Psychosocial Aspects of PCD Tamara Vance MSW LICSW






- Slides: 25
Psychosocial Aspects of PCD Tamara Vance, MSW, LICSW Anne Griffiths, MD Children’s Minnesota, PCDF Clinical and Research Network Accredited Center
No disclosures. © 2017
Learning Objectives • Present a case highlighting psychosocial needs/interventions • Review mental health issues in chronic medical conditions and impact • Discuss psychosocial issues in PCD patients and caregivers • Share our center’s process and experience screening for anxiety/depression • Future directions for the PCD community © 2017
Case Example: Meet Jack • 14 year old male • Clinical: NRD, chronic sinusitis, OM, bronchiectasis, SA, anxiety, depression • PCD suspected @ age 3, however diagnosis not confirmed until age 12 • Multiple school transfers, 504 plan in place, missed days, homebound program • Nonadherent to PCD medical therapy or psych f/u © 2017

Mental Health Issues in Chronic Medical Conditions • Elevated levels of stress, anxiety and depression found in patients and families with multiple chronic diseases • Chronic medical illness is a risk factor for psychiatric disorders • CF TIDES Study [Quittner, et al. 2014] • Depression: 10% of adolescents, 19% adults, 37% of mothers, 31% of fathers • Anxiety: 22% of adolescents , 32% of adults, 48% of mothers, 36% of fathers • HIGHEST anxiety and depression in CF caregivers increased risk in adolescents © 2017

