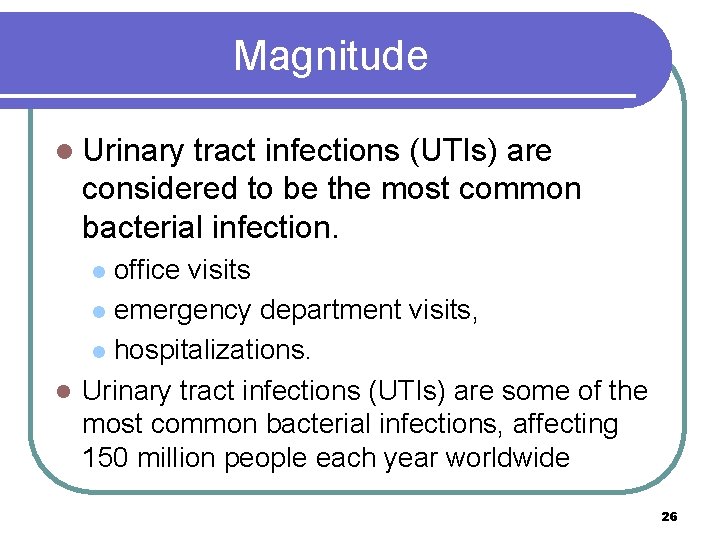
Magnitude l Urinary tract infections (UTIs) are considered to be the most common bacterial infection. office visits l emergency department visits, l hospitalizations. l Urinary tract infections (UTIs) are some of the most common bacterial infections, affecting 150 million people each year worldwide l 26
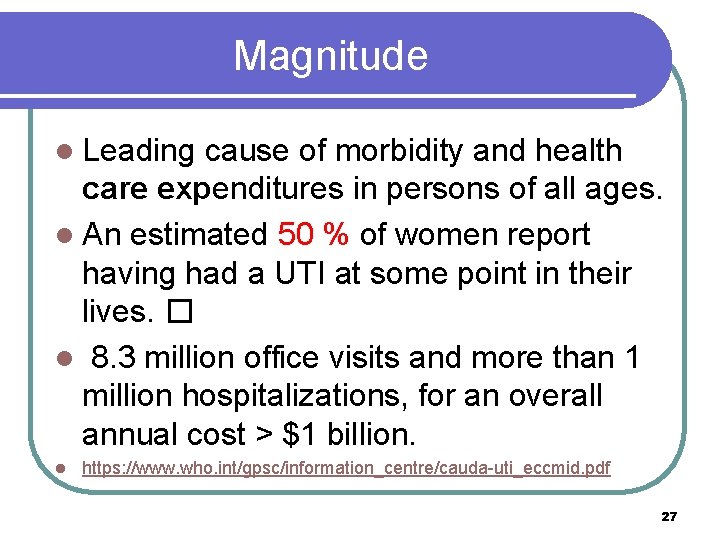
Magnitude l Leading cause of morbidity and health care expenditures in persons of all ages. l An estimated 50 % of women report having had a UTI at some point in their lives. � l 8. 3 million office visits and more than 1 million hospitalizations, for an overall annual cost > $1 billion. l https: //www. who. int/gpsc/information_centre/cauda-uti_eccmid. pdf 27
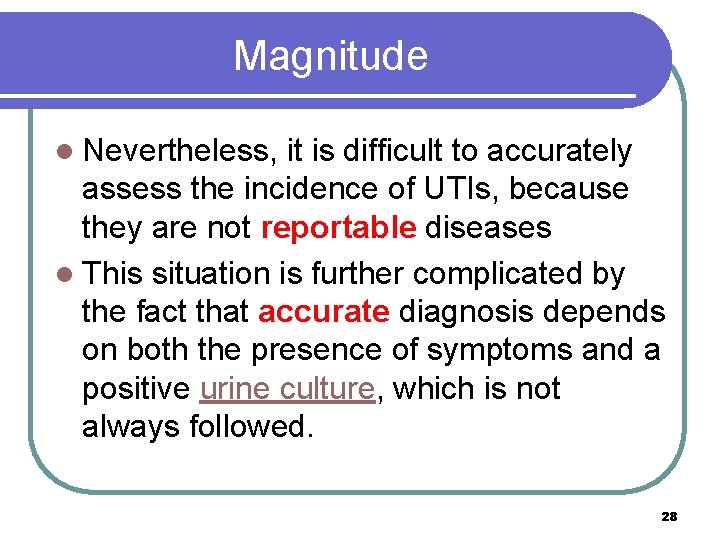
Magnitude l Nevertheless, it is difficult to accurately assess the incidence of UTIs, because they are not reportable diseases l This situation is further complicated by the fact that accurate diagnosis depends on both the presence of symptoms and a positive urine culture, which is not always followed. 28
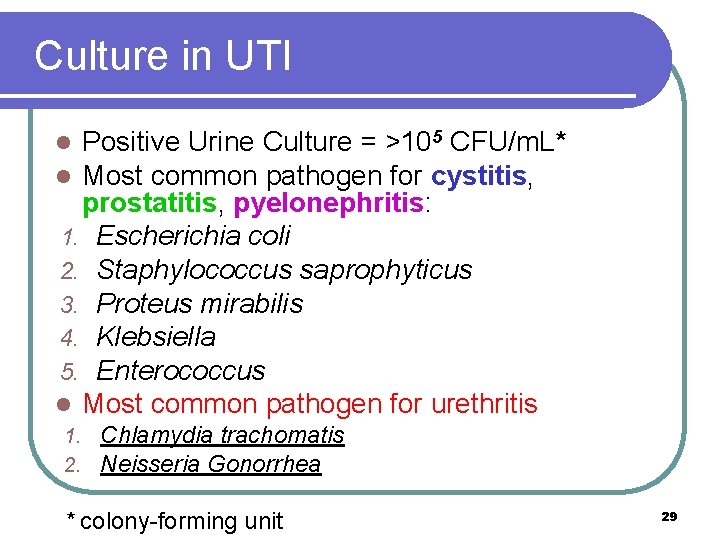
Culture in UTI Positive Urine Culture = >105 CFU/m. L* Most common pathogen for cystitis, prostatitis, pyelonephritis: 1. Escherichia coli 2. Staphylococcus saprophyticus 3. Proteus mirabilis 4. Klebsiella 5. Enterococcus l Most common pathogen for urethritis l l 1. 2. Chlamydia trachomatis Neisseria Gonorrhea * colony-forming unit 29
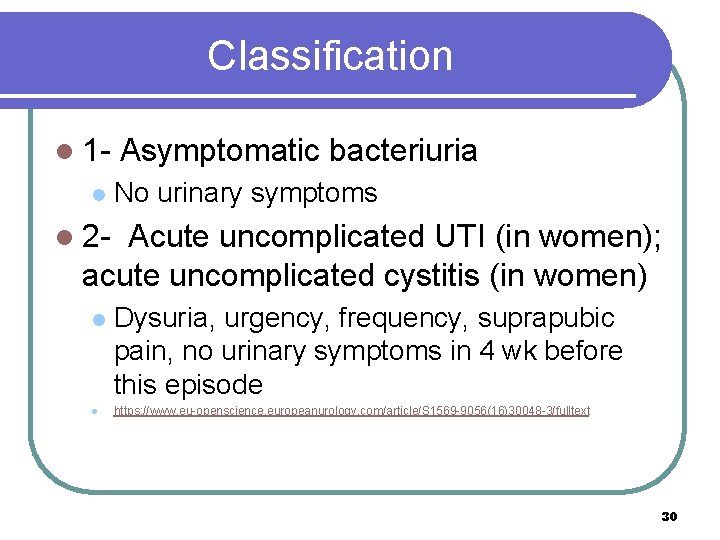
Classification l 1 l Asymptomatic bacteriuria No urinary symptoms l 2 - Acute uncomplicated UTI (in women); acute uncomplicated cystitis (in women) l l Dysuria, urgency, frequency, suprapubic pain, no urinary symptoms in 4 wk before this episode https: //www. eu-openscience. europeanurology. com/article/S 1569 -9056(16)30048 -3/fulltext 30
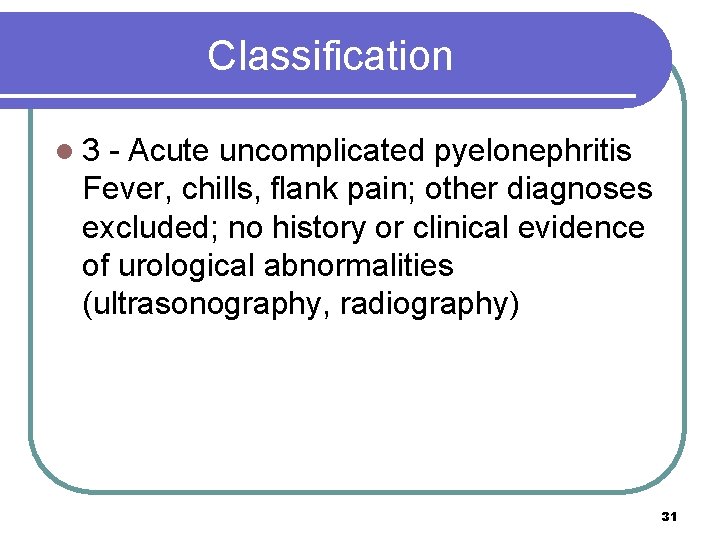
Classification l 3 - Acute uncomplicated pyelonephritis Fever, chills, flank pain; other diagnoses excluded; no history or clinical evidence of urological abnormalities (ultrasonography, radiography) 31
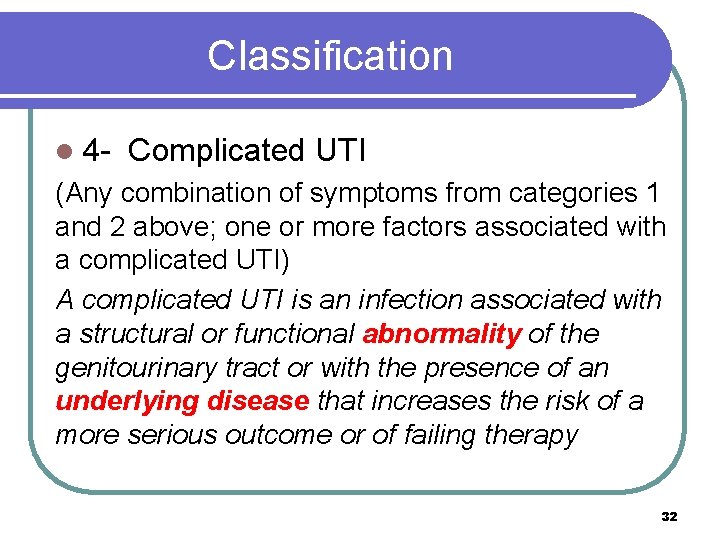
