Psychotherapy in Psychotic disorders Principles and practice of





- Slides: 33
Psychotherapy in Psychotic disorders: Principles and practice of Personal therapy Matcheri S Keshavan MD Harvard Medical School, and University of Pittsburgh NIMH MH 60902, 92440 and 105596; Disclosures: Sunovion, Otsuka
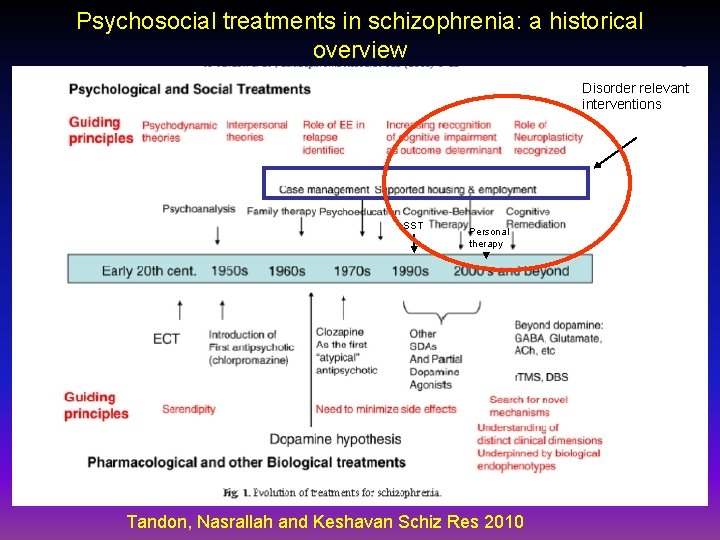
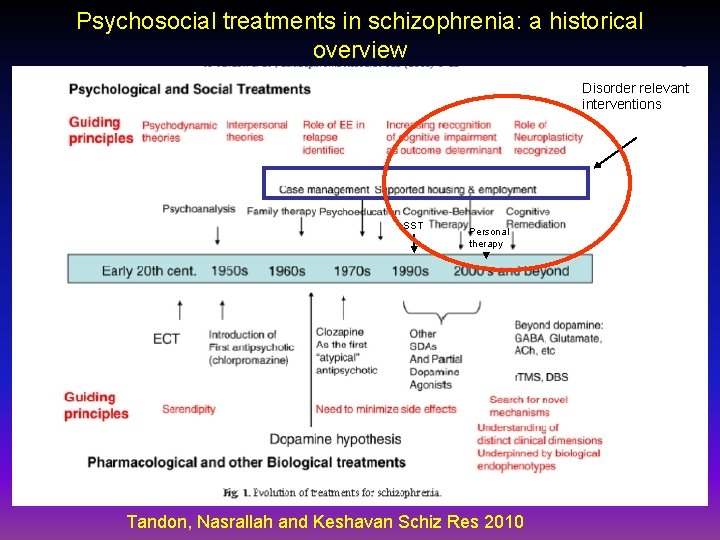
Psychosocial treatments in schizophrenia: a historical overview Disorder relevant interventions SST Personal therapy Tandon, Nasrallah and Keshavan Schiz Res 2010
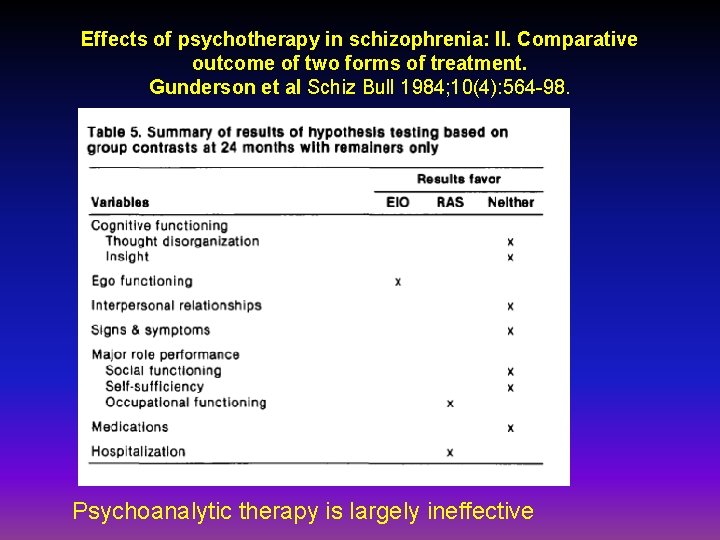
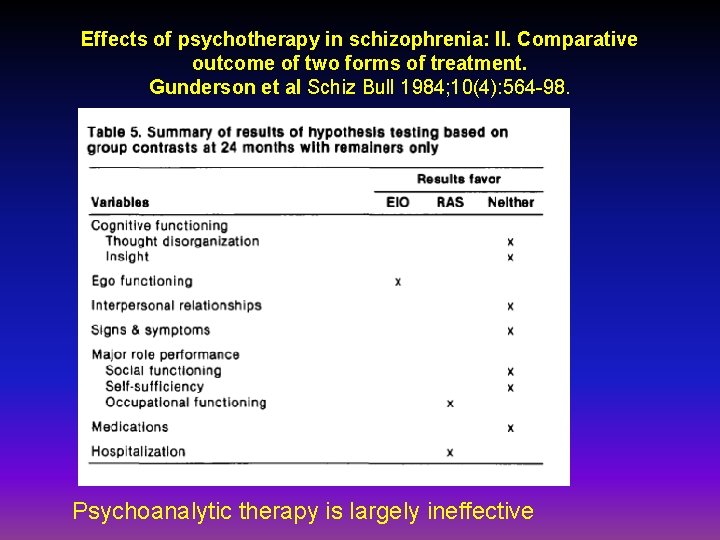
Effects of psychotherapy in schizophrenia: II. Comparative outcome of two forms of treatment. Gunderson et al Schiz Bull 1984; 10(4): 564 -98. Psychoanalytic therapy is largely ineffective
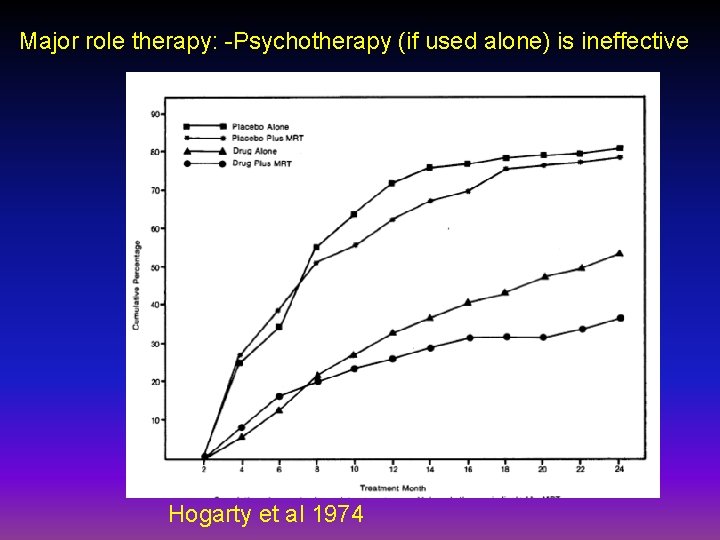
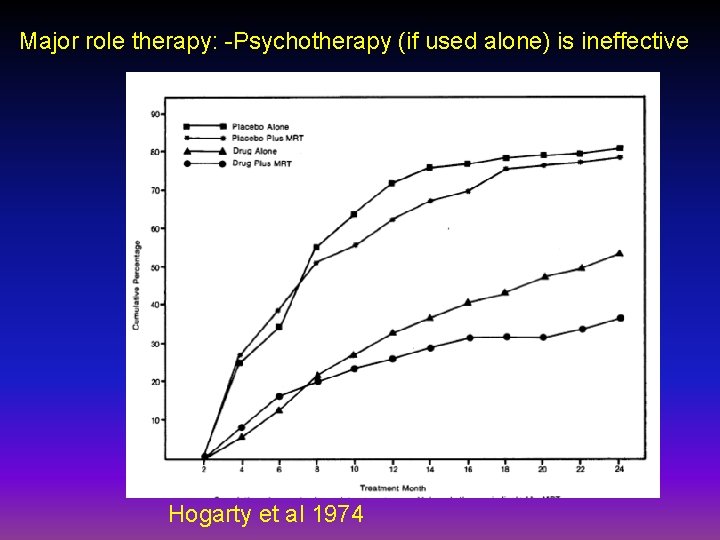
Major role therapy: -Psychotherapy (if used alone) is ineffective Hogarty et al 1974