Mental Health Issues with Chronic Medical Conditions • Increased medical symptoms and diminished health status • Lower health-related quality of life (HRQol) • Increased healthcare costs • Poor treatment adherence and symptom management • Increased hospitalizations © 2017

Psychosocial Topics in PCD Literature SLEEP DISTURBANCES SOCIAL FUNCTIONING Relationships Work/school Adjustment to diagnosis Alienation TREATMENT BURDEN & ADHERENCE © 2017 ANXIETY & DEPRESSION MALADAPTIVE COPING Embarrassment Concealment/Isolation Cognitive Dissonance SYMPTOMS Cough Secretion drainage Hearing loss Subfertility HRQo. L FAMILY FUNCTIONING DISEASE PROGRESSION Lucas et al. , Behan et al. , Mc. Manus et al. , Dell et al. , Carotenuto et al. , Schofield et al. , Taelman, Pifferi et al. , Madsen et al. , Whalley et al. Sha, YW et al.
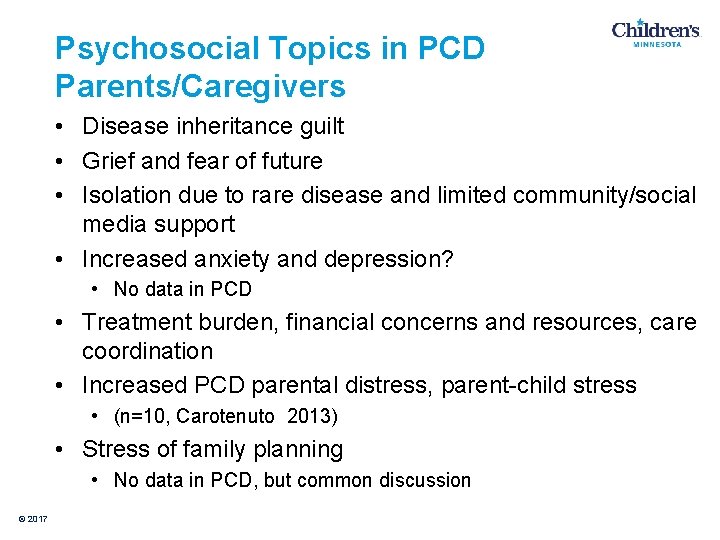
Psychosocial Topics in PCD Parents/Caregivers • Disease inheritance guilt • Grief and fear of future • Isolation due to rare disease and limited community/social media support • Increased anxiety and depression? • No