Classification l 4 - Complicated UTI (Any combination of symptoms from categories 1 and 2 above; one or more factors associated with a complicated UTI) A complicated UTI is an infection associated with a structural or functional abnormality of the genitourinary tract or with the presence of an underlying disease that increases the risk of a more serious outcome or of failing therapy 32
Classification l 5 - Recurrent UTI At least three episodes of uncomplicated infection documented by culture in past 12 mo common among young healthy women, even though they have anatomically and physiologically normal urinary tracts 33
Risk Factors l Increase UTI risk l Increase bacterial l Host defences virulence Definitions: A bacterial pathogen is usually defined as any l Protect against UTI bacterium that has the capacity to cause disease. Its ability to cause disease is called pathogenicity. Virulence provides a quantitative measure of the pathogenicity or the likelihood of 34 causing disease.
Risk Factors UTIs are more common in women because the rectum and urethra are close to each other, making infection more likely. Other factors that may increase chance of a UTI include: 1. Being sexually active 2. New sexual partner 3. Using a diaphragm for birth control 4. Menopause 35
Risk Factors Other factors that may increase chance of a UTI include: 5. Diabetes 6. Blockage in the urinary tract 1. Kidney stones 2. Enlarged prostate 7. Weak immune system 8. Abnormalities of the urinary system, such as vesicoureteral reflux or polycystic kidneys 36
Risk factors Paraplegia or quadriplegia 10. Sickle-cell anemia 11. History of urinary surgery or kidney transplant 12. Bladder catheter in place, or recent device inserted into the urinary system 13. Pregnancy 9. 37
Complications l When treated promptly and properly, lower urinary tract infections rarely lead to complications. l But left untreated, a urinary tract infection can have serious consequences. 38
Complications l Complications of a UTI may include: Recurrent infections, especially in women who experience two or more UTIs in a sixmonth period or four or more within a year. l Permanent kidney damage from an acute or chronic kidney infection (pyelonephritis) due to an untreated UTI. l Increased risk in pregnant women of delivering low birth weight or premature infants. l 39