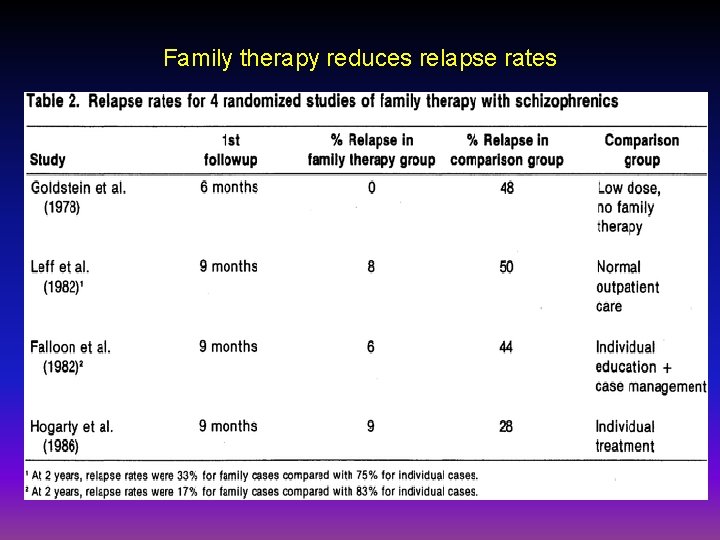
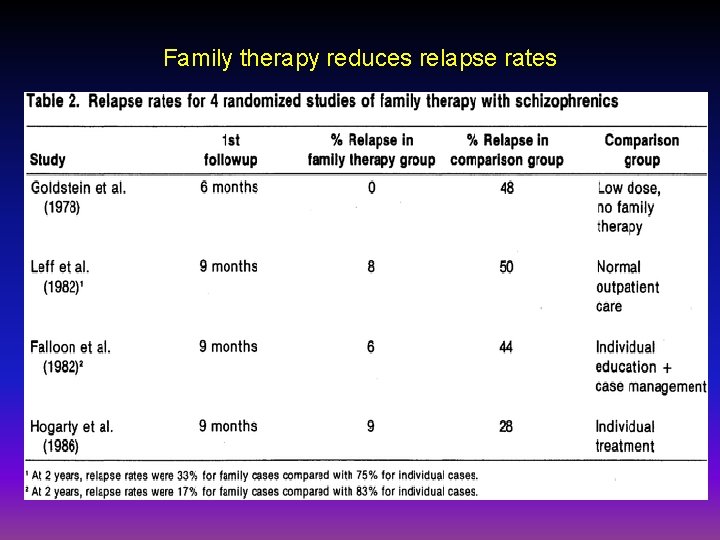
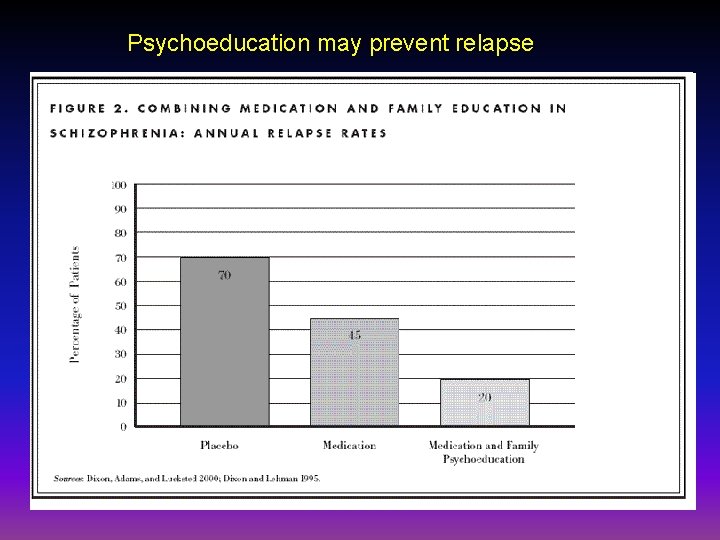
Family therapy reduces relapse rates
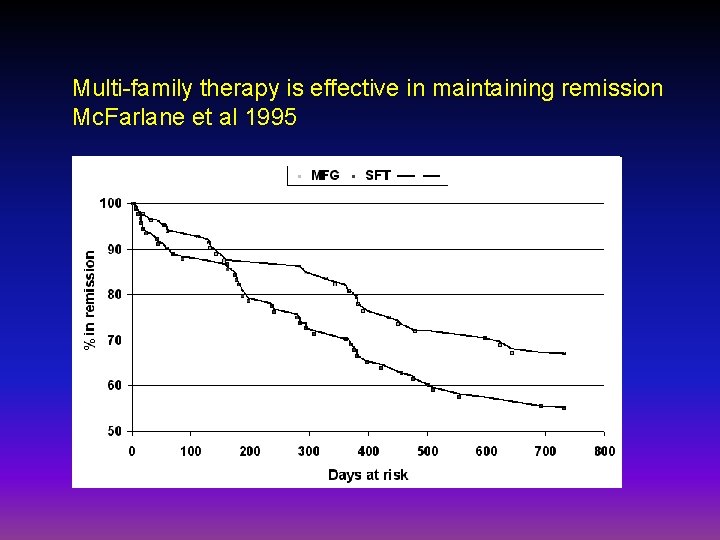
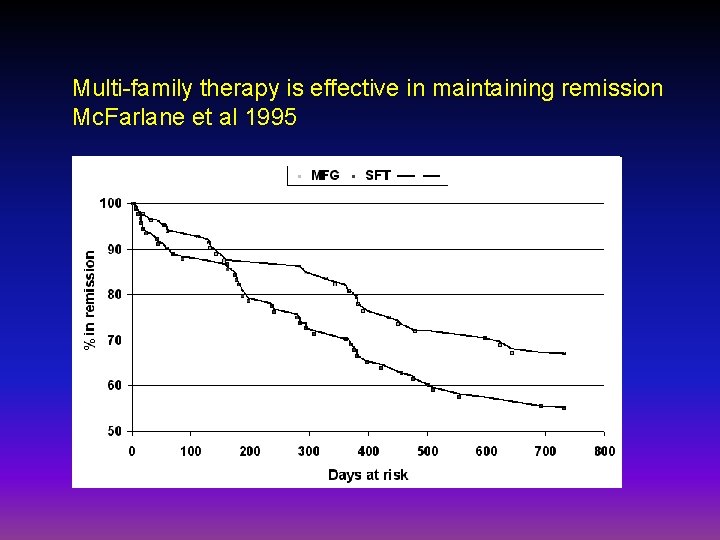
Multi-family therapy is effective in maintaining remission Mc. Farlane et al 1995
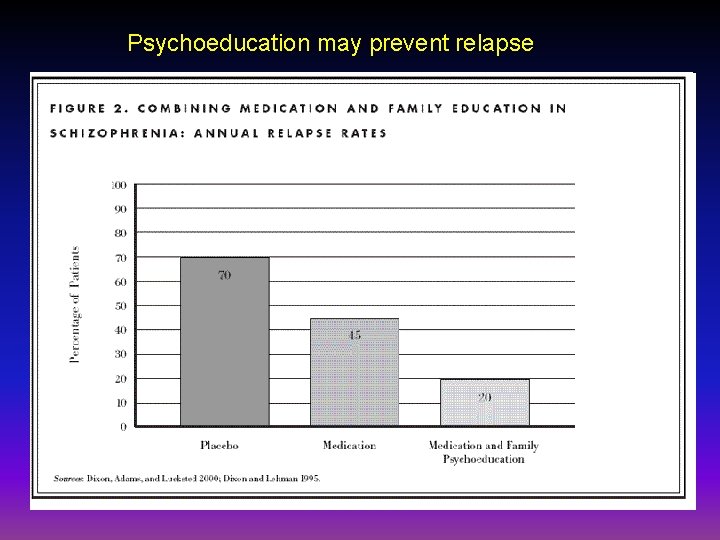
Psychoeducation may prevent relapse
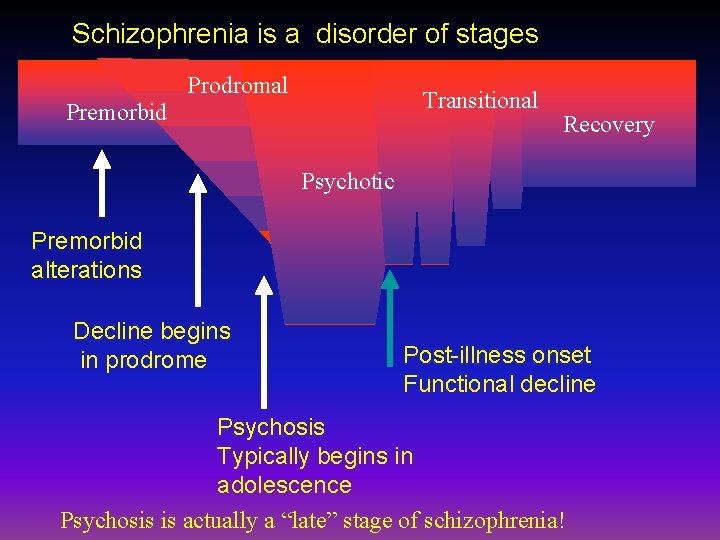
Key aspects of schizophrenia relevant for personal therapy: Schizophrenia is. . • A disease of Brain Development • A disease of risk and diathesis (Zubin: Environmental stress- Biological vulnerability model) • A disease of stages • A disease of affect as well as cognition.
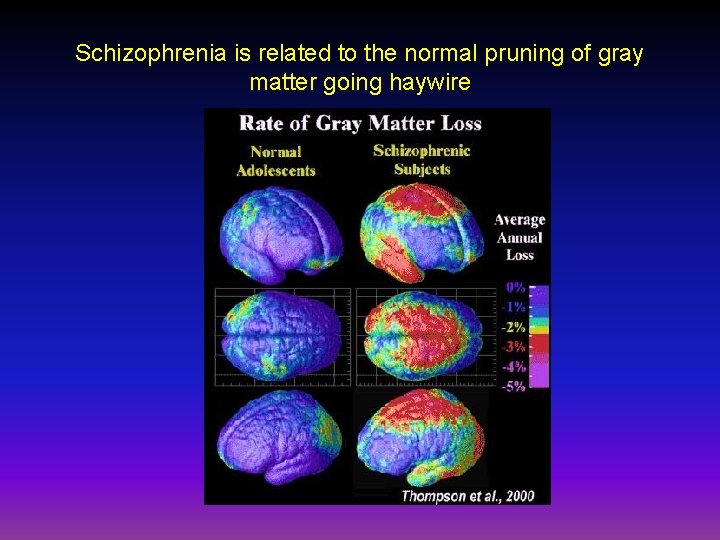
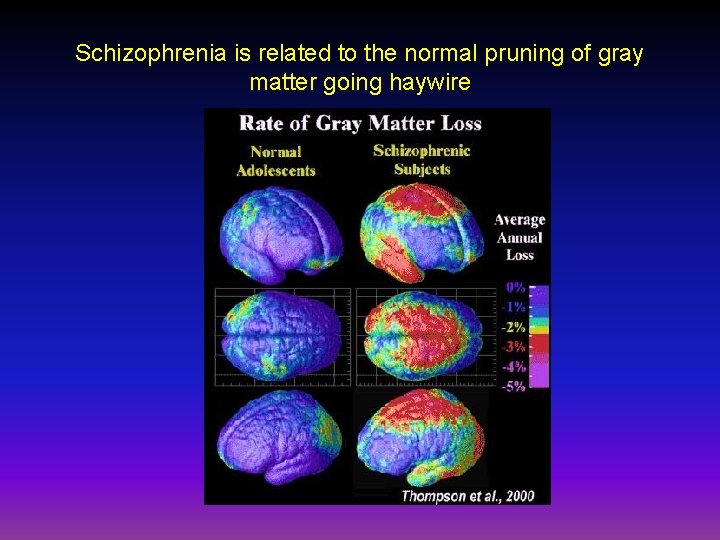
Schizophrenia is related to the normal pruning of gray matter going haywire

Gray matter loss might heighten stress responsivity (Zubin)
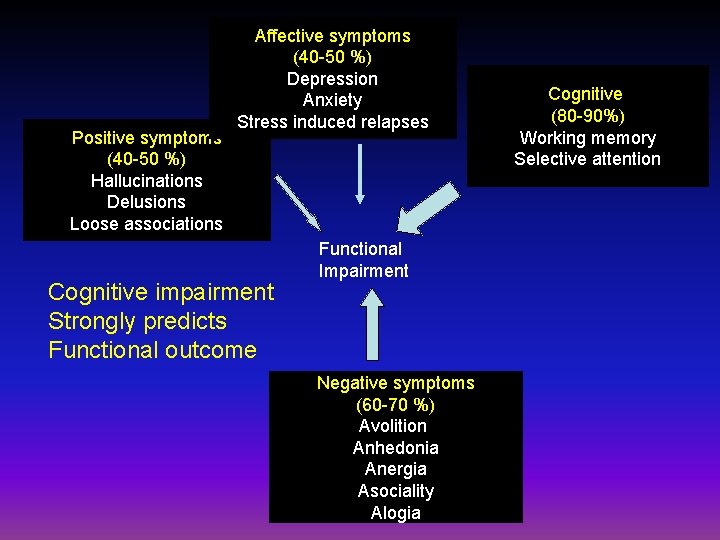