data in PCD • Treatment burden, financial concerns and resources, care coordination • Increased PCD parental distress, parent-child stress • (n=10, Carotenuto 2013) • Stress of family planning • No data in PCD, but common discussion © 2017
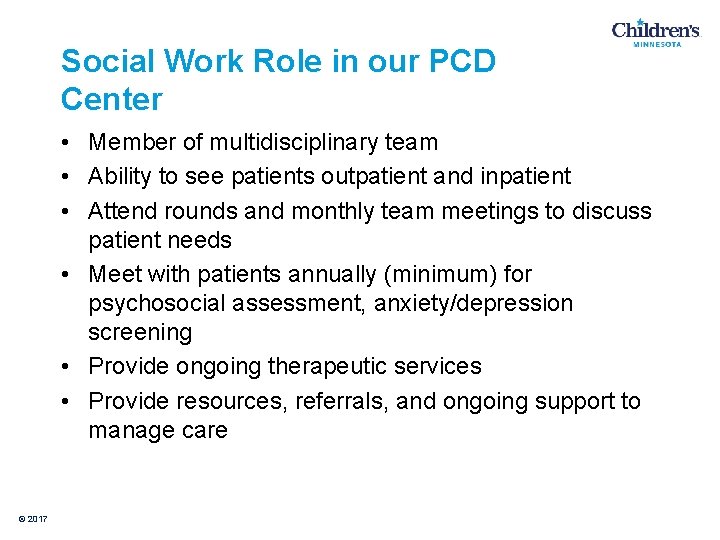
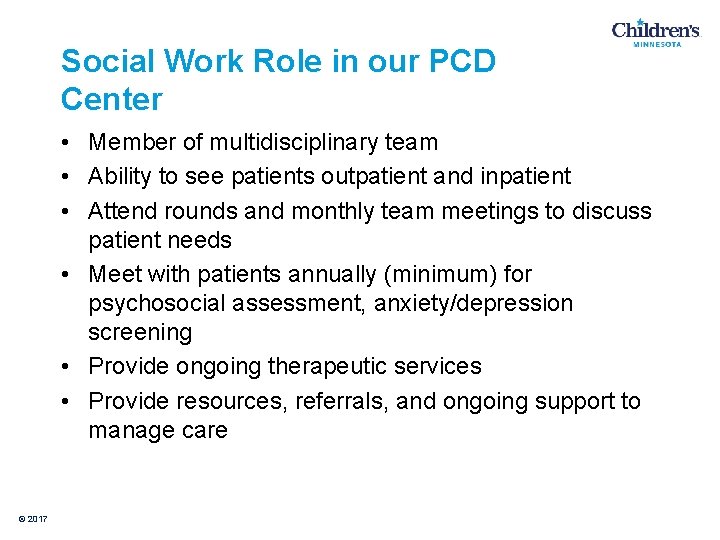
Social Work Role in our PCD Center • Member of multidisciplinary team • Ability to see patients outpatient and inpatient • Attend rounds and monthly team meetings to discuss patient needs • Meet with patients annually (minimum) for psychosocial assessment, anxiety/depression screening • Provide ongoing therapeutic services • Provide resources, referrals, and ongoing support to manage care © 2017
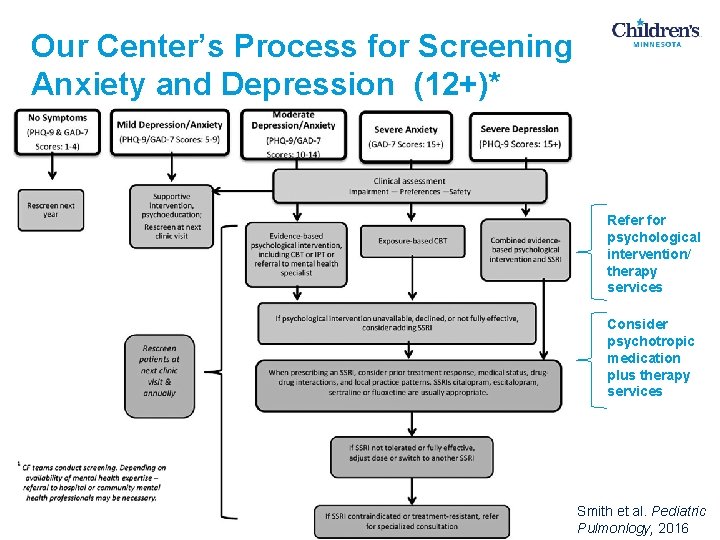
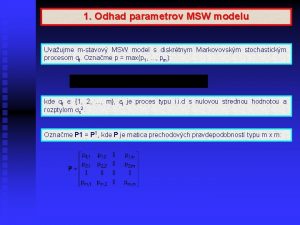
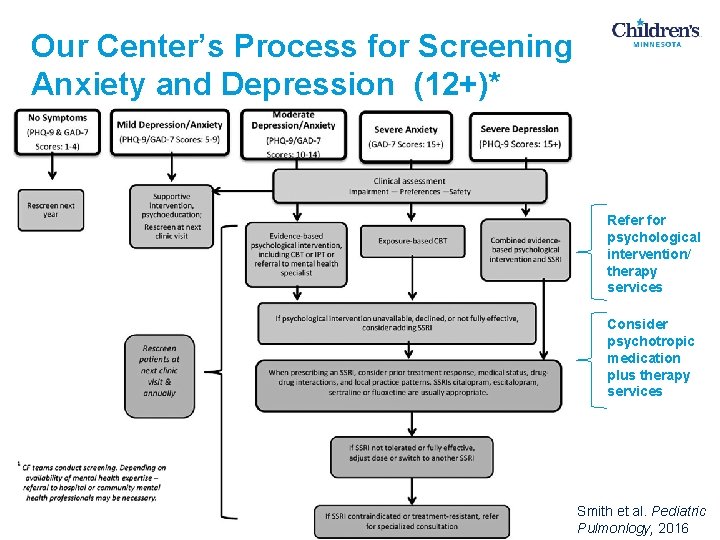
Our Center’s Process for Screening Anxiety and Depression (12+)* Refer for psychological intervention/ therapy services Consider psychotropic medication plus therapy services © 2017 Smith et al. Pediatric Pulmonlogy, 2016
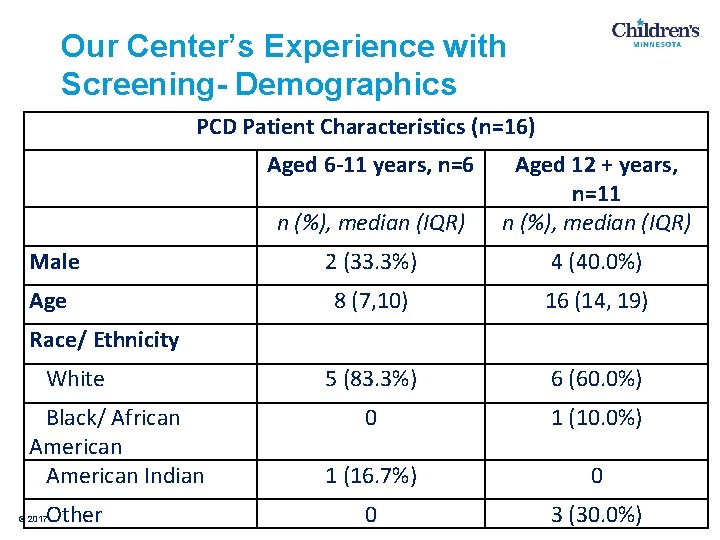
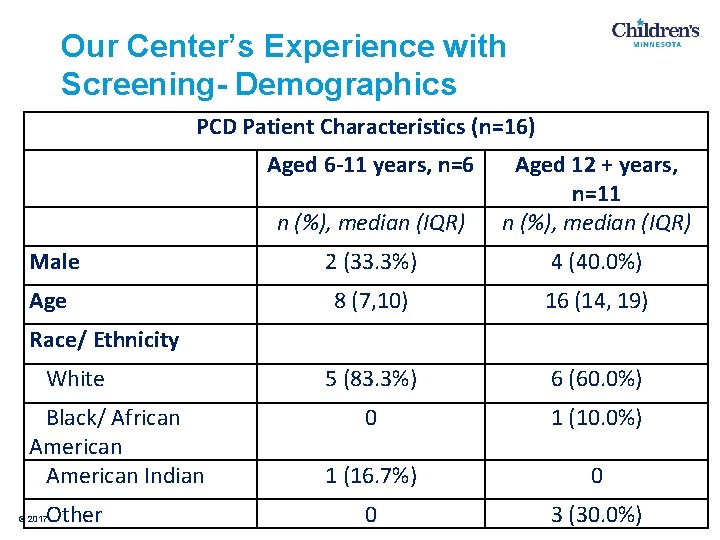