Complications l l l l of a UTI may include: Urethral narrowing (stricture) in men from recurrent urethritis, previously seen with gonococcal urethritis. Sepsis, a potentially life-threatening complication of an infection, especially if the infection works its way up your urinary tract to your kidneys. Bacterial resistance may add more to the complications https: //www. mayoclinic. org/diseases-conditions/urinary-tract-infection/symptomscauses/syc-20353447 40
Complications Recurrent UTIs were associated with an economic burden due to both sick leave and physician visits. l It has a negative impact on the quality of life (Qo. L) l https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 6502976/ 41
Complications The burden of recurrent UTIs has both personal and societal aspects. l The societal burden includes the clinical and economic burden of the illness, l and the personal burden includes social and psychological effects which have a negative impact on quality of life (Qo. L). l 42
Complications l Recurrent UTIs are associated with symptoms of anxiety and depression. l The personal and societal impacts of recurrent UTIs often overlap. For example, in cases where multiple urine cultures or imaging studies may be required, the diagnostic burden both affects Qo. L and has a substantial negative economic impact. Costs may be both direct and indirect: work absenteeism, for example, can impact both the economy and a patient’s sense of wellbeing. 43
Prevention To help keep bacteria out of the urinary tract: ü Drink plenty of fluids throughout the day. Cranberry juice is a good choice. ü Urinate when you feel the need and do not resist the urge. ü Empty your bladder completely ü Wash genitals daily. ü Take showers instead of baths. 44
Prevention To help keep bacteria out of the urinary tract: ü For women: ü Always wipe from the front to the back after having a bowel movement. ü Wash up before sex and urinate after it. ü Avoid irritating feminine products. Skip douches, deodorant sprays, scented powders, and other potentially irritating feminine products ü Avoid some birth control methods; a diaphragm, spermicide, or spermicide-lubricated condom can contribute to bacterial growth. 45

46
- Slides: 46