Schizophrenia is a Cognitive and an affective disorder • Pervasive cognitive deficits – Speed – Memory – Attention – Reasoning – Tact – Synthesis • Affect (the “affective paradox”) – Decreased expression – Increased arousal – Impaired regulation
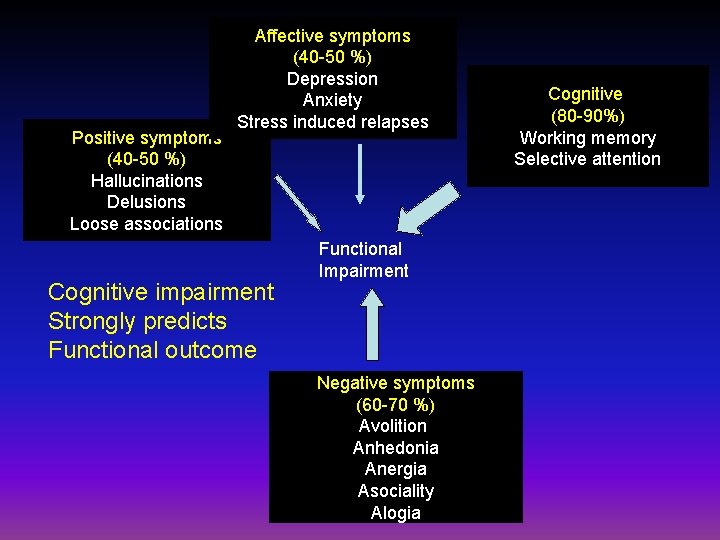
Positive symptoms (40 -50 %) Hallucinations Delusions Loose associations Affective symptoms (40 -50 %) Depression Anxiety Stress induced relapses Cognitive impairment Strongly predicts Functional outcome Functional Impairment Negative symptoms (60 -70 %) Avolition Anhedonia Anergia Asociality Alogia Cognitive (80 -90%) Working memory Selective attention
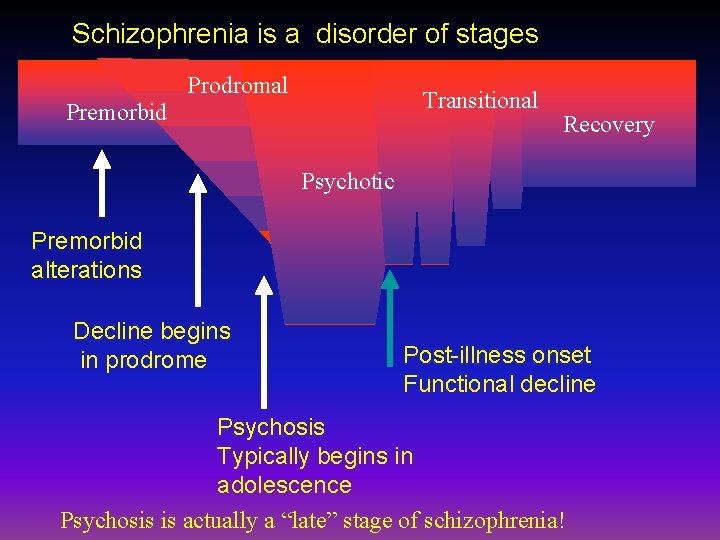
Schizophrenia is a disorder of stages Prodromal Transitional Premorbid Recovery Psychotic Premorbid alterations Decline begins in prodrome Post-illness onset Functional decline Psychosis Typically begins in adolescence Psychosis is actually a “late” stage of schizophrenia!