Our Center’s Experience with Screening- Demographics PCD Patient Characteristics (n=16) Aged 6 -11 years, n=6 n (%), median (IQR) Aged 12 + years, n=11 n (%), median (IQR) Male 2 (33. 3%) 4 (40. 0%) Age 8 (7, 10) 16 (14, 19) 5 (83. 3%) 6 (60. 0%) 0 1 (10. 0%) 1 (16. 7%) 0 0 3 (30. 0%) Race/ Ethnicity White Black/ African American Indian Other © 2017
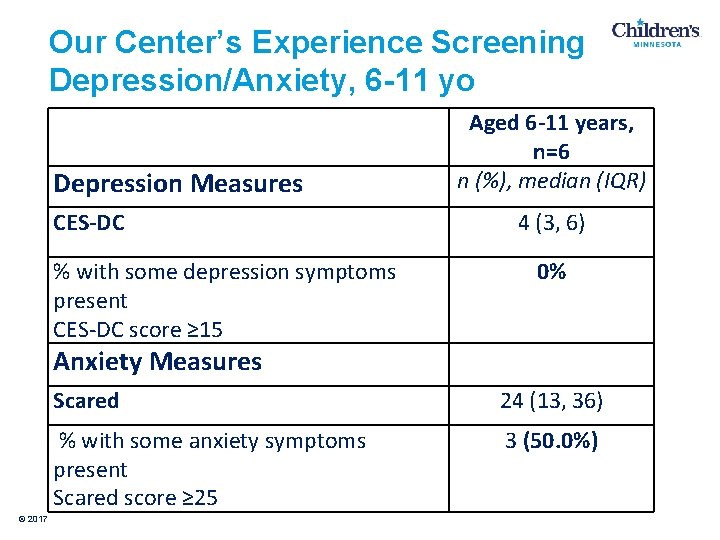
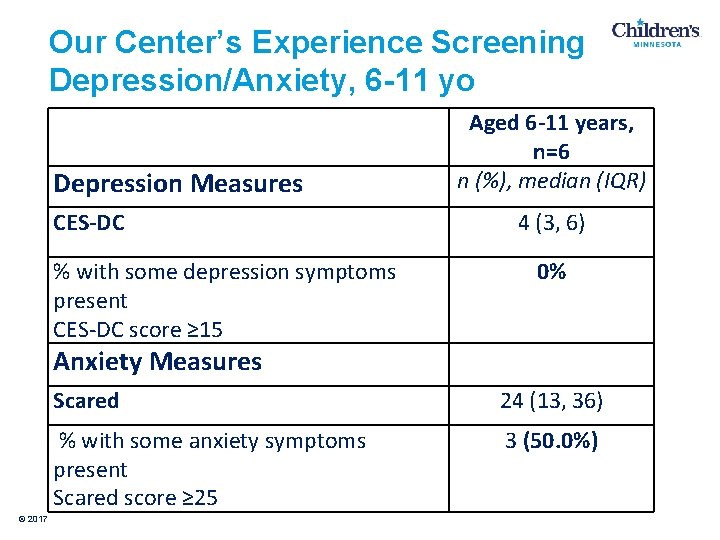
Our Center’s Experience Screening Depression/Anxiety, 6 -11 yo Depression Measures CES-DC % with some depression symptoms present CES-DC score ≥ 15 Aged 6 -11 years, n=6 n (%), median (IQR) 4 (3, 6) 0% Anxiety Measures © 2017 Scared 24 (13, 36) % with some anxiety symptoms present Scared score ≥ 25 3 (50. 0%)
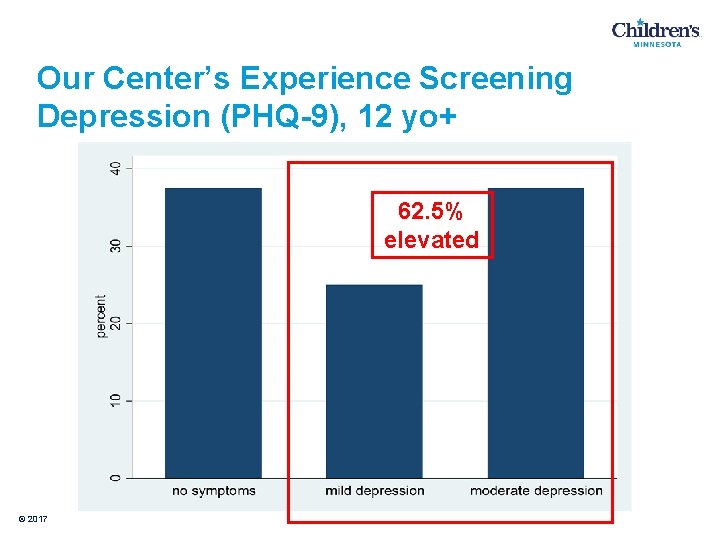
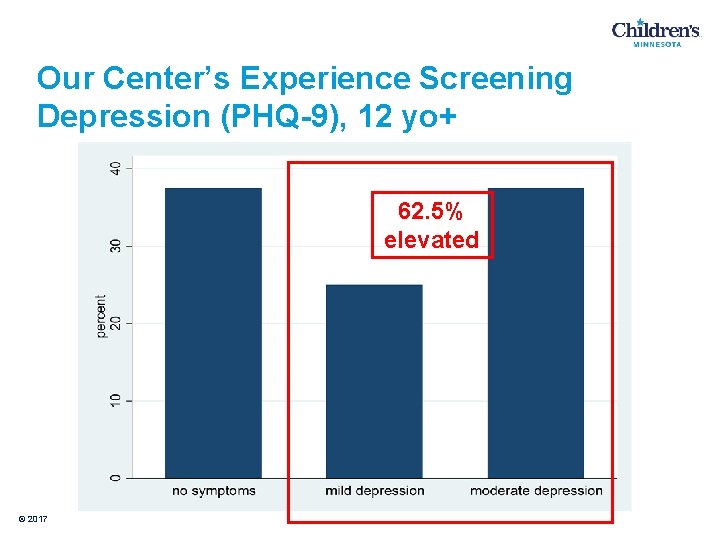
Our Center’s Experience Screening Depression (PHQ-9), 12 yo+ 62. 5% elevated © 2017
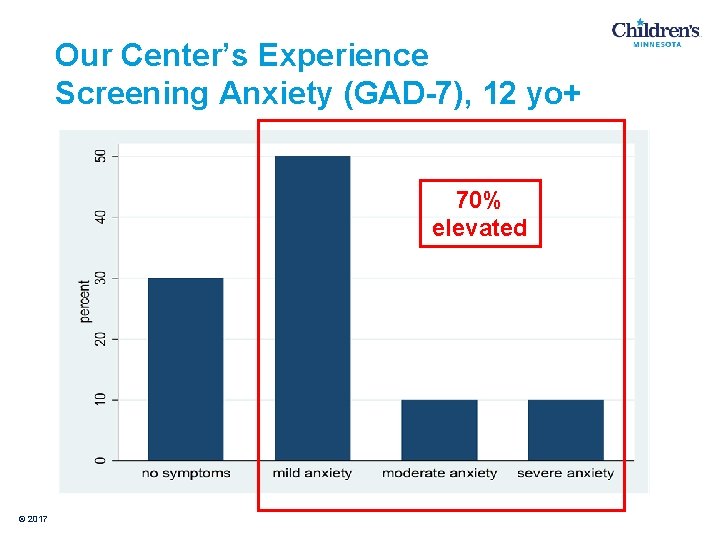
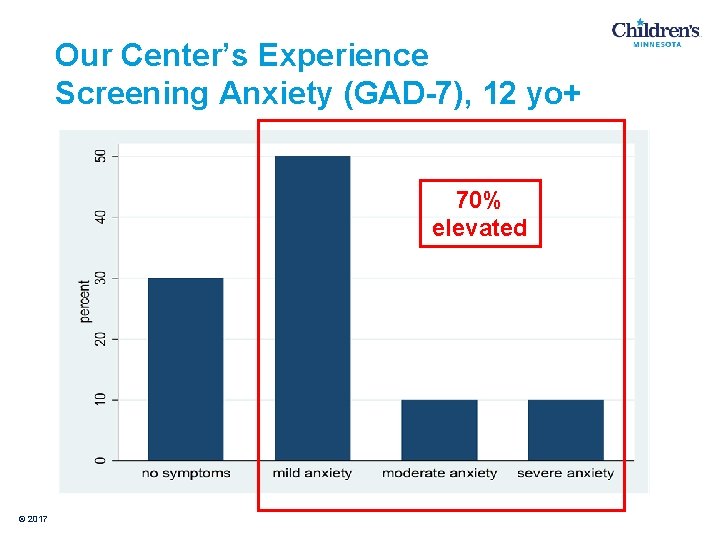
Our Center’s Experience Screening Anxiety (GAD-7), 12 yo+ 70% elevated © 2017
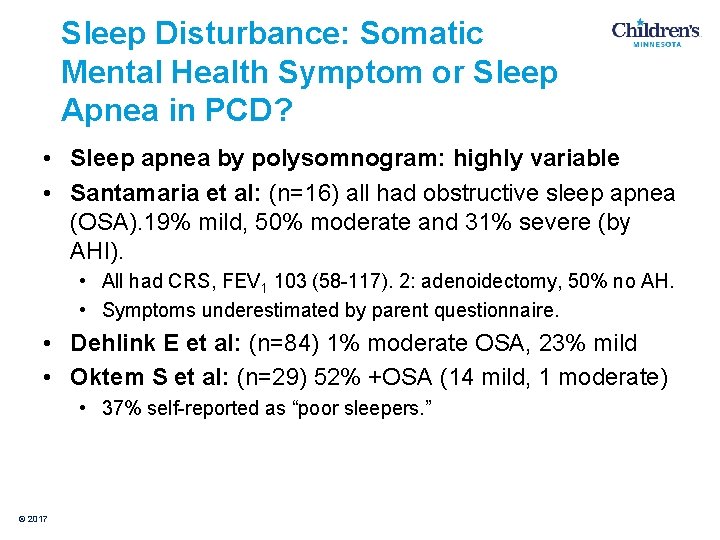
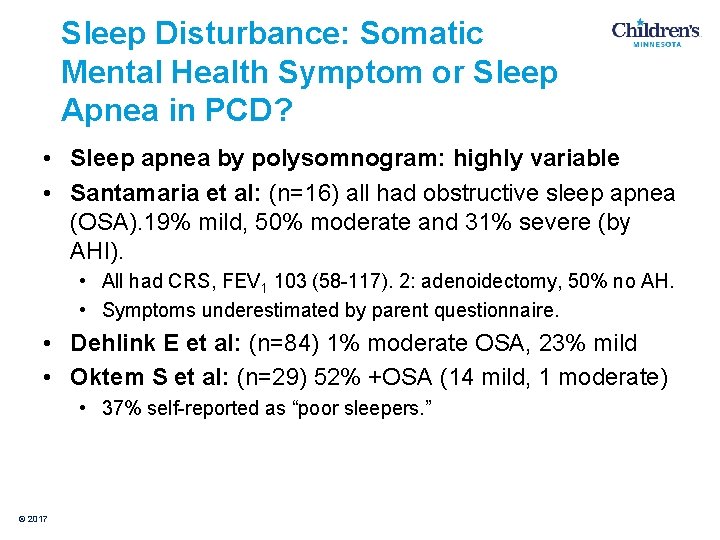
Sleep Disturbance: Somatic Mental Health Symptom or Sleep Apnea in PCD? • Sleep apnea by polysomnogram: highly variable • Santamaria et al: (n=16) all had obstructive sleep apnea (OSA). 19% mild, 50% moderate and 31% severe (by AHI). • All had CRS, FEV 1 103 (58 -117). 2: adenoidectomy, 50% no AH. • Symptoms underestimated by parent questionnaire. • Dehlink E et al: (n=84) 1% moderate OSA, 23% mild • Oktem S et al: (n=29) 52% +OSA (14 mild, 1 moderate) • 37% self-reported as “poor sleepers. ” © 2017

Our Center’s Experience. Sleep/Somatic Overlap, 6 -11 yo Table 1. Summary of Responses to Specific Depression/ Anxiety Scores Related to Sleep Quality in Children Aged 6 -11 years, n=6. Scared Q 2. I get headaches when I’m at school. CES-DC Q 5. I felt like I couldn’t pay attention to what I was doing. CES-DC Q 7. I felt like I was too tired to do things. © 2017 % Answered in affirmative 5 (83. 3%) 1 (16. 7%) 5 (83. 3%) CES-DC Q 11. I didn’t sleep as well as I usually sleep. 0 (0%) CES-DC Q 20. It was hard to get started doing things. 1 (16. 7%)
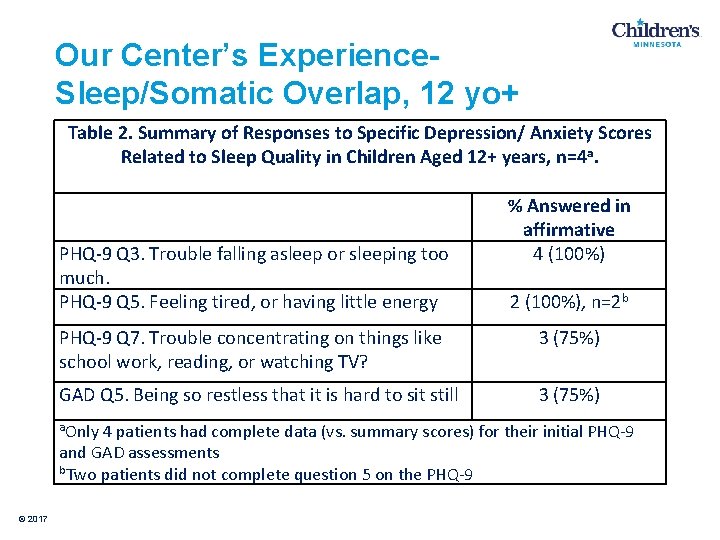
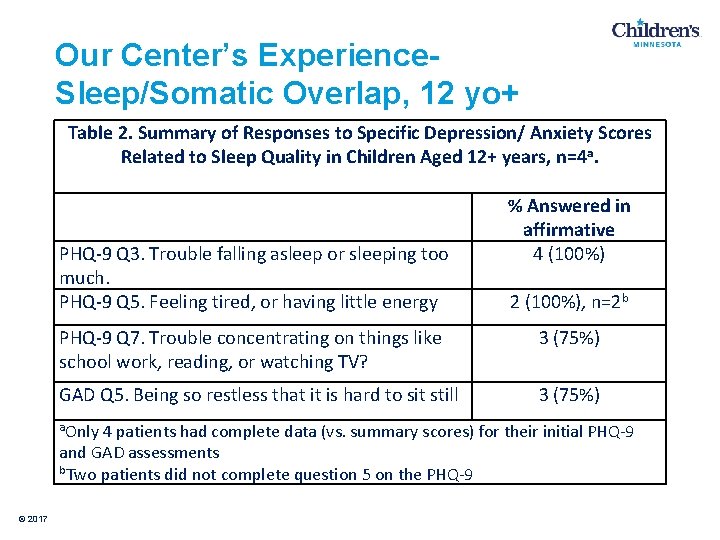
Our Center’s Experience. Sleep/Somatic Overlap, 12 yo+ Table 2. Summary of Responses to Specific Depression/ Anxiety Scores Related to Sleep Quality in Children Aged 12+ years, n=4 a. PHQ-9 Q 3. Trouble falling asleep or sleeping too much. PHQ-9 Q 5. Feeling tired, or having little energy % Answered in affirmative 4 (100%) 