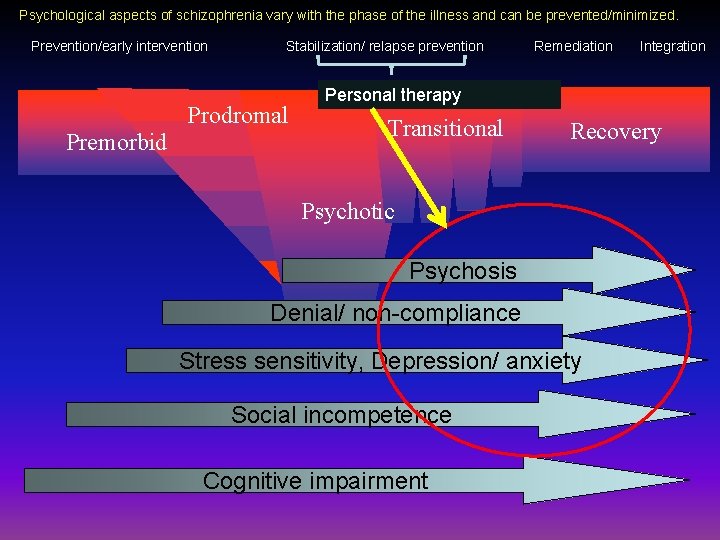
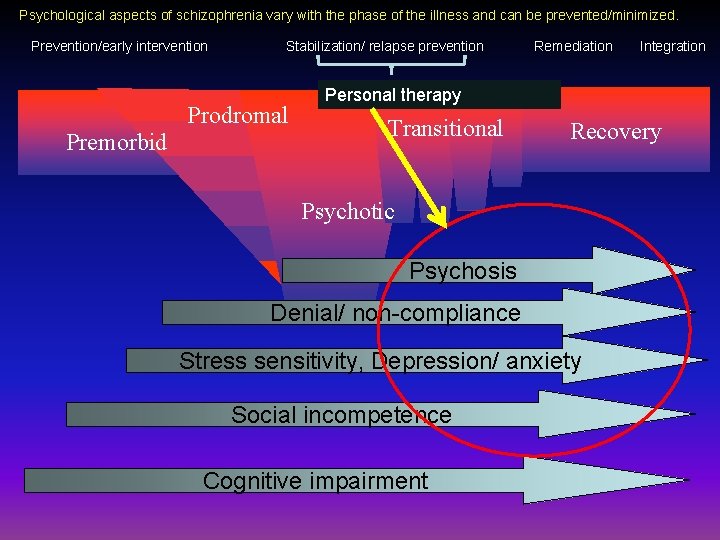
Psychological aspects of schizophrenia vary with the phase of the illness and can be prevented/minimized. Prevention/early intervention Stabilization/ relapse prevention Remediation Integration Prodromal Premorbid Personal therapy Transitional Recovery Psychotic Psychosis Denial/ non-compliance Stress sensitivity, Depression/ anxiety Social incompetence Cognitive impairment
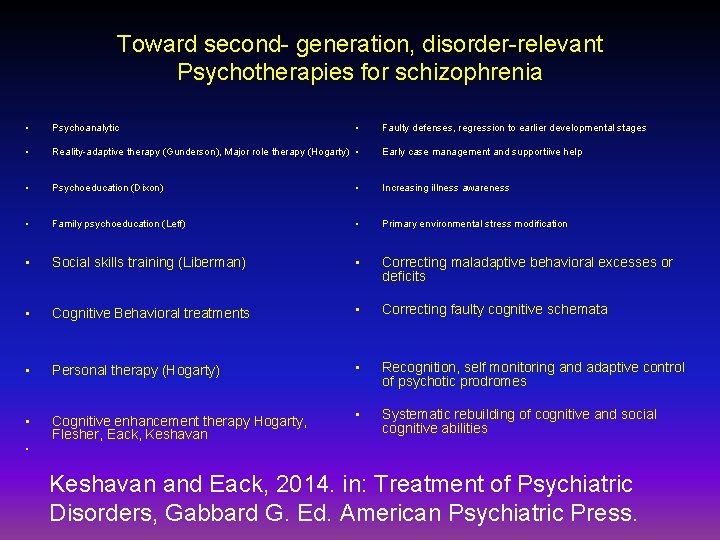
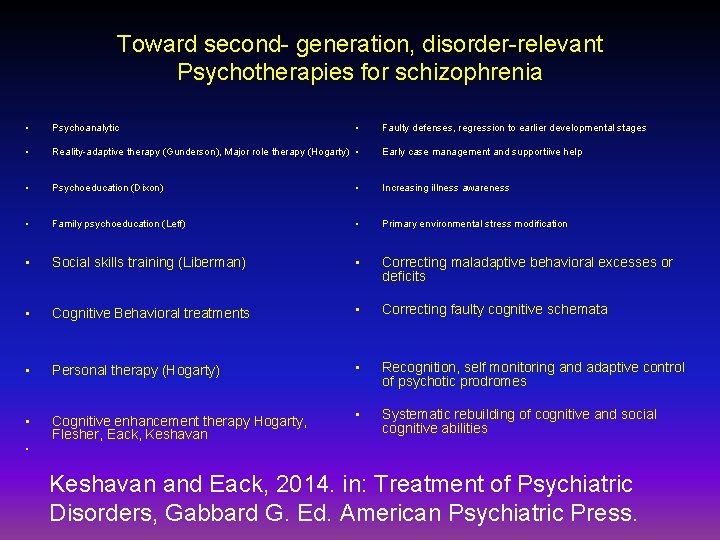
Toward second- generation, disorder-relevant Psychotherapies for schizophrenia • Psychoanalytic • • Reality-adaptive therapy (Gunderson), Major role therapy (Hogarty) • • Psychoeducation (Dixon) • Increasing illness awareness • Family psychoeducation (Leff) • Primary environmental stress modification • Social skills training (Liberman) • Correcting maladaptive behavioral excesses or deficits • Cognitive Behavioral treatments • Correcting faulty cognitive schemata • Personal therapy (Hogarty) • Recognition, self monitoring and adaptive control of psychotic prodromes • Cognitive enhancement therapy Hogarty, Flesher, Eack, Keshavan • Systematic rebuilding of cognitive and social cognitive abilities • Faulty defenses, regression to earlier developmental stages Early case management and supportiive help Keshavan and Eack, 2014. in: Treatment of Psychiatric Disorders, Gabbard G. Ed. American Psychiatric Press.