2 (100%), n=2 b PHQ-9 Q 7. Trouble concentrating on things like school work, reading, or watching TV? 3 (75%) GAD Q 5. Being so restless that it is hard to sit still 3 (75%) a. Only 4 patients had complete data (vs. summary scores) for their initial PHQ-9 and GAD assessments b. Two patients did not complete question 5 on the PHQ-9 © 2017
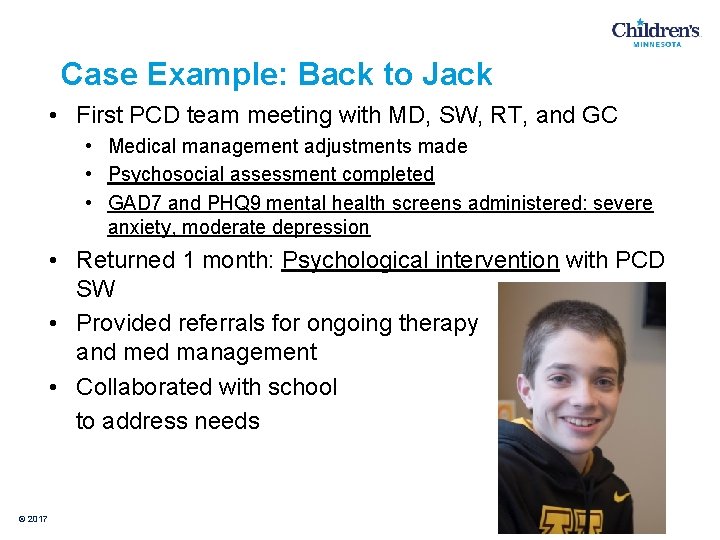
Case Example: Back to Jack • First PCD team meeting with MD, SW, RT, and GC • Medical management adjustments made • Psychosocial assessment completed • GAD 7 and PHQ 9 mental health screens administered: severe anxiety, moderate depression • Returned 1 month: Psychological intervention with PCD SW • Provided referrals for ongoing therapy and med management • Collaborated with school to address needs © 2017
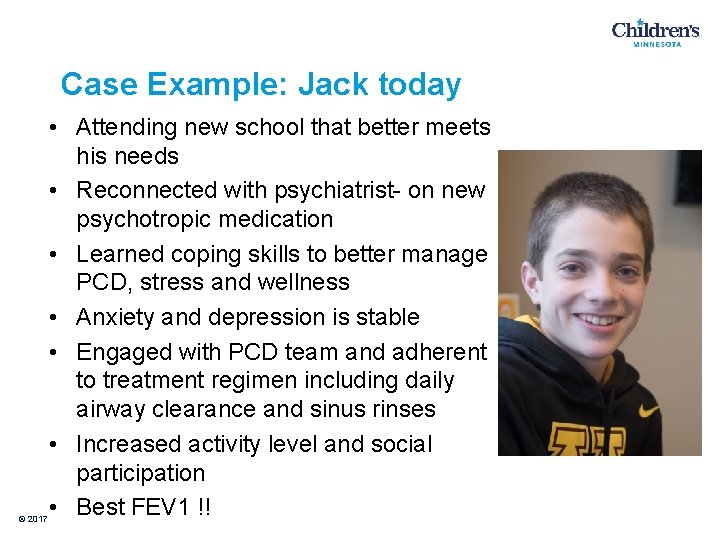
Case Example: Jack today © 2017 • Attending new school that better meets his needs • Reconnected with psychiatrist- on new psychotropic medication • Learned coping skills to better manage PCD, stress and wellness • Anxiety and depression is stable • Engaged with PCD team and adherent to treatment regimen including daily airway clearance and sinus rinses • Increased activity level and social participation • Best FEV 1 !!
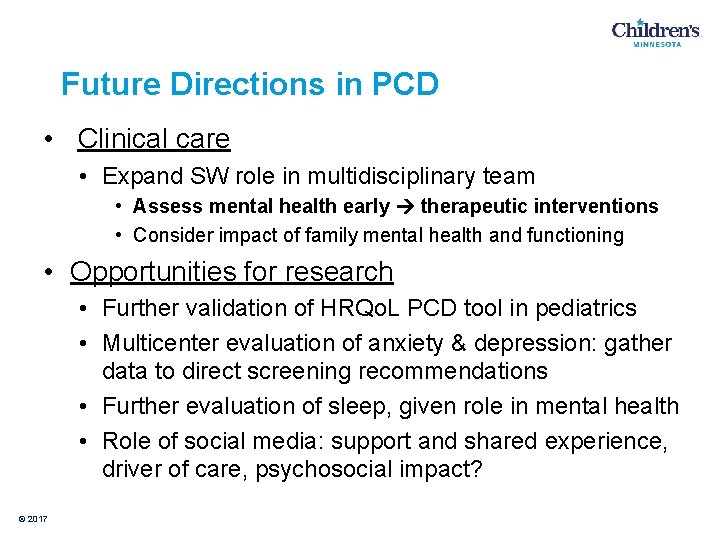
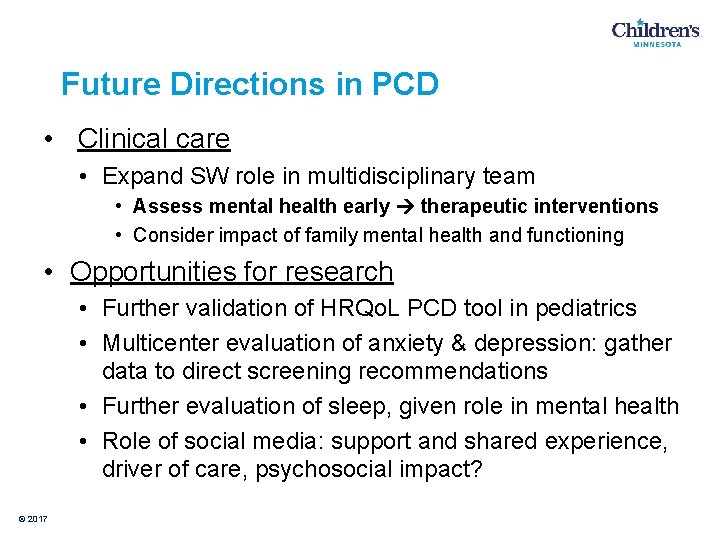
Future Directions in PCD • Clinical care • Expand SW role in multidisciplinary team • Assess mental health early therapeutic interventions • Consider impact of family mental health and functioning • Opportunities for research • Further validation of HRQo. L PCD tool in pediatrics • Multicenter evaluation of anxiety & depression: gather data to direct screening recommendations • Further evaluation of sleep, given role in mental health • Role of social media: support and shared experience, driver of care, psychosocial impact? © 2017

Children’s Minnesota PCD Center Pulmonary PCD Center Director and Associate Director: Bill Wheeler and Anne Griffiths Pulmonologists: Cindy Brady, Keith Cavanaugh, Julie Herda, Paul Kubic, Steve Kurachek, John Mc. Namara, Christina Mikesell, Brooke Moore, Mike Pryor, Mike Shreve, and Daniela Zgherea Genetics: Renee Temme Respiratory Therapy: John Plante Pulmonary Diagnostics: Julie Griffin, Kay Kufahl, Katie Johnson Social Worker: Tami Vance RN CNP Center Coordinator: Mary Sachs Patient Care Coordinator: Sarah Bevin © 2017 PCD Nursing Staff: Rachel Scholz and Rachel Barrett Clinical Research: Anne Mills, Elizabeth Thompson, Christine Benoit, and Mike Finch Otolaryngology: Bob Tibesar Pathology: Megan Dishop Specialty Care Division Senior Medical Director: Nancy Mendelsohn Radiology: Bill Mize Neonatology: Jane Barthell, Anastasia Ketko Cardiology: Charles Baker Immunology: Tamara Pozos Adult Pulmonology: Joanne Billings and Jordan Dunitz
References Behan L, Leigh MW, Dell SD, et al. Validation of a health related quality of life instrument for primary ciliary dyskinesia (QOL-PCD). Thorax 2017; 0: 1 -8. doi: 10. 1136/thoraxjnl-2016 -209356 Behan L, et al. The patient’s experience of primary ciliary dyskinesia: a systematic review. Qual Life Res. 30 March 2017 doi: 10. 1007/s 11136 -017 -1564 -y Boat, TF, Filigno, S and RS Amin. Wellness for Families of Children With Chronic Health Disorder. JAMA Pediatr. 2017. doi: 10. 1001/jamapedatrics. 2017. 1682. Carotenuto M, Esposito M, Di Pasquale F, De Stefano S, Santamaria F. Psychological, Cognitive and Maternal Stress Assessment in Children with Primary Ciliary Dyskinesia. World J Pediatr. 2013; 9: 312 -7. Compas, BE, et al. Coping with Chronic Illness in Childhood and Adolescence. Annu Rev Clin Psychol. 2012; 8: 455 -80. Dell SD, et al. Primary Ciliary Dyskinesia: First Health-Related Quality-of-Life Measures for Pediatric Patients. Ann Am Thorac Soc. 2016; 13: 1726 -35. De. Coster, VA. Challenges of type 2 diabetes and role of health care social work: a neglected area of practice. Health Soc Work. 2001; 26: 26 -37. Dehlink E et al. Sleep disordered breathing in children with primary ciliary dyskinesia (PCD). Eur Respir J 016; 48: PA 376. Di. Matteo MR, Lepper HS, and TW Croghan. Depression is a Risk Factor for Noncompliance with Medical Treatment: meta-analysis of the effects of Anxiety and Depression on Patient Adherence. Arch Intern Med. 2000; 160: 2101 -7. Ede LV, et al. Prevalence of depression in patients with chronic obstructive pulmonary disease: a systematic review. Thorax 1999; 54: 688 -92. Garber, J. and Weersing, VR. Comorbidity of Anxiety and Depression in Youth: Implications for Treatment and Prevention. Clin Psychol (New York). 2010 December; 17(4): 293 -306. © 2017
References Hosie P, et al. Primary ciliary dyskinesia: Overlooked and undertreated in children. J Pediatr Child Health. 2014; 50: 952 -8. Katon W, Lin EH and K Kroenke. The Association of Depression and Anxiety with Medical Symptom Burden in Patients with Chronic Medical Illness. Gen Hosp Psychiatry. 2007; 29: 147 -55. Kuehni CE, et al. Factors influencing age at diagnosis of primary ciliary dyskinesia in European children. Eur Respir J. 2010; 36: 1248 -58. Lucas JS, et al. A Quality-of-Life Measure For Adults With Primary Ciliary Dyskinesia: QOL-PCD. Eur Respir J 2015; 46: 375 -83. Mackner LM et al. Psychosocial Issues in Pediatric Inflammatory Bowel Disease: a clinical report of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2013; 56: 449 -58. Mc. Manus IC, Stubbings GF, & N. Martin. Stigmatization Physical Illness and Mental Health in Primary Ciliary Dyskinesia. J Health Psychol, 2006; 11: 467 -82. Mc. Manus IC, et al. Primary ciliary dyskinesia (Siewert’s / Kartagener’s Syndrome): Respiratory symptoms and psycho-social impact. BMC Pulm Med, 2003; 3: 4 Nathan, AM, et al. Review: Quality of Life in Children with Non-cystic Fibrosis Bronchiectasis. Front. Pediatr. 