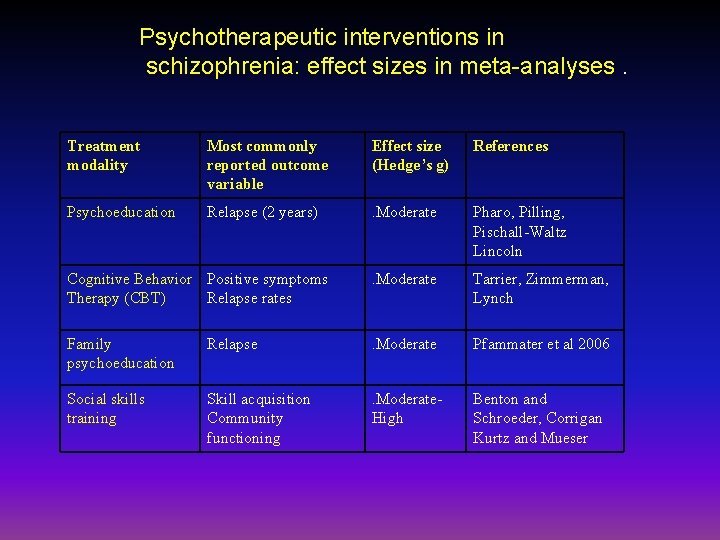
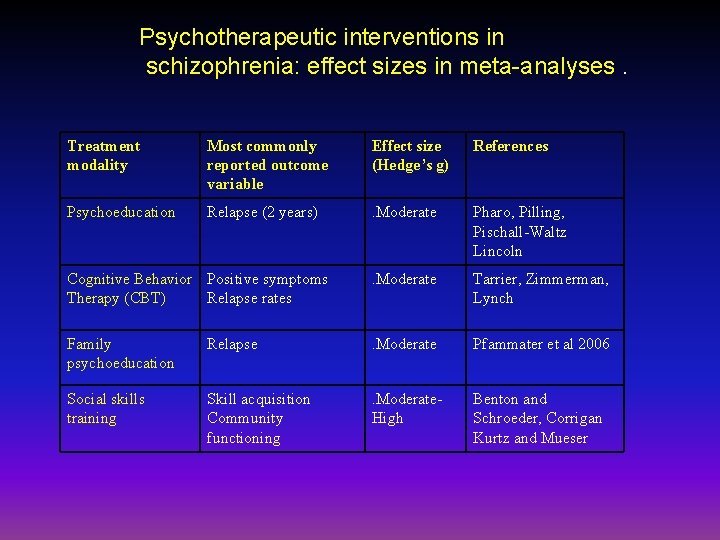
Psychotherapeutic interventions in schizophrenia: effect sizes in meta-analyses. Treatment modality Most commonly reported outcome variable Effect size (Hedge’s g) References Psychoeducation Relapse (2 years) . Moderate Pharo, Pilling, Pischall-Waltz Lincoln Cognitive Behavior Positive symptoms Therapy (CBT) Relapse rates . Moderate Tarrier, Zimmerman, Lynch Family psychoeducation Relapse . Moderate Pfammater et al 2006 Social skills training Skill acquisition Community functioning . Moderate. High Benton and Schroeder, Corrigan Kurtz and Mueser
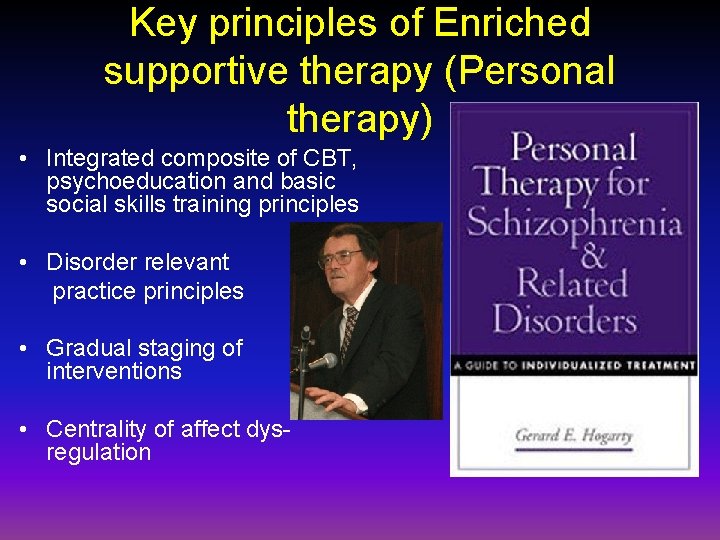
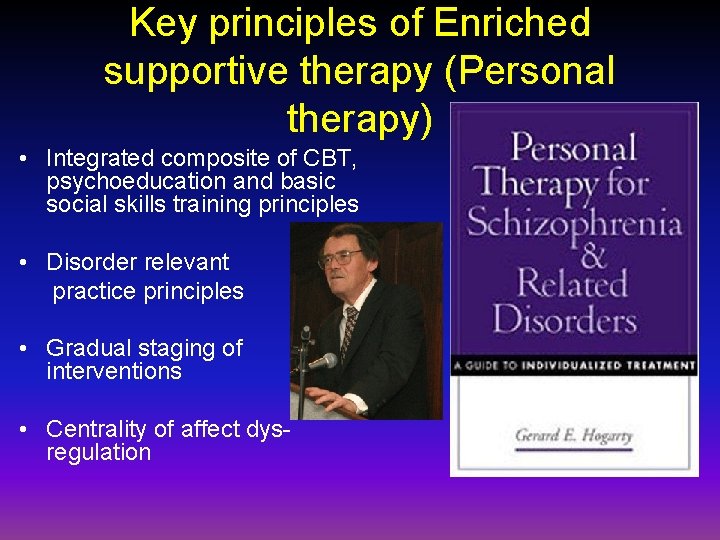
Key principles of Enriched supportive therapy (Personal therapy) • Integrated composite of CBT, psychoeducation and basic social skills training principles • Disorder relevant practice principles • Gradual staging of interventions • Centrality of affect dysregulation
Hogarty et al 1995
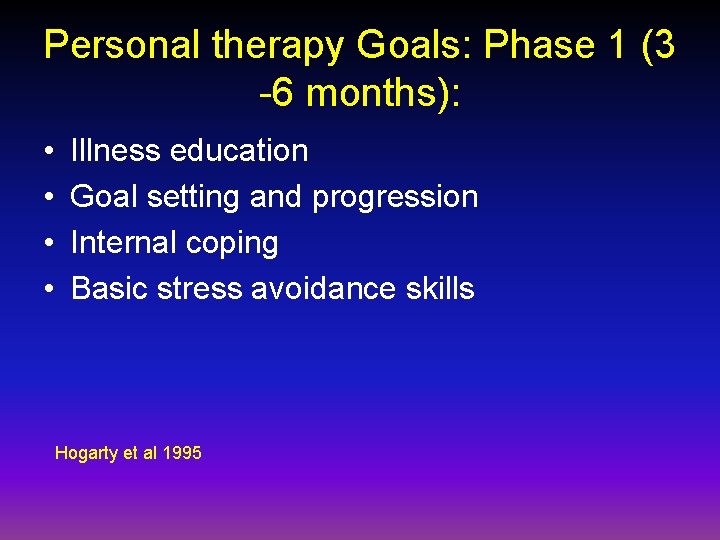
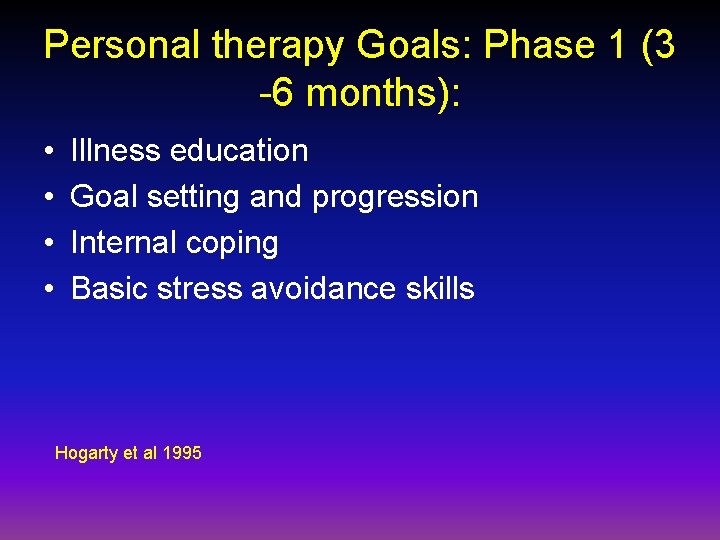
Personal therapy Goals: Phase 1 (3 -6 months): • • Illness education Goal setting and progression Internal coping Basic stress avoidance skills Hogarty et al 1995
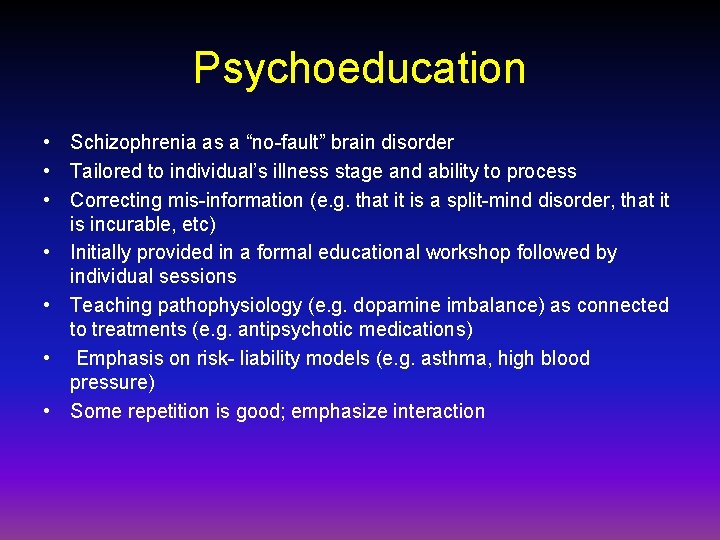
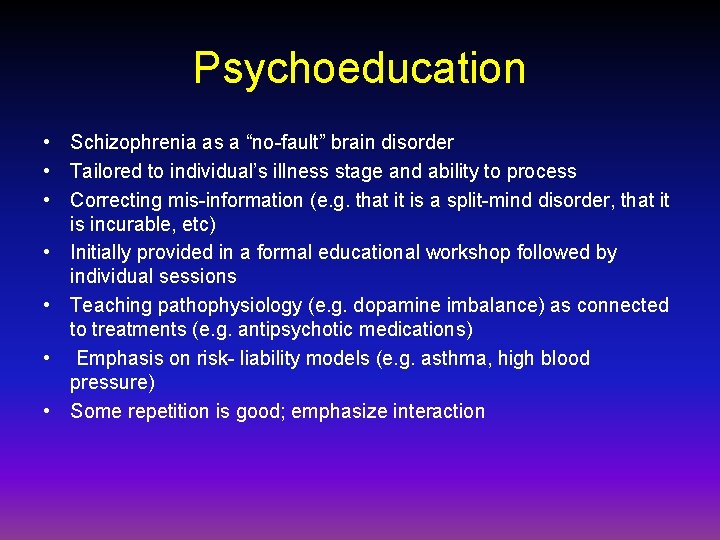
Psychoeducation • Schizophrenia as a “no-fault” brain disorder • Tailored to individual’s illness stage and ability to process • Correcting mis-information (e. g. that it is a split-mind disorder, that it is incurable, etc) • Initially provided in a formal educational workshop followed by individual sessions • Teaching pathophysiology (e. g. dopamine imbalance) as connected to treatments (e. g. antipsychotic medications) • Emphasis on risk- liability models (e. g. asthma, high blood pressure) • Some repetition is good; emphasize interaction

Resumption of daily tasks • Goal setting: Start from basic steps ( Focus on self care personal hygeine, nutrition, sleep) • Set up reasonable goals: “Internal yardstick” approach • Expectations to be adjusted to clinical state • Connect small goals to larger, long term goals • Expect set-backs; “ one step back and 2 steps forward rule) How do I measure Up to them? How do I measure Up to myself, then and now?
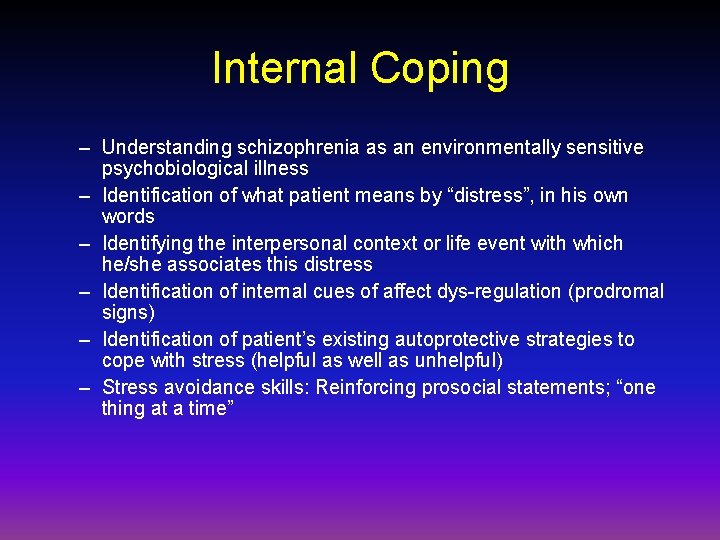
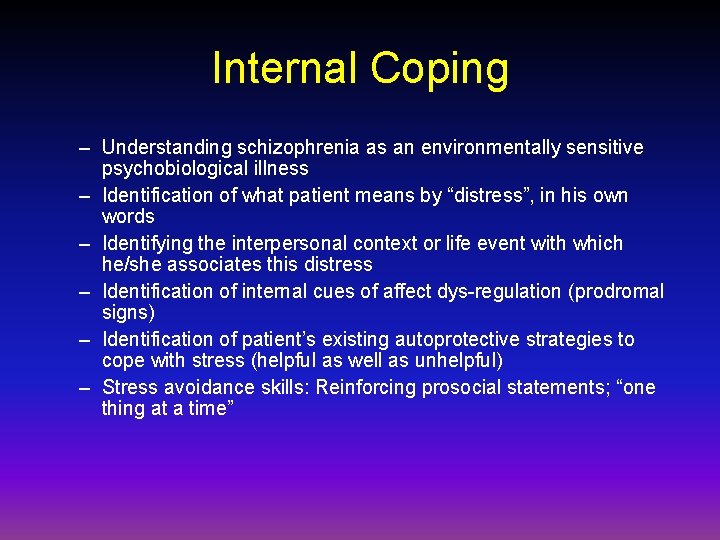