5: 84. doi: 10. 3389/fped. 2017. 00084. O’Connor MG, et al. Early Diagnosis of Primary Ciliary Dyskinesia: The Role of the Pediatrician. Clin Pediatr. 2017; 1 -4. Oktem S, et al. Sleep disordered breathing in patients with primary ciliary dyskinesia. Pediatr Pulmonol 2013; 48: 897 -903. Pao M and A Bosk. Anxiety in Medically Ill Children/Adolescents. Depress Anxiety. 2011; 28: 40 -9. Pifferi M et al. Health-Related Quality of Life and Unmet Needs in Patients with Primary Ciliary Dsykinesia. Eur Respir J. 2010; 35: 787 -94. © 2017
References Polsky D, et al. Long-term Risk for Depressive Symptoms After a Medical Diagnosis. Arch Intern Med. 2005; 165: 1260 -6. Rich, TA, et al. Comparison of Attitudes Regarding Preimplantation Genetic Diagnosis Among Patients with Hereditary Cancer Syndromes. Fam Cancer. 2014; 13(2)291 -99. Santamaria F, et al. Sleep disordered breathing and airway disease in primary ciliary dyskinesia. Respirology. 2014; 19: 570 -5. Schofield LM and Horobin, HE. Growing up with Primary Ciliary Dyskinesia in Bradford, UK: exploring patients experiences as a physiotherapist. Physiother Theory Pract. 2014; 30(3): 157 -64. Sha YW, Ding L, Li P. Management of primary ciliary dyskinesia/Kartagener’s syndrome in infertile male patients and current progress in defining the underlying genetic mechanism. Asian J Androl 2014; 16: 101 -6. Shapiro et al. Diagnosis, Monitoring, and Treatment of Primary Ciliary Dyskinesia: PCD Foundation Consensus Recommendations Based on State of the Art Review. Ped Pulmonol 2016; 51: 115 -132. Smith BA, Georgiopoulos AM, Quittner, AL. Maintaining Mental Health and Function for the Long Run in Cystic Fibrosis. Pediatr Pulm. 2016; DOI: 10. 1002/ppul. 23522. Smith, BA et al. Depressive Symptoms in Children With Cystic Fibrosis and Parents and Its Effects on Adherence to Airway Clearance. Pediatr Pulm. 2010; 45: 756 -63. Taelman A. , et al. Living with primary ciliary dyskinesia. Eur Respir J 2014; 44: 3676 Quittner AL, Saez-Flores E, Barton JD. The psychological burden of cystic fibrosis. Curr Opin Pulm Med. 2016; 22: 187 -91. Quittner AL, Goldbeck L, et al. Prevalence of Depression and Anxiety in Patients with Cystic Fibrosis and Parent Caregivers: results of The International Depression Epidemiological Study across nine countries. Thorax. 2014; 69: 1090 -7. Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000; 320: 569 -572. Whalley, S and Mc. Manus, IC. Living with primary ciliary dyskinesia: a prospective qualitative study of knowledge sharing, symptom concealment, embarrassment, mistrust, and stigma. BMC Pulm Med. 2006; 6: 24 © 2017

© 2017
 Tamara vance
Tamara vance Process challenge devices
Process challenge devices Psychosocial aspects of living with diabetes
Psychosocial aspects of living with diabetes Vance county water
Vance county water Lynne jones waylon jennings wife
Lynne jones waylon jennings wife Sarah s. vance
Sarah s. vance Psu factbook
Psu factbook Vance afb clinic
Vance afb clinic Urban realsm model
Urban realsm model Kendall vance model age
Kendall vance model age Vance holmes
Vance holmes Intertextual references in riptide
Intertextual references in riptide Vance kirkland paintings
Vance kirkland paintings Vance mosley
Vance mosley Eaton vance wholesaler map
Eaton vance wholesaler map Erikson's psychosocial theory of development
Erikson's psychosocial theory of development Psychosocial assessment
Psychosocial assessment Psychosocial development in early childhood
Psychosocial development in early childhood Emerging adulthood psychosocial development
Emerging adulthood psychosocial development Interdependence is a psychosocial concept
Interdependence is a psychosocial concept Define physical cognitive and psychosocial development
Define physical cognitive and psychosocial development Erickson's psychosocial theory of development
Erickson's psychosocial theory of development Erikson's psychosocial crisis
Erikson's psychosocial crisis Psychosocial approach definition
Psychosocial approach definition Biopsychosocial model of health
Biopsychosocial model of health Psychosocial module 1
Psychosocial module 1