Internal Coping – Understanding schizophrenia as an environmentally sensitive psychobiological illness – Identification of what patient means by “distress”, in his own words – Identifying the interpersonal context or life event with which he/she associates this distress – Identification of internal cues of affect dys-regulation (prodromal signs) – Identification of patient’s existing autoprotective strategies to cope with stress (helpful as well as unhelpful) – Stress avoidance skills: Reinforcing prosocial statements; “one thing at a time”
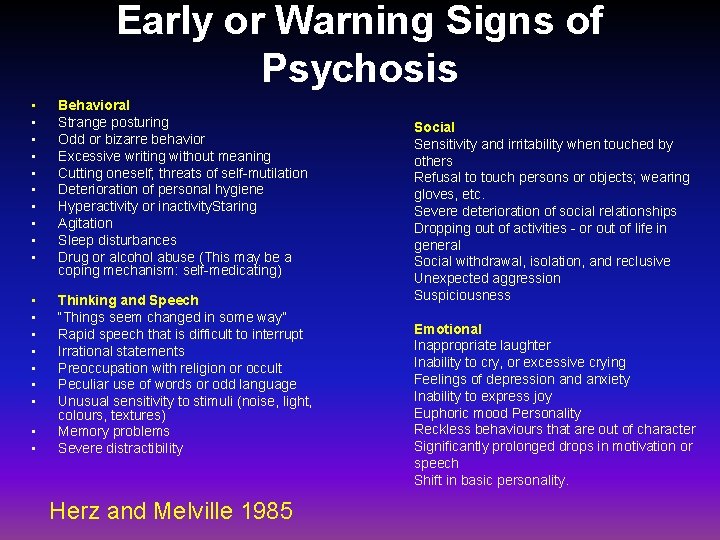
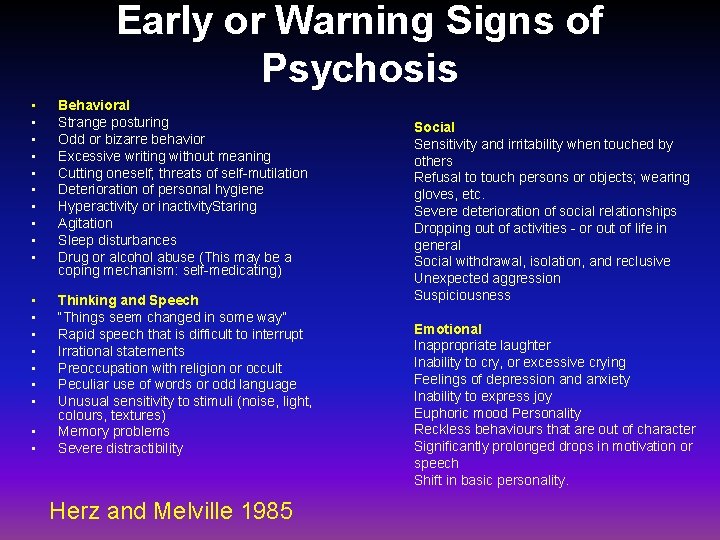
Early or Warning Signs of Psychosis • • • Behavioral Strange posturing Odd or bizarre behavior Excessive writing without meaning Cutting oneself; threats of self-mutilation Deterioration of personal hygiene Hyperactivity or inactivity. Staring Agitation Sleep disturbances Drug or alcohol abuse (This may be a coping mechanism: self-medicating) • • Thinking and Speech “Things seem changed in some way” Rapid speech that is difficult to interrupt Irrational statements Preoccupation with religion or occult Peculiar use of words or odd language Unusual sensitivity to stimuli (noise, light, colours, textures) Memory problems Severe distractibility • • Herz and Melville 1985 Social Sensitivity and irritability when touched by others Refusal to touch persons or objects; wearing gloves, etc. Severe deterioration of social relationships Dropping out of activities - or out of life in general Social withdrawal, isolation, and reclusive Unexpected aggression Suspiciousness Emotional Inappropriate laughter Inability to cry, or excessive crying Feelings of depression and anxiety Inability to express joy Euphoric mood Personality Reckless behaviours that are out of character Significantly prolonged drops in motivation or speech Shift in basic personality.
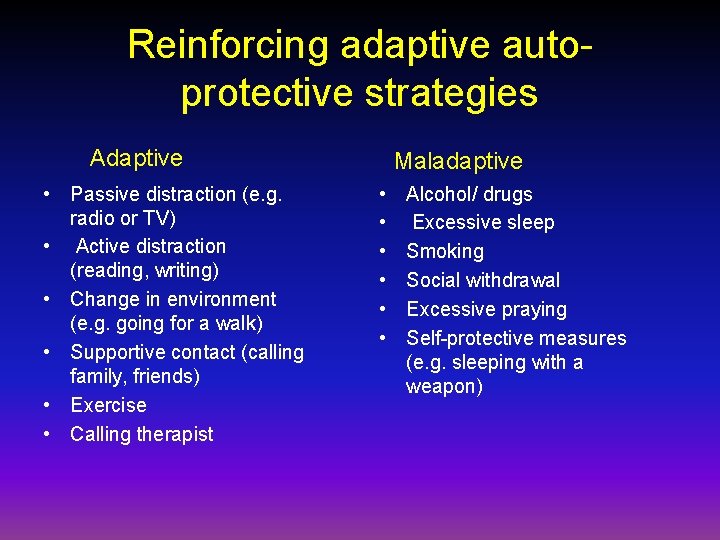
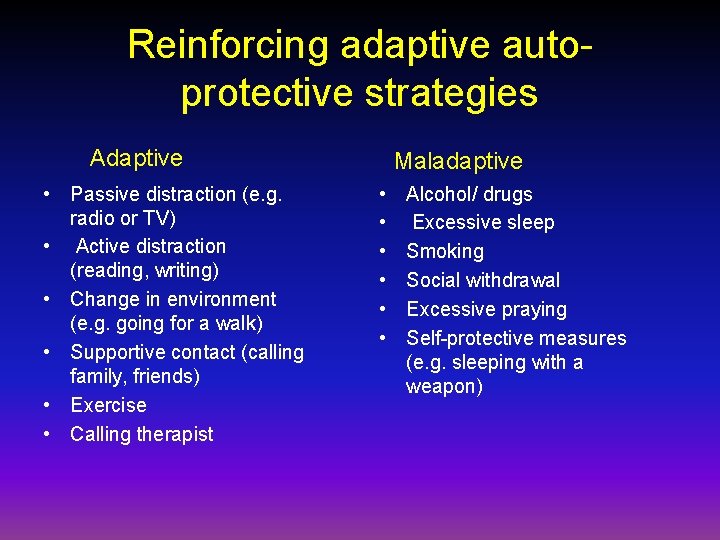
Reinforcing adaptive autoprotective strategies Adaptive • Passive distraction (e. g. radio or TV) • Active distraction (reading, writing) • Change in environment (e. g. going for a walk) • Supportive contact (calling family, friends) • Exercise • Calling therapist Maladaptive • • • Alcohol/ drugs Excessive sleep Smoking Social withdrawal Excessive praying Self-protective measures (e. g. sleeping with a weapon)
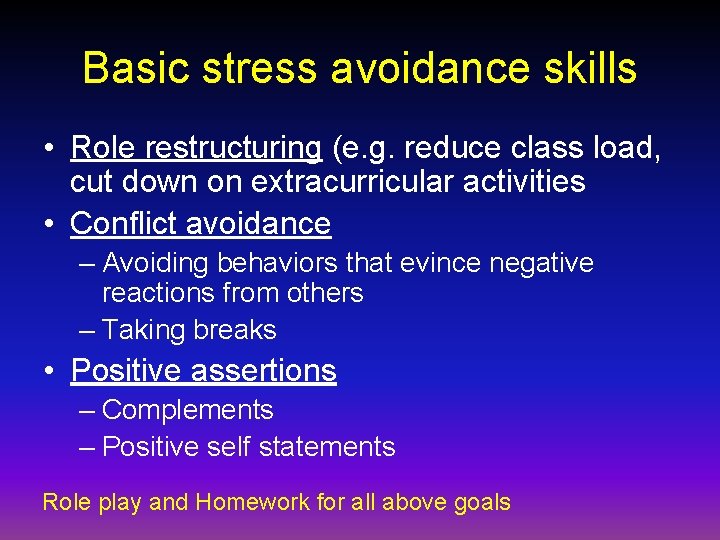
Basic stress avoidance skills • Role restructuring (e. g. reduce class load, cut down on extracurricular activities • Conflict avoidance – Avoiding behaviors that evince negative reactions from others – Taking breaks • Positive assertions – Complements – Positive self statements Role play and Homework for all above goals

Personal therapy: stages (contd) • Phase II (intermediate; 7 - 18 months) – Continued psychoeducation (goal: self- awareness; recognition of prodromal signs of relapse – Acquisition of adaptive techniques: Relaxation training; guided imagery/ music; active distraction techniques; basic conflict resolution skills Hogarty et al 1995
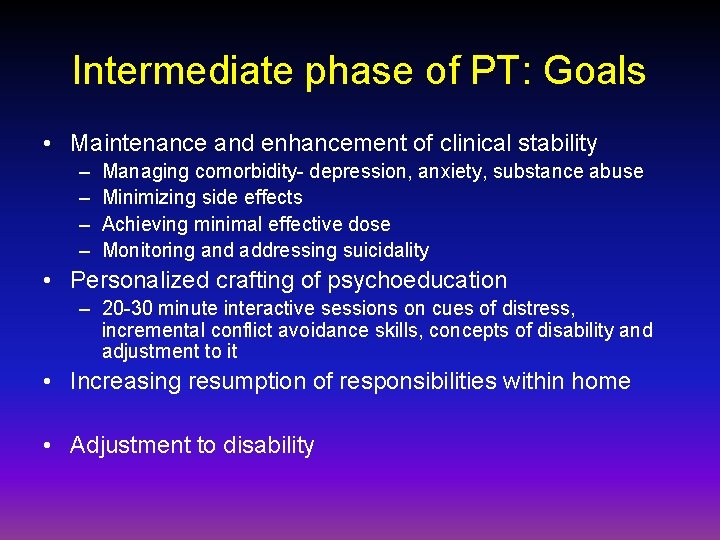
Intermediate phase of PT: Goals • Maintenance and enhancement of clinical stability – – Managing comorbidity- depression, anxiety, substance abuse Minimizing side effects Achieving minimal effective dose Monitoring and addressing suicidality • Personalized crafting of psychoeducation – 20 -30 minute interactive sessions on cues of distress, incremental conflict avoidance skills, concepts of disability and adjustment to it • Increasing resumption of responsibilities within home • Adjustment to disability
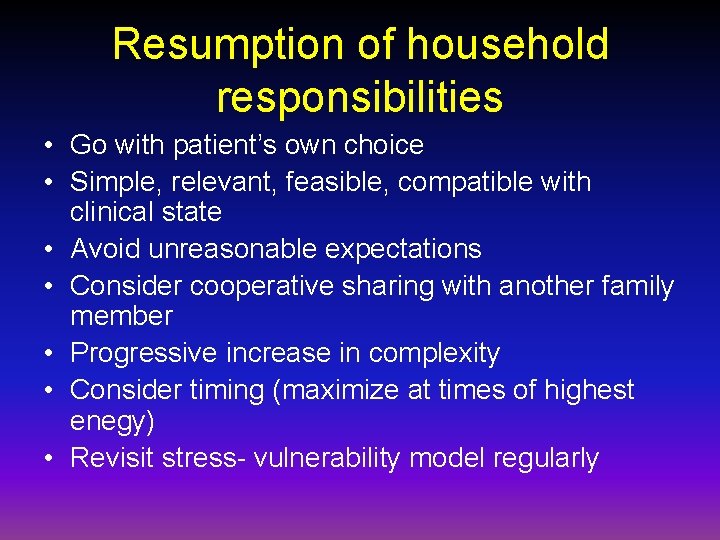
Resumption of household responsibilities • Go with patient’s own choice • Simple, relevant, feasible, compatible with clinical state • Avoid unreasonable expectations • Consider cooperative sharing with another family member • Progressive increase in complexity • Consider timing (maximize at times of highest enegy) • Revisit stress- vulnerability model regularly

Adjustment to disability • Exclusive strengths based approach may be counterproductive • Address denial, “Flight to normalcy” • Learning what to say and not say about one’s illness
Other techniques • Deep breathing and simple relaxation • Visual imagery • Criticism management
PT advanced phase (Interfaces and overlaps with Cognitive enhancement therapy 19 - 36 months) • Psychoeducation with a greater emphasis placed on the refined assessment of genuine, individual prodromes. • Addressing social and cognitive deficits, “one step at a time” • Managing Criticism, an assessment of its validity, learning a repertoire of verbal and behavioral responses designed to lessen the other person's intensity and to enhance the patient's social perception and negotiation skills • Advanced internal coping strategies include progressive relaxation training, which is designed to reduce autonomic arousal. • Independent application of various PT strategies in differing social contexts,

Conclusions • Schizophrenia is a developmental disorder of affect, behavior and cognition • Schizophrenia sequentially evolves with prodromal and psychotic phases Characterized by psychosis and affective dysregulation, followed by a transitional phase with recurrent relapses before finally a stable, chronic phase sets in, primarily with cognitive and negative symptoms • Treatment is best tailored to the aspects of illness prominently manifesting at the specific phases of the illness • Personal therapy is designed as a compehensive, step-wise approach to early phases of schizophrenia, involving psychoeducation, stress management and development of coping skills, setting a stage for rehabilitative approaches such as cognitive remediation •
 Types of psychotic disorders
Types of psychotic disorders Neurosis vs psychosis
Neurosis vs psychosis Qualities of a psychopath
Qualities of a psychopath Schizophreniform disorder icd-10
Schizophreniform disorder icd-10 Schizophrenia
Schizophrenia Distinguish between guidance and counseling
Distinguish between guidance and counseling Dodo bird conjecture
Dodo bird conjecture Counselling psychology doctorate
Counselling psychology doctorate Andrew pethebridge
Andrew pethebridge Transference ap psychology
Transference ap psychology Types of individual psychotherapy
Types of individual psychotherapy Child parent psychotherapy triangle
Child parent psychotherapy triangle Cognitive psychology ppt
Cognitive psychology ppt What is bracketing in counseling
What is bracketing in counseling General issues in psychotherapy
General issues in psychotherapy 19 propositions rogers
19 propositions rogers Psychotherapy refers to
Psychotherapy refers to Sadaf sajjad
Sadaf sajjad Counselling ppt
Counselling ppt Quantum psychotherapy
Quantum psychotherapy Imaginal disputation
Imaginal disputation Common factors approach psychotherapy integration
Common factors approach psychotherapy integration Modelo cognitivo
Modelo cognitivo Advanced psychotherapy
Advanced psychotherapy Psychotherapy examples
Psychotherapy examples Limitations of psychotherapy
Limitations of psychotherapy Scope of psychotherapy
Scope of psychotherapy Tension reduction cycle
Tension reduction cycle World council for psychotherapy
World council for psychotherapy Myeplg
Myeplg Sustainability principles and practice
Sustainability principles and practice Objectives of auditing
Objectives of auditing Computer security principles and practice
Computer security principles and practice Computer security principles and practice solutions
Computer security principles and practice solutions